Abstract
Despite improvements in early detection and advances in treatment, patients with prostate cancer continue to die from their disease. Minimal residual disease after primary definitive treatment can lead to relapse and distant metastases, and increasing evidence suggests that circulating tumour cells (CTCs) and bone marrow-derived disseminated tumour cells (BM-DTCs) can offer clinically relevant biological insights into prostate cancer dissemination and metastasis. Using epithelial markers to accurately detect CTCs and BM-DTCs is associated with difficulties, and prostate-specific markers are needed for the detection of these cells using rare cell assays. Putative prostate-specific markers have been identified, and an optimized strategy for staining rare cancer cells from liquid biopsies using these markers is required. The ideal prostate-specific marker will be expressed on every CTC or BM-DTC throughout disease progression (giving high sensitivity) and will not be expressed on non-prostate-cancer cells in the sample (giving high specificity). Some markers might not be specific enough to the prostate to be used as individual markers of prostate cancer cells, whereas others could be truly prostate-specific and would make ideal markers for use in rare cell assays. The goal of future studies is to use sensitive and specific prostate markers to consistently and reliably identify rare cancer cells.
Key points
-
Liquid biopsies, particularly from bone marrow, might enable the detection of recurrent disease before overt lethal metastasis develops.
-
Prostate cancer cells in liquid biopsies, particularly bone marrow, are rare and extremely difficult to identify accurately.
-
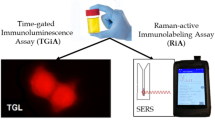
Prostate-specific markers analysed using rare cell immunofluorescence assays might help identify rare prostate cancer cells from liquid biopsies.
-
Expression of putative prostate-specific markers is not always constrained to prostate cells. The sensitivity and specificity of assays of expression of candidate markers for rare cells must be ascertained on an individual basis.
-
Immune cells in the blood and bone marrow are a considerable source of nonspecific staining, so measures must be taken to reduce this background staining.
-
Combinatorial staining of multiple prostate-specific markers will increase accuracy for identifying rare prostate cancer cells in liquid biopsies, and improve understanding of the role of important cells in prostate cancer metastasis and aid clinical application.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2015. CA Cancer J. Clin. 65, 5–29 (2015).
Han, M. et al. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J. Urol. 169, 517–523 (2003).
Mehra, R. et al. Characterization of bone metastases from rapid autopsies of prostate cancer patients. Clin. Cancer Res. 17, 3924–3932 (2011).
Ruppender, N. S., Morrissey, C., Lange, P. H. & Vessella, R. L. Dormancy in solid tumors: implications for prostate cancer. Cancer Metastasis Rev. 32, 501–509 (2013).
Lam, H. M., Vessella, R. L. & Morrissey, C. The role of the microenvironment-dormant prostate disseminated tumor cells in the bone marrow. Drug Discov. Today Technol. 11, 41–47 (2014).
Mishra, A., Shiozawa, Y., Pienta, K. J. & Taichman, R. S. Homing of cancer cells to the bone. Cancer Microenviron. 4, 221–235 (2011).
Nguyen, D. X., Bos, P. D. & Massague, J. Metastasis: from dissemination to organ-specific colonization. Nat. Rev. Cancer 9, 274–284 (2009).
Rowe, S. P. et al. PSMA-based [(18)F]DCFPyL PET/CT is superior to conventional imaging for lesion detection in patients with metastatic prostate cancer. Mol. Imaging Biol. 18, 411–419 (2016).
Mohler, J. L. et al. Prostate cancer, version 1.2016. J. Natl Compr. Canc. Netw. 14, 19–30 (2016).
Li, F. et al. Cell surface Thomsen-Friedenreich proteome profiling of metastatic prostate cancer cells reveals potential link with cancer stem cell-like phenotype. Oncotarget 8, 98598–98608 (2017).
Cheung, K. J. et al. Polyclonal breast cancer metastases arise from collective dissemination of keratin 14-expressing tumor cell clusters. Proc. Natl Acad. Sci. USA 113, E854–E863 (2016).
Pantel, K. & Alix-Panabieres, C. Real-time liquid biopsy in cancer patients: fact or fiction? Cancer Res. 73, 6384–6388 (2013).
Alix-Panabieres, C. & Pantel, K. Challenges in circulating tumour cell research. Nat. Rev. Cancer 14, 623–631 (2014).
Friedlander, T. W. et al. Detection and characterization of invasive circulating tumor cells derived from men with metastatic castration-resistant prostate cancer. Int. J. Cancer 134, 2284–2293 (2014).
Gold, B., Cankovic, M., Furtado, L. V., Meier, F. & Gocke, C. D. Do circulating tumor cells, exosomes, and circulating tumor nucleic acids have clinical utility? A report of the association for molecular pathology. J. Mol. Diagn. 17, 209–224 (2015).
Perakis, S. & Speicher, M. R. Emerging concepts in liquid biopsies. BMC Med. 15, 75 (2017).
Zhang, W. et al. Liquid biopsy for cancer: circulating tumor cells, circulating free DNA or exosomes? Cell Physiol. Biochem. 41, 755–768 (2017).
Di Meo, A., Bartlett, J., Cheng, Y., Pasic, M. D. & Yousef, G. M. Liquid biopsy: a step forward towards precision medicine in urologic malignancies. Mol. Cancer 16, 80 (2017).
de Bono, J. S. et al. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin. Cancer Res. 14, 6302–6309 (2008).
Scher, H. I. et al. Phenotypic heterogeneity of circulating tumor cells informs clinical decisions between AR signaling inhibitors and taxanes in metastatic prostate cancer. Cancer Res. 77, 5687–5698 (2017).
Scher, H. I. et al. Nuclear-specific AR-V7 protein localization is necessary to guide treatment selection in metastatic castration-resistant prostate cancer. Eur. Urol. 71, 874–882 (2017).
Scher, H. I. et al. Circulating tumor cell biomarker panel as an individual-level surrogate for survival in metastatic castration-resistant prostate cancer. J. Clin. Oncol. 33, 1348–1355 (2015).
Scher, H. I. et al. Association of AR-V7 on circulating tumor cells as a treatment-specific biomarker with outcomes and survival in castration-resistant prostate cancer. JAMA Oncol. 2, 1441–1449 (2016).
Kuske, A. et al. Improved detection of circulating tumor cells in non-metastatic high-risk prostate cancer patients. Sci. Rep. 6, 39736 (2016).
Xu, L. et al. The novel association of circulating tumor cells and circulating megakaryocytes with prostate cancer prognosis. Clin. Cancer Res. 23, 5112–5122 (2017).
Amann, R. & Fuchs, B. M. Single-cell identification in microbial communities by improved fluorescence in situ hybridization techniques. Nat. Rev. Microbiol. 6, 339–348 (2008).
Yap, T. A., Lorente, D., Omlin, A., Olmos, D. & de Bono, J. S. Circulating tumor cells: a multifunctional biomarker. Clin. Cancer Res. 20, 2553–2568 (2014).
Campton, D. E. et al. High-recovery visual identification and single-cell retrieval of circulating tumor cells for genomic analysis using a dual-technology platform integrated with automated immunofluorescence staining. BMC Cancer 15, 360 (2015).
Werner, S. L. et al. Analytical validation and capabilities of the epic CTC platform: enrichment-free circulating tumour cell detection and characterization. J. Circ. Biomark. 4, 3 (2015).
