Abstract
Sperm selection in the female reproductive tract (FRT) is sophisticated. Only about 1,000 sperm out of millions in an ejaculate reach the fallopian tube and thus have a chance of fertilizing an oocyte. In assisted reproduction techniques, sperm are usually selected using their density or motility, characteristics that do not reflect their fertilization competence and, therefore, might result in failure to fertilize the oocyte. Although sperm processing in in vitro fertilization (IVF) and intrauterine insemination (IUI) bypasses many of the selection processes in the FRT, selection by the cumulus mass and the zona pellucida remain intact. By contrast, the direct injection of a sperm into an oocyte in intracytoplasmic sperm injection (ICSI) bypasses all natural selection barriers and, therefore, increases the risk of transferring paternal defects such as fragmented DNA and genomic abnormalities in sperm to the resulting child. Research into surrogate markers of fertilization potential and into simulating the natural sperm selection processes has progressed. However, methods of sperm isolation — such as hyaluronic acid-based selection and microfluidic isolation based on sperm tactic responses — use only one or two parameters and are not comparable with the multistep sperm selection processes naturally occurring within the FRT. Fertilization-competent sperm require a panel of molecules, including zona pellucida-binding proteins and ion channel proteins, that enable them to progress through the FRT to achieve fertilization. The optimal artificial sperm selection method will, therefore, probably need to use a multiparameter tool that incorporates the molecular signature of sperm with high fertilization potential, and their responses to external cues, within a microfluidic system that can replicate the physiological processes of the FRT in vitro.
Key points
-
Conventional sperm selection methods use surrogate markers that do not reflect the fertilization competence of the selected sperm and might, therefore, result in fertilization failure.
-
Current assisted reproductive techniques (ARTs) bypass many of the natural sperm selection processes in the female reproductive tract (FRT). In particular, intracytoplasmic sperm injection (ICSI) bypasses all the selection processes and thus has increased risk of transferring fragmented DNA and genomic defects in sperm to the resulting child.
-
Multiple mechanisms to select the most fertilization-competent sperm have evolved within the FRT.
-
Sperm need to have a panel of molecules that enable appropriate interactions within the FRT and the cumulus–oocyte complex at the fertilization site for selection.
-
Sperm selection methods based on a single sperm characteristic or the simulation of one selection event in the reproductive tract are unlikely to be sufficient to isolate the most fertilization-competent sperm.
-
A microfluidic system replicating the FRT using multiple selection mechanisms will probably be the optimal tool for selecting the most fertilization-competent sperm for an ART.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Croxatto, H. B. Physiology of gamete and embryo transport through the fallopian tube. Reprod. Biomed. Online 4, 160–169 (2002).
Sakkas, D., Ramalingam, M., Garrido, N. & Barratt, C. L. Sperm selection in natural conception: what can we learn from Mother Nature to improve assisted reproduction outcomes? Hum. Reprod. Update 21, 711–726 (2015).
Agarwal, A., Mulgund, A., Hamada, A. & Chyatte, M. R. A unique view on male infertility around the globe. Reprod. Biol. Endocrinol. 13, 37 (2015).
Buckett, W. & Sierra, S. The management of unexplained infertility: an evidence-based guideline from the Canadian Fertility and Andrology Society. Reprod. Biomed. Online 39, 633–640 (2019).
Bosch, E. et al. ALWAYS ICSI? A SWOT analysis. J. Assist. Reprod. Genet. 37, 2081–2092 (2020).
Johnson, L. N., Sasson, I. E., Sammel, M. D. & Dokras, A. Does intracytoplasmic sperm injection improve the fertilization rate and decrease the total fertilization failure rate in couples with well-defined unexplained infertility? A systematic review and meta-analysis. Fertil. Steril. 100, 704–711 (2013).
Silber, S. J. et al. Conventional in-vitro fertilization versus intracytoplasmic sperm injection for patients requiring microsurgical sperm aspiration. Hum. Reprod. 9, 1705–1709 (1994).
Mazzilli, R. et al. Severe male factor in in vitro fertilization: definition, prevalence, and treatment. Asian J. Androl. https://doi.org/10.4103/aja.aja_53_21 (2021).
Pereira, N., O’Neill, C., Lu, V., Rosenwaks, Z. & Palermo, G. D. The safety of intracytoplasmic sperm injection and long-term outcomes. Reproduction 154, F61–F70 (2017).
Grunewald, S. & Paasch, U. Sperm selection for ICSI using annexin V. Methods Mol. Biol. 927, 257–262 (2013).
Simon, L., Ge, S. Q. & Carrell, D. T. Sperm selection based on electrostatic charge. Methods Mol. Biol. 927, 269–278 (2013).
Albertini, D. F. et al. IVF, from the past to the future: the inheritance of the Capri Workshop Group. Hum. Reprod. Open. 2020, hoaa040 (2020).
World Health Organization. WHO laboratory manual for the examination and processing of human semen 6th edn (WHO, 2010).
Zini, A., Finelli, A., Phang, D. & Jarvi, K. Influence of semen processing technique on human sperm DNA integrity. Urology 56, 1081–1084 (2000).
Younglai, E. V., Holt, D., Brown, P., Jurisicova, A. & Casper, R. F. Sperm swim-up techniques and DNA fragmentation. Hum. Reprod. 16, 1950–1953 (2001).
Borges, E. Jr. et al. Intracytoplasmic morphologically selected sperm injection outcomes: the role of sperm preparation techniques. J. Assist. Reprod. Genet. 30, 849–854 (2013).
Gupta, S., Sekhon, L., Kim, Y. & Agarwal, A. The role of oxidative stress and antioxidants in assisted reproduction. Curr. Womens Health Rev. 6, 227–238 (2010).
Tomlinson, M. J. et al. Interrelationships between seminal parameters and sperm nuclear DNA damage before and after density gradient centrifugation: implications for assisted conception. Hum. Reprod. 16, 2160–2165 (2001).
Morrell, J. et al. Reduced senescence and retained nuclear DNA integrity in human spermatozoa prepared by density gradient centrifugation. J. Assist. Reprod. Genet. 21, 217–222 (2004).
Karamahmutoglu, H. et al. The gradient technique improves success rates in intrauterine insemination cycles of unexplained subfertile couples when compared to swim up technique; a prospective randomized study. J. Assist. Reprod. Genet. 31, 1139–1145 (2014).
Twigg, J. et al. Iatrogenic DNA damage induced in human spermatozoa during sperm preparation: protective significance of seminal plasma. Mol. Hum. Reprod. 4, 439–445 (1998).
Marzano, G. et al. Centrifugation force and time alter casa parameters and oxidative status of cryopreserved stallion sperm. Biology 9, 22 (2020).
Henkel, R. R. & Schill, W. B. Sperm preparation for ART. Reprod. Biol. Endocrinol. 1, 108 (2003).
Boomsma, C. M., Heineman, M. J., Cohlen, B. J. & Farquhar, C. Semen preparation techniques for intrauterine insemination. Cochrane Database Syst. Rev. 17, 4 (2007).
Berntsen, S. et al. The health of children conceived by ART: ‘the chicken or the egg?’ Hum. Reprod. Update 25, 137–158 (2019).
Pinborg, A., Henningsen, A. K., Malchau, S. S. & Loft, A. Congenital anomalies after assisted reproductive technology. Fertil. Steril. 99, 327–332 (2013).
Wang, J. X., Norman, R. J. & Kristiansson, P. The effect of various infertility treatments on the risk of preterm birth. Hum. Reprod. 17, 945–949 (2002).
Pinborg, A. et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum. Reprod. Update 19, 87–104 (2013).
Henningsen, A. K. et al. Perinatal outcome of singleton siblings born after assisted reproductive technology and spontaneous conception: Danish national sibling-cohort study. Fertil. Steril. 95, 959–963 (2011).
Esteves, S. C., Roque, M., Bedoschi, G., Haahr, T. & Humaidan, P. Intracytoplasmic sperm injection for male infertility and consequences for offspring. Nat. Rev. Urol. 15, 535–562 (2018).
Kissin, D. M. et al. Association of assisted reproductive technology (ART) treatment and parental infertility diagnosis with autism in ART-conceived children. Hum. Reprod. 30, 454–465 (2015).
Boulet, S. L. et al. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA 313, 255–263 (2015).
