Abstract
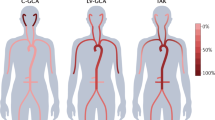
Behçet syndrome is a rare, chronic inflammatory disease of unknown aetiopathogenesis, most commonly presenting with mucocutaneous and ocular manifestations. Vascular involvement, most frequently superficial vein and deep vein thrombosis, can occur in up to 50% of patients with Behçet syndrome. Venous thrombosis at atypical sites (inferior and superior vena cava, suprahepatic veins with Budd–Chiari syndrome, portal vein, cerebral sinuses and right atrium and/or ventricle) and arterial involvement (mostly in situ thrombosis and aneurysms of the pulmonary arteries, as well as aneurysms of the abdominal aorta, and peripheral and visceral arteries) are also unique features of Behçet syndrome. Behçet syndrome is considered a natural model of inflammation-induced thrombosis in humans, with an impaired immune-inflammatory response rather than traditional cardiovascular risk factors contributing to thrombogenesis. Specifically, neutrophil hyperactivation and neutrophil-mediated mechanisms of damage directly promote endothelial dysfunction, platelet activation and thrombogenesis in Behçet syndrome. This unusual pathogenesis directly determines the treatment approach, which relies mostly on immunosuppressants rather than anticoagulants for treatment of thrombosis and for secondary prevention. This Review discusses the main histopathological, pathogenetic and clinical aspects of vascular Behçet syndrome, addressing their implications for therapeutic management. Future perspectives in terms of pathogenetic studies, disease monitoring and treatment strategies are also discussed.
Key points
-
Vascular involvement occurs in up to 50% of patients with Behçet syndrome, mostly in the form of superficial and deep vein thrombosis.
-
Behçet syndrome is considered a natural model of inflammation-induced thrombosis in humans, as thrombogenesis is mostly due to an impaired immune-inflammatory response rather than traditional cardiovascular risk factors.
-
Neutrophil hyperactivation and neutrophil-mediated mechanisms of damage directly sustain endothelial dysfunction, platelet activation and thrombogenesis in Behçet syndrome.
-
Venous thrombosis at atypical sites (such as Budd–Chiari syndrome, inferior and superior vena cava, and cerebral venous sinus thrombosis), and pulmonary and non-pulmonary artery involvement are also unique features of Behçet syndrome.
-
Thrombosis treatment and secondary prevention in Behçet syndrome currently relies mostly on immunosuppressants rather than on anticoagulants.
-
Research is needed to address the contribution of epigenetic modulators in Behçet syndrome thrombogenesis, to assess the diagnostic performance of vascular imaging to support Behçet syndrome diagnosis, and to identify new pharmacological and non-pharmacological therapeutic approaches.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Yazici, H., Ugurlu, S. & Seyahi, E. Behçet syndrome: is it one condition? Clin. Rev. Allergy Immunol. 43, 275–280 (2012).
Seyahi, E. Phenotypes in Behçet’s syndrome. Intern. Emerg. Med. 14, 677–689 (2019).
Bettiol, A., Prisco, D. & Emmi, G. Behçet: the syndrome. Rheumatology 59, iii101–iii107 (2020).
Tascilar, K. et al. Vascular involvement in Behçet’s syndrome: a retrospective analysis of associations and the time course. Rheumatology 53, 2018–2022 (2014).
Alkaabi, J. K. & Pathare, A. Pattern and outcome of vascular involvement of Omani patients with Behcet’s disease. Rheumatol. Int. 31, 731–735 (2011).
Kural-Seyahi, E. et al. The long-term mortality and morbidity of Behçet syndrome: a 2-decade outcome survey of 387 patients followed at a dedicated center. Medicine 82, 60–76 (2003).
Davatchi, F. et al. Behcet’s disease: epidemiology, clinical manifestations, and diagnosis. Expert. Rev. Clin. Immunol. 13, 57–65 (2017).
Ames, P. R., Steuer, A., Pap, A. & Denman, A. M. Thrombosis in Behçet’s disease: a retrospective survey from a single UK centre. Rheumatology 40, 652–655 (2001).
Kara Kivanc, B. et al. Why are male patients with Behçet’s disease prone to thrombosis? A rotational thromboelastographic analysis. Clin. Exp. Rheumatol. 36, 63–67 (2018).
Nasr, H. & Scriven, J. M. Superficial thrombophlebitis (superficial venous thrombosis). Br. Med. J. 350, h2039 (2015).
Sarr, S. A. et al. Superior vena cava syndrome revealing a Behçet’s disease. Thromb. J. 13, 7 (2015).
Toledo-Samaniego, N. et al. Arterial and venous involvement in Behçet’s syndrome: a narrative review. J. Thromb. Thrombolysis 54, 162–171 (2022).
Emmi, G. et al. Vascular Behçet’s syndrome: an update. Intern. Emerg. Med. 14, 645–652 (2019).
Becatti, M. et al. Behçet’s syndrome as a tool to dissect the mechanisms of thrombo-inflammation: clinical and pathogenetic aspects. Clin. Exp. Immunol. 195, 322–333 (2019).
Khalid, U. & Saleem, T. Hughes-Stovin syndrome. Orphanet J. Rare Dis. 6, 15 (2011).
Uzun, O., Akpolat, T. & Erkan, L. Pulmonary vasculitis in Behçet disease: a cumulative analysis. Chest 127, 2243–2253 (2005).
Mattioli, I., Bettiol, A., Saruhan-Direskeneli, G., Direskeneli, H. & Emmi, G. Pathogenesis of Behçet’s syndrome: genetic, environmental and immunological factors. Front. Med. 8, 713052 (2021).
Bettiol, A. et al. Treating the different phenotypes of Behçet’s syndrome. Front. Immunol. 10, 2830 (2019).
Demirkesen, C., Oz, B. & Goksel, S. in Behçet’s syndrome 171–189 (Springer, 2020).
Emmi, G. et al. Thrombosis in vasculitis: from pathogenesis to treatment. Thromb. J. 13, 15 (2015).
