Abstract
Status epilepticus is a life-threatening neurological emergency that affects both adults and children. Approximately 36% of episodes of status epilepticus do not respond to the current preferred first-line treatment, benzodiazepines. The proportion of episodes that are refractory to benzodiazepines is higher in low-income and middle-income countries (LMICs) than in high-income countries (HICs). Evidence suggests that longer episodes of status epilepticus alter brain physiology, thereby contributing to the emergence of benzodiazepine resistance. Such changes include alterations in GABAA receptor function and in the transmembrane gradient for chloride, both of which erode the ability of benzodiazepines to enhance inhibitory synaptic signalling. Often, current management guidelines for status epilepticus do not account for these duration-related changes in pathophysiology, which might differentially impact individuals in LMICs, where the average time taken to reach medical attention is longer than in HICs. In this Perspective article, we aim to combine clinical insights and the latest evidence from basic science to inspire a new, context-specific approach to efficiently managing status epilepticus.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Code availability
All code used to generate Fig. 1 and Supplementary Fig. 1 can be accessed at https://github.com/richardjburman/bzp_review.
Data availability
All data used to generate Fig. 1 and Supplementary Fig. 1. can be accessed at https://github.com/richardjburman/bzp_review.
Change history
18 May 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41582-022-00673-2
References
The World Health Organization. Epilepsy: a Public Health Imperative (WHO, 2019).
Trinka, E. et al. A definition and classification of status epilepticus — report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia 56, 1515–1523 (2015).
Abend, N. S. & Loddenkemper, T. Management of pediatric status epilepticus. Curr. Treat. Options Neurol. 16, 301 (2014).
Brophy, G. M. et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit. Care 17, 3–23 (2012).
Crawshaw, A. A. & Cock, H. R. Medical management of status epilepticus: emergency room to intensive care unit. Seizure 75, 145–152 (2020).
Glauser, T. et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the guideline committee of the american epilepsy society. Epilepsy Curr. 16, 48–61 (2016).
Trinka, E., Höfler, J., Leitinger, M. & Brigo, F. Pharmacotherapy for status epilepticus. Drugs 75, 1499–1521 (2015).
Burman, R. J. et al. A Comparison of parenteral phenobarbital vs. parenteral phenytoin as second-line management for pediatric convulsive status epilepticus in a resource-limited setting. Front. Neurol. 10, 506 (2019).
Kapur, J. et al. Randomized trial of three anticonvulsant medications for status epilepticus. N. Eng. J. Med. 381, 2103–2113 (2019).
Dalziel, S. R. et al. Levetiracetam versus phenytoin for second-line treatment of convulsive status epilepticus in children (ConSEPT): an open-label, multicentre, randomised controlled trial. Lancet 393, 2135–2145 (2019).
Lyttle, M. D. et al. Levetiracetam versus phenytoin for second-line treatment of paediatric convulsive status epilepticus (EcLiPSE): a multicentre, open-label, randomised trial. Lancet 393, 2125–2134 (2019).
Prabhakar, H. & Kalaivani, M. Propofol versus thiopental sodium for the treatment of refractory status epilepticus. Cochrane Database Syst. Rev. 2, CD009202 (2017).
Shorvon, S. & Ferlisi, M. The outcome of therapies in refractory and super-refractory convulsive status epilepticus and recommendations for therapy. Brain 135, 2314–2328 (2012).
Gaínza-Lein, M. et al. Association of time to treatment with short-term outcomes for pediatric patients with refractory convulsive status epilepticus. JAMA Neurol. 75, 410–418 (2018).
Beghi, E. et al. Global, regional, and national burden of epilepsy, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 357–375 (2019).
Feigin, V. L. et al. Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 16, 877–897 (2017).
Lee, B. Treatment gap for convulsive status epilepticus in resource-poor countries. Epilepsia 59, 135–139 (2018).
Newton, C. R. & Garcia, H. H. Epilepsy in poor regions of the world. Lancet 380, 1193–1201 (2012).
Newton, C. R. J. C. Status epilepticus in resource-poor countries. Epilepsia 50, 54–55 (2009).
Kantanen, A.-M., Sairanen, J. & Kälviäinen, R. Incidence of the different stages of status epilepticus in Eastern Finland: A population-based study. Epilepsy Behav. 101, 106413 (2019).
Leitinger, M. et al. Epidemiology of status epilepticus in adults: Apples, pears, and oranges — A critical review. Epilepsy Behav. 103, 106720 (2020).
Lu, M. et al. Epidemiology of status epilepticus in the United States: A systematic review. Epilepsy Behav. 112, 107459 (2020).
Shorvon, S. & Sen, A. What is status epilepticus and what do we know about its epidemiology? Seizure 75, 131–136 (2020).
Chin, R. F. et al. Incidence, cause, and short-term outcome of convulsive status epilepticus in childhood: prospective population-based study. Lancet 368, 222–229 (2006).
Sadarangani, M. et al. Incidence and outcome of convulsive status epilepticus in Kenyan children: a cohort study. Lancet Neurol. 7, 145–150 (2008).
Schubert-Bast, S. et al. Burden and epidemiology of status epilepticus in infants, children, and adolescents: A population-based study on German health insurance data. Epilepsia 60, 911–920 (2019).
Leitinger, M. et al. Epidemiology of status epilepticus in adults: A population-based study on incidence, causes, and outcomes. Epilepsia 60, 53–62 (2019).
Nazerian, P. et al. Incidence, management and short-term prognosis of status epilepticus in the emergency department: a population survey. Eur. J. Emerg. Med. 26, 228–230 (2019).
Tiamkao, S., Pranboon, S., Thepsuthammarat, K. & Sawanyawisuth, K. Incidences and outcomes of status epilepticus: A 9-year longitudinal national study. Epilepsy Behav. 49, 135–137 (2015).
Sánchez, S. & Rincon, F. Status epilepticus: epidemiology and public health needs. J. Clin. Med. 5, 71 (2016).
Chamberlain, J. M. et al. Efficacy of levetiracetam, fosphenytoin, and valproate for established status epilepticus by age group (ESETT): a double-blind, responsive-adaptive, randomised controlled trial. Lancet 395, 1217–1224 (2020).
Strzelczyk, A., Knake, S., Oertel, W. H., Rosenow, F. & Hamer, H. M. Inpatient treatment costs of status epilepticus in adults in Germany. Seizure 22, 882–885 (2013).
Kariuki, S. M. et al. Prevalence and factors associated with convulsive status epilepticus in Africans with epilepsy. Neurology 84, 1838–1845 (2015).
Newton, C. R. & Kariuki, S. M. Status epilepticus in sub-Saharan Africa: New findings. Epilepsia 54, 50–53 (2013).
Treiman, D. M. The role of benzodiazepines in the management of status epilepticus. Neurology 40, 32–42 (1990).
Burman, R. J. et al. Excitatory GABAergic signalling is associated with benzodiazepine resistance in status epilepticus. Brain 142, 3482–3501 (2019).
Sánchez Fernández, I. et al. Time from convulsive status epilepticus onset to anticonvulsant administration in children. Neurology 84, 2304–2311 (2015).
Guterman, E. L. et al. Prehospital midazolam use and outcomes among patients with out-of-hospital status epilepticus. Neurology 95, e3203–e3212 (2020).
Sathe, A. G. et al. Underdosing of benzodiazepines in patients with status epilepticus enrolled in established status epilepticus treatment trial. Acad. Emerg. Med. 26, 940–943 (2019).
