Abstract
One of the challenges for the surgical management of prostate cancer is the lymphatic spread of metastases. Lymph node metastases vary in size (micrometastases (<2 mm) or macrometastases (>2 mm)), and their interactions with the lymphatic environment differ (whether they are hypoxic or connected to blood flow). Thus, devising a universal imaging system and an image-guided surgical approach that supports the resection of all affected lymph nodes is difficult. Two complementary approaches to identifying affected lymph nodes have been described as alternatives to performing a traditional pelvic lymph node dissection: lymphatic mapping using radioguidance (the most widely applied modality), fluorescence guidance, integrated hybrid radioguidance and fluorescence guidance or magnetic guidance; and surgery guided by radiolabelled prostate-specific membrane antigen. Careful patient selection using preoperative imaging seems to be a crucial aspect in determining whether one of the individual image-guided surgery procedures alone would be optimal or whether a combination would be considered to be the most desirable course of action. The successful implementation and dissemination of both lymph-node-targeted and disease-targeted procedures are very much reliant on ongoing technical developments in the field and their standardization and interpretation. However, when these innovative surgical procedures are fully refined, evaluation of their influence on oncological outcome is imperative.
Key points
-
Technologies for image-guided surgery for the management of lymphatic prostate cancer metastases are in much demand.
-
Lymphatic mapping procedures are the most reliable modalities for identifying micrometastases.
-
To date, approaches targeting prostate-specific membrane antigen seem to yield the most reliable identification of macrometastases, enabling efficient resection.
-
Preoperative imaging is an essential aspect of image-guided surgery as it provides the anatomical context required to guide the urologist to the area of interest, enabling optimal application of intraoperative imaging or tracing modalities.
-
The physical restrictions of the imaging signatures and tracers used to achieve surgical guidance (such as specificity, tissue penetration and spatial resolution) define the way in which imaging modalities are applied in medical care.
-
Combining the ability of lymphatic mapping to identify micrometastases (<2 mm) with tumour-targeted approaches that pinpoint the location of macrometastases (>2 mm) could provide superior identification of tumour-infiltrated lymph nodes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
American Cancer Society. Cancer Facts and Figures 2017. ACS https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html (2017).
Center, M. M. et al. International variation in prostate cancer incidence and mortality rates. Eur. Urol. 61, 1079–1092 (2012).
Hamdy, F. C. et al. 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N. Engl. J. Med. 375, 1415–1424 (2016).
Seisen, T. et al. Efficacy of local treatment in prostate cancer patients with clinically pelvic lymph node-positive disease at initial diagnosis. Eur. Urol. 73, 452–461 (2017).
James, N. D. et al. Abiraterone for prostate cancer not previously treated with hormone therapy. N. Engl. J. Med. 377, 338–351 (2017).
Gundem, G. et al. The evolutionary history of lethal metastatic prostate cancer. Nature 520, 353–357 (2015).
Shou, J., Zhang, Q., Wang, S. & Zhang, D. The prognosis of different distant metastases pattern in prostate cancer: a population based retrospective study. Prostate 78, 491–497 (2018).
Duchesne, G. M. et al. Health-related quality of life for immediate versus delayed androgen-deprivation therapy in patients with asymptomatic, non-curable prostate cancer (TROG 03.06 and VCOG PR 01-03 [TOAD]): a randomised, multicentre, non-blinded, phase 3 trial. Lancet Oncol. 18, 1192–1201 (2017).
Morizane, S. et al. Comparison of the diagnostic efficacy and perioperative outcomes of limited versus extended pelvic lymphadenectomy during robot-assisted radical prostatectomy: a multi-institutional retrospective study in Japan. Int. J. Clin. Oncol. 23, 568–575 (2017).
Touijer, K. A. et al. Survival outcomes of men with lymph node-positive prostate cancer after radical prostatectomy: a comparative analysis of different postoperative management strategies. Eur. Urol. 73, 890–896 (2017).