Emmi, G. et al. Behçet’s syndrome as a model of thrombo-inflammation: the role of neutrophils. Front. Immunol. 10, 1085 (2019).
Ruf, W. & Ruggeri, Z. M. Neutrophils release brakes of coagulation. Nat. Med. 16, 851–852 (2010).
Soehnlein, O. Multiple roles for neutrophils in atherosclerosis. Circ. Res. 110, 875–888 (2012).
Kobayashi, M. et al. Neutrophil and endothelial cell activation in the vasa vasorum in vasculo-Behçet disease. Histopathology 36, 362–371 (2000).
Sahin, S., Akoglu, T., Direskeneli, H., Sen, L. S. & Lawrence, R. Neutrophil adhesion to endothelial cells and factors affecting adhesion in patients with Behçet’s disease. Ann. Rheum. Dis. 55, 128–133 (1996).
Eksioglu-Demiralp, E. et al. Neutrophil activation in Behçet’s disease. Clin. Exp. Rheumatol. 19, S19–S24 (2001).
Yavuz, S. et al. Dual effects of testosterone in Behcet’s disease: implications for a role in disease pathogenesis. Genes. Immun. 17, 335–341 (2016).
Durmazlar, S. P. et al. Significance of serum interleukin-8 levels in patients with Behcet’s disease: high levels may indicate vascular involvement. Int. J. Dermatol. 48, 259–264 (2009).
Becatti, M. et al. Neutrophil activation promotes fibrinogen oxidation and thrombus formation in Behçet disease. Circulation 133, 302–311 (2016). This study investigated the pathogenesis of thrombo-inflammation in vascular Behçet syndrome, and demonstrated how oxidative stress can induce pro-thrombotic modifications of fibrinogen, a key molecule involved in the coagulation pathway.
Orem, A. et al. Relationship between lipid peroxidation and disease activity in patients with Behçet’s disease. J. Dermatol. Sci. 16, 11–16 (1997).
Orem, A., Cimsit, G., Deger, O., Vanizor, B. & Karahan, S. C. Autoantibodies against oxidatively modified low-density lipoprotein in patients with Behçet’s disease. Dermatology 198, 243–246 (1999).
Orem, A. et al. The evaluation of autoantibodies against oxidatively modified low-density lipoprotein (LDL), susceptibility of LDL to oxidation, serum lipids and lipid hydroperoxide levels, total antioxidant status, antioxidant enzyme activities, and endothelial dysfunction in patients with Behçet’s disease. Clin. Biochem. 35, 217–224 (2002).
Stoiber, W., Obermayer, A., Steinbacher, P. & Krautgartner, W. D. The role of reactive oxygen species (ROS) in the formation of extracellular traps (ETs) in humans. Biomolecules 5, 702–723 (2015).
Delgado-Rizo, V. et al. Neutrophil extracellular traps and its implications in inflammation: an overview. Front. Immunol. 8, 81 (2017).
Chen, J., Liu, T., He, J. & Liu, Y. Correspondence on ‘Critical role of neutrophil extracellular traps (NETs) in patients with Behcet’s disease’. Ann. Rheum. Dis. https://doi.org/10.1136/annrheumdis-2020-21947 (2020).
Safi, R. et al. Neutrophils contribute to vasculitis by increased release of neutrophil extracellular traps in Behçet’s disease. J. Dermatol. Sci. 92, 143–150 (2018).
Le Joncour, A. et al. Critical role of neutrophil extracellular traps (NETs) in patients with Behcet’s disease. Ann. Rheum. Dis. 78, 1274–1282 (2019). This study showed the role of NETs as a potential mechanism of neutrophil-induced thrombo-inflammation.
Bettiol, A. et al. Neutrophil-mediated mechanisms of damage and in-vitro protective effect of colchicine in non-vascular Behçet’s syndrome. Clin. Exp. Immunol. 206, 410–421 (2021).
Li, L. et al. Neutrophil extracellular traps promote aberrant macrophages activation in Behçet’s disease. Front. Immunol. 11, 590622 (2020).
Nakazawa, D. et al. The responses of macrophages in interaction with neutrophils that undergo NETosis. J. Autoimmun. 67, 19–28 (2016).
Folco, E. J. et al. Neutrophil extracellular traps induce endothelial cell activation and tissue factor production through interleukin-1ɑ and cathepsin G. Arterioscler. Thromb. Vasc. Biol. 38, 1901–1912 (2018).
Consolandi, C. et al. Behçet’s syndrome patients exhibit specific microbiome signature. Autoimmun. Rev. 14, 269–276 (2015). This study demonstrated how Behçet’s syndrome is characterized by a specific microbiome signature and microbiota dysbiosis.
Brown, J. M. & Hazen, S. L. Microbial modulation of cardiovascular disease. Nat. Rev. Microbiol. 16, 171–181 (2018).
Emmi, G. et al. Butyrate-rich diets improve redox status and fibrin lysis in Behçet’s syndrome. Circ. Res. 128, 278–280 (2021). This pilot study investigated for the first time the effects of tailored nutritional interventions to reduce redox status and the consequent pro-thrombotic milieu in patients with Behçet syndrome.
Pagliai, G. et al. Modulation of gut microbiota through nutritional interventions in Behçet’s syndrome patients (the MAMBA study): study protocol for a randomized controlled trial. Trials 21, 511 (2020).
Kawakami, T. et al. Presence of neutrophil extracellular traps in superficial venous thrombosis of Behçet’s disease. J. Dermatol. 49, 741–745 (2022).
Onur, E. et al. Oxidative stress impairs endothelial nitric oxide levels in Behçets’ disease. Cutan. Ocul. Toxicol. 30, 217–220 (2011).
Sahin, M. et al. Asymmetric dimethylarginine and nitric oxide levels as signs of endothelial dysfunction in Behcet’s disease. Ann. Clin. Lab. Sci. 36, 449–454 (2006).
Ozoran, K., Dugun, N., Gurler, A., Tutkak, H. & Tokgoz, G. Plasma von Willebrand factor, tissue plasminogen activator, plasminogen activator inhibitor, and antithrombin III levels in Behçet’s disease. Scand. J. Rheumatol. 24, 376–382 (1995).