Levron, J. et al. Sperm chromosome abnormalities in men with severe male factor infertility who are undergoing in vitro fertilization with intracytoplasmic sperm injection. Fertil. Steril. 76, 479–484 (2001).
Kobayashi, H. et al. Aberrant DNA methylation of imprinted loci in sperm from oligospermic patients. Hum. Mol. Genet. 16, 2542–2551 (2007).
Kobayashi, H. et al. DNA methylation errors at imprinted loci after assisted conception originate in the parental sperm. Eur. J. Hum. Genet. 17, 1582–1591 (2009).
Garrett, C., Liu, D. Y. & Baker, H. W. Selectivity of the human sperm–zona pellucida binding process to sperm head morphometry. Fertil. Steril. 67, 362–371 (1997).
Rezaei, M., Nikkhoo, B., Moradveisi, B. & Allahveisi, A. Effect of sperm selection methods on ICSI outcomes in patients with oligoteratzoospermia. Am. J. Clin. Exp. Urol. 9, 170–176 (2021).
Liu, D. Y., Garrett, C. & Baker, H. W. Low proportions of sperm can bind to the zona pellucida of human oocytes. Hum. Reprod. 18, 2382–2389 (2003).
Rodrigo, L. et al. Impact of different patterns of sperm chromosomal abnormalities on the chromosomal constitution of preimplantation embryos. Fertil. Steril. 94, 1380–1386 (2010).
Palermo, G., Joris, H., Devroey, P. & Van Steirteghem, A. C. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 340, 17–18 (1992).
Loutradi, K. E. et al. The effects of sperm quality on embryo development after intracytoplasmic sperm injection. J. Assist. Reprod. Genet. 23, 69–74 (2006).
Hotaling, J. M., Smith, J. F., Rosen, M., Muller, C. H. & Walsh, T. J. The relationship between isolated teratozoospermia and clinical pregnancy after in vitro fertilization with or without intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil. Steril. 95, 1141–1145 (2011).
van den Hoven, L., Hendriks, J. C., Verbeet, J. G., Westphal, J. R. & Wetzels, A. M. Status of sperm morphology assessment: an evaluation of methodology and clinical value. Fertil. Steril. 103, 53–58 (2015).
Lee, S.-H. et al. Intracytoplasmic sperm injection may lead to vertical transmission, expansion, and de novo occurrence of Y-chromosome microdeletions in male fetuses. Fertil. Steril. 85, 1512–1515 (2006).
Sakkas, D. et al. Sperm chromatin anomalies can influence decondensation after intracytoplasmic sperm injection. Hum. Reprod. 11, 837–843 (1996).
Bonduelle, M. Prenatal testing in ICSI pregnancies: incidence of chromosomal anomalies in 1586 karyotypes and relation to sperm parameters. Hum. Reprod. 17, 2600–2614 (2002).
Evans, E. P. P. et al. Male subfertility and oxidative stress. Redox Biol. 46, 102071 (2021).
Aitken, R. J. & Baker, M. A. The role of genetics and oxidative stress in the etiology of male infertility — a unifying hypothesis? Front. Endocrinol. 11, 581838 (2020).
Raad, G. et al. Differential impact of four sperm preparation techniques on sperm motility, morphology, DNA fragmentation, acrosome status, oxidative stress, and mitochondrial activity: a prospective study. Andrology 9, 1549–1559 (2021).
Tesarik, J. Late, but not early, paternal effect on human embryo development is related to sperm DNA fragmentation. Hum. Reprod. 19, 611–615 (2004).
Zhao, J., Zhang, Q., Wang, Y. & Li, Y. Whether sperm deoxyribonucleic acid fragmentation has an effect on pregnancy and miscarriage after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil. Steril. 102, 998–1005.e8 (2014).
Larson-Cook, K. L. et al. Relationship between the outcomes of assisted reproductive techniques and sperm DNA fragmentation as measured by the sperm chromatin structure assay. Fertil. Steril. 80, 895–902 (2003).
Khambata, K. et al. DNA methylation defects in spermatozoa of male partners from couples experiencing recurrent pregnancy loss. Hum. Reprod. 36, 48–60 (2021).
Chen, Q., Zhao, J. Y., Xue, X. & Zhu, G. X. The association between sperm DNA fragmentation and reproductive outcomes following intrauterine insemination, a meta analysis. Reprod. Toxicol. 86, 50–55 (2019).
Fernández-Gonzalez, R. et al. Long-term effects of mouse intracytoplasmic sperm injection with DNA-fragmented sperm on health and behavior of adult offspring. Biol. Reprod. 78, 761–772 (2008).
Björndahl, L. & Kvist, U. Sequence of ejaculation affects the spermatozoon as a carrier and its message. Reprod. Biomed. Online 7, 440–448 (2003).
Björndahl, L. & Kvist, U. Influence of seminal vesicular fluid on the zinc content of human sperm chromatin. Int. J. Androl. 13, 232–237 (1990).
Lilja, H., Oldbring, J., Rannevik, G. & Laurell, C. B. Seminal vesicle-secreted proteins and their reactions during gelation and liquefaction of human semen. J. Clin. Invest. 80, 281–285 (1987).
Sakaguchi, D. et al. Human semenogelin 1 promotes sperm survival in the mouse female reproductive tract. Int. J. Mol. Sci. 21, 3961 (2020).
Katz, D. F., Slade, D. A. & Nakajima, S. T. Analysis of pre-ovulatory changes in cervical mucus hydration and sperm penetrability. Adv. Contracept. 13, 143–151 (1997).
Muytjens, C. M., Vasiliou, S. K., Oikonomopoulou, K., Prassas, I. & Diamandis, E. P. Putative functions of tissue kallikrein-related peptidases in vaginal fluid. Nat. Rev. Urol. 13, 596–607 (2016).
Martyn, F., McAuliffe, F. M. & Wingfield, M. The role of the cervix in fertility: is it time for a reappraisal? Hum. Reprod. 29, 2092–2098 (2014).
Eggert-Kruse, W., Köhler, A., Rohr, G. & Runnebaum, B. The pH as an important determinant of sperm–mucus interaction. Fertil. Steril. 59, 617–628 (1993).
Keel, B. A. & Webster, B. W. Correlation of human sperm motility characteristics with an in vitro cervical mucus penetration test. Fertil. Steril. 49, 138–143 (1988).
Khayamabed, R., Tavalaee, M., Taherian, S. S. & Nasr-Esfahani, M. H. Effect of recombinant β-defensin 1 protein on human sperm motility and viability. Andrologia 52, e13455 (2020).
Diao, R. et al. CCR6 is required for ligand-induced CatSper activation in human sperm. Oncotarget 8, 91445–91458 (2017).
Tollner, T. L. et al. A common mutation in the defensin DEFB126 causes impaired sperm function and subfertility. Sci. Transl Med. 3, 92ra65 (2011).
Boroujeni, P. B. et al. The role of DEFB126 variation in male infertility and medically assisted reproduction technique outcome. Reprod. Biomed. Online 39, 649–657 (2019).
Suarez, S. S. Mammalian sperm interactions with the female reproductive tract. Cell Tissue Res. 363, 185–194 (2016).
Kunz, G., Beil, D., Deininger, H., Wildt, L. & Leyendecker, G. The dynamics of rapid sperm transport through the female genital tract: evidence from vaginal sonography of uterine peristalsis and hysterosalpingoscintigraphy. Hum. Reprod. 11, 627–632 (1996).
Krzanowska, H. The passage of abnormal spermatozoa through the uterotubal junction of the mouse. J. Reprod. Fertil. 38, 81–90 (1974).
Scott, M. A., Liu, I. K., Overstreet, J. W. & Enders, A. C. The structural morphology and epithelial association of spermatozoa at the uterotubal junction: a descriptive study of equine spermatozoa in situ using scanning electron microscopy. J. Reprod. Fertil. Suppl. 56, 415–421 (2000).
Shalgi, R., Smith, T. T. & Yanagimachi, R. A quantitative comparison of the passage of capacitated and uncapacitated hamster spermatozoa through the uterotubal junction. Biol. Reprod. 46, 419–424 (1992).
Larasati, T. et al. Tmprss12 is required for sperm motility and uterotubal junction migration in mice. Biol. Reprod. 103, 254–263 (2020).
