Abstract
Whether the human fetus and the prenatal intrauterine environment (amniotic fluid and placenta) are stably colonized by microbial communities in a healthy pregnancy remains a subject of debate. Here we evaluate recent studies that characterized microbial populations in human fetuses from the perspectives of reproductive biology, microbial ecology, bioinformatics, immunology, clinical microbiology and gnotobiology, and assess possible mechanisms by which the fetus might interact with microorganisms. Our analysis indicates that the detected microbial signals are likely the result of contamination during the clinical procedures to obtain fetal samples or during DNA extraction and DNA sequencing. Furthermore, the existence of live and replicating microbial populations in healthy fetal tissues is not compatible with fundamental concepts of immunology, clinical microbiology and the derivation of germ-free mammals. These conclusions are important to our understanding of human immune development and illustrate common pitfalls in the microbial analyses of many other low-biomass environments. The pursuit of a fetal microbiome serves as a cautionary example of the challenges of sequence-based microbiome studies when biomass is low or absent, and emphasizes the need for a trans-disciplinary approach that goes beyond contamination controls by also incorporating biological, ecological and mechanistic concepts.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Macpherson, A. J., de Aguero, M. G. & Ganal-Vonarburg, S. C. How nutrition and the maternal microbiota shape the neonatal immune system. Nat. Rev. Immunol. 17, 508–517 (2017).
Kalbermatter, C., Fernandez Trigo, N., Christensen, S. & Ganal-Vonarburg, S. C. Maternal microbiota, early life colonization and breast milk drive immune development in the newborn. Front. Immunol. 12, 683022 (2021).
Gensollen, T., Iyer, S. S., Kasper, D. L. & Blumberg, R. S. How colonization by microbiota in early life shapes the immune system. Science 352, 539–544 (2016).
Jain, N. The early life education of the immune system: moms, microbes and (missed) opportunities. Gut Microbes 12, 1824564 (2020).
Hornef, M. W. & Torow, N. ‘Layered immunity’ and the ‘neonatal window of opportunity’ — timed succession of non-redundant phases to establish mucosal host–microbial homeostasis after birth. Immunology 159, 15–25 (2020).
Torow, N., Marsland, B. J., Hornef, M. W. & Gollwitzer, E. S. Neonatal mucosal immunology. Mucosal Immunol. 10, 5–17 (2017).
Schreurs, R. et al. Human fetal TNF-α-cytokine-producing CD4+ effector memory T cells promote intestinal development and mediate inflammation early in life. Immunity 50, 462–476 (2019).
Stras, S. F. et al. Maturation of the human intestinal immune system occurs early in fetal development. Dev. Cell 51, 357–373 (2019).
Zhang, X. et al. CD4 T cells with effector memory phenotype and function develop in the sterile environment of the fetus. Sci. Transl. Med. 6, 238ra272 (2014).
Tissier, H. Recherches sur la flore intestinale des nourrissons: (état normal et pathologique). Doctoral dissertation, BIU Santé (1900).
He, Q. et al. The meconium microbiota shares more features with the amniotic fluid microbiota than the maternal fecal and vaginal microbiota. Gut Microbes 12, 1794266 (2020).
Stinson, L. et al. Comparison of bacterial DNA profiles in mid-trimester amniotic fluid samples from preterm and term deliveries. Front. Microbiol. 11, 415 (2020).
Younge, N. et al. Fetal exposure to the maternal microbiota in humans and mice. JCI Insight 4, e127806 (2019).
Stinson, L. F., Boyce, M. C., Payne, M. S. & Keelan, J. A. The not-so-sterile womb: evidence that the human fetus is exposed to bacteria prior to birth. Front. Microbiol. 10, 1124 (2019).
Aagaard, K. et al. The placenta harbors a unique microbiome. Sci. Transl. Med. 6, 237ra265 (2014).
D’Argenio, V. The prenatal microbiome: a new player for human health. High Throughput 7, 38 (2018).
Funkhouser, L. J. & Bordenstein, S. R. Mom knows best: the universality of maternal microbial transmission. PLoS Biol. 11, e1001631 (2013).
