Abstract
Treating patients who have cancer with vaccines that stimulate a targeted immune response is conceptually appealing, but cancer vaccine trials have not been successful in late-stage patients with treatment-refractory tumours1,2. We are testing melanoma FixVac (BNT111)—an intravenously administered liposomal RNA (RNA-LPX) vaccine, which targets four non-mutated, tumour-associated antigens that are prevalent in melanoma—in an ongoing, first-in-human, dose-escalation phase I trial in patients with advanced melanoma (Lipo-MERIT trial, ClinicalTrials.gov identifier NCT02410733). We report here data from an exploratory interim analysis that show that melanoma FixVac, alone or in combination with blockade of the checkpoint inhibitor PD1, mediates durable objective responses in checkpoint-inhibitor (CPI)-experienced patients with unresectable melanoma. Clinical responses are accompanied by the induction of strong CD4+ and CD8+ T cell immunity against the vaccine antigens. The antigen-specific cytotoxic T-cell responses in some responders reach magnitudes typically reported for adoptive T-cell therapy, and are durable. Our findings indicate that RNA-LPX vaccination is a potent immunotherapy in patients with CPI-experienced melanoma, and suggest the general utility of non-mutant shared tumour antigens as targets for cancer vaccination.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from U.S. upon reasonable request. Upon completion of this clinical trial, summary-level results will be made public and shared in line with clinical data-sharing guidelines.
Code availability
For alignment of TCR sequences, an in-house bash pipeline using MiXCR 2.1.5 with default repseqio code was applied. For identification of paired TCR sequences from single-cell TCR sequencing data, an in-house Java tool was used. For bulk TCR profiling, an in-house bash pipeline using VDJTools and in-house Python scripts (for tracking of TCRs between samples) was used. In-house code is available from U.S. upon reasonable request.
References
Melero, I. et al. Therapeutic vaccines for cancer: an overview of clinical trials. Nat. Rev. Clin. Oncol. 11, 509–524 (2014).
Romero, P. et al. The Human Vaccines Project: a roadmap for cancer vaccine development. Sci. Transl. Med. 8, 334ps9 (2016).
Coulie, P. G., Van den Eynde, B. J., van der Bruggen, P. & Boon, T. Tumour antigens recognized by T lymphocytes: at the core of cancer immunotherapy. Nat. Rev. Cancer 14, 135–146 (2014).
Kyewski, B. & Derbinski, J. Self-representation in the thymus: an extended view. Nat. Rev. Immunol. 4, 688–698 (2004).
Holtkamp, S. et al. Modification of antigen-encoding RNA increases stability, translational efficacy, and T-cell stimulatory capacity of dendritic cells. Blood 108, 4009–4017 (2006).
Orlandini von Niessen, A. G. et al. Improving mRNA-based therapeutic gene delivery by expression-augmenting 3′ UTRs identified by cellular library screening. Mol. Ther. 27, 824–836 (2019).
Kreiter, S. et al. Increased antigen presentation efficiency by coupling antigens to MHC class I trafficking signals. J. Immunol. 180, 309–318 (2008).
Kranz, L. M. et al. Systemic RNA delivery to dendritic cells exploits antiviral defence for cancer immunotherapy. Nature 534, 396–401 (2016).
De Vries, J. & Figdor, C. Immunotherapy: cancer vaccine triggers antiviral-type defences. Nature 534, 329–331 (2016).
Simon, P. et al. Functional TCR retrieval from single antigen-specific human T cells reveals multiple novel epitopes. Cancer Immunol. Res. 2, 1230–1244 (2014).
Cheever, M. A. et al. The prioritization of cancer antigens: a national cancer institute pilot project for the acceleration of translational research. Clin. Cancer Res. 15, 5323–5337 (2009).
Pektor, S. et al. Toll like receptor mediated immune stimulation can be visualized in vivo by [18F]FDG-PET. Nucl. Med. Biol. 43, 651–660 (2016).
Reinhard, K. et al. An RNA vaccine drives expansion and efficacy of claudin-CAR-T cells against solid tumors. Science 367, 446–453 (2020).
Pektor, S. et al. In vivo imaging of the immune response upon systemic RNA cancer vaccination by FDG-PET. EJNMMI Res. 8, 80 (2018).
Jackson, H. et al. Striking immunodominance hierarchy of naturally occurring CD8+ and CD4+ T cell responses to tumor antigen NY-ESO-1. J. Immunol. 176, 5908–5917 (2006).