Haznedaroglu, I. C., Ozcebe, O., Celik, I., Dundar, S. V. & Kirazhi, S. Haemostatic markers of procoagulant imbalance in Behçet’s disease. Eur. J. Haematol. 57, 107–108 (1996).
Butta, N. V., Fernandez-Bello, I., Lopez-Longo, F. J. & Jimenez-Yuste, V. Endothelial dysfunction and altered coagulation as mediators of thromboembolism in Behçet disease. Semin. Thromb. Hemost. 41, 621–628 (2015).
Emmi, G. et al. Stem-cell-derived circulating progenitors dysfunction in Behçet’s syndrome patients correlates with oxidative stress. Front. Immunol. 10, 2877 (2019).
Triolo, G. et al. Enhancement of endothelial cell E-selectin expression by sera from patients with active Behçet’s disease: moderate correlation with anti-endothelial cell antibodies and serum myeloperoxidase levels. Clin. Immunol. 91, 330–337 (1999).
Sari, R. A., Kiziltunc, A., Tays’y, S., Akdem’yr, S. & Gundogdu, M. Levels of soluble E-selectin in patients with active Behçet’s disease. Clin. Rheumatol. 24, 55–59 (2005).
Turkoz, Y. et al. Serum levels of soluble P-selectin are increased and associated with disease activity in patients with Behçet’s syndrome. Mediators Inflamm. 2005, 237–241 (2005).
Martinez, M. et al. Platelet activation and red blood cell phosphatidylserine exposure evaluated by flow cytometry in patients with Behçet’s disease: are they related to thrombotic events? Pathophysiol. Haemost. Thromb. 36, 18–22 (2007).
Polat, G. et al. Association of the platelet glycoprotein Ia C807T/G873A gene polymorphism and thrombosis in Behçet patients. Haematologia 32, 121–128 (2002).
Haim, S. et al. Platelet function in Behçet’s disease. J. Dermatol. 11, 117–120 (1984).
Akar, S. et al. Circulated activated platelets and increased platelet reactivity in patients with Behçet’s disease. Clin. Appl. Thromb. Hemost. 12, 451–457 (2006).
Wilson, A. P., Efthimiou, J. & Betteridge, D. J. Decreased prostacyclin sensitivity of platelets in patients with Behçet’s syndrome. Eur. J. Clin. Invest. 18, 410–414 (1988).
Niccolai, E. et al. Microparticles: bridging the gap between autoimmunity and thrombosis. Semin. Thromb. Hemost. 41, 413–422 (2015).
Macey, M. et al. Age, gender and disease-related platelet and neutrophil activation ex vivo in whole blood samples from patients with Behçet’s disease. Rheumatol 50, 1849–1859 (2011).
Khan, E. et al. A low balance between microparticles expressing tissue factor pathway inhibitor and tissue factor is associated with thrombosis in Behçet’s Syndrome. Sci. Rep. 6, 38104 (2016).
Emmi, G. et al. A unique circulating miRNA profile highlights thrombo-inflammation in Behçet’s syndrome. Ann. Rheum. Dis. 81, 386–397 (2022). This study investigated for the first time the role of circulating miRNA in thrombo-inflammation in Behçet syndrome.
Bagni, G. et al. Circulating miRNome profiling data in Behçet’s syndrome. Data Brief. 38, 107435 (2021).
Caramaschi, P. et al. A study on thrombophilic factors in Italian Behcet’s patients. Jt. Bone Spine 77, 330–334 (2010).
Haznedaroglu, I. C. et al. Impaired haemostatic kinetics and endothelial function in Behçet’s disease. J. Intern. Med. 240, 181–187 (1996).
Aitchison, R., Chu, P., Cater, D. R., Harris, R. J. & Powell, R. J. Defective fibrinolysis in Behçet’s syndrome: significance and possible mechanisms. Ann. Rheum. Dis. 48, 590–593 (1989).
Hampton, K. K., Chamberlain, M. A., Menon, D. K. & Davies, J. A. Coagulation and fibrinolytic activity in Behçet’s disease. Thromb. Haemost. 66, 292–294 (1991).
Lee, Y. J. et al. Coagulation parameters and plasma total homocysteine levels in Behcet’s disease. Thromb. Res. 106, 19–24 (2002).
Beyan, E., Sadikoglu, B., Ertugrul, E. & Beyan, C. Von Willebrand factor antigen levels in Behçet disease. Am. J. Hematol. 79, 70–72 (2005).
Esmat, S. et al. Lipoprotein (a) and nitrites in Behcet’s disease: relationship with disease activity and vascular complications. Eur. J. Dermatol. 16, 67–71 (2006).
Gurbuz, O., Ozdemir, Y., Cosar, C. B. & Kural, G. Lipoprotein (a) in Behçet’s disease as an indicator of disease activity and in thrombotic complications. Eur. J. Ophthalmol. 11, 62–65 (2001).
Leiba, M. et al. Thrombophilic factors are not the leading cause of thrombosis in Behçet’s disease. Ann. Rheum. Dis. 63, 1445–1449 (2004).
Ricart, J. M., Vaya, A., Santaolaria, M., Espana, F. & Aznar, J. Dyslipidaemia in Behçet’s disease as a thrombotic risk factor. Ann. Rheum. Dis. 65, 1248–1249 (2006).
Lenk, N., Ozet, G., Alli, N., Coban, O. & Erbasi, S. Protein C and protein S activities in Behçet’s disease as risk factors of thrombosis. Int. J. Dermatol. 37, 124–125 (1998).
Nalcaci, M. & Pekcelen, Y. Antithrombin III, protein C and protein S plasma levels in patients with Behçet’s disease. J. Int. Med. Res. 26, 206–208 (1998).
Espinosa, G. et al. Vascular involvement in Behçet’s disease: relation with thrombophilic factors, coagulation activation, and thrombomodulin. Am. J. Med. 112, 37–43 (2002).