Silbergleit, R. et al. Intramuscular versus Intravenous Therapy for Prehospital Status Epilepticus. N. Eng. J. Med. 366, 591–600 (2012).
Alldredge, B. K. et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N. Eng. J. Med. 345, 631–637 (2001).
Betjemann, J. P. & Lowenstein, D. H. Status epilepticus in adults. Lancet Neurol. 14, 615–624 (2015).
Olsen, R. W. GABAA receptor: Positive and negative allosteric modulators. Neuropharmacology 136, 10–22 (2018).
Olsen, R. W. & Sieghart, W. GABAA receptors: subtypes provide diversity of function and pharmacology. Neuropharmacology 56, 141–148 (2009).
Benke, D. et al. Analysis of the presence and abundance of GABAA receptors containing two different types of α subunits in murine brain using point-mutated α subunits. J. Biol. Chem. 279, 43654–43660 (2004).
Simon, J., Wakimoto, H., Fujita, N., Lalande, M. & Barnard, E. A. Analysis of the Set of GABAA receptor genes in the human genome. J. Biol. Chem. 279, 41422–41435 (2004).
Sigel, E. & Steinmann, M. E. Structure, function, and modulation of gabaa receptors. J. Biol. Chem. 287, 40224–40231 (2012).
Edwards, F. A., Konnerth, A. & Sakmann, B. Quantal analysis of inhibitory synaptic transmission in the dentate gyrus of rat hippocampal slices: a patch-clamp study. J. Physiol. 430, 213–249 (1990).
Nusser, Z., Cull-Candy, S. & Farrant, M. Differences in Synaptic GABAA receptor number underlie variation in GABA mini amplitude. Neuron 19, 697–709 (1997).
Brickley, S. G., Cull-Candy, S. G. & Farrant, M. Single-channel properties of synaptic and extrasynaptic GABAA receptors suggest differential targeting of receptor subtypes. J. Neurosci. 19, 2960–2973 (1999).
Farrant, M. & Nusser, Z. Variations on an inhibitory theme: phasic and tonic activation of GABAA receptors. Nat. Rev. Neurosci. 6, 215–229 (2005).
Rudolph, U. & Möhler, H. GABA-based therapeutic approaches: GABAA receptor subtype functions. Curr. Opin. Pharmacol. 6, 18–23 (2006).
Sigel, E. & Steinmann, M. E. Structure, function and modulation of GABAA receptors. J. Biol. Chem. 287, 40224–40231 (2012).
Simon, J., Wakimoto, H., Fujita, N., Lalande, M. & Barnard, E. A. Analysis of the set of GABAA genes in the Human Genome. J. Biol. Chem. 279, 41422–41435 (2004).
Farrant, M. & Kaila, K. in Progress in Brain Research (eds Tepper, J. M., Abercrombie, E. D. & Bolam, J. P.) 59–87 (Elsevier, 2007).
Caraiscos, V. B. et al. Tonic inhibition in mouse hippocampal CA1 pyramidal neurons is mediated by α5 subunit-containing gamma-aminobutyric acid type A receptors. Proc. Natl Acad. Sci. USA 101, 3662–3667 (2004).
Vithlani, M., Terunuma, M. & Moss, S. J. The Dynamic Modulation of GABAA receptor trafficking and its role in regulating the plasticity of inhibitory synapses. Physiol. Rev. 91, 1009–1022 (2011).
Richter, L. et al. Diazepam-bound GABAA receptor models identify new benzodiazepine binding-site ligands. Nat. Chem. Biol. 8, 455–464 (2012).
Phulera, S. et al. Cryo-EM structure of the benzodiazepine-sensitive α1β1γ2S tri-heteromeric GABAA receptor in complex with GABA. eLife 7, e39383 (2018).
Kaila, K. Ionic basis of GABAA receptor channel function in the nervous system. Prog. Neurobiol. 42, 489–537 (1994).
Kaila, K., Pasternack, M., Saarikoski, J. & Voipio, J. Influence of GABA-gated bicarbonate conductance on potential, current and intracellular chloride in crayfish muscle fibres. J. Physiol. 416, 161–181 (1989).
Kaila, K. & Voipio, J. Postsynaptic fall in intracellular pH induced by GABA-activated bicarbonate conductance. Nature 330, 163–165 (1987).
Krogsgaard-Larsen, P., Froelund, B., Joergensen, F. S. & Schousboe, A. GABAA receptor agonists, partial agonists, and antagonists. design and therapeutic prospects. J. Med. Chem. 37, 2489–2505 (1994).
Müller, W. & Wollert, U. Characterization of the binding of benzodiazepines to human serum albumin. Naunyn Schmiedeberg’s Arch. Pharmacol. 280, 229–237 (1973).
Haefely, W. E., Martin, J. R., Richards, J. G. & Schoch, P. The multiplicity of actions of benzodiazepine receptor ligands. Can. J. Psychiatry 38, 102–108 (1993).
Costa, E. & Guidotti, A. Endogenous ligands for benzodiazepine recognition sites. Biochem. Pharmacol. 34, 3399–3403 (1985).
Farzampour, Z., Reimer, R. J. & Huguenard, J. Endozepines. Adv. Pharmacol. 72, 147–164 (2015).
Christian, C. A. & Huguenard, J. R. Astrocytes potentiate GABAergic transmission in the thalamic reticular nucleus via endozepine signaling. Proc. Natl Acad. Sci. USA 110, 20278–20283 (2013).
Christian, C. A. et al. Endogenous positive allosteric modulation of GABAA receptors by diazepam binding inhibitor. Neuron 78, 1063–1074 (2013).
Wieland, H. A., Lüddens, H. & Seeburg, P. H. A single histidine in GABAA receptors is essential for benzodiazepine agonist binding. J. Biol. Chem. 267, 1426–1429 (1992).
Duncalfe, L. L., Carpenter, M. R., Smillie, L. B., Martin, I. L. & Dunn, S. M. J. The major site of photoaffinity labeling of the γ-aminobutyric acid type A receptor by [3H]flunitrazepam is histidine 102 of the α subunit. J. Biol. Chem. 271, 9209–9214 (1996).
Goldschen-Ohm, M. P., Wagner, D. A., Petrou, S. & Jones, M. V. An epilepsy-related region in the GABAA receptor mediates long-distance effects on GABA and benzodiazepine binding sites. Mol. Pharmacol. 77, 35–45 (2010).
Haefely, W., Kulcsár, A. & Möhler, H. Possible involvement of GABA in the central actions of benzodiazepines. Psychopharmacol. Bull. 11, 58–59 (1975).
Vicini, S., Mienville, J. M. & Costa, E. Actions of benzodiazepine and beta-carboline derivatives on gamma-aminobutyric acid-activated Cl- channels recorded from membrane patches of neonatal rat cortical neurons in culture. J. Pharmacol. Exp. Ther. 243, 1195–1201 (1987).
Rogers, C. J., Twyman, R. E. & Macdonald, R. L. Benzodiazepine and beta-carboline regulation of single GABAA receptor channels of mouse spinal neurones in culture. J. Physiol. 475, 69–82 (1994).
Ben-Ari, Y. Excitatory actions of GABA during development: the nature of the nurture. Nat. Rev. Neurosci. 3, 728–739 (2002).
Blaesse, P., Airaksinen, M. S., Rivera, C. & Kaila, K. Cation-chloride cotransporters and neuronal function. Neuron 61, 820–838 (2009).
