Abstract
A burgeoning epidemic of drug-resistant tuberculosis (TB) threatens to derail global control efforts. Although the mechanisms remain poorly clarified, drug-resistant strains are widely believed to be less infectious than drug-susceptible strains. Consequently, we hypothesized that lower proportions of patients with drug-resistant TB would have culturable Mycobacterium tuberculosis from respirable, cough-generated aerosols compared to patients with drug-susceptible TB, and that multiple factors, including mycobacterial genomic variation, would predict culturable cough aerosol production. We enumerated the colony forming units in aerosols (≤10 µm) from 452 patients with TB (227 with drug resistance), compared clinical characteristics, and performed mycobacterial whole-genome sequencing, dormancy phenotyping and drug-susceptibility analyses on M. tuberculosis from sputum. After considering treatment duration, we found that almost half of the patients with drug-resistant TB were cough aerosol culture-positive. Surprisingly, neither mycobacterial genomic variants, lineage, nor dormancy status predicted cough aerosol culture positivity. However, mycobacterial sputum bacillary load and clinical characteristics, including a lower symptom score and stronger cough, were strongly predictive, thereby supporting targeted transmission-limiting interventions. Effective treatment largely abrogated cough aerosol culture positivity; however, this was not always rapid. These data question current paradigms, inform public health strategies and suggest the need to redirect TB transmission-associated research efforts toward host–pathogen interactions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The deidentified datasets generated and/or analyzed during the study are available from the corresponding author without restriction. The sequencing data are available at the Sequence Read Archive under accession no. PRJNA600338). Source data for Figs. 1–3 and Extended Data Figs. 2–5 are included with this paper.
References
Dheda, K. et al. The epidemiology, pathogenesis, transmission, diagnosis, and management of multidrug-resistant, extensively drug-resistant, and incurable tuberculosis. Lancet Respir. Med. 5, 291–360 (2017).
Riley, R. et al. Infectiousness of air from a tuberculosis ward. Ultraviolet irradiation of infected air: comparative infectiousness of different patients. Am. Rev. Respir. Dis. 85, 511–525 (1962).
Sultan, L. et al. Tuberculosis disseminators. A study of the variability of aerial infectivity of tuberculous patients. Am. Rev. Respir. Dis. 82, 358–369 (1960).
Tostmann, A. et al. Tuberculosis transmission by patients with smear-negative pulmonary tuberculosis in a large cohort in the Netherlands. Clin. Infect. Dis. 47, 1135–1142 (2008).
Walker, T. M. et al. Whole-genome sequencing to delineate Mycobacterium tuberculosis outbreaks: a retrospective observational study. Lancet Infect. Dis. 13, 137–146 (2013).
van Geuns, H., Meijer, J. & Styblo, K. Results of contact examination in Rotterdam, 1967–1969. Bull. Int. Union Tuberc. 50, 107–121 (1975).
Melsew, Y. A. et al. The role of super-spreading events in Mycobacterium tuberculosis transmission: evidence from contact tracing. BMC Infect. Dis. 19, 244 (2019).
Ypma, R. J., Altes, H. K., van Soolingen, D., Wallinga, J. & van Ballegooijen, W. M. A sign of superspreading in tuberculosis: highly skewed distribution of genotypic cluster sizes. Epidemiology 24, 395–400 (2013).
Lloyd-Smith, J. O., Schreiber, S. J., Kopp, P. E. & Getz, W. Superspreading and the effect of individual variation on disease emergence. Nature 438, 355–359 (2005).
McCreesh, N. & White, R. G. An explanation for the low proportion of tuberculosis that results from transmission between household and known social contacts. Sci. Rep. 8, 5382 (2018).
Woolhouse, M. E. et al. Heterogeneities in the transmission of infectious agents: implications for the design of control programs. Proc. Natl Acad. Sci. USA 94, 338–342 (1997).
Kodama, C. et al. Mycobacterium tuberculosis transmission from patients with drug-resistant compared to drug-susceptible TB: a systematic review and meta-analysis. Eur Respir. J. 50, 1701044 (2017).