Stinson, L. F., Payne, M. S. & Keelan, J. A. Planting the seed: origins, composition, and postnatal health significance of the fetal gastrointestinal microbiota. Crit. Rev. Microbiol. 43, 352–369 (2017).
Walker, R. W., Clemente, J. C., Peter, I. & Loos, R. J. F. The prenatal gut microbiome: are we colonized with bacteria in utero? Pediatr. Obes. 12 (Suppl. 1), 3–17 (2017).
Bolte, E. E., Moorshead, D. & Aagaard, K. M. Maternal and early life exposures and their potential to influence development of the microbiome. Genome Med. 14, 4 (2022).
Berg, G. et al. Microbiome definition re-visited: old concepts and new challenges. Microbiome 8, 103 (2020).
Blaser, M. J. et al. Lessons learned from the prenatal microbiome controversy. Microbiome 9, 8 (2021). Discussion about the prenatal microbiome controversy by several experts in the microbiome field.
Bushman, F. D. De-discovery of the placenta microbiome. Am. J. Obstet. Gynecol. 220, 213–214 (2019).
Editorial. Microbiome studies and “blue whales in the Himalayas”. Lancet Infect. Dis. 18, 925 https://doi.org/10.1016/S1473-3099(18)30503-6 (2018).
Hornef, M. & Penders, J. Does a prenatal bacterial microbiota exist? Mucosal Immunol. 10, 598–601 (2017).
Perez-Muñoz, M. E., Arrieta, M. C., Ramer-Tait, A. E. & Walter, J. A critical assessment of the “sterile womb” and “in utero colonization” hypotheses: implications for research on the pioneer infant microbiome. Microbiome 5, 48 (2017).
Segata, N. No bacteria found in healthy placentas. Nature 572, 317–318 (2019).
Walter, J. & Hornef, M. W. A philosophical perspective on the prenatal in utero microbiome debate. Microbiome 9, 5 (2021).
de Goffau, M. C. et al. Human placenta has no microbiome but can contain potential pathogens. Nature 572, 329–334 (2019). Sequencing study using robust controls, concluding that there is no evidence for a placental microbiome.
Kennedy, K. M. et al. Fetal meconium does not have a detectable microbiota before birth. Nat. Microbiol. 6, 865–873 (2021). The only sequencing study so far that characterized the microbial populations in human fetuses using meconium samples obtained after C-section, concluding that there is no evidence for a microbiota.
Kuperman, A. A. et al. Deep microbial analysis of multiple placentas shows no evidence for a placental microbiome. BJOG 127, 159–169 (2020).
Lauder, A. P. et al. Comparison of placenta samples with contamination controls does not provide evidence for a distinct placenta microbiota. Microbiome 4, 29 (2016).
Leiby, J. S. et al. Lack of detection of a human placenta microbiome in samples from preterm and term deliveries. Microbiome 6, 196 (2018).
Theis, K. R. et al. Does the human placenta delivered at term have a microbiota? Results of cultivation, quantitative real-time PCR, 16S rRNA gene sequencing, and metagenomics. Am. J. Obstet. Gynecol. 220, 267.e1–267.e39 (2019).
Sterpu, I. et al. No evidence for a placental microbiome in human pregnancies at term. Am. J. Obstet. Gynecol. 224, 296.e1–296.e23 (2021).
de Goffau, M. C. et al. Recognizing the reagent microbiome. Nat. Microbiol. 3, 851–853 (2018).
Olomu, I. N. et al. Elimination of “kitome” and “splashome” contamination results in lack of detection of a unique placental microbiome. BMC Microbiol. 20, 157 (2020).
Salter, S. J. et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 12, 87 (2014).
Rackaityte, E. et al. Viable bacterial colonization is highly limited in the human intestine in utero. Nat. Med. 26, 599–607 (2020). Microbial characterization of fetal samples obtained after vaginal delivery, reporting highly limited bacterial colonization.