Hu, Y. et al. Immunologic hierarchy, class II MHC promiscuity, and epitope spreading of a melanoma helper peptide vaccine. Cancer Immunol. Immunother. 63, 779–786 (2014).
Hanagiri, T., van Baren, N., Neyns, B., Boon, T. & Coulie, P. G. Analysis of a rare melanoma patient with a spontaneous CTL response to a MAGE-A3 peptide presented by HLA-A1. Cancer Immunol. Immunother. 55, 178–184 (2006).
Grunwitz, C. et al. HPV16 RNA-LPX vaccine mediates complete regression of aggressively growing HPV-positive mouse tumors and establishes protective T cell memory. OncoImmunology 8, e1629259 (2019).
Robert, C. et al. Pembrolizumab versus ipilimumab in advanced melanoma. N. Engl. J. Med. 372, 2521–2532 (2015).
Rosenberg, S. A., Yang, J. C. & Restifo, N. P. Cancer immunotherapy: moving beyond current vaccines. Nat. Med. 10, 909–915 (2004).
Ribas, A. & Wolchok, J. D. Cancer immunotherapy using checkpoint blockade. Science 359, 1350–1355 (2018).
Hugo, W. et al. Genomic and transcriptomic features of response to anti-PD-1 therapy in metastatic melanoma. Cell 165, 35–44 (2016).
Simpson, A. J. G., Caballero, O. L., Jungbluth, A., Chen, Y.-T. & Old, L. J. Cancer/testis antigens, gametogenesis and cancer. Nat. Rev. Cancer 5, 615–625 (2005).
Hofbauer, G. F., Kamarashev, J., Geertsen, R., Böni, R. & Dummer, R. Tyrosinase immunoreactivity in formalin-fixed, paraffin-embedded primary and metastatic melanoma: frequency and distribution. J. Cutan. Pathol. 25, 204–209 (1998).
Nishino, M., Gargano, M., Suda, M., Ramaiya, N. H. & Hodi, F. S. Optimizing immune-related tumor response assessment: does reducing the number of lesions impact response assessment in melanoma patients treated with ipilimumab? J. Immunother. Cancer 2, 17 (2014).
Sahin, U. et al. Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer. Nature 547, 222–226 (2017).
Grabbe, S. et al. Translating nanoparticulate-personalized cancer vaccines into clinical applications: case study with RNA-lipoplexes for the treatment of melanoma. Nanomedicine 11, 2723–2734 (2016).
Batzri, S. & Korn, E. D. Single bilayer liposomes prepared without sonication. Biochim. Biophys. Acta 298, 1015–1019 (1973).
Barichello, J. M., Ishida, T. & Kiwada, H. Complexation of siRNA and pDNA with cationic liposomes: the important aspects in lipoplex preparation. Methods Mol. Biol. 605, 461–472 (2010).
Carey, T. E., Takahashi, T., Resnick, L. A., Oettgen, H. F. & Old, L. J. Cell surface antigens of human malignant melanoma: mixed hemadsorption assays for humoral immunity to cultured autologous melanoma cells. Proc. Natl Acad. Sci. USA 73, 3278–3282 (1976).
Brochet, X., Lefranc, M.-P. & Giudicelli, V. IMGT/V-QUEST: the highly customized and integrated system for IG and TR standardized V-J and V-D-J sequence analysis. Nucleic Acids Res. 36, W503–W508 (2008).
Bolotin, D. A. et al. MiXCR: software for comprehensive adaptive immunity profiling. Nat. Methods 12, 380–381 (2015).
Shugay, M. et al. VDJtools: unifying post-analysis of T cell receptor repertoires. PLOS Comput. Biol. 11, e1004503 (2015).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Patro, R., Mount, S. M. & Kingsford, C. Sailfish enables alignment-free isoform quantification from RNA-seq reads using lightweight algorithms. Nat. Biotechnol. 32, 462–464 (2014).
Robinson, D. R. et al. Integrative clinical genomics of metastatic cancer. Nature 548, 297–303 (2017).
