As pharmaceutical companies seek patent protection for combinations of cancer therapeutics, it is worthwhile to assess what constitutes an ‘unexpected result’ for the purpose of an appropriate patent and whether randomized, controlled trials of drug combinations have the ability to generate them.
The patent system is designed so that inventors who bear the burden of innovation risks and are successful in their efforts have the potential to reap substantial rewards. From a constitutional perspective, however, the ultimate goal is not the benefit of individual inventors but the benefit to society as a whole1. The government provides particular citizens the right to exclude others from certain products or activities for a limited time, in the hope that doing so will lead to benefits for everyone2.
Pharmaceutical companies have become adept at legal and business strategies aimed at extending the period of protection, frequently through minor modifications to a drug’s dosage, formulation or delivery system3,4,5. Commonly known as ‘evergreening’, these strategies allow innovators to increase the period of time during which their successful drug can generate revenue against limited competition, while imposing financial and patient care costs on society3,4. Here, we review the legal concepts of obviousness and unexpected results — terms with which both physicians and regulators (for example, the US Food and Drug Administration (FDA)) should be familiar in light of the emergence of pharmaceutical combination patents — and examine their interaction with current clinical research. In the highly profitable oncology sector, we evaluated whether pharma companies are employing a new variant of these strategies by combining ‘backbone’ drugs (widely accepted standards of care) with other drugs likely to be used to treat a given disease state3,4. Specifically, we focused our efforts on a subset of combination therapies developed in cancer as a case study. Using publicly available information, we assess the current patent and clinical trial landscapes for this combination. We demonstrate that this new front in evergreening not only lacks the inventive nature typically justifying the 20-year patent reward but also leads to the design and development of clinical trials that lack even the potential to yield unexpected results characteristic of a patentable invention — a finding similar to the strategic behaviors of drug- and device-makers in generating and studying drug–device combinations6. Given the implications of these emerging strategic behaviors, we close by offering a proposal for clinical trial elements that are necessary to provide a thoughtful evaluation of the non-obviousness of combination therapy patents, as well as suggesting ways in which inter-agency collaboration at the federal level could help both industry and researchers focus on achieving optimal innovation in the public interest.
A brief review of patentability
Five canonical elements are required of an innovation for it to be patentable under US law: the invention must be of proper subject matter, useful, novel, non-obvious and the application must include proper disclosure7. Of particular relevance to combination therapy patents, the inventor must demonstrate that the invention would not have been obvious to a person having ordinary skill in the art (POSITA), which is defined as a person who has the capability to understand the scientific and engineering principles applicable to the relevant art8,9. Precise requirements vary according to the case and the invention, but in most patent cases involving drug development, the POSITA has skills commensurate with an advanced degree (for example, PhD or MD) along with experience in the research or treatment of the specific disease state(s)10. As the US Supreme Court has noted, a POSITA is expected to be a person of ordinary creativity, one who is able to fit the teachings of multiple patents together like pieces of a puzzle8. Some recent courts have found that a POSITA would also be supported by the insights of a multi-disciplinary drug discovery and development team10. If an invention would be obvious to this creative POSITA who is backed by a team, then the court should reject the patent.
Importantly, the term ‘invention’ goes beyond the notion of tinkering. A related concept, ‘obvious to try’, holds that an invention is unpatentable when it is comprised of a set of re-combined elements, the various permutations of which would be predictable to try8. Absolute predictability is not required, nor does it matter whether the trials of the re-combined elements require extensive time, money and effort to test11. Rather, the invention is unpatentable if there is a finite number of identified solutions — that is, a set of things to try — and a POSITA would have a reasonable expectation of success if he or she were to try each of these solutions in turn8,11. Multiple courts have explicitly stated that it is normal for scientists to optimize each of the variables in a known process to improve on what is generally known already — but that acts of optimization are not themselves patentable11,12.
