Abstract
Hypertension affects two-thirds of people aged >60 years and significantly increases the risk of both vascular cognitive impairment and Alzheimer’s disease. Hypertension compromises the structural and functional integrity of the cerebral microcirculation, promoting microvascular rarefaction, cerebromicrovascular endothelial dysfunction and neurovascular uncoupling, which impair cerebral blood supply. In addition, hypertension disrupts the blood–brain barrier, promoting neuroinflammation and exacerbation of amyloid pathologies. Ageing is characterized by multifaceted homeostatic dysfunction and impaired cellular stress resilience, which exacerbate the deleterious cerebromicrovascular effects of hypertension. Neuroradiological markers of hypertension-induced cerebral small vessel disease include white matter hyperintensities, lacunar infarcts and microhaemorrhages, all of which are associated with cognitive decline. Use of pharmaceutical and lifestyle interventions that reduce blood pressure, in combination with treatments that promote microvascular health, have the potential to prevent or delay the pathogenesis of vascular cognitive impairment and Alzheimer’s disease in patients with hypertension.
Key points
-
Hypertension is associated with ageing and significantly increases the risk of vascular cognitive impairment and Alzheimer’s disease.
-
In older individuals, hypertension leads to maladaptation of the cerebral circulation, resulting in dysregulation of cerebral blood flow, microvascular rarefaction, blood–brain barrier disruption, oxidative stress and impaired neurovascular coupling.
-
Hypertension causes pathological alterations in cerebral microvessels that damage microvascular structure, network architecture and function, and contribute to the genesis of cerebral microhaemorrhages, lacunar infarcts and white matter injury; these factors are associated with cognitive decline.
-
Potential mechanisms by which hypertension could exacerbate the progression of Alzheimer’s disease include increased oxidative microvascular damage, brain inflammation and blood–brain barrier disruption, as well as impaired glymphatic (also known as glial-lymphatic) clearance of amyloid-β.
-
Use of pharmaceutical and/or lifestyle interventions that reduce blood pressure in combination with treatments that promote microvascular health could potentially prevent or delay cognitive decline in patients with hypertension.
Similar content being viewed by others
Introduction
Vascular cognitive impairment (VCI) and Alzheimer’s disease (AD) are major obstacles to healthy ageing and the principal causes of chronic disability and decreased quality of life among elderly people in the industrialized world. The prevalence of AD and VCI is projected to quadruple in the next 50 years owing to rapid ageing of the populations of Europe, Japan and the USA. The economic impact of dementia has been estimated at US $200 billion per year in the USA1 and US $600 billion per year worldwide2, including market costs associated with nursing home care and the economic burden of unpaid care-givers. The maintenance of cognitive health and prevention of dementia among older adults is a critical scientific and public health priority.
Among the potential targets for improvement of cognitive health among older adults, arterial hypertension is one of the most prevalent and potentially modifiable pathologies. Hypertension, especially in older adults, substantially increases the risk of VCI3 and exacerbates the pathogenesis of AD4,5,6,7,8. The interactions of hypertension and ageing and the contributions of hypertension to cognitive dysfunction in older individuals are multifaceted. First, hypertension itself is a disease of ageing. Second, ageing is associated with the generalized impairment of several homeostatic mechanisms, including regulation of cerebral blood flow and microvascular pressure. Third, ageing is associated with impaired cellular stress resilience, which exacerbates cellular and molecular damage resulting from hypertension-induced haemodynamic and oxidative stress. Fourth, several key cellular and molecular mechanisms, including oxidative stress, endothelial dysfunction, inflammatory processes and blood–brain barrier (BBB) dysfunction, are common to vascular ageing and hypertension-induced vascular dysfunction and end organ damage. Hypertension-induced vascular pathologies can therefore be considered to be the result of accelerated vascular ageing. Chronic hypertension can also promote the development of atherosclerotic plaques in larger cerebral arteries9, which may adversely impact cerebral blood flow and lead to ischaemic strokes that contribute to cognitive decline in the elderly3.
