Abstract
Historically, rheumatic diseases have not received much attention in Africa, particularly in sub-Saharan Africa, possibly owing to a focus on the overwhelming incidence of infectious diseases and the decreased life span of the general population in this region. Global attention and support, together with better health policies and planning, have improved outcomes for many infectious diseases; thus, increasing attention is being turned to chronic non-communicable diseases. Rheumatic diseases were previously considered to be rare among Africans but there is now a growing interest in these conditions, particularly as the number of rheumatologists on the continent increases. This interest has resulted in a growing number of publications from Africa on the more commonly encountered rheumatic diseases, as well as case reports of rare diseases. Despite the limited amount of available data, some aspects of the epidemiology, genetics and clinical and laboratory features of rheumatic diseases in African populations are known, as is some detail on the use of therapeutics. Similarities and differences in these conditions can be seen across the multi-ethnic and genetically diverse African continent, and it is hoped that increased awareness of rheumatic diseases in Africa will lead to earlier diagnosis and better outcomes for patients.
Key points
-
In the past, there has been an emphasis on communicable diseases in Africa, but attention has now shifted towards non-communicable diseases such as rheumatic diseases.
-
Common rheumatic diseases are seen in Africa and are both comparable and different from presentations seen outside of Africa.
-
Diverse genetic and environmental factors affect the presentation of common rheumatic diseases among different African nations.
-
A shortage of appropriately trained staff, laboratory testing capacity and effective medications exists across the whole continent.
-
Advocacy and research are needed to increase awareness of the risk factors, presentations and management of rheumatic diseases in Africa.
-
Specialized treatment guidelines are needed for resource-poor countries in Africa.
Similar content being viewed by others
Introduction
The growing burden of rheumatic diseases has been well documented all over the world1; however, there is relatively little information from Africa, particularly sub-Saharan Africa, and the limited health resources of many African countries are prioritized to address the challenges of infectious and communicable diseases. Non-communicable diseases, including rheumatic diseases, also contribute to poor health outcomes in Africa and are starting to receive more attention. Within this sphere, rheumatology has emerged as a slowly growing discipline in Africa. Over the past two decades, there have been an increasing number of reports of rheumatic diseases from all over Africa. The presence of a wide spectrum of rheumatic diseases and the challenges associated with their diagnosis and management has been previously reviewed elsewhere2,3,4. The extent of the burden of rheumatic diseases in Africa is unknown as there are limited epidemiological data; however, many patients with rheumatic diseases present to health-care facilities all over the continent. The burden of rheumatic diseases in Africa is probably greater than in other parts of the world in terms of morbidity and mortality, as patients often present at a later stage of disease3,5.
The purpose of this Review is to provide an overview of the common types of chronic inflammatory arthritis (gout, rheumatoid arthritis (RA) and spondyloarthritis (SpA)) and connective tissue diseases (systemic lupus erythematosus (SLE) and systemic sclerosis (SSc)) reported among adults in Africa. To do so, we reviewed all the available publications from Africa in each of these diseases and selected studies in which there were sufficient data to permit comparison among the studies and with studies from other parts of the world. However, only limited data are available for some of these diseases or for some aspects of the diseases in different regions of Africa. As a result, we are unable to provide comparative data for all aspects of these diseases. In this Review, we also highlight the progress and challenges related to the study, diagnosis and management of rheumatic diseases in such a geographically vast and ethnically diverse continent as Africa, and discuss opportunities and advances made in the training of rheumatologists in Africa.
Gout
Gout has received increasing global attention as it has emerged as the most common cause of inflammatory arthritis in many parts of the world6. In Africa, however, many patients with gout currently present to primary care practitioners, who might not document them or might even miss the diagnosis. Thus, it is important to raise awareness of the occurrence of gout in Black Africans so that patients can be correctly diagnosed and receive appropriate treatment at an earlier stage.
Prevalence and risk factors
Before 1980, gout was uncommonly reported in Black Africans, and early reports comprised only small case series7,8. However, since then, an increasing number of publications on gout have emanated from all over Africa. Many factors are likely to be responsible for the increased number of reports of larger series of patients with gout, including urbanization, the adoption of a Western lifestyle, increased alcohol consumption and the rising incidence of obesity, hypertension, diabetes and renal disease in African populations9,10,11.
Limited epidemiological data are available on the prevalence of hyperuricaemia and gout in Africa. Clinical and radiographic surveys conducted in the 1970s of 1,185 Black individuals in a rural setting and of 424 Black individuals in an urban setting in South Africa failed to detect any patients with gout12,13. The authors also found that the mean serum uric acid levels were significantly higher in the urban community than in the rural community (P < 0.001)12,13. Subsequent community-based studies of rural and semi-urban populations have shown that gout is uncommon. The prevalence of gout was 0.1% in a survey of 2,484 people in a semi-urban setting in Nigeria, 0.06% in a survey of 1,500 people in a rural setting in the Democratic Republic of Congo (DRC) and 0.29% in a survey of 5,120 people in Egypt14,15,16.
A genetic study of 46 South African patients with gout showed a statistically significant association with HLA-B14 alleles in patients with primary gout compared with healthy individuals9. To date, there have not been any other studies investigating the relationship between genetics and gout in Africans, which is not surprising given that Africans have a wide genetic diversity. The findings from some of the larger studies on gout from different parts of Africa9,10,11,17,18,19,20 are shown in Table 1, including the prevalence of hypertension, obesity, diabetes, alcohol intake, kidney disease and diuretics (where this information was available). Alcohol intake ranged from 67% to 83% in most studies and is probably an important risk factor, except in Mali and Nigeria, where there was a lower prevalence of alcohol use of 5% and 17.8%, respectively9,10,11,17,18,19,20. This low rate of alcohol use might be attributable to abstinence on religious grounds. The other major comorbidities and risk factors identified in the studies were obesity, hypertension and the use of diuretics. One study also included a case–control analysis and found that obesity, ‘white collar’ occupation, hypertension and alcohol intake were risk factors for men, whereas alcohol intake was the only statistically significant risk factor for women10.
Demographics, presentation and management
As most of the studies in Table 1 report data from hospital-based patients, the disease described is often a more severe form. The mean age at presentation ranged from 47.5 to 55 years in most studies, with a slightly younger age of 44 years reported in Togo11, and there was a delay of between 3.4 and 7.5 years before patients presented to hospital. A wide variation exists in the sex distribution of patients among the studies, with most showing a higher prevalence of gout in men; however, an almost equal number of men and women were reported in Cameroon, and a greater number of women than men had gout in Mali17,19. Although most patients had a monoarticular or oligoarticular presentation, 27–44% of patients had polyarticular involvement. The joints most commonly involved were the large joints such as the knees and ankles and, less often, the first metatarsophalangeal joints. A lower prevalence of tophi occurred in Mali and Nigeria (4.0% and 6.2%, respectively), whereas tophi occurred in between 21.9% and 51% of individuals in most of the other studies. In many patients, the tophi are large and can be numerous. Little information is currently available on the socioeconomic effects of gout, quality of life, course of the disease and adherence and response to therapy. Treatment is mostly with NSAIDs, colchicine and glucocorticoids for acute attacks, and although the urate-lowering therapies allopurinol and probenecid are available, febuxostat is only available in some African countries. Drugs such as pegloticase, rilonacept and canakinumab are unavailable. A clear need exists to treat gout at an early stage — an approach that would be of good economic benefit to the governments concerned — and there is also a need for longitudinal studies on the outcomes of gout.
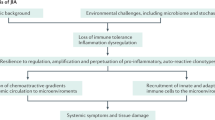
Rheumatoid arthritis
Although RA was first recognized as a distinct entity in 1800 (ref.21), it was only in 1956 that the first two cases of RA were reported in Black Africans in Malawi22. Subsequently, small case series from Zimbabwe, Uganda, Kenya, Nigeria and Lesotho were published5,23. However, since then, larger series of patients with RA have been reported from all regions of Africa. The reasons for these observations are probably multifactorial and include the increasing urbanization of the population, improvements in access to health services, a greater awareness of the disease alongside the development of rheumatology services in major academic centres and the possibility that autoimmune diseases such as RA are truly emerging diseases on the African continent. The increase in number of patients with RA has provided an opportunity to study the clinical expression, serological manifestations, disease course, response to treatment and outcomes compared with patients from other ethnic groups around the world.
