Abstract
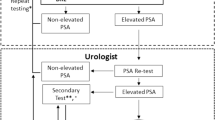
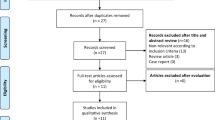
In the pre-PSA-detection era, a large proportion of men were diagnosed with metastatic prostate cancer and died of the disease; after the introduction of the serum PSA test, randomized controlled prostate cancer screening trials in the USA and Europe were conducted to assess the effect of PSA screening on prostate cancer mortality. Contradictory outcomes of the trials and the accompanying overdiagnosis resulted in recommendations against prostate cancer screening by organizations such as the United States Preventive Services Task Force. These recommendations were followed by a decline in PSA testing and a rise in late-stage diagnosis and prostate cancer mortality. Re-evaluation of the randomized trials, which accounted for contamination, showed that PSA-based screening does indeed reduce prostate cancer mortality; however, the debate about whether to screen or not to screen continues because of the considerable overdiagnosis that occurs using PSA-based screening. Meanwhile, awareness among the population of prostate cancer as a potentially lethal disease stimulates opportunistic screening practices that further increase overdiagnosis without the benefit of mortality reduction. However, in the past decade, new screening tools have been developed that make the classic PSA-only-based screening an outdated strategy. With improved use of PSA, in combination with age, prostate volume and with the application of prostate cancer risk calculators, a risk-adapted strategy enables improved stratification of men with prostate cancer and avoidance of unnecessary diagnostic procedures. This combination used with advanced detection techniques (such as MRI and targeted biopsy), can reduce overdiagnosis. Moreover, new biomarkers are becoming available and will enable further improvements in risk stratification.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Stang, A. & Jöckel, K. H. The impact of cancer screening on all-cause mortality: what is the best we can expect? Dtsch. Arztebl Int. 115, 481–486 (2018).
Loeb, S. et al. Overdiagnosis and overtreatment of prostate cancer. Eur. Urol. 65, 1046–1055 (2014).
Aizer, A. A. et al. Cost implications and complications of overtreatment of low-risk prostate cancer in the United States. J. Natl Compr. Cancer Netw. 13, 61–68 (2015).
Wang, M. C. et al. Purification of a human prostate specific antigen. Investig. Urol. 17, 159–163 (1979).
Papsidero, L. D. et al. A prostate antigen in sera of prostatic cancer patients. Cancer Res. 40, 2428–2432 (1980).
Kuriyama, M. et al. Quantitation of prostate-specific antigen in serum by a sensitive enzyme immunoassay. Cancer Res. 40, 4658–4662 (1980).
Kuriyama, M. et al. Use of human prostate-specific antigen in monitoring prostate cancer. Cancer Res. 41, 3874–3876 (1981).
Nadler, R. B., Humphrey, P. A., Smith, D. S., Catalona, W. J. & Ratliff, T. L. Effect of inflammation and benign prostatic hyperplasia on elevated serum prostate specific antigen levels. J. Urol. 154, 407–413 (1995).
Ming-Chu, T. Prostate specific antigen (PSA): the historical perspective. MJM https://doi.org/10.26443/mjm.v2i2.564 (1996).
Chu, T. M., Wang M. C. & Papsidero, L. Purified human prostate antigen United States Patent and Trademark Office. https://patft.uspto.gov/netacgi/nph-Parser?Sect1=PTO2&Sect2=HITOFF&p=1&u=%2Fnetahtml%2FPTO%2Fsearch-bool.html&r=5&f=G&l=50&co1=AND&d=PTXT&s1=316954.AP.&OS=APN/316954&RS=APN/316954 (1984).
Stamey, T. A. et al. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N. Engl. J. Med. 317, 909–916 (1987).
Roth, J. A., Gulati, R., Gore, J. L., Cooperberg, M. R. & Etzioni, R. Economic analysis of prostate-specific antigen screening and selective treatment strategies. JAMA Oncol. 2, 890–898 (2016).