Mishra, A. et al. Microbial exposure during early human development primes fetal immune cells. Cell 184, 3394–3409 (2021). Analysis of fetal tissues obtained after medical termination of pregnancy in the second trimester and vaginal delivery, reporting microbial colonization of the fetus and bacterial priming of fetal immune cells.
Li, Y. et al. In utero human intestine harbors unique metabolomic features including bacterial metabolites. JCI Insight 5, e138751 (2020). Characterization of the microbiota in fetuses obtained by vaginal delivery, reporting no evidence for bacterial colonization.
Lim, E. S., Rodriguez, C. & Holtz, L. R. Amniotic fluid from healthy term pregnancies does not harbor a detectable microbial community. Microbiome 6, 87 (2018).
Liu, Y. et al. Midtrimester amniotic fluid from healthy pregnancies has no microorganisms using multiple methods of microbiologic inquiry. Am. J. Obstet. Gynecol. 223, 248.e1–248.e21 (2020).
Rehbinder, E. M. et al. Is amniotic fluid of women with uncomplicated term pregnancies free of bacteria? Am. J. Obstet. Gynecol. 219, 289.e1–289.e12 (2018).
de Goffau, M. C., Charnock-Jones, D. S., Smith, G. C. S. & Parkhill, J. Batch effects account for the main findings of an in utero human intestinal bacterial colonization study. Microbiome 9, 6 (2021).
Powell, S., Perry, J. & Meikle, D. Microbial contamination of non-disposable instruments in otolaryngology out-patients. J. Laryngol. Otol. 117, 122–125 (2003).
Wistrand, C., Soderquist, B. & Sundqvist, A. S. Time-dependent bacterial air contamination of sterile fields in a controlled operating room environment: an experimental intervention study. J. Hosp. Infect. 110, 97–102 (2021).
Gomez de Aguero, M. et al. The maternal microbiota drives early postnatal innate immune development. Science 351, 1296–1302 (2016). Study demonstrating that aspects of prenatal immune development induced by maternal microbial compounds can occur in the absence of live microorganisms in the fetus.
Vuong, H. E. et al. The maternal microbiome modulates fetal neurodevelopment in mice. Nature 586, 281–286 (2020).
Baker, J. M., Chase, D. M. & Herbst-Kralovetz, M. M. Uterine microbiota: residents, tourists, or invaders? Front. Immunol. 9, 208 (2018).
Cherry, S. H., Filler, M. & Harvey, H. Lysozyme content of amniotic fluid. Am. J. Obstet. Gynecol. 116, 639–642 (1973).
Soto, E. et al. Human β-defensin-2: a natural antimicrobial peptide present in amniotic fluid participates in the host response to microbial invasion of the amniotic cavity. J. Matern. Fetal Neonatal Med. 20, 15–22 (2007).
Reichhardt, M. P. et al. The salivary scavenger and agglutinin in early life: diverse roles in amniotic fluid and in the infant intestine. J. Immunol. 193, 5240–5248 (2014).
Sinha, R. et al. Assessment of variation in microbial community amplicon sequencing by the Microbiome Quality Control (MBQC) project consortium. Nat. Biotechnol. 35, 1077–1086 (2017).
Grettenberger, C. L. Novel Gloeobacterales spp. from diverse environments across the globe. mSphere 6, e0006121 (2021).
Ravel, J. et al. Vaginal microbiome of reproductive-age women. Proc. Natl Acad. Sci. USA 108 (Suppl. 1), 4680–4687 (2011).
Megli, C. J. & Coyne, C. B. Infections at the maternal-fetal interface: an overview of pathogenesis and defence. Nat. Rev. Microbiol. 20, 67–82 (2022).
Armistead, B., Oler, E., Adams Waldorf, K. & Rajagopal, L. The double life of group B Streptococcus: asymptomatic colonizer and potent pathogen. J. Mol. Biol. 431, 2914–2931 (2019).
Dodd, J. M. & Crowther, C. A. Misoprostol for induction of labour to terminate pregnancy in the second or third trimester for women with a fetal anomaly or after intrauterine fetal death. Cochrane Database Syst. Rev. 2010, CD004901 (2010).
