Abstract
Fibromyalgia is characterized by chronic widespread pain, fatigue, sleep disturbances and functional symptoms. The etiopathogenesis, diagnostic criteria and classification criteria of fibromyalgia are still debated and, consequently, so are the strategies for treating this condition. Fibromyalgia is the third most frequent musculoskeletal condition, and its prevalence increases with age. However, although diagnosis has improved with the evolution of more accurate diagnostic criteria, a considerable proportion of physicians still fail to recognize the syndrome. Many factors contribute to the development of fibromyalgia in a unique manner: genetic predisposition, personal experiences, emotional–cognitive factors, the mind–body relationship and a biopsychological ability to cope with stress. The multiple components of the pathogenesis and maintenance of the condition necessitate a multi-modal treatment approach. Individually tailored treatment is an important consideration, with the increasing recognition that different fibromyalgia subgroups exist with different clinical characteristics. Consequently, although an evidence-based approach to fibromyalgia management is always desirable, the approach of physicians is inevitably empirical, and must have the aim of creating a strong alliance with the patient and formulating shared, realistic treatment goals.
Key points
-
Fibromyalgia is a fairly common syndrome in the general population, reaching a prevalence of 2–3% worldwide.
-
The complex polysymptomatology of fibromyalgia comprises not only chronic widespread pain, fatigue and sleep alterations but also autonomic disturbances, cognitive dysfunction, hypersensitivity to external stimuli, somatic symptoms and psychiatric disorders.
-
Owing to the subjectivity of the symptoms and the lack of biomarkers, diagnosis is exquisitely clinical, and diagnostic criteria are constantly evolving; early diagnosis and prevention are still elusive goals.
-
Fibromyalgia severity and progression or improvement can be evaluated by means of a plethora of composite tests.
-
Fibromyalgia pathogenesis is not fully understood; hypotheses state that genetic predisposition, stressful life events, peripheral (inflammatory) and central (cognitive–emotional) mechanisms interplay to create pain dysperception owing to neuromorphological modifications (‘nociplastic pain’).
-
Treatment should be multimodal and built on four pillars (patient education; fitness; pharmacotherapy; and psychotherapy); the approach should be individualized, symptom-based and stepwise, establishing shared goals with the patient.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Queiroz, L. P. Worldwide epidemiology of fibromyalgia. Curr. Pain. Headache Rep. 17, 356 (2013).
Jones, G. T. et al. The prevalence of fibromyalgia in the general population: a comparison of the American College of Rheumatology 1990, 2010, and modified 2010 classification criteria. Arthritis Rheumatol. 67, 568–575 (2015).
Perrot, S. Fibromyalgia: a misconnection in a multiconnected world? Eur. J. Pain. 23, 866–873 (2019).
Macfarlane, G. J. et al. EULAR revised recommendations for the management of fibromyalgia. Ann. Rheum. Dis. 76, 318–328 (2017).
Branco, J. C. et al. Prevalence of fibromyalgia: a survey in five European countries. Semin. Arthritis Rheum. 39, 448–453 (2009).
Chaaya, M. et al. High burden of rheumatic diseases in Lebanon: a COPCORD study. Int. J. Rheum. Dis. 15, 136–143 (2011).
Nakamura, I. et al. An epidemiologic internet survey of fibromyalgia and chronic pain in Japan. Arthritis Care Res. 66, 1093–1101 (2014).
Turhanoglu, A. D. et al. The epidemiological aspects of fibromyalgia syndrome in adults living in Turkey: a population based study. J. Musculoskelet. Pain 16, 141–147 (2008).
Guermazi, M. et al. [Fibromyalgia prevalence in Tunisia]. Tunis. Med. 86, 806–811 (2008).
Rodrigues Senna, E. et al. Prevalence of rheumatic diseases in Brazil: a study using the COPCORD approach. J. Rheumatol. 31, 594–597 (2004).
White, K. P., Speechley, M., Harth, M. & Ostbye, T. The London fibromyalgia epidemiology study: the prevalence of fibromyalgia syndrome in London, Ontario. J. Rheumatol. 26, 1570–1576 (1999).
Vincent, A. et al. Prevalence of fibromyalgia: a population-based study in Olmsted County, Minnesota, utilizing the Rochester epidemiology project. Arthritis Care Res. 65, 786–792 (2013).
Scudds, R. A., Li, E. K. M. & Scudds, R. J. The prevalence of fibromyalgia syndrome in Chinese people in Hong Kong. J. Musculoskelet. Pain 14, 3–11 (2006).
Ablin, J. N. et al. Prevalence of fibromyalgia in the Israeli population: a population-based study to estimate the prevalence of fibromyalgia in the Israeli population using the London Fibromyalgia Epidemiology Study Screening Questionnaire (LFESSQ). Clin Exp Rheumatol 30, 39–43 (2012).
Prescott, E. et al. Fibromyalgia in the adult danish population. I. A prevalence study. Scand. J. Rheumatol. 22, 233–237 (1993).
Salaffi, F. et al. Prevalence of musculoskeletal conditions in an Italian population sample: Results of a regional community-based study. I. The MAPPING study. Clin. Exp. Rheumatol. 23, 819–828 (2005).
Spaeth, M. Epidemiology, costs, and the economic burden of fibromyalgia. Arthritis Res. Ther. 11, 2–3 (2009).
Häuser, W., Sarzi-Puttini, P. & Fitzcharles, M. A. Fibromyalgia syndrome: under-, over- and misdiagnosis. Clin. Exp. Rheumatol. 37, 90–97 (2019).
Lachaine, J., Beauchemin, C. & Landry, P.-A. Clinical and economic characteristics of patients with fibromyalgia syndrome. Clin. J. Pain 26, 284–290 (2010).
Berger, A., Dukes, E., Martin, S., Edelsberg, J. & Oster, G. Characteristics and healthcare costs of patients with fibromyalgia syndrome. Int. J. Clin. Pract. 61, 1498–1508 (2007).
Knight, T. et al. Health-resource use and costs associated with fibromyalgia in France, Germany, and the United States. Clinicoecon. Outcomes Res. 5, 171–180 (2013).
Lacasse, A., Bourgault, P. & Choinière, M. Fibromyalgia-related costs and loss of productivity: a substantial societal burden. BMC Musculoskelet. Disord. 17, 168 (2016).
Guymer, E. K., Littlejohn, G. O., Brand, C. K. & Kwiatek, R. A. Fibromyalgia onset has a high impact on work ability in Australians. Intern. Med. J. 46, 1069–1074 (2016).
