Abstract
A key driver of patients’ well-being and clinical trials for Parkinson’s disease (PD) is the course that the disease takes over time (progression and prognosis). To assess how genetic variation influences the progression of PD over time to dementia, a major determinant for quality of life, we performed a longitudinal genome-wide survival study of 11.2 million variants in 3,821 patients with PD over 31,053 visits. We discover RIMS2 as a progression locus and confirm this in a replicate population (hazard ratio (HR) = 4.77, P = 2.78 × 10−11), identify suggestive evidence for TMEM108 (HR = 2.86, P = 2.09 × 10−8) and WWOX (HR = 2.12, P = 2.37 × 10−8) as progression loci, and confirm associations for GBA (HR = 1.93, P = 0.0002) and APOE (HR = 1.48, P = 0.001). Polygenic progression scores exhibit a substantial aggregate association with dementia risk, while polygenic susceptibility scores are not predictive. This study identifies a novel synaptic locus and polygenic score for cognitive disease progression in PD and proposes diverging genetic architectures of progression and susceptibility.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
A Nature Research Reporting Summary is available for this paper. Human brain cell type-specific expression data from BRAINcode47 RNA-seq data are accessible through a user-friendly webportal at http://www.humanbraincode.org and individual-level data through dbGAP (accession no. phs001556.v1.p1). The gene expression profiles of human tissues used in this study can be downloaded from the GTEx Portal v7 (https://gtexportal.org/). The GWSS summary statistics for the combined analysis of discovery and replicate populations are publicly accessible through the EGA database at https://ega-archive.org/ (accession no. EGAS00001005110). Individual-level genetic data for the NIH-funded Illumina Multi-Ethnic Genotyping Array analyses of the HBS2 and EPIPARK cohorts are accessible in dbGAP with accession no. phs002328.v1.p1 in accordance with NIH Genomic Data Sharing Policy. The WGS and clinical data for PPMI included in this study are publicly available upon request to ppmi@loni.usc.edu through a PPMI Whole Genome Sequencing Data Agreement. Clinical data for PDBP included in this study are publicly available through https://pdbp.ninds.nih.gov. Clinical longitudinal data for the other cohorts included are accessible through appropriate data sharing agreements that protect patient privacy with the institutions that conducted or are conducting study consents and clinical assessments under local institutional review board approvals.
Code availability
Analysis code is available at https://github.com/sixguns1984/GWSS.PDD.
References
Nalls, M. A. et al. Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson’s disease. Nat. Genet. 46, 989–993 (2014).
Chang, D. et al. A meta-analysis of genome-wide association studies identifies 17 new Parkinson’s disease risk loci. Nat. Genet. 49, 1511–1516 (2017).
Wijmenga, C. & Zhernakova, A. The importance of cohort studies in the post-GWAS era. Nat. Genet. 50, 322–328 (2018).
Locascio, J. J. & Atri, A. An overview of longitudinal data analysis methods for neurological research. Dement. Geriatr. Cogn. Dis. Extra 1, 330–357 (2011).
Dorsey, E. R. & Bloem, B. R. The Parkinson pandemic—a call to action. JAMA Neurol. 75, 9–10 (2018).
Liu, G. et al. Specifically neuropathic Gaucher’s mutations accelerate cognitive decline in Parkinson’s. Ann. Neurol. 80, 674–685 (2016).
Liu, G. et al. Prediction of cognition in Parkinson’s disease with a clinical-genetic score: a longitudinal analysis of nine cohorts. Lancet Neurol. 16, 620–629 (2017).
Aarsland, D. et al. Cognitive decline in Parkinson disease. Nat. Rev. Neurol. 13, 217–231 (2017).
Schrag, A., Jahanshahi, M. & Quinn, N. What contributes to quality of life in patients with Parkinson’s disease? J. Neurol. Neurosurg. Psychiatry 69, 308–312 (2000).
Svenningsson, P., Westman, E., Ballard, C. & Aarsland, D. Cognitive impairment in patients with Parkinson’s disease: diagnosis, biomarkers, and treatment. Lancet Neurol. 11, 697–707 (2012).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211 (2003).
