Abstract
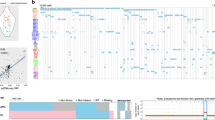
Myelodysplastic syndromes (MDS) frequently progress to acute myeloid leukemia (AML); however, the cells leading to malignant transformation have not been directly elucidated. As progression of MDS to AML in humans provides a biological system to determine the cellular origins and mechanisms of neoplastic transformation, we studied highly fractionated stem cell populations in longitudinal samples of patients with MDS who progressed to AML. Targeted deep sequencing combined with single-cell sequencing of sorted cell populations revealed that stem cells at the MDS stage, including immunophenotypically and functionally defined pre-MDS stem cells (pre-MDS-SC), had a significantly higher subclonal complexity compared to blast cells and contained a large number of aging-related variants. Single-cell targeted resequencing of highly fractionated stem cells revealed a pattern of nonlinear, parallel clonal evolution, with distinct subclones within pre-MDS-SC and MDS-SC contributing to generation of MDS blasts or progression to AML, respectively. Furthermore, phenotypically aberrant stem cell clones expanded during transformation and stem cell subclones that were not detectable in MDS blasts became dominant upon AML progression. These results reveal a crucial role of diverse stem cell compartments during MDS progression to AML and have implications for current bulk cell–focused precision oncology approaches, both in MDS and possibly other cancers that evolve from premalignant conditions, that may miss pre-existing rare aberrant stem cells that drive disease progression and leukemic transformation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The high-throughput DNA sequencing data have been deposited in the database of Genotypes and Phenotypes (dbGaP) .
Change history
19 December 2018
In the version of this article originally published, Ulrich Steidl’s name was listed as “and Ulrich Steidl.” His name has been updated to “Ulrich Steidl.” The error has been fixed in the print, PDF and HTML versions of this article.
References
Greenberg, P. L. et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood 120, 2454–2465 (2012).
Ades, L., Itzykson, R. & Fenaux, P. Myelodysplastic syndromes. Lancet 383, 2239–2252 (2014).
Fialkow, P. J. et al. Clonal development, stem-cell differentiation, and clinical remissions in acute nonlymphocytic leukemia. N. Engl. J.Med. 317, 468–473 (1987).
Nilsson, L. et al. Involvement and functional impairment of the CD34+CD38-Thy-1+ hematopoietic stem cell pool in myelodysplastic syndromes with trisomy 8. Blood 100, 259–267 (2002).
Steidl, U. et al. Essential role of Jun family transcription factors in PU.1 knockdown-induced leukemic stem cells. Nat. Genet. 38, 1269–1277 (2006).
Will, B. et al. Stem and progenitor cells in myelodysplastic syndromes show aberrant stage-specific expansion and harbor genetic and epigenetic alterations. Blood 120, 2076–2086 (2012).
Jan, M. et al. Clonal evolution of preleukemic hematopoietic stem cells precedes human acute myeloid leukemia. Sci. Transl. Med. 4, 149ra118 (2012).
Pang, W. W. et al. Hematopoietic stem cell and progenitor cell mechanisms in myelodysplastic syndromes. Proc. Natl Acad. Sci. USA 110, 3011–3016 (2013).
Corces-Zimmerman, M. R., Hong, W. J., Weissman, I. L., Medeiros, B. C. & Majeti, R. Preleukemic mutations in human acute myeloid leukemia affect epigenetic regulators and persist in remission. Proc. Natl Acad. Sci. USA 111, 2548–2553 (2014).
Shlush, L. I. et al. Identification of pre-leukaemic haematopoietic stem cells in acute leukaemia. Nature 506, 328–333 (2014).
Will, B. et al. Minimal PU.1 reduction induces a preleukemic state and promotes development of acute myeloid leukemia. Nat. Med. 21, 1172–1181 (2015).
Walter, M. J. et al. Clonal architecture of secondary acute myeloid leukemia. N. Engl. J. Med. 366, 1090–1098 (2012).