A claimant can potentially overcome obviousness rejections by demonstrating what are known as objective indicia of an invention’s non-obviousness. These may include achievement of commercial success, fulfillment of a long felt but unsolved need, prior unsuccessful attempts by other POSITAs to solve the problem, evidence that the field’s conventional wisdom ‘teaches away’ from the inventor’s solution, or unexpected results that a POSITA would not anticipate8. Among the objective indicia, generation of unexpected results is the most common avenue for successfully demonstrating non-obviousness, particularly for pharmaceutical inventions13,14. As courts explain, the principle behind the doctrine of unexpected results is straightforward: an invention that exhibits a superior characteristic or advantage in a way that surprises even a skilled artisan immersed in the field is clearly not obvious15. Courts have determined that for a result to be unexpected, it must differ from the POSITA’s expected results in kind rather than degree16. In the context of a combination of two drugs that are each effective when given sequentially, the patent claimant must demonstrate that the properties of the combination are specifically the result of having combined the drugs, rather than reflecting properties of one or both of the drugs, given alone or sequentially. Consider, for example, two modestly effective drugs that each improves survival by two months when given in sequence. Prolongation of survival by, say, not two months but two years and an observed decrease in side effects by administering the two drugs as a combination would be an unexpected result.
Combination therapy in medicine
The prior art
Combining two active therapies into a single regimen is a common practice in medicine: angiotensin-converting enzyme inhibitors and diuretics in hypertension, long-acting beta agonists and inhaled corticosteroids in chronic obstructive pulmonary disease, and combinations of antiretrovirals and protease inhibitors in HIV are but three widely prescribed examples. Oncology is particularly fertile ground, as chemotherapy combinations have been used to treat cancer for well over a half-century, leading to the cures of select malignancies in the 1960s and 1970s17,18,19,20,21. Consequently, combining two or more drugs has become a standard approach in the treatment of the vast majority of cancers22. Testing whether patients who receive the combination of therapies A and B (A + B) have improved outcomes, relative to those who receive either A or B alone, became a standard approach in oncology drug development23
With decades of accumulated experience, key principles of oncology clinical trial design have been derived and are distilled in Box 1. These precepts are understood not only by the sophisticated multi-disciplinary drug discovery and development teams of the modern age but, at the very least, are intuited by clinical practitioners. Combining active anticancer drugs in the search for more efficacious regimens has been employed for decades. Consequently, the resulting patent claims may be entirely unpatentable, as the combination approach has long existed in the prior art and was obvious to try. In light of these obviousness concerns, the question becomes whether a clinical trial — in any subspecialty of medicine — might produce results so surprising that they would meet the threshold of ‘unexpected’.
Discovering the unexpected
From the clinical trial precepts in Box 1 flow features necessary of a clinical trial of an oncology combination therapy (A + B) to demonstrate an unexpected result. First, clinical trial participants ought to be randomly assigned to either the intervention or the comparator arm(s) — they must be randomized controlled trials (RCTs). Randomization helps ensure that the observed outcome of the clinical trial is due to differences in the treatments rather than biased treatment arm assignment. Without randomization, differences in outcomes can be driven by baseline patient characteristics, rather than differences in the treatments.
Second, the most appropriate comparator arm(s) is a sequence (or sequences) of the two drugs that make up the combination (for example, A → B and/or B → A). If A + B confers 12 months of survival while A → B confers 6 months of survival, then combining A and B is clearly advantageous. Alternatively, if the comparator arm is, say, A followed by something else, then claims about the benefit act of combining cannot be made. Clinical trials that allow crossover from comparator to intervention arm at progression are unable to make strong conclusions about overall survival (OS — the amount of time between randomization and the patient’s death) without assuming that subsequent treatments are similar in their effects on outcomes24. Only utilization of pre-determined sequences of therapy allow for meaningful comparison, albeit with limitation of freedom of choice at first progression.
Finally, the primary outcome measure of the RCT ought to be OS. This is contrasted with progression-free survival (PFS), a surrogate outcome that measures the time between randomization and the patient’s disease getting worse (progressing) that has controversially been relied on for recent regulatory decisions25,26. As demonstrated in Box 1, due to the nature of combining individually active therapies, none of the possible patentable PFS results would be unexpected: given the individual activity in the disease state of both A and B, the POSITA would expect A + B to have equal or greater PFS benefit to A → B or B → A, and if A + B has lower PFS benefit, then the point is moot.
Armed with a basic understanding of patentability, oncology’s prior art, and principles of clinical trials that ought to be present to enable identification of truly unexpected results, we can now turn our attention to real-world applications. Let us examine an emerging combination therapy in oncology as a case example.
