Abstract
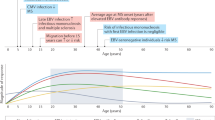
Epidemiological studies have provided compelling evidence that multiple sclerosis (MS) is a rare complication of infection with the Epstein–Barr virus (EBV), a herpesvirus that infects more than 90% of the global population. This link was long suspected because the risk of MS increases markedly after infectious mononucleosis (symptomatic primary EBV infection) and with high titres of antibodies to specific EBV antigens. However, it was not until 2022 that a longitudinal study demonstrated that MS risk is minimal in individuals who are not infected with EBV and that it increases over 30-fold following EBV infection. Over the past few years, a number of studies have provided clues on the underlying mechanisms, which might help us to develop more targeted treatments for MS. In this Review, we discuss the evidence linking EBV to the development of MS and the mechanisms by which the virus is thought to cause the disease. Furthermore, we discuss implications for the treatment and prevention of MS, including the use of antivirals and vaccines.
Key points
-
In a longitudinal study that followed individuals seronegative for Epstein–Barr virus (EBV) over time, multiple sclerosis (MS) risk increased more than 30-fold after EBV infection. The results are unlikely to be explained by reverse causation or confounding factors.
-
Among individuals who are EBV positive, those with a history of infectious mononucleosis or with high antibody titres against EBV nuclear antigens have an increased risk of developing MS.
-
Several mechanisms have been proposed to explain the link between EBV and MS, including molecular mimicry and an altered immune response to poorly controlled EBV infection.
-
Vaccines that might prevent EBV infection are currently being developed. If effective, these vaccines would be expected to prevent most MS cases.
-
Targeting EBV with therapeutic vaccines or antiviral drugs could represent a novel treatment strategy for MS.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Murray, J. Infection as a cause of multiple sclerosis. BMJ 325, 1128 (2002).
Cook, S. D. Multiple sclerosis. Arch. Neurol. 55, 421–423 (1998).
Kurtzke, J. F. An epidemiologic approach to multiple sclerosis. Arch. Neurol. 14, 213–222 (1966).
Gale, C. R. & Martyn, C. N. Migrant studies in multiple sclerosis. Prog. Neurobiol. 47, 425–448 (1995).
Kurtzke, J. F. & Heltberg, A. Multiple sclerosis in the Faroe Islands: an epitome. J. Clin. Epidemiol. 54, 1–22 (2001).
Kurtzke, J. F., Gudmundsson, K. R. & Bergmann, S. Multiple sclerosis in Iceland: 1. Evidence of a postwar epidemic. Neurology 32, 143–150 (1982).
Poskanzer, D. C., Prenney, L. B., Sheridan, J. L. & Kondy, J. Y. Multiple sclerosis in the Orkney and Shetland Islands. I: Epidemiology, clinical factors, and methodology. J. Epidemiol. Commun. Health 34, 229–239 (1980).
Bray, P. F., Bloomer, L. C., Salmon, V. C., Bagley, M. H. & Larsen, P. D. Epstein–Barr virus infection and antibody synthesis in patients with multiple sclerosis. Arch. Neurol. 40, 406–408 (1983).
Larsen, P. D., Bloomer, L. C. & Bray, P. F. Epstein–Barr nuclear antigen and viral capsid antigen antibody titers in multiple sclerosis. Neurology 35, 435–438 (1985).
Sumaya, C. V., Myers, L. W. & Ellison, G. W. Epstein–Barr virus antibodies in multiple sclerosis. Arch. Neurol. 37, 94–96 (1980).
Thacker, E. L., Mirzaei, F. & Ascherio, A. Infectious mononucleosis and risk for multiple sclerosis: a meta-analysis. Ann. Neurol. 59, 499–503 (2006).
DeLorenze, G. N. et al. Epstein–Barr virus and multiple sclerosis: evidence of association from a prospective study with long-term follow-up. Arch. Neurol. 63, 839–844 (2006).
Levin, L. I. et al. Temporal relationship between elevation of Epstein–Barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis. JAMA 293, 2496–2500 (2005).
Munger, K. L., Levin, L. I., O’Reilly, E. J., Falk, K. I. & Ascherio, A. Anti-Epstein–Barr virus antibodies as serological markers of multiple sclerosis: a prospective study among United States military personnel. Mult. Scler. 17, 1185–1193 (2011).
Sundstrom, P. et al. An altered immune response to Epstein–Barr virus in multiple sclerosis: a prospective study. Neurology 62, 2277–2282 (2004).
Nielsen, T. R. et al. Multiple sclerosis after infectious mononucleosis. Arch. Neurol. 64, 72–75 (2007).
Jacobs, B. M., Giovannoni, G., Cuzick, J. & Dobson, R. Systematic review and meta-analysis of the association between Epstein–Barr virus, multiple sclerosis and other risk factors. Mult. Scler. 26, 1281–1297 (2020).