Langston, J. W. The Parkinson’s complex: parkinsonism is just the tip of the iceberg. Ann. Neurol. 59, 591–596 (2006).
Williams-Gray, C. H. et al. The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. J. Neurol. Neurosurg. Psychiatry 84, 1258–1264 (2013).
Cilia, R. et al. Survival and dementia in GBA-associated Parkinson’s disease: the mutation matters. Ann. Neurol. 80, 662–673 (2016).
Pang, S., Li, J., Zhang, Y. & Chen, J. Meta-analysis of the relationship between the APOE gene and the onset of Parkinson’s disease dementia. Parkinsons Dis. 2018, 9497147 (2018).
Healy, D. G. et al. Phenotype, genotype, and worldwide genetic penetrance of LRRK2-associated Parkinson’s disease: a case-control study. Lancet Neurol. 7, 583–590 (2008).
Guella, I. et al. alpha-synuclein genetic variability: a biomarker for dementia in Parkinson disease. Ann. Neurol. 79, 991–999 (2016).
Markopoulou, K. et al. Does alpha-synuclein have a dual and opposing effect in preclinical vs. clinical Parkinson’s disease? Parkinsonism Relat. Disord. 20, 584–589 (2014).
Mata, I. F. et al. APOE, MAPT, and SNCA genes and cognitive performance in Parkinson disease. JAMA Neurol. 71, 1405–1412 (2014).
Paul, K. C., Schulz, J., Bronstein, J. M., Lill, C. M. & Ritz, B. R. Association of polygenic risk score with cognitive decline and motor progression in Parkinson disease. JAMA Neurol. 75, 360–366 (2018).
Mata, I. F. et al. Large-scale exploratory genetic analysis of cognitive impairment in Parkinson’s disease. Neurobiol. Aging 56, 211 e1–211 e7 (2017).
Locascio, J. J. et al. Association between alpha-synuclein blood transcripts and early, neuroimaging-supported Parkinson’s disease. Brain 138, 2659–2671 (2015).
Pankratz, N. et al. Meta-analysis of Parkinson’s disease: identification of a novel locus, RIT2. Ann. Neurol. 71, 370–384 (2012).
Jankovic, J. et al. Variable expression of Parkinson’s disease: a base-line analysis of the DATATOP cohort. The Parkinson Study Group. Neurology 40, 1529–1534 (1990).
Ravina, B. et al. A longitudinal program for biomarker development in Parkinson’s disease: a feasibility study. Mov. Disord. 24, 2081–2090 (2009).
Winder-Rhodes, S. E. et al. Glucocerebrosidase mutations influence the natural history of Parkinson’s disease in a community-based incident cohort. Brain 136, 392–399 (2013).
Marinus, J. et al. A short scale for the assessment of motor impairments and disabilities in Parkinson’s disease: the SPES/SCOPA. J. Neurol. Neurosurg. Psychiatry 75, 388–395 (2004).
Breen, D. P., Evans, J. R., Farrell, K., Brayne, C. & Barker, R. A. Determinants of delayed diagnosis in Parkinson’s disease. J. Neurol. 260, 1978–1981 (2013).
Rosenthal, L. S. et al. The NINDS Parkinson’s disease biomarkers program. Mov. Disord. 30, 915–923 (2016).
Writing Group for the NINDS Exploratory Trials in Parkinson Disease (NET-PD) Investigators et al. Effect of creatine monohydrate on clinical progression in patients with Parkinson disease: a randomized clinical trial. JAMA 313, 584–593 (2015).
1000 Genomes Project Consortium et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Browning, S. R. & Browning, B. L. Rapid and accurate haplotype phasing and missing-data inference for whole-genome association studies by use of localized haplotype clustering. Am. J. Hum. Genet. 81, 1084–1097 (2007).
Li, Y., Willer, C. J., Ding, J., Scheet, P. & Abecasis, G. R. MaCH: using sequence and genotype data to estimate haplotypes and unobserved genotypes. Genet. Epidemiol. 34, 816–834 (2010).