Nagrath, S. et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature 450, 1235–1239 (2007).
Valkenburg, K. C. et al. A simple selection-free method for detecting disseminated tumor cells (DTCs) in murine bone marrow. Oncotarget 7, 69794–69803 (2016).
Helo, P. et al. Circulating prostate tumor cells detected by reverse transcription-PCR in men with localized or castration-refractory prostate cancer: concordance with CellSearch assay and association with bone metastases and with survival. Clin. Chem. 55, 765–773 (2009).
O’Hara, S. M. et al. Multigene reverse transcription-PCR profiling of circulating tumor cells in hormone-refractory prostate cancer. Clin. Chem. 50, 826–835 (2004).
Patel, K. et al. The use of real-time reverse transcription-PCR for prostate-specific antigen mRNA to discriminate between blood samples from healthy volunteers and from patients with metastatic prostate cancer. Clin. Cancer Res. 10, 7511–7519 (2004).
Cho, W. J. et al. Gene expression analysis of bone metastasis and circulating tumor cells from metastatic castrate-resistant prostate cancer patients. J. Transl Med. 14, 72 (2016).
Danila, D. C. et al. Clinical validity of detecting circulating tumor cells by AdnaTest assay compared with direct detection of tumor mRNA in stabilized whole blood, as a biomarker predicting overall survival for metastatic castration-resistant prostate cancer patients. Cancer J. 22, 315–320 (2016).
Ma, Y. et al. Droplet digital PCR based androgen receptor variant 7 (AR-V7) detection from prostate cancer patient blood biopsies. Int. J. Mol. Sci. 17, 1264 (2016).
Pixberg, C. F. et al. Analysis of DNA methylation in single circulating tumor cells. Oncogene 36, 3223–3231 (2017).
Yates, D. R. et al. Quantitative RT-PCR analysis of PSA and prostate-specific membrane antigen mRNA to detect circulating tumor cells improves recurrence-free survival nomogram prediction after radical prostatectomy. Prostate 72, 1382–1388 (2012).
van der Toom, E. E., Verdone, J. E., Gorin, M. A. & Pienta, K. J. Technical challenges in the isolation and analysis of circulating tumor cells. Oncotarget 7, 62754–62766 (2016).
Adams, D. L. et al. Circulating giant macrophages as a potential biomarker of solid tumors. Proc. Natl Acad. Sci. USA 111, 3514–3519 (2014).
Eisenwort, G. et al. Identification of TROP2 (TACSTD2), an EpCAM-like molecule, as a specific marker for TGF-beta1-dependent human epidermal Langerhans cells. J. Invest. Dermatol. 131, 2049–2057 (2011).
Shetye, J. D. et al. Spectrum of cytokeratin-positive cells in the bone marrows of colorectal carcinoma patients. Anticancer Res. 24, 2375–2383 (2004).
Lammers, R. et al. Monoclonal antibody 9C4 recognizes epithelial cellular adhesion molecule, a cell surface antigen expressed in early steps of erythropoiesis. Exp. Hematol. 30, 537–545 (2002).
Daskalaki, A. et al. Detection of cytokeratin-19 mRNA-positive cells in the peripheral blood and bone marrow of patients with operable breast cancer. Br. J. Cancer 101, 589–597 (2009).
Dimmler, A. et al. Transcription of cytokeratins 8, 18, and 19 in bone marrow and limited expression of cytokeratins 7 and 20 by carcinoma cells: inherent limitations for RT-PCR in the detection of isolated tumor cells. Lab. Invest. 81, 1351–1361 (2001).
Han, Y. et al. Hepatocyte growth factor increases the invasive potential of PC-3 human prostate cancer cells via an ERK/MAPK and Zeb-1 signaling pathway. Oncol. Lett. 11, 753–759 (2016).
McDaniel, A. S. et al. Phenotypic diversity of circulating tumour cells in patients with metastatic castration-resistant prostate cancer. BJU Int. 120, E30–E44 (2016).
Miyamoto, D. T. et al. Androgen receptor signaling in circulating tumor cells as a marker of hormonally responsive prostate cancer. Cancer Discov. 2, 995–1003 (2012).
Mulholland, D. J. et al. Pten loss and RAS/MAPK activation cooperate to promote EMT and metastasis initiated from prostate cancer stem/progenitor cells. Cancer Res. 72, 1878–1889 (2012).
Palapattu, G. S. et al. Selective expression of CD44, a putative prostate cancer stem cell marker, in neuroendocrine tumor cells of human prostate cancer. Prostate 69, 787–798 (2009).
Smith, B. N. & Bhowmick, N. A. Role of EMT in metastasis and therapy resistance. J. Clin. Med. 5, E17 (2016).
Ramirez, J. M. et al. Prognostic relevance of viable circulating tumor cells detected by EPISPOT in metastatic breast cancer patients. Clin. Chem. 60, 214–221 (2014).
Baccelli, I. et al. Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. Nat. Biotechnol. 31, 539–544 (2013).
Lallo, A., Schenk, M. W., Frese, K. K., Blackhall, F. & Dive, C. Circulating tumor cells and CDX models as a tool for preclinical drug development. Transl Lung Cancer Res. 6, 397–408 (2017).
Rao, C. G. et al. Expression of epithelial cell adhesion molecule in carcinoma cells present in blood and primary and metastatic tumors. Int. J. Oncol. 27, 49–57 (2005).
Srinivasan, M. & Parwani, A. V. Diagnostic utility of p63/P501S double sequential immunohistochemical staining in differentiating urothelial carcinoma from prostate carcinoma. Diagn. Pathol. 6, 67 (2011).
Salman, J. W., Schoots, I. G., Carlsson, S. V., Jenster, G. & Roobol, M. J. Prostate specific antigen as a tumor marker in prostate cancer: biochemical and clinical aspects. Adv. Exp. Med. Biol. 867, 93–114 (2015).
Bostwick, D. G. Prostate-specific antigen. Current role in diagnostic pathology of prostate cancer. Am. J. Clin. Pathol. 102, S31–S37 (1994).
Epstein, J. I. PSA and PAP as immunohistochemical markers in prostate cancer. Urol. Clin. North Am. 20, 757–770 (1993).
Alanen, K. A. et al. Immunohistochemical labelling for prostate-specific antigen in breast carcinomas. Breast Cancer Res. Treat. 56, 169–176 (1999).
Goldstein, N. S. Immunophenotypic characterization of 225 prostate adenocarcinomas with intermediate or high Gleason scores. Am. J. Clin. Pathol. 117, 471–477 (2002).
Queisser, A. et al. Comparison of different prostatic markers in lymph node and distant metastases of prostate cancer. Mod. Pathol. 28, 138–145 (2015).
Kristiansen, G. & Epstein, J. I. Immunohistochemisty in prostate pathology. Patologi https://www.patologi.com/DAKO%20immun%20-prostate-pathology.pdf (2014).
Grignon, D. J., Ro, J. Y., Ayala, A. G., Johnson, D. E. & Ordonez, N. G. Primary adenocarcinoma of the urinary bladder. A clinicopathologic analysis of 72 cases. Cancer 67, 2165–2172 (1991).
Kraus, T. S., Cohen, C. & Siddiqui, M. T. Prostate-specific antigen and hormone receptor expression in male and female breast carcinoma. Diagn. Pathol. 5, 63 (2010).