Dobson, R., Kuhle, J., Middeldorp, J. & Giovannoni, G. Epstein–Barr-negative MS: a true phenomenon? Neurol. Neuroimmunol. Neuroinflamm. 4, e318 (2017).
Abrahamyan, S. et al. Complete Epstein–Barr virus seropositivity in a large cohort of patients with early multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 91, 681–686 (2020).
Bjornevik, K. et al. Longitudinal analysis reveals high prevalence of Epstein–Barr virus associated with multiple sclerosis. Science 375, 296–301 (2022).
Burkitt, D. A sarcoma involving the jaws in African children. Br. J. Surg. 46, 218–223 (1958).
Epstein, M. A., Achong, B. G. & Barr, Y. M. Virus particles in cultured lymphoblasts from Burkitt’s lymphoma. Lancet 1, 702–703 (1964).
Hjalgrim, H., Friborg, J. & Melbye, M. in Human Herpesviruses: Biology, Therapy, and Immunoprophylaxis (eds Arvin, A. et al.) (2007).
Cohen, J. I. Epstein–Barr virus infection. N. Engl. J. Med. 343, 481–492 (2000).
Damania, B., Kenney, S. C. & Raab-Traub, N. Epstein–Barr virus: biology and clinical disease. Cell 185, 3652–3670 (2022).
Balfour, H. H. Jr. et al. Behavioral, virologic, and immunologic factors associated with acquisition and severity of primary Epstein–Barr virus infection in university students. J. Infect. Dis. 207, 80–88 (2013).
Houen, G. & Trier, N. H. Epstein–Barr virus and systemic autoimmune diseases. Front. Immunol. 11, 587380 (2020).
Bakkalci, D. et al. Risk factors for Epstein–Barr virus-associated cancers: a systematic review, critical appraisal, and mapping of the epidemiological evidence. J. Glob. Health 10, 010405 (2020).
Warner, H. B. & Carp, R. I. Multiple sclerosis etiology — an Epstein–Barr virus hypothesis. Med. Hypotheses 25, 93–97 (1988).
Hernan, M. A., Zhang, S. M., Lipworth, L., Olek, M. J. & Ascherio, A. Multiple sclerosis and age at infection with common viruses. Epidemiology 12, 301–306 (2001).
Xu, Y. et al. Hospital-diagnosed infections before age 20 and risk of a subsequent multiple sclerosis diagnosis. Brain 144, 2390–2400 (2021).
Crowcroft, N. S., Vyse, A., Brown, D. W. & Strachan, D. P. Epidemiology of Epstein–Barr virus infection in pre-adolescent children: application of a new salivary method in Edinburgh, Scotland. J. Epidemiol. Community Health 52, 101–104 (1998).
Bach, J. F. The effect of infections on susceptibility to autoimmune and allergic diseases. N. Engl. J. Med. 347, 911–920 (2002).
Ascherio, A. & Munger, K. L. Environmental risk factors for multiple sclerosis. Part I: the role of infection. Ann. Neurol. 61, 288–299 (2007).
Xu, Y. et al. Association of infectious mononucleosis in childhood and adolescence with risk for a subsequent multiple sclerosis diagnosis among siblings. JAMA Netw. Open. 4, e2124932 (2021).
Khalil, M. et al. Neurofilaments as biomarkers in neurological disorders. Nat. Rev. Neurol. 14, 577–589 (2018).
Bjornevik, K. et al. Serum neurofilament light chain levels in patients with presymptomatic multiple sclerosis. JAMA Neurol. 77, 58–64 (2020).
Jons, D. et al. Axonal injury in asymptomatic individuals preceding onset of multiple sclerosis. Ann. Clin. Transl. Neurol. https://doi.org/10.1002/acn3.51568 (2022).
Dowd, J. B., Aiello, A. E. & Alley, D. E. Socioeconomic disparities in the seroprevalence of cytomegalovirus infection in the US population: NHANES III. Epidemiol. Infect. 137, 58–65 (2009).
Ishii, T. et al. Clinical differentiation of infectious mononucleosis that is caused by Epstein–Barr virus or cytomegalovirus: a single-center case-control study in Japan. J. Infect. Chemother. 25, 431–436 (2019).
Lipsitch, M., Tchetgen Tchetgen, E. & Cohen, T. Negative controls: a tool for detecting confounding and bias in observational studies. Epidemiology 21, 383–388 (2010).
Grut, V. et al. Cytomegalovirus seropositivity is associated with reduced risk of multiple sclerosis-a presymptomatic case-control study. Eur. J. Neurol. 28, 3072–3079 (2021).
VanderWeele, T. J. & Ding, P. Sensitivity analysis in observational research: introducing the e-value. Ann. Intern. Med. 167, 268–274 (2017).