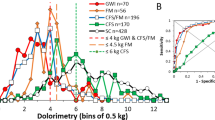
Gracely, R. H., Grant, M. A. & Giesecke, T. Evoked pain measures in fibromyalgia. Best Pract. Res. Clin. Rheumatol. 17, 593–609 (2003).
Koroschetz, J. et al. Fibromyalgia and neuropathic pain — differences and similarities. A comparison of 3057 patients with diabetic painful neuropathy and fibromyalgia. BMC Neurol. 11, 55 (2011).
Rehm, S. E. et al. A cross-sectional survey of 3035 patients with fibromyalgia: subgroups of patients with typical comorbidities and sensory symptom profiles. Rheumatology 49, 1146–1152 (2010).
Rossi, A. et al. Fibromyalgia and nutrition: what news? Clin. Exp. Rheumatol. 33, S117–S125 (2015).
Bossema, E. R., Van Middendorp, H., Jacobs, J. W. G., Bijlsma, J. W. J. & Geenen, R. Influence of weather on daily symptoms of pain and fatigue in female patients with fibromyalgia: a multilevel regression analysis. Arthritis Care Res. 65, 1019–1025 (2013).
Staud, R., Robinson, M. E., Weyl, E. E. & Price, D. D. Pain variability in fibromyalgia is related to activity and rest: role of peripheral tissue impulse input. J. Pain 11, 1376–1383 (2010).
Casale, R. et al. Fibromyalgia and the concept of resilience. Clin. Exp. Rheumatol. 37, 105–113 (2019).
Sandıkçı, S. C. & Özbalkan, Z. Fatigue in rheumatic diseases. Eur. J. Rheumatol. 2, 109–113 (2015).
Kleinman, L. et al. Assessment of sleep in patients with fibromyalgia: qualitative development of the fibromyalgia sleep diary. Health Qual. Life Outcomes 12, 111 (2014).
Bennett, R. M., Jones, J., Turk, D. C., Russell, I. J. & Matallana, L. An internet survey of 2,596 people with fibromyalgia. BMC Musculoskelet. Disord. 8, 27 (2007).
Glass, J. M. Review of cognitive dysfunction in fibromyalgia: a convergence on working memory and attentional control impairments. Rheum. Dis. Clin. North Am. 35, 299–311 (2009).
Walitt, B. et al. The longitudinal outcome of fibromyalgia: a study of 1555 patients. J. Rheumatol. 38, 2238–2246 (2011).
Ifergane, G., Buskila, D., Simiseshvely, N., Zeev, K. & Cohen, H. Prevalence of fibromyalgia syndrome in migraine patients. Cephalalgia 26, 451–456 (2006).
Mathieu, N. [Somatic comorbidities in irritable bowel syndrome: fibromyalgia, chronic fatigue syndrome, and interstitial cystitis]. Gastroenterol. Clin. Biol. 33, S17–S25 (2009).
Nickel, J. C. et al. Interstitial cystitis/painful bladder syndrome and associated medical conditions with an emphasis on irritable bowel syndrome, fibromyalgia and chronic fatigue syndrome. J. Urol. 184, 1358–1363 (2010).
Kalichman, L. Association between fibromyalgia and sexual dysfunction in women. Clin. Rheumatol. 28, 365–369 (2009).
Arnold, L. M. et al. AAPT diagnostic criteria for fibromyalgia. J. Pain 20, 611–628 (2018).
Solano, C. et al. Autonomic dysfunction in fibromyalgia assessed by the composite autonomic symptoms scale (COMPASS). J. Clin. Rheumatol. 15, 172–176 (2009).
Vincent, A. et al. A report of the autonomic symptom profile in patients with fibromyalgia. J. Clin. Rheumatol. 20, 106–108 (2014).
Wolfe, F. et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 33, 160–172 (1990).
Yunus, M. B. & Aldag, J. C. Restless legs syndrome and leg cramps in fibromyalgia syndrome: a controlled study. BMJ 312, 1339 (1996).
Viola-Saltzman, M., Watson, N. F., Bogart, A., Goldberg, J. & Buchwald, D. High prevalence of restless legs syndrome among patients with fibromyalgia: a controlled cross-sectional study. J. Clin. Sleep Med. 6, 423–427 (2010).
Stehlik, R., Arvidsson, L. & Ulfberg, J. Restless legs syndrome is common among female patients with fibromyalgia. Eur. Neurol. 61, 107–111 (2009).
Jones, K. D., Horak, F. B., Winters-Stone, K., Irvine, J. M. & Bennett, R. M. Fibromyalgia is associated with impaired balance and falls. J. Clin. Rheumatol. 15, 16–21 (2009).
Galvez-Sánchez, C. M., Duschek, S. & Del Paso, G. A. R. Psychological impact of fibromyalgia: current perspectives. Psychol. Res. Behav. Manag. 12, 117–127 (2019).
González, E., Elorza, J. & Failde, I. Fibromyalgia and psychiatric comorbidity: their effect on the quality of life patients. Actas Esp. Psiquiatr. 38, 295–300 (2010).
Kessler, R. C. et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289, 3095–3105 (2003).
Dreyer, L., Kendall, S., Danneskiold-Samsøe, B., Bartels, E. M. & Bliddal, H. Mortality in a cohort of Danish patients with fibromyalgia: Increased frequency of suicide. Arthritis Rheum. 62, 3101–3108 (2010).
Gill, H. et al. The prevalence of suicidal behaviour in fibromyalgia patients. Prog. Neuropsychopharmacol. Biol. Psychiatry https://doi.org/10.1016/j.pnpbp.2020.110078 (2020).
Bennett, R. M. Fibrositis: misnomer for a common rheumatic disorder. West. J. Med. 134, 405–413 (1981).
Wolfe, F. et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR preliminary diagnostic criteria for fibromyalgia. J. Rheumatol. 38, 1113–1122 (2011).
Wolfe, F. et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 62, 600–610 (2010).
Wolfe, F. et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin. Arthritis Rheum. 46, 319–329 (2016).
Atzeni, F. et al. One year in review 2019: fibromyalgia. Clin. Exp. Rheumatol. 37, S3–S10 (2019).
Perrot, S., Bouhassira, D. & Fermanian, J. Development and validation of the fibromyalgia rapid screening tool (FiRST). Pain 150, 250–256 (2010).
Baron, R. et al. Improving the primary care physicians’ decision making for fibromyalgia in clinical practice: development and validation of the fibromyalgia detection (FibroDetect®) screening tool. Health Qual. Life Outcomes 12, 128 (2014).