Evergreening combinations
The results of analyses in numerous clinical trials suggesting the exceptional benefit of combining vascular endothelial growth factor (VEGF) inhibitors with immune checkpoint blockade (also referred to as immunotherapy (IO)) were presented at the European Society of Molecular Oncology 2020 Annual Meeting27,28,29,30. VEGF and IO have individually demonstrated efficacy in a variety of cancers, including advanced and metastatic renal cell carcinoma (mRCC)31,32. VEGF inhibitors reduce a tumor’s growth by blocking its ability to recruit and build a blood supply, while IO acts by inhibiting the signals that a cancer uses to evade the body’s immune system33. VEGF inhibitors may also increase intratumoral T-cell infiltration, an immunologic change that likely enhances IO’s anticancer efficacy34.
Given the decades-long approach in oncology of combining drugs with different mechanisms of action, it would be obvious for a POSITA to consider combining these two therapies. In fact, VEGF–IO combinations have been hypothesized since 2006 (ref. 34), trialed in a variety of cancers33, and have since become, arguably, standard of care for the first-line treatment of advanced or mRCC35. All of this occurred before the 2020 trial result announcements.
The VEGF–IO patent landscape
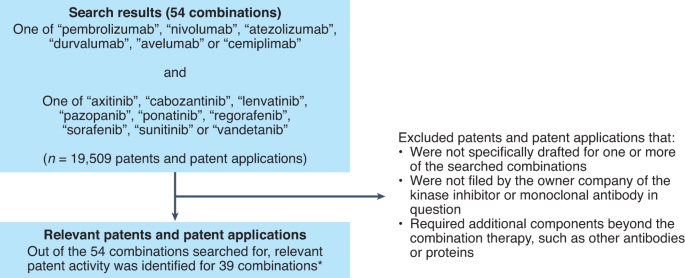
Given the ongoing clinical investigation surrounding VEGF–IO, it would be consistent with the self-interested behavior of a corporation to seek out patent protection for this combination. We therefore set out to determine whether substantial patent activity — evidence beyond anecdote — is occurring for combinations of drugs ordinarily known by relevant oncology practitioners. Given oncology’s prior knowledge, these combinations are likely to constitute obvious (or obvious to try) formulations8. We searched TotalPatent One (LexisNexis) during July and August 2020 for 54 combinations of drugs, containing one each of FDA-approved VEGF or multi-tyrosine kinase inhibitors — axitinib, cabozantinib, lenvatinib, pazopanib, ponatinib, regorafenib, sorafenib, sunitinib, and vandetanib — and FDA-approved programmed cell death protein 1 (PD-1)-axis-inhibiting IO monoclonal antibodies — pembrolizumab, nivolumab, atezolizumab, durvalumab, avelumab and cemiplimab.
Our database search yielded 19,509 patents and patent applications (Fig. 1). Among these, we considered only patents filed by the owner company of the VEGF drug or IO monoclonal antibody in question, given that such patents are the most likely to suggest that a company is attempting to evergreen the protections on an existing drug therapy3. To verify that at least some of the claims within the patents were specifically drafted to the drug combination in question, and to eliminate any patents that specified additional components beyond the combination therapy, such as other antibodies or proteins, we examined in detail those patents determined to be the most relevant for a given drug combination. Selection of the most relevant patent is best illustrated with an example: if two similar patent applications were identified for the same drug combination, one mentioning the drug combination in the specifications and the other mentioning it in both the specifications and the claims, we evaluated the latter. Once an example of patent activity meeting these criteria for one of the 54 drug combinations was identified, we proceeded to the subsequent drug combination.
TotalPatentOne (LexisNexis), a repository of patents and patent applications, was searched for patents and patent applications covering the combinations of VEGF-inhibiting small molecules and IO drugs listed. *Note: for each of the 15 combinations where initial analysis did not yield any patents or patent applications meeting our criteria for inclusion, it remains possible that, within the thousands of claims in these patents or others, there exist ones that could be asserted for the purpose of evergreening the combination therapy.
In this manner, we identified patent activity pertaining to 39 of the 54 drug combinations searched, presented in Supplementary Table 1. The results demonstrate that, across a variety of specific formulations, those companies likely to have incentive to engage in evergreening behavior have been, and continue to be, engaged in substantial patent activity for drug combinations known to those in the field. Given the discussion above and the potential implications of evergreening, this area of patenting and drug development merited critical evaluation.
