Abstract
The clinical translation of cationic α-helical antimicrobial peptides (AMPs) has been hindered by structural instability, proteolytic degradation and in vivo toxicity from nonspecific membrane lysis. Although analyses of hydrophobic content and charge distribution have informed the design of synthetic AMPs with increased potency and reduced in vitro hemolysis, nonspecific membrane toxicity in vivo continues to impede AMP drug development. Here, we analyzed a 58-member library of stapled AMPs (StAMPs) based on magainin II and applied the insights from structure–function–toxicity measurements to devise an algorithm for the design of stable, protease-resistant, potent and nontoxic StAMP prototypes. We show that a lead double-stapled StAMP named Mag(i+4)1,15(A9K,B21A,N22K,S23K) can kill multidrug-resistant Gram-negative pathogens, such as colistin-resistant Acinetobacter baumannii in a mouse peritonitis–sepsis model, without observed hemolysis or renal injury in murine toxicity studies. Inputting the amino acid sequences alone, we further generated membrane-selective StAMPs of pleurocidin, CAP18 and esculentin, highlighting the generalizability of our design platform.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
The datasets generated for the current study are included in the published article and supplementary information. Requests for any additional information can be made to the corresponding author.
Code availability
The LI and HNM user interface, and the associated source code, can be accessed at www.walenskylab.org/HNM/ and is subject to a user agreement (Supplementary Note). The content and design of the LI and HNM user interface are protected by US and international copyright laws. The LI and HNM user interface or any portion thereof may not be reproduced, distributed, altered or used in any manner, beyond the user’s personal, academic and noncommercial use under the user agreement, without prior written consent from the Dana-Farber Cancer Institute. ‘Dana-Farber Cancer Institute’ is a service mark of Dana-Farber Cancer Institute, Inc., 450 Brookline Avenue, Boston, MA 02215. Inquiries regarding further information on a permitted use or a license to use any content should be addressed to the Office of General Counsel, BP 376, Dana-Farber Cancer Institute, 450 Brookline Avenue, Boston, MA 02215, USA.
References
Brogden, K. A. Antimicrobial peptides: pore formers or metabolic inhibitors in bacteria? Nat. Rev. Microbiol. 3, 238–250 (2005).
Brown, K. L. & Hancock, R. E. Cationic host defense (antimicrobial) peptides. Curr. Opin. Immunol. 18, 24–30 (2006).
Hancock, R. E. & Sahl, H. G. Antimicrobial and host-defense peptides as new anti-infective therapeutic strategies. Nat. Biotechnol. 24, 1551–1557 (2006).
Fjell, C. D., Hiss, J. A., Hancock, R. E. & Schneider, G. Designing antimicrobial peptides: form follows function. Nat. Rev. Drug Discov. 11, 37–51 (2012).
Theuretzbacher, U. Global antimicrobial resistance in Gram-negative pathogens and clinical need. Curr. Opin. Microbiol. 39, 106–112 (2017).
Woodford, N. & Wareham, D. W. Tackling antibiotic resistance: a dose of common antisense? J. Antimicrob. Chemother. 63, 225–229 (2009).
Blair, J. M., Webber, M. A., Baylay, A. J., Ogbolu, D. O. & Piddock, L. J. Molecular mechanisms of antibiotic resistance. Nat. Rev. Microbiol. 13, 42–51 (2015).
Steiner, H., Hultmark, D., Engstrom, A., Bennich, H. & Boman, H. G. Sequence and specificity of two antibacterial proteins involved in insect immunity. Nature 292, 246–248 (1981).
Zasloff, M. Magainins, a class of antimicrobial peptides from Xenopus skin: isolation, characterization of two active forms, and partial cDNA sequence of a precursor. Proc. Natl Acad. Sci. USA 84, 5449–5453 (1987).
Wade, D. et al. All-D amino acid-containing channel-forming antibiotic peptides. Proc. Natl Acad. Sci. USA 87, 4761–4765 (1990).