Racaniello, V. R. One hundred years of poliovirus pathogenesis. Virology 344, 9–16 (2006).
Bodily, J. & Laimins, L. A. Persistence of human papillomavirus infection: keys to malignant progression. Trends Microbiol. 19, 33–39 (2011).
Mechelli, R. et al. Epstein–Barr virus genetic variants are associated with multiple sclerosis. Neurology 84, 1362–1368 (2015).
Munger, K. L., Levin, L. I., Hollis, B. W., Howard, N. S. & Ascherio, A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA 296, 2832–2838 (2006).
Salzer, J. et al. Vitamin D as a protective factor in multiple sclerosis. Neurology 79, 2140–2145 (2012).
Hernan, M. A., Olek, M. J. & Ascherio, A. Cigarette smoking and incidence of multiple sclerosis. Am. J. Epidemiol. 154, 69–74 (2001).
Salzer, J. et al. Smoking as a risk factor for multiple sclerosis. Mult. Scler. 19, 1022–1027 (2013).
Munger, K. L. et al. Childhood body mass index and multiple sclerosis risk: a long-term cohort study. Mult. Scler. 19, 1323–1329 (2013).
Munger, K. L., Chitnis, T. & Ascherio, A. Body size and risk of MS in two cohorts of US women. Neurology 73, 1543–1550 (2009).
Munk Nielsen, N. et al. Multiple sclerosis among first- and second-generation immigrants in Denmark: a population-based cohort study. Brain 142, 1587–1597 (2019).
Hernan, M. A., Olek, M. J. & Ascherio, A. Geographic variation of MS incidence in two prospective studies of US women. Neurology 53, 1711–1718 (1999).
Wallin, M. T., Page, W. F. & Kurtzke, J. F. Multiple sclerosis in US veterans of the Vietnam era and later military service: race, sex, and geography. Ann. Neurol. 55, 65–71 (2004).
Wallin, M. T. et al. The Gulf War era multiple sclerosis cohort: age and incidence rates by race, sex and service. Brain 135, 1778–1785 (2012).
Koch-Henriksen, N., Thygesen, L. C., Stenager, E., Laursen, B. & Magyari, M. Incidence of MS has increased markedly over six decades in Denmark particularly with late onset and in women. Neurology 90, e1954–e1963 (2018).
Moutsianas, L. et al. Class II HLA interactions modulate genetic risk for multiple sclerosis. Nat. Genet. 47, 1107–1113 (2015).
Ricigliano, V. A. et al. EBNA2 binds to genomic intervals associated with multiple sclerosis and overlaps with vitamin D receptor occupancy. PLoS One 10, e0119605 (2015).
Harley, J. B. et al. Transcription factors operate across disease loci, with EBNA2 implicated in autoimmunity. Nat. Genet. 50, 699–707 (2018).
Afrasiabi, A., Parnell, G. P., Swaminathan, S., Stewart, G. J. & Booth, D. R. The interaction of multiple sclerosis risk loci with Epstein–Barr virus phenotypes implicates the virus in pathogenesis. Sci. Rep. 10, 193 (2020).
Olsson, T., Barcellos, L. F. & Alfredsson, L. Interactions between genetic, lifestyle and environmental risk factors for multiple sclerosis. Nat. Rev. Neurol. 13, 25–36 (2017).
Ascherio, A. & Munger, K. L. Epidemiology of multiple sclerosis: from risk factors to prevention — an update. Semin. Neurol. 36, 103–114 (2016).
Lennette, E. T. et al. Disease-related differences in antibody patterns against EBV-encoded nuclear antigens EBNA 1, EBNA 2 and EBNA 6. Eur. J. Cancer 29A, 1584–1589 (1993).
Munger, K. L. et al. Epstein–Barr virus and multiple sclerosis risk in the finnish maternity cohort. Ann. Neurol. 86, 436–442 (2019).
Hedstrom, A. K. et al. High levels of Epstein–Barr virus nuclear antigen-1-specific antibodies and infectious mononucleosis act both independently and synergistically to increase multiple sclerosis risk. Front. Neurol. 10, 1368 (2019).
Makhani, N. & Tremlett, H. The multiple sclerosis prodrome. Nat. Rev. Neurol. 17, 515–521 (2021).
Boshoff, C. & Weiss, R. AIDS-related malignancies. Nat. Rev. Cancer 2, 373–382 (2002).
Gold, J. et al. HIV and lower risk of multiple sclerosis: beginning to unravel a mystery using a record-linked database study. J. Neurol. Neurosurg. Psychiatry 86, 9–12 (2015).
Drosu, N. C., Edelman, E. R. & Housman, D. E. Tenofovir prodrugs potently inhibit Epstein–Barr virus lytic DNA replication by targeting the viral DNA polymerase. Proc. Natl Acad. Sci. USA 117, 12368–12374 (2020).