Nijman, T. A. et al. Association between infection and fever in terminations of pregnancy using misoprostol: a retrospective cohort study. BMC Pregnancy Childbirth 17, 7 (2017).
Rackaityte, E. et al. Corroborating evidence refutes batch effect as explanation for fetal bacteria. Microbiome 9, 10 (2021).
Duar, R. M. et al. Lifestyles in transition: evolution and natural history of the genus Lactobacillus. FEMS Microbiol. Rev. 41, S27–S48 (2017).
Dominguez-Bello, M. G. et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc. Natl Acad. Sci. USA 107, 11971–11975 (2010).
Dos Santos, S. J. et al. Early neonatal meconium does not have a demonstrable microbiota determined through use of robust negative controls with cpn60-based microbiome profiling. Microbiol. Spectr. 9, e0006721 (2021).
Heida, F. H. et al. Weight shapes the intestinal microbiome in preterm infants: results of a prospective observational study. BMC Microbiol. 21, 219 (2021).
Backhed, F. et al. Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe 17, 690–703 (2015).
Shao, Y. et al. Stunted microbiota and opportunistic pathogen colonization in caesarean-section birth. Nature 574, 117–121 (2019).
Podlesny, D. & Fricke, W. F. Strain inheritance and neonatal gut microbiota development: a meta-analysis. Int. J. Med. Microbiol. 311, 151483 (2021).
Bajorek, S. et al. Initial microbial community of the neonatal stomach immediately after birth. Gut Microbes 10, 289–297 (2019).
Kim, S. M. et al. Gastric fluid versus amniotic fluid analysis for the identification of intra-amniotic infection due to Ureaplasma species. J. Matern. Fetal Neonatal Med. 29, 2579–2587 (2016).
Martin, R. et al. Early-life events, including mode of delivery and type of feeding, siblings and gender, shape the developing gut microbiota. PLoS One 11, e0158498 (2016).
Yassour, M. et al. Natural history of the infant gut microbiome and impact of antibiotic treatment on bacterial strain diversity and stability. Sci. Transl. Med. 8, 343ra381 (2016).
Mitchell, C. M. et al. Delivery mode affects stability of early infant gut microbiota. Cell Rep. Med. 1, 100156 (2020).
Ferretti, P. et al. Mother-to-infant microbial transmission from different body sites shapes the developing infant gut microbiome. Cell Host Microbe 24, 133–145 (2018).
Yassour, M. et al. Strain-level analysis of mother-to-child bacterial transmission during the first few months of life. Cell Host Microbe 24, 146–154 (2018).
Korpela, K. et al. Maternal fecal microbiota transplantation in cesarean-born infants rapidly restores normal gut microbial development: a proof-of-concept study. Cell 183, 324–334 (2020).
Davis, N. M., Proctor, D. M., Holmes, S. P., Relman, D. A. & Callahan, B. J. Simple statistical identification and removal of contaminant sequences in marker-gene and metagenomics data. Microbiome 6, 226 (2018).
Dyrhovden, R. et al. Managing contamination and diverse bacterial loads in 16S rRNA deep sequencing of clinical samples: implications of the law of small numbers. mBio 12, e0059821 (2021).
Laurence, M., Hatzis, C. & Brash, D. E. Common contaminants in next-generation sequencing that hinder discovery of low-abundance microbes. PLoS One 9, e97876 (2014).
Read, S. J. Recovery efficiences on nucleic acid extraction kits as measured by quantitative LightCycler PCR. Mol. Pathol. 54, 86–90 (2001).
Walker, S. P. et al. Non-specific amplification of human DNA is a major challenge for 16S rRNA gene sequence analysis. Sci. Rep. 10, 16356 (2020).
Cebra, J. J., Periwal, S. B., Lee, G., Lee, F. & Shroff, K. E. Development and maintenance of the gut-associated lymphoid tissue (GALT): the roles of enteric bacteria and viruses. Dev. Immunol. 6, 13–18 (1998).
Gaboriau-Routhiau, V. et al. The key role of segmented filamentous bacteria in the coordinated maturation of gut helper T cell responses. Immunity 31, 677–689 (2009).