Salaffi, F. et al. Development and validation of the SImple FIbromyalgia Screening questionnaire for improving the recognition of fibromyalgia in daily practice. Clin. Exp. Rheumatol. 38, 9–16 (2019).
Yunus, M. B. Central sensitivity syndromes: a new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin. Arthritis Rheum. 37, 339–352 (2008).
Wolfe, F. Fibromyalgianess. Arthritis Care Res. 61, 715–716 (2009).
Salaffi, F., Di Carlo, M., Arcà, S. & Galeazzi, M. Categorisation of disease severity states in fibromyalgia: a first step to support decision-making in health care policy. Clin. Exp. Rheumatol. 36, 1074–1081 (2018).
Davis, F. et al. Characterizing classes of fibromyalgia within the continuum of central sensitization syndrome. J. Pain Res. 11, 2551–2560 (2018).
Ballantyne, J. C. & Sullivan, M. D. Intensity of chronic pain — the wrong metric? N. Engl. J. Med. 373, 2098–2099 (2015).
Salaffi, F., Sarzi-Puttini, P., Ciapetti, A. & Atzeni, F. Clinimetric evaluations of patients with chronic widespread pain. Best Pract. Res. Clin. Rheumatol. 25, 249–270 (2011).
Burckhardt, C. S., Clark, S. R. & Bennett, R. M. The fibromyalgia impact questionnaire: development and validation. J. Rheumatol. 18, 728–733 (1991).
Bennett, R. M. et al. The Revised Fibromyalgia Impact Questionnaire (FIQR): validation and psychometric properties. Arthritis Res. Ther. 11, R120 (2009).
Salaffi, F. et al. Psychometric characteristics of the Italian version of the revised Fibromyalgia Impact Questionnaire using classical test theory and Rasch analysis. Clin. Exp. Rheumatol. 31, S41–S49 (2013).
Salaffi, F. et al. Development and validation of the self-administered Fibromyalgia Assessment Status: a disease-specific composite measure for evaluating treatment effect. Arthritis Res. Ther. 11, R125 (2009).
Iannuccelli, C. et al. Psychometric properties of the Fibromyalgia Assessment Status (FAS) index: a national web-based study of fibromyalgia. Clin. Exp. Rheumatol. 29, S49–S54 (2011).
Häuser, W. et al. Validation of the fibromyalgia survey questionnaire within a cross-sectional survey. PLoS ONE 7, e37504 (2012).
Häuser, W., Brähler, E., Wolfe, F. & Henningsen, P. Patient Health Questionnaire 15 as a generic measure of severity in fibromyalgia syndrome: surveys with patients of three different settings. J. Psychosom. Res. 76, 307–311 (2014).
Kosek, E. et al. Do we need a third mechanistic descriptor for chronic pain states? Pain 157, 1382–1386 (2016).
Yunus, M. B. Central sensitivity syndromes: a unified concept for fibromyalgia and other similar maladies. J. Indian Rheumatol. Assoc. 8, 27–33 (2000).
Borchers, A. T. & Gershwin, M. E. Fibromyalgia: a critical and comprehensive review. Clin. Rev. Allergy Immunol. 49, 100–151 (2015).
Ceko, M., Bushnell, M. C. & Gracely, R. H. Neurobiology underlying fibromyalgia symptoms. Pain Res. Treat. https://doi.org/10.1155/2012/585419 (2012).
Desmeules, J. A. et al. Neurophysiologic evidence for a central sensitization in patients with fibromyalgia. Arthritis Rheum. 48, 1420–1429 (2003).
Sörensen, J., Graven-Nielsen, T., Henriksson, K. G., Bengtsson, M. & Arendt-Nielsen, L. Hyperexcitability in fibromyalgia. J. Rheumatol. 25, 152–155 (1998).
Staud, R., Vierck, C. J., Cannon, R. L., Mauderli, A. P. & Price, D. D. Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome. Pain 91, 165–175 (2001).
McDermid, A. J., Rollman, G. B. & McCain, G. A. Generalized hypervigilance in fibromyalgia: evidence of perceptual amplification. Pain 66, 133–144 (1996).
Geisser, M. E. et al. A psychophysical study of auditory and pressure sensitivity in patients with fibromyalgia and healthy controls. J. Pain 9, 417–422 (2008).
Martenson, M. E. et al. A possible neural mechanism for photosensitivity in chronic pain. Pain 157, 868–878 (2016).
Harris, R. E. & Clauw, D. J. How do we know that the pain in fibromyalgia is “Real”? Curr. Pain Headache Rep. 10, 403–407 (2006).
Gracely, R. H., Petzke, F., Wolf, J. M. & Clauw, D. J. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 46, 1333–1343 (2002).
Cook, D. B. et al. Functional imaging of pain in patients with primary fibromyalgia. J. Rheumatol. 31, 364–378 (2004).
Burgmer, M. et al. Altered brain activity during pain processing in fibromyalgia. Neuroimage 44, 502–508 (2009).
Jensen, K. B. et al. Evidence of dysfunctional pain inhibition in fibromyalgia reflected in rACC during provoked pain. Pain 144, 95–100 (2009).
Dehghan, M. et al. Coordinate-based (ALE) meta-analysis of brain activation in patients with fibromyalgia. Hum. Brain Mapp. 37, 1749–1758 (2016).
Napadow, V. et al. Intrinsic brain connectivity in fibromyalgia is associated with chronic pain intensity. Arthritis Rheum. 62, 2545–2555 (2010).
Pujol, J. et al. Mapping brain response to pain in fibromyalgia patients using temporal analysis of fMRI. PLoS ONE 4, e5224 (2009).
Jensen, K. B. et al. Patients with fibromyalgia display less functional connectivity in the brain’s pain inhibitory network. Mol. Pain 8, 32 (2012).
Julien, N., Goffaux, P., Arsenault, P. & Marchand, S. Widespread pain in fibromyalgia is related to a deficit of endogenous pain inhibition. Pain 114, 295–302 (2005).
Vierck, C. J. et al. The effect of maximal exercise on temporal summation of second pain (windup) in patients with fibromyalgia syndrome. J. Pain 2, 334–344 (2001).
Normand, E. et al. Pain inhibition is deficient in chronic widespread pain but normal in major depressive disorder. J. Clin. Psychiatry 72, 219–224 (2011).
Lutz, J. et al. White and gray matter abnormalities in the brain of patients with fibromyalgia: a diffusion-tensor and volumetric imaging study. Arthritis Rheum. 58, 3960–3969 (2008).
Russell, I. J. et al. Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome. Arthritis Rheum. 37, 1593–1601 (1994).