Ryo, Y. et al. Disruption of ADAM3 impairs the migration of sperm into oviduct in mouse. Biol. Reprod. 81, 142 (2009).
Nakanishi, T. et al. Selective passage through the uterotubal junction of sperm from a mixed population produced by chimeras of calmegin-knockout and wild-type male mice. Biol. Reprod. 71, 959–965 (2004).
Hagaman, J. R. et al. Angiotensin-converting enzyme and male fertility. Proc. Natl Acad. Sci. USA 95, 2552–2557 (1998).
Shen, C. et al. Prss37 is required for male fertility in the mouse. Biol. Reprod. 88, 123 (2013).
Fujihara, Y. et al. Expression of TEX101, regulated by ACE, is essential for the production of fertile mouse spermatozoa. Proc. Natl Acad. Sci. USA 110, 8111–8116 (2013).
Suarez, S. S. & Pacey, A. A. Sperm transport in the female reproductive tract. Hum. Reprod. Update 12, 23–37 (2006).
Li, W. et al. Tex101 is essential for male fertility by affecting sperm migration into the oviduct in mice. J. Mol. Cell Biol. 5, 345–347 (2013).
Liu, J. et al. Low levels of PRSS37 protein in sperm are associated with many cases of unexplained male infertility. Acta Biochim. Biophys. Sin. 48, 1058–1065 (2016).
Li, S. & Winuthayanon, W. Oviduct: roles in fertilization and early embryo development. J. Endocrinol. 232, 1–26 (2017).
Camara Pirez, M., Steele, H., Reese, S. & Kölle, S. Bovine sperm–oviduct interactions are characterized by specific sperm behaviour, ultrastructure and tubal reactions which are impacted by sex sorting. Sci. Rep. 10, 16522 (2020).
Mahé, C. et al. Sperm migration, selection, survival, and fertilizing ability in the mammalian oviduct. Biol. Reprod. 105, 317–331 (2021).
Racey, P. A. The prolonged storage and survival of spermatozoa in Chiroptera. J. Reprod. Fertil. 56, 391–402 (1979).
Baillie, H. S., Pacey, A. A., Warren, M. A., Scudamore, I. W. & Barratt, C. L. Greater numbers of human spermatozoa associate with endosalpingeal cells derived from the isthmus compared with those from the ampulla. Hum. Reprod. 12, 1985–1992 (1997).
Vigil, P., Salgado, A. M. & Cortés, M. E. Ultrastructural interaction between spermatozoon and human oviductal cells in vitro. J. Electron. Microsc. 61, 123–126 (2012).
Ahlgren, M. Sperm transport to and survival in the human fallopian tube. Gynecol. Invest. 6, 206–214 (1975).
Wilcox, A. J., Weinberg, C. R. & Baird, D. D. Timing of sexual intercourse in relation to ovulation. Effects on the probability of conception, survival of the pregnancy, and sex of the baby. N. Engl. J. Med. 333, 1517–1521 (1995).
Williams, M. et al. Sperm numbers and distribution within the human fallopian tube around ovulation. Hum. Reprod. 8, 2019–2026 (1993).
Yeung, W. S., Ng, V. K., Lau, E. Y. & Ho, P. C. Human oviductal cells and their conditioned medium maintain the motility and hyperactivation of human spermatozoa in vitro. Hum. Reprod. 9, 656–660 (1994).
Choudhary, S. et al. Effect of recombinant and native buffalo OVGP1 on sperm functions and in vitro embryo development: a comparative study. J. Anim. Sci. Biotechnol. 8, 69 (2017).
Pacey, A. A., Davies, N., Warren, M. A., Barratt, C. L. & Cooke, I. D. Hyperactivation may assist human spermatozoa to detach from intimate association with the endosalpinx. Hum. Reprod. 10, 2603–2609 (1995).
Gualtieri, R. et al. Bovine oviductal monolayers cultured under three-dimension conditions secrete factors able to release spermatozoa adhering to the tubal reservoir in vitro. Theriogenology 79, 429–435 (2013).
Perez-Cerezales, S., Boryshpolets, S. & Eisenbach, M. Behavioral mechanisms of mammalian sperm guidance. Asian J. Androl. 17, 628–632 (2015).
Tesarík, J., Mendoza Oltras, C. & Testart, J. Effect of the human cumulus oophorus on movement characteristics of human capacitated spermatozoa. J. Reprod. Fertil. 88, 665–675 (1990).
Carrell, D. T., Middleton, R. G., Peterson, C. M., Jones, K. P. & Urry, R. L. Role of the cumulus in the selection of morphologically normal sperm and induction of the acrosome reaction during human in vitro fertilization. Arch. Androl. 31, 133–137 (1993).
Fatehi, A. N., Zeinstra, E. C., Kooij, R. V., Colenbrander, B. & Bevers, M. M. Effect of cumulus cell removal of in vitro matured bovine oocytes prior to in vitro fertilization on subsequent cleavage rate. Theriogenology 57, 1347–1355 (2002).
Mortimer, D., Leslie, E. E., Kelly, R. W. & Templeton, A. A. Morphological selection of human spermatozoa in vivo and in vitro. J. Reprod. Fertil. 64, 391 (1982).
Kruger, T. F. et al. Sperm morphologic features as a prognostic factor in in vitro fertilization. Fertil. Steril. 46, 1118–1123 (1986).
Grow, D. & Oehninger, S. Strict criteria for the evaluation of human sperm morphology and its impact on assisted reproduction. Andrologia 27, 325–333 (1995).
Fesahat, F., Henkel, R. & Agarwal, A. Globozoospermia syndrome: an update. Andrologia 52, e13459 (2020).
De Braekeleer, M., Nguyen, M. H., Morel, F. & Perrin, A. Genetic aspects of monomorphic teratozoospermia: a review. J. Assist. Reprod. Genet. 32, 615–623 (2015).
Bartoov, B. et al. Real-time fine morphology of motile human sperm cells is associated with IVF-ICSI outcome. J. Androl. 23, 1–8 (2002).
Bartoov, B. Selection of spermatozoa with normal nuclei to improve the pregnancy rate with intracytoplasmic sperm injection. N. Engl. J. Med. 345, 1067–1068 (2001).
Setti, A. S., Paes de Almeida Ferreira Braga, D., Iaconelli, A., Aoki, T. & Borges, E. Twelve years of MSOME and IMSI: a review. Reprod. Biomed. Online 27, 338–352 (2013).
Cassuto, N. G. et al. Correlation between DNA defect and sperm-head morphology. Reprod. Biomed. Online 24, 211–218 (2011).
Mangiarini, A. et al. Specific sperm defects are differentially correlated with DNA fragmentation in both normozoospermic and teratozoospermic subjects. Andrology 1, 838–844 (2013).
Hammoud, I. et al. Selection of normal spermatozoa with a vacuole-free head (×6300) improves selection of spermatozoa with intact DNA in patients with high sperm DNA fragmentation rates. Andrologia 45, 163–170 (2013).
McQueen, D. B., Zhang, J. & Robins, J. C. Sperm DNA fragmentation and recurrent pregnancy loss: a systematic review and meta-analysis. Fertil. Steril. 112, 54–60.e53 (2019).
Pocate-Cheriet, K. et al. Predicting the clinical outcome of ICSI by sperm head vacuole examination. Syst. Biol. Reprod. Med. 63, 29–36 (2017).
Zanetti, B. F. et al. Sperm morphological normality under high magnification is correlated to male infertility and predicts embryo development. Andrology 6, 420–427 (2018).
Teixeira, D. M. et al. Regular (ICSI) versus ultra-high magnification (IMSI) sperm selection for assisted reproduction. Cochrane Database Syst. Rev. 2, CD010167 (2020).
De Vos, A., Polyzos, N. P., Verheyen, G. & Tournaye, H. Intracytoplasmic morphologically selected sperm injection (IMSI): a critical and evidence-based review. Basic Clin. Androl. 23, 10 (2013).
Vanderzwalmen, P. et al. Blastocyst development after sperm selection at high magnification is associated with size and number of nuclear vacuoles. Reprod. Biomed. Online 17, 617–627 (2008).
Cassuto, N. G. M. D. et al. A new real-time morphology classification for human spermatozoa: a link for fertilization and improved embryo quality. Fertil. Steril. 92, 1616–1625 (2009).