Prevalence and risk factors
Limited epidemiological data are available on the prevalence of RA in Africa. A systematic review on the burden of RA in Africa published in 2012 noted that there were limited epidemiological data on the prevalence of RA in Africa24. Similarly, a meta-analysis on the prevalence of arthritis in Africa in 2015 found that there was a paucity of prevalence data on arthritis25. Table 2 shows a summary of the published population-based epidemiological studies on RA and describes the setting in which each study was conducted14,26,27,28,29,30,31,32,33,34,35. Most of the studies shown in Table 2 had small numbers of participants, ranging from 543 to 1,070. In 1975, a South African study reported a prevalence of RA of 0.90% in an urban Black population, which was similar to the ~1% prevalence of RA reported in most parts of the world27. However, the picture seems quite different in rural populations. In the same year, another South African study reported a prevalence of RA of only 0.12% in a rural Black population28. A 1993 survey of 1,994 people in rural Nigeria failed to detect any patients with RA32 and, similarly, a 2017 study of a semi-urban Nigerian population identified only three individuals with RA (0.12%) among the 2,454 people studied14. Other studies with larger numbers of participants reported prevalence of 0.29% in Egypt and 0.60% in the DRC33,34. These findings are similar to observations in other parts of the world, where the prevalence of RA ranges from 0.2% to 0.5% in most rural communities in low-income and middle-income countries16. An Algerian study of 52,504 urban residents also reported a low prevalence of 0.13%35.
Early genetic studies showed that an increased susceptibility to RA was associated with different alleles of HLA-DRB1 (ref.36). In 1987, Gregersen et al. found that these alleles carried the ‘shared epitope’ (a common sequence of five amino acids at positions 70–74), which was associated with increased susceptibility to RA37. Studies from South Africa and Zimbabwe have reported a genetic association between HLA-DR4 and RA in Black individuals23. Genetic studies from Nigeria showed that HLA-DR4 was present in <1% of the population, suggesting that different genetic factors are associated with RA in different populations38. In the DRC, the prevalence of HLA-DRB1*04:01 alleles is low among both patients with RA and healthy individuals, but there is a higher prevalence of other HLA-DRB1 alleles, suggesting a different genetic risk profile compared with patients in Southern Africa and those of European ancestry39. A study from Cameroon confirmed the association between susceptibility to RA and HLA-DRB1-shared epitope alleles; however, the allele frequency was only 30%, which is much lower than the 50–70% reported in individuals with European ancestry40. Genome-wide association studies have revealed over 100 susceptibility loci that have important variations among different ethnic groups36. A high-resolution HLA-typing study in 266 Black patients with RA from South Africa revealed an increased risk of RA in patients with a histidine at position 13 or a valine at position 11 of the third hypervariable region of the beta chain of HLA-DRB1 (ref.41). Conversely, alleles that carried a serine at position 11 conferred protection in this population. These findings are in agreement with the earlier observations in North America and Europe42. Outside the HLA region, a polymorphism in PTPN22 is associated with the highest risk of RA in patients of European ancestry43. However, this gene was non-polymorphic in Black South Africans and therefore not associated with RA in this population44. Previous studies have acknowledged that despite Africa having the highest genetic diversity in the world, very few genetic studies in African populations have been published45,46. As highlighted by these findings, a great need exists for large-scale genetic studies across Africa. Such studies will help researchers to identify the similarities and differences within African populations compared with other populations, and to understand the role of genetic factors in disease severity and response to drugs such as methotrexate.
Environmental risk factors for RA include smoking, which is linked to the development of RA and is associated with more severe disease47. A low prevalence of smoking has been reported in African countries including Sudan (1.2%) and the DRC (1.6%)39,48. However, a South African study noted a likely under-reporting of smoking, as many patients had high nicotine levels, despite reportedly being non-smokers49. In addition, many of the patients in this study were using smokeless tobacco, which can be sniffed, sucked, chewed or just applied to the teeth or gums50. The use of smokeless tobacco varies widely in Africa, ranging from 24.7% in men and 19.6% in women in Madagascar, to 3.8% in men and 0.5% in women in Nigeria, and 0.03% in men and 0.31% in women in Burundi51. Although smokeless tobacco is also considered a risk factor for RA, a Swedish study of 1,998 patients with RA and 2,252 healthy individuals did not find any increase in moist snuff (smokeless tobacco) users among those with RA52. Further studies are required to determine whether smokeless tobacco is associated with an increased risk and/or severity of RA. Another environmental risk factor for RA is periodontal infection, which shows a significant association with RA in many systemic reviews and meta-analysis studies53,54. Statistically significant associations between periodontal infection and RA have also been reported in studies from Senegal and Sudan55,56.
Demographics, presentation and management
The reported manifestations of RA varied in early studies in Africa, but seemed to be characterized by a young age at onset, a low prevalence of subcutaneous nodules and extra-articular manifestations, and mild disease with less severe radiographic changes5,23. Many studies involving larger numbers of patients have been published from all over Africa in the past two decades39,40,48,57,58,59,60,61,62,63, the results of which are summarized in Table 3. Most of the studies in Table 3 show a higher prevalence of RA in women than in men, with a ratio of nearly 6:1, which is greater than the ratio of 3:1 in patients of European descent64. Long delays often occurred before referral to a specialist, ranging from 3.0 years to 12.9 years. As a result of a delay in referral, untreated or inadequately treated active disease results in high disease activity, greater functional impairment and more severe joint damage. Notably, the shorter mean duration of 11 months (standard deviation (s.d.) 7.1 months) in the 2012 study in South Africa resulted from the inclusion of only patients with early RA (disease duration of <2 years)58.
Subcutaneous nodules are among the most common extra-articular manifestations and occur in up to 30% of patients with RA across Africa (Table 3); however, low prevalence of subcutaneous nodules (3.0–14.4%) was reported in Senegal, the DRC, Cameroon, Egypt and Kenya39,40,59,62,63. The prevalence of rheumatoid factor is low in the DRC (34.7%) and Nigeria (38.7%)40,60, but is nearly 80% in South Africa, Senegal, Algeria and Kenya, similar to reports in most European and North American populations58,59,61,63. Early radiographic studies from Africa noted that erosions were uncommon; however, most of the reports shown in Table 3 found erosions in nearly 50% of patients. Compared with the early observations of low disease activity, all the studies in Table 3 show the presence of moderate or high disease activity based on the 28-joint disease activity score.
The most commonly used DMARD to treat RA is methotrexate, which is often used in combination with hydroxychloroquine or chloroquine. Biologic DMARDs (bDMARDs) are not available in most public-sector hospitals and are used only by patients with private health insurance or those who can afford to pay for them (Box 1), as exemplified by data from the South African Biologics Registry, which mostly comprises patients with private health insurance65.
Analysis of the reports of RA in Africa show that patients with RA often present at a later stage in the course of their disease. Therefore, many patients already have erosive arthritis with considerable functional limitation at presentation. Heterogeneity exists with respect to age of onset, extent of female predominance, prevalence of subcutaneous nodules, seropositivity and genetic associations in different parts of Africa. For RA, there is an urgent need to raise awareness and promote education and training of health professionals so that patients are diagnosed and treated at an early stage and so that better outcomes can be achieved for patients.
Spondyloarthritis
Although SpA is commonly reported in North African countries and among white individuals, people of Indian descent and mixed ethnicity populations in South Africa, it is rarely reported among Black Africans. This rarity might be due to the low prevalence of HLA-B27, an important genetic risk factor for certain types of SpA, in Black Africans (<1%) compared with the prevalence of 3–5% in North Africans and 8% in patients with European ancestry66. The association between HLA-B27 and SpA, particularly ankylosing spondylitis (AS), might be more complex in Black Africans. Although higher frequencies of HLA-B27 have been reported in certain ethnic groups in Gambia (up to 7.8%), and in Mali (9.7%), AS is rarely seen in these populations67,68. A prospective survey among 900 adult Fula men in Gambia (of whom 6 of the 100 tested were HLA-B27 positive) did not identify any patients with AS69. Greater awareness of SpA in Africa is needed, as is further research into genetic heterogeneity among different ethnic groups.
