Abstract
Computerized electrocardiogram (ECG) interpretation plays a critical role in the clinical ECG workflow1. Widely available digital ECG data and the algorithmic paradigm of deep learning2 present an opportunity to substantially improve the accuracy and scalability of automated ECG analysis. However, a comprehensive evaluation of an end-to-end deep learning approach for ECG analysis across a wide variety of diagnostic classes has not been previously reported. Here, we develop a deep neural network (DNN) to classify 12 rhythm classes using 91,232 single-lead ECGs from 53,549 patients who used a single-lead ambulatory ECG monitoring device. When validated against an independent test dataset annotated by a consensus committee of board-certified practicing cardiologists, the DNN achieved an average area under the receiver operating characteristic curve (ROC) of 0.97. The average F1 score, which is the harmonic mean of the positive predictive value and sensitivity, for the DNN (0.837) exceeded that of average cardiologists (0.780). With specificity fixed at the average specificity achieved by cardiologists, the sensitivity of the DNN exceeded the average cardiologist sensitivity for all rhythm classes. These findings demonstrate that an end-to-end deep learning approach can classify a broad range of distinct arrhythmias from single-lead ECGs with high diagnostic performance similar to that of cardiologists. If confirmed in clinical settings, this approach could reduce the rate of misdiagnosed computerized ECG interpretations and improve the efficiency of expert human ECG interpretation by accurately triaging or prioritizing the most urgent conditions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The test dataset used to support the findings of this study is publicly available at https://irhythm.github.io/cardiol_test_set without restriction. Restrictions apply to the availability of the training dataset, which was used under license from iRhythm Technologies, Inc. for the current study. iRhythm Technologies, Inc. will consider requests to access the training data on an individual basis. Any data use will be restricted to noncommercial research purposes, and the data will only be made available on execution of appropriate data use agreements.
Change history
24 January 2019
In the version of this article originally published, the x axis labels in Fig. 1a were incorrect. The labels originally were ‘Specificity,’ but should have been ‘1 – Specificity.’ Also, the x axis label in Fig. 2b was incorrect. It was originally ‘DNN predicted label,’ but should have been ‘Average cardiologist label.’ The errors have been corrected in the PDF and HTML versions of this article.
References
Schläpfer, J. & Wellens, H. J. Computer-interpreted electrocardiograms: benefits and limitations. J. Am. Coll. Cardiol. 70, 1183–1192 (2017).
LeCun, Y., Bengio, Y. & Hinton, G. Deep learning. Nature 521, 436–444 (2015).
Holst, H., Ohlsson, M., Peterson, C. & Edenbrandt, L. A confident decision support system for interpreting electrocardiograms. Clin. Physiol. 19, 410–418 (1999).
Schlant, R. C. et al. Guidelines for electrocardiography. A report of the American College of Cardiology/American Heart Association Task Force on assessment of diagnostic and therapeutic cardiovascular procedures (Committee on Electrocardiography). J. Am. Coll. Cardiol. 19, 473–481 (1992).
Shah, A. P. & Rubin, S. A. Errors in the computerized electrocardiogram interpretation of cardiac rhythm. J. Electrocardiol. 40, 385–390 (2007).
Guglin, M. E. & Thatai, D. Common errors in computer electrocardiogram interpretation. Int. J. Cardiol. 106, 232–237 (2006).
Poon, K., Okin, P. M. & Kligfield, P. Diagnostic performance of a computer-based ECG rhythm algorithm. J. Electrocardiol. 38, 235–238 (2005).
Amodei, D. et al. Deep Speech 2: end-to-end Speech recognition in English and Mandarin. In Proc. 33rd International Conference on Machine Learning, 173–182 (2016).
He, K., Zhang, X., Ren, S. & Sun, J. Delving deep into rectifiers: surpassing human-level performance on ImageNet classification. In Proc. International Conference on Computer Vision, 1026–1034 (IEEE, 2015).
Silver, D. et al. Mastering the game of Go with deep neural networks and tree search. Nature 529, 484–489 (2016).
Gulshan, V. et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA 316, 2402–2410 (2016).
Esteva, A. Dermatologist-level classification of skin cancer with deep neural networks. Nature 542, 115–118 (2017).
Poungponsri, S. & Yu, X. An adaptive filtering approach for electrocardiogram (ECG) signal noise reduction using neural networks. Neurocomputing 117, 206–213 (2013).
Ochoa, A., Mena, L. J. & Felix, V. G. Noise-tolerant neural network approach for electrocardiogram signal classification. In Proc. 3rd International Conference on Compute and Data Analysis, 277–282 (Association for Computing Machinery, 2017).
Mateo, J. & Rieta, J. J. Application of artificial neural networks for versatile preprocessing of electrocardiogram recordings. J. Med. Eng. Technol. 36, 90–101 (2012).
Pourbabaee, B., Roshtkhari, M. J. & Khorasani, K. Deep convolutional neural networks and learning ECG features for screening paroxysmal atrial fibrillation patients. IEEE Trans. Syst. Man Cybern. Syst. 99, 1–10 (2017).
