Abstract
Multiple myeloma (MM) is a neoplastic plasma-cell disorder characterized by clonal proliferation of malignant plasma cells. Despite extensive research, disease heterogeneity within and between treatment-resistant patients is poorly characterized. In the present study, we conduct a prospective, multicenter, single-arm clinical trial (NCT04065789), combined with longitudinal single-cell RNA-sequencing (scRNA-seq) to study the molecular dynamics of MM resistance mechanisms. Newly diagnosed MM patients (41), who either failed to respond or experienced early relapse after a bortezomib-containing induction regimen, were enrolled to evaluate the safety and efficacy of a daratumumab, carfilzomib, lenalidomide and dexamethasone combination. The primary clinical endpoint was safety and tolerability. Secondary endpoints included overall response rate, progression-free survival and overall survival. Treatment was safe and well tolerated; deep and durable responses were achieved. In prespecified exploratory analyses, comparison of 41 primary refractory and early relapsed patients, with 11 healthy subjects and 15 newly diagnosed MM patients, revealed new MM molecular pathways of resistance, including hypoxia tolerance, protein folding and mitochondria respiration, which generalized to larger clinical cohorts (CoMMpass). We found peptidylprolyl isomerase A (PPIA), a central enzyme in the protein-folding response pathway, as a potential new target for resistant MM. CRISPR–Cas9 deletion of PPIA or inhibition of PPIA with a small molecule inhibitor (ciclosporin) significantly sensitizes MM tumor cells to proteasome inhibitors. Together, our study defines a roadmap for integrating scRNA-seq in clinical trials, identifies a signature of highly resistant MM patients and discovers PPIA as a potent therapeutic target for these tumors.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The scRNA-seq data were deposited at the National Center for Biotechnology Information’s Gene Expression Omnibus with accession no. GSE161195. The IA14 release of CoMMpass data was downloaded from the MMRF researcher gateway portal (https://research.themmrf.org). Source data are provided with this paper.
Code availability
Metacell source code can be found at https://github.com/tanaylab/metacell. Source code used for scRNA-seq analysis can be found at https://bitbucket.org/amitlab/multiple-myeloma-2020/.
References
Kyle, R. A. & Rajkumar, S. V. Treatment of multiple myeloma: a comprehensive review. Clin. Lymphoma Myeloma 9, 278–288 (2009).
Palumbo, A. & Anderson, K. Multiple myeloma. N. Engl. J. Med. 364, 1046–1060 (2011).
Yan, Y. et al. The impact of response kinetics for multiple myeloma in the era of novel agents. Blood Adv. 3, 2895–2904 (2019).
Nijhof, I. S., van de Donk, N. W. C. J., Zweegman, S. & Lokhorst, H. M. Current and new therapeutic strategies for relapsed and refractory multiple myeloma: an update. Drugs 78, 19–37 (2018).
Rajkumar, S. V. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am. J. Hematol. https://doi.org/10.1002/ajh.25791 (2020).
Majithia, N. et al. Outcomes of primary refractory multiple myeloma and the impact of novel therapies. Am. J. Hematol. 90, 981–985 (2015).
Cohen, Y. C. et al. Primary failure of bortezomib in newly diagnosed multiple myeloma—understanding the magnitude, predictors, and significance. Leuk. Lymphoma https://doi.org/10.3109/10428194.2015.1121258 (2016).
Corre, J. et al. Early relapse after autologous transplant for myeloma is associated with poor survival regardless of cytogenetic risk. Haematologica https://doi.org/10.3324/haematol.2019.236588 (2019).
Kumar, S. K. et al. Early relapse after autologous hematopoietic cell transplantation remains a poor prognostic factor in multiple myeloma but outcomes have improved over time. Leukemia 32, 986–995 (2018).
Kastritis, E. et al. Early relapse post autologous transplant is associated with very poor survival and identifies an ultra high risk group of myeloma patients. Clin. Lymphoma Myeloma Leuk. https://doi.org/10.1016/j.clml.2019.10.014 (2020).
van de Donk, N. W. C. J. et al. Treatment of relapsed and refractory multiple myeloma in the era of novel agents. Cancer Treatment Rev. 37, 266–283 (2011).