Guermazi, S., Hamza, M. & Dellagi, K. Protein S deficiency and antibodies to protein S in patients with Behçet’s disease. Thromb. Res. 86, 197–204 (1997).
Alkaabi, J. K., Gravell, D., Al-Haddabi, H. & Pathare, A. Haemostatic parameters in patients with Behçet’s disease. Sultan Qaboos Univ. Med. J. 14, e190–e196 (2014).
Demirer, S. et al. Haemostasis in patients with Behçet’s disease. Eur. J. Vasc. Endovasc. Surg. 19, 570–574 (2000).
Conway, E. M. & Rosenberg, R. D. Tumor necrosis factor suppresses transcription of the thrombomodulin gene in endothelial cells. Mol. Cell. Biol. 8, 5588–5592 (1988).
Lentz, S. R., Tsiang, M. & Sadler, J. E. Regulation of thrombomodulin by tumor necrosis factor-ɑ: comparison of transcriptional and posttranscriptional mechanisms. Blood 77, 542–550 (1991).
Navarro, S. et al. Activated protein C levels in Behçet’s disease and risk of venous thrombosis. Br. J. Haematol. 126, 550–556 (2004).
Koşar, A., Haznedaroglu, I. C., Buyukasik, Y., Kirazli, S. & Dundar, S. V. Activated protein C resistance in Behçet’s disease. Rheumatol. Int. 17, 249–250 (1998).
Gül, A. et al. Coagulation factor V gene mutation increases the risk of venous thrombosis in Behçet’s disease. Br. J. Rheumatol. 35, 1178–1180 (1996).
Verity, D. H. et al. Factor V Leiden mutation is associated with ocular involvement in Behçet disease. Am. J. Ophthalmol. 128, 352–356 (1999).
Batioglu, F., Atmaca, L. S., Karabulut, H. G. & Beyza Sayin, D. Factor V Leiden and prothrombin gene G20210A mutations in ocular Behçet disease. Acta Ophthalmol. Scand. 81, 283–285 (2003).
Dagan, E. et al. Vascular Behcet and mutations in thrombogenic genes: methylene tetrahydrofolate reductase, factor V, and prothrombin. Genet. Test. Mol. Biomark. 16, 30–35 (2012).
Akarsu, M. et al. Increased levels of tissue factor pathway inhibitor may reflect disease activity and play a role in thrombotic tendency in Behçet’s disease. Am. J. Hematol. 68, 225–230 (2001).
Gul, A., Aslantas, A. B., Tekinay, T., Konice, M. & Ozcelik, T. Procoagulant mutations and venous thrombosis in Behçet’s disease. Rheumatology 38, 1298–1299 (1999).
Ricart, J. M. et al. Thrombophilic risk factors and homocysteine levels in Behçet’s disease in eastern Spain and their association with thrombotic events. Thromb. Haemost. 95, 618–624 (2006).
Mejia, J. C., Espinosa, G., Tassies, D., Reverter, J. C. & Cervera, R. Endogenous thrombin potential in Behçet’s disease: relationship with thrombosis and anticoagulant therapy. Clin. Exp. Rheumatol. 32, S67–S71 (2014).
Toydemir, P. B. et al. Effects of factor V gene G1691A, methylenetetrahydrofolate reductase gene C677T, and prothrombin gene G20210A mutations on deep venous thrombogenesis in Behçet’s disease. J. Rheumatol. 27, 2849–2854 (2000).
Sayar, Z., Moll, R., Isenberg, D. & Cohen, H. Thrombotic antiphospholipid syndrome: a practical guide to diagnosis and management. Thromb. Res. 198, 213–221 (2021).
Islam, M. A. et al. Prevalence of antiphospholipid antibodies in Behçet’s disease: a systematic review and meta-analysis. PLoS One 15, e0227836 (2020).
Tokay, S., Direskeneli, H., Yurdakul, S. & Akoglu, T. Anticardiolipin antibodies in Behçet’s disease: a reassessment. Rheumatology 40, 192–195 (2001).
Mader, R., Ziv, M., Adawi, M., Mader, R. & Lavi, I. Thrombophilic factors and their relation to thromboembolic and other clinical manifestations in Behçet’s disease. J. Rheumatol. 26, 2404–2408 (1999).
La Regina, M., Orlandini, F., Prisco, D. & Dentali, F. Homocysteine in vascular Behçet disease: a meta-analysis. Arterioscler. Thromb. Vasc. Biol. 30, 2067–2074 (2010).
Choi, B. O. et al. Homozygous C677T mutation in the MTHFR gene as an independent risk factor for multiple small-artery occlusions. Thromb. Res. 111, 39–44 (2003).
Altinbaş, A. et al. Hyperhomocysteinaemia and activated protein C resistance in Behçet’s disease. J. Intern. Med. 248, 267–268 (2000).
Mungan, A. G., Can, M., Açikgöz, S., Eştürk, E. & Altinyazar, C. Lipid peroxidation and homocysteine levels in Behçet’s disease. Clin. Chem. Lab. Med. 44, 1115–1118 (2006).
Buldanlioglu, S. et al. Nitric oxide, lipid peroxidation and antioxidant defence system in patients with active or inactive Behçet’s disease. Br. J. Dermatol. 153, 526–530 (2005).
Canataroglu, A. et al. Methylenetetrahydrofolate reductase gene C677T mutation and plasma homocysteine level in Behçet’s disease. Rheumatol. Int. 23, 236–240 (2003).
Melikoglu, M., Kural-Seyahi, E., Tascilar, K. & Yazici, H. The unique features of vasculitis in Behçet’s syndrome. Clin. Rev. Allergy Immunol. 35, 40–46 (2008).
Chen, Y., Cai, J. F., Lin, C. H. & Guan, J. L. Demography of vascular Behcet’s disease with different gender and age: an investigation with 166 Chinese patients. Orphanet J. Rare Dis. 14, 88 (2019).
Seyahi, E. et al. Clinical and ultrasonographic evaluation of lower-extremity vein thrombosis in Behcet syndrome: an observational study. Medicine 94, e1899 (2015).