Levesque, M., Hu, H., D’Costa, M. & Diamandis, E. P. Prostate-specific antigen expression by various tumors. J. Clin. Lab. Anal. 9, 123–128 (1995).
Shidham, V. B. et al. Prostate-specific antigen expression and lipochrome pigment granules in the differential diagnosis of prostatic adenocarcinoma versus seminal vesicle-ejaculatory duct epithelium. Arch. Pathol. Lab. Med. 123, 1093–1097 (1999).
Tazawa, K., Kurihara, Y., Kamoshida, S., Tsukada, K. & Tsutsumi, Y. Localization of prostate-specific antigen-like immunoreactivity in human salivary gland and salivary gland tumors. Pathol. Int. 49, 500–505 (1999).
Varma, M., Morgan, M., Jasani, B., Tamboli, P. & Amin, M. B. Polyclonal anti-PSA is more sensitive but less specific than monoclonal anti-PSA: implications for diagnostic prostatic pathology. Am. J. Clin. Pathol. 118, 202–207 (2002).
Llanes, L. et al. Quantitative real-time reverse transcription: polymerase chain reaction of prostate-specific antigen (PSA) for detection of circulating prostatic cells in patients with clinically localized prostate cancer. Prostate Cancer Prostatic Dis. 8, 248–252 (2005).
Fujii, Y., Kawakami, S., Okada, Y., Kageyama, Y. & Kihara, K. Regulation of prostate-specific antigen by activin A in prostate cancer LNCaP cells. Am. J. Physiol. Endocrinol. Metab. 286, E927–E931 (2004).
Artibani, W., Porcaro, A. B., De Marco, V., Cerruto, M. A. & Siracusano, S. Management of biochemical recurrence after primary curative treatment for prostate cancer: a review. Urol. Int. 100, 251–262 (2018).
Yousef, G. M., Obiezu, C. V., Luo, L. Y., Black, M. H. & Diamandis, E. P. Prostase/KLK-L1 is a new member of the human kallikrein gene family, is expressed in prostate and breast tissues, and is hormonally regulated. Cancer Res. 59, 4252–4256 (1999).
Takayama, T. K., McMullen, B. A., Nelson, P. S., Matsumura, M. & Fujikawa, K. Characterization of hK4 (prostase), a prostate-specific serine protease: activation of the precursor of prostate specific antigen (pro-PSA) and single-chain urokinase-type plasminogen activator and degradation of prostatic acid phosphatase. Biochemistry 40, 15341–15348 (2001).
Todenhofer, T. et al. AR-V7 transcripts in whole blood RNA of patients with metastatic castration resistant prostate cancer correlate with response to abiraterone acetate. J. Urol. 197, 135–142 (2017).
Braun, K., Sjoberg, D. D., Vickers, A. J., Lilja, H. & Bjartell, A. S. A. Four-kallikrein panel predicts high-grade cancer on biopsy: independent validation in a community cohort. Eur. Urol. 69, 505–511 (2016).
Satkunasivam, R. et al. Human kallikrein-2 gene and protein expression predicts prostate cancer at repeat biopsy. SpringerPlus 3, 295 (2014).
Day, C. H. et al. Characterization of KLK4 expression and detection of KLK4-specific antibody in prostate cancer patient sera. Oncogene 21, 7114–7120 (2002).
Finlay, J. A. et al. Development of monoclonal antibodies specific for human glandular kallikrein (hK2): development of a dual antibody immunoassay for hK2 with negligible prostate-specific antigen cross-reactivity. Urology 51, 804–809 (1998).
Rittenhouse, H. G., Finlay, J. A., Mikolajczyk, S. D. & Partin, A. W. Human Kallikrein 2 (hK2) and prostate-specific antigen (PSA): two closely related, but distinct, kallikreins in the prostate. Crit. Rev. Clin. Lab. Sci. 35, 275–368 (1998).
Cooke, P. S., Young, P. & Cunha, G. R. Androgen receptor expression in developing male reproductive organs. Endocrinology 128, 2867–2873 (1991).
Chang, C., Chodak, G., Sarac, E., Takeda, H. & Liao, S. Prostate androgen receptor: immunohistological localization and mRNA characterization. J. Steroid Biochem. 34, 311–313 (1989).
Sar, M., Lubahn, D. B., French, F. S. & Wilson, E. M. Immunohistochemical localization of the androgen receptor in rat and human tissues. Endocrinology 127, 3180–3186 (1990).
Cunha, G. R. The role of androgens in the epithelio-mesenchymal interactions involved in prostatic morphogenesis in embryonic mice. Anat. Rec. 175, 87–96 (1973).
Takeda, H., Lasnitzki, I. & Mizuno, T. Analysis of prostatic bud induction by brief androgen treatment in the fetal rat urogenital sinus. J. Endocrinol. 110, 467–470 (1986).
Donjacour, A. A. & Cunha, G. R. The effect of androgen deprivation on branching morphogenesis in the mouse prostate. Dev. Biol. 128, 1–14 (1988).
Zhou, Q. et al. Localization of androgen and estrogen receptors in adult male mouse reproductive tract. J. Androl. 23, 870–881 (2002).
Georget, V. et al. Trafficking of the androgen receptor in living cells with fused green fluorescent protein-androgen receptor. Mol. Cell Endocrinol. 129, 17–26 (1997).
Jenster, G., Trapman, J. & Brinkmann, A. O. Nuclear import of the human androgen receptor. Biochem. J. 293, 761–768 (1993).
Nightingale, J. et al. Ligand activation of the androgen receptor downregulates E-cadherin-mediated cell adhesion and promotes apoptosis of prostatic cancer cells. Neoplasia 5, 347–361 (2003).
Cai, C. et al. Androgen receptor gene expression in prostate cancer is directly suppressed by the androgen receptor through recruitment of lysine-specific demethylase 1. Cancer Cell 20, 457–471 (2011).
Zarif, J. C., Lamb, L. E., Schulz, V. V., Nollet, E. A. & Miranti, C. K. Androgen receptor non-nuclear regulation of prostate cancer cell invasion mediated by Src and matriptase. Oncotarget 6, 6862–6876 (2015).
Stanbrough, M., Leav, I., Kwan, P. W., Bubley, G. J. & Balk, S. P. Prostatic intraepithelial neoplasia in mice expressing an androgen receptor transgene in prostate epithelium. Proc. Natl Acad. Sci. USA 98, 10823–10828 (2001).
Zhu, C. et al. Conditional expression of the androgen receptor induces oncogenic transformation of the mouse prostate. J. Biol. Chem. 286, 33478–33488 (2011).
Wu, C. T. et al. Increased prostate cell proliferation and loss of cell differentiation in mice lacking prostate epithelial androgen receptor. Proc. Natl Acad. Sci. USA 104, 12679–12684 (2007).
Cunha, G. R. et al. The endocrinology and developmental biology of the prostate. Endocr. Rev. 8, 338–362 (1987).
Chodak, G. W. et al. Nuclear localization of androgen receptor in heterogeneous samples of normal, hyperplastic and neoplastic human prostate. J. Urol. 147, 798–803 (1992).
Sadi, M. V. & Walsh, P. C. & Barrack, E. R. Immunohistochemical study of androgen receptors in metastatic prostate cancer. Comparison of receptor content and response to hormonal therapy. Cancer 67, 3057–3064 (1991).