Walter, M. J. et al. Clonal diversity of recurrently mutated genes in myelodysplastic syndromes. Leukemia 27, 1275–1282 (2013).
Makishima, H. et al. Dynamics of clonal evolution in myelodysplastic syndromes. Nat. Genet. 49, 204–212 (2017).
Goardon, N. et al. Coexistence of LMPP-like and GMP-like leukemia stem cells in acute myeloid leukemia. Cancer Cell 19, 138–152 (2011).
Jordan, C. et al. The interleukin-3 receptor alpha chain is a unique marker for human acute myelogenous leukemia stem cells. Leukemia 14, 1777 (2000).
Barreyro, L. et al. Overexpression of IL-1 receptor accessory protein in stem and progenitor cells and outcome correlation in AML and MDS. Blood 120, 1290–1298 (2012).
Mitchell, K. et al. IL1RAP potentiates multiple oncogenic signaling pathways in AML. J. Exp. Med. 215, 1709–1727 (2018).
Jan, M. et al. Prospective separation of normal and leukemic stem cells based on differential expression of TIM3, a human acute myeloid leukemia stem cell marker. Proc. Natl Acad. Sci. USA 108, 5009–5014 (2011).
Chung, S. S. et al. CD99 is a therapeutic target on disease stem cells in myeloid malignancies. Sci.Transl. Med. 9, eaaj2025 (2017).
He, J. et al. Integrated genomic DNA/RNA profiling of hematologic malignancies in the clinical setting. Blood 127, 3004–3014 (2016).
McGranahan, N. et al. Clonal status of actionable driver events and the timing of mutational processes in cancer evolution. Sci. Transl. Med. 7, 283ra254 (2015).
Blokzijl, F. et al. Tissue-specific mutation accumulation in human adult stem cells during life. Nature 538, 260–264 (2016).
Adams, P. D., Jasper, H. & Rudolph, K. L. Aging-induced stem cell mutations as drivers for disease and cancer. Cell. Stem. Cell. 16, 601–612 (2015).
Rossi, D. J. et al. Deficiencies in DNA damage repair limit the function of haematopoietic stem cells with age. Nature 447, 725–729 (2007).
Mandal, P. K., Blanpain, C. & Rossi, D. J. DNA damage response in adult stem cells: pathways and consequences. Nat. Rev. Mol. Cell Biol. 12, 198–202 (2011).
Mohrin, M. et al. Hematopoietic stem cell quiescence promotes error-prone DNA repair and mutagenesis. Cell. Stem. Cell. 7, 174–185 (2010).
Miller, C. A. et al. SciClone: inferring clonal architecture and tracking the spatial and temporal patterns of tumor evolution. PLoS Comput. Biol. 10, e1003665 (2014).
Yanagisawa, B., Ghiaur, G., Smith, B. D. & Jones, R. J. Translating leukemia stem cells into the clinical setting: harmonizing the heterogeneity. Exp. Hematol. 44, 1130–1137 (2016).
Haferlach, T. et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia 28, 241–247 (2014).
Cancer Genome Atlas Research, N. et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N. Engl. J. Med. 368, 2059–2074 (2013).
Xie, M. et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat. Med. 20, 1472–1478 (2014).
Genovese, G. et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N. Engl. J. Med. 371, 2477–2487 (2014).
Jaiswal, S. et al. Age-related clonal hematopoiesis associated with adverse outcomes. N. Engl. J. Med. 371, 2488–2498 (2014).
Arends, C. M. et al. Hematopoietic lineage distribution and evolutionary dynamics of clonal hematopoiesis. Leukemia 32, 1908–1919 (2018).
Abelson, S. et al. Prediction of acute myeloid leukaemia risk in healthy individuals. Nature 559, 400–404 (2018).
Desai, P. et al. Somatic mutations precede acute myeloid leukemia years before diagnosis. Nat. Med. 24, 1015 (2018).
Herbaux, C. et al. Incidence of ATRX mutations in myelodysplastic syndromes, the value of microcytosis. Am. J. Hematol. 90, 737–738 (2015).