Perdrix, A. et al. Relationship between conventional sperm parameters and motile sperm organelle morphology examination (MSOME). Int. J. Androl. 35, 491–498 (2012).
Montjean, D., Belloc, S., Benkhalifa, M., Dalleac, A. & Ménézo, Y. Sperm vacuoles are linked to capacitation and acrosomal status. Hum. Reprod. 27, 2927–2932 (2012).
Ebner, T. et al. Easy sperm processing technique allowing exclusive accumulation and later usage of DNA-strandbreak-free spermatozoa. Reprod. Biomed. Online 22, 37–43 (2010).
Seiringer, M. et al. Efficacy of a sperm-selection chamber in terms of morphology, aneuploidy and DNA packaging. Reprod. Biomed. Online 27, 81–88 (2013).
Asghar, W. et al. Selection of functional human sperm with higher DNA integrity and fewer reactive oxygen species. Adv. Healthc. Mater. 3, 1671–1679 (2014).
Quinn, M. M. et al. Microfluidic sorting selects sperm for clinical use with reduced DNA damage compared to density gradient centrifugation with swim-up in split semen samples. Hum. Reprod. 33, 1388–1393 (2018).
Schröter, S., Osterhoff, C., McArdle, W. & Ivell, R. The glycocalyx of the sperm surface. Hum. Reprod. Update 5, 302–313 (1999).
Tecle, E. & Gagneux, P. Sugar-coated sperm: unraveling the functions of the mammalian sperm glycocalyx. Mol. Reprod. Dev. 82, 635–650 (2015).
Chan, P. J., Jacobson, J. D., Corselli, J. U. & Patton, W. C. A simple zeta method for sperm selection based on membrane charge. Fertil. Steril. 85, 481–486 (2006).
Khakpour, S., Sadeghi, E., Tavalaee, M., Bahadorani, M. & Nasr-Esfahani, M. H. Zeta method: a noninvasive method based on membrane charge for selecting spermatozoa expressing high level of phospholipaseCζ. Andrologia 51, e13249 (2019).
Zarei-Kheirabadi, M. et al. Evaluation of ubiquitin and annexin V in sperm population selected based on density gradient centrifugation and zeta potential (DGC-Zeta). J. Assist. Reprod. Genet. 29, 365–371 (2012).
Kheirollahi-Kouhestani, M. et al. Selection of sperm based on combined density gradient and Zeta method may improve ICSI outcome. Hum. Reprod. 24, 2409–2416 (2009).
Karimi, N. et al. DGC/Zeta as a new strategy to improve clinical outcome in male factor infertility patients following intracytoplasmic sperm injection: a randomized, single-blind, clinical trial. Cell J. 22, 55–59 (2020).
Ainsworth, C., Nixon, B. & Aitken, R. J. Development of a novel electrophoretic system for the isolation of human spermatozoa. Hum. Reprod. 20, 2261–2270 (2005).
Simon, L. et al. Optimization of microelectrophoresis to select highly negatively charged sperm. J. Assist. Reprod. Genet. 33, 679–688 (2016).
Fleming, S. D. et al. Prospective controlled trial of an electrophoretic method of sperm preparation for assisted reproduction: comparison with density gradient centrifugation. Hum. Reprod. 23, 2646–2651 (2008).
Sakkas, D., Seli, E., Bizzaro, D., Tarozzi, N. & Manicardi, G. C. Abnormal spermatozoa in the ejaculate: abortive apoptosis and faulty nuclear remodelling during spermatogenesis. Reprod. Biomed. Online 7, 428–432 (2003).
Hichri, R. et al. Apoptotic sperm biomarkers and the correlation between conventional sperm parameters and clinical characteristics. Andrologia 50,12813 (2018).
Oosterhuis, G. J. et al. Measuring apoptosis in human spermatozoa: a biological assay for semen quality? Fertil. Steril. 74, 245–250 (2000).
Said, T. M. et al. Utility of magnetic cell separation as a molecular sperm preparation technique. J. Androl. 29, 134–142 (2008).
Grunewald, S. M. D. et al. Increased sperm chromatin decondensation in selected nonapoptotic spermatozoa of patients with male infertility. Fertil. Steril. 92, 572–577 (2009).
de Vantery Arrighi, C., Lucas, H., Chardonnens, D. & de Agostini, A. Removal of spermatozoa with externalized phosphatidylserine from sperm preparation in human assisted medical procreation: effects on viability, motility and mitochondrial membrane potential. Reprod. Biol. Endocrinol. 7, 1 (2009).
Tavalaee, M., Deemeh, M. R., Arbabian, M. & Nasr-Esfahani, M. H. Density gradient centrifugation before or after magnetic-activated cell sorting: which technique is more useful for clinical sperm selection? J. Assist. Reprod. Genet. 29, 31–38 (2012).
Nadalini, M., Tarozzi, N., Di Santo, M. & Borini, A. Annexin V magnetic-activated cell sorting versus swim-up for the selection of human sperm in ART: is the new approach better then the traditional one? J. Assist. Reprod. Genet. 31, 1045–1051 (2014).
Gil, M., Sar-Shalom, V., Melendez Sivira, Y., Carreras, R. & Checa, M. Sperm selection using magnetic activated cell sorting (MACS) in assisted reproduction: a systematic review and meta-analysis. J. Assist. Reprod. Genet. 30, 479–485 (2013).
Romany, L. P. D. et al. Removal of annexin V-positive sperm cells for intracytoplasmic sperm injection in ovum donation cycles does not improve reproductive outcome: a controlled and randomized trial in unselected males. Fertil. Steril. 102, 1567–1575.e1 (2014).
Agarwal, A., Ikemoto, I. & Loughlin, K. R. Effect of sperm washing on levels of reactive oxygen species in semen. Arch. Androl. 33, 157–162 (1994).
Tang, S., Garrett, C. & Baker, H. W. Comparison of human cervical mucus and artificial sperm penetration media. Hum. Reprod. 14, 2812–2817 (1999).
Ivic, A. et al. Critical evaluation of methylcellulose as an alternative medium in sperm migration tests. Hum. Reprod. 17, 143–149 (2002).
Bianchi, P. G. et al. Human cervical mucus can act in vitro as a selective barrier against spermatozoa carrying fragmented DNA and chromatin structural abnormalities. J. Assist. Reprod. Genet. 21, 97–102 (2004).
Bains, R., Miles, D. M., Carson, R. J. & Adeghe, J. Hyaluronic acid increases motility/intracellular CA2+ concentration in human sperm in vitro. Arch. Androl. 47, 119–125 (2001).
Biljan, M. M. et al. Evaluation of different sperm function tests as screening methods for male fertilization potential — the value of the sperm migration test. Fertil. Steril. 62, 591–598 (1994).
Barbonetti, A. et al. Prevalence of anti-sperm antibodies and relationship of degree of sperm auto-immunization to semen parameters and post-coital test outcome: a retrospective analysis of over 10,000 men. Hum. Reprod. 34, 834–841 (2019).
Pacey, A. A. et al. Andrology: the interaction in vitro of human spermatozoa with epithelial cells from the human uterine (fallopian) tube. Hum. Reprod. 10, 360–366 (1995).
Ellington, J. E. et al. Higher-quality human sperm in a sample selectively attach to oviduct (fallopian tube) epithelial cells in vitro. Fertil. Steril. 71, 924–929 (1999).
Gualtieri, R. & Talevi, R. Selection of highly fertilization-competent bovine spermatozoa through adhesion to the fallopian tube epithelium in vitro. Reproduction 125, 251–258 (2003).
López-Úbeda, R., García-Vázquez, F. A., Gadea, J. & Matás, C. Oviductal epithelial cells selected boar sperm according to their functional characteristics. Asian J. Androl. 19, 396–403 (2017).
Talevi, R. & Gualtieri, R. Molecules involved in sperm-oviduct adhesion and release. Theriogenology 73, 796–801 (2010).
Miller, D. J. Regulation of sperm function by oviduct fluid and the epithelium: insight into the role of glycans. Reprod. Domest. Anim. 50, 31–39 (2015).
Huang, V. W. et al. Sperm fucosyltransferase-5 mediates spermatozoa–oviductal epithelial cell interaction to protect human spermatozoa from oxidative damage. Mol. Hum. Reprod. 21, 516–526 (2015).
