Abstract
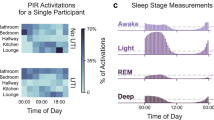
Regular health monitoring can result in early detection of disease, accelerate the delivery of medical care and, therefore, considerably improve patient outcomes for countless medical conditions that affect public health. A substantial unmet need remains for technologies that can transform the status quo of reactive health care to preventive, evidence-based, person-centred care. With this goal in mind, platforms that can be easily integrated into people’s daily lives and identify a range of biomarkers for health and disease are desirable. However, urine — a biological fluid that is produced in large volumes every day and can be obtained with zero pain, without affecting the daily routine of individuals, and has the most biologically rich content — is discarded into sewers on a regular basis without being processed or monitored. Toilet-based health-monitoring tools in the form of smart toilets could offer preventive home-based continuous health monitoring for early diagnosis of diseases while being connected to data servers (using the Internet of Things) to enable collection of the health status of users. In addition, machine learning methods can assist clinicians to classify, quantify and interpret collected data more rapidly and accurately than they were able to previously. Meanwhile, challenges associated with user acceptance, privacy and test frequency optimization should be considered to facilitate the acceptance of smart toilets in society.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
National Science Foundation. Smart and Connected Health. https://www.nsf.gov/funding/pgm_summ.jsp?pims_id=504739 (2016).
U.S. Centers for Medicare & Medicaid Services. National Health Expenditure Fact Sheet. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NHE-Fact-Sheet (2020).
U.S. Centers for Medicare & Medicaid Services. National Health Expenditure Data, Historical. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical (2020).
Department of Health and Human Services Tips about the Health Insurance Marketplace. https://www.healthcare.gov/quick-guide/ (2021).
Sandhu, G. S. & Andriole, G. L. Overdiagnosis of prostate cancer. J. Natl Cancer Inst. Monogr. 2012, 146–151 (2012).
Gilbert, N. The pros and cons of screening. Nature 579, S2–S2 (2020).
Batarseh, F. A., Ghassib, I., Chong, D. S. & Su, P.-H. Preventive healthcare policies in the US: solutions for disease management using Big Data Analytics. J. Big Data 7, 1–25 (2020).
Malone, K. M. & Hinman, A. R. Vaccination mandates: the public health imperative and individual rights. Law Public Health Pract. 338, 339–340 (2003).
American Cancer Society. Key statistics for ovarian cancer. cancer.org https://www.cancer.org/cancer/ovarian-cancer/about/key-statistics.html (2021).
National Heart, Lung, and Blood Institute. Blood tests. nhlbi.nih.gov https://www.nhlbi.nih.gov/health-topics/blood-tests#::text=Specifically%2C%20blood%20tests%20can%20help,risk%20factors%20for%20heart%20disease
Dabbagh, S. R. et al. 3D-printed microneedles in biomedical applications. iScience 24, 102012 (2021).
Topkas, E., Keith, P., Dimeski, G., Cooper-White, J. & Punyadeera, C. Evaluation of saliva collection devices for the analysis of proteins. Clin. Chim. Acta 413, 1066–1070 (2012).
Liu, J. & Duan, Y. Saliva: a potential media for disease diagnostics and monitoring. Oral. Oncol. 48, 569–577 (2012).
Pfaffe, T., Cooper-White, J., Beyerlein, P., Kostner, K. & Punyadeera, C. Diagnostic potential of saliva: current state and future applications. Clin. Chem. 57, 675–687 (2011).
Papacosta, E. & Nassis, G. P. Saliva as a tool for monitoring steroid, peptide and immune markers in sport and exercise science. J. Sci. Med. Sport. 14, 424–434 (2011).
de la Torre, R. et al. Clinical pharmacokinetics of amfetamine and related substances. Clin. Pharmacokinet. 43, 157–185 (2004).