Braunstein, A., Papo, N. & Shai, Y. In vitro activity and potency of an intravenously injected antimicrobial peptide and its DL amino acid analog in mice infected with bacteria. Antimicrob. Agents Chemother. 48, 3127–3129 (2004).
Chen, Y. et al. Role of peptide hydrophobicity in the mechanism of action of alpha-helical antimicrobial peptides. Antimicrob. Agents Chemother. 51, 1398–1406 (2007).
Jiang, Z., Vasil, A. I., Gera, L., Vasil, M. L. & Hodges, R. S. Rational design of alpha-helical antimicrobial peptides to target Gram-negative pathogens, Acinetobacter baumannii and Pseudomonas aeruginosa: utilization of charge, ‘specificity determinants,’ total hydrophobicity, hydrophobe type and location as design parameters to improve the therapeutic ratio. Chem. Biol. Drug Des. 77, 225–240 (2011).
Mant, C. T. et al. De novo designed amphipathic alpha-helical antimicrobial peptides incorporating dab and dap residues on the polar face to treat the gram-negative pathogen, acinetobacter baumannii. J. Med. Chem. 62, 3354–3366 (2019).
Gordon, Y. J., Romanowski, E. G. & McDermott, A. M. A review of antimicrobial peptides and their therapeutic potential as anti-infective drugs. Curr. Eye Res. 30, 505–515 (2005).
Bird, G. H. et al. Hydrocarbon double-stapling remedies the proteolytic instability of a lengthy peptide therapeutic. Proc. Natl Acad. Sci. USA 107, 14093–14098 (2010).
Schafmeister, C. E., Po, J. & Verdine, G. L. An all-hydrocarbon cross-linking system for enhancing the helicity and metabolic stability of peptides. JACS 122, 5891–5892 (2000).
Walensky, L. D. et al. Activation of apoptosis in vivo by a hydrocarbon-stapled BH3 helix. Science 305, 1466–1470 (2004).
Bird, G. H. et al. Biophysical determinants for cellular uptake of hydrocarbon-stapled peptide helices. Nat. Chem. Biol. 12, 845–852 (2016).
Walensky, L. D. & Bird, G. H. Hydrocarbon-stapled peptides: Principles, practice, and progress. J. Med. Chem. 57, 6275–6288 (2014).
Bird, G. H. et al. Mucosal delivery of a double-stapled RSV peptide prevents nasopulmonary infection. J. Clin. Invest. 124, 2113–2124 (2014).
Meric-Bernstam, F. et al. Phase I trial of a novel stapled peptide ALRN-6924 disrupting MDMX- and MDM2-mediated inhibition of WT p53 in patients with solid tumors and lymphomas. J. Clin. Oncol. 35, 2505 (2017).
Chapuis, H. et al. Effect of hydrocarbon stapling on the properties of alpha-helical antimicrobial peptides isolated from the venom of hymenoptera. Amino Acids 43, 2047–2058 (2012).
Dinh, T. T., Kim, D. H., Luong, H. X., Lee, B. J. & Kim, Y. W. Antimicrobial activity of doubly-stapled alanine/lysine-based peptides. Bioorg. Med. Chem. Lett. 25, 4016–4019 (2015).
Migon, D., Neubauer, D. & Kamysz, W. Hydrocarbon stapled antimicrobial peptides. Protein J. 37, 2–12 (2018).
Pham, T. K., Kim, D. H., Lee, B. J. & Kim, Y. W. Truncated and constrained helical analogs of antimicrobial esculentin-2EM. Bioorg. Med. Chem. Lett. 23, 6717–6720 (2013).
Stone, T. A., Cole, G. B., Nguyen, H. Q., Sharpe, S. & Deber, C. M. Influence of hydrocarbon stapling on membrane interactions of synthetic antimicrobial peptides. Bioorg. Med. Chem. 26, 1189–1196 (2017).
Stone, T. A., Cole, G. B., Nguyen, H. Q., Sharpe, S. & Deber, C. M. Influence of hydrocarbon-stapling on membrane interactions of synthetic antimicrobial peptides. Bioorg. Med. Chem. 26, 1189–1196 (2017).
