Abstract
Spinal cord injury (SCI) remains one of the biggest challenges in the development of neuroregenerative therapeutics. Cell transplantation is one of numerous experimental strategies that have been identified and tested for efficacy at both preclinical and clinical levels in recent years. In this Review, we briefly discuss the state of human olfactory cell transplantation as a therapy, considering both its current clinical status and its limitations. Furthermore, we introduce a mesenchymal stromal cell derived from human olfactory tissue, which has the potential to induce multifaceted reparative effects in the environment within and surrounding the lesion. We argue that no single therapy will be sufficient to treat SCI effectively and that a combination of cell-based, rehabilitation and pharmaceutical interventions is the most promising approach to aid repair. For this reason, we also introduce a novel pharmaceutical strategy based on modifying the activity of heparan sulfate, an important regulator of a wide range of biological cell functions. The multi-target approach that is exemplified by these types of strategies will probably be necessary to optimize SCI treatment.
Key points
-
The development of neuroregenerative therapeutics for spinal cord injury (SCI) is hampered by the limited ability of the CNS to regenerate, primarily owing to the non-permissive extracellular environment that is created following damage.
-
Approaches that target multiple biological pathways are likely to be the way forward for SCI treatment; potential multi-target therapeutic strategies include olfactory mucosa-derived mesenchymal stromal cells (OM-MSCs) and heparan sulfate mimetics.
-
OM-MSCs might offer advantages over conventional olfactory tissue transplantation approaches owing to their pro-reparative properties and ease of growth.
-
Heparan sulfates are known to bind many proteins, and their mimetics could affect numerous pathways after SCI, thereby enabling a polypharmacological approach to treatment.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Davies, S. J. et al. Regeneration of adult axons in white matter tracts of the central nervous system. Nature 390, 680–683 (1997).
Aguayo, A. J., David, S. & Bray, G. M. Influences of the glial environment on the elongation of axons after injury: transplantation studies in adult rodents. J. Exp. Biol. 95, 231–240 (1981).
Ramsay, R. R., Popovic-Nikolic, M. R., Nikolic, K., Uliassi, E. & Bolognesi, M. L. A perspective on multi-target drug discovery and design for complex diseases. Clin. Transl. Med. 7, 3 (2018).
Laroni, A., Novi, G., Kerlero de Rosbo, N. & Uccelli, A. Towards clinical application of mesenchymal stem cells for treatment of neurological diseases of the central nervous system. J. Neuroimmune Pharmacol. 8, 1062–1076 (2013).
Mohamed, S. & Coombe, D. R. Heparin mimetics: their therapeutic potential. Pharmaceuticals 10, 78 (2017).
World Health Organization Spinal cord injury. https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury (2013).
Wagner, F. B. et al. Targeted neurotechnology restores walking in humans with spinal cord injury. Nature 563, 65–71 (2018).
Tran, A. P., Warren, P. M. & Silver, J. The biology of regeneration failure and success after spinal cord injury. Physiol. Rev. 98, 881–917 (2018).
Fawcett, J. W. Overcoming inhibition in the damaged spinal cord. J. Neurotrauma 23, 371–383 (2006).
Alizadeh, A., Dyck, S. M. & Karimi-Abdolrezaee, S. Traumatic spinal cord injury: an overview of pathophysiology, models and acute injury mechanisms. Front. Neurol. 10, 282 (2019).
Fitch, M. T. & Silver, J. CNS injury, glial scars, and inflammation: inhibitory extracellular matrices and regeneration failure. Exp. Neurol. 209, 294–301 (2008).
Anderson, M. A. et al. Astrocyte scar formation aids central nervous system axon regeneration. Nature 532, 195–200 (2016).
Fawcett, J. W. The extracellular matrix in plasticity and regeneration after CNS injury and neurodegenerative disease. Prog. Brain Res. 218, 213–226 (2015).
Fouad, K., Krajacic, A. & Tetzlaff, W. Spinal cord injury and plasticity: opportunities and challenges. Brain Res. Bull. 84, 337–342 (2011).
Ulndreaj, A., Badner, A. & Fehlings, M. G. Promising neuroprotective strategies for traumatic spinal cord injury with a focus on the differential effects among anatomical levels of injury. F1000Research 6, 1907 (2017).
McKerracher, L. & Higuchi, H. Targeting Rho to stimulate repair after spinal cord injury. J. Neurotrauma 23, 309–317 (2006).
