Abstract
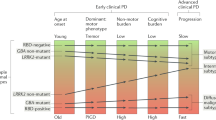
Many advances in understanding the pathophysiology of Parkinson disease (PD) have been based on research addressing its motor symptoms and phenotypes. Various data-driven clinical phenotyping studies supported by neuropathological and in vivo neuroimaging data suggest the existence of distinct non-motor endophenotypes of PD even at diagnosis, a concept further strengthened by the predominantly non-motor spectrum of symptoms in prodromal PD. Preclinical and clinical studies support early dysfunction of noradrenergic transmission in both the CNS and peripheral nervous system circuits in patients with PD that results in a specific cluster of non-motor symptoms, including rapid eye movement sleep behaviour disorder, pain, anxiety and dysautonomia (particularly orthostatic hypotension and urinary dysfunction). Cluster analyses of large independent cohorts of patients with PD and phenotype-focused studies have confirmed the existence of a noradrenergic subtype of PD, which had been previously postulated but not fully characterized. This Review discusses the translational work that unravelled the clinical and neuropathological processes underpinning the noradrenergic PD subtype. Although some overlap with other PD subtypes is inevitable as the disease progresses, recognition of noradrenergic PD as a distinct early disease subtype represents an important advance towards the delivery of personalized medicine for patients with PD.
Key points
-
Parkinson disease (PD) is a phenotypically heterogeneous, multisystem condition that affects the CNS and peripheral nervous system as well as multiple neurotransmitters, rather than a single ‘disease’.
-
PD can present at diagnosis with motor-predominant and non-motor-predominant symptoms.
-
Neuropathological studies, neuroimaging findings and data from animal models suggest that PD with specific non-motor-predominant symptoms is driven by noradrenergic dysfunction in the CNS and peripheral nervous system.
-
Cluster analyses and clinical phenotyping studies confirm the association between PD with specific non-motor-predominant symptoms and noradrenergic dysfunction.
-
The noradrenergic phenotype of PD includes key features of rapid eye movement sleep behaviour disorder and dysautonomia (including orthostatic hypotension and/or urinary dysfunction), pain and anxiety.
-
Formal identification of the noradrenergic phenotype as a clinical subtype of PD would help to define its natural history and promote the development of subtype-specific personalized treatment.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Dorsey, E. R., Sherer, T., Okun, M. S. & Bloem, B. R. The emerging evidence of the Parkinson pandemic. J. Parkinsons Dis. 8, S3–S8 (2018).
Schapira, A. H. V., Chaudhuri, K. R. & Jenner, P. Non-motor features of Parkinson disease. Nat. Rev. Neurosci. 18, 435–450 (2017).
Jellinger, K. A. Neuropathology of sporadic Parkinson’s disease: evaluation and changes of concepts. Mov. Disord. 27, 8–30 (2012).
Calne, D. B. Is “Parkinson’s disease” one disease? J. Neurol. Neurosurg. Psychiatry 52, 18–21 (1989).
Weiner, W. J. There is no Parkinson disease. Arch. Neurol. 65, 705–708 (2008).
Titova, N., Padmakumar, C., Lewis, S. J. G. & Chaudhuri, K. R. Parkinson’s: a syndrome rather than a disease? J. Neural Transm. 124, 907–914 (2017).
Langston, J. W. The Parkinson’s complex: parkinsonism is just the tip of the iceberg. Ann. Neurol. 59, 591–596 (2006).
Bellucci, A. et al. Review: Parkinson’s disease: from synaptic loss to connectome dysfunction. Neuropathol. Appl. Neurobiol. 42, 77–94 (2016).
Berg, D. et al. MDS research criteria for prodromal Parkinson’s disease. Mov. Disord. 30, 1600–1611 (2015).
Chaudhuri, K. R., Jenner, P. & Antonini, A. Should there be less emphasis on levodopa-induced dyskinesia in Parkinson’s disease? Mov. Disord. 34, 816–819 (2019).
Seppi, K. et al. Update on treatments for nonmotor symptoms of Parkinson’s disease – an evidence-based medicine review. Mov. Disord. 34, 180–198 (2019).