Ruizeveld de Winter, J. A. et al. Androgen receptor status in localized and locally progressive hormone refractory human prostate cancer. Am. J. Pathol. 144, 735–746 (1994).
Bubendorf, L. et al. Survey of gene amplifications during prostate cancer progression by high-throughout fluorescence in situ hybridization on tissue microarrays. Cancer Res. 59, 803–806 (1999).
de Bono, J. S. et al. Abiraterone and increased survival in metastatic prostate cancer. N. Engl. J. Med. 364, 1995–2005 (2011).
Scher, H. I. et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N. Engl. J. Med. 367, 1187–1197 (2012).
Huggins, C. Endocrine-induced regression of cancers. Cancer Res. 27, 1925–1930 (1967).
Valkenburg, K. C., De Marzo, A. M. & Williams, B. O. Deletion of tumor suppressors adenomatous polyposis coli and Smad4 in murine luminal epithelial cells causes invasive prostate cancer and loss of androgen receptor expression. Oncotarget 8, 80265–80277 (2017).
Aggarwal, R., Zhang, T., Small, E. J. & Armstrong, A. J. Neuroendocrine prostate cancer: subtypes, biology, and clinical outcomes. J. Natl Compr. Canc. Netw. 12, 719–726 (2014).
Wang, W. & Epstein, J. I. Small cell carcinoma of the prostate. A morphologic and immunohistochemical study of 95 cases. Am. J. Surg. Pathol. 32, 65–71 (2008).
Wright, M. E., Tsai, M. J. & Aebersold, R. Androgen receptor represses the neuroendocrine transdifferentiation process in prostate cancer cells. Mol. Endocrinol. 17, 1726–1737 (2003).
Hu, R. et al. Ligand-independent androgen receptor variants derived from splicing of cryptic exons signify hormone-refractory prostate cancer. Cancer Res. 69, 16–22 (2009).
Antonarakis, E. S. et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N. Engl. J. Med. 371, 1028–1038 (2014).
Onstenk, W. et al. Efficacy of cabazitaxel in castration-resistant prostate cancer is independent of the presence of AR-V7 in circulating tumor cells. Eur. Urol. 68, 939–945 (2015).
Abu, E. O., Horner, A., Kusec, V., Triffitt, J. T. & Compston, J. E. The localization of androgen receptors in human bone. J. Clin. Endocrinol. Metab. 82, 3493–3497 (1997).
Khetawat, G. et al. Human megakaryocytes and platelets contain the estrogen receptor beta and androgen receptor (AR): testosterone regulates AR expression. Blood 95, 2289–2296 (2000).
Mantalaris, A. et al. Localization of androgen receptor expression in human bone marrow. J. Pathol. 193, 361–366 (2001).
Uhlén, M. et al. Tissue-based map of the human proteome. Science 347, 1260419 (2015).
Evans, M. J. et al. Noninvasive measurement of androgen receptor signaling with a positron-emitting radiopharmaceutical that targets prostate-specific membrane antigen. Proc. Natl Acad. Sci. USA 108, 9578–9582 (2011).
Hofman, M. S. et al. A prospective randomized multicentre study of the impact of gallium-68 prostate-specific membrane antigen (PSMA) PET/CT imaging for staging high-risk prostate cancer prior to curative-intent surgery or radiotherapy (proPSMA study): clinical trial protocol. BJU Int. https://doi.org/10.1111/bju.14374 (2018).
Rowe, S. P. et al. PET imaging of prostate-specific membrane antigen in prostate cancer: current state of the art and future challenges. Prostate Cancer Prostatic Dis. 19, 223–230 (2016).
Rowe, S. P. et al. Comparison of prostate-specific membrane antigen-based 18F-DCFBC PET/CT to conventional imaging modalities for detection of hormone-naive and castration-resistant metastatic prostate cancer. J. Nucl. Med. 57, 46–53 (2016).
Wright, G. L. Jr, Haley, C., Beckett, M. L. & Schellhammer, P. F. Expression of prostate-specific membrane antigen in normal, benign, and malignant prostate tissues. Urol. Oncol. 1, 18–28 (1995).
Chang, S. S. et al. Prostate-specific membrane antigen is produced in tumor-associated neovasculature. Clin. Cancer Res. 5, 2674–2681 (1999).
Haffner, M. C. et al. Prostate-specific membrane antigen expression in the neovasculature of gastric and colorectal cancers. Hum. Pathol. 40, 1754–1761 (2009).
Kinoshita, Y. et al. Expression of prostate-specific membrane antigen in normal and malignant human tissues. World J. Surg. 30, 628–636 (2006).
Mhawech-Fauceglia, P. et al. Prostate-specific membrane antigen (PSMA) protein expression in normal and neoplastic tissues and its sensitivity and specificity in prostate adenocarcinoma: an immunohistochemical study using mutiple tumour tissue microarray technique. Histopathology 50, 472–483 (2007).
Samplaski, M. K., Heston, W., Elson, P., Magi-Galluzzi, C. & Hansel, D. E. Folate hydrolase (prostate-specific membrane [corrected] antigen) 1 expression in bladder cancer subtypes and associated tumor neovasculature. Mod. Pathol. 24, 1521–1529 (2011).
Troyer, J. K., Beckett, M. L. & Wright, G. L. Jr. Detection and characterization of the prostate-specific membrane antigen (PSMA) in tissue extracts and body fluids. Int. J. Cancer 62, 552–558 (1995).
Artigas, C. et al. Paget bone disease demonstrated on (68)Ga-PSMA ligand PET/CT. Eur. J. Nucl. Med. Mol. Imaging 43, 195–196 (2016).
Chan, M. & Hsiao, E. Subacute cortical infarct showing uptake on 68Ga-PSMA PET/CT. Clin. Nucl. Med. 42, 110–111 (2017).
Dias, A. H., Holm Vendelbo, M. & Bouchelouche, K. Prostate-specific membrane antigen PET/CT: uptake in lymph nodes with active sarcoidosis. Clin. Nucl. Med. 42, e175–e176 (2017).
Pyka, T. et al. 68Ga-PSMA-HBED-CC PET for differential diagnosis of suggestive lung lesions in patients with prostate cancer. J. Nucl. Med. 57, 367–371 (2016).
Vamadevan, S., Le, K., Bui, C. & Mansberg, R. Incidental PSMA uptake in an undisplaced fracture of a vertebral body. Clin. Nucl. Med. 42, 465–466 (2017).
Chu, D. C. et al. The use of real-time quantitative PCR to detect circulating prostate-specific membrane antigen mRNA in patients with prostate carcinoma. Ann. NY Acad. Sci. 1022, 157–162 (2004).
Reiter, R. E. et al. Prostate stem cell antigen: a cell surface marker overexpressed in prostate cancer. Proc. Natl Acad. Sci. USA 95, 1735–1740 (1998).
Tang, S. et al. Positive and negative regulation of prostate stem cell antigen expression by Yin Yang 1 in prostate epithelial cell lines. PLOS ONE 7, e35570 (2012).
Gu, Z. et al. Prostate stem cell antigen (PSCA) expression increases with high gleason score, advanced stage and bone metastasis in prostate cancer. Oncogene 19, 1288–1296 (2000).