Acknowledgements
We thank C. Gebhardt, M. R. Gaiser, A. Gaul, R. Roth, B. Steege, A. Oelbermann, C. Scharf, M. Kästner, F. Sari, U. Luxemburger, O. Renz, J. Grützner, D. Becker, M. Dorner, M. Hossainzadeh, M. C. Kühnle, M. Knezovic, P. Cienskowski, R. Mafondokoto, E. Godehardt, N. Bidmon, B. Stock, R. Schulz, C. Ecker, S. Wessel, K. Schmoldt, B. Schmitz, C. Anft, S. Jaegle, M. Maas and R. Hilker for technical support, project management and advice.
Author information
Authors and Affiliations
Contributions
U.S. conceptualized the work and strategy. P.O, E.D., T.O., S.A., R.R., A.B., J.Q., I.V., I.L. and S.R. planned and analysed experiments. A.B., C.T., J.C., L.H., A.H. and S.R. performed the experiments. M.G., D.M. and J.S. performed data analysis. A.N.K. and H.H. manufactured the RNA vaccines. R.A.J., D.S.-K., K.C., M.S. and A.K.-B. managed the clinical trial. M.L, V.M., H.M.-R., M.M., S.G, J.U., R.K., A.P. and J.C.H. are clinical investigators. C.L. is the principal clinical investigator. L.M.K., M.D. and S.K. established the RNA-LPX technology. U.S. and Ö.T., supported by P.O., E.D., M.V., M.G. and D.M., interpreted data and wrote the manuscript. All authors supported the review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
U.S., R.A.J., D.S.-K., A.N.K., L.M.K., M.D., S.K., H.H. and Ö.T. are inventors on patents related to the RNA-LPX vaccine technology. Some of the authors have securities from BioNTech.
Additional information
Peer review information Nature thanks Thomas Tueting and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
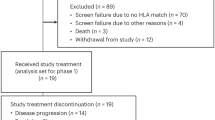
Extended Data Fig. 1 Patient subsets.
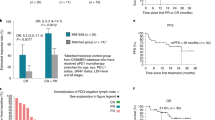
Patients had advanced melanoma either with radiographically measurable disease or with non-measurable disease at baseline. Immune monitoring was performed for 49 patients across all subgroups. Clinical antitumour activity was assessed in those 42 (1 unresected stage III C, 41 stage IV) of a total of 56 patients with measurable disease at baseline for whom follow-up imaging data were available at data cut-off (25 treated with FixVac monotherapy, 17 FixVac in combination with anti-PD1 therapy). The remaining 14 patients (5 receiving FixVac in monotherapy and 9 in combination with anti-PD1 therapy) were not included in the efficacy analyses for the reasons noted in the previous sentence. PD, progressive disease; PR, partial response; SD, stable disease (best objective overall responses as per irRECIST1.1). CR* refers to metabolic complete response of a patient with SD as best response, according to irRECIST1.1. Thirty-three patients with radiographically non-measurable disease at baseline were not subject to exploratory analysis for objective best overall response and are in follow-up for recurrence-free survival.
Extended Data Fig. 2 Characterization of cytokine secretion.
a, b, Peak plasma cytokine levels (6 h after vaccine injection) and body temperature (4 h after vaccine injection) for: a, all available patients; and b, patients treated with RNA-LPX target doses of 50 μg or 100 μg either alone (‘Mono’) or in combination with anti-PD1 therapy (‘aPD1’). Boxes show 25th to 75th quantiles with lines representing medians; whiskers show minimum to maximum values; grey dots show individual values per dose level; dashed lines indicate upper limits of normal. Sample numbers (n) are indicated in the figure. c, Correlation of plasma cytokine levels (y-axis) with plasma IFN-α concentration 6 h after RNA-LPX administration (n = 147 for IFN-γ, IL-12 p70 and IL-6; n = 147 for IP-10).
Extended Data Fig. 3 T-cell immunity induced by FixVac.