Kaila, K., Price, T. J., Payne, J. A., Puskarjov, M. & Voipio, J. Cation-chloride cotransporters in neuronal development, plasticity and disease. Nat. Rev. Neurosci. 15, 637–654 (2014).
Raimondo, J. V., Richards, B. A. & Woodin, M. A. Neuronal chloride and excitability — the big impact of small changes. Curr. Opin. Neurobiol. 43, 35–42 (2017).
Raimondo, J. V., Burman, R. J., Katz, A. A. & Akerman, C. J. Ion dynamics during seizures. Front. Cell. Neurosci. 9, 419 (2015).
Wright, R., Raimondo, J. V. & Akerman, C. J. Spatial and temporal dynamics in the ionic driving force for GABAA receptors. Neural Plast. 2011, 728395 (2011).
Delpire, E. Cation-chloride cotransporters in neuronal communication. Physiology 15, 309–312 (2000).
Düsterwald, K. M. et al. Biophysical models reveal the relative importance of transporter proteins and impermeant anions in chloride homeostasis. eLife 7, e39575 (2018).
Glykys, J. et al. Local impermeant anions establish the neuronal chloride concentration. Science 343, 670–675 (2014).
Payne, J. A., Rivera, C., Voipio, J. & Kaila, K. Cation–chloride co-transporters in neuronal communication, development and trauma. Trends Neurosci. 26, 199–206 (2003).
Hille, B. in Ion Channels of Excitable Membranes (ed. Hille, B.) (Sinauer, 2001).
Aronson, P. S. in Medical Physiology. A Cellular and Molecular Approach (ed. Boron, W. F. & Boulpaep, E. L.) 106–146 (Elsevier, 2012).
Voipio, J. et al. Comment on “Local impermeant anions establish the neuronal chloride concentration”. Science 345, 1130 (2014).
Rivera, C. et al. The K+/Cl− co-transporter KCC2 renders GABA hyperpolarizing during neuronal maturation. Nature 397, 251–255 (1999).
Kakazu, Y., Akaike, N., Komiyama, S. & Nabekura, J. Regulation of intracellular chloride by cotransporters in developing lateral superior olive neurons. J. Neurosci. 19, 2843–2851 (1999).
Yamada, J. et al. Cl− uptake promoting depolarizing GABA actions in immature rat neocortical neurones is mediated by NKCC1. J. Physiol. 557, 829–841 (2004).
Achilles, K. et al. Kinetic properties of Cl− uptake mediated by Na+-dependent K+-2Cl− cotransport in immature rat neocortical neurons. J. Neurosci. 27, 8616–8627 (2007).
Tyzio, R. et al. Postnatal changes in somatic γ-aminobutyric acid signalling in the rat hippocampus. Eur. J. Neurosci. 27, 2515–2528 (2008).
Vanhatalo, S. et al. Slow endogenous activity transients and developmental expression of K+–Cl− cotransporter 2 in the immature human cortex. Eur. J. Neurosci. 22, 2799–2804 (2005).
Sedmak, G. et al. Developmental expression patterns of KCC2 and functionally associated molecules in the human brain. Cereb. Cortex 26, 4574–4589 (2016).
Virtanen, M. A., Uvarov, P., Mavrovic, M., Poncer, J. C. & Kaila, K. The multifaceted roles of KCC2 in cortical development. Trends Neurosci. 44, 378–392 (2021).
Löscher, W. & Kaila, K. CNS pharmacology of NKCC1 inhibitors. Neuropharmacology 205, 108910 (2021).
Saunders, A. et al. Molecular diversity and specializations among the cells of the adult mouse brain. Cell 174, 1015–1030 (2018).
Bakken, T. E. et al. Single-cell and single-nucleus RNA-seq uncovers shared and distinct axes of variation in dorsal LGN neurons in mice, non-human primates, and humans. eLife 10, e64875 (2021).
Khirug, S. et al. GABAergic depolarization of the axon initial segment in cortical principal neurons is caused by the Na–K–2Cl cotransporter NKCC1. J. Neurosci. 28, 4635–4639 (2008).
Szabadics, J. et al. Excitatory Effect of GABAergic axo-axonic cells in cortical microcircuits. Science 311, 233–235 (2006).
Lee, H. H. C., Jurd, R. & Moss, S. J. Tyrosine phosphorylation regulates the membrane trafficking of the potassium chloride co-transporter KCC2. Mol. Cell. Neurosci. 45, 173–179 (2010).
Lee, H. H. C., Deeb, T. Z., Walker, J. A., Davies, P. A. & Moss, S. J. NMDA receptor activity downregulates KCC2 resulting in depolarizing GABAA receptor–mediated currents. Nat. Neurosci. 14, 736–743 (2011).
Rivera, C. et al. Mechanism of activity-dependent downregulation of the neuron-specific K-Cl Cotransporter KCC2. J. Neurosci. 24, 4683–4691 (2004).
Pathak, H. R. et al. Disrupted dentate granule cell chloride regulation enhances synaptic excitability during development of temporal lobe epilepsy. J. Neurosci. 27, 14012–14022 (2007).
Bragin, D. E., Sanderson, J. L., Peterson, S., Connor, J. A. & Müller, W. S. Development of epileptiform excitability in the deep entorhinal cortex after status epilepticus. Eur. J. Neuro. 30, 611–624 (2009).
Li, X. et al. Long-term expressional changes of Na+-K+-Cl- co-transporter 1 (NKCC1) and K+-Cl- co-transporter 2 (KCC2) in CA1 region of hippocampus following lithium-pilocarpine induced status epilepticus (PISE). Brain Res. 1221, 141–146 (2008).
Barmashenko, G., Hefft, S., Aertsen, A., Kirschstein, T. & Köhling, R. Positive shifts of the GABAA receptor reversal potential due to altered chloride homeostasis is widespread after status epilepticus. Epilepsia 52, 1570–1578 (2011).
Huberfeld, G. et al. Perturbed chloride homeostasis and GABAergic signaling in human temporal lobe epilepsy. J. Neurosci. 27, 9866–9873 (2007).
Kim, D. Y. et al. GABAA receptor-mediated activation of L-type calcium channels induces neuronal excitation in surgically resected human hypothalamic hamartomas. Epilepsia 49, 861–871 (2008).
Pallud, J. et al. Cortical GABAergic excitation contributes to epileptic activities around human glioma. Sci. Transl. Med. 6, 244ra89 (2014).
Liu, R., Wang, J., Liang, S., Zhang, G. & Yang, X. Role of NKCC1 and KCC2 in epilepsy: from expression to function. Front. Neurol. 10, 1407 (2020).
Haider, B., Duque, A., Hasenstaub, A. R. & McCormick, D. A. Neocortical network activity in vivo is generated through a dynamic balance of excitation and inhibition. J. Neurosci. 26, 4535–4545 (2006).
Trevelyan, A. J., Sussillo, D., Watson, B. O. & Yuste, R. Modular propagation of epileptiform activity: evidence for an inhibitory veto in neocortex. J. Neurosci. 26, 12447–12455 (2006).
Kaila, K., Saarikoski, J. & Vopio, J. Mechanism of action of GABA on intracellular pH and on surface pH in crayfish muscle fibres. J. Physiol. 427, 241–260 (1990).
Staley, K., Soldo, B. & Proctor, W. Ionic mechanisms of neuronal excitation by inhibitory GABAA receptors. Science 269, 977–981 (1995).
Staley, K. J. & Proctor, W. R. Modulation of mammalian dendritic GABAA receptor function by the kinetics of Cl- and HCO3− transport. J. Physiol. 519, 693–712 (1999).
