Abstract
Access to healthcare is a requirement for human well-being that is constrained, in part, by the allocation of healthcare resources relative to the geographically dispersed human population1,2,3. Quantifying access to care globally is challenging due to the absence of a comprehensive database of healthcare facilities. We harness major data collection efforts underway by OpenStreetMap, Google Maps and academic researchers to compile the most complete collection of facility locations to date. Leveraging the geographically variable strengths of our facility datasets, we use an established methodology4 to characterize travel time to healthcare facilities in unprecedented detail. We produce maps of travel time with and without access to motorized transport, thus characterizing travel time to healthcare for populations distributed across the wealth spectrum. We find that just 8.9% of the global population (646 million people) cannot reach healthcare within one hour if they have access to motorized transport, and that 43.3% (3.16 billion people) cannot reach a healthcare facility by foot within one hour. Our maps highlight an additional vulnerability faced by poorer individuals in remote areas and can help to estimate whether individuals will seek healthcare when it is needed, as well as providing an evidence base for efficiently distributing limited healthcare and transportation resources to underserved populations both now and in the future.
Similar content being viewed by others
Main
Access to healthcare is a measure of human well-being that is constrained by numerous geographically varying factors1,2,3, the most immediate of which is the time it takes individuals to travel to a properly equipped and adequately staffed healthcare facility. Due to spatial clustering of healthcare facilities in densely populated areas, individuals living in rural regions often face increased travel times and thus cost when seeking healthcare. This situation can be exacerbated by poor transportation infrastructure and lack of motorized transport, which further increase the time required for travel and could disproportionally affect lower-income populations. As such, people facing long travel times to healthcare facilities are less likely to seek care when it is needed5,6,7,8,9, and the consequences of failing to seek care include increased mortality and morbidity from treatable conditions10,11.
Effectively characterizing travel time can assist in identifying communities that would most benefit from additional healthcare resources. These resources include outreach programs, community healthcare workers, subsidized transportation, telemedicine, transfer of trained personnel to short-staffed facilities and optimally placed future facilities. Providing medical care to communities located in rural or remote areas is critical for ensuring health equity for populations that are often underserved due to a lack of skilled healthcare workers12. Within this context, maps of travel time to healthcare facilities provide a valuable resource for policymakers tasked with allocating personnel and resources to improve health outcomes. The main findings, limitations and policy implications of this work are summarized in Table 1.
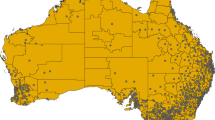
Previous studies on travel time to healthcare facilities13,14,15,16,17 provided the conceptual foundation for the current study, but these could not extend beyond localized or regional analyses without a suitable global dataset of healthcare facilities. We overcame this obstacle by leveraging multiple continental-to-global-scale datasets, which also helped to mitigate challenges associated with inconsistent data quality between countries and between public and private health sector data sources. Geographic locations of hospitals and clinics were acquired from Google Maps (https://www.google.com/maps/), OpenStreetMap (OSM; https://www.openstreetmap.org/) and other published sources18,19, which were combined to create a global map (with a spatial resolution of 1 km × 1 km) in which 376,231 pixels contained one or more facilities (Extended Data Fig. 1). Among the sources, Google and OSM were global in scope and included a mixture of public and private facilities, while the published datasets were continental-scale data for Australia18 and Africa19, containing primarily public facilities. We then used an established methodology4,20 to create maps of travel time for individuals with and without access to motorized transportation. For this process, we first updated global ‘friction surfaces’ containing the estimated time required to traverse each pixel with and without using motorized transportation. The friction surfaces were derived from a variety of geospatial datasets, the most important of which were roads location data from OSM and Google and road speed data from OSM (Supplementary Table 1). Lastly, we used a least-cost-path algorithm to create maps of travel time to the nearest healthcare facility (Methods).
The global map of optimal travel time to a hospital or clinic (Fig. 1) illustrates the spatial heterogeneity of geographically constrained healthcare access experienced by individuals with access to motorized transportation.
The walking-only map of travel time to healthcare facilities (Fig. 2) shows similar spatial patterns but with far longer travel times for rural areas, thus highlighting a stark reality for rural populations in need of healthcare but without access to motorized transportation. Hospitals and clinics are typically located in densely populated areas, thus supplying the local demand for healthcare. As such, while the broad patterns evident in our maps are similar to those within the map of travel time to cities4, the maps of travel time to healthcare are much more nuanced due to the comparatively large number and wide spatial distribution of healthcare facilities.