Pearse, D. D. et al. cAMP and Schwann cells promote axonal growth and functional recovery after spinal cord injury. Nat. Med. 10, 610–616 (2004).
Domeniconi, M. & Filbin, M. T. Overcoming inhibitors in myelin to promote axonal regeneration. J. Neurol. Sci. 233, 43–47 (2005).
Franklin, R. J. & Kotter, M. R. The biology of CNS remyelination: the key to therapeutic advances. J. Neurol. 255, 19–25 (2008).
Merkler, D. et al. Locomotor recovery in spinal cord-injured rats treated with an antibody neutralizing the myelin-associated neurite growth inhibitor Nogo-A. J. Neurosci. 21, 3665–3673 (2001).
Buchli, A. D. & Schwab, M. E. Inhibition of Nogo: a key strategy to increase regeneration, plasticity and functional recovery of the lesioned central nervous system. Ann. Med. 37, 556–567 (2005).
Ito, S. et al. LOTUS inhibits neuronal apoptosis and promotes tract regeneration in contusive spinal cord injury model mice. eNeuro https://doi.org/10.1523/ENEURO.0303-18.2018 (2018).
Sato, Y. et al. Cartilage acidic protein-1B (LOTUS), an endogenous nogo receptor antagonist for axon tract formation. Science 333, 769–773 (2011).
Bradbury, E. J. et al. Chondroitinase ABC promotes functional recovery after spinal cord injury. Nature 416, 636–640 (2002).
Nomura, H., Tator, C. H. & Shoichet, M. S. Bioengineered strategies for spinal cord repair. J. Neurotrauma 23, 496–507 (2006).
Harkema, S. et al. Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: a case study. Lancet 377, 1938–1947 (2011).
Terson de Paleville, D. G. L., Harkema, S. J. & Angeli, C. A. Epidural stimulation with locomotor training improves body composition in individuals with cervical or upper thoracic motor complete spinal cord injury: a series of case studies. J. Spinal Cord. Med. 42, 32–38 (2019).
Houle, J. D. & Cote, M. P. Axon regeneration and exercise-dependent plasticity after spinal cord injury. Ann. N. Y. Acad. Sci. 1279, 154–163 (2013).
Hutson, T. H. & Giovanni, S. The translational landscape in spinal cord injury: focus on neuroplasticity and regeneration. Nat. Rev. Neurol. 15, 732–745 (2019).
Muir, E., De Winter, F., Verhaagen, J. & Fawcett, J. Recent advances in the therapeutic uses of chondroitinase ABC. Exp. Neurol. 321, 113032 (2019).
Courtine, G. & Sofroniew, M. V. Spinal cord repair: advances in biology and technology. Nat. Med. 25, 898–908 (2019).
Chen, K. et al. Sequential therapy of anti-Nogo-A antibody treatment and treadmill training leads to cumulative improvements after spinal cord injury in rats. Exp. Neurol. 292, 135–144 (2017).
Garcia-Alias, G. & Fawcett, J. W. Training and anti-CSPG combination therapy for spinal cord injury. Exp. Neurol. 235, 26–32 (2012).
Karimi-Abdolrezaee, S., Eftekharpour, E., Wang, J., Schut, D. & Fehlings, M. G. Synergistic effects of transplanted adult neural stem/progenitor cells, chondroitinase, and growth factors promote functional repair and plasticity of the chronically injured spinal cord. J. Neurosci. 30, 1657–1676 (2010).
Zhao, R. R. et al. Combination treatment with anti-Nogo-A and chondroitinase ABC is more effective than single treatments at enhancing functional recovery after spinal cord injury. Eur. J. Neurosci. 38, 2946–2961 (2013).
Ruff, C. A., Wilcox, J. T. & Fehlings, M. G. Cell-based transplantation strategies to promote plasticity following spinal cord injury. Exp. Neurol. 235, 78–90 (2012).
Biernaskie, J. et al. Skin-derived precursors generate myelinating Schwann cells that promote remyelination and functional recovery after contusion spinal cord injury. J. Neurosci. 27, 9545–9559 (2007).
Sparling, J. S. et al. Schwann cells generated from neonatal skin-derived precursors or neonatal peripheral nerve improve functional recovery after acute transplantation into the partially injured cervical spinal cord of the rat. J. Neurosci. 35, 6714–6730 (2015).
Toft, A., Tome, M., Barnett, S. C. & Riddell, J. S. A comparative study of glial and non-neural cell properties for transplant-mediated repair of the injured spinal cord. Glia 61, 513–528 (2013).