Tuzun, H. et al. Management and prognosis of nonpulmonary large arterial disease in patients with Behçet disease. J. Vasc. Surg. 55, 157–163 (2012).
Ozguler, Y. et al. Clinical course of acute deep vein thrombosis of the legs in Behçet’s syndrome. Rheumatology 59, 799–806 (2020).
Desbois, A. C. et al. Immunosuppressants reduce venous thrombosis relapse in Behçet’s disease. Arthritis Rheum. 64, 2753–2760 (2012).
Seyahi, E., Karaaslan, H., Ugurlu, S. & Yazici, H. Fever in Behçet’s syndrome. Clin. Exp. Rheumatol. 31, 64–67 (2013).
Yazici, H., Seyahi, E., Hatemi, G. & Yazici, Y. Behçet syndrome: a contemporary view. Nat. Rev. Rheumatol. 14, 107–119 (2018).
Celik, S., Yazici, Y., Sut, N. & Yazici, H. Pulmonary artery aneurysms in Behçet’s syndrome: a review of the literature with emphasis on geographical differences. Clin. Exp. Rheumatol. 33, S54–S59 (2015).
Ideguchi, H. et al. Characteristics of vascular involvement in Behçet’s disease in Japan: a retrospective cohort study. Clin. Exp. Rheumatol. 29, S47–S53 (2011).
Chang, H. K. & Kim, J. W. The clinical features of Behcet’s disease in Yongdong districts: analysis of a cohort followed from 1997 to 2001. J. Korean Med. Sci. 17, 784–789 (2002).
Savey, L. et al. Ethnicity and association with disease manifestations and mortality in Behçet’s disease. Orphanet J. Rare Dis. 9, 42 (2014).
Lee, I. et al. Cardiac Behçet disease presenting as aortic valvulitis/aortitis or right heart inflammatory mass: a clinicopathologic study of 12 cases. Am. J. Surg. Pathol. 32, 390–398 (2008).
Tunc, R., Keyman, E., Melikoglu, M., Fresko, I. & Yazici, H. Target organ associations in Turkish patients with Behçet’s disease: a cross sectional study by exploratory factor analysis. J. Rheumatol. 29, 2393–2396 (2002).
Tunc, R., Saip, S., Siva, A. & Yazici, H. Cerebral venous thrombosis is associated with major vessel disease in Behçet’s syndrome. Ann. Rheum. Dis. 63, 1693–1694 (2004).
Karaca, M., Hatemi, G., Sut, N. & Yazici, H. The papulopustular lesion/arthritis cluster of Behçet’s syndrome also clusters in families. Rheumatology 51, 1053–1060 (2012).
Yazıcı, H. & Seyahi, E. Behçet syndrome: the vascular cluster. Turk. J. Med. Sci. 46, 1277–1280 (2016).
Seyahi, E. Behçet’s disease: how to diagnose and treat vascular involvement. Best. Pract. Res. Clin. Rheumatol. 30, 279–295 (2016).
Hetta, H. F. et al. Possible role of regulatory B cells in different Behçet’s disease phenotypes and therapies: first report from Egypt. J. Inflamm. Res. 14, 737–744 (2021).
Zou, J., Luo, D., Shen, Y. & Guan, J. L. Characteristics and phenotype heterogeneity in late-onset Behçet’s syndrome: a cohort from a referral center in China. Clin. Rheumatol. 40, 2319–2326 (2021).
Attia, D. H. S. Behçet’s disease phenotypes and clinical outcomes: a cohort study in Egyptian patients. Reumatol. Clin. 17, 514–520 (2021).
Saadoun, D. et al. Cerebral venous thrombosis in Behçet’s disease. Arthritis Rheum. 61, 518–526 (2009).
Hussein, M. A., Eissa, I. M. & Dahab, A. A. Vision-threatening Behcet’s Disease: severity of ocular involvement predictors. J. Ophthalmol. 2018, 9518065 (2018).
Zou, L. et al. Long-term outcomes of endovascular treatment for aortic pseudoaneurysm in patients with Behçet’s disease. Vascular https://doi.org/10.1177/17085381211063038 (2021).
Tutar, B., Kantarci, F., Cakmak, O. S., Yazici, H. & Seyahi, E. Assessment of deep venous thrombosis in the lower extremity in Behçet’s syndrome: MR venography versus Doppler ultrasonography. Intern. Emerg. Med. 14, 705–711 (2019).
Esatoglu, S. N. et al. Bronchial artery enlargement may be the cause of recurrent haemoptysis in Behçet’s syndrome patients with pulmonary artery involvement during follow-up. Clin. Exp. Rheumatol. 34, 92–96 (2016).
Zhou, J. et al. The clinical features, risk factors, and outcome of aneurysmal lesions in Behcet’s disease. J. Immunol. Res. 2019, 9198506 (2019).
Seyahi, E. et al. Pulmonary artery involvement and associated lung disease in Behçet disease: a series of 47 patients. Medicine 91, 35–48 (2012).
Saadoun, D. et al. Mortality in Behçet’s disease. Arthritis Rheum. 62, 2806–2812 (2010).
Seyahi, E. et al. An outcome survey of 43 patients with Budd-Chiari syndrome due to Behçet’s syndrome followed up at a single, dedicated center. Semin. Arthritis Rheum. 44, 602–609 (2015).
Torgutalp, M. et al. Analysis of vascular involvement in 460 patients with Behçet’s syndrome: clinical characteristics and associated factors. Jt. Bone Spine 89, 105277 (2022).
Alibaz-Oner, F. et al. Behçet disease with vascular involvement: effects of different therapeutic regimens on the incidence of new relapses. Medicine 94, e494 (2015).
Alibaz-Oner, F. et al. Vascular Behçet’s disease: a comparative study from Turkey and France. Clin. Exp. Rheumatol. 40, 1491–1496 (2022).
Alibaz-Oner, F. et al. Post-thrombotic syndrome and venous disease-specific quality of life in patients with vascular Behçet’s disease. J. Vasc. Surg. Venous Lymphat. Disord. 4, 301–306 (2016).