a, Phenotype (left) and quality (middle and right) of TAA-specific T cells measured by IFN-γ ELISpot post-IVS (left and middle) or ex vivo (right). Only positive responses are shown. b, Example flow cytometry of PBMCs from patient 12-01 stained with NY-ESO-192–100/Cw*0304 multimer. c, Flow cytometry gating strategy for phenotypic characterization of multimer+ T cells. Upper row, from left to right: starting with events acquired with a constant flow stream and fluorescence intensity, we identified single events (singlets). Dump-negative events (viable, CD4−, CD14−, CD16−, CD19−) and lymphocytes were identified and gated. Within lymphocytes, CD8+ HLA multimer positive T cells were gated for further analysis. Lower row, left plot: different subsets of CD8+ T cells (indicated in black) and NY-ESO-1 multimer positive CD8+ T cells (red) were gated on the basis of CD45RA and CCR7 expression into four subsets, analysed for CD27 and CD28 expression in the right-hand plots—central memory (CCR7+ CD45RA−), naive (CCR7+ CD45RA+) effector memory (CCR7− CD45RA−) and effector memory re-expressing RA (CCR7− CD45RA+). The expression of PD1 and OX40 was analysed for multimer-positive (red) and multimer-negative (black) CD8+ T cells. d, Detection of CD8+ T cells of patient A2-09 secreting IFN-γ and TNF after stimulation with MAGE-A3212–220 peptide. e, Comparison of fold induction of ex vivo spot counts after vaccination, between patients with measurable (n = 27) or non-measurable (n = 30) disease (left), patients treated with different vaccine doses (14.4 μg (n = 17), 50 μg (n = 10), 100 μg (n = 24); middle), and patients treated with FixVac alone (Mono (n = 44)) or in combination with anti-PD1 therapy (aPD1 (n = 12); right). Only positive responses at the post-vaccination visit are shown. A fold change of more than 2 compared with baseline was considered as a response to vaccine. If both CD4 and CD8 results were positive at post-treatment, only the ratio of the higher spot count is shown. f, Proportion of patients with vaccine-induced T-cell responses (de novo or amplified) determined by IFN-γ ELISpot pre- and post-vaccination, measured ex vivo from patients treated with FixVac alone (n = 14) or in combination with anti-PD1 therapy (n = 12). Data from patients with measurable disease only are shown.
Extended Data Fig. 4 Disease responses and treatment schedules for patients evaluated for clinical activity.
a, b, Swimmer plots for patients evaluable for efficacy assessments from the start of treatment to disease progression or continued treatment. a, Patients treated with melanoma FixVac in monotherapy. b, Patients treated with FixVac and anti-PD1 therapy. Dark green triangles indicate treatment start and completion. Dark green arrows show patients who are still receiving treatment. Red crosses mark disease progression; patients are sorted by best overall response and progression-free survival time (CR, PD, PR, SD). Light green stars indicate first documented objective responses and light green arrows indicate ongoing disease control. The black vertical lines mark the day planned for the eighth vaccination (study day 64). Single asterisks indicate patients for whom the clinical course and treatment schedules are shown in d. CR**, metabolic complete response of a patient with stable disease as the best response according to irRECIST1.1. Patients with radiologically non-measurable disease at baseline are in follow-up for recurrence-free survival and were not subject to clinical efficacy assessment. c, Tumour burden at baseline in relation to the clinical response upon FixVac treatment. PD, progressive disease; PR, partial response; SD, stable disease. d, Clinical course and treatment schedules of patients Pt 53-02, A2-09, C2-28, A2-10, C2-31 and C1-40. FD, first diagnosis of melanoma at any stage. FD stage IV, first diagnosis of melanoma at stage IV. *New bone lesion diagnosed and treated with radiotherapy.
Extended Data Fig. 5 T-cell immunity in patient 53-02 with partial response under FixVac monotherapy.
a, CT scans of the lower and middle lobes of the right lung before (pre) and after starting (post) melanoma FixVac treatment. b, Kinetics of a NY-ESO-196–104-specific, HLA-Cw*0304-restricted CD8+ T-cell response (see also Fig. 3a). c–f, Discovery and characterization of a NY-ESO-196–104-specific HLA-Cw*0304-restricted TCR. c, Sorting gate of multimer-positive CD8+ T cells (gated within the single, live, CD3+ lymphocyte population) for TCR cloning. Control, fluorescence minus one (FMO) sample. d, Recognition of peptide-pulsed HLA-Cw*0304-transfected K562 cells by NY-ESO-1-TCR-transfected CD8+ T cells in IFN-γ ELISpot. Control, HIV-gag PepMix; NY-ESO-1, NY-ESO-1 PepMix. e, Cytotoxicity of NY-ESO-1-TCR transfected healthy donor CD8+ T cells after 24 h of co-culture with HLA-transfected melanoma cell lines (SK-MEL-37 and SK-MEL-28; E:T = 50:1). f, Kinetics of NY-ESO-1-specific TCR clonotype frequency in TCR repertoire data obtained from pre- and post-vaccination PBMCs. g–j, Discovery and characterization of two NY-ESO-1124–133-specific HLA-B*4001-restricted TCRs. g, PBMCs were stimulated with NY-ESO-1 PepMix, and single IFN-γ positive CD8+ T cells were sorted via flow cytometry for TCR cloning (control, HIV-gag PepMix). h, i, HLA restriction and epitope specificity of NY-ESO-1-TCRs analysed after co-culture of TCR-transfected CD8+ T cells with peptide-pulsed HLA-transfected K562 cells using IFN-γ ELISpot. NY-ESO-1, NY-ESO-1 PepMix. j, Cytotoxicity of NY-ESO-1-specific TCRs identified in post-vaccination samples of the patient. TCR-transfected healthy donor CD8+ T cells were stimulated with HLA-transfected melanoma cell lines (SK-MEL-37, SK-MEL-28) for 12 h at an effector to target ratio of 20:1.