Javadi, M., Arani, S. A., Sajedin, A. & Ebrahimpour, R. Classification of ECG arrhythmia by a modular neural network based on mixture of experts and negatively correlated learning. Biomed. Signal Process. Control 8, 289–296 (2013).
Acharya, U. R. et al. A deep convolutional neural network model to classify heartbeats. Comput. Biol. Med. 89, 389–396 (2017).
Banupriya, C. V. & Karpagavalli, S. Electrocardiogram beat classification using probabilistic neural network. In Proc. Machine Learning: Challenges and Opportunities Ahead 31–37 (2014).
Al Rahhal, M. M. et al. Deep learning approach for active classification of electrocardiogram signals. Inf. Sci. (NY) 345, 340–354 (2016).
Acharya, U. R. et al. Automated detection of arrhythmias using different intervals of tachycardia ECG segments with convolutional neural network. Inf. Sci. (NY) 405, 81–90 (2017).
Zihlmann, M., Perekrestenko, D. & Tschannen, M. Convolutional recurrent neural networks for electrocardiogram classification. Comput. Cardiol. https://doi.org/10.22489/CinC.2017.070-060 (2017).
Xiong, Z., Zhao, J. & Stiles, M. K. Robust ECG signal classification for detection of atrial fibrillation using a novel neural network. Comput. Cardiol. https://doi.org/10.22489/CinC.2017.066-138 (2017).
Clifford, G. et al. AF classification from a short single lead ECG recording: the PhysioNet/Computing in Cardiology Challenge 2017. Comput. Cardiol. https://doi.org/10.22489/CinC.2017.065-469 (2017).
Teijeiro, T., Garcia, C. A., Castro, D. & Felix, P. Arrhythmia classification from the abductive interpretation of short single-lead ECG records. Comput. Cardiol. https://doi.org/10.22489/CinC.2017.166-054 (2017).
Goldberger, A. L. et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation 101, E215–E220 (2000).
Turakhia, M. P. et al. Diagnostic utility of a novel leadless arrhythmia monitoring device. Am. J. Cardiol. 112, 520–524 (2013).
Hand, D. J. & Till, R. J. A simple generalisation of the area under the ROC curve for multiple class classification problems. Mach. Learn. 45, 171–186 (2001).
Smith, M. D. et al.in Best Care at Lower Cost: the Path to Continuously Learning Health Care in America (National Academies Press,: Washington, 2012).
Lyon, A., Mincholé, A., Martínez, J. P., Laguna, P. & Rodriguez, B. Computational techniques for ECG analysis and interpretation in light of their contribution to medical advances. J. R. Soc. Interface 15, pii: 20170821 (2018).
Carrara, M. et al. Heart rate dynamics distinguish among atrial fibrillation, normal sinus rhythm and sinus rhythm with frequent ectopy. Physiol. Meas. 36, 1873–1888 (2015).
Zhou, X., Ding, H., Ung, B., Pickwell-MacPherson, E. & Zhang, Y. Automatic online detection of atrial fibrillation based on symbolic dynamics and Shannon entropy. Biomed. Eng. Online 13, 18 (2014).
Hong, S. et al. ENCASE: an ENsemble ClASsifiEr for ECG Classification using expert features and deep neural networks. Comput. Cardiol. https://doi.org/10.22489/CinC.2017.178-245 (2017).
Nahar, J., Imam, T., Tickle, K. S. & Chen, Y. P. Computational intelligence for heart disease diagnosis: a medical knowledge driven approach. Expert Syst. Appl. 40, 96–104 (2013).
Cubanski, D., Cyganski, D., Antman, E. M. & Feldman, C. L. A neural network system for detection of atrial fibrillation in ambulatory electrocardiograms. J. Cardiovasc. Electrophysiol. 5, 602–608 (1994).
Andreotti, F., Carr, O., Pimentel, M. A. F., Mahdi, A. & De Vos, M. Comparing feature-based classifiers and convolutional neural networks to detect arrhythmia from short segments of ECG. Comput. Cardiol. https://doi.org/10.22489/CinC.2017.360-239 (2017).
Xu, S. S., Mak, M. & Cheung, C. Towards end-to-end ECG classification with raw signal extraction and deep neural networks. IEEE J. Biomed. Health Informatics 14, 1 (2018).
Ong, S. L., Ng, E. Y. K., Tan, R. S. & Acharya, U. R. Automated diagnosis of arrhythmia using combination of CNN and LSTM techniques with variable length heart beats. Comput. Biol. Med. 102, 278–287 (2018).
Shashikumar, S. P., Shah, A. J., Clifford, G. D. & Nemati, S. Detection of paroxysmal atrial fibrillation using attention-based bidirectional recurrent neural networks. In Proc. 24th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining, 715–723 (Association for Computing Machinery, 2018).