Barnett, S. C. & Riddell, J. S. Olfactory ensheathing cell transplantation as a strategy for spinal cord repair — what can it achieve? Nat. Clin. Pract. Neurol. 3, 152–161 (2007).
Brock, J. H., Graham, L., Staufenberg, E., Im, S. & Tuszynski, M. H. Rodent neural progenitor cells support functional recovery after cervical spinal cord contusion. J. Neurotrauma 35, 1069–1078 (2018).
Cummings, B. J. et al. Human neural stem cells differentiate and promote locomotor recovery in spinal cord-injured mice. Proc. Natl Acad. Sci. USA 102, 14069–14074 (2005).
Keirstead, H. S. et al. Human embryonic stem cell-derived oligodendrocyte progenitor cell transplants remyelinate and restore locomotion after spinal cord injury. J. Neurosci. 25, 4694–4705 (2005).
Nori, S. et al. Grafted human-induced pluripotent stem-cell-derived neurospheres promote motor functional recovery after spinal cord injury in mice. Proc. Natl Acad. Sci. USA 108, 16825–16830 (2011).
Maldonado-Lasuncion, I., Verhaagen, J. & Oudega, M. Mesenchymal stem cell–macrophage choreography supporting spinal cord repair. Neurotherapeutics 15, 578–587 (2018).
Graziadei, G. A. & Graziadei, P. P. Neurogenesis and neuron regeneration in the olfactory system of mammals. II. Degeneration and reconstitution of the olfactory sensory neurons after axotomy. J. Neurocytol. 8, 197–213 (1979).
Doucette, R. Glial influences on axonal growth in the primary olfactory system. Glia 3, 433–449 (1990).
Schwob, J. E. Neural regeneration and the peripheral olfactory system. Anat. Rec. 269, 33–49 (2002).
Barber, P. C. Neurogenesis and regeneration in the primary olfactory pathway of mammals. Bibl. Anat. (23), 12–25 (1982).
Fraher, J. P. The CNS–PNS transitional zone of the rat. Morphometric studies at cranial and spinal levels. Prog. Neurobiol. 38, 261–316 (1992).
Ramer, L. M. et al. Peripheral olfactory ensheathing cells reduce scar and cavity formation and promote regeneration after spinal cord injury. J. Comp. Neurol. 473, 1–15 (2004).
Chuah, M. I., Hale, D. M. & West, A. K. Interaction of olfactory ensheathing cells with other cell types in vitro and after transplantation: glial scars and inflammation. Exp. Neurol. 229, 46–53 (2011).
Tennent, R. & Chuah, M. I. Ultrastructural study of ensheathing cells in early development of olfactory axons. Dev. Brain Res. 95, 135–139 (1996).
Chung, R. S. et al. Olfactory ensheathing cells promote neurite sprouting of injured axons in vitro by direct cellular contact and secretion of soluble factors. Cell. Mol. Life Sci. 61, 1238–1245 (2004).
Chehrehasa, F. et al. Olfactory glia enhance neonatal axon regeneration. Mol. Cell. Neurosci. 45, 277–288 (2010).
Nazareth, L. et al. Olfactory ensheathing cells are the main phagocytic cells that remove axon debris during early development of the olfactory system. J. Comp. Neurol. 523, 479–494 (2015).
Su, Z. et al. Olfactory ensheathing cells: the primary innate immunocytes in the olfactory pathway to engulf apoptotic olfactory nerve debris. Glia 61, 490–503 (2013).
Toft, A., Scott, D. T., Barnett, S. C. & Riddell, J. S. Electrophysiological evidence that olfactory cell transplants improve function after spinal cord injury. Brain 130, 970–984 (2007).
Plant, G. W., Christensen, C. L., Oudega, M. & Bunge, M. B. Delayed transplantation of olfactory ensheathing glia promotes sparing/regeneration of supraspinal axons in the contused adult rat spinal cord. J. Neurotrauma 20, 1–16 (2003).
Richter, M. W., Fletcher, P. A., Liu, J., Tetzlaff, W. & Roskams, A. J. Lamina propria and olfactory bulb ensheathing cells exhibit differential integration and migration and promote differential axon sprouting in the lesioned spinal cord. J. Neurosci. 25, 10700–10711 (2005).
Deumens, R. et al. Olfactory ensheathing cells, olfactory nerve fibroblasts and biomatrices to promote long-distance axon regrowth and functional recovery in the dorsally hemisected adult rat spinal cord. Exp. Neurol. 200, 89–103 (2006).