Catalona, W. J. et al. Measurement of prostate-specific antigen serum as a screening test for prostate cancer. N. Engl. J. Med. 324, 1156–1161 (1991).
Thompson, I. M., Ernst, J. J., Gangai, M. P. & Spence, C. R. Adenocarcinoma of the prostate: results of routine urological screening. J. Urol. 132, 690–692 (1984).
Schröder, F. H. et al. Screening and prostate-cancer mortality in a randomized European study. N. Engl. J. Med. 360, 1320–1328 (2009).
Andriole, G. L. et al. Mortality results from a randomized prostate-cancer screening trial. N. Engl. J. Med. 360, 1310–1319 (2009).
Hsing, A. W., Tsao, L. & Devesa, S. S. International trends and patterns of prostate cancer incidence and mortality. Int. J. Cancer 85, 60–67 (2000).
RGHM Cremers, H. E. et al. Prostate cancer: trends in incidence, survival and mortality in the Netherlands, 1989–2006. Eur. J. Urol. 46, 2077–2087 (2010).
Roobol, M. J., Kirkels, W. J. & Schöder, F. H. Features and preliminary results of the Dutch centre of the ERSPC (Rotterdam, the Netherlands). BJU Int https://doi.org/10.1111/j.1464-410X.2003.04390.x (2004).
National Cancer Institute. Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO). NIH https://prevention.cancer.gov/major-programs/prostate-lung-colorectal-and-ovarian-cancer-screening-trial (2020).
The European Randomized study of Screening for Prostate Cancer. ERSPC Background. ERSPC https://www.erspc.org/prostate-cancer/erspc-background/#study-protocol (2021).
Schröder, F. H. & Roobol, M. J. ERSPC and PLCO prostate cancer screening studies: what are the differences? Eur. Urol. 58, 46–52 (2010).
de Koning, H. J. et al. The efficacy of prostate-specific antigen screening: impact of key components in the ERSPC and PLCO trials. Cancer 124, 1197–1206 (2018).
Welch, H. G. & Albertsen, P. C. Reconsidering prostate cancer mortality — the future of PSA screening. N. Engl. J. Med. 382, 1557–1563 (2020).
Culp, M. B., Soerjomataram, I., Efstathiou, J. A., Bray, F. & Jemal, A. Recent global patterns in prostate cancer incidence and mortality rates. Eur. Urol. 77, 38–52 (2020).
Carioli, G. et al. European cancer mortality predictions for the year 2020 with a focus on prostate cancer. Ann. Oncol. 31, 650–658 (2020).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J. Clin. 71, 209–249 (2021).
U.S. Preventive Services Task Force. Screening for prostate cancer: recommendation and rationale. Ann. Intern. Med. 137, 915–916 (2002).
U.S. Preventive Services Task Force. Screening for prostate cancer: US Preventive Services Task Force recommendation statement. Ann. Intern. Med. 149, 185–191 (2008).
Moyer, V. A. Screening for Prostate Cancer: US Preventive Services Task Force recommendation statement. Ann. Intern. Med. 157, 120–134 (2012).
Jemal, A., Culp, M. B., Ma, J., Islami, F. & Fedewa, S. A. Prostate cancer incidence 5 years after US Preventive Services Task Force recommendations against screening. J. Natl Inst. 113, 64–71 (2021).
Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. Prostate cancer screening with the PSA test. IQWIG https://www.iqwig.de/projekte/s19-01.html (2020).
UK National Screening Committee. Screening for prostate cancer. UK National Screening Committee https://view-health-screening-recommendations.service.gov.uk/document/424/download (2020).
Ilic, D. et al. Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ 362, K3519 (2018).
Tikkinen, K. et al. Prostate cancer screening with prostate-specific antigen (PSA) test: a clinical practice guideline. BMJ 362, K3581 (2018).
Lenzen-Schulte, M. Prostatakrebs-screening: Prüffall PSA-test. Dtsch. Arztebl 117, 1–2 (2020).