Caplan, Y. H. & Goldberger, B. A. Alternative specimens for workplace drug testing. J. Anal. Toxicol. 25, 396–399 (2001).
Tai, L.-C. et al. Nicotine monitoring with a wearable sweat band. ACS Sens. 5, 1831–1837 (2020).
Kudo, H., Suzuki, Y., Tojo, Y., Saito, H. & Enomoto, K. in 2019 IEEE 14th International Conference on Nano/Micro Engineered and Molecular Systems (NEMS) 44–47 (IEEE, 2019).
Hourlier-Fargette, A. et al. Skin-interfaced soft microfluidic systems with modular and reusable electronics for in situ capacitive sensing of sweat loss, rate and conductivity. Lab Chip 20, 4391–4403 (2020).
Jadoon, S. et al. Recent developments in sweat analysis and its applications. Int. J. Anal. Chem. 2015, 4391 (2015).
Wang, J., Mercier, P. & Noghera, C. Center for wearable sensors. ucsd.edu https://cws.ucsd.edu/about (2020).
Merriam Webster Online. Definition of urine. https://www.merriam-webster.com/dictionary/urine (2020).
Baig, A. Biochemical composition of normal urine. Nat. Prec. https://doi.org/10.1038/npre.2011.6595.1 (2011).
Dantzler, W. H. in Comparative Physiology of the Vertebrate Kidney 37–80 (Springer, 2016).
Lepowsky, E., Ghaderinezhad, F., Knowlton, S. & Tasoglu, S. Paper-based assays for urine analysis. Biomicrofluidics 11, 051501 (2017).
Beasley-Green, A. Urine proteomics in the era of mass spectrometry. Int. Neurourol. J. 20, S70 (2016).
Antic, T. & DeMay, R. M. The fascinating history of urine examination. J. Am. Soc. Cytopathol. 3, 103–107 (2014).
Sharp, V. J., Antes, L. M., Sanders, M. L. & Lockwood, G. M. Urine Tests — A Case-Based Guide to Clinical Evaluation and Application (Springer, 2020).
Decramer, S. et al. Urine in clinical proteomics. Mol. Cell. Proteom. 7, 1850–1862 (2008).
Barratt, J. & Topham, P. Urine proteomics: the present and future of measuring urinary protein components in disease. CMAJ 177, 361–368 (2007).
Afkarian, M. et al. Optimizing a proteomics platform for urine biomarker discovery. Mol. Cell. Proteom. 9, 2195–2204 (2010).
Ipe, D. S., Horton, E. & Ulett, G. C. The basics of bacteriuria: strategies of microbes for persistence in urine. Front. Cell. Infect. Microbiol. 6, 14 (2016).
Thomas-White, K. J. et al. Urinary microbes and postoperative urinary tract infection risk in urogynecologic surgical patients. Int. Urogynecol. J. 29, 1797–1805 (2018).
Brubaker, L. & Wolfe, A. J. The female urinary microbiota, urinary health and common urinary disorders. Ann. Transl. Med. 5, 34 (2017).
Bae, J.-H. & Lee, H.-K. User health information analysis with a urine and feces separable smart toilet system. IEEE Access. 6, 78751–78765 (2018).
Ramlakhan, S. L., Burke, D. P. & Goldman, R. S. Dipstick urinalysis for the emergency department evaluation of urinary tract infections in infants aged less than 2 years. Eur. J. Emerg. Med. 18, 221–224 (2011).
Sinawe, H. & Casadesus, D. Urine Culture (StatPearls Publishing LLC, 2021).
Yarbrough, M. L., Wallace, M. A., Marshall, C., Mathias, E. & Burnham, C.-A. D. Culture of urine specimens by use of chromID CPS Elite medium can expedite Escherichia coli identification and reduce hands-on time in the clinical laboratory. J. Clin. Microbiol. 54, 2767–2773 (2016).
