Abstract
The identification and treatment of patients with stroke is becoming increasingly complex as more treatment options become available and new relationships between disease features and treatment response are continually discovered. Consequently, clinicians must constantly learn new skills (such as clinical evaluations or image interpretation), stay up to date with the literature and incorporate advances into everyday practice. The use of artificial intelligence (AI) to support clinical decision making could reduce inter-rater variation in routine clinical practice and facilitate the extraction of vital information that could improve identification of patients with stroke, prediction of treatment responses and patient outcomes. Such support systems would be ideal for centres that deal with few patients with stroke or for regional hubs, and could assist informed discussions with the patients and their families. Moreover, the use of AI for image processing and interpretation in stroke could provide any clinician with an imaging assessment equivalent to that of an expert. However, any AI-based decision support system should allow for expert clinician interaction to enable identification of errors (for example, in automated image processing). In this Review, we discuss the increasing importance of imaging in stroke management before exploring the potential and pitfalls of AI-assisted treatment decision support in acute stroke.
Key points
-
Imaging-based treatment guidance has been demonstrated as an effective approach in patients with a suspected stroke.
-
Clinical trials in which imaging is not used for patient selection are likely to include many patients with minor stroke or stroke mimics, making treatment effects difficult to detect.
-
Artificial intelligence (AI) and machine learning could provide image interpretation that equals or exceeds that of experts and could collate key features to assist clinicians with treatment decisions.
-
AI could be used to generate estimations of likely patient outcomes, which would not only be useful for assisting treatment decisions but also for informing family discussions.
-
AI-based decision assistance systems could be especially useful for centres without dedicated stroke specialists.
-
Any decision assistance tools must be validated and applied appropriately, and clear guidelines are needed to define how useful systems are in clinical practice.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Goyal, M. et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387, 1723–1731 (2016). An excellent meta-analysis of thrombectomy trials that demonstrates a very large treatment effect.
Potter, C. A. et al. CT for treatment selection in acute ischemic stroke: a code stroke primer. Radiographics 39, 6 (2019).
Sanelli, P. C. et al. Imaging and treatment of patients with acute stroke: an evidence-based review. Am. J. Neuroradiol. 35, 1045–1051 (2014).
Bacharach, R., Niazi, M. & Ermak, D. Pitfalls of CT perfusion imaging in acute ischemic stroke: a case series. Neurology 90 (Suppl. 15), P3.206 (2018).
Adeoye, O. et al. Recommendations for the establishment of stroke systems of care: a 2019 update. A policy statement from the American Stroke Association. Stroke 50, e187–e210 (2019).
Heit, J. & Wintermark, M. Perfusion computed tomography for the evaluation of acute ischemic stroke: strengths and pitfalls. Stroke 47, 1153–1158 (2016).
Gao, J. et al. Visibility of CT early ischemic change is significantly associated with time from stroke onset to baseline scan beyond the first 3 hours of stroke onset. J. Stroke 19, 340–346 (2017).
Fiebach, J. B. et al. CT and diffusion-weighted MR imaging in randomized order: diffusion-weighted imaging results in higher accuracy and lower interrater variability in the diagnosis of hyperacute ischemic stroke. Stroke 33, 2206–2210 (2002).
Logallo, N. et al. Tenecteplase versus alteplase for management of acute ischaemic stroke (NOR-TEST): a phase 3, randomised, open-label, blinded endpoint trial. Lancet Neurol. 16, 781–788 (2017).
IST-3 collaborative group. et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet 379, 2352–2363 (2012).
Bivard, A. et al. Too good to treat? Ischemic stroke patients with small computed tomography perfusion lesions may not benefit from thrombolysis. Ann. Neurol. 80, 286–293 (2016). A controversial article in which the benefit of thrombolysis for patients with a perfusion lesion <15 ml is questioned.
Nogueira, R. G. et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N. Engl. J. Med. 378, 11–21 (2018).
Albers, G. et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N. Engl. J. Med. 378, 11–21 (2018).
Thomalla, G. et al. MRI-guided thrombolysis for stroke with unknown time of onset. N. Engl. J. Med. 379, 611–622 (2018). Together with Albers et al. (2018), these papers represent medical breakthroughs as they show that the treatment time window for stroke caused by large-vessel occlusion can be extended from 6 h to 24 h with the aid of imaging-based patient selection.
Ma, H. Extending thrombolysis to 9 hours and wake-up stroke using perfusion imaging selection. N. Engl. J. Med. 380, 1795–1803 (2019). A clinical trial of thrombolysis that shows that the treatment time window can be extended to 9 h or that the treatment can be used for patients with an unknown time of onset but have an imaging treatment target seen on CT perfusion.