Bechinger, B., Zasloff, M. & Opella, S. J. Structure and interactions of magainin antibiotic peptides in lipid bilayers: a solid-state nuclear magnetic resonance investigation. Biophys. J. 62, 12–14 (1992).
Zasloff, M., Martin, B. & Chen, H. C. Antimicrobial activity of synthetic magainin peptides and several analogues. Proc. Natl Acad. Sci. USA 85, 910–913 (1988).
Gesell, J., Zasloff, M. & Opella, S. J. Two-dimensional 1H NMR experiments show that the 23-residue magainin antibiotic peptide is an alpha-helix in dodecylphosphocholine micelles, sodium dodecylsulfate micelles, and trifluoroethanol/water solution. J. Biomol. NMR 9, 127–135 (1997).
Reisser, S., Strandberg, E., Steinbrecher, T. & Ulrich, A. S. 3D Hydrophobic moment vectors as a tool to characterize the surface polarity of amphiphilic peptides. Biophys. J. 106, 2385–2394 (2014).
Matsuzaki, K. et al. Mechanism of synergism between antimicrobial peptides magainin 2 and PGLa. Biochemistry 37, 15144–15153 (1998).
Williams, R. W. et al. Raman spectroscopy of synthetic antimicrobial frog peptides magainin 2a and PGLa. Biochemistry 29, 4490–4496 (1990).
Engen, J. R. Analysis of protein conformation and dynamics by hydrogen/deuterium exchange MS. Anal. Chem. 81, 7870–7875 (2009).
Shi, X. E. et al. Hydrogen exchange-mass spectrometry measures stapled peptide conformational dynamics and predicts pharmacokinetic properties. Anal. Chem. 85, 11185–11188 (2013).
Mechler, A. et al. Specific and selective peptide-membrane interactions revealed using quartz crystal microbalance. Biophys. J. 93, 3907–3916 (2007).
Joshi, T., Voo, Z. X., Graham, B., Spiccia, L. & Martin, L. L. Real-time examination of aminoglycoside activity towards bacterial mimetic membranes using quartz crystal microbalance with dissipation monitoring (QCM-D). Biochim. Biophys. Acta 1848, 385–391 (2015).
Wang, K. F., Nagarajan, R. & Camesano, T. A. Differentiating antimicrobial peptides interacting with lipid bilayer: Molecular signatures derived from quartz crystal microbalance with dissipation monitoring. Biophys. Chem. 196, 53–67 (2015).
Murray, B., Pearson, C. S., Aranjo, A., Cherupalla, D. & Belfort, G. Mechanism of four de novo designed antimicrobial peptides. J. Biol. Chem. 291, 25706–25715 (2016).
Molugu, T. R. & Brown, M. F. Cholesterol effects on the physical properties of lipid membranes viewed by solid-state NMR spectroscopy. Adv. Exp. Med. Biol. 1115, 99–133 (2019).
Liu, Y. Y. et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect. Dis. 16, 161–168 (2016).
Moffatt, J. H. et al. Colistin resistance in Acinetobacter baumannii is mediated by complete loss of lipopolysaccharide production. Antimicrob. Agents Chemother. 54, 4971–4977 (2010).
Fox, J. L. Antimicrobial peptides stage a comeback. Nat. Biotechnol. 31, 379–382 (2013).
Zavascki, A. P. & Nation, R. L. Nephrotoxicity of polymyxins: Is there any difference between colistimethate and polymyxin B?. Antimicrob Agents Chemother 61, e02319–16 (2017).
Roberts, K. D. et al. Antimicrobial activity and toxicity of the major lipopeptide components of polymyxin B and colistin: last-line antibiotics against multidrug-resistant Gram-negative bacteria. ASC Infect. Dis. 1, 568–575 (2015).
Gallardo-Godoy, A. et al. Activity and predicted nephrotoxicity of synthetic antibiotics based on polymyxin B. J. Med. Chem. 59, 1068–1077 (2016).