Sun, T., Ye, C., Zhang, Z., Wu, J. & Huang, H. Cotransplantation of olfactory ensheathing cells and Schwann cells combined with treadmill training promotes functional recovery in rats with contused spinal cords. Cell Transpl. 22, S27–S38 (2013).
Zhang, J. et al. The effects of co-transplantation of olfactory ensheathing cells and Schwann cells on local inflammation environment in the contused spinal cord of rats. Mol. Neurobiol. 54, 943–953 (2017).
Muniswami, D. M. & Tharion, G. Therapeutic effect of cell transplantation and chondroitinase in rat spinal cord injury. Int. J. Appl. Basic. Med. Res. 8, 220–226 (2018).
Thornton, M. A. et al. Evidence of axon connectivity across a spinal cord transection in rats treated with epidural stimulation and motor training combined with olfactory ensheathing cell transplantation. Exp. Neurol. 309, 119–133 (2018).
Barnett, S. C. et al. Identification of a human olfactory ensheathing cell that can effect transplant-mediated remyelination of demyelinated CNS axons. Brain 123, 1581–1588 (2000).
Feron, F., Perry, C., McGrath, J. J. & Mackay-Sim, A. New techniques for biopsy and culture of human olfactory epithelial neurons. Arch. Otolaryngol. Head. Neck Surg. 124, 861–866 (1998).
Choi, D., Law, S., Raisman, G. & Li, D. Olfactory ensheathing cells in the nasal mucosa of the rat and human. Br. J. Neurosurg. 22, 301–302 (2008).
Lim, F. et al. Reversibly immortalized human olfactory ensheathing glia from an elderly donor maintain neuroregenerative capacity. Glia 58, 546–558 (2010).
Garcia-Escudero, V. et al. A neuroregenerative human ensheathing glia cell line with conditional rapid growth. Cell Transpl. 20, 153–166 (2011).
Yao, R. et al. Olfactory ensheathing cells for spinal cord injury: sniffing out the issues. Cell Transpl. 27, 879–889 (2018).
Choi, D., Li, D., Law, S., Powell, M. & Raisman, G. A prospective observational study of the yield of olfactory ensheathing cells cultured from biopsies of septal nasal mucosa. Neurosurgery 62, 1140–1144 (2008).
Dlouhy, B. J., Awe, O., Rao, R. C., Kirby, P. A. & Hitchon, P. W. Autograft-derived spinal cord mass following olfactory mucosal cell transplantation in a spinal cord injury patient: case report. J. Neurosurg. Spine 21, 618–622 (2014).
Tome, M., Lindsay, S. L., Riddell, J. S. & Barnett, S. C. Identification of nonepithelial multipotent cells in the embryonic olfactory mucosa. Stem Cells 27, 2196–2208 (2009).
Lindsay, S. L. et al. Human mesenchymal stem cells isolated from olfactory biopsies but not bone enhance CNS myelination in vitro. Glia 61, 368–382 (2013).
Delorme, B. et al. The human nose harbors a niche of olfactory ectomesenchymal stem cells displaying neurogenic and osteogenic properties. Stem Cells Dev. 19, 853–866 (2010).
Lindsay, S. L., Johnstone, S. A., McGrath, M. A., Mallinson, D. & Barnett, S. C. Comparative miRNA-based fingerprinting reveals biological differences in human olfactory mucosa- and bone-marrow-derived mesenchymal stromal cells. Stem Cell Rep. 6, 729–742 (2016).
Di Trapani, M. et al. Comparative study of immune regulatory properties of stem cells derived from different tissues. Stem Cells Dev. 22, 2990–3002 (2013).
Antonevich, N. et al. Human olfactory mucosa-derived mesenchymal stem cells suppress cytotoxic functions of CD8+ T-lymphocytes and natural killer cells. J. Allergy Clin. Immunol. 141, AB122 (2018).
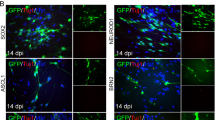
Lindsay, S. L. et al. Human olfactory mesenchymal stromal cell transplants promote remyelination and earlier improvement in gait co-ordination after spinal cord injury. Glia 65, 639–656 (2017).
Pandit, S. R., Sullivan, J. M., Egger, V., Borecki, A. A. & Oleskevich, S. Functional effects of adult human olfactory stem cells on early-onset sensorineural hearing loss. Stem Cells 29, 670–677 (2011).