Lam, J. S. et al. Prostate stem cell antigen is overexpressed in prostate cancer metastases. Clin. Cancer Res. 11, 2591–2596 (2005).
Hara, N. et al. Reverse transcription-polymerase chain reaction detection of prostate-specific antigen, prostate-specific membrane antigen, and prostate stem cell antigen in one milliliter of peripheral blood: value for the staging of prostate cancer. Clin. Cancer Res. 8, 1794–1799 (2002).
Zhigang, Z. & Wenlu, S. The association of prostate stem cell antigen (PSCA) mRNA expression and subsequent prostate cancer risk in men with benign prostatic hyperplasia following transurethral resection of the prostate. Prostate 68, 190–199 (2008).
Fawzy, M. S., Mohamed, R. H. & Elfayoumi, A. R. Prostate stem cell antigen (PSCA) mRNA expression in peripheral blood in patients with benign prostatic hyperplasia and/or prostate cancer. Med. Oncol. 32, 74 (2015).
Lukyanchuk, V. V. et al. Detection of circulating tumor cells by cytokeratin 20 and prostate stem cell antigen RT-PCR in blood of patients with gastrointestinal cancers. Anticancer Res. 23, 2711–2716 (2003).
Bahrenberg, G., Brauers, A., Joost, H. G. & Jakse, G. Reduced expression of PSCA, a member of the LY-6 family of cell surface antigens, in bladder, esophagus, and stomach tumors. Biochem. Biophys. Res. Commun. 275, 783–788 (2000).
Elsamman, E. et al. Prostate stem cell antigen predicts tumour recurrence in superficial transitional cell carcinoma of the urinary bladder. BJU Int. 97, 1202–1207 (2006).
Ono, H. et al. Prostate stem cell antigen, a presumable organ-dependent tumor suppressor gene, is down-regulated in gallbladder carcinogenesis. Genes Chromosomes Cancer 51, 30–41 (2012).
Amara, N. et al. Prostate stem cell antigen is overexpressed in human transitional cell carcinoma. Cancer Res. 61, 4660–4665 (2001).
Elsamman, E. M. et al. The expression of prostate stem cell antigen in human clear cell renal cell carcinoma: a quantitative reverse transcriptase-polymerase chain reaction analysis. BJU Int. 98, 668–673 (2006).
Kawaguchi, T. et al. Clinical significance of prostate stem cell antigen expression in non-small cell lung cancer. Jpn J. Clin. Oncol. 40, 319–326 (2010).
Cao, D., Ji, H. & Ronnett, B. M. Expression of mesothelin, fascin, and prostate stem cell antigen in primary ovarian mucinous tumors and their utility in differentiating primary ovarian mucinous tumors from metastatic pancreatic mucinous carcinomas in the ovary. Int. J. Gynecol. Pathol. 24, 67–72 (2005).
Argani, P. et al. Discovery of new markers of cancer through serial analysis of gene expression: prostate stem cell antigen is overexpressed in pancreatic adenocarcinoma. Cancer Res. 61, 4320–4324 (2001).
Zhang, L. Y. et al. PSCA acts as a tumor suppressor by facilitating the nuclear translocation of RB1CC1 in esophageal squamous cell carcinoma. Carcinogenesis 37, 320–332 (2016).
Study Group of Millennium Genome Project for, C. et al. Genetic variation in PSCA is associated with susceptibility to diffuse-type gastric cancer. Nat. Genet. 40, 730–740 (2008).
Saeki, N., Gu, J., Yoshida, T. & Wu, X. Prostate stem cell antigen: a Jekyll and Hyde molecule? Clin. Cancer Res. 16, 3533–3538 (2010).
Luo, J. et al. Alpha-methylacyl-CoA racemase: a new molecular marker for prostate cancer. Cancer Res. 62, 2220–2226 (2002).
Zha, S. et al. Alpha-methylacyl-CoA racemase as an androgen-independent growth modifier in prostate cancer. Cancer Res. 63, 7365–7376 (2003).
Went, P. T., Sauter, G., Oberholzer, M. & Bubendorf, L. Abundant expression of AMACR in many distinct tumour types. Pathology 38, 426–432 (2006).
Zhou, M., Chinnaiyan, A. M., Kleer, C. G., Lucas, P. C. & Rubin, M. A. Alpha-methylacyl-CoA racemase: a novel tumor marker over-expressed in several human cancers and their precursor lesions. Am. J. Surg. Pathol. 26, 926–931 (2002).
Evans, A. J. Alpha-methylacyl CoA racemase (P504S): overview and potential uses in diagnostic pathology as applied to prostate needle biopsies. J. Clin. Pathol. 56, 892–897 (2003).
Farinola, M. A. & Epstein, J. I. Utility of immunohistochemistry for alpha-methylacyl-CoA racemase in distinguishing atrophic prostate cancer from benign atrophy. Hum. Pathol. 35, 1272–1278 (2004).
Zhou, M., Jiang, Z. & Epstein, J. I. Expression and diagnostic utility of alpha-methylacyl-CoA-racemase (P504S) in foamy gland and pseudohyperplastic prostate cancer. Am. J. Surg. Pathol. 27, 772–778 (2003).
Cardillo, M. R. et al. Can p503s, p504s and p510s gene expression in peripheral-blood be useful as a marker of prostatic cancer? BMC Cancer 5, 111 (2005).
Beach, R. et al. P504S immunohistochemical detection in 405 prostatic specimens including 376 18-gauge needle biopsies. Am. J. Surg. Pathol. 26, 1588–1596 (2002).
Herawi, M., Parwani, A. V., Irie, J. & Epstein, J. I. Small glandular proliferations on needle biopsies: most common benign mimickers of prostatic adenocarcinoma sent in for expert second opinion. Am. J. Surg. Pathol. 29, 874–880 (2005).
Goldfarb, D. A., Stein, B. S., Shamszadeh, M. & Petersen, R. O. Age-related changes in tissue levels of prostatic acid phosphatase and prostate specific antigen. J. Urol. 136, 1266–1269 (1986).
Yam, L. T. Clinical significance of the human acid phosphatases: a review. Am. J. Med. 56, 604–616 (1974).
Gutman, E. B., Sproul, E. E. & Gutman, A. B. Significance of increased phosphatase activity at the site of osteoplastic metastases secondary to carcinoma of the prostate gland. Am. J. Cancer 28, 485–495 (1936).
Burnett, A. L., Chan, D. W., Brendler, C. B. & Walsh, P. C. The value of serum enzymatic acid phosphatase in the staging of localized prostate cancer. J. Urol. 148, 1832–1834 (1992).
Graddis, T. J., McMahan, C. J., Tamman, J., Page, K. J. & Trager, J. B. Prostatic acid phosphatase expression in human tissues. Int. J. Clin. Exp. Pathol. 4, 295–306 (2011).
Jobsis, A. C., De Vries, G. P., Meijer, A. E. & Ploem, J. S. The immunohistochemical detection of prostatic acid phosphatase: its possibilities and limitations in tumour histochemistry. Histochem. J. 13, 961–973 (1981).
Li, C. Y., Lam, W. K. & Yam, L. T. Immunohistochemical diagnosis of prostatic cancer with metastasis. Cancer 46, 706–712 (1980).