Fossati, N. et al. The benefits and harms of different extents of lymph node dissection during radical prostatectomy for prostate cancer: a systematic review. Eur. Urol. 72, 84–109 (2017).
Choo, M. S. et al. Extended versus standard pelvic lymph node dissection in radical prostatectomy on oncological and functional outcomes: a systematic review and meta-analysis. Ann. Surg. Oncol. 24, 2047–2054 (2017).
Abdollah, F. et al. More extensive pelvic lymph node dissection improves survival in patients with node-positive prostate cancer. Eur. Urol. 67, 212–219 (2015).
Grivas, N. et al. The impact of adding sentinel node biopsy to extended pelvic lymph node dissection on the biochemical recurrence of prostate cancer patients treated with robot-assisted radical prostatectomy. J. Nucl. Med. 59, 204–209 (2018).
Colicchia, M. et al. Therapeutic value of standard versus extended pelvic lymph node dissection during radical prostatectomy for high-risk prostate cancer. Curr. Urol. Rep. 18, 51 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01812902 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01555086 (2017).
Mottet, N. et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur. Urol. 71, 618–629 (2017).
Cornford, P. et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur. Urol. 71, 630–642 (2017).
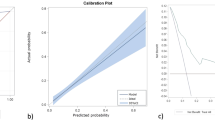
Gandaglia, G. et al. Development and internal validation of a novel model to identify the candidates for extended pelvic lymph node dissection in prostate cancer. Eur. Urol. 72, 632–640 (2017).
Briganti, A. et al. Complications and other surgical outcomes associated with extended pelvic lymphadenectomy in men with localized prostate cancer. Eur. Urol. 50, 1006–1013 (2006).
Briganti, A., Rigatti, P. & Montorsi, F. The importance of the extent of pelvic-lymph-node dissection in the diagnosis of lymph-node metastases in prostate cancer. Lancet Oncol. 9, 915–917 (2008).
Briganti, A. et al. What evidence do we need to support the use of extended pelvic lymph node dissection in prostate cancer? Eur. Urol. 67, 597–598 (2015).
Heck, M. M. et al. Topography of lymph node metastases in prostate cancer patients undergoing radical prostatectomy and extended lymphadenectomy: results of a combined molecular and histopathologic mapping study. Eur. Urol. 66, 222–229 (2014).
Wit, E. M. K. et al. Sentinel node procedure in prostate cancer: a systematic review to assess diagnostic accuracy. Eur. Urol. 71, 596–605 (2017).
Joniau, S. et al. Mapping of pelvic lymph node metastases in prostate cancer. Eur. Urol. 63, 450–458 (2013).
Mattei, A. et al. The template of the primary lymphatic landing sites of the prostate should be revisited: results of a multimodality mapping study. Eur. Urol. 53, 118–125 (2008).
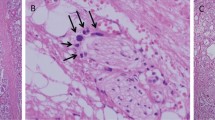
Wawroschek, F. et al. The influence of serial sections, immunohistochemistry, and extension of pelvic lymph node dissection on the lymph node status in clinically localized prostate cancer. Eur. Urol. 43, 132–136; discussion 137 (2003).
Lestingi, J. F. P. et al. Extended versus limited pelvic lymphadenectomy during radical prostatectomy for intermediate- and high-risk prostate cancer: early outcomes from a randomized controlled phase III study [abstract]. J. Clin. Oncol. 35 (Suppl. 15), 5018 (2017).
Harter, P. et al. LION: lymphadenectomy in ovarian neoplasms—a prospective randomized AGO study group led gynecologic cancer intergroup trial. J. Clin. Oncol. 35 (Suppl. 15), 5500 (2017).
Winter, A. et al. [Complications of pelvic lymphadenectomy in clinically localised prostate cancer: different techniques in comparison and dependency on the number of removed lymph nodes]. Aktuelle Urol 42, 179–183 (2011).
Datta, K. et al. Mechanism of lymph node metastasis in prostate cancer. Future Oncol. 6, 823–836 (2010).