Najeeb, S. et al. Comparison of urine dipstick test with conventional urine culture in diagnosis of urinary tract infection. J. Coll. Physicians Surg. Pak. 25, 108–110 (2015).
Mejuto, P., Luengo, M. & Díaz-Gigante, J. Automated flow cytometry: an alternative to urine culture in a routine clinical microbiology laboratory? Int. J. Microbiol. 2017, 8532736 (2017).
Monsen, T. & Rydén, P. Flow cytometry analysis using sysmex UF-1000i classifies uropathogens based on bacterial, leukocyte, and erythrocyte counts in urine specimens among patients with urinary tract infections. J. Clin. Microbiol. 53, 539–545 (2015).
Broeren, M., Nowacki, R., Halbertsma, F., Arents, N. & Zegers, S. Urine flow cytometry is an adequate screening tool for urinary tract infections in children. Eur. J. Pediatr. 178, 363–368 (2019).
Owens, C. L., VandenBussche, C. J., Burroughs, F. H. & Rosenthal, D. L. A review of reporting systems and terminology for urine cytology. Cancer Cytopathol. 121, 9–14 (2013).
Xing, J. & Reynolds, J. P. Diagnostic advances in urine cytology. Surg. Pathol. Clin. 11, 601–610 (2018).
Vap, L. M. & Shropshire, S. B. Urine cytology: collection, film preparation, and evaluation. Vet. Clin. North Am. Small Anim. Pract. 47, 135–149 (2017).
Becker, G. J., Garigali, G. & Fogazzi, G. B. Advances in urine microscopy. Am. J. Kidney Dis. 67, 954–964 (2016).
Goldani, J. C. et al. Urine microscopy as a biomarker of acute kidney injury following cardiac surgery with cardiopulmonary bypass. Braz. J. Nephrol. 42, 18–23 (2020).
Premasiri, W. R., Clarke, R. H. & Womble, M. E. Urine analysis by laser Raman spectroscopy. Lasers Surg. Med. 28, 330–334 (2001).
Žukovskaja, O. et al. Towards Raman spectroscopy of urine as screening tool. J. Biophotonics 13, e201900143 (2020).
Miller, I. J. et al. Real-time health monitoring through urine metabolomics. NPJ Digit. Med. 2, 1–9 (2019).
Mambatta, A. K. et al. Reliability of dipstick assay in predicting urinary tract infection. J. Fam. Med. Prim. Care 4, 265 (2015).
Shimoni, Z., Glick, J., Hermush, V. & Froom, P. Sensitivity of the dipstick in detecting bacteremic urinary tract infections in elderly hospitalized patients. PLoS One 12, e0187381 (2017).
Dadzie, I. et al. The effectiveness of dipstick for the detection of urinary tract infection. Can. J. Infect. Dis. Med. Microbiol. 2019, 8642628 (2019).
Herman-Saffar, O. et al. Early non-invasive detection of breast cancer using exhaled breath and urine analysis. Comput. Biol. Med. 96, 227–232 (2018).
Xylinas, E. et al. Urine markers for detection and surveillance of bladder cancer. Paper presented at: urologic oncology: seminars and original investigations. Urol. Oncol. 32, 222–229 (2014).
Bax, C. et al. Innovative diagnostic methods for early prostate cancer detection through urine analysis: a review. Cancers 10, 123 (2018).
Perazella, M. A. The urine sediment as a biomarker of kidney disease. Am. J. Kidney Dis. 66, 748–755 (2015).
Bach, S. et al. Detection of colorectal cancer in urine using DNA methylation analysis. Sci. Rep. 11, 1–11 (2021).
Ryan, D., Robards, K., Prenzler, P. D. & Kendall, M. Recent and potential developments in the analysis of urine: a review. Anal. Chim. Acta 684, 17–29 (2011).
Kemperman, R. F. et al. Comparative urine analysis by liquid chromatography− mass spectrometry and multivariate statistics: method development, evaluation, and application to proteinuria. J. Proteome Res. 6, 194–206 (2007).