Postuma, R. B. et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 30, 1591–1601 (2015).
Marras, C. & Chaudhuri, K. R. Nonmotor features of Parkinson’s disease subtypes. Mov. Disord. 31, 1095–1102 (2016).
Kingsbury, A. E. et al. Brain stem pathology in Parkinson’s disease: an evaluation of the Braak staging model. Mov. Disord. 25, 2508–2515 (2010).
Ahmed, S. S., Santosh, W., Kumar, S. & Christlet, H. T. Metabolic profiling of Parkinson’s disease: evidence of biomarker from gene expression analysis and rapid neural network detection. J. Biomed. Sci. 16, 63 (2009).
Marras, C. & Lang, A. Parkinson’s disease subtypes: lost in translation. J. Neurol. Neurosurg. Psychiatry 84, 409–415 (2013).
Jankovic, J. & Tan, E. K. Parkinson’s disease: etiopathogenesis and treatment. J. Neurol. Neurosurg. Psychiatry 91, 795–808 (2020).
Goldstein, D. S. & Sharabi, Y. The heart of PD: Lewy body diseases as neurocardiologic disorders. Brain Res. 1702, 74–84 (2019).
Goldstein, D. S. et al. Catechols in post-mortem brain of patients with Parkinson disease. Eur. J. Neurol. 18, 703–710 (2011).
Sauerbier, A., Jenner, P., Todorova, A. & Chaudhuri, K. R. Non motor subtypes and Parkinson’s disease. Parkinsonism Relat. Disord. 22, S41–S46 (2016).
Tipre, D. N. & Goldstein, D. S. Cardiac and extracardiac sympathetic denervation in Parkinson’s disease with orthostatic hypotension and in pure autonomic failure. J. Nucl. Med. 46, 1775–1781 (2005).
Bohnen, N. I. et al. Cholinergic system changes in Parkinson’s disease: emerging therapeutic approaches. Lancet Neurol. 21, 381–392 (2022).
Nahimi, A. et al. Noradrenergic deficits in Parkinson disease imaged with 11C-MeNER. J. Nucl. Med. 59, 659–664 (2018).
Remy, P., Doder, M., Lees, A., Turjanski, N. & Brooks, D. Depression in Parkinson’s disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain 128, 1314–1322 (2005).
Pavese, N., Metta, V., Bose, S. K., Chaudhuri, K. R. & Brooks, D. J. Fatigue in Parkinson’s disease is linked to striatal and limbic serotonergic dysfunction. Brain 133, 3434–3443 (2010).
Pasquini, J., Brooks, D. J. & Pavese, N. The cholinergic brain in Parkinson’s disease. Mov. Disord. Clin. Pract. 8, 1012–1026 (2021).
Wilson, H., Giordano, B., Turkheimer, F. E., Chaudhuri, K. R. & Politis, M. Serotonergic dysregulation is linked to sleep problems in Parkinson’s disease. Neuroimage Clin. 18, 630–637 (2018).
Erro, R. et al. The heterogeneity of early Parkinson’s disease: a cluster analysis on newly diagnosed untreated patients. PLoS ONE 8, e70244 (2013).
Mu, J. et al. Parkinson’s disease subtypes identified from cluster analysis of motor and non-motor symptoms. Front. Aging Neurosci. 9, 301 (2017).
Espay, A. J., LeWitt, P. A. & Kaufmann, H. Norepinephrine deficiency in Parkinson’s disease: the case for noradrenergic enhancement. Mov. Disord. 29, 1710–1719 (2014).
Titova, N. & Chaudhuri, K. R. Personalized medicine in Parkinson’s disease: time to be precise. Mov. Disord. 32, 1147–1154 (2017).
Leta, V. et al. Personalised advanced therapies in Parkinson’s disease: the role of non-motor symptoms profile. J. Pers. Med. https://doi.org/10.3390/jpm11080773 (2021).
Marras, C., Chaudhuri, K. R., Titova, N. & Mestre, T. A. Therapy of Parkinson’s disease subtypes. Neurotherapeutics 17, 1366–1377 (2020).
