Abstract
Amyotrophic lateral sclerosis (ALS) is a devastating and incurable neurodegenerative disease characterized by the progressive loss of upper and lower motor neurons. ALS causes death, usually within 2–5 years of diagnosis. Riluzole, the only drug currently approved in Europe for the treatment of this condition, offers only a modest benefit, increasing survival by 3 months on average. Recent advances in our understanding of causative or disease-modifying genetic variants and in the development of genetic therapy strategies present exciting new therapeutic opportunities for ALS. In addition, the approval of adeno-associated virus-mediated delivery of functional copies of the SMN1 gene to treat spinal muscular atrophy represents an important therapeutic milestone and demonstrates the potential of gene replacement therapies for motor neuron disorders. In this Review, we describe the current landscape of genetic therapies in ALS, highlighting achievements and critical challenges. In particular, we discuss opportunities for gene replacement therapy in subgroups of people with ALS, and we describe loss-of-function mutations that are known to contribute to the pathophysiology of ALS and could represent novel targets for gene replacement therapies.
Key points
-
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease for which no effective disease-modifying therapy is currently available; emerging evidence suggests genetic therapy as an attractive new therapeutic strategy for this disease.
-
Genetic therapy can be classified into silencing, editing or replacement approaches, depending on whether the aim is to reduce the expression of toxic mutant proteins, introduce genomic modifications or provide functional copies of a dysfunctional gene.
-
Adeno-associated viruses (AAVs) are considered the vehicle of choice for the delivery of genetic materials. AAV9 is particularly attractive for neurological applications, as it can penetrate the blood–brain barrier and effectively deliver its cargo to both dividing and non-dividing cells.
-
Challenges that hinder the clinical application of genetic therapies in ALS include the multifactorial and oligogenic nature of the disease and the problem of efficiently and simultaneously targeting both motor neurons and glial cells. Nevertheless, some preclinical and clinical studies are currently testing gene therapy strategies for this disease, mostly focusing on silencing of toxic gene mutations.
-
Accumulating in vitro and in vivo evidence suggests loss of function as the mechanism underlying the effects of mutations in five ALS-associated genes (TBK1, OPTN, NEK1, FIG4 and ANG), and restoring the functions of these genes through replacement strategies could represent a promising therapeutic opportunity.
-
In the future, precision medicine approaches that target specific pathophysiological mechanisms in each affected individual can be envisaged.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hardiman, O. et al. Amyotrophic lateral sclerosis. Nat. Rev. Dis. Prim. 3, 17071 (2017).
Van Damme, P., Robberecht, W. & Van Den Bosch, L. Modelling amyotrophic lateral sclerosis: progress and possibilities. Dis. Model. Mech. 10, 537–549 (2017).
Nagoshi, N., Nakashima, H. & Fehlings, M. G. Riluzole as a neuroprotective drug for spinal cord injury: from bench to bedside. Molecules 20, 7775–7789 (2015).
Fang, T. et al. Stage at which riluzole treatment prolongs survival in patients with amyotrophic lateral sclerosis: a retrospective analysis of data from a dose-ranging study. Lancet Neurol. 17, 416–422 (2018).
Edaravone (MCI-186) ALS 19 Study Group. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 16, 505–512 (2017).
King, A. E., Woodhouse, A., Kirkcaldie, M. T. & Vickers, J. C. Excitotoxicity in ALS: overstimulation, or overreaction? Exp. Neurol. 275, 162–171 (2016).
Benson, B. C., Shaw, P. J., Azzouz, M., Highley, J. R. & Hautbergue, G. M. Proteinopathies as hallmarks of impaired gene expression, proteostasis and mitochondrial function in amyotrophic lateral sclerosis. Front. Neurosci. 15, 783624 (2021).
Smith, E. F., Shaw, P. J. & De Vos, K. J. The role of mitochondria in amyotrophic lateral sclerosis. Neurosci. Lett. 710, 132933 (2019).
Barber, S. C. & Shaw, P. J. Oxidative stress in ALS: key role in motor neuron injury and therapeutic target. Free. Radic. Biol. Med. 48, 629–641 (2010).
Liu, J. & Wang, F. Role of neuroinflammation in amyotrophic lateral sclerosis: cellular mechanisms and therapeutic implications. Front. Immunol. 8, 1005 (2017).
Butti, Z. & Patten, S. A. RNA dysregulation in amyotrophic lateral sclerosis. Front. Genet. 9, 712 (2018).
Al-Chalabi, A. et al. Amyotrophic lateral sclerosis: moving towards a new classification system. Lancet Neurol. 15, 1182–1194 (2016).
Andersen, P. M. & Al-Chalabi, A. Clinical genetics of amyotrophic lateral sclerosis: what do we really know? Nat. Rev. Neurol. 7, 603–615 (2011).
Mejzini, R. et al. ALS genetics, mechanisms, and therapeutics: where are we now? Front. Neurosci. 13, 1310 (2019).
Ranganathan, R. et al. Multifaceted genes in amyotrophic lateral sclerosis-frontotemporal dementia. Front. Neurosci. 14, 684 (2020).
Deng, H., Gao, K. & Jankovic, J. The role of FUS gene variants in neurodegenerative diseases. Nat. Rev. Neurol. 10, 337–348 (2014).
Mendell, J. R. et al. Single-dose gene-replacement therapy for spinal muscular atrophy. N. Engl. J. Med. 377, 1713–1722 (2017).
Al-Zaidy, S. et al. Health outcomes in spinal muscular atrophy type 1 following AVXS-101 gene replacement therapy. Pediatr. Pulmonol. 54, 179–185 (2019).