Swartz, M. A. Immunomodulatory roles of lymphatic vessels in cancer progression. Cancer Immunol. Res. 2, 701–707 (2014).
Eales, K. L., Hollinshead, K. E. & Tennant, D. A. Hypoxia and metabolic adaptation of cancer cells. Oncogenesis 5, e190 (2016).
Jeong, H. S. et al. Investigation of the lack of angiogenesis in the formation of lymph node metastases. J. Natl Cancer Inst. 107, djv155 (2015).
Fee, H. J. et al. The determination of lymph shed by colloidal gold scanning in patients with malignant melanoma: a preliminary study. Surgery 84, 626–632 (1978).
Van Den Berg, N. S. et al. Hybrid tracers for sentinel node biopsy. Q. J. Nucl. Med. Mol. Imaging 58, 193–206 (2014).
Farnsworth, R. H. et al. Vascular remodeling in cancer. Oncogene 33, 3496–3505 (2014).
Jilg, C. A. et al. Diagnostic accuracy of Ga-68-HBED-CC-PSMA-ligand-PET/CT before salvage lymph node dissection for recurrent prostate cancer. Theranostics 7, 1770–1780 (2017).
Rauscher, I. et al. Value of 68Ga-PSMA HBED-CC PET for the assessment of lymph node metastases in prostate cancer patients with biochemical recurrence: comparison with histopathology after salvage lymphadenectomy. J. Nucl. Med. 57, 1713–1719 (2016).
Fortuin, A. S. et al. Value of PET/CT and MR lymphography in treatment of prostate cancer patients with lymph node metastases. Int. J. Radiat. Oncol. Biol. Phys. 84, 712–718 (2012).
Birkhauser, F. D. et al. Combined ultrasmall superparamagnetic particles of iron oxide-enhanced and diffusion-weighted magnetic resonance imaging facilitates detection of metastases in normal-sized pelvic lymph nodes of patients with bladder and prostate cancer. Eur. Urol. 64, 953–960 (2013).
Heesakkers, R. A. et al. MRI with a lymph-node-specific contrast agent as an alternative to CT scan and lymph-node dissection in patients with prostate cancer: a prospective multicohort study. Lancet Oncol. 9, 850–856 (2008).
Evangelista, L. et al. New clinical indications for 18F/11C-choline, new tracers for positron emission tomography and a promising hybrid device for prostate cancer staging: a systematic review of the literature. Eur. Urol. 70, 161–175 (2016).
Fortuin, A. S. et al. Ultra-small superparamagnetic iron oxides for metastatic lymph node detection: back on the block. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 10, e1471 (2018).
Maurer, T. et al. Current use of PSMA-PET in prostate cancer management. Nat. Rev. Urol. 13, 226–235 (2016).
Ploussard, G. et al. Management of node only recurrence after primary local treatment for prostate cancer: a systematic review of the literature. J. Urol. 194, 983–988 (2015).
Woo, S. et al. The diagnostic performance of MRI for detection of lymph node metastasis in bladder and prostate cancer: an updated systematic review and diagnostic meta-analysis. AJR Am. J. Roentgenol. 210, W95–W109 (2018).
KleinJan, G. H. et al. Optimisation of fluorescence guidance during robot-assisted laparoscopic sentinel node biopsy for prostate cancer. Eur. Urol. 66, 991–998 (2014).
Briganti, A. et al. Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur. Urol. 61, 480–487 (2012).
Godoy, G. et al. Extent of pelvic lymph node dissection and the impact of standard template dissection on nomogram prediction of lymph node involvement. Eur. Urol. 60, 195–201 (2011).
Makarov, D. V. et al. Updated nomogram to predict pathologic stage of prostate cancer given prostate-specific antigen level, clinical stage, and biopsy Gleason score (Partin tables) based on cases from 2000 to 2005. Urology 69, 1095–1101 (2007).
Sormani, M. P. The Will Rogers phenomenon: the effect of different diagnostic criteria. J. Neurol. Sci. 287, S46–S49 (2009).