Shoag, J. E., Mittal, S., Hu, J. C. & Reevaluating, P. S. A. Testing rates in the PLCO trial. N. Engl. J. Med. 374, 1795–1796 (2016).
Tsodikov, A. et al. Reconciling the effects of screening on prostate cancer mortality in the ERSPC and PLCO trials. Ann. Intern. Med. 167, 449–455 (2017).
Grossman, D. C. et al. Screening for prostate cancer: US preventive services task force recommendation statement. JAMA 319, 1901–1913 (2018).
European Association of Urology. Archive of the Prostate Cancer guideline. EAU https://uroweb.org/guidelines/archive/prostate-cancer (2020).
Martin, R. M. et al. CAP Trial Group effect of a low-intensity PSA-based screening intervention on prostate cancer mortality: the CAP randomized clinical trial. JAMA 319, 883–895 (2018).
Hugosson, J. et al. Eighteen-year follow-up of the Göteborg randomized population-based prostate cancer screening trial: effect of sociodemographic variables on participation, prostate cancer incidence and mortality. Scand. J. Urol. 52, 27–37 (2018).
Hugosson, J. et al. A 16-yr follow-up of the European randomized study of screening for prostate cancer. Eur. Urol. 76, 43–51 (2019).
Pinsky, P. F. et al. Extended follow-up for prostate cancer incidence and mortality among participants in the Prostate, Lung, Colorectal and Ovarian randomized cancer screening trial. BJU Int. 123, 854–860 (2019).
Roobol., M. J. Screening for prostate cancer: are organized screening programs necessary? Trans. Androl. Urol. 7, 4–11 (2018).
Heijnsdijk, E. A. M. et al. Quality-of-life effects of prostate-specific antigen screening. N. Engl. J. Med. 367, 595–605 (2012).
RIZIV/INAMI, National Institute for Health and Disability Insurance (NIHDI), Nomenclature of medical acts in Belgium, Chapter V, 11 clinical biology (2021).
Heidenreich, A. et al. Early detection of prostate cancer: European Association of Urology recommendation. Eur. Urol. 64, 347–354 (2013).
Yard, D. H. PSA testing: why the U.S. and Europe differ. Renal & Urology News https://www.renalandurologynews.com/home/news/urology/prostate-cancer/psa-testing-why-the-u-s-and-europe-differ/ (2011).
Ciatto, S. et al. Contamination by opportunistic screening in the European Randomized Study of Prostate Cancer Screening. BJU Int. 92 (Suppl 2), 97–100 (2003).
Pinsky, P. F. et al. Assessing contamination and compliance in the prostate component of the prostate, lung, colorectal, and ovarian (PLCO) cancer screening trial. Clin. Trials 7, 303–311 (2010).
Clift, A. K., Coupland, C. A. C. & Hippisley-Cox, J. Prostate-specific antigen testing and opportunistic prostate cancer screening: a cohort study in England, 1998–2017. Br. J. Gen. Pract. 71, e157–e165 (2021).
Rijksinstituut voor Ziekte-en Invaliditeitsverzekering (RIZIV/INAMI) statistical department. Statistieken geneeskundige verzorging https://www.riziv.fgov.be/nl/statistieken/geneesk-verzorging/Paginas/default.aspx (2020).
Belgian Cancer Registry. Cancer Fact Sheet: Prostate Cancer. Belgian Cancer Registry https://kankerregister.org/media/docs/CancerFactSheets/2019/Cancer_Fact_Sheet_ProstateCancer_2019.pdf (2019).
Integraal Kankercentrum Nederland. Prostaatkanker in Nederland. Integraal Kankercentrum Nederland https://iknl.nl/prostaatkanker-in-nederland (2020).
Fleshner, K., Carlsson, S. V. & Roobol, M.J. The effect of the USPSTF PSA screening recommendation on prostate cancer incidence patterns in the USA. Nat. Rev. Urol. 14, 26–37 (2017).