Kessler, M. et al. The Notch and Wnt pathways regulate stemness and differentiation in human fallopian tube organoids. Nat. Commun. 6, 8989 (2015).
Ferraz, M. A. M. M., Henning, H. H. W., Stout, T. A. E., Vos, P. L. A. M. & Gadella, B. M. Designing 3-dimensional in vitro oviduct culture systems to study mammalian fertilization and embryo production. Ann. Biomed. Eng. 45, 1731–1744 (2016).
Huh, D., Hamilton, G. A. & Ingber, D. E. From 3D cell culture to organs-on-chips. Trends Cell Biol. 21, 745–754 (2011).
Hong, S. J. et al. Establishment of a capillary-cumulus model to study the selection of sperm for fertilization by the cumulus oophorus. Hum. Reprod. 19, 1562–1569 (2004).
Rijsdijk, M. M. M. S. & Franken, D. R. P. D. Use of the capillary–cumulus oophorus model for evaluating the selection of spermatozoa. Fertil. Steril. 88, 1595–1602 (2007).
Naknam, W. et al. Effect of sperm selection method by cumulus oophorus complexes and conventional sperm preparation method on sperm quality and DNA fragmentation for assisted reproduction techonology. Eur. J. Obstet. Gynecol. Reprod. Biol. 243, 46–50 (2019).
Hong, S.-J. et al. Cumulus cells and their extracellular matrix affect the quality of the spermatozoa penetrating the cumulus mass. Fertil. Steril. 92, 971–978 (2009).
Wang, C. et al. Cumulus oophorus complexes favor physiologic selection of spermatozoa for intracytoplasmic sperm injection. Fertil. Steril. 109, 823–831 (2018).
Akgul, Y., Holt, R., Mummert, M., Word, A. & Mahendroo, M. Dynamic changes in cervical glycosaminoglycan composition during normal pregnancy and preterm birth. Endocrinology 153, 3493–3503 (2012).
Rodriguez-Martinez, H. et al. The ubiquitous hyaluronan: functionally implicated in the oviduct? Theriogenology 86, 182–186 (2016).
Chen, L. et al. Hyaluronic acid synthesis and gap junction endocytosis are necessary for normal expansion of the cumulus mass. Mol. Reprod. Dev. 26, 236–247 (1990).
Bains, R., Adeghe, J. & Carson, R. J. Human sperm cells express CD44. Fertil. Steril. 78, 307–312 (2002).
Saylan, A. & Duman, S. Efficacy of hyaluronic acid in the selection of human spermatozoa with intact DNA by the swim-up method. Cell J. 18, 83–88 (2016).
Yagci, A., Murk, W., Stronk, J. & Huszar, G. Spermatozoa bound to solid state hyaluronic acid show chromatin structure with high DNA chain integrity: an acridine orange fluorescence study. J. Androl. 31, 566–572 (2010).
Huszar, G. et al. Fertility testing and ICSI sperm selection by hyaluronic acid binding: clinical and genetic aspects. Reprod. Biomed. Online 14, 650–663 (2007).
Huszar, G. et al. Hyaluronic acid binding by human sperm indicates cellular maturity, viability, and unreacted acrosomal status. Fertil. Steril. 79, 1616–1624 (2003).
Ye, H., Huang, G. N., Gao, Y. & Liu, D. Y. Relationship between human sperm–hyaluronan binding assay and fertilization rate in conventional in vitro fertilization. Hum. Reprod. 21, 1545–1550 (2006).
Mokánszki, A. et al. Is sperm hyaluronic acid binding ability predictive for clinical success of intracytoplasmic sperm injection: PICSI vs. ICSI? Syst. Biol. Reprod. Med. 60, 348–354 (2014).
Beck-Fruchter, R., Shalev, E. & Weiss, A. Clinical benefit using sperm hyaluronic acid binding technique in ICSI cycles: a systematic review and meta-analysis. Reprod. Biomed. Online 32, 286–298 (2016).
Kirkman-Brown, J. et al. Sperm selection for assisted reproduction by prior hyaluronan binding: the HABSelect RCT. Effic. Mech. Eval. 6, 1 (2019).
Lepine, S. et al. Advanced sperm selection techniques for assisted reproduction. Cochrane Database Syst. Rev. 7, CD010461 (2019).
Overstreet, J. W. & Hembree, W. C. Penetration of the zona pellucida of nonliving human oocytes by human spermatozoa in vitro. Fertil. Steril. 27, 815–831 (1976).
Burkman, L. J. et al. The hemizona assay (HZA): development of a diagnostic test for the binding of human spermatozoa to the human hemizona pellucida to predict fertilization potential. Fertil. Steril. 49, 688–697 (1988).
Oehninger, S., Franken, D. R., Sayed, E., Barroso, G. & Kolm, P. Sperm function assays and their predictive value for fertilization outcome in IVF therapy: a meta-analysis. Hum. Reprod. Update 6, 160–168 (2000).
Arslan, M. et al. Predictive value of the hemizona assay for pregnancy outcome in patients undergoing controlled ovarian hyperstimulation with intrauterine insemination. Fertil. Steril. 85, 1697–1707 (2006).
Gupta, S. K. & Bhandari, B. Acrosome reaction: relevance of zona pellucida glycoproteins. Asian J. Androl. 13, 97–105 (2011).
Inci, F. et al. A novel on-chip method for differential extraction of sperm in forensic cases. Adv. Sci. 5, 1800121 (2018).
Deshmukh, S. et al. A confirmatory test for sperm in sexual assault samples using a microfluidic-integrated cell phone imaging system. Forensic Sci. Int. Genet. 48, 102313 (2020).
Pang, P.-C. et al. Human sperm binding is mediated by the sialyl-Lewis(x) oligosaccharide on the zona pellucida. Science 333, 1761 (2011).
Bastiaan, H. S. et al. Relationship between zona pellucida-induced acrosome reaction, sperm morphology, sperm-zona pellucida binding, and in vitro fertilization. Fertil. Steril. 79, 49–55 (2003).
Liu, D. Y., Liu, M. L., Clarke, G. N. & Baker, H. W. Hyperactivation of capacitated human sperm correlates with the zona pellucida-induced acrosome reaction of zona pellucida-bound sperm. Hum. Reprod. 22, 2632–2638 (2007).
Liu, D. Y. & Baker, H. W. Human sperm bound to the zona pellucida have normal nuclear chromatin as assessed by acridine orange fluorescence. Hum. Reprod. 22, 1597–1602 (2007).
Franken, D. R., Kruger, T. F., Oehninger, S. C., Kaskar, K. & Hodgen, G. D. Sperm binding capacity of human zona pellucida derived from oocytes obtained from different sources. Andrologia 26, 277–281 (1994).
Braga, D. Pd. A. F. et al. Outcome of ICSI using zona pellucida-bound spermatozoa and conventionally selected spermatozoa. Reprod. Biomed. Online 19, 802–807 (2009).
Black, M., Liu, D. Y., Bourne, H. & Baker, H. W. G. Comparison of outcomes of conventional intracytoplasmic sperm injection and intracytoplasmic sperm injection using sperm bound to the zona pellucida of immature oocytes. Fertil. Steril. 93, 672–674 (2010).
Liu, F. et al. Use of zona pellucida-bound sperm for intracytoplasmic sperm injection produces higher embryo quality and implantation than conventional intracytoplasmic sperm injection. Fertil. Steril. 95, 815–818 (2011).
Jin, R. et al. Outcomes of intracytoplasmic sperm injection using the zona pellucida-bound sperm or manually selected sperm. J. Assist. Reprod. Genet. 33, 597–601 (2016).
Casciani, V. et al. Traditional intracytoplasmic sperm injection provides equivalent outcomes compared with human zona pellucida-bound selected sperm injection. Zygote 22, 565–570 (2014).
Liu, D.-Y. Could using the zona pellucida bound sperm for intracytoplasmic sperm injection (ICSI) enhance the outcome of ICSI? Asian J. Androl. 13, 197–198 (2011).
Reid, A. T., Redgrove, K., Aitken, R. J. & Nixon, B. Cellular mechanisms regulating sperm–zona pellucida interaction. Asian J. Androl. 13, 88–96 (2011).