Taylor, G. S., Long, H. M., Brooks, J. M., Rickinson, A. B. & Hislop, A. D. The immunology of Epstein–Barr virus-induced disease. Annu. Rev. Immunol. 33, 787–821 (2015).
Münz, C. Latency and lytic replication in the oncogenesis of the Epstein–Barr virus. Nat. Rev. Microbiol. 17, 691–700 (2019).
Farrell, P. J. Epstein–Barr virus and cancer. Annu. Rev. Pathol. 14, 29–53 (2019).
Dunmire, S. K., Verghese, P. S. & Balfour, H. H. Jr. Primary Epstein–Barr virus infection. J. Clin. Virol. 102, 84–92 (2018).
Damania, B. & Münz, C. Immunodeficiencies that predispose to pathologies by human oncogenic gamma-herpesviruses. FEMS Microbiol. Rev. 43, 181–192 (2019).
Fournier, B. & Latour, S. Immunity to EBV as revealed by immunedeficiencies. Curr. Opin. Immunol. 72, 107–115 (2021).
Latour, S. & Fischer, A. Signaling pathways involved in the T-cell-mediated immunity against Epstein–Barr virus: lessons from genetic diseases. Immunol. Rev. 291, 174–189 (2019).
McHugh, D. et al. Infection and immune control of human oncogenic gamma-herpesviruses in humanized mice. Philos. Trans. R. Soc. Lond. B Biol. Sci. 374, 20180296 (2019).
Muhe, J. et al. Neutralizing antibodies against Epstein–Barr virus infection of B cells can protect from oral viral challenge in the rhesus macaque animal model. Cell Rep. Med. 2, 100352 (2021).
Muhe, J. & Wang, F. Non-human primate lymphocryptoviruses: past, present, and future. Curr. Top. Microbiol. Immunol. 391, 385–405 (2015).
Gujer, C. et al. Plasmacytoid dendritic cells respond to Epstein–Barr virus infection with a distinct type I interferon subtype profile. Blood Adv. 3, 1129–1144 (2019).
Chijioke, O. et al. Human natural killer cells prevent infectious mononucleosis features by targeting lytic Epstein–Barr virus infection. Cell Rep. 5, 1489–1498 (2013).
Xiang, Z. et al. Targeted activation of human Vγ9Vδ2-T cells controls Epstein–Barr virus-induced B cell lymphoproliferative disease. Cancer Cell 26, 565–576 (2014).
Chung, B. K. et al. Innate immune control of EBV-infected B cells by invariant natural killer T cells. Blood 122, 2600–2608 (2013).
Strowig, T. et al. Priming of protective T cell responses against virus-induced tumors in mice with human immune system components. J. Exp. Med. 206, 1423–1434 (2009).
Callan, M. F. et al. Direct visualization of antigen-specific CD8+ T cells during the primary immune response to Epstein–Barr virus In vivo. J. Exp. Med. 187, 1395–1402 (1998).
Grant, M. L. & Bollard, C. M. Cell therapies for hematological malignancies: don’t forget non-gene-modified t cells! Blood Rev. 32, 203–224 (2018).
Middeldorp, J. M. Epstein–Barr virus-specific humoral immune responses in health and disease. Curr. Top. Microbiol. Immunol. 391, 289–323 (2015).
Lanz, T. V. et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature 603, 321–327 (2022).
Tengvall, K. et al. Molecular mimicry between Anoctamin 2 and Epstein–Barr virus nuclear antigen 1 associates with multiple sclerosis risk. Proc. Natl Acad. Sci. USA 116, 16955–16960 (2019).
Sundstrom, P., Nystrom, M., Ruuth, K. & Lundgren, E. Antibodies to specific EBNA-1 domains and HLA DRB1*1501 interact as risk factors for multiple sclerosis. J. Neuroimmunol. 215, 102–107 (2009).
Lindsey, J. W. Antibodies to the Epstein–Barr virus proteins BFRF3 and BRRF2 cross-react with human proteins. J. Neuroimmunol. 310, 131–134 (2017).
Cepok, S. et al. Identification of Epstein–Barr virus proteins as putative targets of the immune response in multiple sclerosis. J. Clin. Invest. 115, 1352–1360 (2005).
Wang, Z. et al. Antibodies from multiple sclerosis brain identified Epstein–Barr virus nuclear antigen 1 & 2 epitopes which are recognized by oligoclonal bands. J. Neuroimmune Pharmacol. 16, 567–580 (2021).
Bray, P. F., Luka, J., Bray, P. F., Culp, K. W. & Schlight, J. P. Antibodies against Epstein–Barr nuclear antigen (EBNA) in multiple sclerosis CSF, and two pentapeptide sequence identities between EBNA and myelin basic protein. Neurology 42, 1798–1804 (1992).