Wallington-Beddoe, C. T. & Coghlan, D. W. Resistance Mechanisms to Novel Therapies in Myeloma. in Update on Multiple Myeloma (ed., K. Ahmed Al-Anazi) (IntechOpen, 2019). https://doi.org/10.5772/intechopen.77004
Krishnan, S. R., Jaiswal, R., Brown, R. D., Luk, F. & Bebawy, M. Multiple myeloma and persistence of drug resistance in the age of novel drugs (Review). Int. J. Oncol. 49, 33–50 (2016).
Niewerth, D. et al. Molecular basis of resistance to proteasome inhibitors in hematological malignancies. Drug Resist. Update 18, 18–35 (2015).
Harding, T., Baughn, L. & Kumar, S. & Van Ness, B. The future of myeloma precision medicine: integrating the compendium of known drug resistance mechanisms with emerging tumor profiling technologies. Leukemia 33, 863–883 (2019).
Papadas, A. & Asimakopoulos, F. Mechanisms of Resistance in Multiple Myeloma. Handb. Exp. Pharmacol. 249, 251–288 (Springer, 2018).
Nikesitch, N. & Ling, S. C. W. Molecular mechanisms in multiple myeloma drug resistance. J. Clin. Pathol. 69, 97–101 (2016).
Narayanan, S. et al. Targeting the ubiquitin-proteasome pathway to overcome anti-cancer drug resistance. Drug Resist. Update 48, 100663 (2020).
Vincenz, L., Jäger, R., O’Dwyer, M. & Samali, A. Endoplasmic reticulum stress and the unfolded protein response: targeting the Achilles heel of multiple myeloma. Mol. Cancer Therapeut. 12, 831–843 (2013).
Ling, S. C. W. et al. Response of myeloma to the proteasome inhibitor bortezomib is correlated with the unfolded protein response regulator XBP-1. Haematologica 97, 64–72 (2012).
Klein, A. M. & Treutlein, B. Single cell analyses of development in the modern era. Development https://doi.org/10.1242/dev.181396 (2019).
Ledergor, G. et al. Single cell dissection of plasma cell heterogeneity in symptomatic and asymptomatic myeloma. Nat. Med. 24, 1867–1876 (2018).
Kawano, Y. et al. Targeting the bone marrow microenvironment in multiple myeloma. Immunol. Rev. 263, 160–172 (2015).
Cohen, M. et al. Lung single-cell signaling interaction map reveals basophil role in macrophage imprinting. Cell 175, 1031–1044.e18 (2018).
Medaglia, C. et al. Spatial reconstruction of immune niches by combining photoactivatable reporters and scRNA-seq. Science 358, 1622–1626 (2017).
Baran, Y. et al. MetaCell: analysis of single-cell RNA-seq data using K-nn graph partitions. Genome Biol. 20, 206 (2019).
Bergsagel, P. L. et al. Cyclin D dysregulation: an early and unifying pathogenic event in multiple myeloma. Blood 106, 296–303 (2005).
Zhan, F. et al. The molecular classification of multiple myeloma. Blood 108, 2020–2028 (2006).
Khan, R. et al. Four genes predict high risk of progression from smoldering to symptomatic multiple myeloma (SWOG s0120). Haematologica 100, 1214–1221 (2015).
Decaux, O. et al. Prediction of survival in multiple myeloma based on gene expression profiles reveals cell cycle and chromosomal instability signatures in high-risk patients and hyperdiploid signatures in low-risk patients: a study of the Intergroupe Francophone du Myélome. J. Clin. Oncol. 26, 4798–4805 (2008).
Shaughnessy, J. D. et al. A validated gene expression model of high-risk multiple myeloma is defined by deregulated expression of genes mapping to chromosome 1. Blood 109, 2276–2284 (2007).
Shaughnessy, J. D. et al. Pharmacogenomics of bortezomib test-dosing identifies hyperexpression of proteasome genes, especially PSMD4, as novel high-risk feature in myeloma treated with total therapy 3. Blood 118, 3512–3524 (2011).
