Abstract
Peptidylarginine deiminases (PADs) have an important role in the pathogenesis of rheumatoid arthritis (RA) owing to their ability to generate citrullinated proteins — the hallmark autoantigens of RA. Of the five PAD enzyme isoforms, PAD2 and PAD4 are the most strongly implicated in RA at both genetic and cellular levels, and PAD inhibitors have shown therapeutic efficacy in mouse models of inflammatory arthritis. PAD2 and PAD4 are additionally targeted by autoantibodies in distinct clinical subsets of patients with RA, suggesting anti-PAD antibodies as possible biomarkers for RA diagnosis and prognosis. This Review weighs the evidence that supports a pathogenic role for PAD enzymes in RA as both promoters and targets of the autoimmune response, as well as discussing the mechanistic and therapeutic implications of these findings in the wider context of RA pathogenesis. Understanding the origin and consequences of dysregulated PAD enzyme activity and immune responses against PAD enzymes will be important to fully comprehend the pathogenic mechanisms involved in this disease and for the development of novel strategies to treat and prevent RA.
Key points
-
Peptidylarginine deiminase (PAD) enzymes catalyse the deimination of arginine residues, generating the citrullinated protein targets of anti-citrullinated protein antibodies (ACPAs).
-
PAD2 and PAD4 are the most strongly implicated PAD enzymes in rheumatoid arthritis (RA) pathogenesis on the basis of genetic, histological and animal studies.
-
Anti-PAD4 antibodies are associated with severe joint damage, and anti-PAD2 antibodies are associated with less severe joint and lung disease in patients with RA.
-
A subset of patients with RA who have the most severe joint and lung disease have anti-PAD4 antibodies that cross-react with PAD3 and can activate PAD4 enzyme function.
-
ACPAs and anti-PAD4 antibodies can both develop preclinically, but development of ACPAs typically precedes that of anti-PAD4 antibodies.
-
Dysregulated PAD enzyme activity and the development of citrullination-associated autoantibodies can promote three important features of RA: citrullination, pro-inflammatory cytokine production and bone destruction.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Rogers, G. E., Harding, H. W. J. & Llewellyn-Smith, I. J. The origin of citrulline-containing proteins in the hair follicle and the chemical nature of trichohyalin, an intracellular precursor. Biochim. Biophys. Acta 495, 159–175 (1977).
Fujisaki, M. & Sugawara, K. Properties of peptidylarginine deiminase from the epidermis of newborn rats. J. Biochem. 89, 257–263 (1981).
Nakashima, K., Hagiwara, T. & Yamada, M. Nuclear localization of peptidylarginine deiminase V and histone deimination in granulocytes. J. Biol. Chem. 277, 49562–49568 (2002).
Vossenaar, E. R., Zendman, A. J. W., Venrooij, W. J. van & Pruijn, G. J. M. PAD, a growing family of citrullinating enzymes: genes, features and involvement in disease. Bioessays 25, 1106–1118 (2003).
Lee, C.-Y. et al. Mining the human tissue proteome for protein citrullination. Mol. Cell. Proteom. 17, 1378–1391 (2018).
Amin, B. & Voelter, W. in Progress in the Chemistry of Organic Natural Products 106 (eds Kinghorn, A. D., Falk, H., Gibbons, S. & Kobayashi, J.) 203–240 (Springer International Publishing, 2017).
Suzuki, A. et al. Functional haplotypes of PADI4, encoding citrullinating enzyme peptidylarginine deiminase 4, are associated with rheumatoid arthritis. Nat. Genet. 34, 395–402 (2003).
Vossenaar, E. R. et al. Expression and activity of citrullinating peptidylarginine deiminase enzymes in monocytes and macrophages. Ann. Rheum. Dis. 63, 373–381 (2004).
Freudenberg, J. et al. Genome-wide association study of rheumatoid arthritis in Koreans: population-specific loci as well as overlap with European susceptibility loci. Arthritis Rheum. 63, 884–893 (2011).
Suzuki, A. et al. Decreased severity of experimental autoimmune arthritis in peptidylarginine deiminase type 4 knockout mice. BMC Musculoskelet. Disord. 17, 205 (2016).
Bawadekar, M. et al. Peptidylarginine deiminase 2 is required for tumor necrosis factor alpha-induced citrullination and arthritis, but not neutrophil extracellular trap formation. J. Autoimmun. 80, 1–9 (2017).