KleinJan, G. H. et al. The best of both worlds: a hybrid approach for optimal pre- and intraoperative identification of sentinel lymph nodes. Eur. J. Nucl. Med. Mol. Imaging 45, 1915–1925 (2018).
Land, S. R. et al. Patient-reported outcomes in sentinel node-negative adjuvant breast cancer patients receiving sentinel-node biopsy or axillary dissection: National Surgical Adjuvant Breast and Bowel Project phase III protocol B-32. J. Clin. Oncol. 28, 3929–3936 (2010).
Buckle, T. et al. Relationship between intraprostatic tracer deposits and sentinel lymph node mapping in prostate cancer patients. J. Nucl. Med. 53, 1026–1033 (2012).
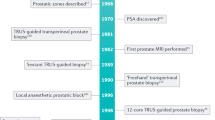
Wawroschek, F. et al. Prostate lymphoscintigraphy and radio-guided surgery for sentinel lymph node identification in prostate cancer. Technique and results of the first 350 cases. Urol. Int. 70, 303–310 (2003).
van Leeuwen, F. W., Hardwick, J. C. & van Erkel, A. R. Luminescence-based imaging approaches in the field of interventional molecular imaging. Radiology 276, 12–29 (2015).
Winter, A., Engels, S. & Wawroschek, F. Sentinel lymph node surgery in prostate cancer using magnetic particles. Curr. Opin. Urol. 28, 184–190 (2018).
Janetschek, G. Radioisotope-guided lymph node dissection for prostate cancer: potential and limitations. Eur. Urol. 53, 16–18; discussion 18–20 (2008).
Kaplan, W. D., Whitmore, W. F. 3rd & Gittes, R. F. Visualization of canine and human prostatic lymph nodes following intraprostatic injection of technetium-99m-antimony sulfide colloid. Invest. Radiol. 15, 34–38 (1980).
Zuckier, L. S. et al. Technetium-99m antimony sulphide colloid lymphoscintigraphy of the prostate by direct transrectal injection. Nucl. Med. Commun. 11, 589–596 (1990).
Brouwer, O. R. et al. Comparing the hybrid fluorescent-radioactive tracer indocyanine green-99mTc-nanocolloid with 99mTc-nanocolloid for sentinel node identification: a validation study using lymphoscintigraphy and SPECT/CT. J. Nucl. Med. 53, 1034–1040 (2012).
Giammarile, F. et al. The EANM and SNMMI practice guideline for lymphoscintigraphy and sentinel node localization in breast cancer. Eur. J. Nucl. Med. Mol. Imaging 40, 1932–1947 (2013).
Wawroschek, F. et al. The sentinel lymph node concept in prostate cancer - first results of gamma probe-guided sentinel lymph node identification. Eur. Urol. 36, 595–600 (1999).
Brenot-Rossi, I. et al. Radioguided sentinel lymph node dissection in patients with localised prostate carcinoma: influence of the dose of radiolabelled colloid to avoid failure of the procedure. Eur. J. Nucl. Med. Mol. Imaging 35, 32–38 (2008).
Holl, G. et al. Validation of sentinel lymph node dissection in prostate cancer: experience in more than 2,000 patients. Eur. J. Nucl. Med. Mol. Imaging 36, 1377–1382 (2009).
Sadeghi, R. et al. Sentinel node mapping in the prostate cancer. Meta-analysis. Nuklearmedizin 50, 107–115 (2011).
Vermeeren, L. et al. Paraaortic sentinel lymph nodes: toward optimal detection and intraoperative localization using SPECT/CT and intraoperative real-time imaging. J. Nucl. Med. 51, 376–382 (2010).
van den Berg, N. S. et al. Sentinel lymph node biopsy for prostate cancer: a hybrid approach. J. Nucl. Med. 54, 493–496 (2013).
Fuerst, B. et al. First robotic SPECT for minimally invasive sentinel lymph node mapping. IEEE Trans. Med. Imaging 35, 830–838 (2016).