Fennelly, K. P. et al. Cough-generated aerosols of Mycobacterium tuberculosis: a new method to study infectiousness. Am. J. Respir. Crit. Care Med. 169, 604–609 (2004).
Gagneux, S. et al. Impact of bacterial genetics on the transmission of isoniazid-resistant Mycobacterium tuberculosis. PLoS Pathog. 2, e61 (2006).
Fennelly, K. P. et al. Variability of infectious aerosols produced during coughing by patients with pulmonary tuberculosis. Am. J. Respir. Crit. Care Med. 186, 450–457 (2012).
Jones-López, E. C. et al. Cough aerosols of Mycobacterium tuberculosis predict new infection: a household contact study. Am. J. Respir. Crit. Care Med. 187, 1007–1015 (2013).
Wejse, C. et al. TBscore: signs and symptoms from tuberculosis patients in a low-resource setting have predictive value and may be used to assess clinical course. Scand. J. Infect. Dis. 40, 111–120 (2008).
Garton, N. J., Christensen, H., Minnikin, D. E., Adegbola, R. A. & Barer, M. R. Intracellular lipophilic inclusions of mycobacteria in vitro and in sputum. Microbiology 148, 2951–2958 (2002).
South African Department of Health Management of Drug-Resistant Tuberculosis (2011); https://health-e.org.za/wp-content/uploads/2014/06/MDR-TB-Clinical-Guidelines-Updated-Jan-2013.pdf
Six and Two Stage Viable Samplers. Instruction Manual (Thermo Fisher Scientific, 2009); http://tools.thermofisher.com/content/sfs/manuals/EPM-manual-SixStageAnd.pdf
Landis, J. R. & Koch, G. G. The measurement of observer agreement for categorical data. Biometrics 33, 159–174 (1977).
Koo, T. K. & Li, M. Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 15, 155–163 (2016).
Stoltz, A. C. et al. Multi-drug resistant TB treatment regimen, including bedaquiline and linezolid, failed to reduce transmission over 14 days. In American Thoracic Society 2017 International Conf. (2020).
Ashley, K. & Fey O’Connor, P. NIOSH Manual of Analytical Methods (NMAM) 5th edn (NIOSH CDC, 2017).
Acuña-Villaorduña, C. et al. Host determinants of infectiousness in smear-positive patients with pulmonary tuberculosis. Open Forum Infect. Dis. 6, ofz184 (2019).
Calligaro, G. L. et al. Effect of new tuberculosis diagnostic technologies on community-based intensified case finding: a multicentre randomised controlled trial. Lancet Infect. Dis. 17, 441–450 (2017).
Rouillon, A., Perdrizet, S. & Parrot, R. Transmission of tubercle bacilli: the effects of chemotherapy. Tubercle 57, 275–299 (1976).
Noble, R. C. Infectiousness of pulmonary tuberculosis after starting chemotherapy: review of the available data on an unresolved question. Am. J. Infect. Control 9, 6–10 (1981).
Dharmadhikari, A. S. et al. Rapid impact of effective treatment on transmission of multidrug-resistant tuberculosis. Int. J. Tuberc. Lung Dis. 18, 1019–1025 (2014).
Dheda, K. et al. Drug-penetration gradients associated with acquired drug resistance in patients with tuberculosis. Am. J. Respir. Crit. Care Med. 198, 1208–1219 (2018).
Fitzwater, S. P. et al. Prolonged infectiousness of tuberculosis patients in a directly observed therapy short-course program with standardized therapy. Clin. Infect. Dis. 51, 371–378 (2010).
Pietersen, E. et al. Long-term outcomes of patients with extensively drug-resistant tuberculosis in South Africa: a cohort study. Lancet 383, 1230–1239 (2014).
Yates, T. A. et al. The transmission of Mycobacterium tuberculosis in high burden settings. Lancet Infect. Dis. 16, 227–238 (2016).