Asaga, H., Nakashima, K., Senshu, T., Ishigami, A. & Yamada, M. Immunocytochemical localization of peptidylarginine deiminase in human eosinophils and neutrophils. J. Leukoc. Biol. 70, 46–51 (2001).
Wang, Y. et al. Histone hypercitrullination mediates chromatin decondensation and neutrophil extracellular trap formation. J. Cell Biol. 184, 205–213 (2009).
Li, P. et al. PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular traps. J. Exp. Med. 207, 1853–1862 (2010).
Brinkmann, V. et al. Neutrophil extracellular traps kill bacteria. Science 303, 1532–1535 (2004).
Zhou, Y. et al. Spontaneous secretion of the citrullination enzyme PAD2 and cell surface exposure of PAD4 by neutrophils. Front. Immunol. 8, 1200 (2017).
Christophorou, M. A. et al. Citrullination regulates pluripotency and histone H1 binding to chromatin. Nature 506, 104 (2014).
Sun, B. et al. Citrullination of NF-κB p65 promotes its nuclear localization and TLR-induced expression of IL-1β and TNFα. Sci. Immunol. 2, eaal3062 (2017).
Li, P. et al. Regulation of p53 target gene expression by peptidylarginine deiminase 4. Mol. Cell. Biol. 28, 4745–4758 (2008).
Guo, Q. & Fast, W. Citrullination of inhibitor of growth 4 (ING4) by peptidylarginine deminase 4 (PAD4) disrupts the interaction between ING4 and p53. J. Biol. Chem. 286, 17069–17078 (2011).
Zhang, X. et al. Peptidylarginine deiminase 2-catalyzed histone H3 arginine 26 citrullination facilitates estrogen receptor target gene activation. Proc. Natl Acad. Sci. USA 109, 13331–13336 (2012).
Schellekens, G. A., de Jong, B. A., van den Hoogen, F. H., van de Putte, L. B. & van Venrooij, W. J. Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J. Clin. Invest. 101, 273–281 (1998).
Aletaha, D. et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 62, 2569–2581 (2010).
Rantapää-Dahlqvist, S. et al. Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum. 48, 2741–2749 (2003).
Sokolove, J. et al. Autoantibody epitope spreading in the pre-clinical phase predicts progression to rheumatoid arthritis. PLoS One 7, e35296 (2012).
van der Helm-van Mil, A. H. M., Verpoort, K. N., Breedveld, F. C., Toes, R. E. M. & Huizinga, T. W. J. Antibodies to citrullinated proteins and differences in clinical progression of rheumatoid arthritis. Arthritis Res. Ther. 7, R958 (2005).
Machold, K. P. et al. Very recent onset rheumatoid arthritis: clinical and serological patient characteristics associated with radiographic progression over the first years of disease. Rheumatology 46, 342–349 (2007).
Chang, X., Zhao, Y., Sun, S., Zhang, Y. & Zhu, Y. The expression of PADI4 in synovium of rheumatoid arthritis. Rheumatol. Int. 29, 1411–1416 (2009).
Kinloch, A. et al. Synovial fluid is a site of citrullination of autoantigens in inflammatory arthritis. Arthritis Rheum. 58, 2287–2295 (2008).
Cornélis, F. et al. New susceptibility locus for rheumatoid arthritis suggested by a genome-wide linkage study. Proc. Natl Acad. Sci. USA 95, 10746–10750 (1998).
Shiozawa, S. et al. Identification of the gene loci that predispose to rheumatoid arthritis. Int. Immunol. 10, 1891–1895 (1998).
Willis, V. C. et al. N-α-Benzoyl-N5-(2-Chloro-1-Iminoethyl)-l-Ornithine amide, a protein arginine deiminase inhibitor, reduces the severity of murine collagen-induced arthritis. J. Immunol. 186, 4396–4404 (2011).
Willis, V. C. et al. Protein arginine deiminase 4 inhibition is sufficient for the amelioration of collagen-induced arthritis. Clin. Exp. Immunol. 188, 263–274 (2017).
Kawalkowska, J. et al. Abrogation of collagen-induced arthritis by a peptidyl arginine deiminase inhibitor is associated with modulation of T cell-mediated immune responses. Sci. Rep. 6, 26430 (2016).
Shelef, M. A. et al. Peptidylarginine deiminase 4 contributes to tumor necrosis factor α-induced inflammatory arthritis. Arthritis Rheumatol. 66, 1482–1491 (2014).