Hoy, S. M. Onasemnogene abeparvovec: first global approval. Drugs 79, 1255–1262 (2019).
High, K. A. & Roncarolo, M. G. Gene therapy. N. Engl. J. Med. 381, 455–464 (2019).
Tang, R. & Xu, Z. Gene therapy: a double-edged sword with great powers. Mol. Cell Biochem. 474, 73–81 (2020).
Amado, D. A. & Davidson, B. L. Gene therapy for ALS: a review. Mol. Ther. 29, 3345–3358 (2021).
Adams, D., Koike, H., Slama, M. & Coelho, T. Hereditary transthyretin amyloidosis: a model of medical progress for a fatal disease. Nat. Rev. Neurol. 15, 387–404 (2019).
Keam, S. J. Inotersen: first global approval. Drugs 78, 1371–1376 (2018).
Mercuri, E., Pera, M. C., Scoto, M., Finkel, R. & Muntoni, F. Spinal muscular atrophy – insights and challenges in the treatment era. Nat. Rev. Neurol. 16, 706–715 (2020).
Li, Q. Nusinersen as a therapeutic agent for spinal muscular atrophy. Yonsei Med. J. 61, 273–283 (2020).
Jablonka, S., Hennlein, L. & Sendtner, M. Therapy development for spinal muscular atrophy: perspectives for muscular dystrophies and neurodegenerative disorders. Neurol. Res. Pract. 4, 2 (2022).
Uddin, F., Rudin, C. M. & Sen, T. CRISPR gene therapy: applications, limitations, and implications for the future. Front. Oncol. 10, 1387 (2020).
Gillmore, J. D. et al. CRISPR-Cas9 in vivo gene editing for transthyretin amyloidosis. N. Engl. J. Med. 385, 493–502 (2021).
Brenner, D., Ludolph, A. C. & Weishaupt, J. H. Gene specific therapies – the next therapeutic milestone in neurology. Neurol. Res. Pract. 2, 25 (2020).
Xu, Y. C. & Guo, Y. L. Less is more, natural loss-of-function mutation is a strategy for adaptation. Plant. Commun. 1, 100103 (2020).
Deverman, B. E., Ravina, B. M., Bankiewicz, K. S., Paul, S. M. & Sah, D. W. Y. Gene therapy for neurological disorders: progress and prospects. Nat. Rev. Drug. Discov. 17, 767 (2018).
Ingusci, S., Verlengia, G., Soukupova, M., Zucchini, S. & Simonato, M. Gene therapy tools for brain diseases. Front. Pharmacol. 10, 724 (2019).
Naso, M. F., Tomkowicz, B., Perry, W. L. & Strohl, W. R. Adeno-associated virus (AAV) as a vector for gene therapy. BioDrugs 31, 317–334 (2017).
Lykken, E. A., Shyng, C., Edwards, R. J., Rozenberg, A. & Gray, S. J. Recent progress and considerations for AAV gene therapies targeting the central nervous system. J. Neurodev. Disord. 10, 16 (2018).
Cearley, C. N. & Wolfe, J. H. Transduction characteristics of adeno-associated virus vectors expressing cap serotypes 7, 8, 9, and Rh10 in the mouse brain. Mol. Ther. 13, 528–537 (2006).
Foust, K. D. et al. Intravascular AAV9 preferentially targets neonatal neurons and adult astrocytes. Nat. Biotechnol. 27, 59–65 (2009).
Gray, S. J. et al. Preclinical differences of intravascular AAV9 delivery to neurons and glia: a comparative study of adult mice and nonhuman primates. Mol. Ther. 19, 1058–1069 (2011).
Hudry, E. & Vandenberghe, L. H. Therapeutic AAV gene transfer to the nervous system: a clinical reality. Neuron 101, 839–862 (2019).
Gessler, D. J., Tai, P. W. L., Li, J. & Gao, G. Intravenous infusion of AAV for widespread gene delivery to the nervous system. Methods Mol. Biol. 1950, 143–163 (2019).
Colella, P., Ronzitti, G. & Mingozzi, F. Emerging issues in AAV-mediated in vivo gene therapy. Mol. Ther. Methods Clin. Dev. 8, 87–104 (2018).
Domenger, C. & Grimm, D. Next-generation AAV vectors – do not judge a virus (only) by its cover. Hum. Mol. Genet. 28, R3–R14 (2019).
Powell, S. K., Rivera-Soto, R. & Gray, S. J. Viral expression cassette elements to enhance transgene target specificity and expression in gene therapy. Discov. Med. 19, 49–57 (2015).
Gray, S. J. et al. Optimizing promoters for recombinant adeno-associated virus-mediated gene expression in the peripheral and central nervous system using self-complementary vectors. Hum. Gene Ther. 22, 1143–1153 (2011).
Fu, H. et al. Self-complementary adeno-associated virus serotype 2 vector: global distribution and broad dispersion of AAV-mediated transgene expression in mouse brain. Mol. Ther. 8, 911–917 (2003).
Inagaki, K. et al. Robust systemic transduction with AAV9 vectors in mice: efficient global cardiac gene transfer superior to that of AAV8. Mol. Ther. 14, 45–53 (2006).
Xu, R. et al. Quantitative comparison of expression with adeno-associated virus (AAV-2) brain-specific gene cassettes. Gene Ther. 8, 1323–1332 (2001).
Nieuwenhuis, B. et al. Optimization of adeno-associated viral vector-mediated transduction of the corticospinal tract: comparison of four promoters. Gene Ther. 28, 56–74 (2021).