Vermeeren, L. et al. Lymphatic drainage from the treated versus untreated prostate: feasibility of sentinel node biopsy in recurrent cancer. Eur. J. Nucl. Med. Mol. Imaging 37, 2021–2026 (2010).
Vermeeren, L. et al. Intraoperative radioguidance with a portable gamma camera: a novel technique for laparoscopic sentinel node localisation in urological malignancies. Eur. J. Nucl. Med. Mol. Imaging 36, 1029–1036 (2009).
Meershoek, P. et al. Robot-assisted laparoscopic surgery using DROP-IN radioguidance: first-in-human translation. Eur. J. Nucl. Med. Mol. Imaging 46, 49–53 (2019).
van Oosterom, M. N. et al. Revolutionizing (robot-assisted) laparoscopic gamma tracing using a drop-in gamma probe technology. Am. J. Nucl. Med. Mol. Imaging 6, 1–17 (2016).
van den Berg, N. S. et al. Multispectral fluorescence imaging during robot-assisted laparoscopic sentinel node biopsy: a first step towards a fluorescence-based anatomic roadmap. Eur. Urol. 72, 110–117 (2017).
Food and Drug Administration. NDA 11-525-S-017: IC-GREEN™: Indocyanine-green for injection. FDA https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/011525s017lbl.pdf (2006).
Jeschke, S. et al. Visualisation of the lymph node pathway in real time by laparoscopic radioisotope- and fluorescence-guided sentinel lymph node dissection in prostate cancer staging. Urology 80, 1080–1086 (2012).
van Leeuwen, A. C. et al. Tracer-cocktail injections for combined pre- and intraoperative multimodal imaging of lymph nodes in a spontaneous mouse prostate tumor model. J. Biomed. Opt. 16, 016004 (2011).
Hruby, S. et al. Fluorescence guided targeted pelvic lymph node dissection for intermediate and high risk prostate cancer. J. Urol. 194, 357–363 (2015).
Chennamsetty, A. et al. Lymph node fluorescence during robot-assisted radical prostatectomy with indocyanine green: prospective dosing analysis. Clin. Genitourin Cancer 15, e529–e534 (2017).
Manny, T. B., Patel, M. & Hemal, A. K. Fluorescence-enhanced robotic radical prostatectomy using real-time lymphangiography and tissue marking with percutaneous injection of unconjugated indocyanine green: the initial clinical experience in 50 patients. Eur. Urol. 65, 1162–1168 (2014).
Morozov, A. O. et al. Near-infrared fluorescence with indocyanine green for diagnostics in urology: initial experience. Urologia 84, 197–202 (2017).
Nguyen, D. P. et al. A specific mapping study using fluorescence sentinel lymph node detection in patients with intermediate- and high-risk prostate cancer undergoing extended pelvic lymph node dissection. Eur. Urol. 70, 734–737 (2016).
Ramirez-Backhaus, M. et al. Indocyanine green guided pelvic lymph node dissection: an efficient technique to classify the lymph node status of patients with prostate cancer who underwent radical prostatectomy. J. Urol. 196, 1429–1435 (2016).
Yuen, K. et al. Intraoperative fluorescence imaging for detection of sentinel lymph nodes and lymphatic vessels during open prostatectomy using indocyanine green. J. Urol. 194, 371–377 (2015).
Buckle, T. et al. A self-assembled multimodal complex for combined pre- and intraoperative imaging of the sentinel lymph node. Nanotechnology 21, 355101 (2010).
KleinJan, G. H. et al. Multimodal hybrid imaging agents for sentinel node mapping as a means to (re)connect nuclear medicine to advances made in robot-assisted surgery. Eur. J. Nucl. Med. Mol. Imaging 43, 1278–1287 (2016).
van der Poel, H. G. et al. Intraoperative laparoscopic fluorescence guidance to the sentinel lymph node in prostate cancer patients: clinical proof of concept of an integrated functional imaging approach using a multimodal tracer. Eur. Urol. 60, 826–833 (2011).
van den Berg, N. S. et al. (Near-infrared) fluorescence-guided surgery under ambient light conditions: a next step to embedment of the technology in clinical routine. Ann. Surg. Oncol. 23, 2586–2595 (2016).