Jakubowiak, A. J. et al. Daratumumab (DARA) in combination with carfilzomib, lenalidomide, and dexamethasone (KRd) in patients (pts) with newly diagnosed multiple myeloma (MMY1001): an open-label, phase 1b study. J. Clin. Oncol. 35, 8000 (2017).
Landgren, O. et al. Bone marrow-based and longitudinal blood-based MRD tracking in newly diagnosed multiple myeloma patients treated with daratumumab, carfilzomib, lenalidomide and dexamethasone (DKRd): a correlative and clinical phase II study. Blood 132, 3281 (2018).
Chari, A. et al. Daratumumab (DARA) in combination with carfilzomib, lenalidomide, and dexamethasone (KRd) in patients with newly diagnosed multiple myeloma (MMY1001): updated results from an open-label, phase 1b study. Blood 130, 3110 (2017).
Van De Donk, N. W. C. J. & Usmani, S. Z. CD38 antibodies in multiple myeloma: mechanisms of action and modes of resistance. Front. Immunol. 9, 2134 (2018).
Krejcik, J. et al. Daratumumab depletes CD38+ immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood 128, 384–394 (2016).
Robak, P., Drozdz, I., Szemraj, J. & Robak, T. Drug resistance in multiple myeloma. Cancer Treat. Rev. 70, 199–208 (2018).
Tsvetkov, P. et al. Mitochondrial metabolism promotes adaptation to proteotoxic stress. Nat. Chem. Biol. 15, 681–689 (2019).
Greaves, M. & Maley, C. C. Clonal evolution in cancer. Nature 481, 306–313 (2012).
Keats, J. J. et al. Clonal competition with alternating dominance in multiple myeloma. Blood 120, 1067–1076 (2012).
Khoo, W. H. et al. A niche-dependent myeloid transcriptome signature defines dormant myeloma cells. Blood 134, 30–43 (2019).
Nigro, P., Pompilio, G. & Capogrossi, M. C. Cyclophilin A: a key player for human disease. Cell Death Dis. 4, e888–e888 (2013).
Kyu, J. C. et al. Overexpressed cyclophilin A in cancer cells renders resistance to hypoxia- and cisplatin-induced cell death. Cancer Res. 67, 3654–3662 (2007).
Matsuda, S. & Koyasu, S. Mechanisms of action of cyclosporine. Immunopharmacology 47, 119–125 (2000).
Nikesitch, N., Lee, J. M., Ling, S. & Roberts, T. L. Endoplasmic reticulum stress in the development of multiple myeloma and drug resistance. Clin. Transl. Immunol. 7, e1007 (2018).
Lee, J. & Kim, S. S. An overview of cyclophilins in human cancers. J. Int. Med. Res. 38, 1561–1574 (2010).
Jaitin, D. A. et al. Massively parallel single-cell RNA-seq for marker-free decomposition of tissues into cell types. Science 343, 776–779 (2014).
Paul, F. et al. Transcriptional heterogeneity and lineage commitment in myeloid progenitors. Cell 163, 1663–1677 (2015).
Keren-Shaul, H. et al. A unique microglia type associated with restricting development of Alzheimer’s disease. Cell 169, 1276–1290.e17 (2017).
Klages, N., Zufferey, R. & Trono, D. A stable system for the high-titer production of multiply attenuated lentiviral vectors. Mol. Ther. 2, 170–176 (2000).
Kumar, S. et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 17, e328–e346 (2016).