Ge, Y. et al. In vitro antibacterial properties of pexiganan, an analog of magainin. Antimicrob. Agents Chemother. 43, 782–788 (1999).
Zuluaga, A. F. et al. Neutropenia induced in outbred mice by a simplified low-dose cyclophosphamide regimen: characterization and applicability to diverse experimental models of infectious diseases. BMC Infect. Dis. 6, 55 (2006).
World Health Organization. Antibacterial agents in clinical development. (WHO, 2017).
Lee, J. H., Jeong, S. H., Cha, S. S. & Lee, S. H. A lack of drugs for antibiotic-resistant Gram-negative bacteria. Nat. Rev. Drug Discov. 6, 938–939 (2007).
Zgurskaya, H. I., Lopez, C. A. & Gnanakaran, S. Permeability barrier of gram-negative cell envelopes and approaches to bypass it. ACS Infect. Dis. 1, 512–522 (2015).
Boman, H. G. Antibacterial peptides: basic facts and emerging concepts. J. Intern. Med. 254, 197–215 (2003).
Marr, A. K., Gooderham, W. J. & Hancock, R. E. Antibacterial peptides for therapeutic use: obstacles and realistic outlook. Curr. Opin. Pharmacol. 6, 468–472 (2006).
Gomes, A., Teixeira, C., Ferraz, R., Prudencio, C. & Gomes, P. Wound-healing peptides for treatment of chronic diabetic foot ulcers and other infected skin injuries. Molecules 22, E1743 (2017).
Bird, G. H., Crannell, W. C. & Walensky, L. D. Chemical synthesis of hydrocarbon-stapled peptides for protein interaction research and therapeutic targeting. Curr. Protoc. Chem. Biol. 3, 99–117 (2011).
Juretic, D., Vukicevic, D., Ilic, N., Antcheva, N. & Tossi, A. Computational design of highly selective antimicrobial peptides. J. Chem. Inf. Model. 49, 2873–2882 (2009).
Kovacs, J. M., Mant, C. T. & Hodges, R. S. Determination of intrinsic hydrophilicity/hydrophobicity of amino acid side chains in peptides in the absence of nearest-neighbor or conformational effects. Biopolymers 84, 283–297 (2006).
Guttman, M., Weis, D. D., Engen, J. R. & Lee, K. K. Analysis of overlapped and noisy hydrogen/deuterium exchange mass spectra. J. Am. Soc. Mass Spectrom. 24, 1906–1912 (2013).
Acknowledgements
We thank D. Hung and R. Bhattacharyya for providing clinical strains of MDR bacteria, K. Kean and P. Barendse for coding assistance, K. Hanford and M. Godes for technical support, A. Watts for helpful discussions, M. Cameron for plasma stability analyses, S. Breegi, C. Sypher and the Dana-Farber Cancer Institute Animal Resource Facility for technical assistance with in vivo studies, D. Neuberg for biostatistical support and R. Bronson for histopathology services and expert slide review. We are also grateful to the Centers for Disease Control and Prevention Antimicrobial Resistance Isolate Bank that provided access to panels of MDR bacteria. This research was supported by a National Institutes of Health grant no. R35CA197583 and a Leukemia and Lymphoma Society Scholar Award to L.D.W. Additional support to L.D.W. was generously provided by the LaTorre Family, the Wolpoff Family Foundation and the Todd J. Schwartz Memorial Fund. The Charles River toxicity study was supported in part by an option agreement between the Dana-Farber Cancer Institute and Aileron Therapeutics. This research was also supported by a National Institutes of Health grant no. R01GM101135 to J.R.E. and a research collaboration between J.R.E. and the Waters Corporation. R.M.’s doctoral research was supported in part by a Doctoral Foreign Study Award (no. DFS-134963) from the Canadian Institutes of Health Research and an IDEA-squared award from the Harvard-MIT Division of Health Sciences and Technology.