Lukashchuk, V., Lewis, K. E., Coldicott, I., Grierson, A. J. & Azzouz, M. AAV9-mediated central nervous system-targeted gene delivery via cisterna magna route in mice. Mol. Ther. Methods Clin. Dev. 3, 15055 (2016).
Deverman, B. E. et al. Cre-dependent selection yields AAV variants for widespread gene transfer to the adult brain. Nat. Biotechnol. 34, 204–209 (2016).
Jackson, K. L., Dayton, R. D., Deverman, B. E. & Klein, R. L. Better targeting, better efficiency for wide-scale neuronal transduction with the synapsin promoter and AAV-PHP.B. Front. Mol. Neurosci. 9, 116 (2016).
McCarty, D. M. Self-complementary AAV vectors; advances and applications. Mol. Ther. 16, 1648–1656 (2008).
McCarty, D. M., Monahan, P. E. & Samulski, R. J. Self-complementary recombinant adeno-associated virus (scAAV) vectors promote efficient transduction independently of DNA synthesis. Gene Ther. 8, 1248–1254 (2001).
High-dose AAV gene therapy deaths. Nat. Biotechnol. 38, 910 (2020).
Philippidis, A. Fourth boy dies in clinical trial of Astellas’ AT132. Hum. Gene Ther. 32, 1008–1010 (2021).
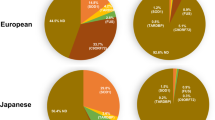
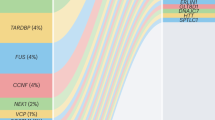
Boutin, S. et al. Prevalence of serum IgG and neutralizing factors against adeno-associated virus (AAV) types 1, 2, 5, 6, 8, and 9 in the healthy population: implications for gene therapy using AAV vectors. Hum. Gene Ther. 21, 704–712 (2010).
Calcedo, R., Vandenberghe, L. H., Gao, G., Lin, J. & Wilson, J. M. Worldwide epidemiology of neutralizing antibodies to adeno-associated viruses. J. Infect. Dis. 199, 381–390 (2009).
Kruzik, A. et al. Prevalence of anti-adeno-associated virus immune responses in international cohorts of healthy donors. Mol. Ther. Methods Clin. Dev. 14, 126–133 (2019).
Weber, T. Anti-AAV antibodies in AAV gene therapy: current challenges and possible solutions. Front. Immunol. 12, 658399 (2021).
Calcedo, R. et al. Adeno-associated virus antibody profiles in newborns, children, and adolescents. Clin. Vaccin. Immunol. 18, 1586–1588 (2011).
Herzog, R. W. Complexity of immune responses to AAV transgene products – example of factor IX. Cell Immunol. 342, 103658 (2019).
Mingozzi, F. & High, K. A. Immune responses to AAV vectors: overcoming barriers to successful gene therapy. Blood 122, 23–36 (2013).
Chowdhury, E. A. et al. Current progress and limitations of AAV mediated delivery of protein therapeutic genes and the importance of developing quantitative pharmacokinetic/pharmacodynamic (PK/PD) models. Adv. Drug. Deliv. Rev. 170, 214–237 (2021).
Vincents, B., von Pawel-Rammingen, U., Bjorck, L. & Abrahamson, M. Enzymatic characterization of the streptococcal endopeptidase, IdeS, reveals that it is a cysteine protease with strict specificity for IgG cleavage due to exosite binding. Biochemistry 43, 15540–15549 (2004).
Elmore, Z. C., Oh, D. K., Simon, K. E., Fanous, M. M. & Asokan, A. Rescuing AAV gene transfer from neutralizing antibodies with an IgG-degrading enzyme. JCI Insight 5, e139881 (2020).
Leborgne, C. et al. IgG-cleaving endopeptidase enables in vivo gene therapy in the presence of anti-AAV neutralizing antibodies. Nat. Med. 26, 1096–1101 (2020).
Ros-Gañán, I. et al. Optimising the IgG-degrading enzyme treatment regimen for enhanced adeno-associated virus transduction in the presence of neutralising antibodies. Clin. Transl. Immunol. 11, e1375 (2022).
Srejovic, I. et al. Galectin-3: roles in neurodevelopment, neuroinflammation, and behavior. Biomolecules 10, 798 (2020).
Denard, J. et al. Human galectin 3 binding protein interacts with recombinant adeno-associated virus type 6. J. Virol. 86, 6620–6631 (2012).
Denard, J. et al. AAV-8 and AAV-9 vectors cooperate with serum proteins differently than AAV-1 and AAV-6. Mol. Ther. Methods Clin. Dev. 10, 291–302 (2018).
Cappella, M., Ciotti, C., Cohen-Tannoudji, M. & Biferi, M. G. Gene therapy for ALS – a perspective. Int. J. Mol. Sci. 20, 4388 (2019).
Scarrott, J. M., Herranz-Martín, S., Alrafiah, A. R., Shaw, P. J. & Azzouz, M. Current developments in gene therapy for amyotrophic lateral sclerosis. Expert. Opin. Biol. Ther. 15, 935–947 (2015).
McCampbell, A. et al. Antisense oligonucleotides extend survival and reverse decrement in muscle response in ALS models. J. Clin. Invest. 128, 3558–3567 (2018).
Miller, T. et al. Phase 1-2 trial of antisense oligonucleotide tofersen for SOD1 ALS. N. Engl. J. Med. 383, 109–119 (2020).
Miller, T. M. et al. Trial of antisense oligonucleotide tofersen for SOD1 ALS. N. Engl. J. Med. 387, 1099–1110 (2022).
Arnold, C. Tailored treatment for ALS poised to move ahead. Nat. Med. https://doi.org/10.1038/d41591-019-00013-w (2019).