Prevalence and risk factors
Few community studies on SpA have been performed in African countries, with the most notable being the Community-Oriented Program for Control of Rheumatic Diseases (COPCORD) studies, in which Egypt had an overall prevalence of SpA of 0.15%70. The prevalence of AS in Egypt was reported in another COPCORD study to be 0.09%, whereas the DRC had a prevalence of SpA of 3.8%15,16. No cases of SpA were reported in other studies in Nigeria and Gambia14,69. Hospital-based studies in rheumatology clinics in Central African countries also noted that AS was uncommon71,72. Studies of patients seen in rheumatology clinics identified only 3 with AS among 2,370 patients in Kinshasa, DRC, 4 patients with AS among 10,000 patients in Brazzaville, Congo and 8 patients with AS among 9,065 patients in Togo71,72,73. A prospective survey of 984 rheumatology outpatients in the DRC found 105 (10.7%) with SpA; the sub-types were non-radiographic axial SpA (5.0%), reactive arthritis (4.3%), AS (1%) and psoriatic arthritis (0.1%)74.
The prevalence of HLA-B27 is 90–95% in patients of European ancestry with AS, compared with only 29–64% in individuals from Algeria, Egypt, Morocco and Tunisia with the disease75,76,77,78. One study from Togo has reported an association between HLA-B14:03 and AS in Black Africans, but this association has not yet been verified in other studies73. Interestingly, an upsurge of SpA accompanied outbreaks of HIV infection in East Africa and Southern Africa79, suggesting HIV infection could be a risk factor for some types of SpA, in particular reactive arthritis and undifferentiated SpA.
Demographics, presentation and management
An audit of 518 patients with SpA in three North African countries (Tunisia, Algeria and Morocco) did not reveal much difference from data from Europe on SpA80. The mean age at onset in this study was 26.6 years (s.d. 10.7 years). The male-to-female ratio was 3:1, and inflammatory back pain was reported in 90% of the cohort. Symptoms of sacroiliitis were reported by 97% of patients, whereas peripheral oligoarthritis was reported by 42% and dactylitis by 10%. However, extra-articular features were infrequently reported; uveitis occurred in 13%, psoriasis in 6% and inflammatory bowel disease in 3%80. In a separate Algerian study, a mean delay of 4.3 years occurred before a diagnosis could be made, and there was a high frequency of hip involvement, which differed from what is usually seen among Europeans81. Although commonly reported in North Africans, familial occurrence has rarely been documented in South Africa82. In addition, non-radiographic axial SpA has been documented in North African countries, the DRC and in South Africa74,82.
The Assessment of Spondyloarthritis International Society criteria for diagnosing early axial disease have been suggested to not be particularly useful in Black individuals because of the low frequency of HLA-B27 in this population. The limited availability and high cost of MRI in Africa also makes implementing the criteria difficult. Conventional synthetic DMARDs were available to patients in all the aforementioned studies, whereas only 14% of patients with SpA in Egypt received bDMARDs76. The 2016 Assessment of Spondyloarthritis International Society–EULAR management recommendations for axial SpA note that, in principle, conventional synthetic DMARDs should not be used for purely axial disease83. Although sulfasalazine, methotrexate and leflunomide are not effective for axial symptoms, they can be used in exceptional situations where no other treatment option is available owing to toxicity, contraindications or costs. Therefore, in the absence of access to bDMARDs, patients with purely axial symptoms in African countries cannot currently be treated adequately.
Systemic sclerosis
SSc (also known as scleroderma) is a rare autoimmune rheumatic disease in which cutaneous and visceral organ fibrosis and vasculopathy are the predominant features. Historically, one of the ground-breaking observations in SSc research was made in Africa. Robert Goetz, a vascular surgeon working in Cape Town, South Africa in 1945, was the first to show in autopsy studies that the disease is not confined to the skin and that fibrotic and vascular changes occur in several visceral organs84. He coined the term ‘progressive systemic sclerosis’ in preference to ‘scleroderma’. Subsequently, the term ‘systemic sclerosis’ was adopted as the most appropriate description of the disorder as the disease is not ‘progressive’ in all individuals.
Prevalence and risk factors
Except for some small studies in South Africa, which have shown that underground gold miners have around a 25-fold higher annual incidence of SSc than the general population (7.73–8.1 per 10,000 versus 0.33 per 10,000)85,86, there have been no formal epidemiological studies in Africa. To date, none of the COPCORD studies in rural Africa has reported any cases of SSc. Although familial clustering of SSc is uncommon, the interplay of genetic factors and environmental triggers is known to be important in the aetiopathogenesis of SSc87. The seminal work of L.D. Erasmus in 1957 showed that white gold miners exposed to silica were at an increased risk of developing SSc88; observations that were subsequently confirmed in Black gold miners in South Africa85. Only a handful of studies have been performed on genetic risk factors for SSc in Africans, and in the only study to date on HLA associations with SSc, HLA-DRB1*15:01 was associated with SSc overall in South Africans, HLA-DQB1*03:01 was associated with diffuse cutaneous SSc (dcSSc) and HLA-DRB*11:01 was associated with anti-U3RNP antibodies89.
Demographics, presentation and management
A distinctive feature of SSc in Africa is that dcSSc is the predominant subset in sub-Saharan Africa90 and in North Africans91,92, whereas limited cutaneous SSc (lcSSc) is more prevalent in white populations. These ethnic differences are mirrored in the USA, where dcSSc is more common than lcSSc in African Americans93. A 2020 systematic review of 1,866 patients with SSc in sub-Saharan Africa based on 90 publications (mainly from South Africa, Nigeria and Senegal) showed that two-thirds of patients have dcSSc and that most patients are female (84%)90. The most striking clinical feature in these patients was the mixed hyper-pigmentary and hypo-pigmentary skin changes, commonly referred to as ‘salt and pepper’ depigmentation94. Raynaud’s phenomenon occurred in 79% of individuals, oesophageal reflux in 70% and interstitial lung disease in ~50%. Digital ulcers, pulmonary hypertension and cardiac involvement were less common, and scleroderma renal crisis was rare.
Antinuclear antibodies (ANAs) were present overall in 65% of individuals, with anti-U3RNP, anti-U1RNP and anti-topoisomerase-1 (Scl-70) antibodies the most common90. The high prevalence of anti-U3RNP antibodies ties in with the predominance of dcSSc and associated ‘salt and pepper’ depigmentation95. By contrast, anti-centromere antibodies are rare96, consistent with lower prevalence of lcSSc in African populations. A report from Tunisia also showed that Raynaud’s phenomenon was more common among those with dcSSc (91%) than in those with lcSSc (43%)92. Anti-centromere antibodies were also uncommon in this population, and renal and cardiac involvement were rarely reported, similar to elsewhere in Africa; however, interstitial lung disease and gastrointestinal manifestations were frequent92.
Treatment of SSc in sub-Saharan Africa has mainly focused on symptom relief, such as NSAIDs for pain relief and proton pump inhibitors for gastro-oesophageal reflux. Glucocorticoids have been prescribed less frequently than NSAIDs to control inflammation, sometimes at high doses of 40–60 mg daily. Other immunosuppressive agents such as methotrexate, cyclophosphamide and azathioprine are rarely prescribed90. No reports have been published on autologous stem cell transplantation in Africa or on the use of agents such as prostanoids or endothelin receptor antagonists for the treatment of pulmonary hypertension. Overall, although SSc is rare in Africa, a need exists for more effective and less costly medications for the treatment of severe skin disease, as well as for the serious vascular and lung complications that are often major causes of morbidity and mortality.