Seri, Y. et al. Peptidylarginine deiminase type 4 deficiency reduced arthritis severity in a glucose-6-phosphate isomerase-induced arthritis model. Sci. Rep. 5, 13041 (2015).
Fan, L. Y. et al. A functional haplotype and expression of the PADI4 gene associated with increased rheumatoid arthritis susceptibility in Chinese. Tissue Antigens 72, 469–473 (2008).
Too, C. L. et al. Polymorphisms in peptidylarginine deiminase associate with rheumatoid arthritis in diverse Asian populations: evidence from MyEIRA study and meta-analysis. Arthritis Res. Ther. 14, R250 (2012).
Hoppe, B. et al. Detailed analysis of the variability of peptidylarginine deiminase type 4 in German patients with rheumatoid arthritis: a case-control study. Arthritis Res. Ther. 8, R34 (2006).
Barton, A. et al. A functional haplotype of the PADI4 gene associated with rheumatoid arthritis in a Japanese population is not associated in a United Kingdom population. Arthritis Rheum. 50, 1117–1121 (2004).
Caponi, L. A family based study shows no association between rheumatoid arthritis and the PADI4 gene in a white French population. Ann. Rheum. Dis. 64, 587–593 (2005).
Terao, C. et al. The human AIRE gene at chromosome 21q22 is a genetic determinant for the predisposition to rheumatoid arthritis in Japanese population. Hum. Mol. Genet. 20, 2680–2685 (2011).
Okada, Y. et al. Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature 506, 376–381 (2014).
Naranbhai, V. et al. Genomic modulators of gene expression in human neutrophils. Nat. Commun. 6, 7545 (2015).
Mergaert, A. M. et al. Reduced anti-histone antibodies and increased risk of rheumatoid arthritis associated with a single nucleotide polymorphism in PADI4 in North Americans. Int. J. Mol. Sci. 20, 3093 (2019).
Chang, X. et al. PADI2 is significantly associated with rheumatoid arthritis. PLoS One 8, e81259 (2013).
Masson-Bessière, C. et al. The major synovial targets of the rheumatoid arthritis-specific antifilaggrin autoantibodies are deiminated forms of the alpha- and beta-chains of fibrin. J. Immunol. 166, 4177–4184 (2001).
Vossenaar, E. R. et al. Rheumatoid arthritis specific anti-Sa antibodies target citrullinated vimentin. Arthritis Res. Ther. 6, R142 (2004).
Snir, O. et al. Multiple antibody reactivities to citrullinated antigens in sera from patients with rheumatoid arthritis: association with HLA-DRB1 alleles. Ann. Rheum. Dis. 68, 736–743 (2009).
Damgaard, D. et al. Relative efficiencies of peptidylarginine deiminase 2 and 4 in generating target sites for anti-citrullinated protein antibodies in fibrinogen, alpha-enolase and histone H3. PLoS One 13, e0203214 (2018).
Sharma, M. et al. Expanding the citrullinome of synovial fibrinogen from rheumatoid arthritis patients. J. Proteom. 208, 103484 (2019).
Darrah, E., Rosen, A., Giles, J. T. & Andrade, F. Peptidylarginine deiminase 2, 3 and 4 have distinct specificities against cellular substrates: novel insights into autoantigen selection in rheumatoid arthritis. Ann. Rheum. Dis. 71, 92–98 (2012).
Guo, Q., Bedford, M. T. & Fast, W. Discovery of peptidylarginine deiminase-4 substrates by protein array: antagonistic citrullination and methylation of human ribosomal protein S2. Mol. Biosyst. 7, 2286–2295 (2011).
Assohou-Luty, C. et al. The human peptidylarginine deiminases type 2 and type 4 have distinct substrate specificities. Biochim. Biophys. Acta 1844, 829–836 (2014).
Blachère, N. E. et al. High-titer rheumatoid arthritis antibodies preferentially bind fibrinogen citrullinated by peptidylarginine deiminase 4. Arthritis Rheumatol. 69, 986–995 (2017).
Bawadekar, M. et al. Tumor necrosis factor alpha, citrullination, and peptidylarginine deiminase 4 in lung and joint inflammation. Arthritis Res. Ther. 18, 173 (2016).
Damgaard, D., Senolt, L., Nielsen, M. F., Pruijn, G. J. & Nielsen, C. H. Demonstration of extracellular peptidylarginine deiminase (PAD) activity in synovial fluid of patients with rheumatoid arthritis using a novel assay for citrullination of fibrinogen. Arthritis Res. Ther. 16, 498 (2014).