Marchini, J., Howie, B., Myers, S., McVean, G. & Donnelly, P. A new multipoint method for genome-wide association studies by imputation of genotypes. Nat. Genet. 39, 906–913 (2007).
Visscher, P. M. et al. 10 years of GWAS discovery: biology, function, and translation. Am. J. Hum. Genet. 101, 5–22 (2017).
Ripatti, S. & Palmgren, J. Estimation of multivariate frailty models using penalized partial likelihood. Biometrics 56, 1016–1022 (2000).
Bulik-Sullivan, B. K. et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295 (2015).
Yang, J. et al. Genomic inflation factors under polygenic inheritance. Eur. J. Hum. Genet. 19, 807–812 (2011).
Dubois, B. et al. Diagnostic procedures for Parkinson’s disease dementia: recommendations from the movement disorder society task force. Mov. Disord. 22, 2314–2324 (2007).
Armstrong, M. J. & Okun, M. S. Diagnosis and treatment of Parkinson disease: a review. JAMA 323, 548–560 (2020).
Kaeser, P. S. et al. RIM proteins tether Ca2+ channels to presynaptic active zones via a direct PDZ-domain interaction. Cell 144, 282–295 (2011).
Liu, C., Kershberg, L., Wang, J., Schneeberger, S. & Kaeser, P. S. Dopamine secretion is mediated by sparse active zone-like release sites. Cell 172, 706–718 e15 (2018).
Mechaussier, S. et al. Loss of function of RIMS2 causes a syndromic congenital cone-rod synaptic disease with neurodevelopmental and pancreatic involvement. Am. J. Hum. Genet. 106, 859–871 (2020).
Powell, C. M. et al. The presynaptic active zone protein RIM1alpha is critical for normal learning and memory. Neuron 42, 143–153 (2004).
Nalls, M. A. et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 18, 1091–1102 (2019).
GTEx, Consortium et al. Genetic effects on gene expression across human tissues. Nature 550, 204–213 (2017).
Dong, X. et al. Enhancers active in dopamine neurons are a primary link between genetic variation and neuropsychiatric disease. Nat. Neurosci. 21, 1482–1492 (2018).
Jiao, H. F. et al. Transmembrane protein 108 is required for glutamatergic transmission in dentate gyrus. Proc. Natl Acad. Sci. USA. 114, 1177–1182 (2017).
Mallaret, M. et al. The tumour suppressor gene WWOX is mutated in autosomal recessive cerebellar ataxia with epilepsy and mental retardation. Brain 137, 411–419 (2014).
Kunkle, B. W. et al. Genetic meta-analysis of diagnosed Alzheimer’s disease identifies new risk loci and implicates Aβ, tau, immunity and lipid processing. Nat. Genet. 51, 414–430 (2019).
Khera, A. V. et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat. Genet. 50, 1219–1224 (2018).
Nalls, M. A. et al. Diagnosis of Parkinson’s disease on the basis of clinical and genetic classification: a population-based modelling study. Lancet Neurol. 14, 1002–1009 (2015).
Lee, J. K., Tran, T. & Tansey, M. G. Neuroinflammation in Parkinson’s disease. J. Neuroimmune Pharmacol. 4, 419–429 (2009).
Johnson, M. E., Stecher, B., Labrie, V., Brundin, L. & Brundin, P. Triggers, facilitators, and aggravators: redefining Parkinson’s disease pathogenesis. Trends Neurosci. 42, 4–13 (2019).
Irwin, D. J. et al. Neuropathologic substrates of Parkinson disease dementia. Ann. Neurol. 72, 587–598 (2012).
Irwin, D. J. et al. Neuropathological and genetic correlates of survival and dementia onset in synucleinopathies: a retrospective analysis. Lancet Neurol. 16, 55–65 (2017).
Guerreiro, R. et al. Investigating the genetic architecture of dementia with Lewy bodies: a two-stage genome-wide association study. Lancet Neurol. 17, 64–74 (2018).