Systemic lupus erythematosus
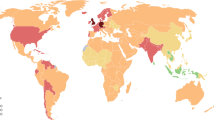
Historically, SLE has rarely been reported among Africans, especially Black Africans. Most of the early reports comprised single cases or small case series. In an article in 1995, Deborah Symmons proposed a gradient theory that suggested that SLE is rare in sub-Saharan Africa and that the prevalence rises moving upwards from North Africa into Europe97, a theory that was corroborated by other analyses98,99. Although early studies found few cases of SLE, subsequent studies have reported larger numbers. This underreporting might have been caused by under-diagnosis, as many individuals with SLE are wrongly diagnosed with infections such as malaria and tuberculosis in areas where these diseases are endemic100.
Prevalence and risk factors
Several rural community COPCORD studies have not documented any patients with SLE14,15,70,101. Similarly, a 1998 study found a cumulative total of only 413 patients with SLE over the period of 1971–1984 in African countries99. However, since 1984, an increasing number of reports of SLE have emerged from all over Africa100,102,103,104,105,106,107,108. A 2020 systematic review and meta-analysis of a pooled population of 28,375 individuals in hospitals revealed a prevalence of SLE of 1.7% (95% CI 0.8–2.9%) across general medicine and rheumatology units109. The authors concluded that there was an increasing prevalence of SLE across sub-Saharan populations109. A study from South Africa had also reported that SLE might be more prevalent in Black Africans than had previously been thought110. This report also identified a high prevalence of comorbid tuberculosis among patients with SLE110.
Although many studies on the genetics of SLE have been performed in other parts of the world, there have been very few studies among Black African populations, even though these populations have wide genetic diversity and complex disease mapping45,46. In addition, the clinical heterogeneity of SLE has led to efforts to identify genetic variants that might account for the different clinical phenotypes of SLE. In a study in South Africa, the prevalence of HLA-DRB1*02 was higher in Black individuals with SLE than in ethnically matched healthy individuals, and HLA-DQB1*02:01 was associated with the presence of anti-Ro antibodies, rather than with SLE itself111. An additive genetic model, rather than environmental factors, has been proposed to be responsible for the differences between Black African, African American and Afro-Caribbean patients with SLE and those of European ancestry112,113. The association between apolipoprotein L1 and non-diabetic renal diseases, such as lupus nephritis, in African Americans might also be applicable to Black Africans114. Looking at epigenetics, a South African study in Black individuals with SLE or SSc revealed more hypomethylated genes in both diseases than in healthy individuals115.
Demographics, presentation and management
The demographic data, clinical manifestations and autoantibody profiles of patients with SLE in Africa, as reported in some of the larger studies published between 2009 and 2020, are shown in Table 4100,102,103,104,105,106,107,108. In a South African study of a multi-ethnic cohort of 408 patients comprising mostly Indians (58.1%) and Black Africans (33.6%), no significant differences were reported in the age at onset or gender between the two groups103. The mean age at presentation ranges from 29.2 years in a large Egyptian study105, to around 33–36 years in most of the other studies105 (Table 4). The female-to-male ratio is overwhelmingly high in many African populations, with ratios of between 18:1 and 32:1 reported in South Africa, Nigeria, Sudan and Kenya100,104,107,108. In addition, there is a striking delay before presentation to a rheumatologist (15.6 months in Tunisia and 30 months in Nigeria). In Egypt there was a similar delay, with the mean age at onset being 25.9 years (s.d. 10.8 years) and the age at the first visit being 29.2 years (s.d. 11.5 years)105. The delay has been attributed to mistaken diagnoses by general practitioners of malarial fever, bacterial infections, tuberculosis and even HIV. Valuable time is therefore lost before these patients are seen by rheumatologists.
The most common manifestations of SLE in the studies included in Table 4 are arthritis (70–90%) and mucocutaneous manifestations (78–82%). Among the cutaneous manifestations, discoid lupus was less common in North Africa (5.4–11.9%) than in sub-Saharan Africa, specifically Nigeria, South Africa and Kenya (22–44%)100,104,108. In the USA, discoid lupus is also more common in African Americans than in white Americans, at a ratio of 5.4:1.0 (refs116,117). A surprisingly low prevalence of photosensitivity was reported in Nigeria (9%) compared with the prevalence in most of the other studies, which ranged from 39% to 68%. Oftentimes, patients with a malar rash or indeed, other skin rashes, apply various astringents to the skin, thus presenting with atypical rashes. The prevalence of renal disease is also high, ranging from 33 to 50% in most of the studies (Table 4).
Autoantibody testing is not readily available in many hospitals, particularly in sub-Saharan Africa. ANAs were found in 97–99% of individuals in all studies in Table 4, except in Kenya, where a lower prevalence of 82% was reported. A study in a cohort of patients with SLE in Nigeria showed a speckled ANA staining pattern to be predominant (77.5%), compared with homogeneous (16.2%), speckled with homogeneous (3.8%) and ribosomal (2.5%) patterns102. Anti-double stranded DNA antibodies were present in 45–55% of patients with SLE in Kenya, Nigeria and South Africa, with a lower prevalence of 35% in Sudan and a higher prevalence of 77–79% in Tunisia and Egypt (Table 4). The prevalence of anti-Sm antibodies was similarly variable, ranging from 22.5% in Egypt to 63.6% in Nigeria. A comparative study of cohorts of patients with SLE from Sudan and Sweden found that anti-histone antibodies and anti-double stranded DNA antibodies were more common in Sweden than in Sudan, whereas anti-Sm antibodies were more common in Sudan than in Sweden107, thus confirming the importance of anti-Sm antibodies in Black populations. Reports from Tunisia have also shown a relatively high occurrence of anti-Sm antibodies, among others118. The ACR–EULAR SLE classification criteria (which are often used for diagnosis) require an ANA titre of 1:80, yet serologies are unavailable in many centres or are too expensive for patients to afford. Therefore, the argument could be made for developing a set of clinical criteria to be used when diagnosing SLE in sub-Saharan Africa that does not require serology, to avoid missing potential patients.
Antimalarial agents such as chloroquine and, to a lesser extent, hydroxychloroquine, are readily available; chloroquine is often prescribed for endemic malarial fever in many African countries. Glucocorticoids are also readily available, as are immunosuppressive agents, such as methotrexate, azathioprine, mycophenolate mofetil and cyclophosphamide, although the cost of such medications can be prohibitive, especially for the majority of patients who pay out of pocket. bDMARDs are mostly unavailable (Box 1).
Challenges and unmet needs
Rheumatic and musculoskeletal diseases have been estimated by the World Health Organization (WHO) to be the second largest cause of disability worldwide, as measured by years lived with disability119. The burden of these diseases is projected to be higher in low-income and middle-income countries owing to limited access to clinical services and treatments120. However, over the past two decades, great strides have been made in the diagnosis and management of rheumatic diseases in Africa, and the number of rheumatologists has increased, albeit from a low base.
Many challenges to the delivery of optimal health-care in Africa exist. Foremost among them is the fact that more than half of the countries in Africa are among the poorest nations in the world121. Many interests compete for the limited health-care resources available, including poverty-associated nutritional diseases, vaccination programmes and the triple burden of HIV, tuberculosis and malaria. A lack of education, low socioeconomic status, limited access to health care and some religious and cultural beliefs also contribute to a reluctance or delay in seeking medical care. Many patients might attribute their illness to cultural influences and seek help from traditional healers or alternative care practitioners. When patients do seek conventional medical attention, they are often seen at community health centres and receive symptomatic treatment only. As such, their condition might worsen and they can lose faith in traditional medical care. In addition, there is often a long delay before a patient is seen by a rheumatologist, during which time they can experience considerable disability and tissue damage. Thus, it is not surprising that many patients, especially those living in rural communities, are seen at an advanced stage of their illness and account for some of the extreme phenotypes that are reported. The possible contribution of genetic factors to this more severe disease still needs to be studied. The African League Against Rheumatism (AFLAR) has provided recommendations on the management of rheumatic diseases during the COVID-19 pandemic122. However, a report from a survey of African rheumatologists concerning the effect of the COVID-19 pandemic on rheumatology practice concluded that rheumatologists are generally avoiding performing physical examinations on patients and are relying mostly on telephone calls, messaging apps or video calls, and that there is a lack of national rheumatology guidelines or registries, as 57% of the respondents reported the presence of specific COVID-19 recommendations, and only 13% confirmed the availability of a national rheumatology COVID-19 registry in their country123.