Lillis, K. P., Karmer, M. A., Mertz, J., Staley, K. J. & White, J. A. Pyramidal cells accumulate chloride at seizure onset. Neurobiol. Dis. 47, 358–366 (2012).
Raimondo, J. V., Markram, H. & Akerman, C. J. Short-term ionic plasticity at GABAergic synapses. Front. Synaptic Neurosci. 4, 5 (2012).
Gulledge, A. T. & Stuart, G. J. Excitatory actions of GABA in the cortex. Neuron 37, 299–309 (2003).
Lombardi, A., Luhmann, H. J. & Kilb, W. Modelling the spatial and temporal constrains of the GABAergic influence on neuronal excitability. bioRxiv https://doi.org/10.1101/2021.06.22.449394 (2021).
Kaila, K., Lamsa, K., Smirnov, S., Taira, T. & Voipio, J. Long-lasting GABA-mediated depolarization evoked by high-frequency stimulation in pyramidal neurons of rat hippocampal slice is attributable to a network-driven, bicarbonate-dependent K+ transient. J. Neurosci. 17, 7662–7672 (1997).
Viitanen, T., Ruusuvuori, E., Kaila, K. & Voipio, J. The K+-Cl− cotransporter KCC2 promotes GABAergic excitation in the mature rat hippocampus: GABA excitation and KCC2. J. Physiol. 588, 1527–1540 (2010).
Ellender, T. J., Raimondo, J. V., Irkle, A., Lamsa, K. P. & Akerman, C. J. Excitatory effects of parvalbumin-expressing interneurons maintain hippocampal epileptiform activity via synchronous afterdischarges. J. Neurosci. 34, 15208–15222 (2014).
Fujiwara-Tsukamoto, Y. et al. Prototypic seizure activity driven by mature hippocampal fast-spiking interneurons. J. Neurosci. 30, 13679–13689 (2010).
Ilie, A., Raimondo, J. V. & Akerman, C. J. Adenosine release during seizures attenuates GABAA receptor-mediated depolarization. J. Neurosci. 32, 5321–5332 (2012).
Sulis Sato, S. et al. Simultaneous two-photon imaging of intracellular chloride concentration and pH in mouse pyramidal neurons in vivo. Proc. Natl Acad. Sci. USA 114, 8770–8779 (2017).
Kapur, J. & Coulter, D. A. Experimental status epilepticus alters γ-aminobutyric acid Type A Receptor Function in CA1 pyramidal neurons. Ann. Neurol. 38, 893–900 (1995).
Naylor, D. E. Trafficking of GABAA receptors, loss of inhibition, and a mechanism for pharmacoresistance in status epilepticus. J. Neurosci. 25, 7724–7733 (2005).
Feng, H.-J., Mathews, G. C., Kao, C. & Macdonald, R. L. Alterations of GABAA-receptor function and allosteric modulation during development of status epilepticus. J. Neurophysiol. 99, 1285–1293 (2008).
Terunuma, M. et al. Deficits in Phosphorylation of GABAA receptors by intimately associated protein kinase c activity underlie compromised synaptic inhibition during status epilepticus. J. Neurosci. 28, 376–384 (2008).
Goodkin, H. P., Joshi, S., Mtchedlishvili, Z., Brar, J. & Kapur, J. Subunit-specific trafficking of GABAA receptors during status epilepticus. J. Neurosci. 28, 2527–2538 (2008).
Rice, A., Rafiq, A., Shapiro, S. M. & Delorenzo, R. J. Long-lasting reduction of inhibitory function and y-aminobutyric acid type A receptor subunit mRNA expression in a model of temporal lobe epilepsy. Proc. Natl Acad. Sci. USA 93, 9665–9669 (1996).
Goodkin, H. P. Status epilepticus increases the intracellular accumulation of GABAA receptors. J. Neurosci. 25, 5511–5520 (2005).
Hand, K. S. P. et al. Central benzodiazepine receptor autoradiography in hippocampal sclerosis. Br. J. Pharmacol. 122, 358–364 (1997).
Savic, I. et al. In-vivo demonstration of reduced benzodiazepine receptor binding in human epileptic foci. Lancet 332, 863–866 (1988).
Bouvard, S. et al. Seizure-related short-term plasticity of benzodiazepine receptors in partial epilepsy: a [11C]flumazenil−PET study. Brain 128, 1330–1343 (2005).
Ryvlin, P. et al. Clinical utility of flumazenil-PET versus [18F]fluorodeoxyglucose-PET and MRI in refractory partial epilepsy. A prospective study in 100 patients. Brain 121, 2067–2081 (1998).
Deeb, T. Z., Nakamura, Y., Frost, G. D., Davies, P. A. & Moss, S. J. Disrupted Cl− homeostasis contributes to reductions in the inhibitory efficacy of diazepam during hyperexcited states. Eur. J. Neurosci. 38, 2453–2467 (2013).
Sivakumaran, S. & Maguire, J. Bumetanide reduces seizure progression and the development of pharmacoresistant status epilepticus. Epilepsia 57, 222–232 (2016).
DeLorenzo, R. J., Pal, S. & Sombati, S. Prolonged activation of the N-methyl-D-aspartate receptor–Ca2+ transduction pathway causes spontaneous recurrent epileptiform discharges in hippocampal neurons in culture. Proc. Natl Acad. Sci. USA 95, 14482–14487 (1998).
Bannai, H. et al. Bidirectional control of synaptic GABAAR clustering by glutamate and calcium. Cell Rep. 13, 2768–2780 (2015).
Joshi, S. & Kapur, J. N-Methyl-D-aspartic acid receptor activation downregulates expression of δ subunit-containing GABAa receptors in cultured hippocampal neurons. Mol. Pharmacol. 84, 1–11 (2013).
Bannai, H. et al. Activity-dependent tuning of inhibitory neurotransmission based on GABAAR diffusion dynamics. Neuron 62, 670–682 (2009).
Eckel, R., Szulc, B., Walker, M. C. & Kittler, J. T. Activation of calcineurin underlies altered trafficking of α2 subunit containing GABAA receptors during prolonged epileptiform activity. Neuropharmacology 88, 82–90 (2015).
Rajasekaran, K., Todorovic, M. & Kapur, J. P. Calcium-permeable AMPA receptors are expressed in a rodent model of status epilepticus. Ann. Neurol. 72, 91–102 (2012).
Burman, R. J., Raimondo, J. V., Jefferys, J. G. R., Sen, A. & Akerman, C. J. The transition to status epilepticus: how the brain meets the demands of perpetual seizure activity. Seizure 75, 137–144 (2020).
Macdonald, R. L. & Barker, J. L. Different actions of anticonvulsant and anesthetic barbiturates revealed by use of cultured mammalian neurons. Science 200, 775–777 (1978).
Nardou, R. et al. Phenobarbital but not diazepam reduces AMPA/kainate receptor mediated currents and exerts opposite actions on initial seizures in the neonatal rat hippocampus. Front. Cell. Neurosci. 5, 16 (2011).
Yi-Ping Lee, Ko,G., Brown-Croyts, L. M. & Teyler, T. J. The effects of anticonvulsant drugs on NMDA-EPSP, AMPA-EPSP, and GABA-IPSP in the rat hippocampus. Brain Res. Bull. 42, 297–302 (1997).
Su, Y. et al. Phenobarbital versus valproate for generalized convulsive status epilepticus in adults: a prospective randomized controlled trial in China. CNS Drugs 30, 1201–1207 (2016).