Escombe, A. R. et al. The detection of airborne transmission of tuberculosis from HIV-infected patients, using an in vivo air sampling model. Clin. Infect. Dis. 44, 1349–1357 (2007).
Dharmadhikari, A. S. et al. Natural infection of guinea pigs exposed to patients with highly drug-resistant tuberculosis. Tuberculosis 91, 329–338 (2011).
Lin, P. L. et al. Early events in Mycobacterium tuberculosis infection in cynomolgus macaques. Infect. Immun. 74, 3790–3803 (2006).
Jones-López, E. C. et al. Cough aerosols of Mycobacterium tuberculosis predict incident tuberculosis disease in household contacts. Clin. Infect. Dis. 63, 10–20 (2016).
Chengalroyen, M. D. et al. Detection and quantification of differentially culturable tubercle bacteria in sputum from patients with tuberculosis. Am. J. Respir. Crit. Care Med. 194, 1532–1540 (2016).
Johnson, R. et al. Drug-resistant tuberculosis epidemic in the Western Cape driven by a virulent Beijing genotype strain. Int. J. Tuberc. Lung Dis. 14, 119–121 (2010).
Yu, X. et al. Sensititre® MYCOTB MIC plate for drug susceptibility testing of Mycobacterium tuberculosis complex isolates. Int. J. Tuberc. Lung Dis. 20, 329–334 (2016).
Dheda, K. et al. Outcomes, infectiousness, and transmission dynamics of patients with extensively drug-resistant tuberculosis and home-discharged patients with programmatically incurable tuberculosis: a prospective cohort study. Lancet Respir. Med. 5, 269–281 (2017).
Te Riele, J. B. et al. Relationship between chest radiographic characteristics, sputum bacterial load, and treatment outcomes in patients with extensively drug-resistant tuberculosis. Int. J. Infect. Dis. 79, 65–71 (2019).
World Health Organization Mycobacteriology Laboratory Manual 1st edn (Global Laboratory Initiative, 2014); https://www.who.int/tb/laboratory/mycobacteriology-laboratory-manual.pdf
Rieder, H. L. et al. The Public Health Service National Tuberculosis Reference Laboratory and the National Laboratory Network. Minimum Requirements, Role and Operation in a Low-Income Country (International Union Against Tuberculosis and Lung Disease, 1998); https://www.ghdonline.org/uploads/The_Public_Health_Service_National_Tuberculosis_Reference_La.pdf
Lee, J. et al. Sensititre MYCOTB MIC plate for testing Mycobacterium tuberculosis susceptibility to first- and second-line drugs. Antimicrob. Agents Chemother. 58, 11–18 (2014).
Sloan, D. J. et al. Pharmacodynamic modeling of bacillary elimination rates and detection of bacterial lipid bodies in sputum to predict and understand outcomes in treatment of pulmonary tuberculosis. Clin. Infect. Dis. 61, 1–8 (2015).
Warren, R. et al. Safe Mycobacterium tuberculosis DNA extraction method that does not compromise integrity. J. Clin. Microbiol. 44, 254–256 (2006).
R Core Team R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2016).
Casali, N. et al. Evolution and transmission of drug-resistant tuberculosis in a Russian population. Nat. Genet. 46, 279–286 (2014).
Trauner, A., Borrell, S., Reither, K. & Gagneux, S. Evolution of drug resistance in tuberculosis: recent progress and implications for diagnosis and therapy. Drugs 74, 1063–1072 (2014).
Song, T. et al. Fitness costs of rifampicin resistance in Mycobacterium tuberculosis are amplified under conditions of nutrient starvation and compensated by mutation in the β' subunit of RNA polymerase. Mol. Microbiol. 91, 1106–1119 (2014).
de Vos, M. et al. Putative compensatory mutations in the rpoC gene of rifampin-resistant Mycobacterium tuberculosis are associated with ongoing transmission. Antimicrob. Agents Chemother. 57, 827–832 (2013).
Farhat, M. R. et al. Genomic analysis identifies targets of convergent positive selection in drug-resistant Mycobacterium tuberculosis. Nat. Genet. 45, 1183–1189 (2013).