Nociti, V. et al. Epstein–Barr virus antibodies in serum and cerebrospinal fluid from multiple sclerosis, chronic inflammatory demyelinating polyradiculoneuropathy and amyotrophic lateral sclerosis. J. Neuroimmunol. 225, 149–152 (2010).
Kyllesbech, C. et al. Virus-specific antibody indices may supplement the total IgG index in diagnostics of multiple sclerosis. J. Neuroimmunol. 367, 577868 (2022).
Jog, N. R. et al. Epstein–Barr virus nuclear antigen 1 (EBNA-1) peptides recognized by adult multiple sclerosis patient sera induce neurologic symptoms in a murine model. J. Autoimmun. 106, 102332 (2020).
Kalchschmidt, J. S. et al. Epstein–Barr virus nuclear protein EBNA3C directly induces expression of AID and somatic mutations in B cells. J. Exp. Med. 213, 921–928 (2016).
He, B., Raab-Traub, N., Casali, P. & Cerutti, A. EBV-encoded latent membrane protein 1 cooperates with BAFF/BLyS and APRIL to induce T cell-independent Ig heavy chain class switching. J. Immunol. 171, 5215–5224 (2003).
Thorley-Lawson, D. A. Epstein–Barr virus: exploiting the immune system. Nat. Rev. Immunol. 1, 75–82 (2001).
Cencioni, M. T., Mattoscio, M., Magliozzi, R., Bar-Or, A. & Muraro, P. A. B cells in multiple sclerosis - from targeted depletion to immune reconstitution therapies. Nat. Rev. Neurol. 17, 399–414 (2021).
Studer, V., Rossi, S., Motta, C., Buttari, F. & Centonze, D. Peripheral B cell depletion and central proinflammatory cytokine reduction following repeated intrathecal administration of rituximab in progressive Multiple Sclerosis. J. Neuroimmunol. 276, 229–231 (2014).
Angelini, D. F. et al. Increased CD8+ T cell response to Epstein–Barr virus lytic antigens in the active phase of multiple sclerosis. PLoS Pathog. 9, e1003220 (2013).
Hollsberg, P., Hansen, H. J. & Haahr, S. Altered CD8+ T cell responses to selected Epstein–Barr virus immunodominant epitopes in patients with multiple sclerosis. Clin. Exp. Immunol. 132, 137–143 (2003).
Jilek, S. et al. Strong EBV-specific CD8+ T-cell response in patients with early multiple sclerosis. Brain 131, 1712–1721 (2008).
Lunemann, J. D. et al. Increased frequency and broadened specificity of latent EBV nuclear antigen-1-specific T cells in multiple sclerosis. Brain 129, 1493–1506 (2006).
Lunemann, J. D. et al. EBNA1-specific T cells from patients with multiple sclerosis cross react with myelin antigens and co-produce IFN-γ and IL-2. J. Exp. Med. 205, 1763–1773 (2008).
Schneider-Hohendorf, T. et al. Broader Epstein–Barr virus-specific T cell receptor repertoire in patients with multiple sclerosis. J. Exp. Med. 219, e20220650 (2022).
Lossius, A. et al. High-throughput sequencing of TCR repertoires in multiple sclerosis reveals intrathecal enrichment of EBV-reactive CD8+ T cells. Eur. J. Immunol. 44, 3439–3452 (2014).
Pender, M. P., Csurhes, P. A., Burrows, J. M. & Burrows, S. R. Defective T-cell control of Epstein–Barr virus infection in multiple sclerosis. Clin. Transl. Immunol. 6, e126 (2017).
Erdur, H. et al. EBNA1 antigen-specific CD8+ T cells in cerebrospinal fluid of patients with multiple sclerosis. J. Neuroimmunol. 294, 14–17 (2016).
Jilek, S. et al. HLA-B7-restricted EBV-specific CD8+ T cells are dysregulated in multiple sclerosis. J. Immunol. 188, 4671–4680 (2012).
Zdimerova, H. et al. Attenuated immune control of Epstein–Barr virus in humanized mice is associated with the multiple sclerosis risk factor HLA-DR15. Eur. J. Immunol. 51, 64–75 (2021).
Wang, J. et al. HLA-DR15 molecules jointly shape an autoreactive T cell repertoire in multiple sclerosis. Cell 183, 1264–1281.e20 (2020).
Wucherpfennig, K. W. & Strominger, J. L. Molecular mimicry in T cell-mediated autoimmunity: viral peptides activate human T cell clones specific for myelin basic protein. Cell 80, 695–705 (1995).
Lang, H. L. et al. A functional and structural basis for TCR cross-reactivity in multiple sclerosis. Nat. Immunol. 3, 940–943 (2002).
Leung, C. S. et al. Robust T-cell stimulation by Epstein–Barr virus-transformed B cells after antigen targeting to DEC-205. Blood 121, 1584–1594 (2013).