Elgamal, A. A. et al. Detection of prostate specific antigen in pancreas and salivary glands: a potential impact on prostate cancer overestimation. J. Urol. 156, 464–468 (1996).
Haines, A. M., Larkin, S. E., Richardson, A. P., Stirling, R. W. & Heyderman, E. A novel hybridoma antibody (PASE/4LJ) to human prostatic acid phosphatase suitable for immunohistochemistry. Br. J. Cancer 60, 887–892 (1989).
Kamoshida, S. & Tsutsumi, Y. Extraprostatic localization of prostatic acid phosphatase and prostate-specific antigen: distribution in cloacogenic glandular epithelium and sex-dependent expression in human anal gland. Hum. Pathol. 21, 1108–1111 (1990).
Tepper, S. L., Jagirdar, J., Heath, D. & Geller, S. A. Homology between the female paraurethral (Skene’s) glands and the prostate. Immunohistochemical demonstration. Arch. Pathol. Lab. Med. 108, 423–425 (1984).
Tomlins, S. A. et al. Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 310, 644–648 (2005).
Shah, R. B. Clinical applications of novel ERG immunohistochemistry in prostate cancer diagnosis and management. Adv. Anatom. Pathol. 20, 117–124 (2013).
Hagglof, C. et al. TMPRSS2-ERG expression predicts prostate cancer survival and associates with stromal biomarkers. PLOS ONE 9, e86824 (2014).
Petrovics, G. et al. Frequent overexpression of ETS-related gene-1 (ERG1) in prostate cancer transcriptome. Oncogene 24, 3847–3852 (2005).
Hessels, D. et al. Detection of TMPRSS2-ERG fusion transcripts and prostate cancer antigen 3 in urinary sediments may improve diagnosis of prostate cancer. Clin. Cancer Res. 13, 5103–5108 (2007).
Hernandez-Llodra, S. et al. ERG overexpression plus SLC45A3 (prostein) and PTEN expression loss: strong association of the triple hit phenotype with an aggressive pathway of prostate cancer progression. Oncotarget 8, 74106–74118 (2017).
Tomlins, S. A. et al. TMPRSS2:ETV4 gene fusions define a third molecular subtype of prostate cancer. Cancer Res. 66, 3396–3400 (2006).
Robinson, D. et al. Integrative clinical genomics of advanced prostate cancer. Cell 161, 1215–1228 (2015).
Bussemakers, M. J. et al. DD3: a new prostate-specific gene, highly overexpressed in prostate cancer. Cancer Res. 59, 5975–5979 (1999).
Gezer, U., Tiryakioglu, D., Bilgin, E., Dalay, N. & Holdenrieder, S. Androgen stimulation of PCA3 and miR-141 and their release from prostate cancer cells. Cell J. 16, 488–493 (2015).
Salagierski, M. et al. Differential expression of PCA3 and its overlapping PRUNE2 transcript in prostate cancer. Prostate 70, 70–78 (2010).
Salameh, A. et al. PRUNE2 is a human prostate cancer suppressor regulated by the intronic long noncoding RNA PCA3. Proc. Natl Acad. Sci. USA 112, 8403–8408 (2015).
de Kok, J. B. et al. DD3(PCA3), a very sensitive and specific marker to detect prostate tumors. Cancer Res. 62, 2695–2698 (2002).
Loeb, S. & Partin, A. W. Review of the literature: PCA3 for prostate cancer risk assessment and prognostication. Rev. Urol. 13, e191–e195 (2011).
Tomlins, S. A. et al. Urine TMPRSS2:ERG plus PCA3 for individualized prostate cancer risk assessment. Eur. Urol. 70, 45–53 (2016).
Gurel, B. et al. NKX3.1 as a marker of prostatic origin in metastatic tumors. Am. J. Surg. Pathol. 34, 1097–1105 (2010).
Xu, L. L. et al. Expression profile of an androgen regulated prostate specific homeobox gene NKX3.1 in primary prostate cancer. J. Urol. 163, 972–979 (2000).
He, W. W. et al. A novel human prostate-specific, androgen-regulated homeobox gene (NKX3.1) that maps to 8p21, a region frequently deleted in prostate cancer. Genomics 43, 69–775 (1997).
Bethel, C. R. et al. Decreased NKX3.1 protein expression in focal prostatic atrophy, prostatic intraepithelial neoplasia, and adenocarcinoma: association with gleason score and chromosome 8p deletion. Cancer Res. 66, 10683–10690 (2006).
Bowen, C. et al. Loss of NKX3.1 expression in human prostate cancers correlates with tumor progression. Cancer Res. 60, 6111–6115 (2000).
Gelmann, E. P., Bowen, C. & Bubendorf, L. Expression of NKX3.1 in normal and malignant tissues. Prostate 55, 111–117 (2003).
Voeller, H. J. et al. Coding region of NKX3.1, a prostate-specific homeobox gene on 8p21, is not mutated in human prostate cancers. Cancer Res. 57, 4455–4459 (1997).
Kim, Y. R. et al. HOXB13 promotes androgen independent growth of LNCaP prostate cancer cells by the activation of E2F signaling. Mol. Cancer 9, 124 (2010).
Norris, J. D. et al. The homeodomain protein HOXB13 regulates the cellular response to androgens. Mol. Cell 36, 405–416 (2009).
Kim, S. D. et al. HOXB13 is co-localized with androgen receptor to suppress androgen-stimulated prostate-specific antigen expression. Anat. Cell Biol. 43, 284–293 (2010).
Zabalza, C. V. et al. HOXB13 overexpression is an independent predictor of early PSA recurrence in prostate cancer treated by radical prostatectomy. Oncotarget 6, 12822–12834 (2015).
Varinot, J. et al. HOXB13 is a sensitive and specific marker of prostate cells, useful in distinguishing between carcinomas of prostatic and urothelial origin. Virchows Arch. 463, 803–809 (2013).
Alshenawy, H. A. & Saied, E. Do HOXB13 and P63 have a role in differentiating poorly differentiated prostatic carcinoma from urothelial high-grade carcinoma? APMIS 123, 772–778 (2015).
Varinot, J. et al. HOXB13 protein expression in metastatic lesions is a promising marker for prostate origin. Virchows Arch. 468, 619–622 (2016).
Ewing, C. M. et al. Germline mutations in HOXB13 and prostate-cancer risk. N. Engl. J. Med. 366, 141–149 (2012).
Barresi, V. et al. HOXB13 as an immunohistochemical marker of prostatic origin in metastatic tumors. APMIS 124, 188–193 (2016).
Lilja, H. & Abrahamsson, P. A. Three predominant proteins secreted by the human prostate gland. Prostate 12, 29–38 (1988).
Akiyama, K. et al. The amino acid sequence of human beta-microseminoprotein. Biochim. Biophys. Acta 829, 288–294 (1985).
Seidah, N. G., Arbatti, N. J., Rochemont, J., Sheth, A. R. & Chretien, M. Complete amino acid sequence of human seminal plasma beta-inhibin. Prediction of post Gln-Arg cleavage as a maturation site. FEBS Lett. 175, 349–355 (1984).
Dube, J. Y. et al. Isolation from human seminal plasma of an abundant 16-kDa protein originating from the prostate, its identification with a 94-residue peptide originally described as beta-inhibin. J. Androl. 8, 182–189 (1987).