Biogen. Biogen and Ionis announce topline phase 1 study results of investigational drug in C9orf72 amyotrophic lateral sclerosis. Biogen https://investors.biogen.com/news-releases/news-release-details/biogen-and-ionis-announce-topline-phase-1-study-results (2022).
Pena, S. A. et al. Gene therapy for neurological disorders: challenges and recent advancements. J. Drug. Target. 28, 111–128 (2020).
Tora, M. S., Keifer, O. P., Lamanna, J. J. & Boulis, N. M. The challenges of developing a gene therapy for amyotrophic lateral sclerosis. Expert. Rev. Neurother. 17, 323–325 (2017).
Tang, X. et al. Divergence, convergence, and therapeutic implications: a cell biology perspective of C9ORF72-ALS/FTD. Mol. Neurodegener. 15, 34 (2020).
Hautbergue, G. M., Cleary, J. D., Guo, S. & Ranum, L. P. W. Therapeutic strategies for C9orf72 amyotrophic lateral sclerosis and frontotemporal dementia. Curr. Opin. Neurol. 34, 748–755 (2021).
Lee, E. B., Lee, V. M. & Trojanowski, J. Q. Gains or losses: molecular mechanisms of TDP43-mediated neurodegeneration. Nat. Rev. Neurosci. 13, 38–50 (2011).
An, H. et al. ALS-linked FUS mutations confer loss and gain of function in the nucleus by promoting excessive formation of dysfunctional paraspeckles. Acta Neuropathol. Commun. 7, 7 (2019).
Weskamp, K. & Barmada, S. J. TDP43 and RNA instability in amyotrophic lateral sclerosis. Brain Res. 1693, 67–74 (2018).
Wood, A., Gurfinkel, Y., Polain, N., Lamont, W. & Lyn Rea, S. Molecular mechanisms underlying TDP-43 pathology in cellular and animal models of ALS and FTLD. Int. J. Mol. Sci. 22, 4705 (2021).
Benkler, C., Barhum, Y., Ben-Zur, T. & Offen, D. Multifactorial gene therapy enhancing the glutamate uptake system and reducing oxidative stress delays symptom onset and prolongs survival in the SOD1-G93A ALS mouse model. J. Mol. Neurosci. 58, 46–58 (2016).
Rosenblum, L. T. & Trotti, D. EAAT2 and the molecular signature of amyotrophic lateral sclerosis. Adv. Neurobiol. 16, 117–136 (2017).
Goyal, N. A. et al. Addressing heterogeneity in amyotrophic lateral sclerosis clinical trials. Muscle Nerve 62, 156–166 (2020).
Bendotti, C. et al. Focus on the heterogeneity of amyotrophic lateral sclerosis. Amyotroph. Lateral Scler. Frontotemporal Degener. 21, 485–495 (2020).
Yang, Q., Jiao, B. & Shen, L. The development of C9orf72-related amyotrophic lateral sclerosis and frontotemporal dementia disorders. Front. Genet. 11, 562758 (2020).
Smeyers, J., Banchi, E. G. & Latouche, M. C9ORF72: what it is, what it does, and why it matters. Front. Cell Neurosci. 15, 661447 (2021).
Prasad, A., Bharathi, V., Sivalingam, V., Girdhar, A. & Patel, B. K. Molecular mechanisms of TDP-43 misfolding and pathology in amyotrophic lateral sclerosis. Front. Mol. Neurosci. 12, 25 (2019).
Suk, T. R. & Rousseaux, M. W. C. The role of TDP-43 mislocalization in amyotrophic lateral sclerosis. Mol. Neurodegener. 15, 45 (2020).
Cirulli, E. T. et al. Exome sequencing in amyotrophic lateral sclerosis identifies risk genes and pathways. Science 347, 1436–1441 (2015).
Freischmidt, A. et al. Haploinsufficiency of TBK1 causes familial ALS and fronto-temporal dementia. Nat. Neurosci. 18, 631–636 (2015).
Zhou, R., Zhang, Q. & Xu, P. TBK1, a central kinase in innate immune sensing of nucleic acids and beyond. Acta Biochim. Biophys. Sin. 52, 757–767 (2020).
Herhaus, L. TBK1 (TANK-binding kinase 1)-mediated regulation of autophagy in health and disease. Matrix Biol. 100–101, 84–98 (2021).
Perry, A. K., Chow, E. K., Goodnough, J. B., Yeh, W. C. & Cheng, G. Differential requirement for TANK-binding kinase-1 in type I interferon responses to toll-like receptor activation and viral infection. J. Exp. Med. 199, 1651–1658 (2004).
Zhao, W. Negative regulation of TBK1-mediated antiviral immunity. FEBS Lett. 587, 542–548 (2013).
Miyahira, A. K., Shahangian, A., Hwang, S., Sun, R. & Cheng, G. TANK-binding kinase-1 plays an important role during in vitro and in vivo type I IFN responses to DNA virus infections. J. Immunol. 182, 2248–2257 (2009).
Oakes, J. A., Davies, M. C. & Collins, M. O. TBK1: a new player in ALS linking autophagy and neuroinflammation. Mol. Brain 10, 5 (2017).
Pomerantz, J. L. & Baltimore, D. NF-κB activation by a signaling complex containing TRAF2, TANK and TBK1, a novel IKK-related kinase. EMBO J. 18, 6694–6704 (1999).
Jin, J. et al. The kinase TBK1 controls IgA class switching by negatively regulating noncanonical NF-κB signaling. Nat. Immunol. 13, 1101–1109 (2012).
Zhao, P. et al. TBK1 at the crossroads of inflammation and energy homeostasis in adipose tissue. Cell 172, 731–743.e12 (2018).