Here, we review the synergistic deleterious effects of elevated blood pressure and old age on the structural and functional integrity of the cerebral microcirculation and cognitive function. We discuss the role of advanced age in cerebrovascular maladaptation to hypertension and the resulting exacerbation of microvascular pathologies. We then focus on microvascular contributions to exacerbated hypertension-induced cognitive impairment in ageing, including small vessel disease, capillary rarefaction and BBB disruption, neurovascular dysfunction and the pathogenesis of cerebral microhaemorrhages, lacunar infarcts and white matter lesions (also known as leukoaraiosis), as well as the role of hypertension in the pathogenesis of AD in older adults.
Epidemiology
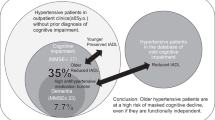
Hypertension (defined as systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg10) affects 1 billion individuals worldwide, and the prevalence significantly increases with age11. In the USA, the estimated prevalence of hypertension is 76% among adults aged 65−74 years and 82% among adults aged ≥75 years12. Despite increasing awareness of the deleterious effects of hypertension, rates of blood pressure control remain suboptimal. In the past decade, only ~50% of adult US patients with hypertension achieved adequate blood pressure control11. The deleterious effects of high blood pressure on cognitive function were recognized at the end of the nineteenth century13, and studies in the 1960s and 1970s provided evidence that hypertension impairs various domains of cognition14. Subsequently, many prospective longitudinal studies have demonstrated a causal relationship between blood pressure and the incidence of VCI and AD15.
The Honolulu-Asia Aging Study5 demonstrated an association between mid-life blood pressure and VCI and AD in old age. Among participants who were never treated for hypertension, higher blood pressure was associated with a significantly increased risk of dementia owing to VCI or AD (odds ratio (OR) 3.8 for DBP 90–94 mmHg, and 4.3 for DBP ≥95 mmHg compared with DBP 80–89 mmHg)5. Compared with normotensive individuals, patients with hypertension (SBP ≥160 mmHg) had a 4.8-fold higher risk of dementia5. In a retrospective cohort study in Northern California, USA, the presence of hypertension at midlife substantially increased the risk of late-life dementia16. Similar results were obtained in a prospective, population-based study in eastern Finland, which showed that hypertension in midlife increases the risk of AD in later life17. The prospective Adult Health Study in Japan confirmed the association between mid-life hypertension and VCI in old age. In the US ARIC study, midlife hypertension was associated with increased cognitive decline during 20 years of follow-up18.
The Swedish Gothenburg H-70 study showed that participants who developed dementia at age 79–85 years had significantly higher SBP (mean 178 vs 164 mmHg) and higher DBP (mean 101 vs 92 mmHg) at age 70 than those who did not develop dementia19. Another Swedish study showed that older adults with SBP >180 mmHg are at a significantly increased risk of AD20. A US prospective cohort study demonstrated that high SBP (≥160 mmHg) was associated with an increased risk of dementia among young elderly people (aged 64–75 years)21. Studies in Japan22 and the USA23 reported that hypertension is an independent risk factor for vascular dementia in individuals aged ≥65 years. In addition, hypertension was a risk factor for mild cognitive impairment in elderly participants (mean age 75 years) in a US longitudinal population study24.
The cognitive domains that are negatively affected by hypertension include abstract reasoning and/or executive function, memory and mental processing speed3. A study that used the Digit Symbol Substitution Test, which is a more sensitive measure of cognitive impairment than the Mini-Mental State Examination (MMSE), showed that in men aged 45–55 years, higher SBP and DBP were significantly associated with lower cognitive performance at 8 years of follow-up25. In women, higher SBP was associated with better cognition at younger ages and poorer cognition at older ages. The association between midlife patterns of SBP and cognitive decline was confirmed in a prospective study of the 10-year change in performance in tests including the Digit Symbol Substitution Test and MMSE. In this study, participants with high SBP in midlife experienced a greater decline in cognitive performance and had larger white matter hyperintensity (WMH) volumes at 10-year follow-up than those with low SBP in midlife26.