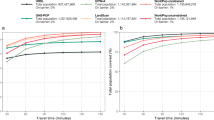
By intersecting the maps of travel time with a gridded population surface, we quantified the proportional travel times to hospitals and clinics for the global population relative to each facility location dataset, as well as for the combined facility dataset (Fig. 3). With access to motorized transportation, 60.3% of the Earth’s population lives within 10 min of a hospital or clinic, while 82.6% and 91.1% live within 30 and 60 min, respectively. These percentages correspond to 4.39, 6.02 and 6.64 billion people, respectively. These results suggest that the spatial coverage of healthcare facilities is very good in most regions for individuals with access to the fastest means of transportation. By contrast, the walking-only results show that just 14.2%, 39.8% and 56.9% (1.19, 2.86 and 4.13 billion) of people live within 10, 30 and 60 min, respectively, of a healthcare facility when traveling by foot. The disparity between motorized and nonmotorized travel times illuminates a potential causal association between individuals’ decisions on whether to seek healthcare and their available modes of transportation. Furthermore, because a lack of financial resources could constrain an individual’s transportation options, as well as their ability to pay for healthcare, wealth and travel time to a healthcare facility are intrinsically linked and combine to influence whether individuals seek healthcare when it is needed2,3,21. While we present a dichotomy of people either moving at the optimal speed or having to walk to healthcare facilities, in reality large numbers of people will fall between these estimates if, for example, their journeys combine walking and public transport. Furthermore, the urgency of individual healthcare needs will affect their choice of transportation mode and being unwell could increase travel times.
The completeness and accuracy of the healthcare facility dataset vary by country (Supplementary Table 2) and are important limitations of this analysis that should be considered when interpreting the maps. Despite using the best available data, the constituent healthcare facility datasets, and hence the combined dataset, were susceptible to errors of omission, could be outdated as a consequence of facilities opening or closing and might contain incorrect facility locations. These concerns provide the rationale for only including datasets that were published in 2019 and, in the cases of Google Maps and OSM data, are frequently updated products with robust quality controls. Although the quality of the healthcare facility dataset could not be fully ascertained, technical validation showed that the travel time estimates derived from the friction surface were generally accurate4,22, with the caveat that they did not account for daily or seasonal variability in travel times or factors such as delays in journeys incurred while waiting for public transportation. Similarly, the facility location data are not temporally dynamic and thus do not reflect when facilities are open but understaffed, closed for nights, weekends, holidays or closed seasonally or permanently.
Additional limitations of the maps of travel time relate to whether individuals receive care at their closest facility. First among these considerations is that an individual who is capable of physically reaching a healthcare facility cannot necessarily receive care at that facility if, for example, the cost of care is prohibitive for the patient23. Second, all hospitals and facilities do not offer the same services, such as emergency care, and travel times to more specialized services could be much greater than our maps indicate. As such, the provided maps are not a universally applicable assessment of healthcare access in all circumstances, but are indicative of access only to basic services, such as care provided by a general practitioner or trained nurse. Third, our maps of travel time to healthcare provide estimates of potential rather than actual travel times to healthcare, because although individuals have a propensity for choosing the closest facility24, they could choose to seek healthcare from facilities farther from home. Addressing the disparity between potential and actual travel time to healthcare is a priority for future research. Such research is now feasible due to advances in the quality and availability of empirical human movement data such as user locations logged by GPS-equipped smartphones and collated by technology companies. Finally, our research focuses exclusively on the location of geographically fixed facilities and ignores the potential use of mobile or temporary clinics for providing healthcare in remote areas.
Despite these limitations, the maps of global travel time to hospitals and clinics highlight areas most in need of additional healthcare facilities, and thus could be used to assess the adequacy of healthcare provision, optimally position new facilities and allocate funding toward subsidized transportation or telemedicine to communities most in need. Our results could also benefit travelers, as specialists in some countries use access to healthcare to determine whether to issue standby emergency treatments to individuals who will be in areas far from facilities. Furthermore, we freely provide the friction surfaces and the travel time mapping code; thus, our approach can readily be used to produce custom maps of travel time, such as those for specific healthcare services like pediatric emergency care25. Additionally, the underlying approach we developed can be adapted for new applications such as assessing disease outbreak preparedness26 or helping to define healthcare facility catchment areas. Our maps are also useful for estimating healthcare treatment-seeking behavior of individuals, which declines with increased travel time and is also affected by access to motorized transport (Extended Data Fig. 2). Improved characterization of healthcare seeking is critical because individuals failing to seek care face an increased risk of death from treatable conditions, and thus this metric is a much-needed predictor in datasets for modeling mortality27. Lastly, by creating the walking-only map, we provide a means of highlighting regions in which individuals lacking resources for motorized transport are particularly disadvantaged in their ability to seek healthcare.