Greenland, J. C., Williams-Gray, C. H. & Barker, R. A. The clinical heterogeneity of Parkinson’s disease and its therapeutic implications. Eur. J. Neurosci. 49, 328–338 (2019).
Ghosh, P. et al. A dual centre study of pain in Parkinson’s disease and its relationship with other non-motor symptoms. J. Parkinsons Dis. 10, 1817–1825 (2020).
Matsui, H. et al. Metaiodobenzylguanidine (MIBG) uptake in Parkinson’s disease also decreases at thyroid. Ann. Nucl. Med. 19, 225–229 (2005).
Benarroch, E. E. Locus coeruleus. Cell Tissue Res. 373, 221–232 (2018).
Blesa, J., Trigo-Damas, I. & Obeso, J. A. Parkinson’s disease and thalamus: facts and fancy. Lancet Neurol. 15, e2 (2016).
Pifl, C., Kish, S. J. & Hornykiewicz, O. Thalamic noradrenaline in Parkinson’s disease: deficits suggest role in motor and non-motor symptoms. Mov. Disord. 27, 1618–1624 (2012).
Zerbi, V. et al. Rapid reconfiguration of the functional connectome after chemogenetic locus coeruleus activation. Neuron 103, 702–718.e5 (2019).
Mills, E. P. et al. Brainstem pain-control circuitry connectivity in chronic neuropathic pain. J. Neurosci. 38, 465–473 (2018).
Jacob, S. N. & Nienborg, H. Monoaminergic neuromodulation of sensory processing. Front. Neural Circuits 12, 51 (2018).
Bylund, D. B. et al. International Union of Pharmacology nomenclature of adrenoceptors. Pharmacol. Rev. 46, 121–136 (1994).
Hieble, J. P. et al. International Union of Pharmacology. X. Recommendation for nomenclature of α1-adrenoceptors: consensus update. Pharmacol. Rev. 47, 267–270 (1995).
Zhou, J. Norepinephrine transporter inhibitors and their therapeutic potential. Drugs Future 29, 1235–1244 (2004).
Abosamak, N. R. & Shahin, M. H. Beta 2 Receptor Agonists/Antagonists (StatPearls, 2023).
German, D. C. et al. Disease-specific patterns of locus coeruleus cell loss. Ann. Neurol. 32, 667–676 (1992).
Bertrand, E., Lechowicz, W., Szpak, G. M. & Dymecki, J. Qualitative and quantitative analysis of locus coeruleus neurons in Parkinson’s disease. Folia Neuropathol. 35, 80–86 (1997).
Braak, E. et al. α-Synuclein immunopositive Parkinson’s disease-related inclusion bodies in lower brain stem nuclei. Acta Neuropathol. 101, 195–201 (2001).
Zarow, C., Lyness, S. A., Mortimer, J. A. & Chui, H. C. Neuronal loss is greater in the locus coeruleus than nucleus basalis and substantia nigra in Alzheimer and Parkinson diseases. Arch. Neurol. 60, 337–341 (2003).
Paulus, W. & Jellinger, K. The neuropathologic basis of different clinical subgroups of Parkinson’s disease. J. Neuropathol. Exp. Neurol. 50, 743–755 (1991).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211 (2003).
Goldstein, D. S. et al. Differential abnormalities of cerebrospinal fluid dopaminergic versus noradrenergic indices in synucleinopathies. J. Neurochem. 158, 554–568 (2021).
Huynh, B., Fu, Y., Kirik, D., Shine, J. M. & Halliday, G. M. Comparison of locus coeruleus pathology with nigral and forebrain pathology in Parkinson’s disease. Mov. Disord. 36, 2085–2093 (2021).
Antonini, A. et al. The progression of non-motor symptoms in Parkinson’s disease and their contribution to motor disability and quality of life. J. Neurol. 259, 2621–2631 (2012).
Fereshtehnejad, S. M. et al. New clinical subtypes of Parkinson disease and their longitudinal progression: a prospective cohort comparison with other phenotypes. JAMA Neurol. 72, 863–873 (2015).