Dube, J. Y., Pelletier, G., Gagnon, P. & Tremblay, R. R. Immunohistochemical localization of a prostatic secretory protein of 94 amino acids in normal prostatic tissue, in primary prostatic tumors and in their metastases. J. Urol. 138, 883–887 (1987).
Hara, M. & Kimura, H. Two prostate-specific antigens, gamma-seminoprotein and beta-microseminoprotein. J. Lab. Clin. Med. 113, 541–548 (1989).
Kwong, J., Xuan, J. W., Chan, P. S., Ho, S. M. & Chan, F. L. A comparative study of hormonal regulation of three secretory proteins (prostatic secretory protein-PSP94, probasin, and seminal vesicle secretion II) in rat lateral prostate. Endocrinology 141, 4543–4551 (2000).
Anahi Franchi, N. et al. β-Microseminoprotein in human spermatozoa and its potential role in male fertility. Reproduction 136, 157–166 (2008).
Edstrom Hagerwall, A. M. et al. β-Microseminoprotein endows post coital seminal plasma with potent candidacidal activity by a calcium- and pH-dependent mechanism. PLOS Pathog. 8, e1002625 (2012).
Weiber, H. et al. Beta microseminoprotein is not a prostate-specific protein. Its identification in mucous glands and secretions. Am. J. Pathol. 137, 593–603 (1990).
Ma, J. X. et al. PSP94, an upstream signaling mediator of prostasin found highly elevated in ovarian cancer. Cell Death Dis. 5, e1407 (2014).
Liu, A. Y., Bradner, R. C. & Vessella, R. L. Decreased expression of prostatic secretory protein PSP94 in prostate cancer. Cancer Lett. 74, 91–99 (1993).
Garde, S., Sheth, A., Porter, A. T. & Pienta, K. J. Effect of prostatic inhibin peptide (PIP) on prostate cancer cell growth in vitro and in vivo. Prostate 22, 225–233 (1993).
Garde, S. V. et al. Prostate secretory protein (PSP94) suppresses the growth of androgen-independent prostate cancer cell line (PC3) and xenografts by inducing apoptosis. Prostate 38, 118–125 (1999).
Shukeir, N., Arakelian, A., Kadhim, S., Garde, S. & Rabbani, S. A. Prostate secretory protein PSP-94 decreases tumor growth and hypercalcemia of malignancy in a syngenic in vivo model of prostate cancer. Cancer Res. 63, 2072–2078 (2003).
Shukeir, N., Garde, S., Wu, J. J., Panchal, C. & Rabbani, S. A. Prostate secretory protein of 94 amino acids (PSP-94) and its peptide (PCK3145) as potential therapeutic modalities for prostate cancer. Anticancer Drugs 16, 1045–1051 (2005).
Imasato, Y. et al. PSP94 expression after androgen deprivation therapy: a comparative study with prostate specific antigen in benign prostate and prostate cancer. J. Urol. 164, 1819–1824 (2000).
Chang, B. L. et al. Fine mapping association study and functional analysis implicate a SNP in MSMB at 10q11 as a causal variant for prostate cancer risk. Hum. Mol. Genet. 18, 1368–1375 (2009).
Sutcliffe, S., De Marzo, A. M., Sfanos, K. S. & Laurence, M. MSMB variation and prostate cancer risk: clues towards a possible fungal etiology. Prostate 74, 569–578 (2014).
Beke, L., Nuytten, M., Van Eynde, A., Beullens, M. & Bollen, M. The gene encoding the prostatic tumor suppressor PSP94 is a target for repression by the Polycomb group protein EZH2. Oncogene 26, 4590–4595 (2007).
Lamy, S. et al. A prostate secretory protein94-derived synthetic peptide PCK3145 inhibits VEGF signalling in endothelial cells: implication in tumor angiogenesis. Int. J. Cancer 118, 2350–2358 (2006).
Xu, J. et al. Identification and characterization of prostein, a novel prostate-specific protein. Cancer Res. 61, 1563–1568 (2001).
Sheridan, T., Herawi, M., Epstein, J. I. & Illei, P. B. The role of P501S and PSA in the diagnosis of metastatic adenocarcinoma of the prostate. Am. J. Surg. Pathol. 31, 1351–1355 (2007).
Kalos, M. et al. Prostein expression is highly restricted to normal and malignant prostate tissues. Prostate 60, 246–256 (2004).
Yin, M., Dhir, R. & Parwani, A. V. Diagnostic utility of p501s (prostein) in comparison to prostate specific antigen (PSA) for the detection of metastatic prostatic adenocarcinoma. Diagn. Pathol. 2, 41 (2007).
Lane, Z., Hansel, D. E. & Epstein, J. I. Immunohistochemical expression of prostatic antigens in adenocarcinoma and villous adenoma of the urinary bladder. Am. J. Surg. Pathol. 32, 1322–1326 (2008).
Valkenburg, K. C. & Pienta, K. J. Drug discovery in prostate cancer mouse models. Expert Opin. Drug Discov. 10, 1011–1024 (2015).
Valkenburg, K. C. & Williams, B. O. Mouse models of prostate cancer. Prostate Cancer 2011, 895238 (2011).
El-Alfy, M., Pelletier, G., Hermo, L. S. & Labrie, F. Unique features of the basal cells of human prostate epithelium. Microsc. Res. Tech. 51, 436–446 (2000).
Diamandis, E. P., Yousef, G. M. & Olsson, A. Y. An update on human and mouse glandular kallikreins. Clin. Biochem. 37, 258–260 (2004).
Thota, A. et al. Mouse PSP94 expression is prostate tissue-specific as demonstrated by a comparison of multiple antibodies against recombinant proteins. J. Cell. Biochem. 88, 999–1011 (2003).
Kozak, C. A., Adamson, M. C. & Horowitz, M. Genetic mapping of the mouse prosaposin gene (Psap) to mouse chromosome 10. Genomics 23, 508–510 (1994).
Schmittgen, T. D. et al. Expression pattern of mouse homolog of prostate-specific membrane antigen (FOLH1) in the transgenic adenocarcinoma of the mouse prostate model. Prostate 55, 308–316 (2003).
Sreenath, T., Orosz, A., Fujita, K. & Bieberich, C. J. Androgen-independent expression of hoxb-13 in the mouse prostate. Prostate 41, 203–207 (1999).
Hubbard, G. K. et al. Combined MYC activation and Pten loss are sufficient to create genomic instability and lethal metastatic prostate cancer. Cancer Res. 76, 283–292 (2016).
Sciavolino, P. J. et al. Tissue-specific expression of murine Nkx3.1 in the male urogenital system. Dev. Dyn. 209, 127–138 (1997).
Abdulkadir, S. A. et al. Conditional loss of Nkx3.1 in adult mice induces prostatic intraepithelial neoplasia. Mol. Cell. Biol. 22, 1495–1503 (2002).
Bhatia-Gaur, R. et al. Roles for Nkx3.1 in prostate development and cancer. Genes Dev. 13, 966–977 (1999).
Autio, K. J. et al. Role of AMACR (alpha-methylacyl-CoA racemase) and MFE-1 (peroxisomal multifunctional enzyme-1) in bile acid synthesis in mice. Biochem. J. 461, 125–135 (2014).
Diez-Roux, G. et al. A high-resolution anatomical atlas of the transcriptome in the mouse embryo. PLOS Biol. 9, e1000582 (2011).