To our knowledge, the maps of travel time to hospitals and clinics are the first, global-scale, high-resolution maps of this critical healthcare accessibility metric yet published. As such, the maps have the potential to make substantial contributions to the public health and epidemiological research communities by providing estimates for the time required to reach healthcare from every inhabited region on Earth. By combining the strengths of multiple healthcare facility data sources, this project demonstrates the power of data amalgamation for creating outputs that were, until recently, prohibitively expensive and time consuming to make. However, because the results of this work are contingent upon the accuracy of hospital and clinic locations, this project also represents a call for action to improve the quality, consistency, completeness and availability of healthcare facility data globally.
Methods
Facility data
Until recently, large and comparable datasets of healthcare facility locations have been rare, and even the most comprehensive sources continue to have geographically heterogeneous levels of data quality and completeness. To mitigate these limitations, we used healthcare facility location data from two of the largest global databases: (1) OSM data that was collated and made available for download at https://www.healthsites.io/28 and (2) data from Google Maps that was extracted specifically for this project. We augmented the global datasets with continental-scale facility locations that were recently published for Africa19 and Australia18. To align temporally, each of these datasets was extracted in mid-2019. To facilitate comparisons between data sources, we used only facilities defined as hospitals and clinics, which matched the definition used in the published datasets18,19 and was distinguishable within the OSM data by using the facility-type attribute. In contrast, Google Maps data were filtered to isolate hospitals and clinics from the full set of geolocated entities. For each dataset, multiple points found within the same ~1 km × 1 km pixel were merged to match the resolution of the subsequent maps of travel time. The resulting counts of pixels containing one or more hospitals or clinics, by data source, were 201,799 from Google Maps, 148,522 from OSM and 87,402 from the published sources18,19. Maps of travel time were prepared for each set of healthcare facility pixels and then combined to form the final travel time map, in which a total of 376,231 pixels contained one or more hospitals or clinics. A sensitivity analysis confirmed that slight spatial misalignments were not responsible for the differences between the facility databases. As such, the lack of agreement between the data sources (Extended Data Fig. 1) suggests that they vary considerably in their completeness from country to country, or they capture fundamentally different segments of healthcare systems such as public versus private facilities. For example, the published data for Africa19 contains primarily public facilities, while OSM and Google are a mixture of both data types. Finally, because the published data are not global in scale, the implication of Extended Data Fig. 1 is that the Google data lack many of the hospitals and clinics in the focal areas of the published results (Africa in particular).
The healthcare facility location points used for this research were obtained from Google Maps, OSM and recently published healthcare facility datasets18,19. The OSM dataset is a global extraction of healthcare facilities collated and distributed by https://www.healthsites.io/. OSM is a collaborative project designed to create a free and editable geospatial database of the whole world. OSM is one of the most successful examples of a volunteered geographic information project29. OSM is built by a large user community that uses aerial imagery, GPS devices and low-tech field maps to verify that OSM is accurate and up to date. By February 2020, the project had more than 6 million registered users, while the number of contributors was 1.4 million. OSM follows the peer production model that created Wikipedia; intrinsic within this model are three approaches to ensure data quality: crowdsourcing, social and geographic30. A considerable number of scientific studies have evaluated different data quality elements of OSM data31,32,33,34,35,36,37, including completeness, logical consistency, positional accuracy, temporal accuracy and thematic accuracy38. Overall, these studies agree that different quality elements show heterogeneous patterns across space, and that dense areas with a high number of OSM contributors assessed have higher accuracy and completeness than rural areas. However, these studies do not attempt to define minimum acceptable levels of quality for geographic data, suggesting that OSM data may have different degrees of suitability for specific purposes. In the case of geospatial features representing health facilities, the Global Healthsites Mapping Project (https://www.healthsites.io/)28 provides a domain-specific view of OSM data, focusing on health facility data. The healthsites.io platform integrates OSM data with several databases from trusted partners. To enhance the reliability of health facilities data, healthsites.io performs manual and automated processes to assess the quality of data through a validity index, for example, calling the facilities by telephone and comparing the street address associated with the facilities with the corresponding address returned by external geocoding services, respectively.