Heo, J. M., Ordureau, A., Paulo, J. A., Rinehart, J. & Harper, J. W. The PINK1-PARKIN mitochondrial ubiquitylation pathway drives a program of OPTN/NDP52 recruitment and TBK1 activation to promote mitophagy. Mol. Cell 60, 7–20 (2015).
Vicencio, E. et al. Implications of selective autophagy dysfunction for ALS pathology. Cells 9, 381 (2020).
Tsai, P. C. et al. Mutational analysis of TBK1 in Taiwanese patients with amyotrophic lateral sclerosis. Neurobiol. Aging 40, 191.e11–191.e16 (2016).
Williams, K. L. et al. Novel TBK1 truncating mutation in a familial amyotrophic lateral sclerosis patient of Chinese origin. Neurobiol. Aging 36, 3334.e1–3334.e5 (2015).
Shu, S. et al. Screening of the TBK1 gene in familial and sporadic amyotrophic lateral sclerosis patients of Chinese origin. Amyotroph. Lateral Scler. Frontotemporal Degener. 17, 605–607 (2016).
Pozzi, L. et al. TBK1 mutations in Italian patients with amyotrophic lateral sclerosis: genetic and functional characterisation. J. Neurol. Neurosurg. Psychiatry 88, 869–875 (2017).
de Majo, M. et al. ALS-associated missense and nonsense TBK1 mutations can both cause loss of kinase function. Neurobiol. Aging 71, 266.e1–266.e10 (2018).
Weinreich, M. et al. Neuropathological characterization of a novel TANK binding kinase (TBK1) gene loss of function mutation associated with amyotrophic lateral sclerosis. Neuropathol. Appl. Neurobiol. 46, 279–291 (2020).
Ye, J. et al. Effects of ALS-associated TANK binding kinase 1 mutations on protein-protein interactions and kinase activity. Proc. Natl Acad. Sci. USA 116, 24517–24526 (2019).
Gijselinck, I. et al. Loss of TBK1 is a frequent cause of frontotemporal dementia in a Belgian cohort. Neurology 85, 2116–2125 (2015).
Pottier, C. et al. Whole-genome sequencing reveals important role for TBK1 and OPTN mutations in frontotemporal lobar degeneration without motor neuron disease. Acta Neuropathol. 130, 77–92 (2015).
van der Zee, J. et al. TBK1 mutation spectrum in an extended European patient cohort with frontotemporal dementia and amyotrophic lateral sclerosis. Hum. Mutat. 38, 297–309 (2017).
Foster, A. D. et al. ALS-associated TBK1 variant p.G175S is defective in phosphorylation of p62 and impacts TBK1-mediated signalling and TDP-43 autophagic degradation. Mol. Cell Neurosci. 108, 103539 (2020).
Harding, O. et al. ALS- and FTD-associated missense mutations in TBK1 differentially disrupt mitophagy. Proc. Natl Acad. Sci. USA 118, e2025053118 (2021).
Bonnard, M. et al. Deficiency of T2K leads to apoptotic liver degeneration and impaired NF-κB-dependent gene transcription. EMBO J. 19, 4976–4985 (2000).
Brenner, D. et al. Heterozygous Tbk1 loss has opposing effects in early and late stages of ALS in mice. J. Exp. Med. 216, 267–278 (2019).
Gerbino, V. et al. The loss of TBK1 kinase activity in motor neurons or in all cell types differentially impacts ALS disease progression in SOD1 mice. Neuron 106, 789–805.e5 (2020).
Bruno, C. et al. Haploinsufficiency of TANK-binding kinase 1 prepones age-associated neuroinflammatory changes without causing motor neuron degeneration in aged mice. Brain Commun. 2, fcaa133 (2020).
Duan, W. et al. Deletion of Tbk1 disrupts autophagy and reproduces behavioral and locomotor symptoms of FTD-ALS in mice. Aging 11, 2457–2476 (2019).
Ying, H. & Yue, B. Y. Optineurin: the autophagy connection. Exp. Eye Res. 144, 73–80 (2016).
Bansal, M., Swarup, G. & Balasubramanian, D. Functional analysis of optineurin and some of its disease-associated mutants. IUBMB Life 67, 120–128 (2015).
Sippl, C., Zeilbeck, L. F., Fuchshofer, R. & Tamm, E. R. Optineurin associates with the podocyte Golgi complex to maintain its structure. Cell Tissue Res. 358, 567–583 (2014).
Sahlender, D. A. et al. Optineurin links myosin VI to the Golgi complex and is involved in Golgi organization and exocytosis. J. Cell Biol. 169, 285–295 (2005).
Park, B. C., Shen, X., Samaraweera, M. & Yue, B. Y. Studies of optineurin, a glaucoma gene: Golgi fragmentation and cell death from overexpression of wild-type and mutant optineurin in two ocular cell types. Am. J. Pathol. 169, 1976–1989 (2006).
Fifita, J. A. et al. A novel amyotrophic lateral sclerosis mutation in OPTN induces ER stress and Golgi fragmentation in vitro. Amyotroph. Lateral Scler. Frontotemporal Degener. 18, 126–133 (2017).
Feng, S. M. et al. Novel mutation in optineurin causing aggressive ALS+/-frontotemporal dementia. Ann. Clin. Transl. Neurol. 6, 2377–2383 (2019).
Korac, J. et al. Ubiquitin-independent function of optineurin in autophagic clearance of protein aggregates. J. Cell Sci. 126, 580–592 (2013).
McCall, A. L. et al. Respiratory pathology in the Optn−/− mouse model of amyotrophic lateral sclerosis. Respir. Physiol. Neurobiol. 282, 103525 (2020).