Bandini, M. et al. Increase in the annual rate of newly diagnosed metastatic prostate cancer: a contemporary analysis of the surveillance, epidemiology and end result database. Eur. Urol. Oncol. 1, 314–320 (2018).
Siegel, D. A., O’Neil, M. E., Richards, T. B., Dowling, N. F. & Weir, H. K. Prostate cancer incidence and survival, by stage and race/ethnicity — United States, 2001–2017. MMWR Morb. Mortal. Wkly. Rep. 69, 1473–1480 (2020).
Ferlay, J. et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur. J. Cancer 103, 356–387 (2018).
Sharma, V., Venkataramana, A., Comulada, W. S., Litwin, M. S. & Saigal, C. Association of reductions in PSA screening across states with increased metastatic prostate cancer in the United States. J. Clin. Oncol. 39, 228 (2021).
Prostate Cancer UK. We call on UK to step up as new figures show prostate cancer now a bigger killer than breast cancer. Prostate Cancer UK https://prostatecanceruk.org/about-us/news-and-views/2018/2/we-call-on-uk-to-step-up-as-new-figures-show-prostate-cancer-now-a-bigger-killer-than-breast-cancer (2018).
Butler, E. B., Kelly, S. P., Coupland, V. H., Rosenberg, P. S. & Cook, M. B. Fatal prostate cancer incidence trends in the United States and England by race, stage, and treatment. Br. J. Cancer 123, 487–494 (2020).
Arnsrud Godtman, R., Holmberg, E., Lilja, H., Stranne, J. & Hugosson, J. Opportunistic testing versus organized prostate-specific antigen screening: outcome after 18 years in the Göteborg randomized population-based prostate cancer screening trial. Eur. Urol. 68, 354–360 (2015).
Pickles, K., Carter, S. M. & Rychetnik, L. C. Doctors’ approaches to PSA testing and overdiagnosis in primary healthcare: a qualitative study. BMJ Open 5, e006367 (2015).
Guessous, I. et al. Prostate cancer screening in Switzerland: 20-year trends and socioeconomic disparities. Prev. Med. 82, 83–91 (2016).
Jessen, K., Sondergaard, J., Veldt Larsen, P. & Thomsen, J. L. Danish general practitioners’ use of prostate-specific antigen in opportunistic screening for prostate cancer: a survey comprising 174 GPs. Int. J. Fam. Med. https://doi.org/10.1155/2013/540707 (2013).
Matti, B. & Zargar-Shoshtari, K. Opportunistic prostate cancer screening: a population-based analysis. Urol. Oncol. 38, 393–400 (2020).
Fossa, S. D. & Eri, L. M. Norske legers rutiner for opportunistisk screening for prostatekreft. Tidsskr. Nor. Laegeforen. 199, 3572–3576 (1999).
Bertuccio, P. et al. Mortality trends from urologic cancers in Europe over the period 1980–2017 and a projection to 2025. Eur. Urol. Oncol. 4, 677–696 (2021).
Patasius, A. & Smailyte, G. Changing incidence and stage distribution of prostate cancer in a Lithuanian population — evidence from national PSA-based screening program. Int. J. Environ. Res. Public Health 16, 4856 (2019).
Patasius, A. et al. Prostate cancer incidence and mortality in the Baltic states Belarus, the Russian Federation and Ukraine. BMJ Open. 9, e031856 (2019).
Moyer, V. A. & U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 157, 120–134 (2012).
Basch, E. et al. Screening for prostate cancer with prostate-specific antigen testing: American Society of Clinical Oncology provisional clinical opinion. J. Clin. Oncol. 30, 3020–3025 (2012).
Wolf, A. M. et al. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J. Clin. 60, 70–98 (2010).
Carter, H. B. et al. Early detection of prostate cancer: AUA Guideline. J. Urol. 190, 419–426 (2013).
National Comprehensive Cancer Network. Prostate Cancer Early Detection. NCCN http://www.nccn.org/professionals/physician_gls/pdf/prostate_detection.pdf (2021).