Comas, I. et al. Whole-genome sequencing of rifampicin-resistant Mycobacterium tuberculosis strains identifies compensatory mutations in RNA polymerase genes. Nat. Genet. 44, 106–110 (2012).
Walker, T. M. et al. Whole-genome sequencing for prediction of Mycobacterium tuberculosis drug susceptibility and resistance: a retrospective cohort study. Lancet Infect. Dis. 15, 1193–1202 (2015).
Coll, F. et al. Rapid determination of anti-tuberculosis drug resistance from whole-genome sequences. Genome Med. 7, 51 (2015).
Sirgel, F. A. The rationale for using rifabutin in the treatment of MDR and XDR tuberculosis outbreaks. PLoS ONE 8, e59414 (2013).
Whitfield, M. G. et al. Mycobacterium tuberculosis pncA polymorphisms that do not confer pyrazinamide resistance at a breakpoint concentration of 100 micrograms per milliliter in MGIT. J. Clin. Microbiol. 53, 3633–3635 (2015).
Definitions and Reporting Framework for Tuberculosis, 2013 Revision (World Health Organization, 2013); https://www.who.int/tb/publications/definitions/en/
De Stavola, B. L. & Cox, D. R. On the consequences of overstratification. Biometrika 95, 992–996 (2008).
WHO Treatment Guidelines for Drug-Resistant Tuberculosis (2016 Update) (World Health Organization, 2016); http://apps.who.int/iris/bitstream/10665/250125/5/9789241549639-webannexes-eng.pdf
Automated Ral-Time Nucleic Acid Amplification Technology for Rapid and Simultaneous Detection of Tuberculosis and Rifampicin Resistance: Xpert MTB/RIF System. Policy Statement (World Health Organization, 2011); https://www.who.int/tb/publications/tb-amplificationtechnology-statement/en/
Demay, C. et al. SITVITWEB: a publicly available international multimarker database for studying Mycobacterium tuberculosis genetic diversity and molecular epidemiology. Infect. Genet. Evol. 12, 755–766 (2012).
Coll, F. et al. SpolPred: rapid and accurate prediction of Mycobacterium tuberculosis spoligotypes from short genomic sequences. Bioinformatics 28, 2991–2993 (2012).
Global Tuberculosis Report 2016 (World Health Organization, 2016); https://apps.who.int/iris/handle/10665/250441
Acknowledgements
We are indebted to the patients who participated. The study would not have been possible without the remarkable efforts of R. Wilson and G. Pretorius. We also thank for their invaluable assistance M. Pienaar and M. Pretorius, P. Spiller, M. Barnard, J. Simpson, T. Dolby, R. van Aarde, C. Clarke and B. Derendinger. The WGS computations were done using facilities provided by the University of Cape Town’s ICTS High Performance Computing team. The project was funded by the National Institutes of Health (grant no. 1R01AI104817-01), Wellcome Trust (grant no. 099854/Z/12/Z), South African Medical Research Council (Career Development Award, Self-initiated Research Award) and the National Research Foundation of South Africa. The content is solely the responsibility of the authors and does not necessarily represent the official views of the South African Medical Research Council. G.T. acknowledges funding from the South African Medical Research Council (grant no. RFA-IFSP-01-2013), the EDCTP2 programme supported by the European Union (grant no. SF1401, OPTIMAL DIAGNOSIS) and the Faculty of Medicine and Health Sciences, Stellenbosch University. K.D. acknowledges funding from the South African Medical Research Council (grant no. RFA-EMU-02-2017), EDCTP (grant nos. TMA-2015SF-1043, TMA-1051-TESAII and TMA-CDF2015), UK Medical Research Council (grant no. MR/S03563X/1) and the Wellcome Trust (grant no. MR/S027777/1). K.F. was supported by the Intramural Research Program of the National Institutes of Health, National Heart, Lung, and Blood Institute. We acknowledge the financial assistance of the National Research Foundation toward this research. The opinions expressed and conclusions arrived at are those of the author(s) and should not necessarily to be attributed to the National Research Foundation.