Damgaard, D., Senolt, L. & Nielsen, C. H. Increased levels of peptidylarginine deiminase 2 in synovial fluid from anti-CCP-positive rheumatoid arthritis patients: association with disease activity and inflammatory markers. Rheumatology 55, 918–927 (2016).
Vossenaar, E. R. et al. Absence of citrulline-specific autoantibodies in animal models of autoimmunity. Arthritis Rheum. 50, 2370–2372 (2004).
Sun, B. et al. Reciprocal regulation of Th2 and Th17 cells by PAD2-mediated citrullination. JCI Insight 4, 129687 (2019).
Nissinen, R. et al. Peptidylarginine deiminase, the arginine to citrulline converting enzyme, is frequently recognized by sera of patients with rheumatoid arthritis, systemic lupus erythematosus and primary Sjögren syndrome. Scand. J. Rheumatol. 32, 337–342 (2003).
Vossenaar, E. R. et al. Expression of PAD enzymes and occurrence of citrulline-containing proteins in human blood and synovial fluid cells. Arthritis Res. Ther. 4, 24 (2002).
Altschul, S. F. et al. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 25, 3389–3402 (1997).
Takizawa, Y. et al. Peptidylarginine deiminase 4 (PADI4) identified as a conformation-dependent autoantigen in rheumatoid arthritis. Scand. J. Rheumatol. 34, 212–215 (2005).
Halvorsen, E. H. et al. Serum IgG antibodies to peptidylarginine deiminase 4 in rheumatoid arthritis and associations with disease severity. Ann. Rheum. Dis. 67, 414–417 (2008).
Harris, M. L. et al. Association of autoimmunity to peptidyl arginine deiminase type 4 with genotype and disease severity in rheumatoid arthritis. Arthritis Rheum. 58, 1958–1967 (2008).
Kolfenbach, J. R. et al. Autoimmunity to peptidyl arginine deiminase type 4 precedes clinical onset of rheumatoid arthritis. Arthritis Rheum. 62, 2633–2639 (2010).
Reyes-Castillo, Z. et al. Comparative analysis of autoantibodies targeting peptidylarginine deiminase type 4, mutated citrullinated vimentin and cyclic citrullinated peptides in rheumatoid arthritis: associations with cytokine profiles, clinical and genetic features. Clin. Exp. Immunol. 182, 119–131 (2015).
Zhao, J., Zhao, Y., He, J., Jia, R. & Li, Z. Prevalence and significance of anti-peptidylarginine deiminase 4 antibodies in rheumatoid arthritis. J. Rheumatol. 35, 969–974 (2008).
Guderud, K. et al. Lack of association among peptidyl arginine deiminase type 4 autoantibodies, PADI4 polymorphisms, and clinical characteristics in rheumatoid arthritis. J. Rheumatol. 45, 1211–1219 (2018).
Martinez-Prat, L., Lucia, D., Ibarra, C., Mahler, M. & Dervieux, T. Antibodies targeting protein-arginine deiminase 4 (PAD4) demonstrate diagnostic value in rheumatoid arthritis. Ann. Rheumatic Dis. 78, 434–436 (2019).
Rönnelid, J. et al. Anticitrullinated protein/peptide antibody multiplexing defines an extended group of ACPA-positive rheumatoid arthritis patients with distinct genetic and environmental determinants. Ann. Rheumatic Dis. 77, 203–211 (2018).
Vander Cruyssen, B. et al. Diagnostic value of anti-human citrullinated fibrinogen ELISA and comparison with four other anti-citrullinated protein assays. Arthritis Res. Ther. 8, R122 (2006).
Coenen, D., Verschueren, P., Westhovens, R. & Bossuyt, X. Technical and diagnostic performance of 6 assays for the measurement of citrullinated protein/peptide antibodies in the diagnosis of rheumatoid arthritis. Clin. Chem. 53, 498–504 (2007).
Fisher, B. A. et al. Smoking, the HLA-DRB1 shared epitope and ACPA fine-specificity in Koreans with rheumatoid arthritis: evidence for more than one pathogenic pathway linking smoking to disease. Ann. Rheumatic Dis. 73, 741–747 (2014).