Teaching away
A patent claimant can overcome obviousness concerns by demonstrating objective indicia of non-obviousness, such as when the prior art teaches away from an invention. That is, was there evidence in the prior art telling inventors not to combine VEGF and IO? Early phase 1 clinical trial work conducted between 2012 and 2014 and publicly disclosed in 2014 evaluated two VEGF–IO combinations in mRCC. In these clinical trials, sunitinib–nivolumab and pazopanib–nivolumab demonstrated approximately 70% and 60%, respectively, grade 3/4 adverse event rates36,37. A subsequent phase 1/2 study of pazopanib–pembrolizumab in mRCC conducted between 2013 and 2017 and publicly disclosed in 2017 demonstrated grade 3/4 adverse events of >80% and at the time concluded that certain VEGF–IO combinations were unsuitable for RCTs38,39. At first glance, these studies — having raised the possibility of a VEGF–IO combination conferring prohibitive toxicity — may have taught away from VEGF–IO combination therapy. To the POSITA with experience in drug discovery and development, though, the observed toxicities were ‘off-target’ effects of the particular VEGF drugs tested that would not be expected to generalize to all VEGF inhibitors, as demonstrated by the first-in-class axitinib–pembrolizumab combination40.
VEGF–IO clinical trials
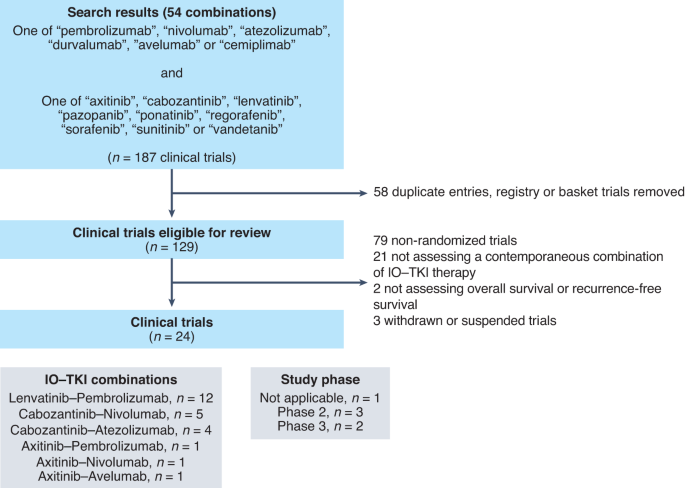
As the most commonly used objective indicium for overcoming obviousness concerns is demonstration of an unexpected result, we asked whether the RCTs in the VEGF–IO development space have the capacity to demonstrate an unexpected result, if one were to exist. To examine this landscape, we searched the National Clinical Trials Registry (ClinicalTrials.gov) on 20 August 2020 for each of the 54 combinations of one of the above VEGF inhibitors and one of the above IO drugs. Building on two of the key clinical trial principles described above — (1) randomization; and (2) evaluation of OS as a primary or co-primary endpoint — we excluded any clinical trials that were not randomized; did not contemporaneously administer one of the above combinations; assessed a primary endpoint(s) other than OS, PFS or recurrence-free survival; or indexed in ClinicalTrials.gov as having a status other than ‘active, not recruiting’ or ‘completed’ (Fig. 2).
Starting with search results of 187 clinical trials, 129 distinct clinical trials were identified. Out of these, 105 trials were excluded from further analysis for non-randomized design, failure to utilize contemporaneous combination or withdrawal/suspension of the study. The remaining 24 RCTs were included in the final analysis. TKI, tyrosine kinase inhibitor; IO, immunotherapy.
We identified 24 eligible RCTs, summarized in Supplementary Table 2, with total anticipated enrollment of 14,614 patient volunteers. Twelve (50%) trials evaluate lenvatinib–pembrolizumab and cabozantinib–nivolumab and cabozantinib–atezolizumab are each evaluated by four (17%). Twenty-one (88%) are phase 3 trials, and the remaining three (13%) are randomized phase 2 trials. Nineteen (79%) are industry-funded trials and five (21%) are government-funded. These trials used five dominant designs:
Type 1: A + B versus A;
Type 2: A + B versus B;
Type 3: A + B versus C;
Type 4: A + B versus D;
Type 5: A + B versus E;
in which A is one of the VEGF inhibitors listed above, B is one of the IO agents listed above, C is an established and related VEGF inhibitor (for example, sunitinib), D is an established but unrelated standard of care (for example, chemotherapy, physician’s choice) and E is a non-active comparator (placebo or otherwise).