Maruyama, H. et al. Mutations of optineurin in amyotrophic lateral sclerosis. Nature 465, 223–226 (2010).
Tümer, Z. et al. Novel heterozygous nonsense mutation of the OPTN gene segregating in a Danish family with ALS. Neurobiol. Aging 33, 208.e1–208.e5 (2012).
Goldstein, O. et al. OPTN 691_692insAG is a founder mutation causing recessive ALS and increased risk in heterozygotes. Neurology 86, 446–453 (2016).
Gotkine, M. et al. A recessive S174X mutation in optineurin causes amyotrophic lateral sclerosis through a loss of function via allele-specific nonsense-mediated decay. Neurobiol. Aging 106, 1–6 (2021).
Farhan, S. M. K., Gendron, T. F., Petrucelli, L., Hegele, R. A. & Strong, M. J. OPTN p.Met468Arg and ATXN2 intermediate length polyQ extension in families with C9orf72 mediated amyotrophic lateral sclerosis and frontotemporal dementia. Am. J. Med. Genet. B Neuropsychiatr. Genet. 177, 75–85 (2018).
Millecamps, S. et al. Screening of OPTN in French familial amyotrophic lateral sclerosis. Neurobiol. Aging 32, 557.e11–557.e13 (2011).
Kamada, M. et al. Clinicopathologic features of autosomal recessive amyotrophic lateral sclerosis associated with optineurin mutation. Neuropathology 34, 64–70 (2014).
Shen, W. C., Li, H. Y., Chen, G. C., Chern, Y. & Tu, P. H. Mutations in the ubiquitin-binding domain of OPTN/optineurin interfere with autophagy-mediated degradation of misfolded proteins by a dominant-negative mechanism. Autophagy 11, 685–700 (2015).
Sundaramoorthy, V. et al. Defects in optineurin- and myosin VI-mediated cellular trafficking in amyotrophic lateral sclerosis. Hum. Mol. Genet. 24, 3830–3846 (2015).
Evans, C. S. & Holzbaur, E. L. Degradation of engulfed mitochondria is rate-limiting in optineurin-mediated mitophagy in neurons. Elife 9, e50260 (2020).
Moore, A. S. & Holzbaur, E. L. Dynamic recruitment and activation of ALS-associated TBK1 with its target optineurin are required for efficient mitophagy. Proc. Natl Acad. Sci. USA 113, E3349–E3358 (2016).
Nakazawa, S. et al. Linear ubiquitination is involved in the pathogenesis of optineurin-associated amyotrophic lateral sclerosis. Nat. Commun. 7, 12547 (2016).
Akizuki, M. et al. Optineurin suppression causes neuronal cell death via NF-κB pathway. J. Neurochem. 126, 699–704 (2013).
Surpili, M. J., Delben, T. M. & Kobarg, J. Identification of proteins that interact with the central coiled-coil region of the human protein kinase NEK1. Biochemistry 42, 15369–15376 (2003).
Melo-Hanchuk, T. D. et al. NEK1 kinase domain structure and its dynamic protein interactome after exposure to cisplatin. Sci. Rep. 7, 5445 (2017).
Nguyen, H. P. et al. NEK1 genetic variability in a Belgian cohort of ALS and ALS-FTD patients. Neurobiol. Aging 61, 255.e1–255.e7 (2018).
Fry, A. M., O’Regan, L., Sabir, S. R. & Bayliss, R. Cell cycle regulation by the NEK family of protein kinases. J. Cell Sci. 125, 4423–4433 (2012).
Chen, Y., Craigen, W. J. & Riley, D. J. Nek1 regulates cell death and mitochondrial membrane permeability through phosphorylation of VDAC1. Cell Cycle 8, 257–267 (2009).
Chen, Y., Gaczynska, M., Osmulski, P., Polci, R. & Riley, D. J. Phosphorylation by Nek1 regulates opening and closing of voltage dependent anion channel 1. Biochem. Biophys. Res. Commun. 394, 798–803 (2010).
Brenner, D. et al. NEK1 mutations in familial amyotrophic lateral sclerosis. Brain 139, e28 (2016).
Lattante, S. et al. Novel variants and cellular studies on patients’ primary fibroblasts support a role for NEK1 missense variants in ALS pathogenesis. Hum. Mol. Genet. 30, 65–71 (2021).
Higelin, J. et al. NEK1 loss-of-function mutation induces DNA damage accumulation in ALS patient-derived motoneurons. Stem Cell Res. 30, 150–162 (2018).
Mah, L. J., El-Osta, A. & Karagiannis, T. C. gammaH2AX: a sensitive molecular marker of DNA damage and repair. Leukemia 24, 679–686 (2010).
Nicholson, G. et al. Distinctive genetic and clinical features of CMT4J: a severe neuropathy caused by mutations in the PI(3,5)P2 phosphatase FIG4. Brain 134, 1959–1971 (2011).
Marat, A. L. & Haucke, V. Phosphatidylinositol 3-phosphates – at the interface between cell signalling and membrane traffic. EMBO J. 35, 561–579 (2016).
Chow, C. Y. et al. Deleterious variants of FIG4, a phosphoinositide phosphatase, in patients with ALS. Am. J. Hum. Genet. 84, 85–88 (2009).
Osmanovic, A. et al. FIG4 variants in central European patients with amyotrophic lateral sclerosis: a whole-exome and targeted sequencing study. Eur. J. Hum. Genet. 25, 324–331 (2017).