Simerville, J. A., Maxted, W. C. & Pahira, J. J. Urinalysis: a comprehensive review. Am. Fam. Physician 71, 1153–1162 (2005).
Zamanzad, B. Accuracy of dipstick urinalysis as a screening method for detection of glucose, protein, nitrites and blood. East. Mediterr. Health J. 15, 1323–1328 (2009).
Sarabi, M. R., Ahmadpour, A., Yetisen, A. K. & Tasoglu, S. Finger-actuated microneedle array for sampling body fluids. Appl. Sci. 11, 5329 (2021).
Leipheimer, J. M. et al. First-in-human evaluation of a hand-held automated venipuncture device for rapid venous blood draws. Technology 7, 98–107 (2019).
WHO. WHO best practices for injections and related procedures toolkit. Report No. 9245599256, https://www.who.int/publications/i/item/who-best-practices-for-injections-and-related-procedures-toolkit (2010).
Lapostolle, F. et al. Prospective evaluation of peripheral venous access difficulty in emergency care. Intensive Care Med. 33, 1452–1457 (2007).
Hess, H. A. A biomedical device to improve pediatric vascular access success. Pediatr. Nurs. 36, 259–263 (2010).
Mishra, A., Greaves, R. & Massie, J. The relevance of sweat testing for the diagnosis of cystic fibrosis in the genomic era. Clin. Biochem. Rev. 26, 135 (2005).
McAdams, E. et al. Wearable sensor systems: the challenges. 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society. 3648–3651 (IEEE, 2011).
Gambhir, S. S., Ge, T. J., Vermesh, O. & Spitler, R. Toward achieving precision health. Sci. Transl. Med. 10 (2018).
Gambhir, S. S., Ge, T. J., Vermesh, O., Spitler, R. & Gold, G. E. Continuous health monitoring: an opportunity for precision health. Sci. Transl. Med. 13, eaao3612 (2021).
Centers for Disease Control and Prevention. Chronic kidney disease in the United States, 2021. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021 https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html (CDC, 2021).
Luyckx, V. A., Tonelli, M. & Stanifer, J. W. The global burden of kidney disease and the sustainable development goals. Bull. World Health Organ. 96, 414 (2018).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Centers for Disease Control and Prevention. Chronic Kidney Disease in the United States, 2021. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2021 Chronic Kidney Disease Initiative, https://www.cdc.gov/kidneydisease/basics.html (CDC, 2020).
Park, S.-m et al. A mountable toilet system for personalized health monitoring via the analysis of excreta. Nat. Biomed. Eng. 4, 624–635 (2020).
Mohanty, M. D. & Mohanty, M. N. A cognitive approach for design of smart toilet in healthcare units. In: Mallick P., Balas V., Bhoi A., Zobaa A. (eds) Cognitive Informatics and Soft Computing. Advances in Intelligent Systems and Computing, vol 768 771–780 (Springer, 2019).
Shaikh, F., Shaikh, F., Sayed, K., Mittha, N. & Khan, N. Smart Toilet Based on IoT. In: 2019 3rd International Conference on Computing Methodologies and Communication (ICCMC) 248–250 (IEEE, 2019).
Mohanty, M. D., Pattnaik, D., Parida, M., Mohanty, S. & Mohanty, M. N. Design of intelligent PID controller for smart toilet of CCU/ICU patients in healthcare systems. In: Bhaskar M., Dash S., Das S., Panigrahi B. (eds) International Conference on Intelligent Computing and Applications. Advances in Intelligent Systems and Computing, vol 846. (Springer, 2019).
Ikenaga, T., Shigematsu, T., Kusumoto, A., Yamamoto, K. & Yada, M. Toilet device with health examination system. U.S. Patent 4961431 (1990).
