Abstract
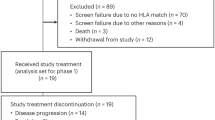
Personal neoantigen vaccines have been envisioned as an effective approach to induce, amplify and diversify antitumor T cell responses. To define the long-term effects of such a vaccine, we evaluated the clinical outcome and circulating immune responses of eight patients with surgically resected stage IIIB/C or IVM1a/b melanoma, at a median of almost 4 years after treatment with NeoVax, a long-peptide vaccine targeting up to 20 personal neoantigens per patient (NCT01970358). All patients were alive and six were without evidence of active disease. We observed long-term persistence of neoantigen-specific T cell responses following vaccination, with ex vivo detection of neoantigen-specific T cells exhibiting a memory phenotype. We also found diversification of neoantigen-specific T cell clones over time, with emergence of multiple T cell receptor clonotypes exhibiting distinct functional avidities. Furthermore, we detected evidence of tumor infiltration by neoantigen-specific T cell clones after vaccination and epitope spreading, suggesting on-target vaccine-induced tumor cell killing. Personal neoantigen peptide vaccines thus induce T cell responses that persist over years and broaden the spectrum of tumor-specific cytotoxicity in patients with melanoma.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
All requests for raw and analyzed data and materials will be promptly reviewed by the Belfer Office for Dana-Farber Innovations to verify whether the request is subject to any intellectual property or confidentiality obligations. Patient-related data not included in the paper were generated as part of clinical trials and may be subject to patient confidentiality. Any data and materials that can be shared will be released via a Material Transfer Agreement. DNA and RNA sequencing data are available through dbGaP (https://www.ncbi.nlm.nih.gov/gap) with accession number phs001451.3.1. TCR sequencing data are available in Supplementary Tables 7 and 8.
Code availability
Code used for data analysis including Broad Picard Pipeline v.2.22.4 (WES/RNA-seq), GATK4 v.4.0, Mutect2 v.2.7.0 (sSNV and indel identification), NetMHCpan v.2.4 and 4.0 (neoantigen prediction), NetMHCIIpan v.4.0 (MHC class II binding peptide prediction), ContEST v.1 (contamination estimation), ABSOLUTE v.1.1 (purity/ploidy estimation), STAR v.2.6.1c (sequencing alignment), RSEM v.1.3.1 (gene expression quantification), Flexbar v.3.4, WebGestalt 2019 (gene set enrichment analysis), HLAthena (neoantigen prediction), Seurat v.3.1.0 (single cell sequencing analysis), IGV v.2.6.3 (genomic variant visualization), PhylogicNDT v.1, Inform 2.4 and FlowJo v.10, are publicly available from the indicated references.
References
Ott, P. A. et al. An immunogenic personal neoantigen vaccine for patients with melanoma. Nature 547, 217–221 (2017).
Keskin, D. B. et al. Neoantigen vaccine generates intratumoral T cell responses in phase Ib glioblastoma trial. Nature 565, 234–239 (2019).
Carreno, B. M. et al. Cancer immunotherapy. A dendritic cell vaccine increases the breadth and diversity of melanoma neoantigen-specific T cells. Science 348, 803–808 (2015).
Sahin, U. et al. Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer. Nature 547, 222–226 (2017).
Verma, V. et al. PD-1 blockade in subprimed CD8 cells induces dysfunctional PD-1(+)CD38(hi) cells and anti-PD-1 resistance. Nat. Immunol. 20, 1231–1243 (2019).
Stuart, T. et al. Comprehensive integration of single-cell data. Cell 177, 1888–1902 (2019).
Nussing, S. et al. Divergent SATB1 expression across human life span and tissue compartments. Immunol. Cell Biol. 97, 498–511 (2019).
Willinger, T. et al. Human naive CD8 T cells down-regulate expression of the WNT pathway transcription factors lymphoid enhancer binding factor 1 and transcription factor 7 (T cell factor-1) following antigen encounter in vitro and in vivo. J. Immunol. 176, 1439–1446 (2006).