Treiman, D. M. et al. Comparison of four treatments for generalized convulsive status epilepticus. N. Eng. J. Med. 339, 792–798 (1998).
Brodie, M. J. & Kwan, P. Current position of phenobarbital in epilepsy and its future. Epilepsia 53, 40–46 (2012).
Camfield, C. S. et al. Side effects of phenobarbital in toddlers; behavioral and cognitive aspects. J. Pediatr. 95, 361–365 (1979).
Farwell, J. R. et al. Phenobarbital for febrile seizures — effects on intelligence and on seizure recurrence. N. Eng. J. Med. 322, 364–369 (1990).
Hassan Tonekaboni, S., Beyraghi, N., Sahar Tahbaz, H., Abdolmajid Bahreynian, S. & Aghamohammadpoor, M. Neurocognitive effects of phenobarbital discontinuation in epileptic children. Epilepsy Behav. 8, 145–148 (2006).
Meador, K. J. et al. Comparative cognitive effects of phenobarbital, phenytoin, and valproate in healthy adults. Neurology 45, 1494–1499 (1995).
Riva, D. & Devoti, M. Discontinuation of phenobarbital in children: effects on neurocognitive behavior. Pediatr. Neurol. 14, 36–40 (1996).
Sulzbacher, S., Farwell, J. R., Temkin, N., Lu, A. S. & Hirtz, D. G. Late cognitive effects of early treatment with phenobarbital. Clin. Pediatr. 38, 387–394 (1999).
Ding, D. et al. Cognitive and mood effects of phenobarbital treatment in people with epilepsy in rural China: a prospective study. J. Neurol. Neurosurg. Psychiatry 83, 1139–1144 (2012).
Pal, D. K., Das, T., Chaudhury, G., Johnson, A. L. & Neville, B. G. Randomised controlled trial to assess acceptability of phenobarbital for childhood epilepsy in rural India. Lancet 351, 19–23 (1998).
Satischandra, P. et al. The effect of phenobarbitone on cognition in adult patients with new onset epilepsy: a multi-centric prospective study from India. Epilepsy Res. 108, 928–936 (2014).
Wang, W. et al. Efficacy assessment of phenobarbital in epilepsy: a large community-based intervention trial in rural China. Lancet Neurol. 5, 46–52 (2006).
Wolf, S. M., Forsythe, A., Stunden, A. A., Friedman, R. & Diamond, H. Long-term effect of phenobarbital on cognitive function in children with febrile convulsions. Pediatrics 68, 820–823 (1981).
Watkins, L. V., Cock, H. R., Angus-Leppan, H. & Shankar, R. Valproate and the Pregnancy Prevention Programme: exceptional circumstances. Br. J. Gen. Pract. 69, 166–167 (2019).
Bhalla, D. et al. Undue regulatory control on phenobarbital — an important yet overlooked reason for the epilepsy treatment gap. Epilepsia 56, 659–662 (2015).
Trinka, E., Brigo, F. & Shorvon, S. Recent advances in status epilepticus. Curr. Opin. Neurol. 29, 189–198 (2016).
Neligan, A., Rajakulendran, S. & Walker, M. C. Advances in the management of generalized convulsive status epilepticus: what have we learned? Brain 144, 1336–1341 (2021).
Amengual-Gual, M., Sánchez Fernández, I. & Wainwright, M. S. Novel drugs and early polypharmacotherapy in status epilepticus. Seizure 68, 79–88 (2019).
Leo, A., Giovannini, G., Russo, E. & Meletti, S. The role of AMPA receptors and their antagonists in status epilepticus. Epilepsia 59, 1098–1108 (2018).
Prisco, L. et al. A pragmatic approach to intravenous anaesthetics and electroencephalographic endpoints for the treatment of refractory and super-refractory status epilepticus in critical care. Seizure 75, 153–164 (2020).
Kapur, J. Role of NMDA receptors in the pathophysiology and treatment of status epilepticus. Epilepsia Open 3, 165–168 (2018).
Brigo, F. et al. Perampanel in the treatment of status epilepticus: A systematic review of the literature. Epilepsy Behav. 86, 179–186 (2018).
Rosati, A., De Masi, S. & Guerrini, R. Ketamine for refractory status epilepticus: a systematic review. CNS Drugs 32, 997–1009 (2018).
Vossler, D. G. et al. Treatment of refractory convulsive status epilepticus: a comprehensive review by the american epilepsy society treatments committee. Epilepsy Curr. 20, 245–264 (2020).
Yen, W., Williamson, J., Bertram, E. H. & Kapur, J. A comparison of three NMDA receptor antagonists in the treatment of prolonged status epilepticus. Epilepsy Res. 59, 43–50 (2004).
Zhang, T., Todorovic, M. S., Williamson, J. & Kapur, J. Flupirtine and diazepam combination terminates established status epilepticus: results in three rodent models. Ann. Clin. Transl. Neurol. 4, 888–896 (2017).
Ulvi, H., Yoldas, T., Müngen, B. & Yigiter, R. Continuous infusion of midazolam in the treatment of refractory generalized convulsive status epilepticus. Neurol. Sci. 23, 177–182 (2002).
Fernandez, A. et al. High-dose midazolam infusion for refractory status epilepticus. Neurology 82, 359–365 (2014).
Koul, R. L., Aithala, G. R., Chacko, A., Joshi, R. & Elbualy, M. S. Continuous midazolam infusion as treatment of status epilepticus. Arch. Dis. Child. 76, 445–448 (1997).
Eissa, T. L. et al. Cross-scale effects of neural interactions during human neocortical seizure activity. Proc. Natl Acad. Sci. USA 114, 10761–10766 (2017).
Liou, J. et al. A model for focal seizure onset, propagation, evolution, and progression. eLife 9, e50927 (2020).
Stell, B. M., Brickley, S. G., Tang, C. Y., Farrant, M. & Mody, I. Neuroactive steroids reduce neuronal excitability by selectively enhancing tonic inhibition mediated by δ subunit-containing GABAA receptors. Proc. Natl Acad. Sci. USA 100, 14439–14444 (2003).
Rogawski, M. A., Loya, C. M., Reddy, K., Zolkowska, D. & Lossin, C. Neuroactive steroids for the treatment of status epilepticus. Epilepsia 54, 93–98 (2013).
Vaitkevicius, H. et al. First-in-man allopregnanolone use in super-refractory status epilepticus. Ann. Clin. Trans. Neurol. 4, 411–414 (2017).
Rossetti, A. O. Place of neurosteroids in the treatment of status epilepticus. Epilepsia 59, 216–219 (2018).
Rosenthal, E. S. et al. Brexanolone as adjunctive therapy in super-refractory status epilepticus. Ann. Neurol. 82, 342–352 (2017).
Prasad, M., Krishnan, P. R., Sequeira, R. & Al-Roomi, K. Anticonvulsant therapy for status epilepticus. Cochrane Database Sys. Rev. 9, CD003723 (2014).
Das, K. et al. Clinical feature and outcome of childhood status epilepticus in a teaching hospital, Odisha, India. Cureus 12, e10927 (2020).
Hassan, H. et al. An audit of the predictors of outcome in status epilepticus from a resource-poor country: a comparison with developed countries. Epileptic Disord. 18, 163–172 (2016).
Thakker, A. & Shanbag, P. A randomized controlled trial of intranasal−midazolam versus intravenous-diazepam for acute childhood seizures. J. Neurol. 260, 470–474 (2013).