Acknowledgements
We thank the following: the patients and their families; the clinical study research teams across all participating sites; the clinical research associates, L. Poor Porges, S. Shaibi and Y. Piltz; N. Lowenton-Spier for managing the study team; K. Bjorklof and F. Suzan from Amgen and A. Grossman from Medison for their support in the setup of the clinical trial; and A. Giladi for a review of the manuscript. We thank T. Wiesel from the Scientific Illustration unit of the Weizmann Institute for artwork, and members of the I. Amit’s lab for fruitful discussions. Extended Data Figs. 4d and 9a were created using BioRender.com. I. Amit is an Eden and Steven Romick Professorial Chair, supported by Merck KGaA, Darmstadt, Germany, the Chan Zuckerberg Initiative, the ISF Israel Precision Medicine Program (IPMP; 607/20, grant no. P128245), the HHMI International Scholar award, the European Research Council Consolidator Grant (ERC-COG; grant no. 724471, HemTree2.0), an SCA award of the Wolfson Foundation and Family Charitable Trust, the Thompson Family Foundation, an MRA Established Investigator Award (no. 509044), the Israel Science Foundation (703/15), the Ernest and Bonnie Beutler Research Program for Excellence in Genomic Medicine, the Helen and Martin Kimmel award for innovative investigation, the NeuroMac DFG/Transregional Collaborative Research Center Grant, an International Progressive MS Alliance/NMSS PA-1604 08459, Dan and Betty Kahn Foundation and an Adelis Foundation grant. Y.C. received an investigator-initiated research grant from Amgen for the present study (AMGEN IIS grant protocal KRD-OW-TA009; REF#20167107). S.-Y.W. is an EMBO long‐term fellow (ALTF 263‐2018) and received the NWO Rubicon award (019.181EN.038).
Author information
Authors and Affiliations
Contributions
Y.C, M.Z., A.W., S.-Y.W. and I. Amit conceived and designed the study. M.Z. performed flow cytometry sorting experiments and other experiments. A.W. and S-Y.W. designed and performed single-cell bioinformatic analyses. Y.C. and I. Avivi collected clinical data and participant samples and supervised the clinical trial. C.B. and M.Z performed in vitro CRISPR experiments. E.L. analyzed clinical data using SPSS. Y.C, M.Z., A.W., S.-Y.W. and I. Amit generated the figures and wrote the manuscript. I. Amit supervised the project. All authors critically reviewed and approved the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The clinical trial was an investigator-initiated study (IIS); as such, Y.C. acted as sponsor for the study. The IIS was approved by Amgen, who provided funding and supply of the clinical drug CFZ. Y.C. is a consultant for Janssen, Amgen, Neopharm, Takeda and Madison. A patent application has been filed related to this work. The other authors declare no competing interests.
Additional information
Peer review information Javier Carmona was the primary editor on this article, and managed its editorial process and peer review in collaboration with the rest of the editorial team. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Sorting strategy of plasma cells and overview single cell data collection from the patients.
a-c, Flow cytometry plots showing sorting strategy (CD38+CD138+) for plasma cells after doublet exclusion from 3 representative patients. Plots were generated using FlowJo software. (Methods). d, Schematic diagram showing the statists of patient enrollment to KYDAR clinical trial and their current status.
Extended Data Fig. 2 Overview of quality control and data analysis for the single bone marrow plasma cells.
a, Dot plots showing number of reads, number of UMIs, and percentage of cells analyzed per batch of 384 cells (that were pooled for library construction) for all CD38+CD138+ bone marrow single cells from 66 participants (11 control donors, 15 NDMM patients, and 40 PRMM patients). (Methods). b, Heat map showing clustering analysis of 3,862 ‘contamination’ cells that pass quality control but do not express key plasma genes. Shown are representative genes of non-PC. c, Heat map showing clustering analysis of 51,297 PC sorted from all the 66 participants featuring normalized single cell expression levels of a selected set of most variable genes. Clustering is performed using 2,038 genes as features. d, Heat maps showing clustering analysis of PC from patient KYDAR 21 (left) together with the same number of PC from healthy control group (right) using 1,393 gene features.
Extended Data Fig. 3 The robustness of differential expression z-score.
a, comparison of standard log2 fold change vs. our z-score for patient KYDAR 24 clone 1 relative to healthy control. Size of the dots corresponds to the mean expression (UMIs) in the healthy control samples. b, Scatter plot showing the -log10 p-value from the two-sided Mann-Whitney test and the z-score. c, scatter plot comparing our z-score to variance/mean showing no clear bias with high z-score and cell-cell variability. d, z-score scatter plots comparing different sub-sampling of cells (100, 400 and 800 cells). e, z-score scatter plots comparing different sub-sampling of UMIs per cell (300, 400 and 500 cells). f, The distribution of the z-score from patient KYDAR 24.