Spitzer, M. H. et al. Systemic immunity is required for effective cancer immunotherapy. Cell 168, 487–502 (2017).
Haabeth, O. A. et al. Idiotype-specific CD4(+) T cells eradicate disseminated myeloma. Leukemia 30, 1216–1220 (2016).
Hirschhorn-Cymerman, D. et al. Induction of tumoricidal function in CD4+ T cells is associated with concomitant memory and terminally differentiated phenotype. J. Exp. Med. 209, 2113–2126 (2012).
Oh, D. Y. et al. Intratumoral CD4(+) T cells mediate anti-tumor cytotoxicity in human bladder cancer. Cell 181, 1612–1625 (2020).
Gattinoni, L., Speiser, D. E., Lichterfeld, M. & Bonini, C. T memory stem cells in health and disease. Nat. Med. 23, 18–27 (2017).
Deng, Q. et al. Characteristics of anti-CD19 CAR T cell infusion products associated with efficacy and toxicity in patients with large B cell lymphomas. Nat. Med. 26, 1878–1887 (2020).
Pauken, K. E. et al. The PD-1 pathway regulates development and function of memory CD8(+) T cells following respiratory viral infection. Cell Rep. 31, 107827 (2020).
Ott, P. A. et al. A phase Ib trial of personalized neoantigen therapy plus anti-PD-1 in patients with advanced melanoma, non-small cell lung cancer, or bladder cancer. Cell 183, 347–362 (2020).
Corbiere, V. et al. Antigen spreading contributes to MAGE vaccination-induced regression of melanoma metastases. Cancer Res. 71, 1253–1262 (2011).
Fisher, S. et al. A scalable, fully automated process for construction of sequence-ready human exome targeted capture libraries. Genome Biol. 12, R1 (2011).
Chapman, M. A. et al. Initial genome sequencing and analysis of multiple myeloma. Nature 471, 467–472 (2011).
Berger, M. F. et al. The genomic complexity of primary human prostate cancer. Nature 470, 214–220 (2011).
Cibulskis, K. et al. ContEst: estimating cross-contamination of human samples in next-generation sequencing data. Bioinformatics 27, 2601–2602 (2011).
Robinson, J. T. et al. Integrative genomics viewer. Nat. Biotechnol. 29, 24–26 (2011).
McKenna, A. et al. The genome analysis toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Carter, S. L. et al. Absolute quantification of somatic DNA alterations in human cancer. Nat. Biotechnol. 30, 413–421 (2012).
Dobin, A. et al. STAR: ultrafast universal RNA−seq aligner. Bioinformatics 29, 15–21 (2013).
Li, B. & Dewey, C. N. RSEM: accurate transcript quantification from RNA-seq data with or without a reference genome. BMC Bioinf. 12, 323 (2011).
DeLuca, D. S. et al. RNA-SeQC: RNA-seq metrics for quality control and process optimization. Bioinformatics 28, 1530–1532 (2012).
Roemer, M. G. et al. Classical Hodgkin lymphoma with reduced β2M/MHC class I expression is associated with inferior outcome independent of 9p24.1 status. Cancer Immunol. Res. 4, 910–916 (2016).
Carey, C. D. et al. Topological analysis reveals a PD-L1-associated microenvironmental niche for Reed–Sternberg cells in Hodgkin lymphoma. Blood 130, 2420–2430 (2017).
Truex, N. L. et al. Automated flow synthesis of tumor neoantigen peptides for personalized immunotherapy. Sci. Rep. 10, 723 (2020).
Cai, A. et al. Mutated BCR-ABL generates immunogenic T-cell epitopes in CML patients. Clin. Cancer Res. 18, 5761–5772 (2012).
Borducchi, E. N. et al. Antibody and TLR7 agonist delay viral rebound in SHIV-infected monkeys. Nature 563, 360–364 (2018).