Hospitals and clinics that were open in August 2019 were extracted from the full set of geolocated places within Google Maps. The set of hospitals and clinics was derived based on a proprietary ontology of geographic entities and a coarse classification relying on estimates produced by machine-learning models. Facilities were retained if they were broadly categorized as hospitals, clinics or facilities providing urgent or emergency medical care with an entry subtype indicating they were a hospital or clinic. The underlying sources of the geolocated entities within Google Maps included publicly available data, licensed third-party data and data contributed by users39. Publicly available and third-party data may be associated with dataset-specific metadata that describe their accuracy and completeness, and, as with OSM, users of Google Maps can flag and report potential errors.
The published dataset for Africa19 contained healthcare facilities created through a multiyear project that collated publicly available data (for example, from online repositories) and data obtained via personal communication with researchers and officials from numerous countries. All facilities without coordinates were manually name matched to known geographic locations by, for example, searching for place names within Google Maps. The Africa dataset was limited to facilities defined as hospitals or clinics and, with the exception of Botswana, included only public facilities. The published hospitals and clinics dataset for Australia18 consisted of a mixture of public and private hospitals from an inventory distributed by the Australian Institute of Health and Welfare.
The set of facility locations from Google Maps was used to generate source-specific maps of travel time, which were later merged (using a minimum function) with similar maps of travel time made from the OSM and published facility locations. The OSM and published facility points were downloaded from their repositories and only marginally modified from their original forms. The only changes consisted of removing any points that lacked spatial coordinates, had coordinates of 0° latitude and 0° longitude, were otherwise erroneously located in the ocean or were located outside the analysis window (for example, two points in Antarctica). In cases where multiple facilities were found within single pixels, or where a facility was in multiple datasets, the points were effectively merged such that the pixel was considered a single source location of healthcare.
Travel time mapping
The first method for modeling travel time globally was established by Nelson20 and substantially improved upon by Weiss et al. 4. This approach was predicated on the creation of friction surfaces that quantified the time required to traverse each pixel within a ~1 km × 1 km gridded representation of the Earth’s surface. The movement rates encapsulated within the friction surfaces were based on landscape characteristics and transportation infrastructure, and no individual movement data were used to create them. The friction surfaces were made by combining geographic datasets that each characterized a layer-specific cost of moving through the landscape4. These datasets consisted of roads, railways, navigable waterways, bodies of water, land cover types, topographic conditions (elevation and slope angle) and national borders. Descriptions of these datasets and their associated processing steps are provided in Weiss et al. 4. Note, however, that we did not consider air travel in this analysis.
As people typically take the path of least resistance when traveling, the route calculated to the most accessible healthcare facility typically relied on road networks for a large portion of the journey distance. As such, the road layers used to derive the friction surfaces were the most critical inputs for overall model accuracy. The roads datasets used for this project were the OSM and Google Roads datasets. Firstly, OSM roads data were extracted in October 2019 and converted into a rasterized surface of road types whereby the fastest road type in each pixel took precedence. In a second processing step, the OSM data were analyzed to determine the median speed limit value for each road type in each country (Supplementary Table 1). These values were subsequently used to attribute road speeds to specific pixels using a lookup table. In cases where a road type was present in a country, but associated speed limit information was unavailable, a global average speed limit for that road type was used instead. The Google roads data consisted of a distance to road layer, which effectively became a rasterized roads surface by defining all pixels with distance values of less than 500 m as roads. Because the OSM data were split by road type for which we had speed limit information, these roads data took precedence when both datasets indicated the existence of a road within a pixel. In cases where only Google roads data indicated the presence of a road, those pixels were assigned the generic ‘road’ classification for the purposes of assigning speed limits via the lookup tables. While the approach for making the friction surface was identical to the one used in earlier research4, reanalysis was warranted because substantial additions have since been made to OSM. These changes included the addition of many previously missing roads, particularly in developing countries, and far more comprehensive speed limit information to support country-specific road speed attribution.