Health disparities
Widening disparities in the prevalence of hypertension and dementia exist worldwide27,28. The prevalence of hypertension is higher in low- and middle-income countries (LMICs; 31.5%) than in high-income countries (HICs; 28.5%)27. Similarly, the prevalence of dementia is higher in LMICs than HICs. Estimates suggest that in 2001, 60% of people with dementia lived in LMICs and that this proportion will increase to 71% by 2040 (ref.29). Moreover, the rates of increase are not uniform; the number of people with dementia in HICs is forecast to increase by 100% between 2001 and 2040, whereas a >300% increase is forecast in India, China and south Asian and Western Pacific countries. These differences can be partially attributed to differences in environmental and lifestyle factors, duration with disease and age-specific incidence.
Disparities in the prevalence of hypertension and dementia also exist within countries. African Americans have a higher prevalence of hypertension than people of European descent27 and a 1.5–4-fold increased risk of developing dementia compared with non-Hispanic white people28. A study that analysed longitudinal data for 34,349 participants in various large US cohort studies concluded that differences in cumulative blood pressure levels might contribute to racial differences in cognitive decline at older age30. The factors that underlie racial disparities in hypertension and hypertension-related diseases are likely to be related to social determinants of health, including education, social support, family income, employment and access to health services, which lead to differences in factors, including hypertension awareness, access to treatment, medication adherence and modifiable lifestyle factors including physical activity, smoking, alcohol consumption and dietary habits such as sodium and potassium intake31.
Comorbidities
In HICs, more than half of older individuals have three or more chronic conditions in addition to hypertension, including type 2 diabetes mellitus (T2DM), pre-diabetes, obesity, chronic kidney disease (CKD) and cardiovascular diseases (ischaemic heart disease, stroke or heart failure)32. The prevalence of obesity and T2DM among people with hypertension is more than double that of normotensive adults. Thus, the elderly often present with hypertension in a comorbid setting, which probably exacerbates the deleterious effects of high blood pressure on the brain. Strong evidence suggests that T2DM33, obesity34,35,36, CKD37 and heart failure38 impair the cerebral microvasculature, compromise cerebral blood flow and promote cognitive impairment. These effects are synergistic or additive to the vascular effects of hypertension and thereby exacerbate the pathogenesis of VCI and AD in older individuals with comorbidities.
Adaptation of the cerebral circulation
Preclinical studies have provided mechanistic evidence that in young organisms, the cerebral circulation exhibits structural and functional adaptations to chronic elevations of blood pressure that lead to compensatory increases in cerebrovascular resistance39. The structural adaptations include remodelling of the cerebral arteries and arterioles, which results in an increased wall-to-lumen ratio that reduces wall stress and increases segmental resistance39,40. Cerebrovascular remodelling is an active process, guided by mechanosensitive signalling mechanisms that are triggered by haemodynamic stimuli and dynamic interactions between growth factors, cytokines and vasoactive substances produced by cells within the vascular wall. Vascular structural remodelling involves adaptive changes in cell growth and proliferation, cell death, cell migration, and changes in the synthesis, deposition and degradation of extracellular matrix components.
Functional adaptations to high blood pressure include an enhanced pressure-induced myogenic constriction response of segmentally connected cerebral arteries and arterioles41. This important homeostatic mechanism ensures that high arterial pressure is not transmitted to the distal portion of the microcirculation where it would damage the thin-walled arteriolar and capillary microvessels in the brain42. Myogenic constriction of resistance vessels is also responsible for autoregulation, which keeps cerebral blood flow fairly stable during fluctuations in blood pressure. Owing to the enhanced myogenic response of cerebral vessels, the autoregulatory curve of cerebral blood flow is shifted to the right in patients and animal models with hypertension, extending the limits of autoregulation towards higher pressure values41,43.