Isonaka, R., Sullivan, P. & Goldstein, D. S. Pathophysiological significance of increased α-synuclein deposition in sympathetic nerves in Parkinson’s disease: a post-mortem observational study. Transl. Neurodegener. 11, 15 (2022).
Todorova, A., Jenner, P. & Chaudhuri, K. R. Non-motor Parkinson’s: integral to motor Parkinson’s, yet often neglected. Pract. Neurol. 14, 310–322 (2014).
Coughlin, D. G., Hurtig, H. I. & Irwin, D. J. Pathological influences on clinical heterogeneity in Lewy body diseases. Mov. Disord. 35, 5–19 (2020).
Priovoulos, N. et al. High-resolution in vivo imaging of human locus coeruleus by magnetization transfer MRI at 3T and 7T. Neuroimage 168, 427–436 (2018).
Betts, M. J. et al. Locus coeruleus imaging as a biomarker for noradrenergic dysfunction in neurodegenerative diseases. Brain 142, 2558–2571 (2019).
García-Lorenzo, D. et al. The coeruleus/subcoeruleus complex in rapid eye movement sleep behaviour disorders in Parkinson’s disease. Brain 136, 2120–2129 (2013).
Kinnerup, M. B. et al. Preserved noradrenergic function in Parkinson’s disease patients with rest tremor. Neurobiol. Dis. 152, 105295 (2021).
Sommerauer, M. et al. Evaluation of the noradrenergic system in Parkinson’s disease: an 11C-MeNER PET and neuromelanin MRI study. Brain 141, 496–504 (2018).
Knudsen, K. et al. In-vivo staging of pathology in REM sleep behaviour disorder: a multimodality imaging case–control study. Lancet Neurol. 17, 618–628 (2018).
Horsager, J. et al. Brain-first versus body-first Parkinson’s disease: a multimodal imaging case–control study. Brain 143, 3077–3088 (2020).
Doppler, C. E. J. et al. Regional locus coeruleus degeneration is uncoupled from noradrenergic terminal loss in Parkinson’s disease. Brain 144, 2732–2744 (2021).
Doppler, C. E. J. et al. Microsleep disturbances are associated with noradrenergic dysfunction in Parkinson’s disease. Sleep https://doi.org/10.1093/sleep/zsab040 (2021).
Ye, R. et al. Locus coeruleus integrity from 7 T MRI relates to apathy and cognition in parkinsonian disorders. Mov. Disord. https://doi.org/10.1002/mds.29072 (2022).
Madelung, C. F. et al. Locus coeruleus shows a spatial pattern of structural disintegration in Parkinson’s disease. Mov. Disord. 37, 479–489 (2022).
Janzen, A. et al. Rapid eye movement sleep behavior disorder: abnormal cardiac image and progressive abnormal metabolic brain pattern. Mov. Disord. 37, 624–629 (2022).
Nagayama, H., Hamamoto, M., Ueda, M., Nagashima, J. & Katayama, Y. Reliability of MIBG myocardial scintigraphy in the diagnosis of Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 76, 249–251 (2005).
Goldstein, D. S., Holmes, C., Cannon, R. O. III, Eisenhofer, G. & Kopin, I. J. Sympathetic cardioneuropathy in dysautonomias. N. Engl. J. Med. 336, 696–702 (1997).
Saiki, S. et al. Cardiac 123I-MIBG scintigraphy can assess the disease severity and phenotype of PD. J. Neurol. Sci. 220, 105–111 (2004).
Goldstein, D. S. & Cheshire, W. P. Jr Roles of cardiac sympathetic neuroimaging in autonomic medicine. Clin. Auton. Res. 28, 397–410 (2018).
Halliday, G. M. & Stevens, C. H. Glia: initiators and progressors of pathology in Parkinson’s disease. Mov. Disord. 26, 6–17 (2011).
Mollenhauer, B. et al. Nonmotor and diagnostic findings in subjects with de novo Parkinson disease of the DeNoPa cohort. Neurology 81, 1226–1234 (2013).
Zis, P., Erro, R., Walton, C. C., Sauerbier, A. & Chaudhuri, K. R. The range and nature of non-motor symptoms in drug-naive Parkinson’s disease patients: a state-of-the-art systematic review. NPJ Parkinsons Dis. 1, 15013 (2015).