Ugurlu, S. et al. Venous claudication in Behçet’s disease. J. Vasc. Surg. 62, 698–703.e691 (2015).
Aksoy, A. et al. Predictors for the risk and severity of post-thrombotic syndrome in vascular Behçet’s disease. J. Vasc. Surg. Venous Lymphat. Disord. 9, 1451–1459 (2021).
Desbois, A. C. et al. Behcet’s disease in Budd-Chiari syndrome. Orphanet J. Rare Dis. 9, 104 (2014).
Sakr, M. A. et al. Characteristics and outcome of primary Budd-Chiari syndrome due to Behçet’s syndrome. Clin. Res. Hepatol. Gastroenterol. 44, 503–512 (2020).
Akyol, L. et al. Budd-Chiari syndrome in Behçet’s disease: a retrospective multicenter study. Clin. Rheumatol. 41, 177–186 (2022).
Martens, P. & Nevens, F. Budd-Chiari syndrome. United European Gastroenterol. J. 3, 489–500 (2015).
Rossi, G. M., Emmi, G. & Vaglio, A. Hemoptysis in Behçet’s syndrome: from bedside to bench? Intern. Emerg. Med. 13, 467–469 (2018).
Gokturk, A. et al. Increased frequency of obstructive sleep apnea syndrome in Behçet’s syndrome patients with superior vena cava syndrome. Clin. Exp. Rheumatol. 37, 132–136 (2019).
Yesilot, N. et al. Cerebral venous thrombosis in Behçet’s disease compared to those associated with other etiologies. J. Neurol. 256, 1134–1142 (2009).
Uluduz, D. et al. Behçet’s disease as a causative factor of cerebral venous sinus thrombosis: subgroup analysis of data from the VENOST study. Rheumatology 58, 600–608 (2019).
Uluduz, D. et al. Clinical characteristics of pediatric-onset neuro-Behçet disease. Neurology 77, 1900–1905 (2011).
Duman, T. et al. A multicenter study of 1144 patients with cerebral venous thrombosis: the VENOST study. J. Stroke Cerebrovasc. Dis. 26, 1848–1857 (2017).
Prisco, D., Silvestri, E., Di Scala, G. & Emmi, G. Behçet’s disease as a cause of cerebral sinus vein thrombosis: an emerging role. Rheumatology 58, 563–564 (2019).
Aguiar de Sousa, D., Mestre, T. & Ferro, J. M. Cerebral venous thrombosis in Behçet’s disease: a systematic review. J. Neurol. 258, 719–727 (2011).
Seyahi, E. et al. The estimated pulmonary artery pressure can be elevated in Behçet’s syndrome. Respir. Med. 105, 1739–1747 (2011).
Yıldızeli, Ş. et al. Outcomes of patients with Behçet’s syndrome after pulmonary endarterectomy. Thorac. Cardiovasc. Surg. 66, 187–192 (2018).
Tuzun, H. et al. Surgical treatment of pulmonary complications in Behçet’s syndrome. Semin. Thorac. Cardiovasc. Surg. 30, 369–378 (2018).
Hamuryudan, V. et al. Pulmonary artery aneurysms in Behçet syndrome. Am. J. Med. 117, 867–870 (2004).
Saadoun, D. et al. Long-term outcome of arterial lesions in Behçet disease: a series of 101 patients. Medicine 91, 18–24 (2012).
Geri, G. et al. Spectrum of cardiac lesions in Behçet disease: a series of 52 patients and review of the literature. Medicine 91, 25–34 (2012).
Mogulkoc, N., Burgess, M. I. & Bishop, P. W. Intracardiac thrombus in Behçet’s disease: a systematic review. Chest 118, 479–487 (2000).
Emmungil, H. et al. A rare but serious manifestation of Behçet’s disease: intracardiac thrombus in 22 patients. Clin. Exp. Rheumatol. 32, S87–S92 (2014).
Fei, Y. et al. Major vascular involvement in Behçet’s disease: a retrospective study of 796 patients. Clin. Rheumatol. 32, 845–852 (2013).
Vural, U., Kizilay, M. & Aglar, A. A. Coronary involvement in Behçet’s disease: what are its risks and prognosis? (Rare cases and literature review). Braz. J. Cardiovasc. Surg. 34, 749–758 (2019).
Tunaci, A., Berkmen, Y. M. & Gökmen, E. Thoracic involvement in Behçet’s disease: pathologic, clinical, and imaging features. AJR Am. J. Roentgenol. 164, 51–56 (1995).
Bonneville, F. Imaging of cerebral venous thrombosis. Diagn. Interv. Imaging 95, 1145–1150 (2014).
Bradbury, A. W., Milne, A. A. & Murie, J. A. Surgical aspects of Behçet’s disease. Br. J. Surg. 81, 1712–1721 (1994).
Mehdipoor, G., Davatchi, F., Ghoreishian, H. & Arjmand Shabestari, A. Imaging manifestations of Behcet’s disease: key considerations and major features. Eur. J. Radiol. 98, 214–225 (2018).
Erkan, F., Gül, A. & Tasali, E. Pulmonary manifestations of Behçet’s disease. Thorax 56, 572–578 (2001).
Cho, S. B. et al. Detection of cardiovascular system involvement in Behçet’s disease using fluorodeoxyglucose positron emission tomography. Semin. Arthritis Rheum. 40, 461–466 (2011).
Trad, S. et al. 18F-fluorodeoxyglucose-positron emission tomography scanning is a useful tool for therapy evaluation of arterial aneurysm in Behçet’s disease. Jt. Bone Spine 80, 420–423 (2013).
Xi, X. Y. et al. Multiple cardiovascular involvements in Behçet’s disease: unique utility of 18F-FDG PET/CT in diagnosis and follow-up. Eur. J. Nucl. Med. Mol. Imaging 46, 2210–2211 (2019).
Kuzu, A., Köksoy, C., Ozaslan, C., Gürler, A. & Tüzüner, A. Evaluation of peripheral vascular system disorders in vascular symptom-free Behçet’s disease. Cardiovasc. Surg. 4, 381–383 (1996).