Harris, R. E. et al. Decreased central mu-opioid receptor availability in fibromyalgia. J. Neurosci. 27, 10000–10006 (2007).
Baraniuk, J. N., Whalen, G., Cunningham, J. & Clauw, D. J. Cerebrospinal fluid levels of opioid peptides in fibromyalgia and chronic low back pain. BMC Musculoskelet. Disord. 5, 48 (2004).
Russell, I. J., Vaeroy, H., Javors, M. & Nyberg, F. Cerebrospinal fluid biogenic amine metabolites in fibromyalgia/fibrositis syndrome and rheumatoid arthritis. Arthritis Rheum. 35, 550–556 (1992).
Yunus, M. B., Dailey, J. W., Aldag, J. C., Masi, A. T. & Jobe, P. C. Plasma tryptophan and other amino acids in primary fibromyalgia: a controlled study. J. Rheumatol. 19, 90–94 (1992).
Wood, P. B. et al. Fibromyalgia patients show an abnormal dopamine response to pain. Eur. J. Neurosci. 25, 3576–3582 (2007).
Wood, P. B. et al. Reduced presynaptic dopamine activity in fibromyalgia syndrome demonstrated with positron emission tomography: a pilot study. J. Pain 8, 51–58 (2007).
Harris, R. E. Elevated excitatory neurotransmitter levels in the fibromyalgia brain. Arthritis Res. Ther. 12, 141 (2010).
Foerster, B. R. et al. Reduced insular γ-aminobutyric acid in fibromyalgia. Arthritis Rheum. 64, 579–583 (2012).
Arnold, L. M. et al. Family study of fibromyalgia. Arthritis Rheum. 50, 944–952 (2004).
Stormorken, H. & Brosstad, F. Fibromyalgia: family clustering and sensory urgency with early onset indicate genetic predisposition and thus a “true” disease. Scand. J. Rheumatol. 21, 207 (1992).
Buskila, D., Neumann, L., Hazanov, I. & Carmi, R. Familial aggregation in the fibromyalgia syndrome. Semin. Arthritis Rheum. 26, 605–611 (1996).
Ablin, J. N. & Buskila, D. Update on the genetics of the fibromyalgia syndrome. Best Pract. Res. Clin. Rheumatol. 29, 20–28 (2015).
Smith, S. B. et al. Large candidate gene association study reveals genetic risk factors and therapeutic targets for fibromyalgia. Arthritis Rheum. 64, 584–593 (2012).
Haliloglu, S., Carlioglu, A., Akdeniz, D., Karaaslan, Y. & Kosar, A. Fibromyalgia in patients with other rheumatic diseases: prevalence and relationship with disease activity. Rheumatol. Int. 34, 1275–1280 (2014).
Fan, A. et al. Frequency of concomitant fibromyalgia in rheumatic diseases: monocentric study of 691 patients. Semin. Arthritis Rheum. 47, 129–132 (2017).
Affaitati, G. et al. Effects of treatment of peripheral pain generators in fibromyalgia patients. Eur. J. Pain 15, 61–69 (2011).
Doppler, K., Rittner, H. L., Deckart, M. & Sommer, C. Reduced dermal nerve fiber diameter in skin biopsies of patients with fibromyalgia. Pain 156, 2319–2325 (2015).
Clauw, D. J. What is the meaning of “small fiber neuropathy” in fibromyalgia? Pain 156, 2115–2116 (2015).
Ren, K. & Dubner, R. Interactions between the immune and nervous systems in pain. Nat. Med. 16, 1267–1276 (2010).
Sarzi-Puttini, P. et al. Anti-polymer antibodies are correlated with pain and fatigue severity in patients with fibromyalgia syndrome. Autoimmunity 41, 74–79 (2008).
Bazzichi, L. et al. Association between thyroid autoimmunity and fibromyalgic disease severity. Clin. Rheumatol. 26, 2115–2120 (2007).
Cassisi, G., Sarzi-Puttini, P. & Cazzola, M. Chronic widespread pain and fibromyalgia: could there be some relationships with infections and vaccinations? Clin. Exp. Rheumatol. 29, S118–S126 (2011).
Wormser, G. P. et al. Long-term assessment of fibromyalgia in patients with culture-confirmed Lyme disease. Arthritis Rheumatol. 67, 837–839 (2015).
Häuser, W., Kosseva, M., Üceyler, N., Klose, P. & Sommer, C. Emotional, physical, and sexual abuse in fibromyalgia syndrome: a systematic review with meta-analysis. Arthritis Care Res. 63, 808–820 (2011).
Häuser, W. et al. Self-reported childhood maltreatment, lifelong traumatic events and mental disorders in fibromyalgia syndrome: a comparison of US and German outpatients. Clin. Exp. Rheumatol. 33, S86–S92 (2015).
Paras, M. L. et al. Sexual abuse and lifetime diagnosis of somatic disorders. JAMA 302, 550 (2009).
Meeus, M. et al. Heart rate variability in patients with fibromyalgia and patients with chronic fatigue syndrome: a systematic review. Semin. Arthritis Rheum. 43, 279–287 (2013).
Furlan, R. et al. Abnormalities of cardiovascular neural control and reduced orthostatic tolerance in patients with primary fibromyalgia. J. Rheumatol. 32, 1787–1793 (2005).
Martínez-Martínez, L. A., Mora, T., Vargas, A., Fuentes-Iniestra, M. & Martínez-Lavín, M. Sympathetic nervous system dysfunction in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis: a review of case-control studies. J. Clin. Rheumatol. 20, 146–150 (2014).
Martínez-Lavín, M. & Hermosillo, A. G. Autonomic nervous system dysfunction may explain the multisystem features of fibromyalgia. Semin. Arthritis Rheum. 29, 197–199 (2000).
Carnevali, L., Koenig, J., Sgoifo, A. & Ottaviani, C. Autonomic and brain morphological predictors of stress resilience. Front. Neurosci. 12, 228 (2018).
Rodriguez-Raecke, R., Niemeier, A., Ihle, K., Ruether, W. & May, A. Brain gray matter decrease in chronic pain is the consequence and not the cause of pain. J. Neurosci. 29, 13746–13750 (2009).
Tan, A. C., Jaaniste, T. & Champion, D. Chronic widespread pain and fibromyalgia syndrome: life-course risk markers in young people. Pain Res. Manag. https://doi.org/10.1155/2019/6584753 (2019).
Thompson, R. W., Arnkoff, D. B. & Glass, C. R. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma Violence Abuse 12, 220–235 (2011).