Blanche, P., Dartigues, J. F. & Jacqmin-Gadda, H. Estimating and comparing time-dependent areas under receiver operating characteristic curves for censored event times with competing risks. Stat. Med. 32, 5381–5397 (2013).
Alves, G. et al. Incidence of Parkinson’s disease in Norway: the Norwegian ParkWest study. J. Neurol. Neurosurg. Psychiatry 80, 851–857 (2009).
Parkinson Progression Marker, I. The Parkinson Progression Marker Initiative (PPMI). Prog. Neurobiol. 95, 629–635 (2011).
Verbaan, D. et al. Patient-reported autonomic symptoms in Parkinson disease. Neurology 69, 333–341 (2007).
Beach, T. G. et al. Arizona Study of Aging and Neurodegenerative Disorders and Brain and Body Donation Program. Neuropathology 35, 354–389 (2015).
Lucero, C. et al. Cognitive reserve and β-amyloid pathology in Parkinson disease. Parkinsonism Relat. Disord. 21, 899–904 (2015).
Corvol, J. C. et al. Longitudinal analysis of impulse control disorders in Parkinson disease. Neurology 91, e189–e201 (2018).
Parkinson Study Group. DATATOP: a multicenter controlled clinical trial in early Parkinson’s disease. Arch. Neurol. 46, 1052–1060 (1989).
Williams-Gray, C. H. et al. The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain 132, 2958–2969 (2009).
Hughes, A. J., Daniel, S. E., Ben-Shlomo, Y. & Lees, A. J. The accuracy of diagnosis of parkinsonian syndromes in a specialist movement disorder service. Brain 125, 861–870 (2002).
Goetz, C. G. et al. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov. Disord. 19, 1020–1028 (2004).
Hoops, S. et al. Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology 73, 1738–1745 (2009).
van Steenoven, I. et al. Conversion between mini-mental state examination, montreal cognitive assessment, and dementia rating scale-2 scores in Parkinson’s disease. Mov. Disord. 29, 1809–1815 (2014).
Uc, E. Y. et al. Incidence of and risk factors for cognitive impairment in an early Parkinson disease clinical trial cohort. Neurology 73, 1469–1477 (2009).
Mollenhauer, B. et al. Baseline predictors for progression 4 years after Parkinson’s disease diagnosis in the De Novo Parkinson Cohort (DeNoPa). Mov. Disord. 34, 67–77 (2019).
Kasten, M. et al. Cohort Profile: a population-based cohort to study non-motor symptoms in parkinsonism (EPIPARK). Int. J. Epidemiol. 42, 128–128k (2013).
Bien, S. A. et al. Strategies for enriching variant coverage in candidate disease loci on a multiethnic genotyping array. PLoS ONE 11, e0167758 (2016).
Purcell, S. et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 81, 559–575 (2007).
Anderson, C. A. et al. Data quality control in genetic case-control association studies. Nat. Protoc. 5, 1564–1573 (2010).
1000 Genomes Project Consortium et al. A map of human genome variation from population-scale sequencing. Nature 467, 1061–1073 (2010).
Price, A. L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909 (2006).
Das, S. et al. Next-generation genotype imputation service and methods. Nat. Genet. 48, 1284–1287 (2016).
McCarthy, S. et al. A reference panel of 64,976 haplotypes for genotype imputation. Nat. Genet. 48, 1279–1283 (2016).
Loh, P. R. et al. Reference-based phasing using the Haplotype Reference Consortium panel. Nat. Genet. 48, 1443–1448 (2016).
Desikan, R. S. et al. Genetic assessment of age-associated Alzheimer disease risk: development and validation of a polygenic hazard score. PLoS Med. 14, e1002258 (2017).
Cuellar-Partida, G., Renteria, M. E. & MacGregor, S. LocusTrack: integrated visualization of GWAS results and genomic annotation. Source Code Biol. Med. 10, 1 (2015).