Importantly, none of the 24 eligible RCTs possess the three criteria needed to demonstrate an unexpected result that were derived above: randomization, sequential treatment with A and B as a comparator, and OS as the primary or co-primary endpoint. The absence of sequential treatments is clear. Thirteen of the 24 eligible RCTs employ comparator arms that include at least one drug from the VEGF–IO combination. None incorporate A → B or B → A as a comparator, and there is no pre-specified OS or PFS analysis of A + B compared to A → B or B → A subpopulations. Consequently, these RCTs cannot demonstrate an unexpected result attributable to the act of combining6. Nine of the 13 trials that include either A or B as a component of the comparator arm employ OS as the primary or co-primary endpoint (Supplementary Table 2). Representative RCTs are discussed in Box 2.
Importantly, five (21%) type-3 trials were identified. Four of these trials were conducted in mRCC and compared VEGF–IO combinations to sunitinib; all have reported results. First, axitinib–avelumab, in the JAVELIN Renal-101 study reported on 21 March 2019, failed to demonstrate benefit of the combination41. Second, axitinib–pembrolizumab, in the KEYNOTE-426 study also reported on 21 March 2019, demonstrated an OS benefit35. The remaining two RCTs, evaluating cabozantinib–nivolumab and lenvatinib–pembrolizumab, continued to randomize patients to sunitinib control arms after the announcement of KEYNOTE-426 results42,43. Nearly 24 months after KEYNOTE-426 publication, in March 2021, the CheckMate 9ER trial of cabozantinib–nivolumab was published, demonstrating modest PFS and OS benefits44; FDA approval had occurred 6 weeks earlier45. One month later, in April 2021, the CLEAR trial evaluating lenvatinib–pembrolizumab in mRCC failed to demonstrate any more than a modest benefit in OS46, yet FDA approval followed 4 months later47. Complicating interpretation of the mRCC VEGF–IO trials still further, nearly all enrolled a substantial number of patients from countries where access to IO only occurs through clinical trials, increasing the likelihood that patients randomized to the sunitinib arms of these studies would never receive standard-of-care, second-line IO in the event of disease progression, and thereby overestimating the OS benefit of VEGF–IO48.
Recommendations
Reviewing the available evidence, the RCTs of VEGF–IO combinations appear designed to achieve FDA approval, rather than identify truly unexpected or scientifically novel results that would overcome obviousness concerns. While such approvals will yield significant financial rewards for the drug sponsor(s), they should not result in extension of exclusivity in the absence of a demonstration of non-obviousness through the discovery of unexpected results.
In truth, encouraging combination patents and RCTs that do not aim to identify unexpected results carries societal costs. First, the limited resources that can be dedicated to research and development efforts are directed away from the truly innovative approaches that represent the constitutional goal of the patent system and toward the commercialization of combinations that are, in the context of oncology’s prior art, non-innovative. Second, even if VEGF–IO patents were to be invalidated in court, the time and expense required to challenge them often deters competitors from entering the market, interfering with the natural competitive forces expected to discipline high prices4. In short, this new frontier in evergreening raises serious societal concerns and requires coordinated action from all involved parties — from the end users who have demand for these products and the government-supported entities that enable patent-seeking research rather than true innovation, through to the executive branch entities responsible for conferring patents.
Physicians, as end users of combination therapies, bear a societal responsibility to be thoughtful producers and consumers of biomedical research — industry-sponsored or not. As with any therapy, physicians should reflect on the designs of the relevant combination therapy clinical trials. In the context of cancer, oncologists need to disabuse themselves of the notion that ‘more therapy is better and in the best interests of the patient’. Learning health systems would be wise to assess the real-world outcomes of patients treated with combination therapies, especially as the gap between performance as observed in clinical trials versus real life yawns. Finally, disclosure of the shortcomings of clinical trial design is an absolutely necessary component in the desired goal of clinical care — shared clinical decision-making.