Bennett, J. M., Rohleder, N. & Sturmberg, J. P. Biopsychosocial approach to understanding resilience: Stress habituation and where to intervene. J. Eval. Clin. Pract. 24, 1339–1346 (2018).
Hassett, A. L. & Finan, P. H. The role of resilience in the clinical management of chronic pain. Curr. Pain. Headache Rep. 20, 39 (2016).
Engel, G. The need for a new medical model: a challenge for biomedicine. Science 196, 129–136 (1977).
Gracely, R. H. et al. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain 127, 835–843 (2004).
Ellingson, L. D., Stegner, A. J., Schwabacher, I. J., Lindheimer, J. B. & Cook, D. B. Catastrophizing interferes with cognitive modulation of pain in women with fibromyalgia. Pain Med. 19, 2408–2422 (2018).
Geisser, M. E. et al. Perception of noxious and innocuous heat stimulation among healthy women and women with fibromyalgia: association with mood, somatic focus, and catastrophizing. Pain 102, 243–250 (2003).
Lami, M. J., Martínez, M. P., Miró, E., Sánchez, A. I. & Guzmán, M. A. Catastrophizing, acceptance, and coping as mediators between pain and emotional distress and disability in fibromyalgia. J. Clin. Psychol. Med. Settings 25, 80–92 (2018).
Broadbent, P., Liossi, C. & Schoth, D. E. Attentional bias to somatosensory stimuli in chronic pain patients: a systematic review and meta-analysis. Pain https://doi.org/10.1097/j.pain.0000000000002040 (2020).
Alciati, A. et al. Childhood adversities in patients with fibromyalgia: are they related to comorbid lifetime major depression? Clin. Exp. Rheumatol. 35, 112–118 (2017).
Epstein, S. A. et al. Psychiatric disorders in patients with fibromyalgia. Psychosomatics 40, 57–63 (1999).
Alciati, A., Sgiarovello, P., Atzeni, F. & Sarzi-Puttini, P. Psychiatric problems in fibromyalgia: clinical and neurobiological links between mood disorders and fibromyalgia. Reumatismo 64, 268–274 (2012).
Sarzi-Puttini, P. et al. Dysfunctional syndromes and fibromyalgia: a 2012 critical digest. Clin. Exp. Rheumatol. 30, 143–151 (2012).
Choy, E. H. S. The role of sleep in pain and fibromyalgia. Nat. Rev. Rheumatol. 11, 513–520 (2015).
Rizzi, M. et al. Influence of autonomic nervous system dysfunction in the genesis of sleep disorders in fibromyalgia patients. Clin. Exp. Rheumatol. 35, 74–80 (2017).
Lentz, M. J., Landis, C. A., Rothermel, J. & Shaver, J. L. Effects of selective slow wave sleep disruption on musculoskeletal pain and fatigue in middle aged women. J. Rheumatol. 26, 1586–1592 (1999).
Smith, M. T., Edwards, R. R., McCann, U. D. & Haythornthwaite, J. A. The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep 30, 494–505 (2007).
Moldofsky, H., Scarisbrick, P., England, R. & Smythe, H. Musculosketal symptoms and non-REM sleep disturbance in patients with “fibrositis syndrome” and healthy subjects. Psychosom. Med. 37, 341–351 (1975).
Yalinay Dikmen, P., Yavuz, B. G. & Aydinlar, E. I. The relationships between migraine, depression, anxiety, stress, and sleep disturbances. Acta Neurol. Belg. 115, 117–122 (2015).
Sivertsen, B., Harvey, A. G., Pallesen, S. & Hysing, M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J. Sleep. Res. 24, 11–18 (2015).
Haase, L. et al. When the brain does not adequately feel the body: links between low resilience and interoception. Biol. Psychol. 113, 37–45 (2016).
Giusti, E. M., Castelnuovo, G., & Molinari, E. Differences in multidisciplinary and interdisciplinary treatment programs for fibromyalgia: a mapping review. Pain Res. Manag. https://doi.org/10.1155/2017/7261468 (2017).
Gendelman, O. et al. Time to diagnosis of fibromyalgia and factors associated with delayed diagnosis in primary care. Best Pract. Res. Clin. Rheumatol. 32, 489–499 (2018).
García-Ríos, M. C. et al. Effectiveness of health education in patients with fibromyalgia: a systematic review. Eur. J. Phys. Rehabil. Med. 55, 301–313 (2019).
Clauw, D. J. Fibromyalgia: a clinical review. JAMA 311, 1547–1555 (2014).
Häuser, W. & Fitzcharles, M. A. Facts and myths pertaining to fibromyalgia. Dialogues Clin. Neurosci. 20, 53–62 (2018).
Fitzcharles, M. A., Ste-Marie, P. A. & Pereira, J. X. Fibromyalgia: evolving concepts over the past 2 decades. Can. Med. Assoc. J. 185, 645–651 (2013).
Pearson, J. et al. Fibromyalgia self-management: mapping the behaviour change techniques used in a practice-based programme. Musculoskelet. Care 18, 372–382 (2020).
Schrepf, A. et al. Improvement in the spatial distribution of pain, somatic symptoms, and depression after a weight loss intervention. J. Pain 18, 1542–1550 (2017).
Busch, A. J., Barber, K. A. R., Overend, T. J., Peloso, P. M. J. & Schachter, C. L. Exercise for treating fibromyalgia syndrome. Cochrane Database Syst. Rev. 17, CD003786 (2007).
O’Dwyer, T., Maguire, S., Mockler, D., Durcan, L. & Wilson, F. Behaviour change interventions targeting physical activity in adults with fibromyalgia: a systematic review. Rheumatol. Int. 39, 805–817 (2019).
Bjørklund, G., Dadar, M., Chirumbolo, S. & Aaseth, J. Fibromyalgia and nutrition: therapeutic possibilities? Biomed. Pharmacother. 103, 531–538 (2018).
Pagliai, G., Giangrandi, I., Dinu, M., Sofi, F. & Colombini, B. Nutritional Interventions in the management of fibromyalgia syndrome. Nutrients 12, 2525 (2020).
Clauw, D. J. Diagnosing and treating chronic musculoskeletal pain based on the underlying mechanism(s). Best Pract. Res. Clin. Rheumatol. 29, 6–19 (2015).
Häuser, W., Petzke, F., Üçeyler, N. & Sommer, C. Comparative efficacy and acceptability of amitriptyline, duloxetine and milnacipran in fibromyalgia syndrome: a systematic review with meta-analysis. Rheumatology 50, 532–543 (2011).