Halvorsen, E. H. et al. Serum IgG antibodies to peptidylarginine deiminase 4 predict radiographic progression in patients with rheumatoid arthritis treated with tumour necrosis factor-alpha blocking agents. Ann. Rheumatic Dis. 68, 249–252 (2009).
Navarro-Millán, I. et al. Association of anti-peptidyl arginine deiminase antibodies with radiographic severity of rheumatoid arthritis in African Americans. Arthritis Res. Ther. 18, 241 (2016).
Darrah, E. et al. Association of baseline peptidylarginine deiminase 4 autoantibodies with favorable response to treatment escalation in rheumatoid arthritis. Arthritis Rheumatol. 71, 696–702 (2019).
Ferucci, E. D. et al. Prevalence of anti-peptidylarginine deiminase type 4 antibodies in rheumatoid arthritis and unaffected first-degree relatives in indigenous North American populations. J. Rheumatol. 40, 1523–1528 (2013).
Cappelli, L. C., Konig, M. F., Gelber, A. C., Bingham, C. O. & Darrah, E. Smoking is not linked to the development of anti-peptidylarginine deiminase 4 autoantibodies in rheumatoid arthritis. Arthritis Res. Ther. 20, 59 (2018).
Darrah, E. et al. Erosive rheumatoid arthritis is associated with antibodies that activate PAD4 by increasing calcium sensitivity. Sci. Transl Med. 5, 186ra65 (2013).
Terakawa, H., Takahara, H. & Sugawara, K. Three types of mouse peptidylarginine deiminase: characterization and tissue distribution. J. Biochem. 110, 661–666 (1991).
Shi, J. et al. Affinity maturation shapes the function of agonistic antibodies to peptidylarginine deiminase type 4 in rheumatoid arthritis. Ann. Rheum. Dis. 77, 141–148 (2018).
Giles, J. T. et al. Association of cross-reactive antibodies targeting peptidyl-arginine deiminase 3 and 4 with rheumatoid arthritis-associated interstitial lung disease. PLoS One 9, e98794 (2014).
Darrah, E. et al. Autoantibodies to peptidylarginine deiminase 2 are associated with less severe disease in rheumatoid arthritis. Front. Immunol. 9, 2696 (2018).
Roth, E. B., Stenberg, P., Book, C. & Sjöberg, K. Antibodies against transglutaminases, peptidylarginine deiminase and citrulline in rheumatoid arthritis — new pathways to epitope spreading. Clin. Exp. Rheumatol. 24, 12–18 (2006).
Darrah, E. et al. Proteolysis by granzyme B enhances presentation of autoantigenic peptidylarginine deiminase 4 epitopes in rheumatoid arthritis. J. Proteome Res. 16, 355–365 (2017).
Holoshitz, J. The rheumatoid arthritis HLA–DRB1 shared epitope. Curr. Opin. Rheumatol. 22, 293–298 (2010).
Arend, W. P. & Firestein, G. S. Pre-rheumatoid arthritis: predisposition and transition to clinical synovitis. Nat. Rev. Rheumatol. 8, 573–586 (2012).
Umeda, N. et al. Prevalence of soluble peptidylarginine deiminase 4 (PAD4) and anti-PAD4 antibodies in autoimmune diseases. Clin. Rheumatol. 35, 1181–1188 (2016).
Gourraud, P.-A. et al. A new classification of HLA-DRB1 alleles differentiates predisposing and protective alleles for autoantibody production in rheumatoid arthritis. Arthritis Res. Ther. 9, R27 (2007).
Ruyssen-Witrand, A. et al. A new classification of HLA-DRB1 alleles based on acid–base properties of the amino acids located at positions 13, 70 and 71: impact on ACPA status or structural progression, and meta-analysis on 1235 patients with rheumatoid from two cohorts (ESPOIR and EAC cohort). RMD Open 1, e000099 (2015).
Stolt, P. et al. Quantification of the influence of cigarette smoking on rheumatoid arthritis: results from a population based case-control study, using incident cases. Ann. Rheum. Dis. 62, 835–841 (2003).
Klareskog, L. et al. A new model for an etiology of rheumatoid arthritis: smoking may trigger HLA-DR (shared epitope)-restricted immune reactions to autoantigens modified by citrullination. Arthritis Rheum. 54, 38–46 (2006).
Hedström, A. K., Rönnelid, J., Klareskog, L. & Alfredsson, L. Complex relationships of smoking, HLA-DRB1 genes, and serologic profiles in patients with early rheumatoid arthritis: update from a Swedish population-based case–control study. Arthritis Rheumatol. 71, 1504–1511 (2019).