Nivet, E. et al. Engraftment of human nasal olfactory stem cells restores neuroplasticity in mice with hippocampal lesions. J. Clin. Invest. 121, 2808–2820 (2011).
Chopp, M. et al. Spinal cord injury in rat: treatment with bone marrow stromal cell transplantation. Neuroreport 11, 3001–3005 (2000).
Himes, B. T. et al. Recovery of function following grafting of human bone marrow-derived stromal cells into the injured spinal cord. Neurorehabil. Neural Repair. 20, 278–296 (2006).
Neuhuber, B., Timothy Himes, B., Shumsky, J. S., Gallo, G. & Fischer, I. Axon growth and recovery of function supported by human bone marrow stromal cells in the injured spinal cord exhibit donor variations. Brain Res. 1035, 73–85 (2005).
Willison, A. G. & Barnett, S. C. A scoping review of trials for cell-based therapies in human spinal cord injury. Spinal Cord (in the press).
Dai, G. et al. Transplantation of autologous bone marrow mesenchymal stem cells in the treatment of complete and chronic cervical spinal cord injury. Brain Res. 1533, 73–79 (2013).
Chhabra, H. S. et al. Autologous bone marrow cell transplantation in acute spinal cord injury — an Indian pilot study. Spinal Cord. 54, 57–64 (2016).
Rosenbaum, A. J., Grande, D. A. & Dines, J. S. The use of mesenchymal stem cells in tissue engineering: a global assessment. Organogenesis 4, 23–27 (2008).
Ra, J. C. et al. Safety of intravenous infusion of human adipose tissue-derived mesenchymal stem cells in animals and humans. Stem Cells Dev. 20, 1297–1308 (2011).
Hur, J. W. et al. Intrathecal transplantation of autologous adipose-derived mesenchymal stem cells for treating spinal cord injury: a human trial. J. Spinal Cord. Med. 39, 655–664 (2016).
Mackay-Sim, A. et al. Autologous olfactory ensheathing cell transplantation in human paraplegia: a 3-year clinical trial. Brain 131, 2376–2386 (2008).
Tabakow, P. et al. Functional regeneration of supraspinal connections in a patient with transected spinal cord following transplantation of bulbar olfactory ensheathing cells with peripheral nerve bridging. Cell Transpl. 23, 1631–1655 (2014).
Larson, C. A. & Dension, P. M. Effectiveness of intense, activity-based physical therapy for individuals with spinal cord injury in promoting motor and sensory recovery: is olfactory mucosa autograft a factor? J. Spinal Cord. Med. 36, 44–57 (2013).
Lammertse, D. et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial design. Spinal Cord. 45, 232–242 (2007).
Siddiqui, A. M., Khazaei, M. & Fehlings, M. G. Translating mechanisms of neuroprotection, regeneration, and repair to treatment of spinal cord injury. Prog. Brain Res. 218, 15–54 (2015).
Vismara, I., Papa, S., Rossi, F., Forloni, G. & Veglianese, P. Current options for cell therapy in spinal cord injury. Trends Mol. Med. 23, 831–849 (2017).
Badner, A., Siddiqui, A. M. & Fehlings, M. G. Spinal cord injuries: how could cell therapy help? Expert. Opin. Biol. Ther. 17, 529–541 (2017).
Lemons, M. L., Howland, D. R. & Anderson, D. K. Chondroitin sulfate proteoglycan immunoreactivity increases following spinal cord injury and transplantation. Exp. Neurol. 160, 51–65 (1999).
Rudge, J. S. & Silver, J. Inhibition of neurite outgrowth on astroglial scars in vitro. J. Neurosci. 10, 3594–3603 (1990).
Sarrazin, S., Lamanna, W. C. & Esko, J. D. Heparan sulfate proteoglycans. Cold Spring Harb. Perspect. Biol. 3, a004952 (2011).
Xu, D., Arnold, K. & Liu, J. Using structurally defined oligosaccharides to understand the interactions between proteins and heparan sulfate. Curr. Opin. Struct. Biol. 50, 155–161 (2018).
Turnbull, J., Powell, A. & Guimond, S. Heparan sulfate: decoding a dynamic multifunctional cell regulator. Trends Cell Biol. 11, 75–82 (2001).
Hardingham, T. E. & Fosang, A. J. Proteoglycans: many forms and many functions. FASEB J. 6, 861–870 (1992).
Poole, A. R. Proteoglycans in health and disease: structures and functions. Biochem. J. 236, 1–14 (1986).