Ikenaga, T., Shigematsu, T., Yada, M., Makita, S. & Kitaura. Toilet with urine constituent measuring device. U.S. Patent 4962550 (1990).
Nakayama, C. et al. Toilet-bowl-mounted urinalysis unit. U.S. Patent 5730149 (1998).
Zakaria, F. et al. Evaluation of a smart toilet in an emergency camp. Int. J. Disaster Risk Reduct. 27, 512–523 (2018).
Choden, P., Seesaard, T., Dorji, U., Sriphrapradang, C. & Kerdcharoen, T. Urine odor detection by electronic nose for smart toilet application. In: 2017 14th International Conference on Electrical Engineering/Electronics, Computer, Telecommunications and Information Technology (ECTI-CON) 190–193 (IEEE, 2017).
Syafaah, L., Azizah, D. F., Sofiani, I. R., Lestandy, M. & Faruq, A. Self-monitoring and detection of diabetes with art toilet based on image processing and K-means technique. In 2020 IEEE International Conference on Automatic Control and Intelligent Systems (I2CACIS) 87–91 (IEEE, 2020).
Huang, J.-J., Yu, S.-I. & Syu, H.-Y. Development of the smart toilet equipment with measurements of physiological parameters. In 2012 9th International Conference on Ubiquitous Intelligence and Computing and 9th International Conference on Autonomic and Trusted Computing 9–16 (IEEE, 2012).
OutSense. Transforming human waste into lifesaving medical insights https://outsensediagnostics.com/ (2020).
Toi Labs. Effortless health monitoring with every flush https://www.toilabs.com/ (2021).
Szondy, D. Nightclub urinal tells patrons when they’ve had one too many. https://newatlas.com/pee-analyzer/28371/ (2013).
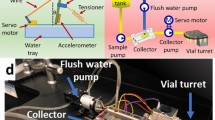
Temirel, M., Yenilmez, B. & Tasoglu, S. Long-term cyclic use of a sample collector for toilet-based urine analysis. Sci. Rep. 11, 2170 (2021).
Oyaert, M. & Delanghe, J. Progress in automated urinalysis. Ann. Lab. Med. 39, 15 (2019).
Jiang, N., Mück, J. E. & Yetisen, A. K. The regulation of wearable medical devices. Trends Biotechnol. 38, 129–133 (2020).
Yu, Z., Jiang, N., Kazarian, S. G., Tasoglu, S. & Yetisen, A. K. Optical sensors for continuous glucose monitoring. Prog. Biomed. Eng. 3, 022004 (2021).
Kim, S. H., Oh, S. A. & Oh, S. J. Voiding diary might serve as a useful tool to understand differences between bladder pain syndrome/interstitial cystitis and overactive bladder. Int. J. Urol. 21, 179–183 (2014).
Nassiff, A. et al. Voiding diary: proposal and assessment of a tool. Int. J. Urol. Nurs. 11, 144–150 (2017).
Smith, G. T. et al. Robust dipstick urinalysis using a low-cost, micro-volume slipping manifold and mobile phone platform. Lab Chip 16, 2069–2078 (2016).
Magnay, J. L., O’Brien, S., Gerlinger, C. & Seitz, C. A systematic review of methods to measure menstrual blood loss. BMC Women’s Health 18, 1–13 (2018).
Mukherjee, M., Naqvi, S. A., Verma, A., Sengupta, D. & Parnami, A. MenstruLoss: sensor for menstrual blood loss monitoring. ACM J. 3, 1–21 (2019).
Marcin, A. Black, brown, bright red, and more: what does each period blood color mean? https://www.healthline.com/health/womens-health/period-blood#_noHeaderPrefixedContent (2019).
American College of Obstetricians and Gynecologists Committee. American College of Obstetricians and Gynecologists Committee on adolescent health care menstruation in girls and adolescents: using the menstrual cycle as a vital sign. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2015/12/menstruation-in-girls-and-adolescents-using-the-menstrual-cycle-as-a-vital-sign?utm_source=redirect&utm_medium=web&utm_campaign=int (2015).