Polachek, A. et al. Sputum anticitrullinated protein antibodies in patients with long-standing rheumatoid arthritis. J. Clin. Rheumatol. 24, 122–126 (2018).
Willis, V. C. et al. Sputum autoantibodies in patients with established rheumatoid arthritis and subjects at risk of future clinically apparent disease. Arthritis Rheum. 65, 2545–2554 (2013).
Demoruelle, M. K. et al. Antibody responses to citrullinated and noncitrullinated antigens in the sputum of subjects with rheumatoid arthritis and subjects at risk for development of rheumatoid arthritis. Arthritis Rheumatol. 70, 516–527 (2018).
Demoruelle, M. K. et al. Anti-citrullinated protein antibodies are associated with neutrophil extracellular traps in the sputum in relatives of rheumatoid arthritis patients. Arthritis Rheumatol. 69, 1165–1175 (2017).
Holers, V. M. et al. Rheumatoid arthritis and the mucosal origins hypothesis: protection turns to destruction. Nat. Rev. Rheumatol. 14, 542–557 (2018).
Potempa, J., Mydel, P. & Koziel, J. The case for periodontitis in the pathogenesis of rheumatoid arthritis. Nat. Rev. Rheumatol. 13, 606–620 (2017).
Konig, M. F. et al. Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci. Transl Med. 8, 369ra176 (2016).
Gómez-Bañuelos, E., Mukherjee, A., Darrah, E. & Andrade, F. Rheumatoid arthritis-associated mechanisms of Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. J. Clin. Med. 8, 1309 (2019).
Wegner, N. et al. Peptidylarginine deiminase from Porphyromonas gingivalis citrullinates human fibrinogen and α-enolase: implications for autoimmunity in rheumatoid arthritis. Arthritis Rheum. 62, 2662–2672 (2010).
Romero, V. et al. Immune-mediated pore-forming pathways induce cellular hypercitrullination and generate citrullinated autoantigens in rheumatoid arthritis. Sci. Transl Med. 5, 209ra150 (2013).
Konig, M. F. & Andrade, F. A critical reappraisal of neutrophil extracellular traps and NETosis mimics based on differential requirements for protein citrullination. Front. Immunol. 7, 461 (2016).
Spengler, J. et al. Release of active peptidyl arginine deiminases by neutrophils can explain production of extracellular citrullinated autoantigens in rheumatoid arthritis synovial fluid. Arthritis Rheumatol. 67, 3135–3145 (2015).
Naik, P., Shi, J., Andrade, F. & Darrah, E. Antibodies to PAD4 drive monocyte activation and differentiation into osteoclast-like cells [abstract]. Arthritis Rheumatol. 70 (suppl 10), 2902 (2018).
Tak, P. P. et al. The levels of soluble granzyme A and B are elevated in plasma and synovial fluid of patients with rheumatoid arthritis (RA). Clin. Exp. Immunol. 116, 366–370 (1999).
Darrah, E. & Rosen, A. Granzyme B cleavage of autoantigens in autoimmunity. Cell Death Differ. 17, 624–632 (2010).
Andrade, F. et al. Autocitrullination of human peptidyl arginine deiminase type 4 regulates protein citrullination during cell activation. Arthritis Rheum. 62, 1630–1640 (2010).
Slack, J. L., Jones, L. E. Jr., Bhatia, M. M. & Thompson, P. R. Autodeimination of protein arginine deiminase 4 alters protein–protein interactions but not activity. Biochemistry 50, 3997–4010 (2011).
Méchin, M.-C. et al. Deimination is regulated at multiple levels including auto-deimination of peptidylarginine deiminases. Cell. Mol. Life Sci. 67, 1491–1503 (2010).
Darrah, E. et al. Citrullination is not a major determinant in the recognition of peptidylarginine deiminase 2 and 4 by autoantibodies in rheumatoid arthritis. Arthritis Rheumatol. https://doi.org/10.1002/art.41276 (2020)
Auger, I., Martin, M., Balandraud, N. & Roudier, J. Rheumatoid arthritis-specific autoantibodies to peptidyl arginine deiminase type 4 inhibit citrullination of fibrinogen. Arthritis Rheum. 62, 126–131 (2010).
Dieterich, W. et al. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat. Med. 3, 797–801 (1997).