Author information
Authors and Affiliations
Contributions
K.D., K.F., R.W. and G.T. conceived the study and acquired the funding. G.T., J.L., R.V., L.S., E.P., A.E., G.C., J.t.R. and M.d.K. acquired the data. K.D., P.v.H., T.G., T.G.C. and R.W. provided important research infrastructure. G.T., K.D., J.L., R.V. and L.S. carried out the analyses. G.T. prepared the first draft of the manuscript. All authors provided critical feedback.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Alison Farrell is the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
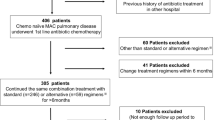
Extended Data Fig. 1 Study profile and participant overview.
Abbreviations: CASS, cough aerosol sampling system; DS, drug-susceptible; INH, isoniazid; MDR, multidrug-resistant; MGIT, mycobacterial growth indicator tube; RIF, rifampicin; TB, tuberculosis; XDR, extensively drug-resistant; VL, viral load; WGS, whole genome sequencing. *Done using Sensititre MYCOTB plates for isoniazid, rifampicin, ethambutol, ethionamide, kanamycin, ofloxacin, p-aminosalicylic acid, rifabutin, streptomycin, cycloserine, amikacin, and moxifloxacin.
Extended Data Fig. 2 M. tuberculosis CFU from cough aerosol particles at recruitment as a function of days on treatment before CASS stratified by regimen type.
Beyond eight days, no patients receiving the first-line regimen were CASS-positive, whereas patients receiving second-line regimens had CFU in their aerosol for months. The y-axis is logarithmic and one was added to CFU counts. Abbreviations: ACI, Andersen Cascade Impactor; CLF, clofazimine; FQ, fluoroquinolone; IQR, interquartile range; SLID, second-line injectable drug.
Extended Data Fig. 3
Relationships between sputum bacillary load (liquid culture time-to-positivity) and disease extent (a and b) and cavitation score (c), and between CASS-status and cavitation score (d) assessed by chest radiography using the standardised reporting system in Supplementary Table 2. No legend required in addition to title.
Extended Data Fig. 4 Maximum likelihood phylogenetic tree of baseline CASS isolates (n=318) rooted to Mycobacterium bovis BCG.
Heatmaps to the right of the tree denote from left to right CASS status (also denoted on the branch nodes), treatment duration, drug resistance group and M. tuberculosis lineage. No legend required in addition to title.
Extended Data Fig. 5 A Manhattan plot of multivariate genome wide association study (GWAS) using nsSNPs per gene for CASS-positivity including two principal components, patient age, TB symptom score, HIV-status, duration of treatment less than 48h, PCF, culture time to positivity, and drug-resistance category did not detect significant associations.
The horizontal dashed line represents the threshold of statistical significance.
Supplementary information
Supplementary Information
Supplementary Tables 1–22, results text and references.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Rights and permissions
About this article
Cite this article
Theron, G., Limberis, J., Venter, R. et al. Bacterial and host determinants of cough aerosol culture positivity in patients with drug-resistant versus drug-susceptible tuberculosis. Nat Med 26, 1435–1443 (2020). https://doi.org/10.1038/s41591-020-0940-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-0940-2
This article is cited by
-
Multidrug-resistant tuberculosis
Nature Reviews Disease Primers (2024)
-
Frequency, kinetics and determinants of viable SARS-CoV-2 in bioaerosols from ambulatory COVID-19 patients infected with the Beta, Delta or Omicron variants
Nature Communications (2024)
-
Comparison of two diagnostic intervention packages for community-based active case finding for tuberculosis: an open-label randomized controlled trial
Nature Medicine (2023)
-
Early phase of effective treatment induces distinct transcriptional changes in Mycobacterium tuberculosis expelled by pulmonary tuberculosis patients
Scientific Reports (2021)
-
Aggregation state of Mycobacterium tuberculosis impacts host immunity and augments pulmonary disease pathology
Communications Biology (2021)