Clinical trialists and institutions have critical roles in the current pharmaceutical research and development landscape; it is this infrastructure that enables both innovative and non-innovative research. Realizing that the potential benefits of a clinical trial redound to patients other than the ones for which they care, clinical trialists must ask themselves, “Is the trial on which I am proposing to enroll patients something new or is it an incremental step?” It is unlikely physicians can do this alone, but demanding more from the research that we and others design and enact is a good first step, along with thoughtful skepticism toward certain types of patent claims. Similarly, the academic research infrastructure, as well as the cachet, on which many non-innovative clinical trials rest is supported in no small part by federal grants. Within the context of oncology, the National Cancer Institute designated 53 Comprehensive Cancer Centers in the United States, with federal grant support (P30) exceeding US$265 million in fiscal year 2020 (ref. 49). Incorporating review of the relative amounts of industry- versus non-industry-sponsored research activity occurring at a given cancer center in the NCI P30 grant renewal process may help to promote truly innovative research. The concept of taxpayers ‘paying twice’ for drug development — once through government-funded research and again in the form of high drug prices — has gained traction during the COVID-19 pandemic and should be seriously considered.
As the guardian of the patent and drug-making processes, coordinated federal action on the part of the US Patent and Trademark Office (USPTO) and FDA is important. As the prior arts of medicine’s subspecialties become increasingly complex, the case for inter-agency collaboration between the USPTO and FDA becomes stronger. The FDA has the capacity to provide information about all registered clinical trials, fully informing the prior art and context that the USPTO requires to make its determinations. The FDA also has a supply of experts who can provide additional perspective for USPTO examiners, who are rarely (if ever) clinicians (for example, physicians, pharmacists) or pharmaceutical scientists — FDA experts would be, to a first approximation, the government’s best proxy for a well-informed POSITA. In addition, the USPTO is optimally positioned to communicate to researchers and industry the requirements for patentability and to issue guidance on what constitutes unexpected results (positive or negative) in clinical trials.
The challenge in designing interagency cooperation is to ensure that the process is meaningful, rather than pro forma or simply burdensome. Fortunately, the USPTO has a model in place to better inform prior art determinations. In 2019, USPTO director Andrei Iancu reported to the Senate Judiciary Subcommittee on Intellectual Property that the USPTO was piloting projects to help examiners better identify prior art by collaboration between multiple USTPO examiners, as well as examiners from foreign patent offices50. This project could be expanded to include expertise closer to home — specifically at the FDA. Such guidance for the USPTO is in the interests of both drug developers (by providing a measure of certainty) and the public (by enhancing the risk–benefit calculus of biomedical research). Similarly, any regulatory standards that emerge at the USPTO could be incorporated by the FDA into its oversight of clinical trials and more fully inform its safety and efficacy determinations. This would allow both agencies to better carry out their mandates in serving the public interest.
References
Woodbridge v. U.S. 263 50 (Supreme Court, 1923).
Feldman, R. Colum. Sci. Tech. L. Rev. 17, 30–89 (2016).
Feldman, R. J. Law Biosci. 5, 590–647 (2018).
Gaudry, K. S. Nat. Biotechnol. 29, 876–878 (2011).
Gowda, V., Beall, R. F., Kesselheim, A. S. & Sarpatwari, A. Nat. Biotechnol. 39, 414–417 (2021).
Beall, R. F. & Kesselheim, A. S. Nat. Biotechnol. 36, 142–145 (2018).
Conditions for Patentability; Non-Obvious Subject Matter 35 USC§103 (US Congress, 2011).
KSR Int’l Co. v. Teleflex Inc. 550 US 398 (Justia, 2007).
Manual of Patent Examining Procedure (MPEP) Sec. 2141.03 (USPTO, 2020).
Novartis Pharms. Corp. v. Accord Healthcare, Inc. (Lexis, 2020).
Pfizer v. Apotex. 480 1348 F.3d (Federal Circuit, 2007).
In re: Peterson. 315 1325 F.3d (Federal Circuit, 2003).
Thomas, N. A. NYU L. Rev. 86, 2070–2112 (2011).
Pitlick, H. A. J. Pat. Trademark Off. Soc. 86, 169–182 (2004).
In re: Soni. 54 746 F. 3d (Federal Circuit, 1995).
Galderma Labs., LP. v. Tolmar, Incl. 737 731 F.3d (Federal Circuit, 2013).
DeVita, V. T. Jr. Br. J. Haematol. 122, 718–727 (2003).
Frei, E. III et al. Blood 13, 1126–1148 (1958).
Frei, E. III Cancer 18, 1580–1584 (1965).
Einhorn, E. H. Clin. Cancer Res. 3, 2630–2632 (1997).