KleinJan, G. H. et al. Hybrid surgical guidance: does hardware integration of γ- and fluorescence imaging modalities make sense? J. Nucl. Med. 58, 646–650 (2017).
van den Berg, N. S. et al. First-in-human evaluation of a hybrid modality that allows combined radio- and (near-infrared) fluorescence tracing during surgery. Eur. J. Nucl. Med. Mol. Imaging 42, 1639–1647 (2015).
Douek, M. et al. Sentinel node biopsy using a magnetic tracer versus standard technique: SentiMAG Multicentre Trial. Ann. Surg. Oncol. 21, 1237–1245 (2014).
Thill, M. et al. The Central-European SentiMag study: sentinel lymph node biopsy with superparamagnetic iron oxide (SPIO) versus radioisotope. Breast 23, 175–179 (2014).
Ahmed, M., de Rosales, R. T. & Douek, M. Preclinical studies of the role of iron oxide magnetic nanoparticles for nonpalpable lesion localization in breast cancer. J. Surg. Res. 185, 27–35 (2013).
Johnson, L., Pinder, S. E. & Douek, M. Deposition of superparamagnetic iron-oxide nanoparticles in axillary sentinel lymph nodes following subcutaneous injection. Histopathology 62, 481–486 (2013).
Sekino, M. et al. Handheld magnetic probe with permanent magnet and Hall sensor for identifying sentinel lymph nodes in breast cancer patients. Sci. Rep. 8, 1195 (2018).
Winter, A., Woenkhaus, J. & Wawroschek, F. A novel method for intraoperative sentinel lymph node detection in prostate cancer patients using superparamagnetic iron oxide nanoparticles and a handheld magnetometer: the initial clinical experience. Ann. Surg. Oncol. 21, 4390–4396 (2014).
Winter, A. et al. Magnetometer guided sentinel lymphadenectomy after intraprostatic injection of superparamagnetic iron oxide nanoparticles in intermediate- and high-risk prostate cancer patients [abstract PD42-01]. J. Urol. 195 (Suppl. 4), e987 (2016).
Heesakkers, R. A. et al. Prostate cancer: detection of lymph node metastases outside the routine surgical area with ferumoxtran-10-enhanced MR imaging. Radiology 251, 408–414 (2009).
Iida, S. et al. In vivo identification of sentinel lymph nodes using MRI and size-controlled and monodispersed magnetite nanoparticles. J. Magn. Reson. Imaging 38, 1346–1355 (2013).
Stark, D. D. et al. Superparamagnetic iron oxide: clinical application as a contrast agent for MR imaging of the liver. Radiology 168, 297–301 (1988).
Pouw, J. J. et al. Pre-operative sentinel lymph node localization in breast cancer with superparamagnetic iron oxide MRI: the SentiMAG Multicentre Trial imaging subprotocol. Br. J. Radiol. 88, 20150634 (2015).
Winter, A. et al. Magnetic resonance sentinel lymph node imaging in prostate cancer using intraprostatic injection of superparamagnetic iron oxide nanoparticles: the first in-human results [abstract 1060]. Eur. Urol. Suppl. 15, e1060 (2016).
Li, R. et al. The use of PET/CT in prostate cancer. Prostate Cancer Prostatic Dis. 21, 4–21 (2017).
Perera, M. et al. Sensitivity, specificity, and predictors of positive 68Ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur. Urol. 70, 926–937 (2016).
Rauscher, I. et al. Efficacy, predictive factors, and prediction nomograms for 68Ga-labeled prostate-specific membrane antigen-ligand positron-emission tomography/computed tomography in early biochemical recurrent prostate cancer after radical prostatectomy. Eur. Urol. 73, 656–661 (2018).
Eiber, M. et al. Prostate-specific membrane antigen ligands for imaging and therapy. J. Nucl. Med. 58 (Suppl. 2), 67S–76S (2017).