Rose, C., Parker, A., Jefferson, B. & Cartmell, E. The characterization of feces and urine: a review of the literature to inform advanced treatment technology. Crit. Rev. Environ. Sci. Technol. 45, 1827–1879 (2015).
Carabotti, M., Scirocco, A., Maselli, M. A. & Severi, C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 28, 203 (2015).
Cryan, J. F. et al. The microbiota-gut-brain axis. Physiol. Rev. 99, 1877–2013 (2019).
Mück, J. E., Ünal, B., Butt, H. & Yetisen, A. K. Market and patent analyses of wearables in medicine. Trends Biotechnol. 37, 563–566 (2019).
Grand View Research. Smart bathroom market size, share & trends analysis report by product (toilet, soap dispenser, faucet, shower), by application (residential, commercial), by region, and segment forecasts, 2020–2027, https://www.grandviewresearch.com/industry-analysis/smart-bathrooms-market (2020).
Sahu, M. L., Atulkar, M. & Ahirwal, M. K. IOT-based smart healthcare system: a review on constituent technologies. J. Circuits Syst. Comput. 30, 2130008 (2021).
Dabbagh, S. R., Rabbi, F., Doğan, Z., Yetisen, A. K. & Tasoglu, S. Machine learning-enabled multiplexed microfluidic sensors. Biomicrofluidics 14, 061506 (2020).
Paramita, S., Bebartta, H. N. D. & Pattanayak, P. IoT based healthcare monitoring system using 5 G communication and machine learning models in Health Informatics: A Computational Perspective in Healthcare. 159–182 (Springer, 2021).
Dumka, A. Smart information technology for universal healthcare in Healthcare Data Analytics and Management 211–226 (Elsevier, 2019).
Cheng, H. T. & Zhuang, W. Bluetooth-enabled in-home patient monitoring system: early detection of Alzheimer’s disease. IEEE Wirel. Commun. 17, 74–79 (2010).
Lavric, A., Petrariu, A. I. & Popa, V. Long range sigfox communication protocol scalability analysis under large-scale, high-density conditions. IEEE Access. 7, 35816–35825 (2019).
Tengshe, R. R. & Sahoo, A. NB-IoT for Healthcare in Principles and Applications of Narrowband Internet of Things (NBIoT) 127–152 (IGI Global, 2021).
Malik, H., Alam, M. M., Le Moullec, Y. & Kuusik, A. NarrowBand-IoT performance analysis for healthcare applications. Procedia Comput. Sci. 130, 1077–1083 (2018).
Valach, A. & Macko, D. Exploration of the LoRa technology utilization possibilities in healthcare IoT devices. in 2018 16th International Conference on Emerging eLearning Technologies and Applications (ICETA) 623–628 (IEEE, 2018).
Valach, A. & Macko, D. Optimization of LoRa devices communication for applications in healthcare. in 2020 43rd International Conference on Telecommunications and Signal Processing (TSP) 511–514 (IEEE, 2021).
Chang, S.-H., Chiang, R.-D., Wu, S.-J. & Chang, W.-T. A context-aware, interactive M-health system for diabetics. IT Professional 18, 14–22 (2016).
Doukas, C. & Maglogiannis, I. Bringing IoT and cloud computing towards pervasive healthcare. in 2012 Sixth International Conference on Innovative Mobile and Internet Services in Ubiquitous Computing 922–926 (IEEE, 2012).
Shickel, B., Tighe, P. J., Bihorac, A. & Rashidi, P. Deep EHR: a survey of recent advances in deep learning techniques for electronic health record (EHR) analysis. IEEE J. Biomed. Health Inform. 22, 1589–1604 (2017).
Yang, G. et al. A health-IoT platform based on the integration of intelligent packaging, unobtrusive bio-sensor, and intelligent medicine box. IEEE Trans. Ind. Inform. 10, 2180–2191 (2014).