Wesemann, D. R. et al. Microbial colonization influences early B-lineage development in the gut lamina propria. Nature 501, 112–115 (2013).
Li, H. et al. Mucosal or systemic microbiota exposures shape the B cell repertoire. Nature 584, 274–278 (2020).
Bacher, P. et al. Human anti-fungal Th17 immunity and pathology rely on cross-reactivity against Candida albicans. Cell 176, 1340–1355 (2019).
Kabbert, J. et al. High microbiota reactivity of adult human intestinal IgA requires somatic mutations. J. Exp. Med. 217, e20200275 (2020).
Arpaia, N. et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 504, 451–455 (2013).
McGovern, N. et al. Human fetal dendritic cells promote prenatal T-cell immune suppression through arginase-2. Nature 546, 662–666 (2017).
Rechavi, E. et al. Timely and spatially regulated maturation of B and T cell repertoire during human fetal development. Sci. Transl. Med. 7, 276ra225 (2015).
Casas, R. & Bjorksten, B. Detection of Fel d 1-immunoglobulin G immune complexes in cord blood and sera from allergic and non-allergic mothers. Pediatr. Allergy Immunol. 12, 59–64 (2001).
Szepfalusi, Z. et al. Transplacental priming of the human immune system with environmental allergens can occur early in gestation. J. Allergy Clin. Immunol. 106, 530–536 (2000).
Vuillermin, P. J. et al. Maternal carriage of Prevotella during pregnancy associates with protection against food allergy in the offspring. Nat. Commun. 11, 1452 (2020).
Ganal-Vonarburg, S. C., Hornef, M. W. & Macpherson, A. J. Microbial–host molecular exchange and its functional consequences in early mammalian life. Science 368, 604–607 (2020).
Lockhart, P. B. et al. Bacteremia associated with toothbrushing and dental extraction. Circulation 117, 3118–3125 (2008).
Fisher, R. A., Gollan, B. & Helaine, S. Persistent bacterial infections and persister cells. Nat. Rev. Microbiol. 15, 453–464 (2017).
De Boeck, I. et al. Lactobacilli Have a Niche in the Human Nose. Cell Rep. 31, 107674 (2020).
Lebeer, S., Vanderleyden, J. & De Keersmaecker, S. C. Host interactions of probiotic bacterial surface molecules: comparison with commensals and pathogens. Nat. Rev. Microbiol. 8, 171–184 (2010).
Collins, J. et al. Fibrinogen-binding and platelet-aggregation activities of a Lactobacillus salivarius septicaemia isolate are mediated by a novel fibrinogen-binding protein. Mol. Microbiol. 85, 862–877 (2012).
Kankainen, M. et al. Comparative genomic analysis of Lactobacillus rhamnosus GG reveals pili containing a human-mucus binding protein. Proc. Natl Acad. Sci. USA 106, 17193–17198 (2009).
Rampersaud, R. et al. Inerolysin, a cholesterol-dependent cytolysin produced by Lactobacillus iners. J. Bacteriol. 193, 1034–1041 (2011).
Wuyts, S. et al. Large-scale phylogenomics of the Lactobacillus casei group highlights taxonomic inconsistencies and reveals novel clade-associated features. mSystems 2, e00061-17 (2017).
Weinberg, E. D. The Lactobacillus anomaly: total iron abstinence. Perspect. Biol. Med. 40, 578–583 (1997).
Hazards, E. Po. B. et al. Update of the list of QPS-recommended biological agents intentionally added to food or feed as notified to EFSA 7: suitability of taxonomic units notified to EFSA until September 2017. EFSA J. 16, e05131 (2018).
Cannon, J. P., Lee, T. A., Bolanos, J. T. & Danziger, L. H. Pathogenic relevance of Lactobacillus: a retrospective review of over 200 cases. Eur. J. Clin. Microbiol. Infect. Dis. 24, 31–40 (2005).
Richardson, E. J. et al. Gene exchange drives the ecological success of a multi-host bacterial pathogen. Nat. Ecol. Evol. 2, 1468–1478 (2018).