Hong, S. et al. B cells are the dominant antigen-presenting cells that activate naive CD4+ T cells upon immunization with a virus-derived nanoparticle antigen. Immunity 49, 695–708.e4 (2018).
van Zyl, D. G. et al. Immunogenic particles with a broad antigenic spectrum stimulate cytolytic T cells and offer increased protection against EBV infection ex vivo and in mice. PLoS Pathog. 14, e1007464 (2018).
Choi, I. K. et al. Mechanism of EBV inducing anti-tumour immunity and its therapeutic use. Nature 590, 157–162 (2021).
Choi, I. K. et al. Signaling by the Epstein–Barr virus LMP1 protein induces potent cytotoxic CD4+ and CD8+ T cell responses. Proc. Natl Acad. Sci. USA 115, E686–E695 (2018).
Keane, J. T. et al. The interaction of Epstein–Barr virus encoded transcription factor EBNA2 with multiple sclerosis risk loci is dependent on the risk genotype. EBioMedicine 71, 103572 (2021).
Kwak, K., Akkaya, M. & Pierce, S. K. B cell signaling in context. Nat. Immunol. 20, 963–969 (2019).
Ascherio, A. et al. Epstein–Barr virus antibodies and risk of multiple sclerosis: a prospective study. JAMA 286, 3083–3088 (2001).
Lunemann, J. D. et al. Elevated Epstein–Barr virus-encoded nuclear antigen-1 immune responses predict conversion to multiple sclerosis. Ann. Neurol. 67, 159–169 (2010).
Munger, K. L. et al. No association of multiple sclerosis activity and progression with EBV or tobacco use in BENEFIT. Neurology 85, 1694–1701 (2015).
Farrell, R. A. et al. Humoral immune response to EBV in multiple sclerosis is associated with disease activity on MRI. Neurology 73, 32–38 (2009).
Kvistad, S. et al. Antibodies to Epstein–Barr virus and MRI disease activity in multiple sclerosis. Mult. Scler. 20, 1833–1840 (2014).
Sundstrom, P., Nystrom, L., Jidell, E. & Hallmans, G. EBNA-1 reactivity and HLA DRB1*1501 as statistically independent risk factors for multiple sclerosis: a case-control study. Mult. Scler. 14, 1120–1122 (2008).
Waubant, E. et al. Common viruses associated with lower pediatric multiple sclerosis risk. Neurology 76, 1989–1995 (2011).
Serafini, B., Rosicarelli, B., Magliozzi, R., Stigliano, E. & Aloisi, F. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain Pathol. 14, 164–174 (2004).
Magliozzi, R. et al. Meningeal B-cell follicles in secondary progressive multiple sclerosis associate with early onset of disease and severe cortical pathology. Brain 130, 1089–1104 (2007).
Schafflick, D. et al. Integrated single cell analysis of blood and cerebrospinal fluid leukocytes in multiple sclerosis. Nat. Commun. 11, 247 (2020).
Ramesh, A. et al. A pathogenic and clonally expanded B cell transcriptome in active multiple sclerosis. Proc. Natl Acad. Sci. USA 117, 22932–22943 (2020).
Pitteri, M. et al. Cerebrospinal fluid inflammatory profile of cognitive impairment in newly diagnosed multiple sclerosis patients. Mult. Scler. 28, 768–777 (2022).
Nohejlova, H. et al. Paediatric onset of multiple sclerosis: Analysis of chemokine and cytokine levels in the context of the early clinical course. Mult. Scler. Relat. Disord. 46, 102467 (2020).
van Langelaar, J. et al. Induction of brain-infiltrating T-bet-expressing B cells in multiple sclerosis. Ann. Neurol. 86, 264–278 (2019).
White, R. E. et al. EBNA3B-deficient EBV promotes B cell lymphomagenesis in humanized mice and is found in human tumors. J. Clin. Invest. 122, 1487–1502 (2012).
Berer, K. et al. Gut microbiota from multiple sclerosis patients enables spontaneous autoimmune encephalomyelitis in mice. Proc. Natl Acad. Sci. USA 114, 10719–10724 (2017).
Berer, K. et al. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature 479, 538–541 (2011).
Wekerle, H., Berer, K. & Krishnamoorthy, G. Remote control-triggering of brain autoimmune disease in the gut. Curr. Opin. Immunol. 25, 683–689 (2013).
Duc, D. et al. Disrupting myelin-specific Th17 cell gut homing confers protection in an adoptive transfer experimental autoimmune encephalomyelitis. Cell Rep. 29, 378–390.e4 (2019).
Laichalk, L. L., Hochberg, D., Babcock, G. J., Freeman, R. B. & Thorley-Lawson, D. A. The dispersal of mucosal memory B cells: evidence from persistent EBV infection. Immunity 16, 745–754 (2002).