Experimental evidence indicates that hypertension-induced adaptive enhancement of the myogenic response is at least partly due to chronic upregulation of the 20-hydroxyeicosatetraenoic-acid (20-HETE)–short transient receptor potential channel 6 (TRPC6) pathway, which leads to sustained pressure-induced increases in intracellular Ca2+ in vascular smooth muscle cells (VSMCs)39,41,44 (Fig. 1). Other mechanisms may involve hypertension-induced changes in the expression of epithelial sodium channels45, transient receptor potential cation channel subfamily V member 4 (TRPV4) channels46 and/or other ion channels that are involved in pressure-induced depolarization of VSMCs42 as well as altered activation of Rho kinase and protein kinase C47, which modulate the Ca2+ sensitivity of the contractile apparatus. These adaptive changes keep the intracranial blood volume within the normal range and protect the thin-walled, vulnerable distal portion of the cerebral microcirculation from high pressure-induced damage.
a | In the vascular smooth muscle cells (VSMCs) of young cerebral arteries, upregulation of a 20-hydroxyeicosatetraenoic-acid (20-HETE)–short transient receptor potential channel 6 (TRPC6)-dependent pathway results in functional adaptation of cerebral arteries to hypertension. Hypertension is associated with increased expression of 20-HETE-producing cytochrome P4504A (CYP4504A) isoforms and TRPC6. High pressure activates phospholipase A2 (PLA2), leading to activation of arachidonic acid (AA) metabolism and the production of 20-HETE, which activates TRPC6 channels, resulting in increases in Ca2+ levels and myogenic contraction41. 20-HETE also inhibits activation of hyperpolarizing Ca2+-activated potassium channels (BKca), which facilitates pressure-induced activation of voltage-dependent L-type Ca2+ channels (LCa), contributing to Ca2+ influx and myogenic contraction. This adaptation extends the range of cerebrovascular autoregulatory protection to higher blood pressure levels, optimizing tissue perfusion and protecting the cerebral microcirculation from increased arterial pressure and pressure pulsatility. b | In aged cerebral arteries, functional adaptation to hypertension mediated by activation of the VSMC 20-HETE–TRPC-dependent pathway is impaired. The failure of these arteries to exhibit a hypertension-induced adaptive increase in myogenic constriction results in myogenic contraction and cerebrovascular autoregulatory dysfunction. c | In the aged brain, the failure of proximal resistance arteries to functionally adapt to hypertension results in a mismatch between perfusion pressure and segmental vascular resistance that enables increased pulsatile pressure to penetrate the vulnerable downstream portion of the cerebral microcirculation. The resulting haemodynamic burden exacerbates age-related disruption of the blood–brain barrier (BBB), leading to extravasation of plasma factors (e.g. fibrinogen, thrombin, IgG), which promote microglia activation and neuroinflammation. Microglia-derived pro-inflammatory cytokines, activated matrix metalloproteinases (MMPs) and reactive oxygen species (ROS) induce neuronal damage and synaptic dysfunction41,189. Increased microvascular pressure impairs the clearance function of the glymphatic (also known as glial-lymphatic) system and promotes the development of cerebral microhaemorrhages via redox-mediated activation of MMPs and consequential weakening of the vascular wall. The increased pressure also contributes to pathological remodelling of the microvascular network architecture by promoting microvascular thrombosis, capillary regression and microvascular rarefaction, resulting in ghost vessels. We posit that exacerbation of neuroinflammation, cerebral microhaemorrhages, glymphatic dysfunction and/or microvascular rarefaction are causally linked to hypertension-induced cognitive impairment in ageing4,190 and also contribute to the pathogenesis of Alzheimer’s disease in hypertensive elderly individuals. Figure adapted with permission from ref.39, American Physiological Society.