Robu, S. et al. Preclinical evaluation and first patient application of 99mTc-PSMA-I&S for SPECT imaging and radioguided surgery in prostate cancer. J. Nucl. Med. 58, 235–242 (2017).
Schottelius, M. et al. [111In]PSMA-I&T: expanding the spectrum of PSMA-I&T applications towards SPECT and radioguided surgery. EJNMMI Res. 5, 68 (2015).
Herrmann, K., Nieweg, O. E. & Povoski, S. P. (eds) Radioguided Surgery: Current Applications and Innovative Directions in Clinical Practice (Springer, 2016).
Rauscher, I. et al. Value of 111In-prostate-specific membrane antigen (PSMA)-radioguided surgery for salvage lymphadenectomy in recurrent prostate cancer: correlation with histopathology and clinical follow-up. BJU Int. 120, 40–47 (2017).
Suardi, N. et al. Long-term outcomes of salvage lymph node dissection for clinically recurrent prostate cancer: results of a single-institution series with a minimum follow-up of 5 years. Eur. Urol. 67, 299–309 (2015).
Maurer, T. R. et al. 99mTechnetium-based prostate-specific membrane antigen-radioguided surgery in recurrent prostate cancer. Eur. Urol. https://doi.org/10.1016/j.eururo.2018.03.013 (2018).
KleinJan, G. H. et al. Hybrid radioguided occult lesion localization (hybrid ROLL) of 18F-FDG-avid lesions using the hybrid tracer indocyanine green-99mTc-nanocolloid. Rev. Esp. Med. Nucl. Imagen Mol. 35, 292–297 (2016).
Boorjian, S. A. et al. Long-term risk of clinical progression after biochemical recurrence following radical prostatectomy: the impact of time from surgery to recurrence. Eur. Urol. 59, 893–899 (2011).
Ost, P. et al. Metastasis-directed therapy of regional and distant recurrences after curative treatment of prostate cancer: a systematic review of the literature. Eur. Urol. 67, 852–863 (2015).
Keskek, M. et al. Re-evaluation of axillary skip metastases in the era of sentinel lymph node biopsy in breast cancer. Surg. Today 36, 1047–1052 (2006).
Perera, M. et al. Pelvic lymph node dissection during radical cystectomy for muscle-invasive bladder cancer. Nat. Rev. Urol. 15, 686–692 (2018).
Acknowledgements
Reviewer information
Nature Reviews Urology thanks B. Brown, A. Green and the other anonymous reviewer(s), for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
F.W.B.v.L., A.W., H.G.v.D.P., M.E., F.W. and T.M. researched data for the article. F.W.B.v.L., A.W., H.G.v.D.P. and T.M. wrote the manuscript. All authors made a substantial contribution to discussions of content and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Leeuwen, F.W.B., Winter, A., van Der Poel, H.G. et al. Technologies for image-guided surgery for managing lymphatic metastases in prostate cancer. Nat Rev Urol 16, 159–171 (2019). https://doi.org/10.1038/s41585-018-0140-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-018-0140-8
This article is cited by
-
Steerable DROP-IN radioguidance during minimal-invasive non-robotic cervical and endometrial sentinel lymph node surgery
European Journal of Nuclear Medicine and Molecular Imaging (2024)
-
First-in-human validation of a DROP-IN β-probe for robotic radioguided surgery: defining optimal signal-to-background discrimination algorithm
European Journal of Nuclear Medicine and Molecular Imaging (2024)
-
Using PSMA imaging for prognostication in localized and advanced prostate cancer
Nature Reviews Urology (2023)
-
A new bimodal approach for sentinel lymph node imaging in prostate cancer using a magnetic and fluorescent hybrid tracer
European Journal of Nuclear Medicine and Molecular Imaging (2023)
-
Robotgeassisteerde PSMA-radiogeleide chirurgie bij recidiverend prostaatkanker met de DROP-IN-gammaprobe
Tijdschrift voor Urologie (2023)