Gasser, O. et al. HIV patients developing primary CNS lymphoma lack EBV-specific CD4+ T cell function irrespective of absolute CD4+ T cell counts. PLoS Med. 4, e96 (2007).
Roschewski, M. & Phelan, J. D. Sorting biologic subtypes of primary CNS lymphoma. Blood 137, 1436–1437 (2021).
Johnson, D. B. et al. A case report of clonal EBV-like memory CD4+ T cell activation in fatal checkpoint inhibitor-induced encephalitis. Nat. Med. 25, 1243–1250 (2019).
Serafini, B. et al. Dysregulated Epstein–Barr virus infection in the multiple sclerosis brain. J. Exp. Med. 204, 2899–2912 (2007).
Veroni, C., Serafini, B., Rosicarelli, B., Fagnani, C. & Aloisi, F. Transcriptional profile and Epstein–Barr virus infection status of laser-cut immune infiltrates from the brain of patients with progressive multiple sclerosis. J. Neuroinflammation 15, 18 (2018).
Moreno, M. A. et al. Molecular signature of Epstein–Barr virus infection in MS brain lesions. Neurol. Neuroimmunol. Neuroinflamm. 5, e466 (2018).
Peferoen, L. A. et al. Epstein–Barr virus is not a characteristic feature in the central nervous system in established multiple sclerosis. Brain 133, e137 (2010).
Willis, S. N. et al. Epstein–Barr virus infection is not a characteristic feature of multiple sclerosis brain. Brain 132, 3318–3328 (2009).
Serafini, B., Rosicarelli, B., Veroni, C., Mazzola, G. A. & Aloisi, F. Epstein–Barr virus-specific CD8 T cells selectively infiltrate the brain in multiple sclerosis and interact locally with virus-infected cells: clue for a virus-driven immunopathological mechanism. J. Virol. 93, e00980-19 (2019).
Mrozek-Gorska, P. et al. Epstein–Barr virus reprograms human B lymphocytes immediately in the prelatent phase of infection. Proc. Natl Acad. Sci. USA 116, 16046–16055 (2019).
SoRelle, E. D., Reinoso-Vizcaino, N. M., Horn, G. Q. & Luftig, M. A. Epstein–Barr virus perpetuates B cell germinal center dynamics and generation of autoimmune-associated phenotypes in vitro. Front. Immunol. 13, 1001145 (2022).
van Langelaar, J. et al. The association of Epstein–Barr virus infection with CXCR3+ B-cell development in multiple sclerosis: impact of immunotherapies. Eur. J. Immunol. 51, 626–633 (2021).
Soldan, S. S. et al. Epigenetic plasticity enables CNS-trafficking of EBV-infected B lymphocytes. PLoS Pathog. 17, e1009618 (2021).
Epstein, M. A., Morgan, A. J., Finerty, S., Randle, B. J. & Kirkwood, J. K. Protection of cottontop tamarins against Epstein–Barr virus-induced malignant lymphoma by a prototype subunit vaccine. Nature 318, 287–289 (1985).
Bu, W. et al. Immunization with components of the viral fusion apparatus elicits antibodies that neutralize Epstein–Barr virus in B cells and epithelial cells. Immunity 50, 1305–1316.e6 (2019).
Sokal, E. M. et al. Recombinant gp350 vaccine for infectious mononucleosis: a phase 2, randomized, double-blind, placebo-controlled trial to evaluate the safety, immunogenicity, and efficacy of an Epstein–Barr virus vaccine in healthy young adults. J. Infect. Dis. 196, 1749–1753 (2007).
Kanekiyo, M. et al. Rational design of an Epstein–Barr virus vaccine targeting the receptor-binding site. Cell 162, 1090–1100 (2015).
Wei, C. J. et al. A bivalent Epstein–Barr virus vaccine induces neutralizing antibodies that block infection and confer immunity in humanized mice. Sci. Transl. Med. 14, eabf3685 (2022).
Cui, X. et al. Immunization with Epstein–Barr virus core fusion machinery envelope proteins elicit high titers of neutralizing activities and protect humanized mice from lethal dose EBV challenge. Vaccines 9, 285 (2021).
Escalante, G. M. et al. A pentavalent Epstein–Barr virus-like particle vaccine elicits high titers of neutralizing antibodies against Epstein–Barr virus infection in immunized rabbits. Vaccines 8, 169 (2020).
Ruiss, R. et al. A virus-like particle-based Epstein–Barr virus vaccine. J. Virol. 85, 13105–13113 (2011).
Taylor, G. S. et al. A recombinant modified vaccinia ankara vaccine encoding Epstein–Barr Virus (EBV) target antigens: a phase I trial in UK patients with EBV-positive cancer. Clin. Cancer Res. 20, 5009–5022 (2014).