Xia, Y., Wulan, N., Wang, K. & Zhang, H. Detecting atrial fibrillation by deep convolutional neural networks. Comput. Biol. Med. 93, 84–92 (2018).
He, K., Zhang, X., Ren, S. & Sun, J. Identity mappings in deep residual networks. In Proc. European Conference on Computer Vision, 630–645 (Springer, 2016).
Ioffe, S. & Szegedy, C. Batch normalization: accelerating deep network training by reducing internal covariate shift. In Proc. International Conference on Machine Learning, 448–456 (2015).
He, K., Zhang, X., Ren, S. & Sun, J. Deep residual learning for image recognition. In Proc. IEEE Conference on Computer Vision and Pattern Recognition, 770–778 (IEEE, 2016).
Srivastava, N., Hinton, G., Krizhevsky, A., Sutskever, I. & Salakhutdinov, R. Dropout: a simple way to prevent neural networks from overfitting. J. Mach. Learn. Res. 15, 1929–1958 (2014).
Kingma, D. P. & Ba, J. L. Adam: a method for stochastic optimization. In Proc. International Conference on Learning Representations 1–15 (2015).
Hochreiter, S. & Schmidhuber, J. Long short-term memory. Neural Comput. 9, 1735–1780 (1997).
Fawcett, T. An introduction to ROC analysis. Pattern Recognit. Lett. 27, 861–874 (2006).
Hanley, J. A. & McNeil, B. J. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148, 839–843 (1983).
Saito, T. & Rehmsmeier, M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE 10, e0118432 (2015).
Acknowledgements
iRhythm Technologies, Inc. provided financial support for the data annotation in this work. M.H. and C.B. are employees of iRhythm Technologies, Inc. A.Y.H. was funded by an NVIDIA fellowship. G.H.T. received support from the National Institutes of Health (K23 HL135274). The only financial support provided by iRhythm Technologies, Inc. for this study was for the data annotation. Data analysis and interpretation was performed independently from the sponsor. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
M.H., A.Y.N., A.Y.H., and G.H.T. contributed to the study design. M.H. and C.B. were responsible for data collection. P.R. and A.Y.H. ran the experiments and created the figures. G.H.T., P.R., and A.Y.H. contributed to the analysis. G.H.T., A.Y.H., and M.P.T. contributed to the data interpretation and to the writing. G.H.T., M.P.T., and A.Y.N. advised and A.Y.N. was the senior supervisor of the project. All authors read and approved the submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
M.H. and C.B. are employees of iRhythm Technologies, Inc. G.H.T. is an advisor to Cardiogram, Inc. M.P.T. is a consultant to iRhythm Technologies, Inc. None of the other authors have potential conflicts of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Deep Neural Network architecture.
Our deep neural network consisted of 33 convolutional layers followed by a linear output layer into a softmax. The network accepts raw ECG data as input (sampled at 200 Hz, or 200 samples per second), and outputs a prediction of one out of 12 possible rhythm classes every 256 input samples.
Extended Data Fig. 2 Receiver operating characteristic curves for deep neural network predictions on 12 rhythm classes.
Individual cardiologist performance is indicated by the red crosses and averaged cardiologist performance is indicated by the green dot. The line represents the ROC curve of model performance. AF-atrial fibrillation/atrial flutter; AVB- atrioventricular block; EAR-ectopic atrial rhythm; IVR-idioventricular rhythm; SVT-supraventricular tachycardia; VT-ventricular tachycardia. n = 7,544 where each of the 328 30-second ECGs received 23 sequence-level predictions.
Supplementary information
Supplementary Information
Supplementary Tables 1–7
Source data
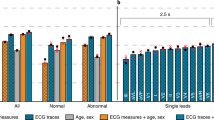
Source data Fig. 1
Sensitivity, specificity and PPV values at different operating points as well as the individual and average cardiologist metrics for the arrhythmias in the figure.
Source data Fig. 2
Absolute confusions counts between arrhythmias for both the model and the cardiologists.
Extended data Fig. 2
Sensitivity and specificity values at different operating points as well as the individual and average cardiologist metrics for all of the arrhythmias.
Rights and permissions
About this article
Cite this article
Hannun, A.Y., Rajpurkar, P., Haghpanahi, M. et al. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat Med 25, 65–69 (2019). https://doi.org/10.1038/s41591-018-0268-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-018-0268-3
This article is cited by
-
Detection of biomagnetic signals from induced pluripotent stem cell-derived cardiomyocytes using deep learning with simulation data
Scientific Reports (2024)
-
Adopting artificial intelligence in cardiovascular medicine: a scoping review
Hypertension Research (2024)
-
Cardiologist-level interpretable knowledge-fused deep neural network for automatic arrhythmia diagnosis
Communications Medicine (2024)
-
Tuning attention based long-short term memory neural networks for Parkinson’s disease detection using modified metaheuristics
Scientific Reports (2024)
-
Congenital heart disease detection by pediatric electrocardiogram based deep learning integrated with human concepts
Nature Communications (2024)