Mottet, N. et al. EAU-EANM-ESTRO-SIOG Guidelines on Prostate Cancer — 2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur. Urol. 79, 243–262 (2021).
Rommel, F. M. et al. The use of prostate specific antigen and prostate specific antigen density in the diagnosis of prostate cancer in community based urology practice. J. Urol. 151, 88–93 (1994).
Nordström, T., Akre, O., Aly, M., Grönberg, H. & Eklund, M. Prostate-specific antigen (PSA) density in the diagnostic algorithm of prostate cancer. Prostate Cancer Prostatic Dis. 21, 57–63 (2018).
Abd-Alazeez, M. et al. The accuracy of multiparametric MRI in men with negative biopsy and elevated PSA level — can it rule out clinically significant prostate cancer? Urol. Oncol. 32, 45.e17–e22 (2014).
Stichting Wetenschappelijk Onderzoek Prostaatkanker, Reeuwijk. Your Prostate Cancer Risk Calculator. prostatecancer-riskcalculator.com https://www.prostatecancer-riskcalculator.com/assess-your-risk-of-prostate-cancer (2022).
Ankerst, D. P. et al. The Prostate Cancer Prevention Trial Risk Calculator 2.0 for the prediction of low- versus high-grade prostate cancer. Urology 83, 1362–1367 (2014).
Roobol., M. J. Rescreening policies and risk calculator. J. Nat. Rev. Urol. 11, 429–430 (2014).
Louie, K. S., Seigneurin, A., Cathcart, P. & Sasieni, P. Do prostate cancer risk models improve the predictive accuracy of PSA screening? A meta-analysis. Ann. Oncol. 26, 848–864 (2015).
Stabile, A. et al. Multiparametric MRI for prostate cancer diagnosis: current status and future directions. Nat. Rev. Urol. 17, 41–61 (2020).
Alberts, A. R. et al. Prediction of high-grade prostate cancer following multiparametric magnetic resonance imaging improving the Rotterdam European Randomized study of screening for prostate cancer risk calculators. Eur. Urol. 75, 310–318 (2019).
Mottet N, et al. EAU guidelines: EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer (EAU Guidelines Office, 2019).
Van Poppel, H. et al. Prostate-specific antigen testing as part of a risk-adapted early detection strategy for prostate cancer: European Association of Urology position and recommendations for 2021. Eur. Urol. 80, 703–711 (2021).
Schröder, F. H. et al. Screening for prostate cancer decreases the risk of developing metastatic disease: findings from the European randomized study of screening for prostate cancer (ERSPC). Eur. Urol. 62, 745–752 (2012).
Vickers, A. J. et al. A panel of kallikrein markers can reduce unnecessary biopsy for prostate cancer: data from the European randomized study of prostate cancer screening in Göteborg, Sweden. BMC Med. 6, 19 (2008).
Jansen, F. H. et al. Prostate-specific antigen (PSA) isoform p2PSA in combination with total PSA and free PSA improves diagnostic accuracy in prostate cancer detection. Eur. Urol. 57, 921–927 (2010).
Osses, D. F., Roobol, M. J. & Schoots., I. G. Prediction medicine: biomarkers, risk calculators and magnetic resonance imaging as risk stratification tools in prostate cancer diagnosis. Int. J. Mol. Sci. 20, 1637 (2019).
Roobol, M. J. et al. Prediction of prostate cancer risk: the role of prostate volume and digital rectal examination in the ERSPC risk calculators. Eur. Urol. 61, 577–583 (2012).
Pereira-Azevedo, N. et al. Prospective evaluation on the effect of interobserver variability of digital rectal examination on the performance of the Rotterdam prostate cancer risk calculator. Int. J. Urol. 24, 826–832 (2017).
Ankerst, D. P. et al. Prostate Cancer Prevention Trial risk calculator 2.0 for the prediction of low- vs high-grade prostate cancer. Urology 83, 1362–1368 (2014).