Bagley, C. M. Jr, Young, R. C., Canellos, G. P. & DeVita, V. T. N. Engl. J. Med. 287, 856–862 (1972).
National Comprehensive Cancer Network. https://www.nccn.org/guidelines/category_1 (2020).
Gyawali, B. & Prasad, V. Nat. Rev. Clin. Oncol. 14, 521–522 (2017).
Prasad, V. & Grady, C. Contemp. Clin. Trials 37, 167–169 (2014).
Kim, C. & Prasad, V. JAMA Intern. Med. 175, 1992–1994 (2015).
Kovic, B. et al. JAMA Intern. Med. 178, 1586–1596 (2018).
Choueri, T. K. et al. Ann. Oncol. https://oncologypro.esmo.org/meeting-resources/esmo-virtual-congress-2020/nivolumab-cabozantinib-vs-sunitinib-in-first-line-treatment-for-advanced-renal-cell-carcinoma-first-results-from-the-randomized-phase-iii-checkmate-9er-trial (2020).
Arance Fernandez, A. M. et al. Ann. Oncol. https://oncologypro.esmo.org/meeting-resources/esmo-virtual-congress-2020/lenvatinib-len-plus-pembrolizumab-pembro-for-advanced-melanoma-mel-that-progressed-on-a-pd-1-or-pd-l1-inhibitor-initial-results-of-leap-004 (2020).
Lwin, Z. et al. Ann. Oncol. https://oncologypro.esmo.org/meeting-resources/esmo-virtual-congress-2020/leap-005-phase-ii-study-of-lenvatinib-len-plus-pembrolizumab-pembro-in-patients-pts-with-previously-treated-advanced-solid-tumours (2020).
Pal, S. Ann. Oncol. https://oncologypro.esmo.org/meeting-resources/esmo-virtual-congress-2020/cabozantinib-c-in-combination-with-atezolizumab-a-as-first-line-therapy-for-advanced-clear-cell-renal-cell-carcinoma-ccrcc-results-from-the (2020).
Motzer, R. J. et al. J. Clin. Oncol. 27, 3584–3590 (2009).
Sternberg, C. N. et al. J. Clin. Oncol. 28, 1061–1068 (2010).
Ciciola, P., Cascetta, P., Bianco, C., Formisano, L. & Bianco, R. J. Clin. Med. 9, 675 (2020).
Dirkx, A. E. et al. FASEB J. 20, 621–630 (2006).
Rini, B. I. et al. N. Engl. J. Med. 380, 1116–1127 (2019).
Amin, A. et al. Am. Soc. Clin. Oncol. https://doi.org/10.1200/jco.2014.32.15_suppl.5010 (2014).
Amin, A. et al. J. Immunother. Cancer 6, 109 (2019).
Chowdhury, S. et al. Am. Soc. Clin. Oncol. https://doi.org/10.1200/JCO.2017.35.15_suppl.4506 (2017).
Chowdhury, S. et al. Clin. Genitourin. Cancer 19, 434–446 (2021).
Atkins, M. B. et al. Lancet Oncol. 19, 405–415 (2018).
Motzer, R. J. et al. N. Engl. J. Med. 380, 1103–1115 (2019).
ClinicalTrials.gov (National Library of Medicine, accessed 1 November 2021); https://clinicaltrials.gov/ct2/history/NCT03141177?A=38&B=39&C=Side-by-Side#StudyPageTop
ClinicalTrials.gov (National Library of Medicine, accessed 1 November 2021); https://clinicaltrials.gov/ct2/history/NCT02811861?A=20&B=21&C=Side-by-Side#StudyPageTop
Choueiri, T. K. et al. N. Engl. J. Med. 384, 829–841 (2021).
US Food and Drug Administration. FDA approves nivolumab plus cabozantinib for advanced renal cell carcinoma. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-nivolumab-plus-cabozantinib-advanced-renal-cell-carcinoma (2021).
Motzer, R. et al. N. Engl. J. Med. 384, 1289–1300 (2021).
US Food and Drug Administration. FDA approves lenvatinib plus pembrolizumab for advanced renal cell carcinoma. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-lenvatinib-plus-pembrolizumab-advanced-renal-cell-carcinoma (2021).
Strohbehn, G. W. & Goldstein, D. A. Nat. Rev. Clin. Oncol. 18, 395–396 (2021).