Call, M. J. et al. In vivo enhancement of peptide display by MHC class II molecules with small molecule catalysts of peptide exchange. J. Immunol. 182, 6342–6352 (2009).
Jang, M. H., Seth, N. P. & Wucherpfennig, K. W. Ex vivo analysis of thymic CD4 T cells in nonobese diabetic mice with tetramers generated from I-A(g7)/class II-associated invariant chain peptide precursors. J. Immunol. 171, 4175–4186 (2003).
Haga-Friedman, A., Horovitz-Fried, M. & Cohen, C. J. Incorporation of transmembrane hydrophobic mutations in the TCR enhance its surface expression and T cell functional avidity. J. Immunol. 188, 5538–5546 (2012).
Cohen, C. J. et al. Enhanced antitumor activity of T cells engineered to express T-cell receptors with a second disulfide bond. Cancer Res. 67, 3898–3903 (2007).
Hu, Z. et al. A cloning and expression system to probe T-cell receptor specificity and assess functional avidity to neoantigens. Blood 132, 1911–1921 (2018).
Picelli, S. et al. Full-length RNA-seq from single cells using Smart-seq2. Nat. Protoc. 9, 171–181 (2014).
Dodt, M., Roehr, J. T., Ahmed, R. & Dieterich, C. FLEXBAR-flexible barcode and adapter processing for next-generation sequencing platforms. Biology 1, 895–905 (2012).
Liao, Y., Wang, J., Jaehnig, E. J., Shi, Z. & Zhang, B. WebGestalt 2019: gene set analysis toolkit with revamped UIs and APIs. Nucleic Acids Res. 47, W199–W205 (2019).
Li, S. et al. RNase H-dependent PCR-enabled T-cell receptor sequencing for highly specific and efficient targeted sequencing of T-cell receptor mRNA for single-cell and repertoire analysis. Nat. Protoc. 14, 2571–2594 (2019).
Hoof, I. et al. NetMHCpan, a method for MHC class I binding prediction beyond humans. Immunogenetics 61, 1–13 (2009).
Lundegaard, C., Lund, O. & Nielsen, M. Prediction of epitopes using neural network based methods. J. Immunol. Methods 374, 26–34 (2011).
Abelin, J. G. et al. Defining HLA-II ligand processing and binding rules with mass spectrometry enhances cancer epitope prediction. Immunity 51, 766–779 (2019).
Jurtz, V. et al. NetMHCpan-4.0: improved peptide-MHC class I interaction predictions integrating eluted ligand and peptide binding affinity data. J. Immunol. 199, 3360–3368 (2017).
Acknowledgements
The authors thank J. Russell, M. Manos, M. Severgnini and the Center for Immuno-Oncology staff, M. Copersino (Regulatory Affairs), B. Meyers, C. Harvey and S. Bartel (Clinical Pharmacy), M. Bowden (Center for Molecular Oncologic Pathology), O. Sturtevant, H. Negre, S.Y. Kim and M.A. Kelley (Cell Manipulation Core Facility), the Pasquarello Tissue Bank (all at DFCI), T. Bowman (DFHCC Specialized Histopathology Core Laboratory), M. Harden, N. Lennon, S. Gabriel, S. Pollack (the Broad Institute’s Biological Samples, Genetic Analysis and Genome Sequencing Platform), J. Ritz (DFCI) and I. Leshchiner, G. Getz (Broad Institute), for