Author information
Authors and Affiliations
Contributions
R.M. and L.D.W. conceived of and designed the study. R.M. synthesized and characterized StAMPs, performed the biochemical and cellular experiments and collaborated with H.D.H. on developing the hydrophobicity network map analysis and performing the in vivo studies. D.Y. conducted the QCM experiments. J.A.M. performed the HX–MS analyses under the supervision of T.E.W. and J.R.E. The paper was written by L.D.W., R.M. and H.D.H., and reviewed by all co-authors.
Corresponding author
Ethics declarations
Competing interests
L.D.W. is a scientific advisory board member and consultant for Aileron Therapeutics.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Integrated supplementary information
Supplementary Figure 1 Antimicrobial and hemolytic activities of an i, i+7-stapled Mag2 library.
The antimicrobial activity (MIC in μg/mL) and percent RBC hemolysis at 25 μg/mL were determined for a library of i, i+7 stapled peptides based on the Mag2 sequence. The MIC is the geometric mean of four independent experiments. Percent hemolysis data are the mean of three independent experiments (shown as dots). X, S5 stapling amino acid; 8, R8 stapling amino acid; B, norleucine (substituted for methionine to maximize the efficiency of ruthenium-catalyzed olefin metathesis).
Supplementary Figure 2 Relationships between StAMP biophysical parameters and hemolysis.
a-e, No direct correlations were observed between percent RBC hemolysis and the total hydrophobicity (a), percent α-helicity (b), HPLC retention time (c), pI (d), or 3D hydrophobic moment magnitude (e) of StAMPs (n=19), as calculated by Pearson correlation.
Supplementary Figure 3
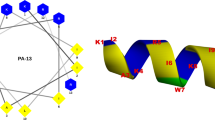
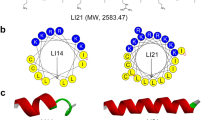
A computational algorithm yields HNMs and lyticity indices for StAMPs.
Supplementary Figure 4
HNMs and lyticity indices of a staple-scanning Mag(i+4) library
Supplementary Figure 5
HNMs and lyticity indices of a lysine-scanning Mag(i+4)15 library
Supplementary Figure 6 Membrane selectivity and insertion mechanism of Mag(i+4)15(A9K).
a, Incubation of Mag(i+4)1,15(A9K) with anionic liposomes that mimic E. coli membranes (POPC:POPG) reduces deuterium exchange, whereas exposure to zwitterionic liposomes that mimic the mammalian membrane condition (POPC:Cholesterol) has no such effect and is identical to the peptide’s deuterium exchange profile in aqueous solution alone. HX-MS experiments were performed independently three times with similar results. b-e, QCM sensorgrams demonstrate uniformity of changes in resonant frequency across harmonics for SLBs mimicking bacterial membranes (POPC:POPG) upon exposure to 6 (b) and 24 (c) μg/mL of Mag(i+4)1,15(A9K), consistent with transmembrane insertion. In contrast, little to no interaction is reflected in the QCM profiles of POPC mammalian-type membranes at low or high peptide dosing (d-e). For each condition, an exemplary sensorgram is shown for experiments performed independently two times with similar results. f, Accordingly, there were no changes in resonant frequency across the third (blue), seventh (red), and eleventh (black) harmonics in response to Mag(i+4)1,15(A9K) treatment (8 μg/mL) of SLBs composed of POPC and increasing concentrations of cholesterol. Data are mean of two independent experiments (shown as dots).
Supplementary Figure 7 Body weights of mice treated intravenously with Mag(i+4)1,15(A9K).
Mice were treated with Mag(i+4)15(A9K) at an intravenous dose of 5 mg/kg twice daily for 8 days. Body weights were measured before (day 1) and after 8 days of treatment (day 9). Data are mean ± s.d. for n=4 mice per sex.
Supplementary Figure 8 Histology of murine tissues after IV treatment with Mag(i+4)1,15(A9K).
Peripheral blood smears (a-d) and H&E stained sections of liver (e-h) and kidney (h-k) from n=8 mice (4 male, 4 female) treated with Mag(i+4)15(A9K) (5 mg/kg IV BID x 8 d). Each vertical pair (a-b, c-d, e-f, g-h, h-i, j-k) represents a low and higher power view (enlargement of boxed image) of the indicated tissue. For each tissue, specimens from two different mice are shown. RBC morphology and liver histology are normal. Whereas some of the treated mice showed predominantly normal kidney histology (h-k), others manifested regions of mild-to-moderate tubular degeneration, as shown in Fig. 4j and Supplementary Fig. 12b.