Human resources
Africa, particularly sub-Saharan Africa, has among the lowest ratios of health-care personnel to the size of the populations in the world124, and there are shortages in all categories of health-care personnel, especially doctors. North African countries and South Africa have a better infrastructure for patients seen in public sector facilities than other African countries, and there is a relatively greater number of doctors and rheumatologists who have access to laboratory tests, imaging facilities and essential medicines. Many countries in Africa do not have any rheumatologists, and others have only a few. Accurate information about the number of rheumatologists in each African country is not available, but on the basis of information provided by rheumatologists in their respective countries, it is estimated that there is about 1 rheumatologist per 110,000 people in Algeria, 1 per 590,000 in South Africa, 1 per 4,120,000 in Nigeria and 1 per 5,300,000 in Kenya (O.A., G.M.M., M.T., O.O. and S.S. unpublished data). As a result, many patients with rheumatic diseases in sub-Saharan Africa are managed by orthopaedic surgeons, internists, family practitioners and at community health-care centres. These practitioners often have limited training and support, which can result in conservative management approaches and in a failure to achieve treatment goals.
Education and training
Rheumatology training programmes have existed for a long time in South Africa, Nigeria and North African countries. Over the past two decades, however, additional training centres have been established in East African countries such as Kenya and in West African countries such as Burkina Faso, Ghana, Senegal and Cameroon. In many countries, rheumatology fellows in training take part in the 2-year EULAR online postgraduate courses, the successful completion of which is a pre-requisite for certification as rheumatologists in the English-speaking West African countries Nigeria, Ghana, Sierra Leone and The Gambia. Planning is currently underway for a EULAR–AFLAR-led webinar series for rheumatology trainees from all over Africa, and there have been major strides in the training of paediatric rheumatologists in Africa, with the formation of a paediatric rheumatology society under AFLAR, known as PAFLAR, that will no doubt help to improve outcomes for children with rheumatic diseases. The major advances in knowledge and management strategies for rheumatic diseases have resulted in improved outcomes for patients in Africa103,125,126.
It is unlikely that there will be enough rheumatologists, or even internists and doctors, to identify and care for patients with rheumatic diseases in Africa; therefore, it could be expedient to train nurses and community health workers to identify patients with common rheumatic diseases. In a 2020 review of the global literature on nurse-led management of RA, the authors proposed strategies to implement programmes in the Middle East and Africa101,127. This proposed model would involve nurses performing an extended role, assuming their own patient caseloads and treating, educating, monitoring and referring as appropriate. Such initiatives should be implemented in parallel with initiatives to improve knowledge about rheumatic diseases among medical students and during the training of internists. The development of digital means of communication, education and training that has occurred during the global COVID-19 pandemic has led to an explosion of opportunities for remote learning that should feature prominently as we strive to address future challenges.
Advocacy
Urgent needs exist to raise awareness of the burden and effects of rheumatic diseases in Africa, promote the education of community and health-care workers, undertake research to inform clinical practice and improve outcomes for patients. In addition, representation to health-care administrators is required to lobby support for patients with rheumatic diseases. Globally, increased attention is being paid to the growing burden of non-communicable diseases, even in low-income and middle-income countries within Africa. Cardiovascular diseases, diabetes, cancers and chronic lung diseases, among others, were identified as priorities in this category128. Unfortunately, rheumatic diseases, including musculoskeletal diseases, are not included in this list. However, global initiatives such as the Bone and Joint Decade initiative in 2000–2010 drew attention to the burden and effects of musculoskeletal diseases, and its successor, the Global Alliance for Musculoskeletal Health, is continuing efforts to get musculoskeletal diseases included in the priority list by the WHO and the United Nations. Such initiatives are important because the health policies and funding of many low-income and middle-income countries are influenced by the health priorities adopted by the WHO and the United Nations.
Research
The shortage of rheumatologists has resulted in limited amounts of high-quality research being undertaken, particularly in sub-Saharan Africa. With the exception of South Africa and North African countries, little funding is available for research. To get around this problem, rheumatologists from some countries in Africa have partnered with colleagues in other parts of the world to receive mentorship and support for their work. However, capacity urgently needs to be developed to enable applications for globally funded competitive research grants to be submitted. The increase in the number of rheumatologists in Africa, especially sub-Saharan Africa, over the past 20 years has resulted in an increased number of research publications. However, most of the work has been undertaken by a small group of rheumatologists from some of the larger academic centres and might not be representative of Africa as a whole. Ongoing challenges to data collection include limited access to laboratory tests, such as serological tests, and difficulties in obtaining a regular supply of conventional synthetic DMARDs, such as methotrexate, not to mention their affordability. However, we now have an opportunity to collect our own information about the standard of care in different African countries, identify risk factors for rheumatic diseases, assess responses to therapy and study patient-reported outcome measures and quality of life. Once this information is available, it will be possible to develop evidence-based guidelines for diagnosis and management in settings with limited resources and a high burden of infectious diseases. A major need also exists for more research into genes that are important in the clinical phenotypes and response to therapies that occur among African individuals, particularly among those in sub-Saharan Africa. The West African heritage of many African Americans adds to the necessity of this research need.
Conclusions
Rheumatology in Africa has advanced substantially from an era of poor knowledge to one of increasing information. Common rheumatic diseases such as gout, RA, osteoarthritis and SLE are increasingly being reported, as are conditions previously considered to be rare such as SSc, psoriatic arthritis and osteoporosis. The clinical presentations and laboratory features of rheumatic diseases are often similar to those seen in other regions of the world, but there are certain differences too. More and better genetic studies might go some way to explaining these differences. Patients are managed according to generally accepted guidelines, although newer therapies such as bDMARDs are invariably unaffordable and unavailable. Future progress depends on education, early diagnosis, the training of more health professionals to diagnose and manage patients and reductions in the costs of newer therapies; greater expenditure on investigations into non-communicable diseases in general will be required to facilitate future advances.
References
Sebbag, E. et al. The world-wide burden of musculoskeletal diseases: a systematic analysis of the World Health Organization burden of diseases database. Ann. Rheum. Dis. 78, 844–848 (2019).
Adelowo, O. O. & Bello, M. K. N. Systemic autoimmune diseases: not so rare in black Africans. Rheumatology (Sunnyvale) 4, 130 (2014).
Mody, G. M. Rheumatology in Africa — challenges and opportunities. Arthritis Res.Ther. 19, 49 (2017).
Tikly, M. & McGill, P. Epidemiology: the challenge of practicing rheumatology in Africa. Nat. Rev. Rheumatol. 12, 630–631 (2016).
Adebajo, A. & Davis, P. Rheumatic diseases in African Blacks. Semin. Arthritis Rheum. 24, 139–153 (1994).
Nuki, G. & Riches, P. Changing paradigms in the management of gout. J. R. Coll. Physicians Edinb. 50, 124–132 (2020).
Fleischmann, V. & Adadevoh, B. K. Hyperuricaemia and gout in Nigerians. Trop. Geogr. Med. 25, 255–261 (1973).
Lowenthal, M. N. & Dymond, I. D. Gout and hyperuricaemia in Blacks. S. Afr. Med. J. 52, 832 (1977).
Cassim, B., Mody, G. M., Deenadayalu, V. K. & Hammond, M. G. Gout in black South Africans: a clinical and genetic study. Ann. Rheum. Dis. 53, 759–762 (1994).
Tikly, M., Bellingan, A., Lincoln, D. & Russell, A. Risk factors for gout: a hospital-based study in urban black South Africans. Rev. Rhum. Engl. Ed. 65, 225–231 (1998).