Pont-Sunyer, C. et al. The onset of nonmotor symptoms in Parkinson’s disease (the ONSET PD study). Mov. Disord. 30, 229–237 (2015).
van Rooden, S. M. et al. Clinical subtypes of Parkinson’s disease. Mov. Disord. 26, 51–58 (2011).
Rodriguez-Sanchez, F. et al. Identifying Parkinson’s disease subtypes with motor and non-motor symptoms via model-based multi-partition clustering. Sci. Rep. 11, 23645 (2021).
MacQueen, J.B. Some methods for classification and analysis of multivariate observations. In Proc. Fifth Berkeley Symposium on Mathematical Statistics and Probability (eds Le Cam, L. M. & Neyman, J.) 281–297 (Univ. California Press, 1967).
Lazarsfeld, P. F. & Henry, N. W. in The American Soldier vol. 4: Measurement and Prediction (Houghton Mifflin, 1968).
Gordon, A. D. A review of hierarchical classification. J. R. Stat. Soc. A 150, 119–137 (1987).
Warren, J. D. et al. Molecular nexopathies: a new paradigm of neurodegenerative disease. Trends Neurosci. 36, 561–569 (2013).
van de Berg, W. D. et al. Patterns of α-synuclein pathology in incidental cases and clinical subtypes of Parkinson’s disease. Parkinsonism Relat. Disord. 18, S28–S30 (2012).
Adler, C. H. & Beach, T. G. Neuropathological basis of nonmotor manifestations of Parkinson’s disease. Mov. Disord. 31, 1114–1119 (2016).
Ahlskog, J. E. Challenging conventional wisdom: the etiologic role of dopamine oxidative stress in Parkinson’s disease. Mov. Disord. 20, 271–282 (2005).
van Wamelen, D. J. et al. Cross-sectional analysis of the Parkinson’s Disease Non-motor International Longitudinal Study baseline non-motor characteristics, geographical distribution and impact on quality of life. Sci. Rep. 11, 9611 (2021).
Williams-Gray, C. H. et al. The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the Campaign cohort. Brain 132, 2958–2969 (2009).
Weintraub, D. et al. Cognitive performance and neuropsychiatric symptoms in early, untreated Parkinson’s disease. Mov. Disord. 30, 919–927 (2015).
Szeto, J. Y. et al. The relationships between mild cognitive impairment and phenotype in Parkinson’s disease. NPJ Parkinsons Dis. 1, 15015 (2015).
Aarsland, D. et al. Parkinson disease-associated cognitive impairment. Nat. Rev. Dis. Prim. 7, 47 (2021).
Mizutani, Y. et al. Hyposmia and cardiovascular dysautonomia correlatively appear in early-stage Parkinson’s disease. Parkinsonism Relat. Disord. 20, 520–524 (2014).
Kim, J. S. et al. Orthostatic hypotension and cardiac sympathetic denervation in Parkinson disease patients with REM sleep behavioral disorder. J. Neurol. Sci. 362, 59–63 (2016).
Rizos, A. et al. Characterizing motor and non-motor aspects of early-morning off periods in Parkinson’s disease: an international multicenter study. Parkinsonism Relat. Disord. 20, 1231–1235 (2014).
Goldstein, D. S., Holmes, C., Sharabi, Y. & Wu, T. Survival in synucleinopathies: a prospective cohort study. Neurology 85, 1554–1561 (2015).
Kaufmann, H. et al. Natural history of pure autonomic failure: a United States prospective cohort. Ann. Neurol. 81, 287–297 (2017).
Fearon, C., Lang, A. E. & Espay, A. J. The logic and pitfalls of Parkinson’s disease as “brain-first” versus “body-first” subtypes. Mov. Disord. 36, 594–598 (2021).
Ross, S. B. & Stenfors, C. DSP4, a selective neurotoxin for the locus coeruleus noradrenergic system. A review of its mode of action. Neurotox. Res. 27, 15–30 (2015).