Sollid, L. M. & Jabri, B. Celiac disease and transglutaminase 2: a model for posttranslational modification of antigens and HLA association in the pathogenesis of autoimmune disorders. Curr. Opin. Immunol. 23, 732–738 (2011).
Pieper, J. et al. Memory T cells specific to citrullinated α-enolase are enriched in the rheumatic joint. J. Autoimmun. 92, 47–56 (2018).
Rims, C. et al. Citrullinated aggrecan epitopes as targets of autoreactive CD4+ T cells in patients with rheumatoid arthritis. Arthritis Rheumatol. 71, 518–528 (2019).
Arnoux, F. et al. Peptidyl arginine deiminase immunization induces anticitrullinated protein antibodies in mice with particular MHC types. Proc. Natl Acad. Sci. USA 114, E10177 (2017).
Sokolove, J., Zhao, X., Chandra, P. E. & Robinson, W. H. Immune complexes containing citrullinated fibrinogen costimulate macrophages via Toll-like receptor 4 and Fcγ receptor. Arthritis Rheum. 63, 53–62 (2011).
Harre, U. et al. Induction of osteoclastogenesis and bone loss by human autoantibodies against citrullinated vimentin. J. Clin. Invest. 122, 1791–1802 (2012).
Krishnamurthy, A. et al. Citrullination controls dendritic cell transdifferentiation into osteoclasts. J. Immunol. 202, 3143–3150 (2019).
Wigerblad, G. et al. Autoantibodies to citrullinated proteins may induce joint pain independent of inflammation. Ann. Rheum. Dis. 75, 730–738 (2016).
Trouw, L. A. et al. Anti-cyclic citrullinated peptide antibodies from rheumatoid arthritis patients activate complement via both the classical and alternative pathways. Arthritis Rheum. 60, 1923–1931 (2009).
Willemze, A., Trouw, L. A., Toes, R. E. M. & Huizinga, T. W. J. The influence of ACPA status and characteristics on the course of RA. Nat. Rev. Rheumatol. 8, 144–152 (2012).
Engdahl, C. et al. Periarticular bone loss in arthritis is induced by autoantibodies against citrullinated vimentin. J. Bone Miner. Res. 32, 1681–1691 (2017).
Krishnamurthy, A. et al. Identification of a novel chemokine-dependent molecular mechanism underlying rheumatoid arthritis-associated autoantibody-mediated bone loss. Ann. Rheum. Dis. 75, 721–729 (2016).
Pollmann, S. et al. Anti-PAD4 autoantibodies in rheumatoid arthritis: levels in serum over time and impact on PAD4 activity as measured with a small synthetic substrate. Rheumatol. Int. 32, 1271–1276 (2012).
Jonsson, M. K. et al. Peptidylarginine deiminase 4 (PAD4) activity in early rheumatoid arthritis. Scand. J. Rheumatol. 49, 87–95 (2019).
Witalison, E. E., Thompson, P. R. & Hofseth, L. J. Protein arginine deiminases and associated citrullination: physiological functions and diseases associated with dysregulation. Curr. Drug. Targets 16, 700–710 (2015).
Ellebrecht, C. T. et al. Reengineering chimeric antigen receptor T cells for targeted therapy of autoimmune disease. Science 353, 179–184 (2016).
Benham, H. et al. Citrullinated peptide dendritic cell immunotherapy in HLA risk genotype-positive rheumatoid arthritis patients. Sci. Transl Med. 7, 290ra87 (2015).
Senshu, T., Kan, S., Ogawa, H., Manabe, M. & Asaga, H. Preferential deimination of keratin K1 and filaggrin during the terminal differentiation of human epidermis. Biochem. Biophys. Res. Commun. 225, 712–719 (1996).
Feng, D. et al. Citrullination preferentially proceeds in glomerular Bowman’s capsule and increases in obstructive nephropathy. Kidney Int. 68, 84–95 (2005).
Keilhoff, G. et al. Expression pattern of peptidylarginine deiminase in rat and human Schwann cells. Dev. Neurobiol. 68, 101–114 (2008).
Liu, Y. et al. Peptidylarginine deiminases 2 and 4 modulate innate and adaptive immune responses in TLR-7-dependent lupus. JCI Insight 3, e124729 (2018).
Wood, D. D. et al. Myelin localization of peptidylarginine deiminases 2 and 4: comparison of PAD2 and PAD4 activities. Lab. Invest. 88, 354–364 (2008).