Lindahl, U., Kusche, M., Lidholt, K. & Oscarsson, L. G. Biosynthesis of heparin and heparan sulfate. Ann. N. Y. Acad. Sci. 556, 36–50 (1989).
Feyerabend, T. B., Li, J. P., Lindahl, U. & Rodewald, H. R. Heparan sulfate C5-epimerase is essential for heparin biosynthesis in mast cells. Nat. Chem. Biol. 2, 195–196 (2006).
Murphy, K. J., McLay, N. & Pye, D. A. Structural studies of heparan sulfate hexasaccharides: new insights into iduronate conformational behavior. J. Am. Chem. Soc. 130, 12435–12444 (2008).
Guglier, S. et al. Minimum FGF2 binding structural requirements of heparin and heparan sulfate oligosaccharides as determined by NMR spectroscopy. Biochemistry 47, 13862–13869 (2008).
Cardozo, M. J., Mysiak, K. S., Becker, T. & Becker, C. G. Reduce, reuse, recycle — developmental signals in spinal cord regeneration. Dev. Biol. 432, 53–62 (2017).
Dani, N. & Broadie, K. Glycosylated synaptomatrix regulation of trans-synaptic signaling. Dev. Neurobiol. 72, 2–21 (2012).
Turnbull, J. E., Fernig, D. G., Ke, Y., Wilkinson, M. C. & Gallagher, J. T. Identification of the basic fibroblast growth factor binding sequence in fibroblast heparan sulfate. J. Biol. Chem. 267, 10337–10341 (1992).
Shen, Y. Traffic lights for axon growth: proteoglycans and their neuronal receptors. Neural Regen. Res. 9, 356–361 (2014).
Verma, P., Garcia-Alias, G. & Fawcett, J. W. Spinal cord repair: bridging the divide. Neurorehabil. Neural Repair 22, 429–437 (2008).
Kantor, D. B. et al. Semaphorin 5a is a bifunctional axon guidance cue regulated by heparan and chondroitin sulfate proteoglycans. Neuron 44, 961–975 (2004).
Shen, Y. et al. PTPσ is a receptor for chondroitin sulfate proteoglycan, an inhibitor of neural regeneration. Science 326, 592–596 (2009).
Coles, C. H. et al. Proteoglycan-specific molecular switch for RPTPσ clustering and neuronal extension. Science 332, 484–488 (2011).
Katagiri, Y. et al. Identification of novel binding sites for heparin in receptor protein-tyrosine phosphatase (RPTPσ): implications for proteoglycan signaling. J. Biol. Chem. 293, 11639–11647 (2018).
Takeuchi, K. et al. Chondroitin sulphate N-acetylgalactosaminyl-transferase-1 inhibits recovery from neural injury. Nat. Commun. 4, 2740 (2013).
Choay, J. et al. Anti-Xa active heparin oligosaccharides. Thromb. Res. 18, 573–578 (1980).
Fareed, J. et al. Pharmacodynamic and pharmacokinetic properties of enoxaparin: implications for clinical practice. Clin. Pharmacokinet. 42, 1043–1057 (2003).
Altinbas, M. et al. A randomized clinical trial of combination chemotherapy with and without low-molecular-weight heparin in small cell lung cancer. J. Thromb. Haemost. 2, 1266–1271 (2004).
Ghezzi, S. et al. Heparin prevents Zika virus induced-cytopathic effects in human neural progenitor cells. Antivir. Res. 140, 13–17 (2017).
Ma, Q. et al. The blood–brain barrier accessibility of a heparin-derived oligosaccharides C3. Thromb. Res. 105, 447–453 (2002).
Dudas, B. et al. Oral and subcutaneous administration of the glycosaminoglycan C3 attenuates Aβ25–35-induced abnormal tau protein immunoreactivity in rat brain. Neurobiol. Aging 23, 97–104 (2002).
Hao, L. N., Zhang, Q. Z., Yu, T. G., Cheng, Y. N. & Ji, S. L. Antagonistic effects of ultra-low-molecular-weight heparin on Aβ25–35-induced apoptosis in cultured rat cortical neurons. Brain Res. 1368, 1–10 (2011).
Zhu, H., Yu, J. & Kindy, M. S. Inhibition of amyloidosis using low-molecular-weight heparins. Mol. Med. 7, 517–522 (2001).
Timmer, N. M. et al. Enoxaparin treatment administered at both early and late stages of amyloid β deposition improves cognition of APPswe/PS1dE9 mice with differential effects on brain Aβ levels. Neurobiol. Dis. 40, 340–347 (2010).