Extended Data Fig. 6 T-cell immunity in patients A2-10, C2-31 and C1-40.
a–f, Patient A2-10, with CPI-refractory melanoma, developed a partial response under FixVac monotherapy. a, CT scans of an inguinal lymph node metastasis obtained before and after the start of vaccination. b, Post-IVS CD4+ T-cell responses pre-vaccination and after eight vaccinations, restimulated in an IFN-γ ELISpot assay with autologous dendritic cells transfected with RNA (encoding one of the TAAs or luciferase as control), or pulsed with TAA-encoding PepMix versus unpulsed dendritic cells (no peptide). c, Cytokine-secreting CD8+ and CD4+ T cells after intradermal challenge with NY-ESO-1 RNA. Skin-infiltrating lymphocytes were recovered from a punch biopsy 15 days after 8 weekly vaccinations and stimulated with PepMix encoding NY-ESO-1 or tyrosinase. d–f, Discovery and characterization of HLA II restricted TAA-specific TCRs. d, CD4+ T cells from IVS cultures were restimulated with PepMix-pulsed dendritic cells and sorted via flow cytometry for TCR cloning (control, HIV-gag PepMix). APC and PE are fluorochrome labels. e, Determination of HLA restriction and epitope specificity using TCR-transfected healthy donor CD4+ T cells and RNA-transfected or peptide-pulsed HLA-transfected K562 cells by IFN-γ ELISpot. DRA, DRB, DQA and DQB numbers refer to specific HLA alleles. Control, K562 cells without peptide (–). f, Kinetics of TCR clonotype frequencies in peripheral blood by ex vivo TCR repertoire analysis. g, TAA-specific CD8+ and CD4+ T-cell responses of patient C2-31 by IFN-γ ELISpot on peptide-loaded autologous dendritic cells after IVS with TAA PepMix. Control, dendritic cells loaded with irrelevant peptide. h, i, Clinical and immune responses of patient C1-40, with CPI-refractory melanoma, who developed a partial response under melanoma FixVac combined with nivolumab. h, CT scans of the right middle and left lower lung lobes before and after the start of melanoma FixVac treatment. i, Ex vivo frequencies of MAGE-A3168–176-specific A*0101-restricted (left panel) and NY-ESO-192–100-specific HLA_Cw*0304-restricted (right panel) CD8+ T cells analysed by HLA multimer staining.
Supplementary information
Supplementary Information
This file contains Supplementary Figures 1 – 9 (Gating strategies) and Supplementary Table 1 (Antigen specific α/β TCRs isolated from single T cells of melanoma patients).
Rights and permissions
About this article
Cite this article
Sahin, U., Oehm, P., Derhovanessian, E. et al. An RNA vaccine drives immunity in checkpoint-inhibitor-treated melanoma. Nature 585, 107–112 (2020). https://doi.org/10.1038/s41586-020-2537-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-020-2537-9
This article is cited by
-
mRNA-based precision targeting of neoantigens and tumor-associated antigens in malignant brain tumors
Genome Medicine (2024)
-
Refining mutanome-based individualised immunotherapy of melanoma using artificial intelligence
European Journal of Medical Research (2024)
-
Genetic fusion of CCL11 to antigens enhances antigenicity in nucleic acid vaccines and eradicates tumor mass through optimizing T-cell response
Molecular Cancer (2024)
-
T-cell stimulating vaccines empower CD3 bispecific antibody therapy in solid tumors
Nature Communications (2024)
-
Stereocontrolled access to thioisosteres of nucleoside di- and triphosphates
Nature Chemistry (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.