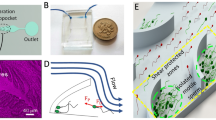
Nosrati, R. et al. Microfluidics for sperm analysis and selection. Nat. Rev. Urol. 14, 707–730 (2017).
Shirota, K. et al. Separation efficiency of a microfluidic sperm sorter to minimize sperm DNA damage. Fertil. Steril. 105, 315–321 (2016).
Miki, K. & Clapham, D. E. Rheotaxis guides mammalian sperm. Curr. Biol. 23, 443–452 (2013).
Seo, D.-b, Agca, Y., Feng, Z. C. & Critser, J. K. Development of sorting, aligning, and orienting motile sperm using microfluidic device operated by hydrostatic pressure. Microfluid. Nanofluidics 3, 561–570 (2007).
Martin, H. et al. Positive rheotaxis extended drop: a one-step procedure to select and recover sperm with mature chromatin for intracytoplasmic sperm injection. J. Assist. Reprod. Genet. 34, 1699–1708 (2017).
Wu, J.-K. et al. High-throughput flowing upstream sperm sorting in a retarding flow field for human semen analysis. Analyst 142, 938–944 (2017).
Zaferani, M., Cheong, S. H. & Abbaspourrad, A. Rheotaxis-based separation of sperm with progressive motility using a microfluidic corral system. Proc. Natl Acad. Sci. USA 115, 8272–8277 (2018).
Zhang, Z. et al. Human sperm rheotaxis: a passive physical process. Sci. Rep. 6, 23553 (2016).
Schiffer, C. et al. Rotational motion and rheotaxis of human sperm do not require functional CatSper channels and transmembrane Ca2+ signaling. EMBO J. 39, e102363 (2020).
Fanaei, H., Keshtgar, S., Bahmanpour, S., Ghannadi, A. & Kazeroni, M. Beneficial effects of α-tocopherol against intracellular calcium overload in human sperm. Reprod. Sci. 18, 978–982 (2011).
Bahat, A. et al. Thermotaxis of mammalian sperm cells: a potential navigation mechanism in the female genital tract. Nat. Med. 9, 149–150 (2003).
Bahat, A., Caplan, S. R. & Eisenbach, M. Thermotaxis of human sperm cells in extraordinarily shallow temperature gradients over a wide range. PLoS ONE 7, e41915 (2012).
De Toni, L. et al. Heat sensing receptor TRPV1 is a mediator of thermotaxis in human spermatozoa. PLoS ONE 11, e0167622 (2016).
Roy, D., Levi, K., Kiss, V., Nevo, R. & Eisenbach, M. Rhodopsin and melanopsin coexist in mammalian sperm cells and activate different signaling pathways for thermotaxis. Sci. Rep. 10, 112–110 (2020).
Boryshpolets, S., Pérez-Cerezales, S. & Eisenbach, M. Behavioral mechanism of human sperm in thermotaxis: a role for hyperactivation. Hum. Reprod. 30, 884–892 (2015).
Pérez-Cerezales, S. et al. Sperm selection by thermotaxis improves ICSI outcome in mice. Sci. Rep. 8, 2902–2902 (2018).
Kaupp, U. B., Kashikar, N. D. & Weyand, I. Mechanisms of sperm chemotaxis. Annu. Rev. Physiol. 70, 93–117 (2008).
Anderson, R. A. Jr, Feathergill, K. A., Rawlins, R. G., Mack, S. R. & Zaneveld, L. J. Atrial natriuretic peptide: a chemoattractant of human spermatozoa by a guanylate cyclase-dependent pathway. Mol. Reprod. Dev. 40, 371–378 (1995).
Oren-Benaroya, R., Orvieto, R., Gakamsky, A., Pinchasov, M. & Eisenbach, M. The sperm chemoattractant secreted from human cumulus cells is progesterone. Hum. Reprod. 23, 2339–2345 (2008).
Xie, L. et al. Integration of sperm motility and chemotaxis screening with a microchannel-based device. Clin. Chem. 56, 1270–1278 (2010).
Sokmensuer, L. K., Palaniappan, S., Toner, M., Toth, T. L. & Wright, D. L. A microfluidic chemotaxis system to select motile and mature sperm. Fertil. Steril. 82, 327–328 (2004).
Li, K. et al. Novel distance-progesterone-combined selection approach improves human sperm quality. J. Transl. Med. 16, 203–203 (2018).
Marc, S. et al. Identification of a testicular odorant receptor mediating human sperm chemotaxis. Science 299, 2054–2058 (2003).
Caballero-Campo, P. et al. A role for the chemokine receptor CCR6 in mammalian sperm motility and chemotaxis. J. Cell Physiol. 229, 68–78 (2014).
Eisenbach, M. Sperm chemotaxis. Rev. Reprod. 4, 56–66 (1999).
Eisenbach, M. & Giojalas, L. C. Sperm guidance in mammals — an unpaved road to the egg. Nat. Rev. Mol. Cell Biol. 7, 276–285 (2006).
Gatica, L. V. et al. Picomolar gradients of progesterone select functional human sperm even in subfertile samples. Mol. Hum. Reprod. 19, 559–569 (2013).
Teves, M. E. et al. Progesterone at the picomolar range is a chemoattractant for mammalian spermatozoa. Fertil. Steril. 86, 745–749 (2006).
Jaiswal, B. S., Tur-Kaspa, I., Dor, J., Mashiach, S. & Eisenbach, M. Human sperm chemotaxis: is progesterone a chemoattractant? Biol. Reprod. 60, 1314–1319 (1999).
Teves, M. E. et al. Molecular mechanism for human sperm chemotaxis mediated by progesterone. PLoS ONE 4, e8211 (2009).
Ko, Y. J., Maeng, J. H., Hwang, S. Y. & Ahn, Y. Design, fabrication, and testing of a microfluidic device for thermotaxis and chemotaxis assays of sperm. SLAS Technol. 23, 507–515 (2018).
Yan, Y., Zhang, B., Fu, Q., Wu, J. & Liu, R. A fully integrated biomimetic microfluidic device for evaluation of sperm response to thermotaxis and chemotaxis. Lab Chip 21, 310–318 (2021).
Suarez, S. S. Interactions of spermatozoa with the female reproductive tract: inspiration for assisted reproduction. Reprod. Fertil. Dev. 19, 103–110 (2007).
Lishko, P. V., Botchkina, I. L. & Kirichok, Y. Progesterone activates the principal Ca2+ channel of human sperm. Nature 471, 387–391 (2011).
Rath, D., Schuberth, H. J., Coy, P. & Taylor, U. Sperm interactions from insemination to fertilization. Reprod. Domest. Anim. 43 (Suppl. 5), 2–11 (2008).
Strünker, T. et al. The CatSper channel mediates progesterone-induced Ca2+ influx in human sperm. Nature 471, 382–386 (2011).
Almiñana, C. et al. The battle of the sexes starts in the oviduct: modulation of oviductal transcriptome by X and Y-bearing spermatozoa. BMC Genomics 15, 293–293 (2014).
Holt, W. V. & Fazeli, A. Do sperm possess a molecular passport? Mechanistic insights into sperm selection in the female reproductive tract. Mol. Hum. Reprod. 21, 491–501 (2015).
Xu, W. et al. Proteomic characteristics of spermatozoa in normozoospermic patients with infertility. J. Proteom. 75, 5426–5436 (2012).
Ayaz, A. et al. Proteomic analysis of sperm proteins in infertile men with high levels of reactive oxygen species. Andrologia 50, e13015 (2018).
Cui, Z., Sharma, R. & Agarwal, A. Proteomic analysis of mature and immature ejaculated spermatozoa from fertile men. Asian J. Androl. 18, 735–746 (2016).
Martínez-Heredia, J., de Mateo, S., Vidal-Taboada, J. M., Ballescà, J. L. & Oliva, R. Identification of proteomic differences in asthenozoospermic sperm samples. Hum. Reprod. 23, 783–791 (2008).
Frapsauce, C. et al. Proteomic identification of target proteins in normal but nonfertilizing sperm. Fertil. Steril. 102, 372–380 (2014).
Zhu, Y. et al. Differential proteomic profiling in human spermatozoa that did or did not result in pregnancy via IVF and AID. Proteom. Clin. Appl. 7, 850–858 (2013).