Häuser, W., Wolfe, F., Tölle, T., Uçeyler, N. & Sommer, C. The role of antidepressants in the management of fibromyalgia syndrome: a systematic review and meta-analysis. CNS Drugs 26, 297–307 (2012).
Calandre, E. P., Rico-Villademoros, F. & Slim, M. An update on pharmacotherapy for the treatment of fibromyalgia. Expert. Opin. Pharmacother. 16, 1347–1368 (2015).
Häuser, W., Urrútia, G., Tort, S., Üçeyler, N. & Walitt, B. Serotonin and noradrenaline reuptake inhibitors (SNRIs) for fibromyalgia syndrome. Cochrane Database Syst. Rev. 31, CD010292 (2013).
Lunn, M. P., Hughes, R. A. & Wiffen, P. J. Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst. Rev. 3, CD007115 (2014).
Pickering, G. et al. Milnacipran poorly modulates pain in patients suffering from fibromyalgia: a randomized double-blind controlled study. Drug Des. Devel. Ther. 12, 2485–2496 (2018).
Üçeyler, N., Sommer, C., Walitt, B. & Häuser, W. Anticonvulsants for fibromyalgia. Cochrane Database Syst. Rev. 16, CD010782 (2013).
Cooper, T. E., Derry, S., Wiffen, P. J. & Moore, R. A. Gabapentin for fibromyalgia pain in adults. Cochrane Database Syst. Rev. 1, CD012188 (2017).
Straube, S., Derry, S., Moore, R. A. & McQuay, H. J. Pregabalin in fibromyalgia: meta-analysis of efficacy and safety from company clinical trial reports. Rheumatology 49, 706–715 (2010).
Derry, S. et al. Pregabalin for pain in fibromyalgia in adults. Cochrane Database Syst. Rev. 9, CD011790 (2016).
Alciati, A. et al. Controlled-release pregabalin in the treatment of fibromyalgia. Expert. Rev. Neurother. 18, 617–623 (2018).
Tofferi, J. K., Jackson, J. L. & O’Malley, P. G. Treatment of fibromyalgia with cyclobenzaprine: a meta-analysis. Arthritis Rheum. 51, 9–13 (2004).
Giovannitti, J. A., Thoms, S. M. & Crawford, J. J. Alpha-2 adrenergic receptor agonists: a review of current clinical applications. Anesth. Prog. 62, 31–38 (2015).
Malanga, G. A., Gwyn, M. W., Smith, R. & Miller, D. Tizanidine is effective in the treatment of myofascial pain syndrome. Pain Physician 5, 422–432 (2002).
See, S. & Ginzburg, R. Choosing a skeletal muscle relaxant. Am. Fam. Physician 78, 365 (2008).
Littlejohn, G. O., Guymer, E. K. & Ngian, G.-S. Is there a role for opioids in the treatment of fibromyalgia? Pain Manag. 6, 347–355 (2016).
Younger, J., Noor, N., McCue, R. & MacKey, S. Low-dose naltrexone for the treatment of fibromyalgia: findings of a small, randomized, double-blind, placebo-controlled, counterbalanced, crossover trial assessing daily pain levels. Arthritis Rheum. 65, 529–538 (2013).
Kim, P. S. & Fishman, M. A. Low-dose naltrexone for chronic pain: update and systemic review. Curr. Pain Headache Rep. 24, 64 (2020).
Painter, J. T. & Crofford, L. J. Chronic opioid use in fibromyalgia syndrome: a clinical review. J. Clin. Rheumatol. 19, 72–77 (2013).
Cazzola, M., Sarzi-Puttini, P., Buskila, D. & Atzeni, F. [Pharmacological treatment of fibromyalgia]. Reumatismo 59, 280–291 (2007).
Clauw, D. J. & Hassett, A. L. The role of centralised pain in osteoarthritis. Clin. Exp. Rheumatol. 35, S79–S84 (2017).
Moldofsky, H., Lue, F. A., Mously, C., Roth-Schechter, B. & Reynolds, W. J. The effect of zolpidem in patients with fibromyalgia: a dose ranging, double blind, placebo controlled, modified crossover study. J. Rheumatol. 23, 529–533 (1996).
Walitt, B., Klose, P., Üçeyler, N., Phillips, T. & Häuser, W. Antipsychotics for fibromyalgia in adults. Cochrane Database Syst. Rev. 2016, CD011804 (2016).
Calandre, E. P. et al. Quetiapine extended-release (Seroquel-XR) versus amitriptyline monotherapy for treating patients with fibromyalgia: a 16-week, randomized, flexible-dose, open-label trial. Psychopharmacology 231, 2525–2531 (2014).
Strouse, T. B. Cannabinoids in medical practice. Cannabis Cannabinoid Res. 1, 38–43 (2016).
Walitt, B., Klose, P., Ma, F., Phillips, T. & Häuser, W. Cannabinoids for fibromyalgia (Review). Cochrane Database Syst. Rev. 7, CD011694 (2016).
Farrell, M. et al. Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions. Pain 159, 1932–1954 (2018).
Aviram, J. & Samuelly-Leichtag, G. Efficacy of cannabis-based medicines for pain management: a systematic review and meta- analysis of randomized controlled trials. Pain Physician 20, E755–E796 (2017).
Hill, K. P., Palastro, M. D., Johnson, B. & Ditre, J. W. Cannabis and pain: a clinical review. Cannabis Cannabinoid Res. 2, 96–104 (2017).
Fiz, J., Duràn, M., Capellà, D., Carbonell, J. & Farré, M. Cannabis use in patients with fibromyalgia: effect on symptoms relief and health-related quality of life. PLoS ONE 6, e18440 (2011).
Sarzi-Puttini, P. et al. Medical cannabis and cannabinoids in rheumatology: where are we now? Expert Rev. Clin. Immunol. 15, 1019–1032 (2019).
Habib, G. & Artul, S. Medical cannabis for the treatment of fibromyalgia. J. Clin. Rheumatol. 24, 255–258 (2018).
van de Donk, T. et al. An experimental randomized study on the analgesic effects of pharmaceutical-grade cannabis in chronic pain patients with fibromyalgia. Pain 160, 860–869 (2019).
Yassin, M., Oron, A. & Robinson, D. Effect of adding medical cannabis to analgesic treatment in patients with low back pain related to fibromyalgia: an observational cross-over single centre study. Clin. Exp. Rheumatol. 37, 13–20 (2019).
Giorgi, V. et al. Adding medical cannabis to standard analgesic treatment for fibromyalgia: a prospective observational study. Clin. Exp. Rheumatol. 38, 53–59 (2020).