Misra, U. K., Kalita, J. & Maurya, P. K. Levetiracetam versus lorazepam in status epilepticus: a randomized, open labeled pilot study. J. Neurol. 259, 645–648 (2012).
Gathwala, G., Goel, M., Singh, J. & Mittal, K. Intravenous diazepam, midazolam and lorazepam in acute seizure control. Ind. J. Pediatr. 79, 327–332 (2012).
Arya, R., Gulati, S., Kabra, M., Sahu, J. K. & Kalra, V. Intranasal versus intravenous lorazepam for control of acute seizures in children: A randomized open-label study. Epilepsia 52, 788–793 (2011).
Chen, W. B. et al. Valproate versus diazepam for generalized convulsive status epilepticus: a pilot study. Eur. J. Neurol. 18, 1391–1396 (2011).
Skinner, H. J. et al. Adult convulsive status epilepticus in the developing country of Honduras. Seizure 19, 363–367 (2010).
Amare, A., Zenebe, G., Hammack, J. & Davey, G. Status epilepticus: Clinical presentation, cause, outcome, and predictors of death in 119 Ethiopian patients. Epilepsia 49, 600–607 (2008).
Mpimbaza, A., Ndeezi, G., Staedke, S., Rosenthal, P. J. & Byarugaba, J. Comparison of buccal midazolam with rectal diazepam in the treatment of prolonged seizures in ugandan children: a randomized clinical trial. Pediatrics 121, 58–64 (2008).
Ahmad, S., Ellis, J. C., Kamwendo, H. & Molyneux, E. Efficacy and safety of intranasal lorazepam versus intramuscular paraldehyde for protracted convulsions in children: an open randomised trial. Lancet 367, 1591–1597 (2006).
Fişgin, T. et al. Effects of intranasal midazolam and rectal diazepam on acute convulsions in children: prospective randomized study. J. Child. Neurol. 17, 123–126 (2002).
Tabarki, B. et al. Infantile status epilepticus in Tunisia. Clinical, etiological and prognostic aspects. Seizure 10, 365–369 (2001).
Theusinger, O. M., Schenk, P., Dette-Oltmann, K., Mariotti, S. & Baulig, W. Treatment of seizures in children and adults in the emergency medical system of the city of Zurich, Switzerland — midazolam vs. diazepam — a retrospective analysis. J. Emerg. Med. 57, 345–353 (2019).
Kay, L. et al. Intranasal midazolam as first-line inhospital treatment for status epilepticus: a pharmaco-EEG cohort study. Ann. Clin. Transl. Neurol. 6, 2413–2425 (2019).
Navarro, V. et al. Prehospital treatment with levetiracetam plus clonazepam or placebo plus clonazepam in status epilepticus (SAMUKeppra): a randomised, double-blind, phase 3 trial. Lancet Neurol. 15, 47–55 (2016).
Chamberlain, J. M. et al. Lorazepam vs diazepam for pediatric status epilepticus: a randomized clinical trial. JAMA 311, 1652–1660 (2014).
Chin, R. F. et al. Treatment of community-onset, childhood convulsive status epilepticus: a prospective, population-based study. Lancet Neurol. 7, 696–703 (2008).
McIntyre, J. et al. Safety and efficacy of buccal midazolam versus rectal diazepam for emergency treatment of seizures in children: a randomised controlled trial. Lancet 366, 205–210 (2005).
Qureshi, A., Wassmer, E., Davies, P., Berry, K. & Whitehouse, W. P. Comparative audit of intravenous lorazepam and diazepam in the emergency treatment of convulsive status epilepticus in children. Seizure 11, 141–144 (2002).
Mayer, S. A. et al. Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch. Neurol. 59, 205 (2002).
Lahat, E., Goldman, M., Barr, J., Bistritzer, T. & Berkovitch, M. Comparison of intranasal midazolam with intravenous diazepam for treating febrile seizures in children: prospective randomised study. BMJ 321, 83–86 (2000).
Coeytaux, A., Jallon, P., Galobardes, B. & Morabia, A. Incidence of status epilepticus in French-speaking Switzerland: (EPISTAR). Neurology 55, 693–697 (2000).
Scott, R. C., Besag, F. M. & Neville, B. G. Buccal midazolam and rectal diazepam for treatment of prolonged seizures in childhood and adolescence: a randomised trial. Lancet 353, 623–626 (1999).
Chamberlain, J. M. et al. A prospective, randomized study comparing intramuscular midazolam with intravenous diazepam for the treatment of seizures in children. Pediatr. Emerg. Care 13, 92–94 (1997).
Appletan, R., Sweeney, A., Choonara, I., Robson, J. & Molyneux, E. Lorazepam versus diazepam in the acute treatment of epileptic seizures and status epilepticus. Dev. Med. Child. Neurol. 37, 682–688 (1995).
Remy, C., Jourdil, N., Villemain, D., Favel, P. & Genton, P. Intrarectal diazepam in epileptic adults. Epilepsia 33, 353–358 (1992).
The World Bank. World Bank Country and Lending Groups https://datahelpdesk.worldbank.org/knowledgebase/articles/378832-what-is-the-world-bank-atlas-method (2020).
Bowser, D. N. et al. Altered kinetics and benzodiazepine sensitivity of a GABAA receptor subunit mutation (γ2(R43Q)] found in human epilepsy. Proc. Natl Acad. Sci. USA 99, 15170–15175 (2002).
Lorenz-Guertin, J. M., Bambino, M. J. & Jacob, T. C. γ2 GABAAR trafficking and the consequences of human genetic variation. Front. Cell Neurosci. 12, 265 (2018).
Macdonald, R. L., Kang, J.-Q. & Gallagher, M. J. in Jasper’s Basic Mechanisms of the Epilepsies (eds Noebels, J. L., Avoli, M., Rogawski, M. A., Olsen, R. W. & Delgado-Escueta, A. V.) (National Center for Biotechnology Information, 2012).
Macdonald, R. L., Bianch, M. T. & Feng, H. Mutations linked to generalized epilepsy in humans reduce GABAA receptor current. Exp. Neurol. 184, 58–67 (2003).
Rosenberg, H. C., Tietz, E. I. & Chiu, T. H. Tolerance to the anticonvulsant action of benzodiazepines. Relationship to decreased receptor density. Neuropharmacology 24, 639–644 (1985).
Avanzini, G. Is tolerance to antiepileptic drugs clinically relevant? Epilepsia 47, 1285–1287 (2006).
Löscher, W. & Schmidt, D. Experimental and clinical evidence for loss of effect (tolerance) during prolonged treatment with antiepileptic drugs. Epilepsia 47, 1253–1284 (2006).
Levy, R. H. Cytochrome P450 isoenzymes and antiepileptic drug interactions. Epilepsia 36, 8–13 (1995).
Verrotti, A., Lattanzi, S., Brigo, F. & Zaccara, G. Pharmacodynamic interactions of antiepileptic drugs: from bench to clinical practice. Epilepsy Behav. 104, 106939 (2020).
Patsalos, P. N. & Perucca, E. Clinically important drug interactions in epilepsy: general features and interactions between antiepileptic drugs. Lancet Neurol. 2, 347–356 (2003).
Griffin, C. E., Kaye, A. M., Bueno, F. R. & Kaye, A. D. Benzodiazepine pharmacology and central nervous system–mediated effects. Ochsner J. 13, 214–223 (2013).
Löscher, W., Rundfeldt, C., Hönack, D. & Ebert, U. Long-term studies on anticonvulsant tolerance and withdrawal characteristics of benzodiazepine receptor ligands in different seizure models in mice. I. Comparison of diazepam, clonazepam, clobazam and abecarnil. J. Pharmacol. Exp. Ther. 279, 561–572 (1996).