discussions. This research was made possible by a generous gift from the Blavatnik Family Foundation, and was supported by grants from the National Institutes of Health (NIH/NCI (R21 CA216772-01A1 and NCI-SPORE-2P50CA101942-11A1 (to D.B.K.); U24CA224331 and R01CA155010 (to C.J.W.); NCI-R50 RCA211482A (to S.A.S.)); NCI-R50 CA251956 (to S.L.); NCI-R01 CA229261 (to P.A.O.); NCI P01 CA163222; NCI-R01 CA238039 (to K.W.W.); 5P30 CA006516 (to A.G.H., R.R. and D.N.) and NCI-K12CA090354 (to J.B.I.)); a Team Science Award from the Melanoma Research Alliance (to C.J.W. and P.A.O.); the Francis and Adele Kittredge Family Immuno-Oncology and Melanoma Research Fund (to P.A.O.); the Faircloth Family Research Fund (to P.A.O.); the Bender Family Research Fund (to P.A.O.), and the DFCI Center for Cancer Immunotherapy Research fellowship and 5 T32 CA 207021-3 (to Z.H. and A.M.L.); a Physician-Scientist Training Award from the Damon Runyon Cancer Research Foundation (to P.B.); an Amy Strelzer Manasevit Scholar Award from the Be The Match Foundation (to P.B.); an American Society of Hematology Fellow Scholar Award (to P.B.); an NSF Graduate Research Fellowships Program fellowship (to R.H.); a Kay Kendall Leukaemia Fund Fellowship (to S.H.G.). L.R.O. is funded by The Free Research Fund Denmark (8048-00078A). C.J.W. is a scholar of the Leukemia and Lymphoma Society. We also acknowledge a gift from a donor to the Developing Innovative Immunological Therapies for Intractable Cancers Fund. This work was further supported in part by The G. Harold and Leila Y. Mathers Foundation and the Bridge Project, a partnership between the Koch Institute for Integrative Cancer Research at MIT and the Dana-Farber/Harvard Cancer Center, the Howard Hughes Medical Institute Medical Research Fellows Program and the Novo Nordisk Foundation (grant agreement NNF14CC0001).
Author information
Authors and Affiliations
Contributions
P.A.O. was the Principal Investigator and IND holder. C.J.W., N.H., P.A.O. and E.F.F. directed the overall study design. Z.H. and D.E.L. designed and performed experimental and data analysis together with S.L., G.O., J.L., T.H., S.G., W.Z., L.P., P.C.L., P.B., K.J.L., D.H.B. and D.B.K; J.S., S.A.S. and E.F.F. analyzed sequencing data and selected neoantigen targets; A.M.L., J.P. and K.W. designed and generated tetramers; R.R., A.G.H. and D.N. designed and performed statistical analyses; O.O. and K.S. coordinated clinical research; P.A.O., E.I.B. and C.H.Y. provided patient samples; J.B.I., Z.C. and S.J.R. performed pathology review; R.H. and B.L.P. generated assay peptides; R.L.A., J.F., S.S., J.S., L.E., M.U., S.A.S. and L.R.O. performed computational analysis; N.H., C.J.W. and E.F.F. developed the overall program strategy. Z.H., D.E.L., E.F.F., C.J.W. and P.A.O. wrote the manuscript; all authors discussed and interpreted results.