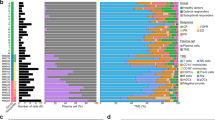
Extended Data Fig. 4 Differential expression and functional enrichment analyses comparing NDMM and PRMM patients.
a, Volcano plot showing a selected set of differential genes between NDMM and PRMM patients. X axis showing the difference between the average z-score of NDMM patients and PRMM patients; Y axis showing the -log10 p-value from a bootstrap test using t-statistic (Methods). b, Heat map showing the correlation map of all the differential genes identified between the NDMM and PRMM patients. Genes are clustered using hierarchical clustering. c, Functional enrichment of the 3 gene modules using Metascape. d, Graphical illustration of non-responder overall PI resistant pathway.
Extended Data Fig. 5 Clinical response to DARA-KRD treatment.
a, Distribution of international myeloma working group (IMWG) response grades in KYDAR trial. b, Waterfall plot shows the best overall responses according to the IMWG in MM. c,d, Kaplan-Meir curve showing the progression free survival (panel c) and overall survival (panel d) of PRMM patients treated with DARA-KRD.
Extended Data Fig. 6 Differential expression analysis of DARA-KRD resistant patients.
a, Volcano plot showing a selected set of differential genes between PRMM responder group and PRMM non-responder group. X axis showing the difference between the average z-score of PRMM responder group and PRMM non-responder group; Y axis showing the log10 p-value from a bootstrap test using t-statistic (Methods). b, Scatter plot on the left showing the overlap between gene module 1 in Fig. 2a and resistance signature 1 in Fig. 4a. X axis showing the difference between the average z-score of NDMM patients and PRMM patients; Y axis showing the difference between the average z-score of PRMM responder group and PRMM non-responder group. Scatter plot on the right showing the same as the left one, but for gene module 3 and resistance signature 2. c, Venn diagram showing the overlap between the PRMM patient groups classified in Fig. 2a and PRMM responder and non-responder groups.
Extended Data Fig. 7 Longitudinal data collection of PRMM patients.
a, Representative flow cytometry plots showing sorting strategy (CD38+CD138+) for post treatment patients’ plasma cells after doublet exclusion, same as in Extended Data Fig. 1a, but for the samples from patient KYDAR 10 after 4 cycles DARA-KDR treatment. b, Same as in panel a, but for patient KYDAR 10 after 10 cycles DARA-KDR treatment. c, Heat map depicting the relative frequency of the immunoglobulin sequences for each clone (including 11 control donor and 15 newly diagnosed patients); left, bottom, immunoglobulin heavy chain constant region (IGHC); middle, immunoglobulin light chain constant region (IGKC and IGLC); right, immunoglobulin light chain variable region (IGKV and IGLV).
Extended Data Fig. 8 Longitudinal single cell analysis of MM patients pre- and post-treatment.
a, Upper part showing 2D projection of malignant PC of patient KYDAR 21, including healthy PC as reference, highlighting all cells (left), cells collected from baseline (middle left), cells collected from Cycle 4 (middle right), cells collected from Cycle 10 (right). The color of the cells represents healthy PC, and malignant clone 1, 2, and 3. Lower part showing 2D projection of expression of a selected set of differential genes over the metacell model. b, Heatmap showing clone composition in each sample from the patient KYDAR 21 and expression of selected differential genes in each clone. (c) and (d) showing the same as panel (a) and (b), but for patients KYDAR 34 with corresponding samples and clones. (e) and (f) showing the same as panel a and b, but for patients KYDAR 30 with corresponding samples and clones. g, The dynamics of S100A11 (left) and S100A10 (right) expression in individual patients during DARA-KRD treatment.
Extended Data Fig. 9 CsA potentiates Carfilzomib and induced cell death in myeloma cell lines.