Kisacik, B. et al. Investigation of the veins in patients with Behçet’s disease with no known vascular event by Doppler ultrasonography. Rheumatol. Int. 32, 303–306 (2012).
Alibaz-Oner, F., Karatay, E., Akpinar, I. N., Ergun, T. & Direskeneli, H. Evaluation of asymptomatic venous disease by venous Doppler ultrasonography in patients with Behcet’s disease without overt thrombosis. Clin. Rheumatol. 33, 277–280 (2014).
Ambrose, N., Pierce, I. T., Gatehouse, P. D., Haskard, D. O. & Firmin, D. N. Magnetic resonance imaging of vein wall thickness in patients with Behçet’s syndrome. Clin. Exp. Rheumatol. 32, S99–S102 (2014).
Alibaz-Oner, F. et al. Venous vessel wall thickness in lower extremity is increased in male patients with Behcet’s disease. Clin. Rheumatol. 38, 1447–1451 (2019). This is the first controlled Doppler ultrasonography study showing increased venous vessel wall thickness of lower-extremity veins in male patients with Behçet syndrome compared with male healthy controls or male patients affected by ankylosing spondylitis.
Seyahi, E. et al. Increased vein wall thickness in Behçet disease. J. Vasc. Surg. Venous Lymphat. Disord. 7, 677–684.e672 (2019). This study showed an increased vein wall thickness of proximal deep and superficial lower-extremity veins in patients with Behçet syndrome without any clinical and radiological vascular involvement.
Kaymaz, S. et al. Ultrasonographic measurement of the vascular wall thickness and intima-media thickness in patients with Behçet’s disease with symptoms or signs of vascular involvement: a cross-sectional study. Arch. Rheumatol. 36, 258–266 (2021).
Tezcan, D. et al. Diagnostic performance of lower extremity venous wall thickness and laboratory findings in the diagnosis of the Behçet disease. J. Clin. Rheumatol. 28, e521–e527 (2022).
Agackiran, S. K. et al. Pulmonary arterial wall thickness is increased in Behçet’s disease patients with major organ involvement: is it a sign of severity? Rheumatology https://doi.org/10.1093/rheumatology/keac452 (2022).
Alibaz-Oner, F. et al. Femoral vein wall thickness measurement: a new diagnostic tool for Behçet’s disease. Rheumatology 60, 288–296 (2021).
Alibaz-Oner, F. et al. Femoral vein wall thickness measurement may be a distinctive diagnostic tool to differentiate Behçet’s disease with intestinal involvement and Crohn’s Disease. Dig. Dis. Sci. 66, 2750–2755 (2021).
Kiafar, M. et al. Diagnosis of Behçet’s disease: clinical characteristics, diagnostic criteria, and differential diagnoses. BMC Rheumatol. 5, 2 (2021).
Atalay, E. et al. A new tool supporting the diagnosis of childhood-onset Behçet’s disease: venous wall thickness. Rheumatology https://doi.org/10.1093/rheumatology/keac314 (2022).
Lawton, G., Bhakta, B. B., Chamberlain, M. A. & Tennant, A. The Behçet’s disease activity index. Rheumatology 43, 73–78 (2004).
Forbess C, Swearingen, C. & Yazici, Y. Behçet’s syndrome activity score (BSAS): a new disease activity assessment tool, composed of patient-derived measures only, is strongly correlated with the Behçet’s disease current activity form (BDCAF). Arthritis Rheum. 58, 854 (2008).
Sharquie, K. E., Najim, R. A. & Abu-Raghif, A. R. Dapsone in Behçet’s disease: a double-blind, placebo-controlled, cross-over study. J. Dermatol. 29, 267–279 (2002).
Shahram, F. et al. Comparison of existing disease activity indices in the follow-up of patients with Behçet’s disease. Mod. Rheumatol. 19, 536–541 (2009).
Hatemi, G. et al. Current status, goals, and research agenda for outcome measures development in Behçet syndrome: report from OMERACT 2014. J. Rheumatol. 42, 2436–2441 (2015).
Gilworth, G. et al. Development of the BD-QoL: a quality of life measure specific to Behçet’s disease. J. Rheumatol. 31, 931–937 (2004).
Kahn, S. R., Partsch, H., Vedantham, S., Prandoni, P. & Kearon, C. Definition of post-thrombotic syndrome of the leg for use in clinical investigations: a recommendation for standardization. J. Thromb. Haemost. 7, 879–883 (2009).
Hatemi, G. et al. Core set of domains for outcome measures in Behçet’s syndrome. Arthritis Care Res. 74, 691–699 (2022).
Sut, N., Seyahi, E., Yurdakul, S., Senocak, M. & Yazici, H. A cost analysis of Behçet’s syndrome in Turkey. Rheumatology 46, 678–682 (2007).
Hatemi, G. et al. 2018 update of the EULAR recommendations for the management of Behcet’s syndrome. Ann. Rheum. Dis. 77, 808–818 (2018). EULAR recommendations for the treatment of Behçet syndrome.
Ozguler, Y. et al. Management of major organ involvement of Behçet’s syndrome: a systematic review for update of the EULAR recommendations. Rheumatology 57, 2200–2212 (2018).
Emmi, G. et al. Adalimumab-based treatment versus disease-modifying antirheumatic drugs for venous thrombosis in Behçet’s syndrome: a retrospective study of seventy patients with vascular involvement. Arthritis Rheumatol. 70, 1500–1507 (2018).
Alpsoy, E., Leccese, P., Emmi, G. & Ohno, S. Treatment of Behçet’s disease: an algorithmic multidisciplinary approach. Front. Med. 8, 624795 (2021).
Aksoy, A. et al. Efficacy of TNFα inhibitors for refractory vascular Behçet’s disease: a multicenter observational study of 27 patients and a review of the literature. Int. J. Rheum. Dis. 23, 256–261 (2020).