Corresponding author
Ethics declarations
Competing interests
Z.H. is a current employee of ElevateBio. J.S. is a current employee of Moderna Therapeutics. E.F.F. is an equity holder and consultant for BioNTech, and equity holder and SAB member of BioEntre. N.H. and C.J.W. are equity holders of BioNTech. N.H. is a consultant for Related Sciences. P.A.O. has received research funding from and has advised Neon Therapeutics, Bristol-Meyers Squibb, Merck, CytomX, Pfizer, Novartis, Celldex, Amgen, Array, AstraZeneca/MedImmune, Armo BioSciences and Roche/Genentech. C.J.W. is subject to a conflict of interest management plan for the reported studies because of her former competing financial interests in Neon Therapeutics, which was acquired by BioNTech. Under this plan, C.J.W. may not access identifiable data for human subjects or otherwise participate directly in the Institutional Review Board-approved protocol reported herein. C.J.W.’s contributions to the overall strategy and data analyses occurred on a de-identified basis. Patent applications have been filed on aspects of the described work entitled as follows: ‘Compositions and methods for personalized neoplasia vaccines’ (N.H., E.F.F. and C.J.W.), ‘Methods for identifying tumour specific neoantigens’ (N.H. and C.J.W.), ‘Formulations for neoplasia vaccines’ (E.F.F.) and ‘Combination therapy for neoantigen vaccine’ (N.H., C.J.W. and E.F.F.). The DFCI, the lead site of this trial, has a proprietary and financial interest in the personalized neoantigen vaccine. P.B. reports equity in Agenus, Amgen, Breakbio Corp., Johnson & Johnson, Exelixis and BioNTech. S.J.R. receives research support from Merck, Bristol Myers Squibb, Affimed and KITE/Gilead, and is on a scientific advisory board for Immunitas Therapeutics. S.A.S. reported nonfinancial support from Bristol-Myers Squibb outside the submitted work. S.A.S. also previously advised and has received consulting fees from Neon Therapeutics and reported equity in Agenus Inc., Agios Pharmaceuticals, Breakbio Corp., Bristol-Myers Squibb and Lumos Pharma, outside the submitted work. B.L.P. is a founder of Resolute Bio and Amide Technologies; both companies develop protein and peptide therapeutics. E.I.B. consults for Apexigen, Novartis, Partner Therapeutics and receives clinical trial support from Eli Lilly, Novartis, BMS, Genentech and BVD. K.W.W. serves on the scientific advisory board of TCR2 Therapeutics, T-Scan Therapeutics, SQZ Biotech, Nextechinvest and receives sponsored research funding from Novartis. He is a co-founder of Immunitas, a biotech company. These activities are not related to the research reported in this publication. D.B.K. has previously advised Neon Therapeutics and has received consulting fees from Neon Therapeutics. D.B.K. also owns equity in Aduro Biotech, Agenus, Armata Pharmaceuticals, Breakbio, BioMarin Pharmaceutical, Bristol Myers Squibb, Celldex Therapeutics, Editas Medicine, Exelixis, Gilead Sciences, IMV, Lexicon Pharmaceuticals, Moderna and Regeneron Pharmaceuticals. BeiGene, a Chine biotech company, supports unrelated research at the Translational Immunogenomics Laboratory. The remaining authors declare no competing interests.
Additional information
Peer review information Saheli Sadanand was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Genomic and immunofluorescence analysis of pre-vaccination and recurrent tumors.
a. Evolution of tumor clones post-NeoVax treatment. Top panel. Sites of primary and relapse tumors in the five patients. Relapse tissue sites are different from the primary in all patients except Pt. 3. Middle panel. Change in cancer cell fraction (CCF) of tumor clones (depicted by different colors) between the pre- and post-vaccination time points (T0 and T1 respectively). Gene targets of the vaccine are indicated next to their corresponding clones. Bottom panel. Phylogenetic relationship between the different clones evolving from the main clonal population (common ancestor). Known cancer drivers are indicated next to their corresponding clones. b. The ARHGEF15, MECOM, and NLRC4 mutations originally targeted by neoantigen vaccination for Pt. 1 are not found in the recurrent tumor specimen, as visualized by the IGV22 c. Multiplex immunofluorescence staining for SOX10, CD8, FOXP3, PD-1, and PD-L1. In the left panel, changes in 1) the cell densities of CD8+ and FOXP3+ TILs, 2) the ratio of FOXP3+ to CD8+ TILs, 3) the percentages of CD8+ TILs and FOXP3+ TILs expressing PD-1, and 4) the PD-L1+expression of SOX10+ melanoma cells are portrayed between pre-vaccine versus recurrent tumor samples for 4 patients with available paired tumor specimens. Pts. 3 and 5 (red lines) had late recurrences, while patients 2 and 6 (black lines) had recurrence during vaccinations and 4 weeks after completion of vaccinations, respectively. Data were derived from 5 to 11 fields of view (median 7) per sample, displayed as mean +/- standard error, and compared using two-sided Wilcoxon rank sum tests. d. Representative multiplexed immunofluorescence micrographs (from among 5 to 11 fields of view per sample) from pre-vaccine versus recurrent tumor samples for the 4 patients with paired tumor specimens. Scale bar = 20 μm.