Mannaerts, C. K. et al. Prostate cancer risk assessment in biopsy-naive patients: the Rotterdam prostate cancer risk calculator in multiparametric magnetic resonance imaging-transrectal ultrasound (TRUS) fusion biopsy and systematic TRUS biopsy. Eur. Urol. Oncol. 1, 109–117 (2018).
Weinreb, J. C. et al. PI-RADS prostate imaging-reporting and data system: 2015, version 2. Eur. Urol. 69, 16–40 (2016).
Pagniez, M. A. et al. Predictive factors of missed clinically significant prostate cancers in men with negative magnetic resonance imaging: a systematic review and meta-analysis. J. Urol. 204, 24–32 (2020).
Ullrich, T. et al. Risk stratification of equivocal lesions on multiparametric magnetic resonance imaging of the prostate. J. Urol. 199, 691–698 (2018).
Shill, D. K., Roobol, M. J., Ehdaie, B., Vickers, A. J. & Carlsson, S. V. Active surveillance for prostate cancer. Trans. Androl. Urol. 10, 2809–2819 (2021).
Desai, M. M. et al. Trends in incidence of metastatic prostate cancer in the US. JAMA Netw. Open 5, e222246 (2022).
Ross, L. E., Hall, I. J., Howard, D. L., Rim, S. H. & Richardson, L. C. Primary care physicians beliefs about prostate-specific antigen evidence uncertainty, screening efficacy, and test use. J. Natl Med. Assoc. 110, 491–500 (2018).
Drummond, F. J., Carsin, A.-E., Sharp, L. & Comber, H. Factors prompting PSA-testing of asymptomatic men in a country with no guidelines: a national survey of general practitioners. BMC Fam. Pract. 10, 1–12 (2009).
Kappen, S., Jurgens, V., Freitag, M. H. & Winter, A. Early detection of prostate cancer using prostate-specific antigen testing: an empirical evaluation among general practitioners and urologists. Cancer Manag. Res. 11, 3079–3097 (2019).
Cajka., P. Issues of an ageing population in European Union. Environ. Sci. Eng. B. 1, 966–970 (2012).
Rawla., P. Epidemiology of prostate cancer. World J. Urol. 10, 63–89 (2019).
Eurostat. Ageing Europe — looking at the lives of older people in the EU — 2019 edition. (2019)
Getaneh, A. M. et al. Assessment of harms, benefits, and cost-effectiveness of prostate cancer screening: a micro-simulation study of 230 scenarios. Cancer Med. 9, 7742–7750 (2020).
Carlsson, S. V. et al. Estimating the harms and benefits of prostate cancer screening as used in common practice versus recommended good practice: a microsimulation screening analysis. Cancer 122, 3386–3393 (2016).
Sanghera, S. et al. Cost-effectiveness of prostate cancer screening: a systematic review of decision-analytical models. BMC Cancer 18, 84 (2018).
Callender, T. et al. Benefit, harm, and cost-effectiveness associated with magnetic resonance imaging before biopsy in age-based and risk-stratified screening for prostate cancer. JAMA Netw. Open 4, e2037657 (2021).
de Rooij, M. et al. Cost-effectiveness of magnetic resonance (MR) imaging and MR-guided targeted biopsy versus systematic transrectal ultrasound-guided biopsy in diagnosing prostate cancer: a modelling study from a health care perspective. Eur. Urol. 66, 430–436 (2014).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 395, 795–808 (2020).
Grönberg, H. et al. Prostate cancer screening in men aged 50–69 years (STHLM3): a prospective population-based diagnostic study. Lancet Oncol. 16, P1667–P1676 (2015).
Mortezavi, A. et al. Head-to-head comparison of conventional, and image- and biomarker-based prostate cancer risk calculators. Eur. Urol. Focus. 7, 546–553 (2021).