Shappell, S. B. et al. Prostate pathology of genetically engineered mice: definitions and classification. The consensus report from the Bar Harbor meeting of the Mouse Models of Human Cancer Consortium Prostate Pathology Committee. Cancer Res. 64, 2270–2305 (2004).
Michiel Sedelaar, J. P., Dalrymple, S. S. & Isaacs, J. T. Of mice and men—warning: intact versus castrated adult male mice as xenograft hosts are equivalent to hypogonadal versus abiraterone treated aging human males, respectively. Prostate 73, 1316–1325 (2013).
Ku, S. Y. et al. Rb1 and Trp53 cooperate to suppress prostate cancer lineage plasticity, metastasis, and antiandrogen resistance. Science 355, 78–83 (2017).
Amling, C. L. et al. Long-term hazard of progression after radical prostatectomy for clinically localized prostate cancer: continued risk of biochemical failure after 5 years. J. Urol. 164, 101–105 (2000).
Chery, L. et al. Characterization of single disseminated prostate cancer cells reveals tumor cell heterogeneity and identifies dormancy associated pathways. Oncotarget 5, 9939–9951 (2014).
Guzvic, M. et al. Combined genome and transcriptome analysis of single disseminated cancer cells from bone marrow of prostate cancer patients reveals unexpected transcriptomes. Cancer Res. 74, 7383–7394 (2014).
Krivacic, R. T. et al. A rare cell detector for cancer. Proc. Natl Acad. Sci. USA 101, 10501–10504 (2004).
Ramos-Vara, J. A. Technical aspects of immunohistochemistry. Vet. Pathol. 42, 405–426 (2005).
Burry, R. W. Controls for immunocytochemistry: an update. J. Histochem. Cytochem. 59, 6–12 (2011).
Angelo, M. et al. Multiplexed ion beam imaging of human breast tumors. Nat. Med. 20, 436–442 (2014).
Gao, J. et al. VISTA is an inhibitory immune checkpoint that is increased after ipilimumab therapy in patients with prostate cancer. Nat. Med. 23, 551–555 (2017).
Nair, N. et al. High-dimensional immune profiling of total and rotavirus VP6-specific intestinal and circulating B cells by mass cytometry. Mucosal Immunol. 9, 68–82 (2016).
Matos, L. L., Trufelli, D. C., de Matos, M. G. & da Silva Pinhal, M. A. Immunohistochemistry as an important tool in biomarkers detection and clinical practice. Biomark. Insights 5, 9–20 (2010).
Lipman, N. S., Jackson, L. R., Trudel, L. J. & Weis-Garcia, F. Monoclonal versus polyclonal antibodies: distinguishing characteristics, applications, and information resources. ILAR J. 46, 258–268 (2005).
Hsi, E. D. A practical approach for evaluating new antibodies in the clinical immunohistochemistry laboratory. Arch. Pathol. Lab. Med. 125, 289–294 (2001).
Leong, A. S. Quantitation in immunohistology: fact or fiction? A discussion of variables that influence results. Appl. Immunohistochem. Mol. Morphol. 12, 1–7 (2004).
Shi, S. R., Liu, C. & Taylor, C. R. Standardization of immunohistochemistry for formalin-fixed, paraffin-embedded tissue sections based on the antigen-retrieval technique: from experiments to hypothesis. J. Histochem. Cytochem. 55, 105–109 (2007).
Billinton, N. & Knight, A. W. Seeing the wood through the trees: a review of techniques for distinguishing green fluorescent protein from endogenous autofluorescence. Anal. Biochem. 291, 175–197 (2001).
Dall, P. et al. Comparison of immunohistochemistry and RT-PCR for detection of CD44v-expression, a new prognostic factor in human breast cancer. Int. J. Cancer 60, 471–477 (1995).
Parra, E. R. et al. Validation of multiplex immunofluorescence panels using multispectral microscopy for immune-profiling of formalin-fixed and paraffin-embedded human tumor tissues. Sci. Rep. 7, 13380 (2017).
Leite, K. R. et al. The use of immunohistochemistry for diagnosis of prostate cancer. Int. Braz. J. Urol. 36, 583–590 (2010).
Lin, J. R., Fallahi-Sichani, M. & Sorger, P. K. Highly multiplexed imaging of single cells using a high-throughput cyclic immunofluorescence method. Nat. Commun. 6, 8390 (2015).
Dago, A. E. et al. Rapid phenotypic and genomic change in response to therapeutic pressure in prostate cancer inferred by high content analysis of single circulating tumor cells. PLOS ONE 9, e101777 (2014).
Miyamoto, D. T., Ting, D. T., Toner, M., Maheswaran, S. & Haber, D. A. Single-cell analysis of circulating tumor cells as a window into tumor heterogeneity. Cold Spring Harb. Symp. Quant. Biol. 81, 269–274 (2016).
Yeo, T. et al. Microfluidic enrichment for the single cell analysis of circulating tumor cells. Sci. Rep. 6, 22076 (2016).
Bostrom, P. J. & Soloway, M. S. Secondary cancer after radiotherapy for prostate cancer: should we be more aware of the risk? Eur. Urol. 52, 973–982 (2007).
Brennen, W. N. & Isaacs, J. T. Mesenchymal stem cells and the embryonic reawakening theory of BPH. Nat. Rev. Urol. https://doi.org/10.1038/s41585-018-0087-9 (2018).
Di Cristofano, A. et al. Pten and p27KIP1 cooperate in prostate cancer tumor suppression in the mouse. Nat. Genet. 27, 222–224 (2001).
Acknowledgements
This work is supported by NCI grants U54CA143803, CA163124, CA093900, and CA143055 as well as the Prostate Cancer Foundation, the Patrick C. Walsh Fund and a gift from the Stutt family. E.E.v.d.T. is supported by the Cure for Cancer Foundation. K.C.V. is supported by NCI grant F32CA206394.
Reviewer information
Nature Reviews Urology thanks Y.-J. Lu, A. Strati, and T. Todenhöfer, for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
E.E.v.d.T., H.D.A., and K.C.V. researched data for the article, E.E.v.d.T., J.J.d.l.R., T.M.d.R., K.J.P., and K.C.V. made substantial contributions to discussions of content. E.E.v.d.T., H.D.A., and K.C.V. wrote the article and all authors reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
van der Toom, E.E., Axelrod, H.D., de la Rosette, J.J. et al. Prostate-specific markers to identify rare prostate cancer cells in liquid biopsies. Nat Rev Urol 16, 7–22 (2019). https://doi.org/10.1038/s41585-018-0119-5
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-018-0119-5
This article is cited by
-
Diagnostic liquid biopsy biomarkers in renal cell cancer
Nature Reviews Urology (2024)
-
Novel insights into the multifaceted roles of m6A-modified LncRNAs in cancers: biological functions and therapeutic applications
Biomarker Research (2023)
-
Suppression of bone metastatic castration-resistant prostate cancer cell growth by a suicide gene delivered by JC polyomavirus-like particles
Gene Therapy (2023)
-
Prostein expression on circulating tumor cells as a prognostic marker in metastatic castration-resistant prostate cancer
Prostate Cancer and Prostatic Diseases (2023)
-
Liquid biopsy for monitoring of tumor dormancy and early detection of disease recurrence in solid tumors
Cancer and Metastasis Reviews (2023)