Acknowledgements
We are grateful to O. Nemirovsky for his philanthropic support, encouragement and insights. We thank all study participants, their families and friends for their support and participation, and our study coordinators for making this work possible. We thank A. Brown at Partners HealthCare Personalized Medicine and Y. Kuras at Brigham and Women’s Hospital for technical assistance. The study was funded in part by philanthropic support (to Brigham & Women’s Hospital and C.R.S.) for Illumina MEGA chip genotyping; and in part by NINDS and NIA R01NS115144 (to C.R.S.), which funded genotyping for the PHS validation cohorts EPIPARK and HBS2. The work of C.R.S. was supported by NIH grants NINDS/NIA R01NS115144, U01NS095736, U01NS100603, and the American Parkinson Disease Association Center for Advanced Parkinson Research. T.M.H. is funded by NIH grant K23NS099380. While this manuscript was in revision, G.L. transferred to a new position at Sun Yat-sen University, where he received support from the National Natural Science Foundation of China (project no. 31900475), the Fundamental Research Funds for the Central Universities (project no. 19ykpy146), Young Talent Recruitment Project of Guangdong (project no. 2019QN01Y139) and Shenzhen Basic Research Project (project no. JCYJ20190807161601692). For each individual cohort, acknowledgements are listed in the Supplementary Note.
Author information
Authors and Affiliations
Consortia
Contributions
C.R.S. conceived and designed the study. G.L. contributed to the study design, and carried out the statistical and bioinformatics analyses with J.P., J.J.L. and C.R.S. X.D. contributed to the analysis. Z.L. and S.S.A. performed genotyping. Patient samples and phenotypic data were collected by J.-C.C., F.Z., J.M.-G., M.C.C., A.E., S.L., A.B., G.M., J.H.G., A.Y.H., M.A.S., M.T.H., A.-M.W., T.M.H., B.R., I.S., S.K., P.T., T.G.B., F.C.-D., G.A., O.-B.T., J.S.P., P.H., J.J.v.H., R.A.B., C.H.W.-G., J.M., M.K., C.K., C.T., B.M. and C.R.S. C.R.S. and G.L. drafted the manuscript. All authors reviewed, edited and approved the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
Brigham and Women’s Hospital holds a US provisional patent application on the PHS for predicting PD progression, on which C.R.S. is named as inventor. Outside this work, C.R.S. has served as consultant, scientific collaborator or on scientific advisory boards for Sanofi, Berg Health, Pfizer and Biogen, and has received grants from the NIH, US Department of Defense, American Parkinson Disease Association, and the Michael J Fox Foundation (MJFF). G.L., J.J.L., J.M., A.E., J.H.G., A.Y.H., S.K., P.T., S.S.A., J.S.P. and M.C.C. report no relevant financial or other conflicts of interest in relation to this study. M.A.S. has no conflict of interest related to this work. Outside this work, M.A.S. has received grants from NINDS, DoD, MJFF, Farmer Family Foundation, and has served as a consultant to commercial programs for Eli Lilly & Co (data monitoring committee), Prevail Therapeutics (scientific advisory board), Denali Therapeutics (scientific advisory board), nQ Medical (scientific advisory board), Chase Therapeutics (scientific advisory board) and Partner Therapeutics (scientific advisory board). A.-M.W. has received research funding from the ALS Association, the Parkinson’s Foundation, has participated in clinical trials funded by Acorda, Biogen, Bristol-Myers Squibb, Sanofi/Genzyme, Pfizer and Abbvie, and received consultant payments from Mitsubishi Tanabe and from Accordant. T.M.H. has no conflict of interest related to this work. Outside this work, he has received honoraria for consulting in advisory boards for Boston Scientific and Medtronic. J.