Sulmasy, L. S., López, A. M. & Horwitch, C. A. Ethical implications of the electronic health record: in the service of the patient. J. Gen. Intern. Med. 32, 935–939 (2017).
Wang, Y., Zhang, A., Zhang, P. & Wang, H. Cloud-assisted EHR sharing with security and privacy preservation via consortium blockchain. IEEE Access. 7, 136704–136719 (2019).
Esposito, C., De Santis, A., Tortora, G., Chang, H. & Choo, K.-K. R. Blockchain: a panacea for healthcare cloud-based data security and privacy? IEEE Cloud Comput. 5, 31–37 (2018).
Xiao, Z. & Xiao, Y. Security and privacy in cloud computing. IEEE Commun. Surv. Tutor. 15, 843–859 (2012).
Karthiban, K. & Smys, S. Privacy preserving approaches in cloud computing. in 2018 2nd International Conference on Inventive Systems and Control (ICISC) 462–467 (IEEE, 2018).
Schönberger, D. Artificial intelligence in healthcare: a critical analysis of the legal and ethical implications. Int. J. Law Inf. Technol. 27, 171–203 (2019).
Singh, N. & Singh, A. K. Data privacy protection mechanisms in cloud. Data Sci. Eng. 3, 24–39 (2018).
Azaria, A., Ekblaw, A., Vieira, T. & Lippman, A. MedRec: Using Blockchain for Medical Data Access and Permission Management in 2016 2nd International Conference on Open and Big Data (OBD) 25–30 (IEEE, 2016).
Zhang, J., Xue, N. & Huang, X. A secure system for pervasive social network-based healthcare. IEEE Access 4, 9239–9250 (2016).
Maher, N. A. et al. Passive data collection and use in healthcare: a systematic review of ethical issues. Int. J. Med. Inform. 129, 242–247 (2019).
Shah, P., Thornton, I., Turrin, D. & Hipskind, J. E. Informed Consent, https://www.ncbi.nlm.nih.gov/books/NBK430827/ (2020).
Zakaria, F. et al. User acceptance of the eSOS® Smart Toilet in a temporary settlement in the Philippines. Water Pract. Technol. 12, 832–847 (2017).
Bettiga, D., Lamberti, L. & Lettieri, E. Individuals’ adoption of smart technologies for preventive health care: a structural equation modeling approach. Health Care Manag. Sci. 23, 1–12 (2019).
Marangunić, N. & Granić, A. Technology acceptance model: a literature review from 1986 to 2013. Univers. Access. Inf. Soc. 14, 81–95 (2015).
Lanter, D. & Essinger, R. User-Centered Design. in International Encyclopedia of Geography: People, the Earth, Environment and Technology: People, the Earth, Environment and Technology 1–4 (Wiley-Blackwell, 2016).
Dabbagh, S. R. et al. Increasing the packing density of assays in paper-based microfluidic devices. Biomicrofluidics 15, 011502 (2021).
Lei, R., Huo, R. & Mohan, C. Current and emerging trends in point-of-care urinalysis tests. Expert. Rev. Mol. Diagn. 20, 69–84 (2020).
Mahoney, E., Kun, J., Smieja, M. & Fang, Q. Point-of-care urinalysis with emerging sensing and imaging technologies. J. Electrochem. Soc. 167, 037518 (2019).
Lin, C.-C., Tseng, C.-C., Chuang, T.-K., Lee, D.-S. & Lee, G.-B. Urine analysis in microfluidic devices. Analyst 136, 2669–2688 (2011).
Yang, Y., Chen, Y., Tang, H., Zong, N. & Jiang, X. Microfluidics for biomedical analysis. Small Methods 4, 1900451 (2020).
Ozdalgic, B. et al. Microfluidics for microalgal biotechnology. Biotechnol. Bioeng. 118, 1716–1734 (2021).