Steensma, D. P., Higgs, D. R., Fisher, C. A. & Gibbons, R. J. Acquired somatic ATRX mutations in myelodysplastic syndrome associated with alpha thalassemia (ATMDS) convey a more severe hematologic phenotype than germline ATRX mutations. Blood 103, 2019–2026 (2004).
Bacher, U., Haferlach, T., Kern, W., Haferlach, C. & Schnittger, S. A comparative study of molecular mutations in 381 patients with myelodysplastic syndrome and in 4130 patients with acute myeloid leukemia. Haematologica 92, 744–752 (2007).
Shastri, A., Will, B., Steidl, U. & Verma, A. Stem and progenitor cell alterations in myelodysplastic syndromes. Blood 129, 1586–1594 (2017).
Thomas, D. & Majeti, R. Biology and relevance of human acute myeloid leukemia stem cells. Blood 129, 1577–1585 (2017).
McIntosh, B. E. et al. Nonirradiated NOD,B6.SCID Il2rγ-/- Kit(W41/W41) (NBSGW) mice support multilineage engraftment of human hematopoietic cells. Stem Cell Reports 4, 171–180 (2015).
Woll, P. S. et al. Myelodysplastic syndromes are propagated by rare and distinct human cancer stem cells in vivo. Cancer Cell. 25, 794–808 (2014).
Terwijn, M. et al. Leukemic stem cell frequency: a strong biomarker for clinical outcome in acute myeloid leukemia. PLoS ONE 9, e107587 (2014).
Wang, C. et al. Non-lethal ionizing radiation promotes aging-like phenotypic changes of human hematopoietic stem and progenitor cells in humanized mice. PLoS ONE 10, e0132041 (2015).
Lu, R., Czechowicz, A., Seita, J., Jiang, D. & Weissman, I. L. Clonal level lineage commitment pathways of hematopoietic stem cells in vivo. Preprint at https://doi.org/10.1101/262774 (2018).
Hosono, S. et al. Unbiased whole-genome amplification directly from clinical samples. Genome Res. 13, 954–964 (2003).
de Bourcy, C. F. et al. A quantitative comparison of single-cell whole genome amplification methods. PLoS ONE 9, e105585 (2014).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
McKenna, A. et al. The genome analysis toolkit: a mapreduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Cibulskis, K. et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 31, 213–219 (2013).
Garrison, E. & Marth, G. Haplotype-based variant detection from short-read sequencing. Preprint at https://arxiv.org/abs/1207.3907 (2012).
Cingolani, P. et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w(1118); iso-2; iso-3. Fly 6, 80–92 (2012).
Rosenthal, R., McGranahan, N., Herrero, J., Taylor, B. S. & Swanton, C. DeconstructSigs: delineating mutational processes in single tumors distinguishes DNA repair deficiencies and patterns of carcinoma evolution. Genome. Biol. 17, 31 (2016).
Shen, R. & Seshan, V. E. FACETS: allele-specific copy number and clonal heterogeneity analysis tool for high-throughput DNA sequencing. Nucleic Acids Res. 44, e131 (2016).
Popic, V. et al. Fast and scalable inference of multi-sample cancer lineages. Genome. Biol. 16, 91 (2015).
Smith, M.A. et al. E-scape: interactive visualization of single-cell phylogenetics and cancer evolution. Nat. Methods 14, 549–550 (2017).
Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. Preprint at https://arxiv.org/abs/1303.3997 (2013).
Yu, Y., Ceredig, R. & Seoighe, C. LymAnalyzer: a tool for comprehensive analysis of next generation sequencing data of T cell receptors and immunoglobulins. Nucleic Acids Res. 44, e31 (2016).