Mijiyawa, M. & Oniankitan, O. Risk factors for gout in Togolese patients. Jt. Bone Spine 67, 441–445 (2000).
Beighton, P., Solomon, L., Soskolne, C. & Sweet, B. Serum uric acid concentrations in a rural Tswana community in Southern Africa. Ann. Rheum. Dis. 32, 346 (1973).
Beighton, P., Solomon, L., Soskolne, C., Sweet, B. & Robin, G. Serum uric acid concentrations in an urbanized South African Negro population. Ann. Rheum. Dis. 33, 442 (1974).
Courage, U. U. et al. Prevalence of musculoskeletal diseases in a semi-urban Nigerian community: results of a cross-sectional survey using COPCORD methodology. Clin. Rheumatol. 36, 2509–2516 (2017).
Divengi Nzambi, J. P. et al. The epidemiology of rheumatic disorders in a rural Democratic Republic of Congo (DRC): a COPCORD study. Afr. J. Rheumatol. 5, 64–69 (2017).
Chopra, A. & Abdel-Nasser, A. Epidemiology of rheumatic musculoskeletal disorders in the developing world. Best Pract. Res. Clin. Rheumatol. 22, 583–604 (2008).
Kodio, B. et al. Step wise approach of gout in the rheumatology ward of point-G University Teaching Hospital of Bamako, Mali. Afr. J. Rheumatol. 3, 22–26 (2015).
Oyoo, G. Gout in patients attending a rheumatology clinic in Nairobi, Kenya. Health Line 8, 37–38 (2004).
Doualla-Bija, M. et al. Prevalence and characteristics of metabolic syndrome in gout patients in a hospital setting in sub-Saharan Africa. Diabetes Metab. Syndr. 12, 1007–1011 (2018).
Adelowo, O., Umar, A. & Oguntona, S. Gouty arthritis in Nigerians: clinical and laboratory correlates. Afr. J. Rheumatol. 2, 23–28 (2014).
Landré-Beauvais, A. J. The first description of rheumatoid arthritis. Unabridged text of the doctoral dissertation presented in 1800. Jt. Bone Spine 68, 130–143 (2001).
Goodall, J. W. Joint swellings in Africans; a review of 90 cases. Cent. Afr. J. Med. 2, 220–223 (1956).
Mody, G. M. Rheumatoid arthritis and connective tissue disorders: sub-Saharan Africa. Baillieres Clin. Rheumatol. 9, 31–44 (1995).
Dowman, B., Campbell, R. M., Zgaga, L., Adeloye, D. & Chan, K. Y. Estimating the burden of rheumatoid arthritis in Africa: a systematic analysis. J. Glob. Health 2, 020406 (2012).
Usenbo, A., Kramer, V., Young, T. & Musekiwa, A. Prevalence of arthritis in Africa: a systematic review and meta-analysis. PLoS ONE 10, e0133858 (2015).
Muller, A. S., Valkenburg, H. A. & Greenwood, B. M. Rheumatoid arthritis in three west African populations. East. Afr. Med. J. 49, 75–83 (1972).
Solomon, L., Robin, G. & Valkenburg, H. A. Rheumatoid arthritis in an urban South African Negro population. Ann. Rheum. Dis. 34, 128–135 (1975).
Beighton, P., Solomon, L. & Valkenburg, H. A. Rheumatoid arthritis in a rural South African Negro population. Ann. Rheum. Dis. 34, 136–141 (1975).
Meyers, O. L., Daynes, G. & Beighton, P. Rheumatoid arthritis in a tribal Xhosa population in the Transkei, Southern Africa. Ann. Rheum. Dis. 36, 62–65 (1977).
Brighton, S. W., de la Harpe, A. L., van Staden, D. J., Badenhorst, J. H. & Myers, O. L. The prevalence of rheumatoid arthritis in a rural African population. J. Rheumatol. 15, 405–408 (1988).
Moolenburgh, J. D., Valkenburg, H. A. & Fourie, P. B. A population study on rheumatoid arthritis in Lesotho, southern Africa. Ann. Rheum. Dis. 45, 691–695 (1986).
Silman, A. J. et al. Absence of rheumatoid arthritis in a rural Nigerian population. J. Rheumatol. 20, 618–622 (1993).
Abdel-Nasser, A. M., Rasker, J. J. & Valkenburg, H. A. Epidemiological and clinical aspects relating to the variability of rheumatoid arthritis. Semin. Arthritis Rheum. 27, 123–140 (1997).
Malemba, J. J. et al. The epidemiology of rheumatoid arthritis in Kinshasa, Democratic Republic of Congo — a population-based study. Rheumatology 51, 1644–1647 (2012).
Slimani, S. & Ladjouze-Rezig, A. Prevalence of rheumatoid arthritis in an urban population of Algeria: a prospective study. Rheumatology 53, 571–573 (2014).
Viatte, S. & Barton, A. Genetics of rheumatoid arthritis susceptibility, severity, and treatment response. Semin. Immunopathol. 39, 395–408 (2017).
Gregersen, P. K., Silver, J. & Winchester, R. J. The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheum. 30, 1205–1213 (1987).
Okoye, R. C. et al. HLA-D region heterogeneity in a Nigerian population. Tissue Antigens 33, 445–456 (1989).
Malemba, J. J. et al. The phenotype and genotype of rheumatoid arthritis in the Democratic Republic of Congo. Arthritis Res. Ther. 15, R89 (2013).
Singwe-Ngandeu, M., Finckh, A., Bas, S., Tiercy, J. M. & Gabay, C. Diagnostic value of anti-cyclic citrullinated peptides and association with HLA-DRB1 shared epitope alleles in African rheumatoid arthritis patients. Arthritis Res. Ther. 12, R36 (2010).
Govind, N. et al. HLA-DRB1 amino acid positions and residues associated with antibody-positive rheumatoid arthritis in black South Africans. J. Rheumatol. 46, 138–144 (2019).
Raychaudhuri, S. et al. Five amino acids in three HLA proteins explain most of the association between MHC and seropositive rheumatoid arthritis. Nat. Genet. 44, 291–296 (2012).
Begovich, A. B. et al. A missense single-nucleotide polymorphism in a gene encoding a protein tyrosine phosphatase (PTPN22) is associated with rheumatoid arthritis. Am. J. Hum. Genet. 75, 330–337 (2004).
Tikly, M., Govind, N., Frost, J. & Ramsay, M. The PTPN22 R620W polymorphism is not associated with systemic rheumatic diseases in South Africans. Rheumatology 49, 820–821 (2010).
Rotimi, C. N. et al. The genomic landscape of African populations in health and disease. Hum. Mol. Genet. 26, R225–R236 (2017).
Campbell, M. C. & Tishkoff, S. A. African genetic diversity: implications for human demographic history, modern human origins, and complex disease mapping. Ann. Rev. Genomics Hum. Genet. 9, 403–433 (2008).
Baka, Z., Buzás, E. & Nagy, G. Rheumatoid arthritis and smoking: putting the pieces together. Arthritis Res. Ther. 11, 238 (2009).
Elshafie, A. I. et al. Active rheumatoid arthritis in Central Africa: a comparative study between Sudan and Sweden. J. Rheumatol. 43, 1777–1786 (2016).
Govind, N. et al. Pitfalls in the assessment of smoking status detected in a cohort of South African RA patients. Rheumatol. Int. 36, 1365–1369 (2016).
Mamudu, H. M., John, R. M., Veeranki, S. P. & Ouma, A. E. O. The odd man out in Sub-Saharan Africa: understanding the tobacco use prevalence in Madagascar. BMC Public Health 13, 856 (2013).
Sreeramareddy, C. T., Pradhan, P. M. & Sin, S. Prevalence, distribution, and social determinants of tobacco use in 30 sub-Saharan African countries. BMC Med. 12, 243 (2014).