National Pain Report. Marijuana rated most effective for treating fibromyalgia, http://nationalpainreport.com/marijuana-rated-most-effective-for-treating-fibromyalgia-8823638.html (2014).
Rathore, F. A. & Afridi, A. Is combination pharmacotherapy effective for management of fibromyalgia in adults? — a Cochrane Review summary with commentary. J. Musculoskelet. Neuronal Interact. 20, 297–300 (2020).
Boomershine, C. S. & Crofford, L. J. A symptom-based approach to pharmacologic management of fibromyalgia. Nat. Rev. Rheumatol. 5, 191–199 (2009).
Thorpe, J., Shum, B., Ra, M., Pj, W. & Gilron, I. Combination pharmacotherapy for the treatment of fibromyalgia in adults (Review). Cochrane Database Syst. Rev. 2018, CD010585 (2018).
Mease, P. J. et al. Milnacipran combined with pregabalin in fibromyalgia: a randomized, open-label study evaluating the safety and efficacy of adding milnacipran in patients with incomplete response to pregabalin. Ther. Adv. Musculoskelet. Dis. 5, 113–126 (2013).
Gilron, I. et al. Combination of pregabalin with duloxetine for fibromyalgia. Pain 157, 1532–1540 (2016).
Arnold, L. M. et al. Efficacy and safety of pregabalin in patients with fibromyalgia and comorbid depression taking concurrent antidepressant medication: a randomized, placebo-controlled study. J. Rheumatol. 42, 1237–1244 (2015).
Bernardy, K., Klose, P., Welsch, P. & Häuser, W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome - A systematic review and meta-analysis of randomized controlled trials. Eur. J. Pain 22, 242–260 (2018).
Jacobs, H. et al. The impact of a group-based multidisciplinary rehabilitation program on the quality of life in patients with fibromyalgia: results from the QUALIFIBRO Study. J. Clin. Rheumatol. https://doi.org/10.1097/RHU.0000000000001120 (2019).
Bernardy, K., Klose, P., Welsch, P. & Häuser, W. Efficacy, acceptability and safety of Internet-delivered psychological therapies for fibromyalgia syndrome: a systematic review and meta-analysis of randomized controlled trials. Eur. J. Pain 23, 3–14 (2019).
Perrot, S. & Russell, I. J. More ubiquitous effects from non-pharmacologic than from pharmacologic treatments for fibromyalgia syndrome: a meta-analysis examining six core symptoms. Eur. J. Pain 18, 1067–1080 (2014).
Gálvez, I., Torres-Piles, S. & Ortega-Rincón, E. Balneotherapy, immune system, and stress response: a hormetic strategy? Int. J. Mol. Sci. 19, 1687 (2018).
Naumann, J. & Sadaghiani, C. Therapeutic benefit of balneotherapy and hydrotherapy in the management of fibromyalgia syndrome: a qualitative systematic review and meta-analysis of randomized controlled trials. Arthritis Res. Ther. 16, R141 (2014).
Fioravanti, A. et al. Is balneotherapy effective for fibromyalgia? Results from a 6-month double-blind randomized clinical trial. Clin. Rheumatol. 37, 2203–2212 (2018).
Honda Y. et al. Effects of physical-agent pain relief modalities for fibromyalgia patients: a systematic review and meta-analysis of randomized controlled trials. Pain Res. Manag. https://doi.org/10.1155/2018/2930632 (2018).
Kurt, E. E., Koçak, F. A., Erdem, H. R., Tuncay, F. & Kelez, F. Which non-pharmacological treatment is more effective on clinical parameters in patients with fibromyalgia: balneotherapy or aerobic exercise? Arch. Rheumatol. 31, 162–169 (2016).
Guidelli, G. M., Tenti, S., de Nobili, E. & Fioravanti, A. Fibromyalgia syndrome and spa therapy: myth or reality? Clin. Med. Insights Arthritis Musculoskelet. Disord. 5, 19–26 (2012).
Langhorst, J., Klose, P., Dobos, G. J., Bernardy, K. & Häuser, W. Efficacy and safety of meditative movement therapies in fibromyalgia syndrome: a systematic review and meta-analysis of randomized controlled trials. Rheumatol. Int. 33, 193–207 (2013).
Mist, S. D., Firestone, K. A. & Jones, K. D. Complementary and alternative exercise for fibromyalgia: a meta-analysis. J. Pain Res. 6, 247–260 (2013).
Cheng, C.-A. et al. Effectiveness of Tai Chi on fibromyalgia patients: a meta-analysis of randomized controlled trials. Complement. Ther. Med. 46, 1–8 (2019).
Wang, C. et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ 360, k851 (2018).
Van Gordon, W., Shonin, E., Dunn, T. J., Garcia-Campayo, J. & Griffiths, M. D. Meditation awareness training for the treatment of fibromyalgia syndrome: a randomized controlled trial. Br. J. Health Psychol. 22, 186–206 (2017).
Haugmark, T., Hagen, K. B., Smedslund, G. & Zangi, H. A. Mindfulness- and acceptance-based interventions for patients with fibromyalgia — a systematic review and meta-analyses. PLoS One 14, e0221897 (2019).
Lauche, R., Cramer, H., Dobos, G., Langhorst, J. & Schmidt, S. A systematic review and meta-analysis of mindfulness-based stress reduction for the fibromyalgia syndrome. J. Psychosom. Res. 75, 500–510 (2013).
Luciano, J. V. et al. Effectiveness of group acceptance and commitment therapy for fibromyalgia: A 6-month randomized controlled trial (EFFIGACT study). Pain 155, 693–702 (2014).
Luciano, J. V. et al. Cost-utility of group acceptance and commitment therapy for fibromyalgia versus recommended Drugs: an economic analysis alongside a 6-month randomized controlled trial conducted in Spain (EFFIGACT Study). J. Pain 18, 868–880 (2017).
Jensen, M. P. Hypnosis for chronic pain management: a new hope. Pain 146, 235–237 (2009).
Zech, N., Hansen, E., Bernardy, K. & Häuser, W. Efficacy, acceptability and safety of guided imagery/hypnosis in fibromyalgia — a systematic review and meta-analysis of randomized controlled trials. Eur. J. Pain 21, 217–227 (2017).
Deare, J. C. et al. Acupuncture for treating fibromyalgia. Cochrane Database Syst. Rev. 2013, CD007070 (2013).
Yang, B. et al. Efficacy of acupuncture on fibromyalgia syndrome: a meta-analysis. J. Tradit. Chin. Med. 34, 381–391 (2014).
Atzeni, F. et al. Hyperbaric oxygen treatment of fibromyalgia: a prospective observational clinical study. Clin. Exp. Rheumatol. 37, 63–69 (2019).