Acknowledgements
We thank P. Schultes from the Department of Cell Biology for expert technical assistance. We thank A. Fiallo from the Einstein Genomics Core Facility for technical assistance in single-cell targeted sequencing, and S. Maqbool and S. Mi from Einstein Epigenomics Core Facility for assistance in targeted sequencing with the HiSeq platform. We thank V. Thiruthuvanathan from the Department of Cell Biology for assistance in processing the patient samples. We also thank W. Li for advice regarding whole-genome amplification, and F. C. Chan, C. Steidl, and H. Steidl for helpful discussion. This work was supported by NIH grants no. R01CA166429, no. R01CA217092 (to U.S.), no. R01HL139487, no. R01DK103961 (to A.V.), and no. K01DK105134 (to B.W.); Translational Research Program grants from the Leukemia & Lymphoma Society (to U.S. and A.V., respectively); a research grant from the Taub Foundation for MDS Research (to U.S.); and a research grant from the Evans Foundation (to A.V.). J.C. was supported by The Einstein Training Program in Stem Cell Research from the Empire State Stem Cell Fund through New York State Department of Health Contract (no. C30292GG). U.S. is a Research Scholar of the Leukemia and Lymphoma Society and the Diane and Arthur B. Belfer Faculty Scholar in Cancer Research of the Albert Einstein College of Medicine. This work was supported through the Albert Einstein Cancer Center core support grant (no. P30CA013330).
Author information
Authors and Affiliations
Contributions
J.C., U.S., and A.V. designed the study and analyzed and interpreted data. J.C., Y.K., and T.I.T. collected and analyzed clinical samples. J.C., Y.K., D.S., S.N., and B.W. performed the FACS experiments. J.C. and S.N. performed the xenotransplantation assays. J.C. performed the methylcellulose assay and TCR sequencing. J.C. and D.R. performed single-cell targeted sequencing. C.M., A.V., and U.S. designed the targeted capture panel. J.C. analyzed the sequencing data. J.C., A.V., and U.S. wrote the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
U.S. has received research funding from GlaxoSmithKline, Bayer Healthcare, Aileron Therapeutics, and Novartis; has received compensation for consultancy services and for serving on scientific advisory boards from GlaxoSmithKline, Bayer Healthcare, Celgene, Aileron Therapeutics, Stelexis Therapeutics, and Pieris Pharmaceuticals; and has equity ownership in and is serving on the board of directors of Stelexis Therapeutics. A.V. has received research funding from GlaxoSmithKline, Incyte, MedPacto, Novartis, and Eli Lilly and Company, has received compensation as a scientific advisor to Novartis, Stelexis Therapeutics, Acceleron Pharma, and Celgene, and has equity ownership in Stelexis Therapeutics. B.W. has received research support from Novartis Pharmaceuticals.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–15
Supplementary Table 1
Patient characteristics
Supplementary Table 2
Genes for targeted capture sequencing
Supplementary Table 3
Somatic mutations detected by targeted capture sequencing in each patient
Supplementary Table 4
Antibodies for FACS experiments
Supplementary Table 5
Primers for single-cell targeted sequencing with Fluidigm platform
Rights and permissions
About this article
Cite this article
Chen, J., Kao, YR., Sun, D. et al. Myelodysplastic syndrome progression to acute myeloid leukemia at the stem cell level. Nat Med 25, 103–110 (2019). https://doi.org/10.1038/s41591-018-0267-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-018-0267-4
This article is cited by
-
Decoding leukemia at the single-cell level: clonal architecture, classification, microenvironment, and drug resistance
Experimental Hematology & Oncology (2024)
-
TMIGD2 is an orchestrator and therapeutic target on human acute myeloid leukemia stem cells
Nature Communications (2024)
-
Immunophenotypic aberrant hematopoietic stem cells in myelodysplastic syndromes: a biomarker for leukemic progression
Leukemia (2023)
-
Aged hematopoietic stem cells entrap regulatory T cells to create a prosurvival microenvironment
Cellular & Molecular Immunology (2023)
-
Single-cell analysis reveals altered tumor microenvironments of relapse- and remission-associated pediatric acute myeloid leukemia
Nature Communications (2023)