Gordon, R. J. & Lowy, F. D. Pathogenesis of methicillin-resistant Staphylococcus aureus infection. Clin. Infect. Dis. 46 (Suppl. 5), S350–359 (2008).
Otto, M. Staphylococcus aureus toxins. Curr. Opin. Microbiol. 17, 32–37 (2014).
Powers, M. E. & Bubeck Wardenburg, J. Igniting the fire: Staphylococcus aureus virulence factors in the pathogenesis of sepsis. PLoS Pathog. 10, e1003871 (2014).
Healy, C. M., Baker, C. J., Palazzi, D. L., Campbell, J. R. & Edwards, M. S. Distinguishing true coagulase-negative Staphylococcus infections from contaminants in the neonatal intensive care unit. J. Perinatol. 33, 52–58 (2013).
Michels, R., Last, K., Becker, S. L. & Papan, C. Update on coagulase-negative staphylococci–what the clinician should know. Microorganisms 9, 830 (2021).
Marchant, E. A., Boyce, G. K., Sadarangani, M. & Lavoie, P. M. Neonatal sepsis due to coagulase-negative staphylococci. Clin. Dev. Immunol. 2013, 586076 (2013).
Zhen, X., Lundborg, C. S., Sun, X., Hu, X. & Dong, H. Economic burden of antibiotic resistance in ESKAPE organisms: a systematic review. Antimicrob. Resist. Infect. Control 8, 137 (2019).
Kamal, S. M., Simpson, D. J., Wang, Z., Ganzle, M. & Romling, U. Horizontal transmission of stress resistance genes shape the ecology of beta- and gamma-proteobacteria. Front. Microbiol. 12, 696522 (2021).
Kramer, A., Schwebke, I. & Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 6, 130 (2006).
Neely, A. N. & Maley, M. P. Survival of enterococci and staphylococci on hospital fabrics and plastic. J. Clin. Microbiol. 38, 724–726 (2000).
Bizzarro, M. J. et al. Neonatal sepsis 2004–2013: the rise and fall of coagulase-negative staphylococci. J. Pediatr. 166, 1193–1199 (2015).
Dong, Y., Speer, C. P. & Glaser, K. Beyond sepsis: Staphylococcus epidermidis is an underestimated but significant contributor to neonatal morbidity. Virulence 9, 621–633 (2018).
Glaser, M. A., Hughes, L. M., Jnah, A. & Newberry, D. Neonatal sepsis: a review of pathophysiology and current management strategies. Adv. Neonatal Care 21, 49–60 (2021).
Nan, C. et al. Maternal group B Streptococcus-related stillbirth: a systematic review. BJOG 122, 1437–1445 (2015).
Vazquez-Boland, J. A., Krypotou, E. & Scortti, M. Listeria placental infection. mBio 8, e00949–17 (2017).
DiGiulio, D. B. et al. Microbial invasion of the amniotic cavity in preeclampsia as assessed by cultivation and sequence-based methods. J. Perinat. Med. 38, 503–513 (2010).
DiGiulio, D. B. et al. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: a molecular and culture-based investigation. PLoS One 3, e3056 (2008). Sequencing study of amniotic fluid of 166 women in preterm labour with PCR and culture that showed near-complete positive correlation of bacterial detection with neonatal morbidity and mortality.
DiGiulio, D. B. et al. Prevalence and diversity of microbes in the amniotic fluid, the fetal inflammatory response, and pregnancy outcome in women with preterm pre-labor rupture of membranes. Am. J. Reprod. Immunol. 64, 38–57 (2010).
DiGiulio, D. B. et al. Microbial invasion of the amniotic cavity in pregnancies with small-for-gestational-age fetuses. J. Perinat. Med. 38, 495–502 (2010).
Enders, G., Daiminger, A., Bader, U., Exler, S. & Enders, M. Intrauterine transmission and clinical outcome of 248 pregnancies with primary cytomegalovirus infection in relation to gestational age. J. Clin. Virol. 52, 244–246 (2011).