National Cancer Institute. Vol. 2021 (2021) 2019 NCI Budget Fact Book: Cancer Centers. https://www.cancer.gov/about-nci/budget/fact-book/extramural-programs/cancer-centers (2019).
US Patent and Trademark Office. Statement by Director Iancu before the United States Senate Subcommittee on Intellectual Property, Committee on the Judiciary. https://www.uspto.gov/about-us/news-updates/statement-director-iancu-united-states-senate-subcommittee-intellectual (2019).
A study of pembrolizumab with or without lenvatinib as first line (1L) intervention in a programmed cell death-ligand 1 (PD-L1) selected population with recurrent or metastatic head and neck squamous cell carcinoma (LEAP-010). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT04199104
Efficacy and safety of pembrolizumab with lenvatinib vs. docetaxel in participants with metastatic non-small cell lung cancer (NSCLC) and progressive disease after platinum doublet chemotherapy and immunotherapy (LEAP-008). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03976375
Efficacy and safety study of pembrolizumab with or without lenvatinib in adults with programmed cell death-ligand 1 (PD-L1)-positive treatment-naive non-small cell lung cancer (LEAP-007). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03829332
Safety and efficacy of lenvatinib in combination with pembrolizumab versus lenvatinib as first-line therapy in participants with advanced hepatocellular carcinoma (LEAP-002). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03713593
Safety and efficacy study of pembrolizumab combined with lenvatinib as first-line intervention in adults with advance melanoma (LEAP-003). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03820986
Safety and efficacy study of pemetrexed + platinum chemotherapy + pembrolizumab with or without lenvatinib as first-line intervention in adults with metastatic nonsquamous non-small cell lung cancer (LEAP-006). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03829319
Study of first-line pembrolizumab with lenvatinib in urothelial carcinoma cisplatin-ineligible participants whose tumors express programmed cell death-ligand 1 and in participants ineligible for platinum-containing chemotherapy (LEAP-011). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03898180
Lenvatinib/everolimus or lenvatinib/pembrolizumab versus sunitinib alone as treatment of advanced renal cell carcinoma (CLEAR). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT02811861
Pembrolizumab and lenvatinib in participants with hepatocellular carcinoma (HCC) before liver transplant (PLENTY202001). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT04425226
Lenvatinib in combination with pembrolizumab versus treatment of physician’s choice in participants with advanced endometrial cancer (KEYNOTE-775). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03517449
Pembrolizumab plus lenvatinib versus chemotherapy for endometrial carcinoma (LEAP-001). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03884101
Safety and efficacy of lenvatinib with pembrolizumab in combination with transarterial chemoembolization in participants with incurable/non-metastatic hepatocellular carcinoma (LEAP-012). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT04246177
FDA. FDA approves avelumab plus axitinib for renal cell carcinoma. (15 May 2019); https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-avelumab-plus-axitinib-renal-cell-carcinoma
Garon, E. B. et al. Lancet 384, 665–673 (2014).
Peer, C. J. et al. Br. J. Clin. Pharmacol. 86, 1769–1777 (2020).
A study to compare treatments for a type of kidney cancer called TFE/translocation renal cell carcinoma (tRCC). National Clinical Trials Registry (accessed 1 November 2021); https://clinicaltrials.gov/ct2/show/NCT03595124
Acknowledgements
The authors wish to thank L. Yang for assistance with patent research, as well as N. Brown and M. Dorji for assistance with legal research. G.W.S. is an employee of the US Federal Government; the views expressed in this manuscript do not reflect the views of the US Federal Government and are his personal views.
Author information
Authors and Affiliations
Contributions
All authors meet International Committee of Medical Journal Editors criteria for authorship in the presented work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Supplementary Information
Supplementary Tables 1 and 2
Rights and permissions
About this article
Cite this article
Strohbehn, G.W., Kacew, A.J., Goldstein, D.A. et al. Combination therapy patents: a new front in evergreening. Nat Biotechnol 39, 1504–1510 (2021). https://doi.org/10.1038/s41587-021-01137-6
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41587-021-01137-6
This article is cited by
-
‘Contribution of component’ and the perioperative immune-checkpoint inhibitor precedent
Nature Reviews Clinical Oncology (2024)
-
Improving combination drug trials using ‘definitive screening designs’
Nature Biotechnology (2022)