Zeng, Y. et al. LMP2-DC vaccine elicits specific EBV-LMP2 response to effectively improve immunotherapy in patients with nasopharyngeal cancer. Biomed. Env. Sci. 33, 849–856 (2020).
Chia, W. K. et al. A phase II study evaluating the safety and efficacy of an adenovirus-DeltaLMP1-LMP2 transduced dendritic cell vaccine in patients with advanced metastatic nasopharyngeal carcinoma. Ann. Oncol. 23, 997–1005 (2012).
Garcia, C. R., Jayswal, R., Adams, V., Anthony, L. B. & Villano, J. L. Multiple sclerosis outcomes after cancer immunotherapy. Clin. Transl. Oncol. 21, 1336–1342 (2019).
Messick, T. E. et al. Structure-based design of small-molecule inhibitors of EBNA1 DNA binding blocks Epstein–Barr virus latent infection and tumor growth. Sci. Transl. Med. 11, eaau5612 (2019).
Soldan, S. S., Messick, T. E. & Lieberman, P. M. Therapeutic approaches to Epstein–Barr virus cancers. Curr. Opin. Virol. 56, 101260 (2022).
Perrine, S. P. et al. A phase 1/2 trial of arginine butyrate and ganciclovir in patients with Epstein–Barr virus-associated lymphoid malignancies. Blood 109, 2571–2578 (2007).
Hui, K. F. et al. Inhibition of class I histone deacetylases by romidepsin potently induces Epstein–Barr virus lytic cycle and mediates enhanced cell death with ganciclovir. Int. J. Cancer 138, 125–136 (2016).
Bollard, C. M. & Cohen, J. I. How I treat T-cell chronic active Epstein–Barr virus disease. Blood 131, 2899–2905 (2018).
Papadopoulou, A. et al. Activity of broad-spectrum T cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci. Transl. Med. 6, 242ra283 (2014).
Huang, J. et al. Epstein–Barr virus-specific adoptive immunotherapy for recurrent, metastatic nasopharyngeal carcinoma. Cancer 123, 2642–2650 (2017).
Pender, M. P. et al. Epstein–Barr virus-specific T cell therapy for progressive multiple sclerosis. JCI Insight 5, e144624 (2020).
Ioannides, Z. A. et al. Sustained clinical improvement in a subset of patients with progressive multiple sclerosis treated with Epstein–Barr virus-specific T cell therapy. Front. Neurol. 12, 652811 (2021).
Lutterotti, A., Hayward-Koennecke, H., Sospedra, M. & Martin, R. Antigen-specific immune tolerance in multiple sclerosis-promising approaches and how to bring them to patients. Front. Immunol. 12, 640935 (2021).
Lutterotti, A. et al. Antigen-specific tolerance by autologous myelin peptide-coupled cells: a phase 1 trial in multiple sclerosis. Sci. Transl. Med. 5, 188ra175 (2013).
McRae, B. L., Vanderlugt, C. L., Dal Canto, M. C. & Miller, S. D. Functional evidence for epitope spreading in the relapsing pathology of experimental autoimmune encephalomyelitis. J. Exp. Med. 182, 75–85 (1995).
Acknowledgements
C.M. is supported by Cancer Research Switzerland (KFS-4962-02-2020), HMZ ImmunoTargET of the University of Zurich, the Sobek Foundation, the Swiss Vaccine Research Institute, the Swiss MS Society (2021-09), the Vontobel Foundation and the Swiss National Science Foundation (310030_204470/1, 310030L_197952/1 and CRSII5_180323). J.I.C. is supported by the intramural research programme of the National Institute of Allergy and Infectious Diseases.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
J.I.C. is named as an inventor on patent applications for Epstein–Barr virus vaccines, which have been filed by the NIH. A.A. has received an honorarium as a speaker from Moderna. K.B. and C.M. declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks W. Robinson and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bjornevik, K., Münz, C., Cohen, J.I. et al. Epstein–Barr virus as a leading cause of multiple sclerosis: mechanisms and implications. Nat Rev Neurol 19, 160–171 (2023). https://doi.org/10.1038/s41582-023-00775-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-023-00775-5
This article is cited by
-
T cells implicate Epstein–Barr virus in multiple sclerosis pathogenesis
Nature Reviews Neurology (2024)
-
Navigating Epstein–Barr virus autoimmunity: role of NK cells and T cells in multiple sclerosis
Signal Transduction and Targeted Therapy (2024)
-
EBV-specific T cells in multiple sclerosis
Nature Reviews Neurology (2024)
-
Ofatumumab: A Novel Anti-CD20 Monoclonal Antibody for Multiple Sclerosis: A Review of Clinical Considerations
SN Comprehensive Clinical Medicine (2024)
-
Impact of the first Gulf war on multiple sclerosis risk in Kuwait: a quasi-experimental study
BMC Neurology (2023)