Douglas Knowles, W., Traub, R. D., Wong, R. K. S. & Miles, R. Properties of neural networks: experimentation and modelling of the epileptic hippocampal slice. Trends Neurosci. 8, 73–79 (1985).
Riss, J., Cloyd, J., Gates, J. & Collins, S. Benzodiazepines in epilepsy: pharmacology and pharmacokinetics. Acta Neurol. Scand. 118, 69–86 (2008).
File, S. E. Tolerance to the behavioral actions of benzodiazepines. Neurosci. Biobehav. Rev. 9, 113–121 (1985).
File, S. E. The history of benzodiazepine dependence: a review of animal studies. Neuro. Biobehav. Rev. 14, 135–146 (1990).
Bateson, A. N. Basic pharmacologic mechanisms involved in benzodiazepine tolerance and withdrawal. Curr. Pharm. Des. 8, 5–21 (2001).
Vinkers, C. H. & Olivier, B. Mechanisms underlying tolerance after long-term benzodiazepine use: a future for subtype-selective gabaa receptor modulators? Adv. Pharmacol. Sci. 2012, 416864 (2012).
Uusi-Oukari, M. & Korpi, E. R. Regulation of GABAA receptor subunit expression by pharmacological agents. Pharmacol. Rev. 62, 97–135 (2010).
Allison, C. & Pratt, J. A. Neuroadaptive processes in GABAergic and glutamatergic systems in benzodiazepine dependence. Pharmacol. Ther. 98, 171–195 (2003).
Feng, J., Cai, X., Zhao, J. & Yan, Z. Serotonin receptors modulate GABAA receptor channels through activation of anchored protein kinase C in prefrontal cortical neurons. J. Neurosci. 21, 6502–6511 (2001).
Wang, X., Zhong, P. & Yan, Z. Dopamine D4 receptors modulate gabaergic signaling in pyramidal neurons of prefrontal cortex. J. Neurosci. 22, 9185–9193 (2002).
Brandon, N. J., Jovanovic, J. N., Smart, T. G. & Moss, S. J. Receptor for activated C kinase-1 facilitates protein kinase C-dependent phosphorylation and functional modulation of GABAA receptors with the activation of G-protein-coupled receptors. J. Neurosci. 22, 6353–6361 (2002).
Wilson, M. A. & Biscardi, R. Effects of gender and gonadectomy on responses to chronic benzodiazepine receptor agonist exposure in rats. Eur. J. Pharm. 215, 99–107 (1992).
Krishnan, G. P. & Bazhenov, M. Ionic dynamics mediate spontaneous termination of seizures and postictal depression state. J. Neurosci. 31, 8870–8882 (2011).
Löscher, W., Puskarjov, M. & Kaila, K. Cation-chloride cotransporters NKCC1 and KCC2 as potential targets for novel antiepileptic and antiepileptogenic treatments. Neuropharmacology 69, 62–74 (2013).
Moore, Y. E., Kelley, M. R., Brandon, N. J., Deeb, T. Z. & Moss, S. J. Seizing control of KCC2: a new therapeutic target for epilepsy. Trends Neurosci. 40, 555–571 (2017).
Magloire, V. et al. KCC2 overexpression prevents the paradoxical seizure-promoting action of somatic inhibition. Nat. Commun. 10, 1225–1237 (2019).
Moore, Y. E., Deeb, T. Z., Chadchankar, H., Brandon, N. J. & Moss, S. J. Potentiating KCC2 activity is sufficient to limit the onset and severity of seizures. Proc. Natl Acad. Sci. USA 115, 10166–10171 (2018).
Sutter, R., Semmlack, S. & Kaplan, P. W. Nonconvulsive status epilepticus in adults — insights into the invisible. Nat. Rev. Neurol. 12, 281–293 (2016).
Sutter, R., Ruegg, S. & Kaplan, P. W. Epidemiology, diagnosis, and management of nonconvulsive status epilepticus: opening Pandora’s box. Neurology 2, 275–286 (2012).
De Negri, M. et al. Treatment of electrical status epilepticus by short diazepam (DZP) cycles after DZP rectal bolus test. Brain Dev. 17, 330–333 (1995).
Hopp, J. L., Sanchez, A., Krumholz, A., Hart, G. & Barry, E. Nonconvulsive status epilepticus: value of a benzodiazepine trial for predicting outcomes. Neurologist 17, 325–329 (2011).
Power, K. N., Gramstad, A., Gilhus, N. E. & Engelsen, B. A. Adult nonconvulsive status epilepticus in a clinical setting: Semiology, aetiology, treatment and outcome. Seizure 24, 102–106 (2015).
Ben-Ari, Y., Gaiarsa, J.-L., Tyzio, R. & Khazipov, R. GABA: a pioneer transmitter that excites immature neurons and generates primitive oscillations. Physiol. Rev. 87, 1215–1284 (2007).
Kahle, K. T. et al. Roles of the cation–chloride cotransporters in neurological disease. Nat. Rev. Neurol. 4, 490–503 (2008).
Akerman, C. J. & Cline, H. T. Depolarizing GABAergic conductances regulate the balance of excitation to inhibition in the developing retinotectal circuit in vivo. J. Neurosci. 26, 5117–5130 (2006).
Leinekugel, X., Medina, I., Khalilov, I., Ben-Ari, Y. & Khazipov, R. Ca2+ oscillations mediated by the synergistic excitatory actions of GABAA and NMDA receptors in the neonatal hippocampus. Neuron 18, 243–255 (1997).
Pfeffer, C. K. et al. NKCC1-Dependent GABAergic excitation drives synaptic network maturation during early hippocampal development. J. Neurosci. 29, 3419–3430 (2009).
Wang, D. D. & Kriegstein, A. R. GABA regulates excitatory synapse formation in the neocortex via NMDA receptor activation. J. Neurosci. 28, 5547–5558 (2008).
Peerboom, C. & Wierenga, C. J. The postnatal GABA shift: a developmental perspective. Neuro. Biobehav. Rev. 124, 179–192 (2021).
Tyzio, R. et al. The establishment of GABAergic and glutamatergic synapses on CA1 pyramidal neurons is sequential and correlates with the development of the apical dendrite. J. Neurosci. 19, 10372–10382 (1999).
Wang, D. D. & Kriegstein, A. R. Defining the role of GABA in cortical development. J. Physiol. 587, 1873–1879 (2009).
Wu, G.-Y., Malinow, R. & Cline, H. T. Maturation of a Central Glutamatergic Synapse. Science 274, 972–976 (1996).
Dzhala, V. I. et al. NKCC1 transporter facilitates seizures in the developing brain. Nat. Med. 11, 1205–1213 (2005).
Ramantani, G. et al. Neonatal Seizures — Are We there Yet? Neuropediatrics 50, 280–293 (2019).
Boylan, G. B. et al. Phenobarbitone, neonatal seizures, and video-EEG. Arch. Dis. Child. Fetal Neonatal Ed. 86, 165–170 (2002).
Boylan, G. B. et al. Outcome of electroclinical, electrographic, and clinical seizures in the newborn infant. Dev. Med. Child. Neurol. 41, 819–825 (1999).
Connell, J., Oozeer, R., Vries, L., de, Dubowitz, L. M. & Dubowitz, V. Clinical and EEG response to anticonvulsants in neonatal seizures. Arch. Dis. Child. 64, 459–464 (1989).