Agarwal, A., Sharma, R., Samanta, L., Durairajanayagam, D. & Sabanegh, E. Proteomic signatures of infertile men with clinical varicocele and their validation studies reveal mitochondrial dysfunction leading to infertility. Asian J. Androl. 18, 282–291 (2016).
Chan, C.-C., Sun, G.-H., Shui, H.-A. & Wu, G.-J. Differential spermatozoal protein expression profiles in men with varicocele compared to control subjects: upregulation of heat shock proteins 70 and 90 in varicocele. Urology 81, 1379.e1–8 (2013).
Panner Selvam, M. K., Agarwal, A., Pushparaj, P. N., Baskaran, S. & Bendou, H. Sperm proteome analysis and identification of fertility-associated biomarkers in unexplained male infertility. Genes 10, 522 (2019).
Redgrove, K. A. et al. Investigation of the mechanisms by which the molecular chaperone HSPA2 regulates the expression of sperm surface receptors involved in human sperm–oocyte recognition. Mol. Hum. Reprod. 19, 120–135 (2013).
Bromfield, E. G., McLaughlin, E. A., Aitken, R. J. & Nixon, B. Heat shock protein member A2 forms a stable complex with angiotensin converting enzyme and protein disulfide isomerase A6 in human spermatozoa. Mol. Hum. Reprod. 22, 93–109 (2016).
Motiei, M., Tavalaee, M., Rabiei, F., Hajihosseini, R. & Nasr-Esfahani, M. H. Evaluation of HSPA2 in fertile and infertile individuals. Andrologia 45, 66–72 (2013).
Teijeiro, J. M., Roldán, M. L. & Marini, P. E. Annexin A2 and S100A10 in the mammalian oviduct. Cell Tissue Res. 363, 567–577 (2015).
Moore, A., Penfold, L. M., Johnson, J. L., Latchman, D. S. & Moore, H. D. M. Human sperm–egg binding is inhibited by peptides corresponding to core region of an acrosomal serine protease inhibitor. Mol. Reprod. Dev. 34, 280–291 (1993).
Frayne, J. & Hall, L. A re-evaluation of sperm protein 17 (Sp17) indicates a regulatory role in an A-kinase anchoring protein complex, rather than a unique role in sperm–zona pellucida binding. Reproduction 124, 767–774 (2002).
Li, C. Y. et al. CFTR is essential for sperm fertilizing capacity and is correlated with sperm quality in humans. Hum. Reprod. 25, 317–327 (2010).
Reddy, V. R. K., Rajeev, S. K. & Gupta, V. α6β1 integrin is a potential clinical marker for evaluating sperm quality in men. Fertil. Steril. 79, 1590–1596 (2003).
Puga Molina, L. C. et al. Essential role of CFTR in PKA-dependent phosphorylation, alkalinization, and hyperpolarization during human sperm capacitation. J. Cell Physiol. 232, 1404–1414 (2017).
Flesch, F. M. & Gadella, B. M. Dynamics of the mammalian sperm plasma membrane in the process of fertilization. Biochim. Biophys. Acta 1469, 197–235 (2000).
Samanta, L., Swain, N., Ayaz, A., Venugopal, V. & Agarwal, A. Post-translational modifications in sperm proteome: the chemistry of proteome diversifications in the pathophysiology of male factor infertility. Biochim. Biophys. Acta 1860, 1450–1465 (2016).
Donà, G. et al. Human sperm capacitation involves the regulation of the Tyr-phosphorylation level of the anion exchanger 1 (AE1). Int. J. Mol. Sci. 21, 4063 (2020).
Andrews, R. E., Galileo, D. S. & Martin-DeLeon, P. A. Plasma membrane Ca2+-ATPase 4: interaction with constitutive nitric oxide synthases in human sperm and prostasomes which carry Ca2+/CaM-dependent serine kinase. Mol. Hum. Reprod. 21, 832–843 (2015).
Kelly, L. A., Amanda, J. H., Eileen, A. M., Brett, N. & Aitken, R. J. Localization and significance of molecular chaperones, heat shock protein 1, and tumor rejection antigen gp96 in the male reproductive tract and during capacitation and acrosome reaction. Biol. Reprod. 72, 328 (2005).
Nixon, B. et al. Evidence for the involvement of PECAM-1 in a receptor mediated signal-transduction pathway regulating capacitation-associated tyrosine phosphorylation in human spermatozoa. J. Cell Sci. 118, 4865–4877 (2005).
BouÃ, F., Blais, J. & Sullivan, R. Surface localization of P34H an epididymal protein, during maturation, capacitation, and acrosome reaction of human spermatozoa. Biol. Reprod. 54, 1009 (1996).
Focarelli, R. et al. Specific localization in the equatorial region of gp20, a 20 kDa sialylglycoprotein of the capacitated human spermatozoon acquired during epididymal transit which is necessary to penetrate zona-free hamster eggs. Mol. Hum. Reprod. 4, 119–125 (1998).
Giuliani, V. et al. Expression of gp20, a human sperm antigen of epididymal origin, is reduced in spermatozoa from subfertile men. Mol. Reprod. Dev. 69, 235–240 (2004).
Chandonnet, L., Roberts, K. D., Chapdelaine, A. & Manjunath, P. Identification of heparin-binding proteins in bovine seminal plasma. Mol. Reprod. Dev. 26, 313–318 (1990).
Marín-Briggiler, C. I. et al. Expression of epithelial cadherin in the human male reproductive tract and gametes and evidence of its participation in fertilization. Mol. Hum. Reprod. 14, 561–571 (2008).
Chiu, P. C. N. et al. Glycodelin-S in human seminal plasma reduces cholesterol efflux and inhibits capacitation of spermatozoa. J. Biol. Chem. 280, 25580–25589 (2005).
de Lamirande, E. Semenogelin, the main protein of the human semen coagulum, regulates sperm function. Semin. Thromb. Hemost. 33, 60–68 (2007).
Hernández-Silva, G. & Chirinos, M. Proteins from male and female reproductive tracts involved in sperm function regulation. Zygote 27, 5–16 (2019).
Fraser, L. R. Mouse sperm capacitation in vitro involves loss of a surface-associated inhibitory component. J. Reprod. Fertil. 72, 373–384 (1984).
Saez, F., Frenette, G. & Sullivan, R. Epididymosomes and prostasomes: their roles in posttesticular maturation of the sperm cells. J. Androl. 24, 149–154 (2003).
Foot, N. J. & Kumar, S. The role of extracellular vesicles in sperm function and male fertility. Subcell. Biochem. 97, 483–500 (2021).
Rodriguez-Martinez, H., Martinez, E. A., Calvete, J. J., Peña Vega, F. J. & Roca, J. Seminal plasma: relevant for fertility? Int. J. Mol. Sci. 22, 4368 (2021).
Jones, J. L. et al. Galectin-3 is associated with prostasomes in human semen. Glycoconj. J. 27, 227–236 (2010).
Frenette, G., Légaré, C., Saez, F. & Sullivan, R. Macrophage migration inhibitory factor in the human epididymis and semen. Mol. Hum. Reprod. 11, 575–582 (2005).
Rooney, I. A. et al. Physiologic relevance of the membrane attack complex inhibitory protein CD59 in human seminal plasma: CD59 is present on extracellular organelles (prostasomes), binds cell membranes, and inhibits complement-mediated lysis. J. Exp. Med. 177, 1409–1420 (1993).
Mei, S. et al. The role of galectin-3 in spermatozoa–zona pellucida binding and its association with fertilization in vitro. Mol. Hum. Reprod. 25, 458–470 (2019).
Giacomini, E., Makieva, S., Murdica, V., Vago, R. & Viganó, P. Extracellular vesicles as a potential diagnostic tool in assisted reproduction. Curr. Opin. Obstet. Gynecol. 32, 179–184 (2020).
Bathala, P. et al. Oviductal extracellular vesicles (oviductosomes, OVS) are conserved in humans: murine OVS play a pivotal role in sperm capacitation and fertility. Mol. Hum. Reprod. 24, 143–157 (2018).
Okunade, G. W. et al. Targeted ablation of plasma membrane Ca2+-ATPase (PMCA) 1 and 4 indicates a major housekeeping function for PMCA1 and a critical role in hyperactivated sperm motility and male fertility for PMCA4. J. Biol. Chem. 279, 33742–33750 (2004).