Scholefield, Z. et al. Heparan sulfate regulates amyloid precursor protein processing by BACE1, the Alzheimer’s β-secretase. J. Cell Biol. 163, 97–107 (2003).
Schworer, R., Zubkova, O. V., Turnbull, J. E. & Tyler, P. C. Synthesis of a targeted library of heparan sulfate hexa- to dodecasaccharides as inhibitors of β-secretase: potential therapeutics for Alzheimer’s disease. Chemistry 19, 6817–6823 (2013).
Keskin, I. et al. Dose-dependent neuroprotective effect of enoxaparin on cold-induced traumatic brain injury. Neural Regen. Res. 12, 761–764 (2017).
Zupan, Z. et al. Effects of enoxaparin in the rat hippocampus following traumatic brain injury. Prog. Neuropsychopharmacol. Biol. Psychiatry 35, 1846–1856 (2011).
Wahl, F., Grosjean-Piot, O., Bareyre, F., Uzan, A. & Stutzmann, J. M. Enoxaparin reduces brain edema, cerebral lesions, and improves motor and cognitive impairments induced by a traumatic brain injury in rats. J. Neurotrauma 17, 1055–1065 (2000).
Li, S. et al. Enoxaparin ameliorates post-traumatic brain injury edema and neurologic recovery, reducing cerebral leukocyte endothelial interactions and vessel permeability in vivo. J. Trauma. Acute Care Surg. 79, 78–84 (2015).
Baharvahdat, H. et al. Enoxaparin in the treatment of severe traumatic brain injury: a randomized clinical trial. Surg. Neurol. Int. 10, 10 (2019).
Hayashi, N. et al. Attenuation of glial scar formation in the injured rat brain by heparin oligosaccharides. Neurosci. Res. 49, 19–27 (2004).
Wang, J. et al. Hyaluronan tetrasaccharide in the cerebrospinal fluid is associated with self-repair of rats after chronic spinal cord compression. Neuroscience 210, 467–480 (2012).
Wakao, N. et al. Hyaluronan oligosaccharides promote functional recovery after spinal cord injury in rats. Neurosci. Lett. 488, 299–304 (2011).
Kovacsovics, T. J. et al. Combination of the low anticoagulant heparin CX-01 with chemotherapy for the treatment of acute myeloid leukemia. Blood Adv. 2, 381–389 (2018).
Nagata, K. et al. Early low-anticoagulant desulfated heparin after traumatic brain injury: reduced brain edema and leukocyte mobilization is associated with improved watermaze learning ability weeks after injury. J. Trauma. Acute Care Surg. 84, 727–735 (2018).
Yates, E. A. et al. 1H and 13C NMR spectral assignments of the major sequences of twelve systematically modified heparin derivatives. Carbohydr. Res. 294, 15–27 (1996).
Higginson, J. R. et al. Differential sulfation remodelling of heparan sulfate by extracellular 6-O-sulfatases regulates fibroblast growth factor-induced boundary formation by glial cells: implications for glial cell transplantation. J. Neurosci. 32, 15902–15912 (2012).
Lakatos, A., Franklin, R. J. & Barnett, S. C. Olfactory ensheathing cells and Schwann cells differ in their in vitro interactions with astrocytes. Glia 32, 214–225 (2000).
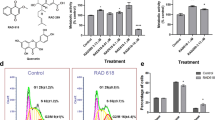
McCanney, G. A. et al. Low sulfated heparins target multiple proteins for central nervous system repair. Glia 67, 668–687 (2019).
Poulain, F. E. & Yost, H. J. Heparan sulfate proteoglycans: a sugar code for vertebrate development? Development 142, 3456–3467 (2015).
Blossom, D. B. et al. Outbreak of adverse reactions associated with contaminated heparin. N. Engl. J. Med. 359, 2674–2684 (2008).
Trehy, M. L., Reepmeyer, J. C., Kolinski, R. E., Westenberger, B. J. & Buhse, L. F. Analysis of heparin sodium by SAX/HPLC for contaminants and impurities. J. Pharm. Biomed. Anal. 49, 670–673 (2009).
Ding, Y., Vara Prasad, C., Bai, H. & Wang, B. Efficient and practical synthesis of fondaparinux. Bioorg Med. Chem. Lett. 27, 2424–2427 (2017).