Age-related maladaptation
Preclinical studies demonstrate that functional and structural adaptation of cerebral arteries to hypertension is impaired in ageing. Aged cerebral arteries do not exhibit hypertension-induced adaptive increases in myogenic tone and the resulting extension of cerebral blood flow autoregulation to high pressure values41,44. Dysregulation of pressure-induced activation of the 20-HETE–TRPC6 pathway has been reported to contribute to age-dependent loss of myogenic protection in hypertension41. Impaired functional adaptation of aged cerebral vessels to hypertension enables high blood pressure to penetrate the distal, injury-prone portion of the cerebral microcirculation39,41,44 (Fig. 1).
In healthy young individuals, the elastic conduit arteries, including the aorta and proximal large arteries, act as a buffering chamber that dampens haemodynamic pulsatility (known as the Windkessel effect) and facilitates continuous blood flow into the cerebral circulation48. Age-related stiffening of the elastic arteries impairs this buffering function and consequently leads to a significant increase in the amplitude of central pulse pressure49. Increased pulsatile pressure can then be readily transmitted into the brain and kidneys, which are characterized by a low hydrodynamic resistance50,51.
The relationship between arterial stiffening and hypertension is bi-directional as increased blood pressure promotes remodelling of the arterial wall. Mechanisms that contribute to vascular remodelling in hypertension include smooth muscle cell hypertrophy and hyperplasia, inflammation, fibrosis, alterations in collagen turnover and remodelling of the extracellular matrix (e.g. elastin degradation) due to changes in matrix metalloproteinases (MMPs)52. These processes are mediated by the renin–angiotensin system, transforming growth factor-β, inflammatory cytokines, endothelin, aldosterone, nitric oxide (NO) deficiency and oxidative stress13.
In older adults with hypertension, complex impairment of functional and structural adaptation to increased pulsatile pressure associated with hypertension probably results in a substantial decline in hydrodynamic resistance in the proximal larger resistance arteries, imposing a substantial burden on the vulnerable downstream portion of the cerebral microcirculation. Accordingly, in older adults increased pulsatile pressure waves are transmitted to the microcirculation, resulting in increased pulsatility of cerebral blood flow and consequential brain damage50,51. Preclinical studies demonstrate that in ageing, impaired myogenic adaptation of resistance arteries to pulsatile pressure may also enable high pressure to penetrate the distal portion of the cerebral microcirculation, contributing to microvascular damage53.
The mechanisms that contribute to age-related maladaptation of cerebral vessels to hypertension are likely to include an age-related decline in the circulating levels of a pleiotropic anabolic hormone54, insulin-like growth factor-1 (IGF1)40,55,56,57. IGF1 receptors are abundantly expressed on VSMCs and endothelial cells and IGF1 has multifaceted trophic and cytoprotective effects in the vasculature57. IGF1 promotes hyperplasia and hypertrophy of VSMCs, regulates smooth muscle contractility and extracellular matrix production, attenuates oxidative stress and protects endothelial function40,55,56. Experimental studies suggest that decreased circulating levels of IGF1 contribute to cerebrovascular ageing and age-related impairment of functional and structural adaptation of cerebral vessels to hypertension40,55,56,58. Mice that lack circulating IGF1 exhibit impaired myogenic adaptation to hypertension and impaired structural remodelling, mimicking the ageing phenotype40,55,56. Decreased circulating levels of IGF1 in humans are associated with an increased risk of hypertension-induced microvascular brain damage59 and stroke60.
Oxidative stress and cellular resilience
Transmission of higher blood pressure into the vulnerable distal portion of the brain microcirculation has been causally linked to cerebromicrovascular damage in older adults50. Higher pressure results in increased wall tension-related cellular stretch, which promotes oxidative stress in endothelial cells and VSMCs by inducing and upregulating NADPH oxidases61 and by upregulating the mitochondrial production of reactive oxygen species (ROS)62. Pressure-induced oxidative stress is exacerbated in ageing62,63 owing to an age-related impairment of cellular resilience to haemodynamic and oxidative stresses. Thus, exposure to the same level of intraluminal pressure results in significantly exacerbated oxidative stress and oxidative stress-related microvascular pathologies in aged brains compared with young brains41,62,63.