Travel times were calculated to the nearest geolocated hospital or clinic. A critical assumption of the travel time calculations, however, was that people moved through the landscape at an optimal speed. In reality, factors such as wealth and the availability of public transportation affect individuals’ decisions on when and how to travel to obtain healthcare, thereby preventing segments of the population from moving this quickly. To account for this aspect of human movement, we also created a walking-only variant of the friction surface. In the optimal friction surface, we assumed that humans traveling along roadways, railways and on water moved at the motorized movement rates assigned to each type. In the walking-only friction surface, we assumed that all road travel was limited to a walking speed of 5 km per hour, and all water travel was reduced to the rate for traversing a wetland or swimming of 1 km per hour. The walking-only friction provided an upper bound of movement rates for individuals who lack access to or cannot use motorized transport. Examples of factors preventing the use of motorized transport include roads being impassible due to natural disasters or the presence of travel restrictions such as those put in place in response to the 2020 coronavirus pandemic. It should be noted, however, that in scenarios where emergency healthcare is required (for example, when someone is injured and incapacitated), even the walking-only estimates may be too optimistic unless transportation assistance such as an ambulance service is available. Lastly, only optimal and walking-only maps were produced because only they could be reasonably parameterized at a global scale. In reality, individuals travel using a variety of modes of transportation that move at a range of speeds, and even those able to travel by motorized vehicle may not be able to do so immediately. As such, understanding the prevalence of varying modes of transportation, as well as their speeds, is critical for contextualizing local travel times within the upper and lower bounds provided by our maps. Likewise, the modes of transportation and routes of transport that individuals use can shift over time as people respond to changing conditions, such as seasonal flooding. Each of these topics warrants additional study, albeit for smaller geographic areas where highly localized conditions, dynamics and adaptations can be adequately characterized.
A least-cost-path algorithm was used to calculate the travel time from every pixel to a hospital or clinic accessible via the shortest journey. The least-cost-path algorithm was developed by Dijkstra40 for use in graphs (that is, networks of connected nodes) and has since been adapted within several software packages for use with gridded datasets. For this work, we used the versions of Dijkstra’s algorithm coded into Google Earth Engine41 (as the cumulativeCost() function) and the gDistance package42 in R (as the accCost() function). The underlying premise of this approach was to effectively test all possible routes from each 1 km × 1 km pixel to every healthcare facility and then display the minimum travel time for each pixel within the map of travel time. The maps extend from 56° S to 83° N and span the full circumference of the Earth (that is, −180° to +180°). This extent includes virtually all land areas on Earth other than Antarctica. The map resolution is 30 × 30 arc-seconds, which is roughly equivalent to 1 km × 1 km at the equator. Ocean areas were masked in the final maps of travel time and set to a no-data value of −9999. The units of the map are in minutes of travel time to the most accessible facility, which need not be the closest facility in terms of geographic distance due to transportation infrastructure patterns.
Model validation
A thorough validation of the underlying method used to calculate travel time was presented by Nelson et al. 22. This validation compared results generated through the least-cost-path algorithm applied to an earlier friction surface4 with travel time estimates for the same journeys as those calculated using the Google Maps API. Unlike our raster-based approach, the Google Maps API estimated travel time using the vector-based road network. These validation results indicated that the travel time estimates from the friction surface were, on average, within ±15.8 min of those from the alternative source. There was, however, spatial variability in the model accuracy, with some areas being more prone to underestimates, while other areas tended to have overestimates22. Cursory analysis of the new, optimal friction surface suggested that it produced similar accuracies.
No validation was performed on the input healthcare facility locations as these data were published elsewhere by research groups that have their own data quality protocols. A caveat for the maps of travel time to healthcare facilities is that definitions for hospitals and clinics are likely to vary from country to country and, in the case of data originating from OSM, between the users entering the data. As such, countries that appear to have few facilities relative to the population may reflect a stricter definition of what constitutes a facility, and vice versa. Supplementary Table 2 enables users of our maps of travel time to better assess the completeness of the facility dataset for individual countries, as well as the percentage of the population living beyond 10, 30 and 60 min from a healthcare facility. In cases where these data (Supplementary Table 2) suggest that our facility set is incomplete (for example, the Democratic People’s Republic of Korea has only 26 facility pixels in our dataset), our code and friction surface provide a ready means of creating updated maps of travel time if improved facility location data become available.