Petitou, M. & van Boeckel, C. A. A synthetic antithrombin III binding pentasaccharide is now a drug! What comes next? Angew. Chem. Int. Ed. Engl. 43, 3118–3133 (2004).
Aikawa, J., Grobe, K., Tsujimoto, M. & Esko, J. D. Multiple isozymes of heparan sulfate/heparin GlcNAc N-deacetylase/GlcN N-sulfotransferase. Structure and activity of the fourth member, NDST4. J. Biol. Chem. 276, 5876–5882 (2001).
Sheng, J., Liu, R., Xu, Y. & Liu, J. The dominating role of N-deacetylase/N-sulfotransferase 1 in forming domain structures in heparan sulfate. J. Biol. Chem. 286, 19768–19776 (2011).
Liu, C. et al. Molecular mechanism of substrate specificity for heparan sulfate 2-O-sulfotransferase. J. Biol. Chem. 289, 13407–13418 (2014).
Habuchi, H. et al. The occurrence of three isoforms of heparan sulfate 6-O-sulfotransferase having different specificities for hexuronic acid adjacent to the targeted N-sulfoglucosamine. J. Biol. Chem. 275, 2859–2868 (2000).
Chen, J., Duncan, M. B., Carrick, K., Pope, R. M. & Liu, J. Biosynthesis of 3-O-sulfated heparan sulfate: unique substrate specificity of heparan sulfate 3-O-sulfotransferase isoform 5. Glycobiology 13, 785–794 (2003).
Thacker, B. E., Xu, D., Lawrence, R. & Esko, J. D. Heparan sulfate 3-O-sulfation: a rare modification in search of a function. Matrix Biol. 35, 60–72 (2014).
Poole, A. R., Webber, C., Pidoux, I., Choi, H. & Rosenberg, L. C. Localization of a dermatan sulfate proteoglycan (DS-PGII) in cartilage and the presence of an immunologically related species in other tissues. J. Histochem. Cytochem. 34, 619–625 (1986).
Kitagawa, H., Tsutsumi, K., Tone, Y. & Sugahara, K. Developmental regulation of the sulfation profile of chondroitin sulfate chains in the chicken embryo brain. J. Biol. Chem. 272, 31377–31381 (1997).
Acknowledgements
The authors’ work was supported by Medical Research Scotland (G.A.M., grant number MRS PhD-769-2014) and the Multiple Sclerosis Society of Great Britain (S.L.L., grant number 56).
Author information
Authors and Affiliations
Contributions
All authors researched data for the article and wrote the manuscript. S.L.L., G.A.M. and S.C.B. made substantial contributions to discussions of the content and edited and/or reviewed the manuscript before submission. A.G.W. researched and wrote the clinical section.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Neurology thanks I. Fischer and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Glossary
- Epimerization
-
A structural change in an epimer, which is one of a pair of stereoisomers. For example, glucose and galactose are epimers of each other, as they differ only in the position of the hydroxyl group at C4 (chiral carbon atom).
- 1C4 chair
-
A cyclohexane conformation is any of several three-dimensional shapes that a cyclohexane molecule can assume while maintaining the integrity of its chemical bonds. The most important shapes are called chair, half-chair, boat and skew/twist-boat. The numbers on the C represent its position in the conformation: the superscript number is above the plane and the subscript number is below the plane. The chair conformation is the most stable conformer.
Rights and permissions
About this article
Cite this article
Lindsay, S.L., McCanney, G.A., Willison, A.G. et al. Multi-target approaches to CNS repair: olfactory mucosa-derived cells and heparan sulfates. Nat Rev Neurol 16, 229–240 (2020). https://doi.org/10.1038/s41582-020-0311-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-020-0311-0
This article is cited by
-
Priming and Combined Strategies for the Application of Mesenchymal Stem Cells in Ischemic Stroke: A Promising Approach
Molecular Neurobiology (2024)
-
Autologous olfactory mucosa mesenchymal stem cells treatment improves the neural network in chronic refractory epilepsy
Stem Cell Research & Therapy (2023)
-
Spatiotemporal Dynamics of the Molecular Expression Pattern and Intercellular Interactions in the Glial Scar Response to Spinal Cord Injury
Neuroscience Bulletin (2023)
-
Human olfactory mesenchymal stromal cell transplantation ameliorates experimental autoimmune encephalomyelitis revealing an inhibitory role for IL16 on myelination
Acta Neuropathologica Communications (2022)
-
Transplantation of mesenchymal stem cells for spinal cord injury: a systematic review and network meta-analysis
Journal of Translational Medicine (2021)