a, Graphical illustration of PRMM non-responder resistant pathway, highlighting PPIA. b, Bar plots showing normalized RNAseq PPIA gene transcription in MM cell lines, highlighted in red lines – RPMI-8226 and U266 cell lines (Methods). c, Barplot showing PPIA mRNA levels measured by qPCR in RPMI-8226 PPIA+/+ and PPIA-/-. d, Western blot of PPIA protein levels in RPMI-8226 PPIA+/+ and PPIA-/- cell lines. Shown are cropped western blots of PPIA protein levels in RPMI-8226 PPIA+/+ and PPIA-/- cell lines (tubulin is used as control). Full image can be found in raw data section. Western Blot experiment was conducted once with 3 successful replicates per cell line group. e, Dose-response curves to determine the half maximal inhibitory concentrations (IC50) of CsA in RPMI-8226 and U266 cell lines (Methods). The dose-response curves and IC50 values were determined by a non-linear regression fit. Results are shown as the mean±SEM (Standard Error of the Mean) of 3 independent experiments. f, Immunofluorescence staining of RPMI 8226 (upper) and U266 (lower) cell lines post treatment with Carfilzomib or in combination with CsA for 48 h. DAPI (Blue) staining for control live cells, Propidium Iodide (Red) staining for late apoptosis (death), FITC (Green) staining for early apoptosis, and merged gate showing all staining. Representative images from two independent experiments are shown. g, Dose-response curves to determine the half maximal inhibitory concentrations (IC50) of CsA in RPMI-8226 PPIA+/+ and PPIA-/- cell lines (Methods). Results are shown as the mean±SEM (Standard Error of the Mean) of 3 independent experiments.
Extended Data Fig. 10 Cyclosporin A, known inhibitor for PPIA shown synergistic effect with the proteasome inhibitor carfilzomib.
a, Representative flow cytometry plots showing sorting strategy for single RPMI-8226 cells. b, 2D projection showing metacell analysis of scRNA-seq of RPMI-8226 cells during CsA, CFZ, and CFZ+CsA treatment at 4 h and 8 h. Different cell states are indicated by colors. c, 2D projection showing the distribution of the cells (down sampled to 299 cells) in each sample over the metacell map in panel b. d, heatmap showing z-score of differentially expressed genes in each cell state. e, gene ontology enrichment of the 115 up regulated genes and 78 down regulated genes. f, Heatmap depicting the z-score of resistance signature 1 and 2 (Fig. 4a) genes in 15 NDMM, 21 PRMM responder, and 7 PRMM non-responder patients, together with ex-vivo cells of one highly resistant PRMM patient Z01. g, barplot showing scores of resistance signature 1 in 15 NDMM, 21 PRMM responder, and 7 PRMM non-responder patients, together with one resistant PRMM patient Z01. h, barplot showing Z-scores of PPIA expression in the same NDMM and PRMM patients in panel g, together with the resistant PRMM patient Z01.
Supplementary information
Supplementary Table 1
Description of patients and single-cell data included in the present study.
Supplementary Table 2
The z-score values for each transcriptional clone in individual MM patients.
Supplementary Table 3
Safety and tolerability.
Supplementary Table 4
Multivariate analysis for KYDAR and CoMMpass patients.
Supplementary Table 5
Differential expression analysis of responders versus nonresponder PRMM patients.
Supplementary Table 6
The scRNA-seq analysis of RPMI-8226 treated with CFZ, CsA and their combination, 4 and 8 h post-treatment.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 9
Statistical source data and western blots.
Source Data Extended Data Fig. 10
Statistical source data.
Rights and permissions
About this article
Cite this article
Cohen, Y.C., Zada, M., Wang, SY. et al. Identification of resistance pathways and therapeutic targets in relapsed multiple myeloma patients through single-cell sequencing. Nat Med 27, 491–503 (2021). https://doi.org/10.1038/s41591-021-01232-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-021-01232-w
This article is cited by
-
Robust detection of clinically relevant features in single-cell RNA profiles of patient-matched fresh and formalin-fixed paraffin-embedded (FFPE) lung cancer tissue
Cellular Oncology (2024)
-
PERCEPTION predicts patient response and resistance to treatment using single-cell transcriptomics of their tumors
Nature Cancer (2024)
-
Single-cell multiomic dissection of response and resistance to chimeric antigen receptor T cells against BCMA in relapsed multiple myeloma
Nature Cancer (2024)
-
An ICD-Associated DAMP Gene signature predicts survival and immunotherapy response of patients with lung adenocarcinoma
Respiratory Research (2023)
-
A novel necroptosis signature for predicting survival in lung adenocarcinoma
BMC Medical Genomics (2023)