-C.C. has no conflict of interest related to this work. Outside this work, J.C.C. has received honoraria for consulting in advisory boards for Abbvie, Actelion, Air Liquide, Biogen, BMS, BrainEver, Clevexel, Denali, Pfizer, Theranexus and Zambon. B.R. is an employee of and holds equity in Praxis Precision Medicines and is advisor for Caraway Therapeutics and Brain Neurotherapy Bio. I.S. is Principal Investigator of a MJFF Computational Science Grant (2017–19). S.K. is supported by Multiple Sclerosis of Western-Australia (MSWA) and the Perron Institute. P.H. is a Scientific Advisor of Neuron23. J.J.v.H. has no conflict of interest related to this work. Outside this work, J.J.v.H. has received grants from the Alkemade-Keuls Foundation, Stichting Parkinson Fonds, Parkinson Vereniging, the Netherlands Organisation for Health Research and Development, the Netherlands Organisation for Scientific Research, Hersenstichting, AbbVie, MJFF, and research support from Hoffmann-La-Roche, Lundbeck and the Centre of Human Drug Research. B.M. has no conflict related to this work. Outside this work, B.M. has received honoraria for consultancy from Roche, Biogen, AbbVie, Servier and Amprion. B.M. is member of the executive steering committee of the Parkinson Progression Marker Initiative and Principal Investigator of the Systemic Synuclein Sampling Study of the MJFF for Parkinson’s Research and has received research funding from the Deutsche Forschungsgemeinschaft (DFG), EU (Horizon2020), Parkinson Fonds Deutschland, Deutsche Parkinson Vereinigung, Parkinson’s Foundation and MJFF. R.A.B. has no conflict of interest related to this work. Outside this work, R.A.B. has received consultancy monies from LCT, FCDI, Novo Nordisk, Cellino, Sana, UC, has received royalties from Wiley and Springer Nature, grant funding from CPT, NIHR Cambridge Biomedical Research Centre (146281), the UK Medical Research Council (MRC), Wellcome Trust (203151/Z/16/Z) and Rosetrees Trust (A1519 M654). C.H.W.-G. has no conflict of interest related to this work. C.H.W.-G. is supported by a RCUK UKRI Research Innovation Fellowship awarded by the MRC (MR/R007446/1) and the NIHR Cambridge Biomedical Research Centre, and receives grant support from MJFF, the Evelyn Trust, the Cure Parkinson’s Trust, Parkinson’s UK, the Rosetrees Trust and the Cambridge Centre for Parkinson-Plus. C.H.W.-G. has received honoraria from Lundbeck and consultancy payments from Modus Outcomes and Evidera. C.T. is supported by EU Grant Horizon 2020/propag-ageing and the MJFF. C.K. serves as a medical advisor to Centogene for genetic testing reports in the fields of movement disorders and dementia, excluding Parkinson’s disease.
Additional information
Peer review information Nature Genetics thanks Robert Graham and the other, anonymous, reviewer for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Genotyping pipeline for discovery and replication cohorts.
Quality control (QC) steps outlined in blue were performed using PLINK v1.90beta75. Note that 509 samples with WGS from the PPMI cohort (after removing three with gender mismatches) were added in Step 10.
Extended Data Fig. 2 Characteristics of loci associated with cognitive progression in PD.
a, RIMS2 locus. b, TMEM108 locus. c, WWOX locus. Top, chromosomal position; middle, -log10(P values) for individual SNPs at each locus (left y-axis) with the rate of recombination indicated by the red line (right y-axis); bottom, gene positions with the locus. Each point represents a SNP colored according to LD with the lead associated variant. Figure panels were generated with LocusTrack83 and r2 values were calculated based on CEU population in the 1000 Genomes Project data set77.
Extended Data Fig. 3 Associations between a second RIMS2 variant rs116918991, TMEM108 rs138073281, and WWOX rs8050111 with cognitive PD progression.
a,c,e, Covariate-adjusted survival curves for PD patients without the indicated variant (blue line) and for those carrying the indicated variant (heterozygotes and homozygotes; red dashed line) are shown. P values Cox PH models with two-sided Wald test. b,d,f, Adjusted mean MMSE scores across time predicted from the estimated fixed-effect parameters of the LMM analysis are shown for cases carrying the variant (heterozygotes and homozygotes; red) and cases without the variant (non-carriers; blue) adjusting for covariates. Shaded ribbons indicate ± s.e.m. around predicted MMSE scores across time. Note that a second RIMS2 variant rs116918991 (correlated with r2 = 0.49 with the lead variant rs182987047; Fig. 1) is shown in a and b, and that the HR and P values shown here for TMEM108 rs138073281 and WWOX rs8050111 are different from the HR and P values from the main analysis (Table 1), where variant alleles were coded as 0, 1, 2. P values from LMM analysis with two-sided t-test.