Efrati, S. et al. Hyperbaric oxygen therapy can diminish fibromyalgia syndrome — prospective clinical trial. PLoS ONE 10, e0127012 (2015).
Moisset, X., Lanteri-Minet, M. & Fontaine, D. Neurostimulation methods in the treatment of chronic pain. J. Neural Transm. 127, 673–686 (2020).
Atzeni, F. et al. Hyperbaric oxygen therapy in fibromyalgia and the diseases involving the central nervous system. Clin. Exp. Rheumatol. 38, S94–S98 (2020).
Brighina, F. et al. Brain modulation by electric currents in fibromyalgia: a structured review on non-invasive approach with transcranial electrical stimulation. Front. Hum. Neurosci. 11, 13–40 (2019).
Mhalla, A. et al. Long-term maintenance of the analgesic effects of transcranial magnetic stimulation in fibromyalgia. Pain 152, 1478–1485 (2011).
López-Solà, M. et al. Towards a neurophysiological signature for fibromyalgia. Pain 158, 34–47 (2017).
Clauw, D. J., Essex, M. N., Pitman, V. & Jones, K. D. Reframing chronic pain as a disease, not a symptom: rationale and implications for pain management. Postgrad. Med. 131, 185–198 (2019).
Bennett, R. Fibromyalgia: shining a light on fibromyalgia treatment. Nat. Rev. Rheumatol. 12, 568–569 (2016).
Arnold, L. M. Duloxetine and other antidepressants in the treatment of patients with fibromyalgia. Pain Med. 8, S63–S74 (2007).
Tzellos, T. G. et al. Gabapentin and pregabalin in the treatment of fibromyalgia: a systematic review and a meta-analysis. J. Clin. Pharm. Ther. 35, 639–656 (2010).
Üçeyler, N., Sommer, C., Walitt, B. & Häuser, W. Anticonvulsants for fibromyalgia. Cochrane Database Syst. Rev. 2017, 2–5 (2017).
Sarzi-Puttini, P. et al. Cannabinoids in the treatment of rheumatic diseases: pros and cons. Autoimmun. Rev. 18, 102409 (2019).
Food and Drug Administration. Drug approval package: Cymbalta (duloxetine hydrochloride), 20, 30, and 60 mg capsules. FDA https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022516_cymbalta_tocEDT.cfm (2010).
IBM Micromedex. Duloxetine (Oral Route). Mayo Foundation for Medical Education and Research (MFMER). https://www.mayoclinic.org/drugs-supplements/duloxetine-oral-route/side-effects/drg-20067247 (2020).
IBM Micromedex. Milnacipran (Oral Route). Mayo Foundation for Medical Education and Research (MFMER)2. https://www.mayoclinic.org/drugs-supplements/milnacipran-oral-route/side-effects/drg-20072479 (2020).
U.S. Food and Drug Administration. Drug approval package: Savella (Milnacipran HCI) Tablets. FDA https://www.accessdata.fda.gov/drugsatfda_docs/nda/2009/022256s000TOC.cfm (2009).
U.S. Food and Drug Administration. Drug approval package: Lyrica (pregabalin) Oral Solution 20 mg/ml. FDA https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022488_lyrica_toc.cfm (2010).
Author information
Authors and Affiliations
Contributions
P.S.-P., V.G. and D.M. wrote the article. P.S.-P. and F.A. substantially contributed to discussion of content. P.S.-P., V.G., D.M. and F.A. researched data for the article and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Rheumatology thanks M.-A. Fitzcharles, G. Littlejohn and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Biopsychosocial model of medicine
-
An interdisciplinary model commonly used in the field of chronic pain that incorporates the interactions among biological factors (such as physio-pathological factors), psychosocial factors (that is, emotional factors, such as distress or fear) and behavioural factors.
- Paraesthesia
-
A qualitative alteration of the sensitivity of the skin (which can be an abnormal sensation of pricking, tingling and numbness).
- Fibro-fog
-
A symptom of fibromyalgia involving an inability to think clearly or difficulties in concentrating.
- Raynaud phenomenon
-
A condition that causes decreased blood flow to the extremities (such as the fingers, toes, ears and nose) due to vasospasm; such spasms occur in response to cold, stress or emotional upset.
- Nociplastic pain
-
A clinical definition of pain arising from altered nociception, despite no evidence of tissue damage causing the activation of nociceptors or evidence of disease or lesions of the somatosensory system causing the pain.
- Central sensitization
-
A neurophysiological process of pain amplification in the central nervous system; this process occurs physiologically after injuries to elicit a protective behaviour and maximize the healing process.
- Hyperalgesia
-
A condition in which a painful stimulus is perceived as being even more painful.
- Allodynia
-
A condition in which a normal stimulus is perceived as being painful.
- Temporal summation
-
The perception of repetitive noxious stimulation as being increasingly painful.
- Dysaesthesia
-
An unpleasant abnormal sensation (that can be spontaneous or evoked) that is usually associated with irritation or injury to a sensory nerve or nerve root.
- Small fibre neuropathy
-
Damage to small myelinated (type Aδ) nerve fibres or unmyelinated C peripheral nerve fibres; these small somatic fibres have sensory functions including thermal perception and nociception.
- Dysautonomia
-
An umbrella term used to describe several different medical conditions that cause a malfunction of the autonomic nervous system.
- Catastrophizing
-
An exaggerated amplification of emotional aspects that leads individuals to consider pain terrible and intolerable.
Rights and permissions
About this article
Cite this article
Sarzi-Puttini, P., Giorgi, V., Marotto, D. et al. Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nat Rev Rheumatol 16, 645–660 (2020). https://doi.org/10.1038/s41584-020-00506-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-020-00506-w
This article is cited by
-
The role of lifestyle factors in the association between education and self-reported fibromyalgia: a mediation analysis
BMC Women's Health (2024)
-
Identification of unique genomic signatures in patients with fibromyalgia and chronic pain
Scientific Reports (2024)
-
Stress Response Pattern of Heart Rate Variability in Patients with Functional Somatic Syndromes
Applied Psychophysiology and Biofeedback (2024)
-
Pharmacological Evidence of Eugenia Brasiliensis Leaves in a Reserpine-Induced Fibromyalgia Model: Antinociceptive, Emotional, Anti-Inflammatory, and Neurotrophic Effects
Molecular Neurobiology (2024)
-
Does self-efficacy mediate the relationship between disease impact and depression symptoms among people with fibromyalgia? A longitudinal multilevel mediation model
Current Psychology (2024)