Luckey, T. D. Germfree Life and Gnotobiology (Academic Press, 1963).
Rasmussen, S. A., Jamieson, D. J., Honein, M. A. & Petersen, L. R. Zika virus and birth defects–reviewing the evidence for causality. N. Engl. J. Med. 374, 1981–1987 (2016).
Falk, P. G., Hooper, L. V., Midtvedt, T. & Gordon, J. I. Creating and maintaining the gastrointestinal ecosystem: what we know and need to know from gnotobiology. Microbiol. Mol. Biol. Rev. 62, 1157–1170 (1998).
Gordon, H. A. & Pesti, L. The gnotobiotic animal as a tool in the study of host microbial relationships. Bacteriol. Rev. 35, 390–429 (1971).
Hooper, L. V. et al. Molecular analysis of commensal host-microbial relationships in the intestine. Science 291, 881–884 (2001).
Wostman, B. S. Germfree and Gnotobiotic Animal Models. Background and Applications (CRC Press, 1996).
Arvidsson, C., Hallen, A. & Backhed, F. Generating and analyzing germ-free mice. Curr. Protoc. Mouse Biol. 2, 307–316 (2012).
Carter, P. B., Norin, E. & Swennes, A. G. Gnotobiotics and the microbiome. In The Laboratory Rat 3rd edn (eds Suckow, M. A. et al.) Ch. 21, 827–848 (2020).
Qv, L. et al. Methods for establishment and maintenance of germ-free rat models. Front. Microbiol. 11, 1148 (2020).
Schoeb, T. R. & Eaton, K. A. Gnotobiotics (Academic Press, 2017).
Jervis-Bardy, J. et al. Deriving accurate microbiota profiles from human samples with low bacterial content through post-sequencing processing of Illumina MiSeq data. Microbiome 3, 19 (2015).
Saffarian, A. et al. Crypt- and mucosa-associated core microbiotas in humans and their alteration in colon cancer patients. mBio 10, e01315-19 (2019).
Jorissen, J. et al. Case–control microbiome study of chronic otitis media with effusion in children points at Streptococcus salivarius as a pathobiont-inhibiting species. mSystems 6, e00056-21 (2021).
Salzberg, S. Does the placenta have a bacterial microbiome? Forbes (1 June 2020); https://www.forbes.com/sites/stevensalzberg/2020/06/01/does-the-placenta-have-a-bacterial-microbiome/?sh=7ae092ea250b.
Jost, T., Lacroix, C., Braegger, C. & Chassard, C. Assessment of bacterial diversity in breast milk using culture-dependent and culture-independent approaches. Br. J. Nutr. 110, 1253–1262 (2013).
Treven, P. et al. Evaluation of human milk microbiota by 16S rRNA gene next-generation sequencing (NGS) and cultivation/MALDI-TOF mass spectrometry identification. Front. Microbiol. 10, 2612 (2019).
Bihl, S. et al. When to suspect contamination rather than colonization—lessons from a putative fetal sheep microbiome. Gut Microbes 14, 2005751 (2022).
Kennedy, K. M. et al. Over-celling fetal microbial exposure. Cell 184, 5839–5841 (2021).
Eisenhofer, R. et al. Contamination in low microbial biomass microbiome studies: issues and recommendations. Trends Microbiol. 27, 105–117 (2019).