The most important limitation of this work, however, is the level of completeness of the healthcare facility inventory, which varies by country. This challenge provided the rationale for using multiple data sources, as they had different strengths in different areas. For example, the Google dataset provided the best source of information on facility location in Asia, OSM was the best source for data on facilities in remote locations such as Pacific Islands and high latitudes, and the published data provided the majority of the facility information in Africa. The implications of incomplete or inaccurate facility locations were a notable concern of this work. While we had no means of discovering facilities that were erroneously attributed to locations many kilometers from their true positions, we did conduct a sensitivity analysis to test whether there were slight spatial discrepancies between the input datasets (for example, whether a hospital attributed to one pixel in Google was likely to be found within a neighboring pixel within OSM). This analysis consisted of aggregating facility location pixels to lower spatial resolutions, calculating the proportion of pixels containing healthcare facility pixels that were merged and then comparing results derived within and between the facility data sources. These results showed that facility pixels from the same dataset were more likely to be merged than those from different datasets (Supplementary Table 3), which suggests that minor discrepancies in facility geolocations between sources did not inflate the combined facility count or cause noteworthy inaccuracies in the final maps. Lastly, because the comprehensiveness and accuracy of the healthcare facility datasets will always be speculative, and new or updated datasets will continue to improve data quality, we have made our code and friction surfaces freely available to support (1) the production of custom maps in cases where users have their own facility location data and (2) frequent updates to our global maps of travel time to hospitals and clinics as new facility locations become available.
Extended analysis
To provide additional context with which to interpret the optimal and walking-only maps of travel time, we explored the association between travel time to a healthcare facility and healthcare utilization. For this, we analyzed treatment seeking among children under five years of age with a fever using household survey data collected by the Demographic and Health Survey Program (DHS). Treatment-seeking data were extracted for geolocated household clusters from 150 surveys collected across 56 countries between 2000 and 2017. Only households within a 2-hour walk of a hospital or clinic were included to retain large sample sizes for households both with and without motorized transportation within each travel time threshold range. The resulting dataset consisted of 257,416 children under the age of five with a fever, 159,863 of whom were taken for medical care.
The results of the extended treatment-seeking analysis (Extended Data Fig. 2) provided additional empirical evidence that the time it takes individuals to reach a hospital or clinic affects the likelihood that they seek medical attention, but the comparison was imperfect as some of the DHS survey responses may have predated the building of facilities contained within our database. A more robust finding, which was consistent whether the optimal or walking-only maps of travel time were used as the basis for the Extended Data Fig. 2, was a strong association between household ownership of motorized transportation (including motorcycles) and care seeking for children with fevers. Interestingly, this relationship was apparent even in cases where a healthcare facility was less than a 10-min walk from the household, which highlights the importance of household wealth as a determinant of healthcare seeking43,44,45 even when travel time is a minor consideration.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The code, friction surfaces and maps of travel time to hospitals and clinics are available for download in GEOTIFF format (.tif) at https://malariaatlas.org/research-project/accessibility_to_healthcare/ and for analysis within Google Earth Engine41. For users with limited computational capacity, we have also created an online tool for freely creating accessibility maps with limited spatial extents at https://access-mapper.appspot.com/. The OSM roads and healthcare facilities are available through https://www.openstreetmap.org/ and https://healthsites.io/, respectively. Google roads and healthcare facilities can be viewed within Google Maps. Published healthcare facility datasets are available through repositories associated with those publications18,19.
References
Fullman, N. et al. Measuring performance on the healthcare access and quality index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet 391, 2236–2271 (2018).
Wang, F. & Luo, W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place 11, 131–146 (2005).
Buzza, C. et al. Distance is relative: unpacking a principal barrier in rural healthcare. J. Gen. Intern. Med. 26, 648–654 (2011).
Weiss, D. J. et al. A global map of travel time to cities to assess inequalities in accessibility in 2015. Nature 553, 333–336 (2018).
Battle, K. E. et al. Treatment-seeking rates in malaria endemic countries. Malar. J. 15, 20 (2016).
Stock, R. Distance and the utilization of health facilities in rural Nigeria. Soc. Sci. Med. 17, 563–570 (1983).
Alegana, V. A., Wright, J., Pezzulo, C., Tatem, A. J. & Atkinson, P. M. Treatment-seeking behaviour in low-and middle-income countries estimated using a Bayesian model. BMC Med. Res. Methodol. 17, 67 (2017).
Nemet, G. F. & Bailey, A. J. Distance and healthcare utilization among the rural elderly. Soc. Sci. Med. 50, 1197–1208 (2000).