Mastelaro de Rezende, M., Ferreira, A. T. & Paredes-Gamero, E. J. Leukemia stem cell immunophenotyping tool for diagnostic, prognosis, and therapeutics. J. Cell Physiol. 235, 4989–4998 (2020).
Sarkar, A. et al. Understanding stem cells and its pivotal role in regenerative medicine. Life Sci. 273, 119270 (2021).
Chemi, F. et al. Early dissemination of circulating tumor cells: biological and clinical insights. Front. Oncol. 11, 672195 (2021).
McDowell, S. et al. Advanced sperm selection techniques for assisted reproduction. Cochrane Database Syst. Rev. 10, CD010461 (2014).
Miller, D. et al. Physiological, hyaluronan-selected intracytoplasmic sperm injection for infertility treatment (HABSelect): a parallel, two-group, randomised trial. Lancet 393, 416–422 (2019).
Quelhas, J. et al. Bovine semen sexing: sperm membrane proteomics as candidates for immunological selection of X- and Y-chromosome-bearing sperm. Vet. Med. Sci. 7, 1633–1641 (2021).
Dias, T. R. et al. Proteomic signatures reveal differences in stress response, antioxidant defense and proteasomal activity in fertile men with high seminal ROS Levels. Int. J. Mol. Sci. 20, 203 (2019).
Dorus, S., Skerget, S. & Karr, T. L. Proteomic discovery of diverse immunity molecules in mammalian spermatozoa. Syst. Biol. Reprod. Med. 58, 218–228 (2012).
Zuccarello, D. et al. How the human spermatozoa sense the oocyte: a new role of SDF1-CXCR4 signalling. Int. J. Androl. 34, e554–e565 (2011).
Rajabi, S. et al. Effect of chemical immobilization of SDF-1α into muscle-derived scaffolds on angiogenesis and muscle progenitor recruitment. J. Tissue Eng. Regen. Med. 12, e438–e450 (2018).
Sutovsky, P., Aarabi, M., Miranda-Vizuete, A. & Oko, R. Negative biomarker based male fertility evaluation: sperm phenotypes associated with molecular-level anomalies. Asian J. Androl. 17, 554–560 (2015).
Sutovsky, P., Terada, Y. & Schatten, G. Ubiquitin-based sperm assay for the diagnosis of male factor infertility. Hum. Reprod. 16, 250–258 (2001).
Ozanon, C., Chouteau, J. & Sutovsky, P. Clinical adaptation of the sperm ubuquitin tag immunoassay (SUTI): relationship of sperm ubiquitylation with sperm quality in gradient-purified semen samples from 93 men from a general infertility clinic population. Hum. Reprod. 20, 2271–2278 (2005).
Odhiambo, J. F. et al. Increased conception rates in beef cattle inseminated with nanopurified bull semen. Biol. Reprod. 91, 97 (2014).
Smith, G. D. & Takayama, S. Application of microfluidic technologies to human assisted reproduction. Mol. Hum. Reprod. 23, 257–268 (2017).
Knowlton, S. M., Sadasivam, M. & Tasoglu, S. Microfluidics for sperm research. Trends Biotechnol. 33, 221–229 (2015).
Hyun, K. A., Lee, T. Y. & Jung, H. I. Negative enrichment of circulating tumor cells using a geometrically activated surface interaction chip. Anal. Chem. 85, 4439–4445 (2013).
Dardikman-Yoffe, G., Mirsky, S. K., Barnea, I. & Shaked, N. T. High-resolution 4-D acquisition of freely swimming human sperm cells without staining. Sci. Adv. 6, 7619 (2020).
McCallum, C. et al. Deep learning-based selection of human sperm with high DNA integrity. Commun. Biol. 2, 250 (2019).
Parmegiani, L. et al. Comparison of two ready-to-use systems designed for sperm–hyaluronic acid binding selection before intracytoplasmic sperm injection: PICSI vs. Sperm Slow: a prospective, randomized trial. Fertil. Steril. 98, 632–637 (2012).
Parmegiani, L. et al. “Physiologic ICSI”: hyaluronic acid (HA) favors selection of spermatozoa without DNA fragmentation and with normal nucleus, resulting in improvement of embryo quality. Fertil. Steril. 93, 598–604 (2010).
Song, W. et al. Functional, UV-curable coating for the capture of circulating tumor cells. Biomater. Sci. 7, 2383–2393 (2019).
Tasoglu, S. et al. Exhaustion of racing sperm in nature-mimicking microfluidic channels during sorting. Small 9, 3374–3384 (2013).
Nosrati, R. et al. Rapid selection of sperm with high DNA integrity. Lab Chip 14, 1142–1150 (2014).
Chinnasamy, T. et al. Guidance and self-sorting of active swimmers: 3D periodic arrays increase persistence length of human sperm selecting for the fittest. Adv. Sci. 5, 1700531 (2018).
Liu, W. et al. Separation of sperm and epithelial cells based on the hydrodynamic effect for forensic analysis. Biomicrofluidics 9, 044127 (2015).
Gode, F. et al. Comparison of microfluid sperm sorting chip and density gradient methods for use in intrauterine insemination cycles. Fertil. Steril. 112, 842–848.e1 (2019).
Berthier, E., Young, E. W. & Beebe, D. Engineers are from PDMS-land, biologists are from Polystyrenia. Lab Chip 12, 1224–1237 (2012).
Raj, M. K. & Chakraborty, S. PDMS microfluidics: a mini review. J. Appl. Polym. Sci. 137, 48958 (2020).
Oseguera-López, I., Ruiz-Díaz, S., Ramos-Ibeas, P. & Pérez-Cerezales, S. Novel techniques of sperm selection for improving IVF and ICSI outcomes. Front. Cell Dev. Biol. 29, 298 (2019).
Björndahl, L. et al. in A Practical Guide to Basic Laboratory Andrology 147–166 (Cambridge Univ. Press, 2010).
Yeh, E. C. et al. Self-powered integrated microfluidic point-of-care low-cost enabling (SIMPLE) chip. Sci. Adv. 3, e1501645 (2017).
Lottero-Leconte, R., Alonso, C. A. I., Castellano, L. & Perez Martinez, S. Mechanisms of the sperm guidance, an essential aid for meeting the oocyte. Transl. Cancer Res. 6 (Suppl. 2), S427–S430 (2017).
Witt, K. D. et al. Hyaluronic acid binding sperm selection for assisted reproduction treatment (HABSelect): study protocol for a multicentre randomised controlled trial. BMJ Open 6, e012609 (2016).
Acknowledgements
The project is supported by the Hong Kong Research Grant Council Grant (17116417); the Hong Kong Health and Medical Research Fund (07182446); the Shenzhen Science and Technology Program (KQTD20190929172749226), the Sanming Project of Medicine in Shenzhen, China (SZSM201612083) and the HKU-SZH Fund for Shenzhen Key Medical Discipline (SZXK2020089).
Author information
Authors and Affiliations
Contributions
E.T.Y.L. and P.C.N.C. researched data for the article. E.T.Y.L., C.-L.L., K.K.W.L., R.H.W.L., E.H.Y.N., W.S.B.Y. and P.C.N.C. made substantial contributions to discussions of content. E.T.Y.L., C.-L.L., E.H.Y.N., W.S.B.Y. and P.C.N.P. wrote the manuscript and all authors reviewed and edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Urology thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leung, E.T.Y., Lee, CL., Tian, X. et al. Simulating nature in sperm selection for assisted reproduction. Nat Rev Urol 19, 16–36 (2022). https://doi.org/10.1038/s41585-021-00530-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-021-00530-9
This article is cited by
-
Sperm Preparation with Microfluidic Sperm Sorting Chip May Improve Intracytoplasmic Sperm Injection Outcomes Compared to Density Gradient Centrifugation
Reproductive Sciences (2024)
-
Basic, translational and clinical studies in reproductive medicine and clinical reproductive sciences
Journal of Translational Medicine (2023)
-
Revolutionizing the female reproductive system research using microfluidic chip platform
Journal of Nanobiotechnology (2023)
-
Sperm quality metrics were improved by a biomimetic microfluidic selection platform compared to swim-up methods
Microsystems & Nanoengineering (2023)
-
A Markov-model simulation of IVF programs for PCOS patients indicates that coupling myo-Inositol with rFSH is cost-effective for the Italian Health System
Scientific Reports (2023)