Duex, J. E., Nau, J. J., Kauffman, E. J. & Weisman, L. S. Phosphoinositide 5-phosphatase Fig 4p is required for both acute rise and subsequent fall in stress-induced phosphatidylinositol 3,5-bisphosphate levels. Eukaryot. Cell 5, 723–731 (2006).
Chow, C. Y. et al. Mutation of FIG4 causes neurodegeneration in the pale tremor mouse and patients with CMT4J. Nature 448, 68–72 (2007).
Lenk, G. M. et al. Pathogenic mechanism of the FIG4 mutation responsible for Charcot-Marie-Tooth disease CMT4J. PLoS Genet. 7, e1002104 (2011).
Bharadwaj, R., Cunningham, K. M., Zhang, K. & Lloyd, T. E. FIG4 regulates lysosome membrane homeostasis independent of phosphatase function. Hum. Mol. Genet. 25, 681–692 (2016).
Katona, I. et al. Distinct pathogenic processes between Fig4-deficient motor and sensory neurons. Eur. J. Neurosci. 33, 1401–1410 (2011).
Zhang, X. et al. Mutation of FIG4 causes a rapidly progressive, asymmetric neuronal degeneration. Brain 131, 1990–2001 (2008).
Ferguson, C. J., Lenk, G. M. & Meisler, M. H. Defective autophagy in neurons and astrocytes from mice deficient in PI(3,5)P2. Hum. Mol. Genet. 18, 4868–4878 (2009).
Kyotani, A. et al. Knockdown of the Drosophila FIG4 induces deficient locomotive behavior, shortening of motor neuron, axonal targeting aberration, reduction of life span and defects in eye development. Exp. Neurol. 277, 86–95 (2016).
Presa, M. et al. AAV9-mediated FIG4 delivery prolongs life span in Charcot-Marie-Tooth disease type 4J mouse model. J. Clin. Invest. 131, e137159 (2021).
Kishimoto, K., Liu, S., Tsuji, T., Olson, K. A. & Hu, G. F. Endogenous angiogenin in endothelial cells is a general requirement for cell proliferation and angiogenesis. Oncogene 24, 445–456 (2005).
Sheng, J. & Xu, Z. Three decades of research on angiogenin: a review and perspective. Acta Biochim. Biophys. Sin. 48, 399–410 (2016).
Lee, S. H., Kim, K. W., Min, K. M., Chang, S. I. & Kim, J. C. Angiogenin reduces immune inflammation via inhibition of TANK-binding kinase 1 expression in human corneal fibroblast cells. Mediat. Inflamm. 2014, 861435 (2014).
Fu, H. et al. Stress induces tRNA cleavage by angiogenin in mammalian cells. FEBS Lett. 583, 437–442 (2009).
Yamasaki, S., Ivanov, P., Hu, G. F. & Anderson, P. Angiogenin cleaves tRNA and promotes stress-induced translational repression. J. Cell Biol. 185, 35–42 (2009).
Wu, D. et al. Angiogenin loss-of-function mutations in amyotrophic lateral sclerosis. Ann. Neurol. 62, 609–617 (2007).
Crabtree, B. et al. Characterization of human angiogenin variants implicated in amyotrophic lateral sclerosis. Biochemistry 46, 11810–11818 (2007).
Thiyagarajan, N., Ferguson, R., Subramanian, V. & Acharya, K. R. Structural and molecular insights into the mechanism of action of human angiogenin-ALS variants in neurons. Nat. Commun. 3, 1121 (2012).
Padhi, A. K., Kumar, H., Vasaikar, S. V., Jayaram, B. & Gomes, J. Mechanisms of loss of functions of human angiogenin variants implicated in amyotrophic lateral sclerosis. PLoS One 7, e32479 (2012).
Padhi, A. K., Jayaram, B. & Gomes, J. Prediction of functional loss of human angiogenin mutants associated with ALS by molecular dynamics simulations. Sci. Rep. 3, 1225 (2013).
Subramanian, V. & Feng, Y. A new role for angiogenin in neurite growth and pathfinding: implications for amyotrophic lateral sclerosis. Hum. Mol. Genet. 16, 1445–1453 (2007).
Subramanian, V., Crabtree, B. & Acharya, K. R. Human angiogenin is a neuroprotective factor and amyotrophic lateral sclerosis associated angiogenin variants affect neurite extension/pathfinding and survival of motor neurons. Hum. Mol. Genet. 17, 130–149 (2008).
Kieran, D. et al. Control of motoneuron survival by angiogenin. J. Neurosci. 28, 14056–14061 (2008).
Skorupa, A. et al. Motoneurons secrete angiogenin to induce RNA cleavage in astroglia. J. Neurosci. 32, 5024–5038 (2012).
Hoang, T. T., Johnson, D. A., Raines, R. T. & Johnson, J. A. Angiogenin activates the astrocytic Nrf2/antioxidant-response element pathway and thereby protects murine neurons from oxidative stress. J. Biol. Chem. 294, 15095–15103 (2019).
Kishikawa, H., Wu, D. & Hu, G. F. Targeting angiogenin in therapy of amyotrophic lateral sclerosis. Expert. Opin. Ther. Targets 12, 1229–1242 (2008).
Aluri, K. C., Salisbury, J. P., Prehn, J. H. M. & Agar, J. N. Loss of angiogenin function is related to earlier ALS onset and a paradoxical increase in ALS duration. Sci. Rep. 10, 3715 (2020).
Balakrishnan, B. & Jayandharan, G. R. Basic biology of adeno-associated virus (AAV) vectors used in gene therapy. Curr. Gene Ther. 14, 86–100 (2014).