Acknowledgements
T.B. receives funding from the Deutsche Forschungsgemeinschaft (German Research Foundation no. BR2925 10-1 & PL241 16-1). F.D.B. is funded by AI045008, AI120489, R33HL137063, CA219871, AI139240, and the PennCHOP Microbiome Program. J.D. acknowledges funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (grant agreement ERC-2017-AdG no. 788191—Homo.symbiosus). W.M.d.V. is supported by the Gravitation grant 024.002.002 of the Netherlands Organization for Scientific Research. W.M.d.V. and A.S. are supported by the Academy of Finland (grants 1308255 and 1325103). A.M.E. is funded in part with Federal funds from the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health, Department of Health and Human Services, under grant number U19AI110818 to the Broad Institute. M.A.E. is funded through grants R01HD102318, R01HD098867 and R01NR014784. S.C.G.-V. was funded through a Peter Hans Hofschneider Professorship provided by the Stiftung Molekulare Biomedizin. M.G.G. and D.M.S are funded by the Canada Research Chairs Program. L.J.H. is supported by Wellcome Trust Investigator Awards 100974/C/13/Z and 220876/Z/20/Z and by the Biotechnology and Biological Sciences Research Council (BBSRC) Institute Strategic Programme Gut Microbes and Health BB/R012490/1 and its constituent projects BBS/E/F/000PR10353 and BBS/E/F/000PR10356. M.W.H. has received funding from the ERC under the European Union’s Horizon 2020 research and innovation programme (grant agreement no. 101019157). S.L. has received funding from the ERC under the European Union’s Horizon 2020 research and innovation programme (grant agreement 852600 Lacto-Be). A.J.M. receives funding from ERCAd HHMM-Neonates and Swiss National Science Sinergia. O.K. is supported by the ERC under the European Union’s Horizon 2020 research and innovation programme (grant agreement ERC-2020-COG no. 101001355). Work in the laboratories of P.W.O., L.O. and J.W. is supported by Science Foundation Ireland (SFI) through a Centre award (APC/SFI/12/RC/2273_P2) to APC Microbiome Ireland. J.W. acknowledges support through an SFI Professorship (19/RP/6853) and thanks V. McMahon for coordination of this review and R. O’Callaghan for encouragement. J.R. acknowledges funding from the Interuniversity Special Research Fund (iBOF) Flanders (FLEXIGUT R-11423), the Rega Institute, VIB and KU Leuven. N.S. receives funding from the ERC (ERC-STG project MetaPG-716575 and ERC-CoG microTOUCH-101045015) and from the European H2020 program (ONCOBIOME-825410 project, MASTER-818368 project and IHMCSA-964590). F.S. is supported in part by Science Foundation Ireland. G.C.S.S. acknowledges funding from the Medical Research Council (UK; MR/K021133/1) and the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre (Women’s Health theme). D.M.S. is funded by the Canadian Institute for Health Research and the Canada Research Chairs Program. A.W.W. receives core funding support from the Scottish Government’s Rural and Environment Science and Analytical Services (RESAS). M.Y. is supported by the Azrieli Faculty Fellowship.
Author information
Authors and Affiliations
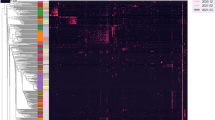
Contributions
N.S. and J.W. conceived the project. K.M.K. and M.C.d.G. performed analyses and generated figures. K.M.K., M.C.d.G., M.E.P.-M., F.D.B., M.A.E., S.C.G.-V., M.G.G., M.W.H., A.J.M., R.C.M., E.G.P., J.P., F.S., D.M.S., G.C.S.S., G.W.T., A.W.W., and J.W. wrote the draft. All authors provided feedback, participated in discussions and contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature thanks David Relman, Julia Segre and Sing Sing Way for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kennedy, K.M., de Goffau, M.C., Perez-Muñoz, M.E. et al. Questioning the fetal microbiome illustrates pitfalls of low-biomass microbial studies. Nature 613, 639–649 (2023). https://doi.org/10.1038/s41586-022-05546-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-022-05546-8
This article is cited by
-
Optimized bacterial community characterization through full-length 16S rRNA gene sequencing utilizing MinION nanopore technology
BMC Microbiology (2024)
-
Dynamic changes in the gut microbiota during three consecutive trimesters of pregnancy and their correlation with abnormal glucose and lipid metabolism
European Journal of Medical Research (2024)
-
The oral microbiome: diversity, biogeography and human health
Nature Reviews Microbiology (2024)
-
CRISPR-Cas-based identification of a sialylated human milk oligosaccharides utilization cluster in the infant gut commensal Bacteroides dorei
Nature Communications (2024)
-
The maternal gut microbiome in pregnancy: implications for the developing immune system
Nature Reviews Gastroenterology & Hepatology (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.