Srinivasan, J. & Schmidt, W. J. Potentiation of parkinsonian symptoms by depletion of locus coeruleus noradrenaline in 6-hydroxydopamine-induced partial degeneration of substantia nigra in rats. Eur. J. Neurosci. 17, 2586–2592 (2003).
Li, Y. et al. Investigation of behavioral dysfunctions induced by monoamine depletions in a mouse model of Parkinson’s disease. Front. Cell Neurosci. 12, 241 (2018).
Schintu, N., Zhang, X. & Svenningsson, P. Studies of depression-related states in animal models of Parkinsonism. J. Parkinsons Dis. 2, 87–106 (2012).
Delaville, C. et al. Emerging dysfunctions consequent to combined monoaminergic depletions in Parkinsonism. Neurobiol. Dis. 45, 763–773 (2012).
Hauser, J., Sontag, T. A., Tucha, O. & Lange, K. W. The effects of the neurotoxin DSP4 on spatial learning and memory in Wistar rats. ADHD Atten. Deficit Hyperactivity Disord. 4, 93–99 (2012).
Song, S. et al. Noradrenergic dysfunction accelerates LPS-elicited inflammation-related ascending sequential neurodegeneration and deficits in non-motor/motor functions. Brain Behav. Immun. 81, 374–387 (2019).
Paredes-Rodriguez, E., Vegas-Suarez, S., Morera-Herreras, T., De Deurwaerdere, P. & Miguelez, C. The noradrenergic system in Parkinson’s disease. Front. Pharmacol. 11, 435 (2020).
Delaville, C., Deurwaerdère, P. D. & Benazzouz, A. Noradrenaline and Parkinson’s disease. Front. Syst. Neurosci. 5, 31 (2011).
Kucharczyk, M. W., Di Domenico, F. & Bannister, K. Distinct brainstem to spinal cord noradrenergic pathways inversely regulate spinal neuronal activity. Brain 145, 2293–2300 (2022).
Chesselet, M. F. et al. A progressive mouse model of Parkinson’s disease: the Thy1-aSyn (“Line 61”) mice. Neurotherapeutics 9, 297–314 (2012).
McDowell, K. A., Shin, D., Roos, K. P. & Chesselet, M. F. Sleep dysfunction and EEG alterations in mice overexpressing α-synuclein. J. Parkinsons Dis. 4, 531–539 (2014).
Hallett, P. J., McLean, J. R., Kartunen, A., Langston, J. W. & Isacson, O. α-Synuclein overexpressing transgenic mice show internal organ pathology and autonomic deficits. Neurobiol. Dis. 47, 258–267 (2012).
Sotiriou, E., Vassilatis, D. K., Vila, M. & Stefanis, L. Selective noradrenergic vulnerability in α-synuclein transgenic mice. Neurobiol. Aging 31, 2103–2114 (2010).
Henrich, M. T. et al. A53T-α-synuclein overexpression in murine locus coeruleus induces Parkinson’s disease-like pathology in neurons and glia. Acta Neuropathol. Commun. 6, 39 (2018).
Butkovich, L. M. et al. Transgenic mice expressing human α-synuclein in noradrenergic neurons develop locus ceruleus pathology and nonmotor features of Parkinson’s disease. J. Neurosci. 40, 7559–7576 (2020).
Hunsley, M. S. & Palmiter, R. D. Norepinephrine-deficient mice exhibit normal sleep-wake states but have shorter sleep latency after mild stress and low doses of amphetamine. Sleep 26, 521–526 (2003).
Kim, S. et al. Transneuronal propagation of pathologic α-synuclein from the gut to the brain models Parkinson’s disease. Neuron 103, 627–641.e7 (2019).
Jovanovic, P. et al. Sustained chemogenetic activation of locus coeruleus norepinephrine neurons promotes dopaminergic neuron survival in synucleinopathy. PLoS ONE 17, e0263074 (2022).
Giorgi, F. S. et al. Locus coeruleus modulates neuroinflammation in parkinsonism and dementia. Int. J. Mol. Sci. https://doi.org/10.3390/ijms21228630 (2020).
Taylor, T. N. et al. Nonmotor symptoms of Parkinson’s disease revealed in an animal model with reduced monoamine storage capacity. J. Neurosci. 29, 8103–8113 (2009).