Extended Data Fig. 2 Vaccination induces strong multi-functional CD4+ T cell responses in two additional patients with high-risk melanoma.
a. Exemplary schema of immunizing (IMP), assay (ASP), and epitope (EPT) peptides. Mutated amino acid is shaded. Each predicted epitope peptide is in colored text and its location is underlined below the IMP peptide. b. PBMCs collected pre- and post- vaccination were tested with individual peptides after one round of in vitro stimulation by IFN-γ ELISpot using week 16 post-vaccination PBMCs, tested in triplicate wells per peptide (error bars, s.e.m.). Only results from positive peptides are shown. c. Deconvolution of T cell reactivity against individual ASP after one round of in vitro stimulation by IFN-γ ELISpot using week 16 post-vaccination PBMCs, tested in triplicate wells per peptide (error bars, s.e.m.). Responses were scored positive if spot-forming units (s.f.u) were at least 2.5-fold over the DMSO control. d. Dual chromogenic immunohistochemical staining of FFPE tumor samples from Pts. 11 and 12 (see Methods for details) for HLA class I and HLA class II. Red: SOX10 (melanoma transcription factor); brown: HLA class I or class II. Representative images of 5 to 11 fields of view (median 7) are shown. e. Summary of immunohistochemical results of seven patients with available FFPE tissue. Semi-quantitative scoring was performed for the intensity of positive staining of melanoma cell membranes for class I or II (0, negative; 1, weak; 2, moderate; 3, strong) and for the percentage of positive staining malignant cells (0–100%). A cumulative H score was obtained by multiplying intensity score by the percentage of malignant cells with positive staining.
Extended Data Fig. 3 Mapping of CD4+ and CD8+ T cell responses to individual ASP and EPT to the IMP for Pts. 11 and 12.
ASP covering the IMP are shown for the IMP that induced T cell responses in Pts. 11 and 12. T cells from week 16 PBMCs were tested. Red bold and shading: mutated amino acids, absent in IMP arising from neoORFs. ((Supplementary Dataset 4). Blue font: peptides that generated a T cell response after one round of in vitro pre-stimulation with individual peptides.
Extended Data Fig. 4 Neoantigen-specific CD4+ T cells are isolated at serial time points after vaccination using tetramer staining and harbor diverse TCR clonotypes.
a. IFN-γ secretion measured by ELISpot from neoantigen-specific T cells co-cultured with B cells nucleofected with minigenes (MG) encoding wildtype or mutant neoantigens chosen for tetramers, with and without anti-HLA DR antibodies (“block”), tested in duplicate wells/condition for Pt. 1 and triplicate wells/condition for all other Pts (error bars, s.e.m.) (figure from our previous publication1). b. Ex vivo HLA class II tetramer staining of Pts. 1, 3 and 5 CD4+ T cells at a series of time points (pre-vaccination, weeks 3-24) following vaccination. Flow plots were pre-gated on CD4+ T cells. c. Schema of representative single-cell TCR and single-cell RNA sequencing analysis of non-specific CD4+ T cells and neoantigen-reactive CD4+ T cells isolated from pre-vaccination PBMCs and post-vaccination PBMCs, respectively, of Pt. 3. d. All TCR clonotypes observed in tetramer-positive T cells generated from PBMCs of Pts. 3, 4 and 5 based on single-cell-targeted TCRαβ sequencing. +: antigen-reactive following mut-ADAMT27 peptide stimulation of selected TCR clonotypes engineered into allogeneic T cells, -: antigen-non reactive.