Syed, S. T., Gerber, B. S. & Sharp, L. K. Traveling towards disease: transportation barriers to healthcare access. J. Community Health 38, 976–993 (2013).
Thaddeus, S. & Maine, D. Too far to walk: maternal mortality in context. Soc. Sci. Med. 38, 1091–1110 (1994).
Manongi, R. et al. Inpatient child mortality by travel time to hospital in a rural area of Tanzania. Trop. Med. Int. Health 19, 555–562 (2014).
World Health Organization. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. https://apps.who.int/iris/bitstream/handle/10665/44369/9789241564014_eng.pdf (WHO, 2010).
Juran, S. et al. Geospatial mapping of access to timely essential surgery in sub-Saharan Africa. BMJ Glob. Health 3, e000875 (2018).
Noor, A., Zurovac, D., Hay, S., Ochola, S. & Snow, R. Defining equity in physical access to clinical services using geographical information systems as part of malaria planning and monitoring in Kenya. Trop. Med. Int. Health 8, 917–926 (2003).
Perry, B. & Gesler, W. Physical access to primary healthcare in Andean Bolivia. Soc. Sci. Med. 50, 1177–1188 (2000).
Tanser, F., Gijsbertsen, B. & Herbst, K. Modelling and understanding primary healthcare accessibility and utilization in rural South Africa: an exploration using a geographical information system. Soc. Sci. Med. 63, 691–705 (2006).
Alegana, V. A. et al. Spatial modelling of healthcare utilisation for treatment of fever in Namibia. Int. J. Health Geogr. 11, 6 (2012).
Barbieri, S. & Jorm, L. Travel times to hospitals in Australia. Sci. Data 6, 248 (2019).
Maina, J. et al. A spatial database of health facilities managed by the public health sector in sub-Saharan Africa. Sci. Data 6, 134 (2019).
Nelson, A. Travel time to major cities: a global map of accessibility. https://forobs.jrc.ec.europa.eu/products/gam/ (Global Environment Monitoring Unit, Joint Research Unit of the European Commission, 2008).
Wong, K. L. M., Brady, O. J., Campbell, O. M. R., Banke-Thomas, A. & Benova, L. Too poor or too far? Partitioning the variability of hospital-based childbirth by poverty and travel time in Kenya, Malawi, Nigeria and Tanzania. Int. J. Equity Health 19, 15 (2020).
Nelson, A. et al. A suite of global accessibility indicators. Sci. Data 6, 266 (2019).
Gulliford, M. et al. What does ‘access to healthcare’ mean? J. Health Serv. Res. Policy 7, 186–188 (2002).
Haynes, R., Lovett, A. & Sünnenberg, G. Potential accessibility, travel time and consumer choice: geographical variations in general medical practice registrations in Eastern England. Environ. Plan. A 35, 1733–1750 (2003).
Johansson, E. W. et al. Accessibility of basic paediatric emergency care in Malawi: analysis of a national facility census. BMC Public Health 20, 992 (2020)
Hulland, E. N. et al. Travel time to health facilities in areas of outbreak potential: maps for guiding local preparedness and response. BMC Med. 17, 232 (2019).
Weiss, D. J. et al. Mapping the global prevalence, incidence and mortality of Plasmodium falciparum, 2000-17: a spatial and temporal modelling study. Lancet 394, 322–331 (2019).
Saameli, R., Kalubi, D., Herringer, M., Sutton, T. & de Roodenbeke, E. Healthsites.io: the Global Healthsites Mapping Project. In Technologies for Development: From Innovation to Social Impact (eds. Hostettler, S. et al.) 53–59 (Springer, 2018).
Goodchild, M. F. Citizens as sensors: the world of volunteered geography. GeoJournal 69, 211–221 (2007).
Goodchild, M. F. & Li, L. Assuring the quality of volunteered geographic information. Spat. Stat. 1, 110–120 (2012).
Brovelli, M. A., Minghini, M., Molinari, M. & Mooney, P. Towards an automated comparison of OpenStreetMap with authoritative road datasets. Trans. GIS 21, 191–206 (2017).
Barrington-Leigh, C. & Millard-Ball, A. The world’s user-generated road map is more than 80% complete. PLoS ONE 12, e0180698 (2017).
Jackson, S. P. et al. Assessing completeness and spatial error of features in volunteered geographic information. ISPRS Int. J. Geoinf. 2, 507–530 (2013).