Keyser, J. D., Schaaf, M. & Teelken, A. Peptidylarginine deiminase activity in postmortem white matter of patients with multiple sclerosis. Neurosci. Lett. 260, 74–76 (1999).
Inagaki, M., Takahara, H., Nishi, Y., Sugawara, K. & Sato, C. Ca2+-dependent deimination-induced disassembly of intermediate filaments involves specific modification of the amino-terminal head domain. J. Biol. Chem. 264, 18119–18127 (1989).
Ishigami, A. et al. Abnormal accumulation of citrullinated proteins catalyzed by peptidylarginine deiminase in hippocampal extracts from patients with Alzheimer’s disease. J. Neurosci. Res. 80, 120–128 (2005).
Jang, B. et al. Involvement of peptidylarginine deiminase-mediated post-translational citrullination in pathogenesis of sporadic Creutzfeldt-Jakob disease. Acta Neuropathol. 119, 199–210 (2010).
Mastronardi, F. G. et al. Increased citrullination of histone H3 in multiple sclerosis brain and animal models of demyelination: a role for tumor necrosis factor-induced peptidylarginine deiminase 4 translocation. J. Neurosci. 26, 11387–11396 (2006).
Hagiwara, T., Nakashima, K., Hirano, H., Senshu, T. & Yamada, M. Deimination of arginine residues in nucleophosmin/B23 and histones in HL-60 granulocytes. Biochem. Biophys. Res. Commun. 290, 979–983 (2002).
Chang, X. et al. Increased PADI4 expression in blood and tissues of patients with malignant tumors. BMC Cancer 9, 40 (2009).
Wright, P. W. et al. ePAD, an oocyte and early embryo-abundant peptidylarginine deiminase-like protein that localizes to egg cytoplasmic sheets. Dev. Biol. 256, 74–89 (2003).
Raijmakers, R. et al. Methylation of arginine residues interferes with citrullination by peptidylarginine deiminases in vitro. J. Mol. Biol. 367, 1118–1129 (2007).
Esposito, G. et al. Peptidylarginine deiminase (PAD) 6 is essential for oocyte cytoskeletal sheet formation and female fertility. Mol. Cell. Endocrinol. 273, 25–31 (2007).
Acknowledgements
The work of A.M.C. and E.D. is supported by a Rheumatology Research Foundation Innovative Research Award.
Review criteria
A search for original articles was performed in PubMed using the following terms alone and in combination: “deiminase”, “rheumatoid”, “arthritis”, “antibodies” and “citrullination”. References cited in selected articles were also traced back to the primary sources.
Author information
Authors and Affiliations
Contributions
A.M.C., P.N. and E.D. researched data for the article. All authors substantially contributed to discussions of content, wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
E.D. and J.T.G. declare that they are authors on licensed patent no. 8,975,033 entitled “Human autoantibodies specific for PAD3 which are cross-reactive with PAD4 and their use in the diagnosis and treatment of rheumatoid arthritis and related diseases”. E.D. declares that she is an author on provisional patent no. 62/481,158 entitled “Anti-PAD2 antibody for treating and evaluating rheumatoid arthritis”. E.D. has received grants from Bristol-Myers Squibb, Celgene and Pfizer, and personal fees from Celgene that are not related to this article. A.M.C. and P.N. declare no competing interests.
Additional information
Peer review information
Nature Reviews Rheumatology thanks J. Roudier, P. Venables and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Curran, A.M., Naik, P., Giles, J.T. et al. PAD enzymes in rheumatoid arthritis: pathogenic effectors and autoimmune targets. Nat Rev Rheumatol 16, 301–315 (2020). https://doi.org/10.1038/s41584-020-0409-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-020-0409-1
This article is cited by
-
The immunopathogenesis of narcolepsy type 1
Nature Reviews Immunology (2024)
-
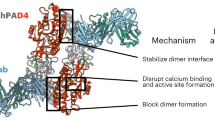
Antibody discovery identifies regulatory mechanisms of protein arginine deiminase 4
Nature Chemical Biology (2024)
-
Evaluating the docetaxel effect in an animal model of polyarthritis
Inflammopharmacology (2024)
-
Genome-wide identification of RNA modification-related single nucleotide polymorphisms associated with rheumatoid arthritis
BMC Genomics (2023)
-
The oral microbiome in autoimmune diseases: friend or foe?
Journal of Translational Medicine (2023)