Mokin, M. et al. Predictive value of RAPID assessed perfusion thresholds on final infarct volume in SWIFT PRIME (Solitaire with the intention for thrombectomy as primary endovascular treatment). Stroke 48, 932–938 (2017).
Hoving, J. W. et al. Volumetric and spatial accuracy of computed tomography perfusion estimated ischemic core volume in patients with acute ischemic stroke. Stroke 49, 2368–2375 (2018).
Campbell, B. C. et al. Cerebral blood flow is the optimal CT perfusion parameter for assessing infarct core. Stroke 42, 3435–3440 (2011).
Huang, X. et al. Alteplase versus tenecteplase for thrombolysis after ischaemic stroke (ATTEST): a phase 2, randomised, open-label, blinded endpoint study. Lancet Neurol. 14, 368–376 (2015).
Parsons, M. et al. A randomized trial of tenecteplase versus alteplase for acute ischemic stroke. N. Engl. J. Med. 366, 1099–1107 (2012).
Bivard, A. et al. Impact of computed tomography perfusion imaging on the response to tenecteplase in ischemic stroke: analysis of 2 randomized controlled trials. Circulation 135, 440–448 (2017).
Takahashi, N. et al. An automated detection method for the MCA dot sign of acute stroke in unenhanced CT. Radiol. Phys. Technol. 7, 79–88 (2014).
Bivard, A. et al. Perfusion computed tomography to assist decision making for stroke thrombolysis. Brain 138, 1919–1931 (2015).
Hussein, H. M., Saleem, M. A. & Qureshi, A. I. Rates and predictors of futile recanalization in patients undergoing endovascular treatment in a multicenter clinical trial. Neuroradiology 60, 557–563 (2018).
Russell, S. J. & Norvig, P. Artificial Intelligence: a Modern Approach 3rd edn (Prentice Hall, 2009).
SAS. Machine learning: what it is and why it matters. https://www.sas.com/en_au/insights/analytics/machine-learning.html (2020).
Domingos, P. A few useful things to know about machine learning. Commun. ACM. 55, 78–87 (2012).
Brzdok, D., Krzywinski, M. & Altman, N. Machine learning: a primer. Nat. Methods. 14, 1119–1120 (2017).
von Kummer, R. Ischemic stroke and tissue hypodensity on computed tomography. Stroke 30, 1974 (1999).
Chen, Y. et al. Automated quantification of cerebral edema following hemispheric infarction: application of a machine-learning algorithm to evaluate CSF shifts on serial head CTs. Neuroimage Clin. 12, 673–680 (2016).
Chen, L., Bentley, P. & Rueckert, D. Fully automatic acute ischemic lesion segmentation in DWI using convolutional neural networks. Neuroimage Clin. 15, 633–643 (2017).
Meretoja, A., Keshtkaran, M., Tatlisumak, T., Donnan, G. A. & Churilov, L. Endovascular therapy for ischemic stroke: save a minute–save a week. Neurology 88, 2123–2127 (2017).
Meretoja, A. et al. Stroke thrombolysis: save a minute, save a day. Stroke 45, 1053–1058 (2014).
Pidd, M. Why modelling and model use matter. J. Oper. Res. Soc. 61, 14–24 (2010).
Tan, J. C. et al. Systematic comparison of perfusion CT and CT-angiography in acute stroke patients. Ann. Neurol. 61, 533–543 (2007).
Maier, O., Schröder, C., Forkert, N. D., Martinetz, T. & Handels, H. Classifiers for ischemic stroke lesion segmentation: a comparison study. PLoS ONE 10, e0145118 (2015).
Wilke, M., de Haan, B., Juenger, H. & Karnath, H. O. Manual, semi-automated, and automated delineation of chronic brain lesions: a comparison of methods. Neuroimage 56, 2038–2046 (2011).
Barber, P. A., Demchuk, A. M., Zhang, J. & Buchan, A. M. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS study group. Alberta stroke programme early CT score. Lancet 355, 1670–1674 (2000).
Kobkitsuksakul, C., Tritanon, O. & Suraratdecha, V. Interobserver agreement between senior radiology resident, neuroradiology fellow, and experienced neuroradiologist in the rating of Alberta stroke program early computed tomography score (ASPECTS). Diagn. Interv. Radiol. 24, 104–107 (2018).