Murray, D. M. et al. Defining the gap between electrographic seizure burden, clinical expression and staff recognition of neonatal seizures. Arch. Dis. Child. Fetal Neonatal Ed. 93, 187–191 (2008).
Rennie, J. M. & Boylan, G. B. Neonatal seizures and their treatment. Curr. Opin. Neurol. 16, 177–181 (2003).
Scher, M. S., Alvin, J., Gaus, L., Minnigh, B. & Painter, M. J. Uncoupling of EEG-clinical neonatal seizures after antiepileptic drug use. Pediatr. Neurol. 28, 277–280 (2003).
Weiner, S. P., Painter, M. J., Geva, D., Guthrie, R. D. & Scher, M. S. Neonatal seizures: electroclinical dissociation. Pediatr. Neurol. 7, 363–368 (1991).
Glykys, J. et al. Differences in cortical versus subcortical GABAergic signaling: a candidate mechanism of electroclinical uncoupling of neonatal seizures. Neuron 63, 657–672 (2009).
Kharod, S. C., Carter, B. M. & Kadam, S. D. Pharmaco-resistant neonatal seizures: critical mechanistic insights from a chemoconvulsant model. Dev. Neurobiol. 11, 1117–1130 (2018).
Dzhala, V. I. et al. Progressive NKCC1-dependent neuronal chloride accumulation during neonatal seizures. J. Neurosci. 30, 11745–11761 (2010).
Glykys, J. & Staley, K. J. Diazepam effect during early neonatal development correlates with neuronal Cl−. Ann. Clin. Transl. Neurol. 2, 1055–1070 (2015).
Johne, M. et al. A combination of phenobarbital and the bumetanide derivative bumepamine prevents neonatal seizures and subsequent hippocampal neurodegeneration in a rat model of birth asphyxia. Epilepsia 62, 1460–1471 (2021).
Lawrence, R. & Inder, T. Neonatal status epilepticus. Sem. Pediatr. Neurol. 17, 163–168 (2010).
Pressler, R. M. et al. Bumetanide for the treatment of seizures in newborn babies with hypoxic ischaemic encephalopathy (NEMO): an open-label, dose finding, and feasibility phase 1/2 trial. Lancet Neurol. 14, 469–477 (2015).
Soul, J. S. et al. A pilot randomized, controlled, double-blind trial of bumetanide to treat neonatal seizures. Ann. Neurol. 89, 327–340 (2021).
Stafstrom, C. E. Mechanism-based treatment for neonatal seizures: still on the horizon. Epilepsy Curr. 20, 53S–55S (2020).
Kang, S. K., Markowitz, G. H., Kim, S. T., Johnston, M. V. & Kadam, S. D. Age-and sex-dependent susceptibility to phenobarbital-resistant neonatal seizures: role of chloride co-transporters. Front. Cell. Neurosci. 9, 173 (2015).
Acknowledgements
The authors thank A. J. Trevelyan (Institute of Neurosciences, Newcastle, UK) for his helpful comments on this manuscript. R.J.B. is supported by a Shaun Johnson Memorial Scholarship through the Leverhulme Trust. R.J.B., R.E.R. and G.R. are supported by project grants from the Theodor and Ida Herzog-Egli Foundation and the Anna Mueller Grocholski Foundation. R.E.R. is supported by a Sir Henry Wellcome Fellowship (209164/Z/17/Z). A.S. is supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC). C.J.A. received funding from the European Research Council under the European Community’s Seventh Framework Programme FP7/2007-2013, ERC Grant Agreement 617670. J.V.R. is supported by the National Research Foundation of South Africa, a Wellcome Trust Seed Award (214042/Z/18/Z), the South African Medical Research Council and by the FLAIR Fellowship Programme (FLR\R1\190829): a partnership between the African Academy of Sciences and the Royal Society funded by the UK Government’s Global Challenges Research Fund.
Author information
Authors and Affiliations
Contributions
R.J.B and J.V.R. researched data for the article, made a substantial contribution to discussion of content, wrote the article, and reviewed and edited the manuscript before submission. All other authors made a substantial contribution to discussion of content, wrote the article, and reviewed and edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
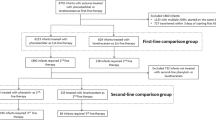
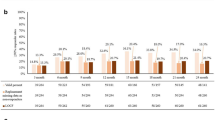
Review criteria
The studies mentioned in Table 1 were found using medical search headings (MeSH) on the PubMed and Embase database search platforms. We searched within the main heading of ‘convulsive status epilepticus’ and included ‘drug therapy’ and ‘prevention and control’ as subheadings. We added ‘benzodiazepines’ with the subheadings ‘administration and dosage’ and ‘therapeutic use’ to our search requirements. We limited our search to studies published from 1 January 1990 to 1 July 2021 and to peer-reviewed studies that were published in English and had the full text available. Studies were included if they were performed in patients, both adult and/or paediatric, presenting in convulsive status epilepticus and where monotherapy with a benzodiazepine (consisting of one or two doses), of any kind or formulation, was assessed in terms of its efficacy in terminating status epilepticus. In addition to this search, we also assessed the studies mentioned in two systematic reviews7,188 and added additional studies that met our inclusion criteria.
Supplementary information
Glossary
- Co-transporters
-
Transmembrane proteins that allow the coupled, simultaneous transport of multiple substances across the membrane.
- Equilibrium potential
-
The electrical potential difference at which the flow of ions down their transmembrane concentration gradient is exactly balanced by the opposing potential difference across the membrane; at the equilibrium potential there is no net flux of ions.
- Ionotropic receptor
-
A ligand-gated ion channel in which ligand binding results in transmembrane ion flux through the receptor’s pore.
- Phasic inhibition
-
The fast activation of synaptic GABAA receptors following pre-synaptic release of GABA.
- Resting membrane potential
-
The electrical potential difference across the cell membrane at rest (that is, when the cell is not receiving synaptic input or engaged in action potential firing).
- Secondary active transport
-
The transport of chemical substances across a membrane (also known as co-transport), where the energy to move one substance against its concentration gradient is provided by the movement of another substance down its concentration gradient.
- Shunting
-
A type of inhibition whereby activated GABAA receptors lower the local membrane resistance, which reduces (or ‘shunts’) the impact of concurrent excitatory synaptic inputs.
- Tonic inhibition
-
The continuous activation of perisynaptic and extrasynaptic GABAA receptors owing to the presence of ambient GABA in the extracellular space, or spontaneous GABAA receptor openings.
Rights and permissions
About this article
Cite this article
Burman, R.J., Rosch, R.E., Wilmshurst, J.M. et al. Why won’t it stop? The dynamics of benzodiazepine resistance in status epilepticus. Nat Rev Neurol 18, 428–441 (2022). https://doi.org/10.1038/s41582-022-00664-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-022-00664-3
This article is cited by
-
Multistate structures in a hydrogen-bonded polycatenation non-covalent organic framework with diverse resistive switching behaviors
Nature Communications (2024)
-
Benzodiazepines for the Treatment of Seizure Clusters
CNS Drugs (2024)
-
Rapid Rescue Treatment with Diazepam Nasal Spray Leads to Faster Seizure Cluster Termination in Epilepsy: An Exploratory Post Hoc Cohort Analysis
Neurology and Therapy (2024)
-
Autophagy and autophagy signaling in Epilepsy: possible role of autophagy activator
Molecular Medicine (2023)
-
Status epilepticus – Detektion und Behandlung auf der Intensivstation
Der Nervenarzt (2023)