Jiang, X., Alfredsson, L., Klareskog, L. & Bengtsson, C. Smokeless tobacco (moist snuff) use and the risk of developing rheumatoid arthritis: results from a case-control study. Arthritis Care Res. 66, 1582–1586 (2014).
de Oliveira Ferreira, R. et al. Does periodontitis represent a risk factor for rheumatoid arthritis? A systematic review and meta-analysis. Ther. Adv. Musculoskelet. Dis. 11, 1759720x19858514 (2019).
Fuggle, N. R., Smith, T. O., Kaul, A. & Sofat, N. Hand to mouth: a systematic review and meta-analysis of the association between rheumatoid arthritis and periodontitis. Front. Immunol. 7, 80 (2016).
Ouédraogo, D. D. et al. Periodontal disease in patients with rheumatoid arthritis in Sub-Saharan Africa: a case-control study. Jt. Bone Spine 84, 113–114 (2017).
Buwembo, W. et al. Periodontitis and rheumatoid arthritis in sub-Saharan Africa, gaps and way forward: a systematic review and meta-analysis. Open J. Stomatol. 9, 215–226 (2019).
Chikanza, I. C., Stein, M., Lutalo, S. & Gibson, T. The clinical, serologic and radiologic features of rheumatoid arthritis in ethnic black Zimbabwean and British Caucasian patients. J. Rheumatol. 21, 2011–2015 (1994).
Hodkinson, B. et al. Response to traditional disease-modifying anti-rheumatic drugs in indigent South Africans with early rheumatoid arthritis. Clin. Rheumatol. 31, 613–619 (2012).
Ndongo, S., Lekpa, F. K., Ka, M. M., Ndiaye, N. & Diop, T. M. Presentation and severity of rheumatoid arthritis at diagnosis in Senegal. Rheumatology 48, 1111–1113 (2009).
Adelowo, O. O., Ojo, O., Oduenyi, I. & Okwara, C. C. Rheumatoid arthritis among Nigerians: the first 200 patients from a rheumatology clinic. Clin. Rheumatol. 29, 593–597 (2010).
Slimani, S. et al. Characteristics of rheumatoid arthritis in Algeria: a multicenter study. Rheumatol. Int. 34, 1235–1239 (2014).
Sakr, B. R. et al. Rheumatoid arthritis: a single-center Egyptian experience. Immunol. Invest. 47, 293–302 (2018).
Owino, B. O., Oyoo, G. O. & Otieno, C. F. Socio-demographic and clinical aspects of rheumatoid arthritis. East Afr. Med. J. 86, 204–211 (2009).
van Vollenhoven, R. F. Sex differences in rheumatoid arthritis: more than meets the eye. BMC Med. 7, 12 (2009).
Pettipher, C. & Benitha, R. Tuberculosis in biologic users for rheumatic diseases: results from the South African biologics registry (SABIO). Ann. Rheum. Dis. 79, 292–299 (2020).
Reveille, J. D., Ball, E. J. & Khan, M. A. HLA-B27 and genetic predisposing factors in spondyloarthropathies. Curr. Opin. Rheumatol. 13, 265–272 (2001).
Allsopp, C. E. et al. Interethnic genetic differentiation in Africa: HLA class I antigens in the Gambia. Am. J. Hum. Genet. 50, 411–421 (1992).
Kalidi, I. et al. Study of HLA antigens in a population of Mali (West Africa). Tissue Antigens 31, 98–102 (1988).
Brown, M. A. et al. Ankylosing spondylitis in West Africans–evidence for a non-HLA-B27 protective effect. Ann. Rheum. Dis. 56, 68–70 (1997).
Chopra, A. The COPCORD world of musculoskeletal pain and arthritis. Rheumatology 52, 1925–1928 (2013).
Malemba, J. J. & Mbuyi-Muamba, J. M. Clinical and epidemiological features of rheumatic diseases in patients attending the university hospital in Kinshasa. Clin. Rheumatol. 27, 47–54 (2008).
Ntsiba, H. & Bazébissa, R. Four first Congolese cases of pelvic ankylosing spondylitis [French]. Bull. Soc. Pathol. Exot. 96, 21–23 (2003).
López-Larrea, C. et al. Association of ankylosing spondylitis with HLA-B*1403 in a West African population. Arthritis Rheum. 46, 2968–2971 (2002).
Lebughe, P., de Vlam, K., Westhovens, R., Mbuyi-Muamba, J. M. & Malemba, J. J. Spondyloarthritis in the Democratic Republic of the Congo: a prospective hospital-based study. BMJ Open 8, e020329 (2018).
Amroun, H. et al. Early-onset ankylosing spondylitis is associated with a functional MICA polymorphism. Hum. Immunol. 66, 1057–1061 (2005).
Tayel, M. et al. Registry of the clinical characteristics of spondyloarthritis in a cohort of Egyptian population. Rheum. Int. 32, 2837–2842 (2012).
Kchir, M. M. et al. HLA-B, DR and DQ antigens polymorphism in Tunisian patients with ankylosing spondylitis (a case–control study). Rheum. Int. 30, 933–939 (2010).
El Mouraghi, I. et al. Polymorphisms of HLA-A,-B,-Cw and DRB1 antigens in Moroccan patients with ankylosing spondylitis and a comparison of clinical features with frequencies of HLA-B* 27. Tissue Antigens 85, 108–116 (2015).
Tikly, M., Njobvu, P. & McGill, P. Spondyloarthritis in sub-Saharan Africa. Curr. Rheumatol. Rep. 16, 421 (2014).
Claudepierre, P. et al. Predictive factors of severity of spondyloarthropathy in North Africa. Rheumatology 34, 1139–1145 (1995).
Haid, S. et al. Les coxites dans la spondyloarthrite [abstract]. Rev. Rhum. 82 (Suppl. 1), A358 (2015).
Shirazy, K. et al. The prevalence of non-radiographic axial spondyloarthritis among patients with inflammatory back pain from northwest and South Africa: data from a noninterventional, cross-sectional study. Rheumatol. Ther. 5, 437–445 (2018).
van der Heijde, D. et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann. Rheum. Dis. 76, 978–991 (2017).
Goetz, R. H. & Berne, M. B. Pathology of progressive systemic sclerosis (generalized scleroderma) with reference to changes in the viscera. Clin. Proc. 4, 337–392 (1945).
Cowie, R. L. Silica-dust-exposed mine workers with scleroderma (systemic sclerosis). Chest 92, 260–262 (1987).
Sluis-Cremer, G. K., Hessel, P. A., Nizdo, E. H., Churchill, A. R. & Zeiss, E. A. Silica, silicosis, and progressive systemic sclerosis. Br. J. Ind. Med. 42, 838–843 (1985).
Barnes, J. & Mayes, M. D. Epidemiology of systemic sclerosis: incidence, prevalence, survival, risk factors, malignancy, and environmental triggers. Curr. Opin. Rheumatol. 24, 165–170 (2012).
Erasmus, L. D. Scleroderma in goldminers on the Witwatersrand with paricular reference to pulmonary manifestations. S. Afr. J. Lab. Clin. Med. 3, 209–231 (1957).
Tikly, M., Rands, A., McHugh, N., Wordsworth, P. & Welsh, K. Human leukocyte antigen class II associations with systemic sclerosis in South Africans. Tissue Antigens 63, 487–490 (2004).
Erzer, J. N., Jaeger, V. K., Tikly, M. & Walker, U. A. Systemic sclerosis in sub-Saharan Africa: a systematic review. Pan Afr. Med. J. 37, 176 (2020).
Yacoub, Y. I. et al. Bone density in Moroccan women with systemic scleroderma and its relationships with disease-related parameters and vitamin D status. Rheumatol. Int. 32, 3143–3148 (2012).
Ben Salah, R. et al. Clinical and serological profile of systemic sclerosis in Tunisia: a retrospective observational study. Presse Med. 48, e284–e291 (2019).
Steen, V., Domsic, R. T., Lucas, M., Fertig, N. & Medsger, T. A. Jr. A clinical and serologic comparison of African American and Caucasian patients with systemic sclerosis. Arthritis Rheum. 64, 2986–2994 (2012).