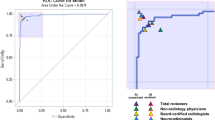
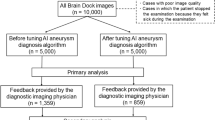
Nagel, S. et al. e-ASPECTS software is non-inferior to neuroradiologists in applying the ASPECT score to computed tomography scans of acute ischemic stroke patients. Int. J. Stroke 12, 615–622 (2017).
Austein, F. et al. Automated versus manual imaging assessment of early ischemic changes in acute stroke: comparison of two software packages and expert consensus. Eur. Radiol. 29, 6285–6292 (2019).
Castle, J. et al. Agreement regarding diagnosis of transient ischemic attack fairly low among stroke-trained neurologists. Stroke 41, 1367–1370 (2010).
Bivard, A. et al. Ischemic core thresholds change with time to reperfusion: a case control study. Ann. Neurol. 82, 995–1003 (2017).
Sillanpaa, N. et al. The clot burden score, the Boston acute stroke imaging scale, the cerebral blood volume ASPECTS, and two novel imaging parameters in the prediction of clinical outcome of ischemic stroke patients receiving intravenous thrombolytic therapy. Neuroradiology 54, 663–672 (2012).
Bivard, A. et al. Validating a predictive model of acute advanced imaging biomarkers in ischemic stroke. Stroke 48, 645–650 (2017).
Kawano, H. et al. Perfusion CT in stroke thrombolysis patients: save a ml of penumbra, save a week of disability-free life. Brain 140, 684–691 (2017).
Liebeskind, D. Artificial intelligence in stroke care: deep learning or superficial insight? EBioMedicine 35, 14–15 (2018).
Campbell, B. C. et al. Advanced imaging improves prediction of hemorrhage after stroke thrombolysis. Ann. Neurol. 73, 510–519 (2013).
van Os, H. J. A. et al. Predicting outcome of endovascular treatment for acute ischemic stroke: potential value of machine learning algorithms. Front. Neurol. 9, 784 (2018).
Bivard, A. et al. Global white matter hypoperfusion on CT predicts larger infarcts and hemorrhagic transformation after acute ischemia. CNS Neurosci. Ther. 22, 238–243 (2016).
Campbell, B. C. et al. Regional very low cerebral blood volume predicts hemorrhagic transformation better than diffusion-weighted imaging volume and thresholded apparent diffusion coefficient in acute ischemic stroke. Stroke 41, 82–88 (2010).
Yassi, N. et al. Prediction of poststroke hemorrhagic transformation using computed tomography perfusion. Stroke 44, 3039–3043 (2013).
Bentley, P. et al. Prediction of stroke thrombolysis outcome using CT brain machine learning. Neuroimage Clin. 4, 635–640 (2014).
FDA. FDA permits marketing of clinical decision support software for alerting providers of a potential stroke in patients. FDA.gov https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm596575.htm (2018).
Wang, X. et al. ChestX-ray8: hospital-scale chest X-ray database and benchmarks on weakly-supervised classification and localization of common thorax diseases. IEEE CVPR https://doi.org/10.1109/CVPR.2017.369 (2017).
Titano, J. J. et al. Automated deep-neural-network surveillance of cranial images for acute neurologic events. Nat. Med. 24, 1337–1341 (2018).
Lobo, J. M., Jiménez-Valverde, A. & Real, R. AUC: a misleading measure of the performance of predictive distribution models. Glob. Ecol. Biogeogr. 17, 145–151 (2008). An important analytical piece that shows how to interpret statistical results.
Saito, T. & Rehmsmeier, M. The precision–recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE 10, e0118432 (2015).
Author information
Authors and Affiliations
Contributions
All authors contributed to all aspects of the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.P. and A.B. have active research collaborations with Siemens Healthineers, Canon medical Systems and Apollo Medical Imaging. L.C. declares no competing interests.
Additional information
Peer review information
Nature Reviews Neurology thanks the anonymous reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bivard, A., Churilov, L. & Parsons, M. Artificial intelligence for decision support in acute stroke — current roles and potential. Nat Rev Neurol 16, 575–585 (2020). https://doi.org/10.1038/s41582-020-0390-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-020-0390-y
This article is cited by
-
Application and risk prediction of thrombolytic therapy in cardio-cerebrovascular diseases: a review
Thrombosis Journal (2023)
-
Neurology beyond big data — the ninth Congress of the EAN
Nature Reviews Neurology (2023)
-
Strokecopilot: a literature-based clinical decision support system for acute ischemic stroke treatment
Journal of Neurology (2023)
-
Intelligent, mobile stroke imaging
Nature Reviews Neurology (2022)
-
Development and implementation of new diagnostic technologies in neurology
Nature Reviews Neurology (2022)