Eklund, M. et al. The Stockholm-3 (STHLM3) model can improve prostate cancer diagnostics in men aged 50–69 yr compared with current prostate cancer testing. Eur. Urol. Focus. 4, 707–710 (2018).
Eklund, M. et al. MRI-targeted or standard biopsy in prostate cancer screening. N. Engl. J. Med. 385, 908–920 (2021).
Twilt, J. J. et al. Artificial intelligence based algorithms for prostate cancer classification and detection on magnetic resonance imaging: a narrative review. Diagnostics 11, 959 (2021).
Knaapila, J. et al. Negative predictive value of biparametric prostate magnetic resonance imaging in excluding significant prostate cancer: a pooled data analysis based on clinical data from four prospective, registered studies. Eur. Urol. Focus. 7, 522–531 (2021).
Wallström, J. et al. Bi- or multiparametric MRI in a sequential screening program for prostate cancer with PSA followed by MRI? Results from the Goteborg prostate cancer screening 2 trial. Eur. Radiol. 31, 8692–8702 (2021).
Remmers, S. & Roobol, M. J. Personalized strategies in population screening for prostate cancer. Int. J. Cancer 147, 2977–2987 (2020).
Van Poppel, H. et al. A European model for an organised risk-stratified early detection programme for prostate cancer. Eur. Urol. Oncol. 5, P731–P739 (2021).
European Association of Urology. Information for patients: prostate cancer. EAU https://patients.uroweb.org/wp-content/uploads/2018/12/12-July-2018_Prostate-cancer.pdf (2014).
National Health Service. PSA testing and prostate cancer: advice for well men aged 50 and over. NHS https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/856976/PSA_testing_for_prostate_cancer_information_for_well_men.pdf (2020).
Xavier, R. et al. Risk prediction tools in cardiovascular disease prevention: a report from the ESC Prevention of CVD Programme led by the European Association of Preventive Cardiology (EAPC) in collaboration with the Acute Cardiovascular Care Association (ACCA) and the Association of Cardiovascular Nursing and Allied Professions (ACNAP). Eur. J. Prev. Cardiol. 26, 1534–1544 (2019).
Mishra, S. C. A discussion on controversies and ethical dilemmas in prostate cancer screening. J. Med. Ethics 47, 152–158 (2021).
Légaré, F. & Thompson-Leduc, P. Twelve myths about shared decision making. Patient Educ. Couns. 96, 281–286 (2014).
Roobol, M. J. Active surveillance for prostate cancer — will the discoveries of the last 5 years change the future? Transl. Androl. Urol. 10, 2828–2831 (2021).
Author information
Authors and Affiliations
Contributions
H.V.P., R.H. and M.R. researched data for the article. H.V.P., T.A., P.B., R.H. and M.R. contributed substantially to discussion of the content. H.V.P., R.H., M.R. and S.C. wrote the article. H.V.P., T.A., P.B., R.H. and M.R. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Quoc-Dien Trinh, Mara Koelker and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer or the World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer or the World Health Organization.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
EU4Health: https://health.ec.europa.eu/funding/eu4health-programme-2021-2027-vision-healthier-european-union_en
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Van Poppel, H., Albreht, T., Basu, P. et al. Serum PSA-based early detection of prostate cancer in Europe and globally: past, present and future. Nat Rev Urol 19, 562–572 (2022). https://doi.org/10.1038/s41585-022-00638-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-022-00638-6
This article is cited by
-
The learning curve for robotic-assisted transperineal MRI/US fusion-guided prostate biopsy
Scientific Reports (2024)
-
Key learning on the promise and limitations of MRI in prostate cancer screening
European Radiology (2024)
-
Preliminary study on miRNA in prostate cancer
World Journal of Surgical Oncology (2023)
-
Genomic and Phenotypic Biomarkers for Precision Medicine Guidance in Advanced Prostate Cancer
Current Treatment Options in Oncology (2023)
-
Characterization of protein-based risk signature to predict prognosis and evaluate the tumor immune environment in breast cancer
Breast Cancer (2023)