Extended Data Fig. 5 Neoantigen-specific CD4+ T cells exhibit transcriptional changes through vaccination.
a. Quantification of tetramer-specific or non-tetramer-specific (pre-vaccination) CD4+ T cells isolated at each time point colored by patient. b. Quantification of tetramer-specific or non-tetramer specific (pre-vaccination) CD4+ T cells isolated at each time point colored by cluster. c. Additional selected feature plots of cluster marker genes. d. Quality control metrics for all clusters. e. i) Patient membership by cluster (left); ii) Cluster membership by patient (center); and iii) time point membership by cluster (right). f. Numbers of neoantigen-specific CD4+ T cells in each i) patient by cluster (left); ii) cluster by patient (center); and iii) time point by cluster (right). g. Heatmaps generated from single-cell transcriptome analysis of CD4+ neoantigen-specific and non-neoantigen specific T cells from Pts. 3 (n = 383), 4 (n = 469), and 5 (n = 370) showing selected immunologic genes.
Extended Data Fig. 6 TCR reconstruction and expression in T cells for reactivity screening.
T cell receptors were selected upon TCR sequencing of tetramer positive CD4+ T cells sorted from 3 patients (Pt 2, 3, 6). These TCRs represented clonotypes that were observed in more than one cell (either as replicates at a single timepoint or at more than one timepoint) or as singletons (observed as a single replicate at a single timepoint). The full-length TCRA and TCRB chains were cloned into a lentiviral vector and expressed in donor T cells through lentiviral transduction (Methods). Transduced T cells were co-cultured with patient-derived B cell lines immortalized with EBV virus and pulsed with different doses of mutated or wild-type neoantigen peptides. TCR reactivity was measured through detection of CD137 surface expression on CD4+ TCR transduced lymphocytes by flow cytometry. The values in the graphs report the percentage of CD137 positive cells with subtraction of background, measured upon coculture of T cells with patient-derived B cells pulsed with DMSO (negative control). Bulk data is showing IFN-γ secretion by neoantigen-reactive T-cell lines against mutated and wild-type peptides at several doses (figure from previous publication)1, tested in triplicate wells/condition (error bars, s.e.m.).
Extended Data Fig. 7 Summary of all CD4+ and CD8+ T cell responses against neoantigen IMPs across all patients.
For each patient, CD4+ responses are shown above and CD8+ responses below. Immunogenic responses are shown in table format and non-immunogenic epitopes are listed below. In each table, from left to right, are shown the following: (1) light blue: ex vivo immune response detected at week 16 of vaccination, (2) dark blue: in vitro immune response detected at week 16 of vaccination, (3) green: in vitro immune response detected after pembrolizumab (only applicable in Pts 2 and 6; otherwise not applicable (gray), (4) dark red: ex vivo immune response detected long-term, (5) orange: in vitro immune response detected long-term. Numbers are IMP numbers. White numbers indicate the number of ASP (CD4+) and EPT (CD8+) peptides stimulating immune responses. Yellow highlight indicates mutations not found in recurrent tumors (applicable in Pt. 1 only). Note: all ex vivo responses were also detectable in vitro; thus, the in vitro responses shown were not detectable ex vivo.
Extended Data Fig. 8 Induction of polyfunctional neoantigen-specific CD4+ T cell responses after vaccination in Pts. 1 and 3.