Adelowo, O. O. & Oguntona, S. Scleroderma (systemic sclerosis) among Nigerians. Clin. Rheumatol. 28, 1121–1125 (2009).
Aggarwal, R., Lucas, M., Fertig, N., Oddis, C. V. & Medsger, T. A. Jr. Anti–U3 RNP autoantibodies in systemic sclerosis. Arthritis Rheum. 60, 1112–1118 (2009).
Admou, B. et al. Low prevalence of anti-centromere antibodies in scleroderma in Morocco (about 272 cases) [French]. Ann. Biol. Clin. 65, 291–297 (2007).
Symmons, D. Frequency of lupus in people of African origin. Lupus 4, 176–178 (1995).
Molokhia, M., McKeigue, P. M., Cuadrado, M. & Hughes, G. Systemic lupus erythematosus in migrants from west Africa compared with Afro-Caribbean people in the UK. Lancet 357, 1414–1415 (2001).
Bae, S. C., Fraser, P. & Liang, M. H. The epidemiology of systemic lupus erythematosus in populations of African ancestry: a critical review of the “prevalence gradient hypothesis”. Arthritis Rheum. 41, 2091–2099 (1998).
Adelowo, O. & Oguntona, S. Pattern of systemic lupus erythematosus among Nigerians. Clin. Rheumatol. 28, 699–703 (2009).
Ekwom, P., Oyoo, G. & Ongore, D. Prevalence of musculoskeletal pain in Nairobi, Kenya: results of a phase 1, stage 1 COPCORD study. Clin. Rheumatol. 32, S121–S121 (2013).
Adelowo, O., Ojo, O. & Oduenyi, I. Auto antibodies in Nigerian lupus patients. Afr. J. Med. Med. Sci. 41, 177–181 (2012).
Budhoo, A., Mody, G., Dubula, T., Patel, N. & Mody, P. Comparison of ethnicity, gender, age of onset and outcome in South Africans with systemic lupus erythematosus. Lupus 26, 438–446 (2017).
Genga, E. et al. Clinical characteristics of patients with systemic lupus erythe-matosus in Nairobi, Kenya. Afr. J. Rheumatol. 3, 62–66 (2015).
El Hadidi, K. et al. Characteristics of systemic lupus erythematosus in a sample of the Egyptian population: a retrospective cohort of 1109 patients from a single center. Lupus 27, 1030–1038 (2018).
Khanfir, M. S. et al. TULUP (TU nisian LUP us): a multicentric study of systemic lupus erythematosus in Tunisia. Int. J. Rheum. Dis. 16, 539–546 (2013).
Elbagir, S. et al. Sudanese and Swedish patients with systemic lupus erythematosus: immunological and clinical comparisons. Rheumatology 59, 968–978 (2020).
Wadee, S., Tikly, M. & Hopley, M. Causes and predictors of death in South Africans with systemic lupus erythematosus. Rheumatology 46, 1487–1491 (2007).
Essouma, M. et al. Systemic lupus erythematosus in Native sub-Saharan Africans: a systematic review and meta-analysis. J. Autoimmun. 106, 102348 (2020).
Dessein, P. H., Gledhill, R. F. & Rossouw, D. S. Systemic lupus erythematosus in black South Africans. S. Afr. Med. J. 74, 387–389 (1988).
Rudwaleit, M., Tikly, M., Gibson, K., Pile, K. & Wordsworth, P. HLA class II antigens associated with systemic lupus erythematosus in black South Africans. Ann. Rheum. Dis. 54, 678–680 (1995).
Molokhia, M. et al. Relation of risk of systemic lupus erythematosus to west African admixture in a Caribbean population. Hum. Genet. 112, 310–318 (2003).
Molokhia, M. & McKeigue, P. Systemic lupus erythematosus: genes versus environment in high risk populations. Lupus 15, 827–832 (2006).
Freedman, B. I. APOL1 and nephropathy progression in populations of African ancestry. Semin. Nephrol. 33, 425–432 (2013).
Matatiele, P., Tikly, M., Tarr, G. & Gulumian, M. DNA methylation similarities in genes of black South Africans with systemic lupus erythematosus and systemic sclerosis. J. Biomed. Sci. 22, 34 (2015).
Santiago-Casas, Y. et al. Association of discoid lupus erythematosus with clinical manifestations and damage accrual in a multiethnic lupus cohort. Arthritis Care Res. 64, 704–712 (2012).
Drenkard, C. et al. Racial disparities in the incidence of primary chronic cutaneous lupus erythematosus in the southeastern US: the Georgia Lupus Registry. Arthritis Care Res. 71, 95–103 (2019).
Houman, M., Smiti-Khanfir, M., Ghorbell, I. B. & Miled, M. Systemic lupus erythematosus in Tunisia: demographic and clinical analysis of 100 patients. Lupus 13, 204–211 (2004).
Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196 (2012).
Mody, G. M. & Brooks, P. M. Improving musculoskeletal health: global issues. Best Pract. Res. Clin. Rheumatol. 26, 237–249 (2012).
World Population Review. Poorest Countries In Africa 2021 https://worldpopulationreview.com/country-rankings/poorest-countries-in-africa (2021).
Akintayo, R. O. et al. African league against rheumatism (AFLAR) preliminary recommendations on the management of rheumatic diseases during the COVID-19 pandemic. Clin. Rheumatol. https://doi.org/10.1007/s10067-020-05355-2 (2020).
Akintayo, R. O. et al. The impact of COVID-19 on rheumatology practice across Africa. Rheumatology 60, 392–398 (2021).
World Health Organization. The World Health Report 2006. https://www.who.int/whr/2006/06_chap1_en.pdf (2006).
Tikly, M., Zannettou, N. & Hopley, M. A longitudinal study of rheumatoid arthritis in South Africans. MedGenMed 5, 2 (2003).
Hodkinson, B., Musenge, E. & Tikly, M. Tight control of rheumatoid arthritis in a resource-constrained setting: a randomized controlled study comparing the clinical disease activity index and simplified disease activity index. Rheumatology 54, 1033–1038 (2015).
Uthman, I. et al. Nurse-led care for the management of rheumatoid arthritis: a review of the global literature and proposed strategies for implementation in Africa and the Middle East. Rheumatol. Int. 41, 529–542 (2021).
World Health Organization. Resolution adopted by the General Assembly. https://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf (2012).
Tubach, F. et al. Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: the three-year prospective French Research Axed on Tolerance of Biotherapies registry. Arthritis Rheum 60, 1884–1894 (2009).
Dixon, W. G. et al. Drug-specific risk of tuberculosis in patients with rheumatoid arthritis treated with anti-TNF therapy: results from the British Society for Rheumatology Biologics Register (BSRBR). Ann. Rheum. Dis. 69, 522–528 (2010).
Acknowledgements
The authors thank A.A. Akpabio for help with the literature search and drawing up the tables.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, provided substantial contributions to discussions of content and wrote the article. O.A., G.M.M. and M.T. reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Rheumatology thanks L. Lewandowski, A. Gcelu, P. Dessein and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Global Alliance for Musculoskeletal Health: https://gmusc.com/
PAFLAR: https://paflar.org/
Rights and permissions
About this article
Cite this article
Adelowo, O., Mody, G.M., Tikly, M. et al. Rheumatic diseases in Africa. Nat Rev Rheumatol 17, 363–374 (2021). https://doi.org/10.1038/s41584-021-00603-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-021-00603-4
This article is cited by
-
Exploring paediatric rheumatology care: a ten-year retrospective analysis of the patient population in Ghana
Pediatric Rheumatology (2024)
-
Exploring complex links: inflammatory rheumatic diseases and men's health
Rheumatology International (2024)
-
Bridging gaps: a qualitative inquiry on improving paediatric rheumatology care among healthcare workers in Kenya
Pediatric Rheumatology (2023)
-
Epidemiology of rheumatic diseases: a cohort of 23,550 patients in rheumatology clinics in Burkina Faso
Clinical Rheumatology (2023)
-
Entzündlich-rheumatische Erkrankungen bei Migranten
Die Innere Medizin (2023)