Ahn, J. K., Lee, Y. S., Jeon, C. H., Koh, E. M. & Cha, H. S. Treatment of venous thrombosis associated with Behcet’s disease: immunosuppressive therapy alone versus immunosuppressive therapy plus anticoagulation. Clin. Rheumatol. 27, 201–205 (2008). This retrospective study suggests that immunosuppressive therapy is essential for the treatment of deep venous thrombosis associated with Behçet syndrome.
Vautier, M. et al. Direct oral anticoagulant for venous thrombosis in Behçet’s syndrome. Autoimmun. Rev. 20, 102783 (2021). This is an observational study on the role of anticoagulation for the treatment of vascular thrombosis in Behçet syndrome.
Hamzaoui, A. et al. Vena cava thrombosis in Behçet’s disease. Anadolu Kardiyol. Derg. 14, 292–293 (2014).
Oblitas, C. M. et al. Chronic Budd-Chiari syndrome in Behçet’s disease successfully managed with transjugular intrahepatic portosystemic shunt: a case report and literature review. Clin. J. Gastroenterol. 13, 572–578 (2020).
Shi, J. et al. Cerebral venous sinus thrombosis in Behçet’s disease: a retrospective case-control study. Clin. Rheumatol. 37, 51–57 (2018).
Le Thi Huong, D. et al. Arterial lesions in Behçet’s disease. A study in 25 patients. J. Rheumatol. 22, 2103–2113 (1995).
Hamuryudan, V. et al. Pulmonary arterial aneurysms in Behçet’s syndrome: a report of 24 cases. Br. J. Rheumatol. 33, 48–51 (1994).
Saba, D. et al. Arterial lesions in Behçet’s disease. Vasa 32, 75–81 (2003).
Desbois, A. C. et al. Efficacy of anti-TNF alpha in severe and refractory major vessel involvement of Behcet’s disease: a multicenter observational study of 18 patients. Clin. Immunol. 197, 54–59 (2018).
Hamuryudan, V. et al. Pulmonary artery involvement in Behçets syndrome: effects of anti-Tnf treatment. Semin. Arthritis Rheum. 45, 369–373 (2015).
Chan, E., Sangle, S. R., Coghlan, J. G. & D’Cruz, D. D. Pulmonary artery aneurysms in Behçet’s disease treated with anti-TNFα: a case series and review of the literature. Autoimmun. Rev. 15, 375–378 (2016).
Yang, S. S. et al. Peripheral arterial involvement in Behcet’s disease: an analysis of the results from a Korean referral center. Rheumatol. Int. 33, 2101–2108 (2013).
Koksoy, C. et al. Surgical treatment of peripheral aneurysms in patients with Behcet’s disease. Eur. J. Vasc. Endovasc. Surg. 42, 525–530 (2011).
Zhong, H. et al. Efficacy and safety of tocilizumab in Behçet’s syndrome with refractory arterial lesions: a single-centre observational cohort study in China. Rheumatology 61, 2923–2930 (2022).
Liu, J. et al. A pilot study of tofacitinib for refractory Behçet’s syndrome. Ann. Rheum. Dis. 79, 1517–1520 (2020).
Chung, S. W. et al. Surgical experience of Behcet’s disease involving the peripheral artery. Ann. Vasc. Surg. 69, 246–253 (2020).
Gaudric, J. et al. Factors influencing the recurrence of arterial involvement after surgical repair in Behçet disease. J. Vasc. Surg. 72, 1761–1769 (2020).
Park, M. C., Hong, B. K., Kwon, H. M. & Hong, Y. S. Surgical outcomes and risk factors for postoperative complications in patients with Behcet’s disease. Clin. Rheumatol. 26, 1475–1480 (2007).
Tüzün, H. et al. Management of aneurysms in Behçet’s syndrome: an analysis of 24 patients. Surgery 121, 150–156 (1997).
Elgengehy, F. T. et al. Vasculitis damage index in Behçet’s disease. Adv. Rheumatol. 61, 33 (2021).
Author information
Authors and Affiliations
Contributions
G.E. and A.B. researched data for the article. All authors contributed substantially to discussion of the content, wrote the article, and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
F.A.-O. has received honoraria, consulting or speaker fees from Pfizer, AbbVie and Amgen. H.D. has received honoraria, consulting and speaker fees from AbbVie, Pfizer, Roche, Novartis, UCB Pharma, Amgen and Celltrione. G.E. has received honoraria and speaker fees from Novartis, Roche, Sobi, AstraZeneca, Boehringer Ingelheim, Janssen, Sanofi and GSK. G.H. has received research grants, honoraria and speaker fees from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Celltrion, Janssen, Novartis, Pfizer, Silk Road Therapeutics and UCB Pharma. D.S. has received honoraria, consulting or speaker fees from Novartis, Amgen, Celltrion, Celgene, Roche Chugai, Viatris, Sanofi and AbbVie. E.S. has received honoraria, consulting or speaker fees from Novartis, Pfizer and AbbVie. A.B. and D.P. declare no competing interests.
Peer review
Peer review information
Nature Reviews Rheumatology thanks J.-L. Guan, J. van Laar and N. Ambrose for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bettiol, A., Alibaz-Oner, F., Direskeneli, H. et al. Vascular Behçet syndrome: from pathogenesis to treatment. Nat Rev Rheumatol 19, 111–126 (2023). https://doi.org/10.1038/s41584-022-00880-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-022-00880-7
This article is cited by
-
Endovascular repair with a physician-modified fenestrated endograft to treat abdominal aortic pseudoaneurysm with Behcet’s disease: a case report
Journal of Cardiothoracic Surgery (2024)
-
Hypertension as a prominent manifestation secondary to renal artery lesions in pediatric Behcet’s disease
Pediatric Rheumatology (2024)
-
Increased inferior vena cava wall thickness as a sign of extensive venous inflammation in Behçet’s Disease
Clinical Rheumatology (2024)
-
Progress of nanomaterials in the treatment of thrombus
Drug Delivery and Translational Research (2024)
-
The impact of Behcet syndrome on total knee arthroplasty outcomes: a retrospective matched cohort study
International Orthopaedics (2023)