a. ASP covering the IMP are shown for the IMP that induced ex vivo T cell responses in Pts. 1 and 3 at week 16. T cells from week 16 PBMCs were tested. Red bold and shading: mutated amino acids. Blue underline: for class II epitopes, predicted epitopes <10th percentile based on the Immune Epitope Database and Analysis Resource (IEDB)-recommended consensus approach combining NN-align, SMM-align, and CombLib if allele predictions are available, otherwise NetMHCIIpan38. Red font, peptides that generated an ex vivo CD4+ T cell response. These data were previously reported1. b. Frequencies of Pt. 3 CD4+ T cells from week 16 and 47 months that were secreting cytokines as measured by ICS after stimulation of PBMCs ex vivo with peptides in Panel a. c. Frequency of PD-1 expression among total, non-cytokine producing, and cytokine-producing CD4+ T cells for Pt. 3. d. Representative flow plot and frequencies of Pt. 1 CD4+ T cells from 55 months that were secreting cytokines as measured by ICS after stimulation of PBMCs ex vivo with peptides in Panel a. e. Frequency of PD-1 expression among total, non-cytokine producing, and cytokine-producing CD4+ T cells for Pt. 1. f. Pie charts depict PD-1 expression, T cell phenotypes, and secretion of individual cytokines among the cytokine-producing CD4+ T cells for Pt. 1. Markers were selected to evaluate cytokine secretion (IFN-γ, IL-2, and TNF-α), activation (PD-1), naïve (blue, CD27+/CD45RA+), effector (red [not visible], CD27-/CD45RA+), central memory (purple, CD27+/CD45RA-), and effector memory (orange, CD27-/CD45RA-) T cell phenotypes.
Extended Data Fig. 9 Mapping of individual ASP and EPT directed CD4+ and CD8+ T cell responses to the non-vaccine IMP and TAAs, and tracking of unique TCR clonotypes identified through single-cell and bulk TCR sequencing during and after vaccination.
a. ASP and EPT covering the non-vaccine IMP that induced T cell responses. Blue font: peptides that generated a T cell response after one round of pre-stimulation with peptides. Red highlight: mutated amino acids. EPT covering the TAA are shown for the TAA that induced T cell responses. Blue underline: assay peptides with class II prediction rank of < 10th percentile by NetMHCIIpan38. Green underline: assay peptides with prediction rank of < 10th percentile by NeonMHC239. Orange underline: assay peptides with class II prediction rank of <10th percentile by both NetMHCIIpan and NeonMHC2. ((Supplementary Datasets 11 and 12). b. TCRαβ clonotypes for Pts. 2-6 originally identified through single-cell TCR sequencing that were identifiable at the long-term time points by bulk TCR sequencing are shown. Beige circles indicate time points of detection by single-cell TCR sequencing. Black circles indicate timepoints of detection by bulk TCR sequencing.
Extended Data Fig. 10 Flow cytometry gating strategy for tetramer staining assays and multiparameter intracellular cytokine staining.
a. Representative flow cytometry gating strategy for tetramer staining assays. Gating scheme was used for assays shown in Figs. 2a and 4a and Extended Data Fig. 4b. b. Representative flow cytometry gating strategy for multiparameter intracellular cytokine staining assay. PD-1 and CD27/CD45RA gating only shown for IFN-γ; similar gating was performed for TNF-α and IL-2. Gating scheme was used for ICS shown in Fig. 5d and Extended Data Fig. 8b–f.
Supplementary information
Supplementary Information
Supplementary Tables 1–6.
Supplementary Data
Supplementary Datasets 1–13
Rights and permissions
About this article
Cite this article
Hu, Z., Leet, D.E., Allesøe, R.L. et al. Personal neoantigen vaccines induce persistent memory T cell responses and epitope spreading in patients with melanoma. Nat Med 27, 515–525 (2021). https://doi.org/10.1038/s41591-020-01206-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-020-01206-4
This article is cited by
-
Refining mutanome-based individualised immunotherapy of melanoma using artificial intelligence
European Journal of Medical Research (2024)
-
Immune characteristics of dedifferentiated retroperitoneal liposarcomas and the reliability of regional samples in evaluating their tumor immune microenvironments
World Journal of Surgical Oncology (2024)
-
Assessment of human leukocyte antigen-based neoantigen presentation to determine pan-cancer response to immunotherapy
Nature Communications (2024)
-
Challenges in developing personalized neoantigen cancer vaccines
Nature Reviews Immunology (2024)
-
PLGA-PEI nanoparticle covered with poly(I:C) for personalised cancer immunotherapy
Drug Delivery and Translational Research (2024)