Cui, K. et al. Restoration of noradrenergic function in Parkinson’s disease model mice. ASN Neuro 13, 17590914211009730 (2021).
Taylor, N. L. et al. The contribution of noradrenergic activity to anxiety-induced freezing of gait. Mov. Disord. 37, 1432–1443 (2022).
Chaudhuri, K. R., Titova, N., Qamar, M. A., Murășan, I. & Falup-Pecurariu, C. The dashboard vitals of Parkinson’s: not to be missed yet an unmet need. J. Pers. Med. 12, 1994 (2022).
Hely, M. A., Reid, W. G., Adena, M. A., Halliday, G. M. & Morris, J. G. The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov. Disord. 23, 837–844 (2008).
Halliday, G. M., Leverenz, J. B., Schneider, J. S. & Adler, C. H. The neurobiological basis of cognitive impairment in Parkinson’s disease. Mov. Disord. 29, 634–650 (2014).
Goodall, M., Kirshner, N. & Rosen, L. Metabolism of noradrenaline in the human. J. Clin. Invest. 38, 707–714 (1959).
Acknowledgements
The views expressed are those of the authors and not necessarily those of the UK National Health Service (NHS), National Institutes of Health Research (NIHR) or the Department of Health. The authors acknowledge the support of the International Parkinson and Movement Disorder Society Non-Motor PD Study Group, the NIHR London South Clinical Research Network and the NIHR Biomedical Research Centre. The authors’ independent collaborative research is part funded by the NIHR Biomedical Research Centre at South London, Maudsley NHS Foundation Trust and King’s College London. P.S. is supported by the John and Lucille Van Geest Foundation. K.R.C. is supported by NIHR Biomedical Research Centre at South London, Maudsley NHS Foundation Trust and King’s College London and the Parkinson Foundation, USA.
Author information
Authors and Affiliations
Contributions
K.R.C. conceived and designed this work. All authors wrote the first draft of the manuscript, contributed to discussions of the article content and critical review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
K.R.C. declares that he has received honoraria for advisory board membership from 4D Pharma, AbbVie, Acadia, Britannia, Global kinetics (GKC), Lobsor, Profile Pharma, Roche, Scion, Stada, Synovion, Therevance, UCB and Zambon; speaker’s honoraria for lectures from AbbVie, Bial, Boeringer Ingelheim, Britannia, Kyowa Kirin, Novartis, SK Pharma, UCB, and Zambon; investigator initiated research grants from AbbVie, Bial; Britannia, UCB, Global Kinetics; and academic grant funding from EU Horizon 2020, Parkinson’s UK, Wellcome Trust, Kirby Laing Foundation and the Medical Research Council; royalty payments or license fees from Oxford University Press, and Cambridge University Press, MAPI institute (King’s Parkinson Disease Pain Scale (KPPS) and Parkinson Disease Sleep Scale 2 (PDSS-2)); and payment for expert testimony from the General Medical Council unrelated to the submitted work. V.L. declares that she has received grants and/or honoraria for speaker-related activities from Abbvie, Bial, Britannia Pharmaceuticals, Invisio, Profile and UCB unrelated to the submitted work. P.S. declares that he has received honoraria for advisory board membership from AbbVie, Kyowa Kirin and Takeda; honoraria for lectures from AbbVie and Zambon; and academic grants from, Lexa International/Nordstjernan, Michael J. Fox Foundation, Stockholm City Council and Wallenberg Clinical Scholarship unrelated to the submitted work. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks Daniela Berg and the other, anonymous, reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ray Chaudhuri, K., Leta, V., Bannister, K. et al. The noradrenergic subtype of Parkinson disease: from animal models to clinical practice. Nat Rev Neurol 19, 333–345 (2023). https://doi.org/10.1038/s41582-023-00802-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-023-00802-5
This article is cited by
-
Constipation and pain in Parkinson’s disease: a clinical analysis
Journal of Neural Transmission (2024)
-
Parkinson’s disease motor progression in relation to the timing of REM sleep behavior disorder presentation: an exploratory retrospective study
Journal of Neural Transmission (2024)