Extended Data Fig. 4 RIMS2, TMEM108, and WWOX are expressed in human brain.
Gene expression profiles were downloaded directly from the GTEx Portal V746. Expression values are shown in Transcript per Million (TPM), calculated from a gene model with isoforms collapsed to a single gene. Box plots visualize first, third quartiles and medians; the ends of the whiskers represent the lowest (or highest) value still within 1.5-times the interquartile range. Outliers are displayed as dots, if they are above or below 1.5-times the interquartile range. n indicates number of individuals for each tissue analyzed in GTEx V7.
Extended Data Fig. 5 Cell-type specific expression of RIMS2, TMEM108, and WWOX in human brain.
Cell type-specific transcriptomes were assayed using laser-capture RNA sequencing (lcRNAseq) as we reported47. Gene expression (FPKM) profiles of RIMS2, TMEM108, and WWOX are from BRAINcode consortium (http://www.humanbraincode.org). n indicates the number of individuals assayed for each cell type. SNDA, indicates dopamine neurons laser-captured from human substantial nigra pars compacta; MCPY, pyramidal neurons from human motor cortex; TCPY, pyramidal neurons from human temporal cortex; PBMC, human peripheral blood mononuclear white cells; FB, primary human fibroblasts. Box plots visualize first, third quartiles, and medians; the ends of the whiskers represent the lowest (or highest) value still within 1.5-times the interquartile range. Each dot represents a sample.
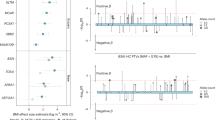
Extended Data Fig. 6 The polygenic hazard score (PHS) is associated with decline in serial MMSE scores.
a, PD cases scoring in the highest quartile (red) of a polygenic risk score (PRS based on 90 susceptibility variants45) compared to PD cases scoring in the lowest quartile of the PRS (blue) are shown. b, PD cases scoring in the highest quartile (red) of the PHS (comprising GBA + APOE ε4 + the 3 novel progression variants) compared to PD cases scoring zero on the PHS (blue) are shown. For a and b, adjusted mean MMSE scores across time predicted from the estimated fixed-effect parameters in the LMM analysis for the combined data set comprising discovery and replication populations are shown. The shaded ribbons indicate ± s.e.m. around predicted MMSE scores across time. The P values from LMM analysis with two-sided t-tests.
Supplementary information
Supplementary Information
Supplementary Note, Figs. 1–5 and Tables 1–5
Supplementary Data 1
PD GWAS-derived lead variants were not statistically significantly associated with motor progression in PD in the combined population.
Rights and permissions
About this article
Cite this article
Liu, G., Peng, J., Liao, Z. et al. Genome-wide survival study identifies a novel synaptic locus and polygenic score for cognitive progression in Parkinson’s disease. Nat Genet 53, 787–793 (2021). https://doi.org/10.1038/s41588-021-00847-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41588-021-00847-6
This article is cited by
-
Disease progression strikingly differs in research and real-world Parkinson’s populations
npj Parkinson's Disease (2024)
-
Proxy-analysis of the genetics of cognitive decline in Parkinson’s disease through polygenic scores
npj Parkinson's Disease (2024)
-
Clinical Application of Polygenic Risk Score in IgA Nephropathy
Phenomics (2024)
-
Early GCase activity is a predictor of long-term cognitive decline in Parkinson’s disease
Translational Neurodegeneration (2023)
-
Circular RNAs in the human brain are tailored to neuron identity and neuropsychiatric disease
Nature Communications (2023)