Supplementary Figure 9 RBC response to Mag(i+4)15(A9K,B21A,N22K,S23K) treatment.
Mag(i+4)15(A9K,B21A,N22K,S23K) shows little to no RBC hemolytic activity across a broad dose-effective range, and even when dosed as high as 800 μg/mL for 90 minutes or 18 hours. The data from two independently performed experiments are shown as dots, with several pairs of replicate data points overlapping. The Gram-negative bactericidal dosing range is highlighted in yellow in the inset.
Supplementary Figure 10 Comparative activity of linear and stapled Mag2 peptides in a peritonitis-sepsis mouse model.
a, Kaplan Meier survival curves of neutropenic mice (n=8 per arm) infected with A. baumannii (ATCC 19606) intraperitoneally and treated with either vehicle (saline) or two 5 mg/kg IP doses of Mag(i+4)15(A9K,B21A,N22K,S23K). p=0.0006 for StAMP vs. vehicle by log rank test (two-sided). b, Kaplan Meier survival curves of neutropenic mice (n=8 per arm) infected with A. baumanii (AR-0303) intraperitoneally and treated with either vehicle (saline) or two 5 mg/kg IP doses of Mag2 or Mag(i+4)15(A9K,B21A,N22K,S23K). p=0.0001 for StAMP vs. Vehicle; p=0.02 for StAMP vs. Mag2; and p=0.1432 (n.s.) for Mag2 vs. Vehicle, as calculated by log rank test (two-sided).
Supplementary Figure 11 Body weights of StAMP-treated mice.
Mice were treated with vehicle or Mag(i+4)15(A9K,B21A,N22K,S23K) at an intravenous dose of 5 mg/kg twice daily for 5 days. Body weights were measured before (day 1) and after 5 days of treatment (day 6). Data are mean ± s.d. for n=8 female mice per arm.
Supplementary Figure 12 Histology of murine kidney after intravenous treatment with StAMPs.
a-b, Mice (n=8 per arm) were treated with vehicle, Mag(i+4)15(A9K,B21A,N22K,S23K), or Mag(i+4)15(A9K) at an intravenous dose of 5 mg/kg twice daily for 5 days. H&E stained sections of kidney tissue from mice treated with Mag(i+4)15(A9K,B21A,N22K,S23K) showed normal histology (a), whereas select mice treated with Mag(i+4)15(A9K) manifested mild-to-moderate renal tubule degeneration (b) (affected regions outlined in dashed black lines). For each image pair, the boxed tissue on the left is enlarged in the image to the right.
Supplementary information
Supplementary Information
Supplementary Figs. 1–12, Supplementary Tables 1–3 and Supplementary Note
Rights and permissions
About this article
Cite this article
Mourtada, R., Herce, H.D., Yin, D.J. et al. Design of stapled antimicrobial peptides that are stable, nontoxic and kill antibiotic-resistant bacteria in mice. Nat Biotechnol 37, 1186–1197 (2019). https://doi.org/10.1038/s41587-019-0222-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41587-019-0222-z
This article is cited by
-
Identification of potent antimicrobial peptides via a machine-learning pipeline that mines the entire space of peptide sequences
Nature Biomedical Engineering (2023)
-
Targeting Toll-like receptor-driven systemic inflammation by engineering an innate structural fold into drugs
Nature Communications (2023)
-
Structural dynamics influences the antibacterial activity of a cell-penetrating peptide (KFF)3K
Scientific Reports (2023)
-
Impact of chemical modifications on the antimicrobial and hemolytic activity of helical amphipathic peptide Lasioglossin LL-III
Amino Acids (2023)
-
Inorganic hollow mesoporous spheres-based delivery for antimicrobial agents
Frontiers of Materials Science (2023)