Pandey, C. M. et al. Microfluidics based point-of-care diagnostics. Biotechnol. J. 13, 1700047 (2018).
Cui, P. & Wang, S. Application of microfluidic chip technology in pharmaceutical analysis: a review. J. Pharm. Anal. 9, 238–247 (2019).
Zhu, H., Fohlerová, Z., Pekárek, J., Basova, E. & Neužil, P. Recent advances in lab-on-a-chip technologies for viral diagnosis. Biosens. Bioelectron. 153, 112041 (2020).
Bhatia, S. N. & Ingber, D. E. Microfluidic organs-on-chips. Nat. Biotechnol. 32, 760–772 (2014).
Tian, C., Tu, Q., Liu, W. & Wang, J. Recent advances in microfluidic technologies for organ-on-a-chip. TrAC Trends Anal. Chem. 117, 146–156 (2019).
Ustun, M., Rahmani Dabbagh, S., Ilci, I. S., Bagci-Onder, T. & Tasoglu, S. Glioma-on-a-chip models. Micromachines 12, 490 (2021).
Wu, Q. et al. Organ-on-a-chip: recent breakthroughs and future prospects. Biomed. Eng. Online 19, 9 (2020).
Sununta, S., Rattanarat, P., Chailapakul, O. & Praphairaksit, N. Microfluidic paper-based analytical devices for determination of creatinine in urine samples. Anal. Sci. 34, 109–113 (2018).
Berthier, J., Brakke, K., Gosselin, D., Berthier, E. & Navarro, F. Thread-based microfluidics: flow patterns in homogeneous and heterogeneous microfiber bundles. Med. Eng. Phys. 48, 55–61 (2017).
Nilghaz, A. et al. Flexible microfluidic cloth-based analytical devices using a low-cost wax patterning technique. Lab Chip 12, 209–218 (2012).
Guan, W., Liu, M. & Zhang, C. Electrochemiluminescence detection in microfluidic cloth-based analytical devices. Biosens. Bioelectron. 75, 247–253 (2016).
Temirel, M., Dabbagh, S. R. & Tasoglu, S. Hemp-based microfluidics. Micromachines 12, 182 (2021).
Vrijburg, K. & Hernández-Peña, P. Global spending on health: weathering the storm 2020 (World Health Organization, 2020).
Ward, B. W., Clarke, T. C., Nugent, C. N. & Schiller, J. S. Early release of selected estimates based on data from the 2015 National Health Interview Survey. Vol. 46 (National Center for Health Statistics, 2016).
Acknowledgements
S.T. acknowledges Alexander von Humboldt Research Fellowship for Experienced Researchers, Marie Skłodowska-Curie Individual Fellowship (101003361), and Royal Academy Newton-Katip Çelebi Transforming Systems Through Partnership award (120N019) for financial support of this research. We acknowledge Prof. Gary Curhan for giving feedback on this manuscript.
Author information
Authors and Affiliations
Contributions
S.T. researched data for the article, decided on the content, wrote the manuscript and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
S.T. is a co-founder of ZetaMatrix, Inc., focusing on novel bioinks for 3D bioprinting technologies.
Additional information
Peer review information
Nature Reviews Urology thanks Teerakiat Kerdcharoen and other anonymous peer reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tasoglu, S. Toilet-based continuous health monitoring using urine. Nat Rev Urol 19, 219–230 (2022). https://doi.org/10.1038/s41585-021-00558-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-021-00558-x
This article is cited by
-
The transition from genomics to phenomics in personalized population health
Nature Reviews Genetics (2024)
-
Artificial urinary biomarker probes for diagnosis
Nature Reviews Bioengineering (2024)
-
Swin-LBP: a competitive feature engineering model for urine sediment classification
Neural Computing and Applications (2023)
-
3D-printed microrobots from design to translation
Nature Communications (2022)