Sonntag, F., Schmidt, K. & Kleinschmidt, J. A. A viral assembly factor promotes AAV2 capsid formation in the nucleolus. Proc. Natl Acad. Sci. USA 107, 10220–10225 (2010).
Yan, Z., Zak, R., Zhang, Y. & Engelhardt, J. F. Inverted terminal repeat sequences are important for intermolecular recombination and circularization of adeno-associated virus genomes. J. Virol. 79, 364–379 (2005).
Choi, V. W., McCarty, D. M. & Samulski, R. J. Host cell DNA repair pathways in adeno-associated viral genome processing. J. Virol. 80, 10346–10356 (2006).
Wang, L. J. et al. Neuroprotective effects of glial cell line-derived neurotrophic factor mediated by an adeno-associated virus vector in a transgenic animal model of amyotrophic lateral sclerosis. J. Neurosci. 22, 6920–6928 (2002).
Mòdol-Caballero, G. et al. Specific expression of glial-derived neurotrophic factor in muscles as gene therapy strategy for amyotrophic lateral sclerosis. Neurotherapeutics 18, 1113–1126 (2021).
Baloh, R. H. et al. Transplantation of human neural progenitor cells secreting GDNF into the spinal cord of patients with ALS: a phase 1/2a trial. Nat. Med. 28, 1813–1822 (2022).
Kaspar, B. K., Lladó, J., Sherkat, N., Rothstein, J. D. & Gage, F. H. Retrograde viral delivery of IGF-1 prolongs survival in a mouse ALS model. Science 301, 839–842 (2003).
Lin, H. et al. Intramuscular delivery of scAAV9-hIGF1 prolongs survival in the hSOD1 G93A ALS mouse model via upregulation of D-amino acid oxidase. Mol. Neurobiol. 55, 682–695 (2018).
Wang, W. et al. Systemic administration of scAAV9-IGF1 extends survival in SOD1G93A ALS mice via inhibiting p38 MAPK and the JNK-mediated apoptosis pathway. Brain Res. Bull. 139, 203–210 (2018).
Cudkowicz, M. E. et al. A randomized placebo-controlled phase 3 study of mesenchymal stem cells induced to secrete high levels of neurotrophic factors in amyotrophic lateral sclerosis. Muscle Nerve 65, 291–302 (2022).
Gothelf, Y., Abramov, N., Harel, A. & Offen, D. Safety of repeated transplantations of neurotrophic factors-secreting human mesenchymal stromal stem cells. Clin. Transl. Med. 3, 21 (2014).
Petrou, P. et al. Safety and clinical effects of mesenchymal stem cells secreting neurotrophic factor transplantation in patients with amyotrophic lateral sclerosis: results of phase 1/2 and 2a clinical trials. JAMA Neurol. 73, 337–344 (2016).
Brenner, D. et al. Hot-spot KIF5A mutations cause familial ALS. Brain 141, 688–697 (2018).
Nicolas, A. et al. Genome-wide analyses identify KIF5A as a novel ALS gene. Neuron 97, 1268–1283.e6 (2018).
Campbell, P. D. et al. Unique function of kinesin Kif5A in localization of mitochondria in axons. J. Neurosci. 34, 14717–14732 (2014).
Nakano, J., Chiba, K. & Niwa, S. An ALS-associated KIF5A mutant forms oligomers and aggregates and induces neuronal toxicity. Genes. Cell 27, 421–435 (2022).
Baron, D. M. et al. ALS-associated KIF5A mutations abolish autoinhibition resulting in a toxic gain of function. Cell Rep. 39, 110598 (2022).
Pant, D. C. et al. ALS-linked KIF5A ΔExon27 mutant causes neuronal toxicity through gain-of-function. EMBO Rep. 23, e54234 (2022).
Acknowledgements
I.G. is supported by a SITraN postdoctoral fellowship. P.J.S. is supported as a National Institute for Health and Care Research (NIHR) Senior Investigator (NF-SI-0617-10077), by the NIHR Sheffield Biomedical Research Centre (IS-BRC-1215-20017). P.J.S. and M.A. are supported by the EU Innovative Medicines Initiative Accelerating Research and Development for Advanced Therapies (IMI ARDAT 945473) and a Medical Research Council (MRC) LifeArc award (MR/V030140/1). M.A. is further sponsored by the European Research Council (ERC Advanced Award 294745), an MRC Award (MR/G1001492), CureAP4, EU Joint Programme — Neurodegenerative Disease Research (MR/V000470/1) and Alzheimer’s Research UK. P.J.S. and J.K. are supported by the Motor Neurone Disease Association (AMBRoSIA 972-797 and NECTAR 974-797).
Author information
Authors and Affiliations
Contributions
I.G. and P.J.S. researched data for the article. I.G., J.K., M.A. and P.J.S. contributed substantially to discussion of the content. All authors wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks M. Sendtner and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ALS type 11: https://www.ncbi.nlm.nih.gov/medgen/393399
Ensembl: https://www.ensembl.org/index.html
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Giovannelli, I., Higginbottom, A., Kirby, J. et al. Prospects for gene replacement therapies in amyotrophic lateral sclerosis. Nat Rev Neurol 19, 39–52 (2023). https://doi.org/10.1038/s41582-022-00751-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-022-00751-5
This article is cited by
-
Rare DNAJC7 Variants May Play a Minor Role in Chinese Patients with ALS
Molecular Neurobiology (2024)
-
Translating the ALS Genetic Revolution into Therapies: A Review
Current Treatment Options in Neurology (2024)
-
The Node of Ranvier as an Interface for Axo-Glial Interactions: Perturbation of Axo-Glial Interactions in Various Neurological Disorders
Journal of Neuroimmune Pharmacology (2023)