Hecht, R., Kunze, C. & Hahmann, S. Measuring completeness of building footprints in OpenStreetMap over space and time. ISPRS Int. J. Geoinf. 2, 1066–1091 (2013).
Canavosio-Zuzelski, R., Agouris, P. & Doucette, P. A photogrammetric approach for assessing positional accuracy of OpenStreetMap roads. ISPRS Int. J. Geoinf. 2, 276–301 (2013).
Haklay, M. How good is volunteered geographical information? a comparative study of OpenStreetMap and Ordnance Survey datasets. Environ. Plann. B Plann. Des. 37, 682–703 (2010).
Girres, J. F. & Touya, G. Quality assessment of the French OpenStreetMap dataset. Trans. GIS 14, 435–459 (2010).
International Organization for Standardization. ISO 19157:2013. Geographic information—data quality (2013).
Google. How Google sources and uses information in local listings https://support.google.com/business/answer/9851099?hl=en/ (2020).
Dijkstra, E. W. A note on two problems in connexion with graphs. Numer. Math. 1, 269–271 (1959).
Gorelick, N. et al. Google Earth Engine: planetary-scale geospatial analysis for everyone. Remote Sens. Environ. 183, 250–264 (2017).
van Etten, J. R package gdistance: distances and routes on geographical grids. J. Stat. Softw. 76, 1–21 (2017).
Kassile, T., Lokina, R., Mujinja, P. & Mmbando, B. P. Determinants of delay in care seeking among children under five with fever in Dodoma region, central Tanzania: a cross-sectional study. Malar. J. 13, 348 (2014).
Yaya, S., Bishwajit, G. & Shah, V. Wealth, education and urban–rural inequality and maternal healthcare service usage in Malawi. BMJ Glob. Health 1, e000085 (2016).
Najnin, N., Bennett, C. M. & Luby, S. P. Inequalities in care-seeking for febrile illness of under-five children in urban Dhaka, Bangladesh. J. Health Popul. Nutr. 29, 523–531 (2011).
Acknowledgements
We thank the OSM project organizers and its dedicated contributors for providing road and healthcare facility data that were essential for this research. The healthsites.io project greatly simplified the process of using the OSM healthcare facility locations. Funding for this work was provided by a Google Earth Engine Research Award entitled “Developing and validating an online accessibility mapping tool powered by Google Earth Engine” and from the Bill and Melinda Gates Foundation (OPP1197730).
Author information
Authors and Affiliations
Contributions
D.J.W. designed and led the analysis and wrote the manuscript. A.N. developed the original modeling approach and contributed to the model validation. C.A.V.-R. extracted the OSM data. K.G., S. Bavadekar and E.G. extracted the Google Maps facility data and produced the Google-specific map of travel time. A.B.-V., H.S.G. and J.J.M. assisted with the analysis. J.R. produced the global maps. T.S. and A.L. provided administrative support at Google. P.G. and S. Bhatt assisted with the conceptual design of the project. All authors provided critical review and assisted in writing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Jennifer Sargent was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended data Fig. 1
Venn diagram of the shared pixels counts of hospital and clinic locations contained within each of the facility datasets. Percentages in parentheses are relative to the combined set of facility pixels (n = 376,231).
Extended data Fig. 2
Proportions of healthcare seeking and linear trendlines for fevers in children under five from households with and without motorized transportation. The geolocated survey data were intersected with the walking-only travel time map and aggregated into ten-minute intervals.
Supplementary information
Rights and permissions
About this article
Cite this article
Weiss, D.J., Nelson, A., Vargas-Ruiz, C.A. et al. Global maps of travel time to healthcare facilities. Nat Med 26, 1835–1838 (2020). https://doi.org/10.1038/s41591-020-1059-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-1059-1
This article is cited by
-
Protocol for spatial prediction of soil transmitted helminth prevalence in the Western Pacific region using a meta-analytical approach
Systematic Reviews (2024)
-
Associations between school-based fluoride mouth-rinse program, medical-dental expense subsidy policy, and children's oral health in Japan: an ecological study
BMC Public Health (2024)
-
Determinants of intention to conceal tuberculosis status among family members: an analysis of seven Sub-Saharan African countries
BMC Infectious Diseases (2024)
-
Effects of climate change and human activities on vector-borne diseases
Nature Reviews Microbiology (2024)
-
Geographic pair matching in large-scale cluster randomized trials
Nature Communications (2024)