Impaired cellular resilience to oxidative stress is due, at least in part, to age-related dysfunction of nuclear factor erythroid 2-related (NRF2)-mediated homeostatic antioxidative defence pathways64,65. NRF2 is a transcription factor that is activated by ROS in the vascular cells of young organisms, leading to the upregulation of various antioxidant genes. Age-related dysfunction of NRF2-mediated free radical detoxification mechanisms in the vasculature is thought to lead to exacerbation of hypertension-induced oxidative stress and cellular injury34,65,66. Both cell-autonomous and non-cell-autonomous mechanisms of ageing, including age-related IGF1 deficiency67,68 and dysregulation of microRNAs (miRNAs) such as miR-144 (refs67,68), have been causally linked to NRF2 dysfunction and impaired cellular oxidative stress resistance in the vasculature. NRF2 also exerts potent anti-inflammatory effects by inhibiting NF-κB69 and promotes angiogenesis and maintenance of the capillary network70. Hypertension-induced pathologies of microvascular origin in which NRF2 dysfunction and exacerbated oxidative stress are likely to have a critical role include small vessel disease, BBB disruption, neuroinflammation and white matter damage, microhaemorrhages, capillary rarefaction and impaired microvascular dilation, which promotes ischaemic neuronal damage, as well as AD pathologies such as amyloid plaques and cerebral amyloid angiopathy71.
Small vessel disease
Hypertension causes complex pathological alterations to the cerebral microvessels (termed small vessel disease), including endothelial damage and dysfunction72, phenotypic changes of the VSMCs, lipohyalinosis, fibrinoid necrosis, pericyte injury41,73, pathological remodelling of the extracellular matrix and activation of MMPs63,73, microaneurysms, enlargement of perivascular spaces, perivascular oedema74, inflammation41,75,76,77 and parenchymal changes such as microhaemorrhages, lacunar infarcts, and white matter lesions (Fig. 2). Advances in MRI have enabled the identification of neuroradiological markers of cerebral small vessel disease, which include WMHs, lacunes, microhaemorrhages, abnormalities of cerebral blood flow and reduced fibre alignment (which can be seen using diffusion tensor imaging). These markers are associated with cognitive deficits78. However, an urgent need exists for further detailed studies that investigate the associations between neuroradiological markers and the histopathological features of cerebral small vessel disease78.
a | Hypertension and ageing promote microvascular injury, including damage to the extracellular matrix (ECM), smooth muscle cells, endothelial cells and pericytes. These effects lead to microvascular rupture, rarefaction and thrombosis as well as impaired vasodilation and blood–brain barrier dysfunction, which result in brain ischaemia and neuroinflammation. This damage is visible as microhaemorrhages, lacunar infarcts and white matter damage on MRI. b | Cerebral microhaemorrhages (arrows) visible on axial T2*-GRE MRI sequences in a 72-year-old man with chronic hypertension, a history of smoking and non-adherence to medical therapy who was admitted for hypertensive emergency with initial blood pressure readings of 230/126 mmHg. The cerebral microhaemorrhages involve the grey–white matter junction and deeper brain regions. c | Silent lacunar infarct (arrow) in the basal ganglia of a 74-year old woman with poorly controlled hypertension who was admitted for confusion. T1-weighted MRI. d | White matter hyperintensities in a 68-year-old man with diabetes mellitus and poorly controlled hypertension who underwent MRI of his head because of progressive worsening of his gait. MRI axial fluid-attenuated inversion recovery sequence image obtained using a 1.5-T field strength scanner.
White matter hyperintensities
The prevalence of brain WMHs increases with age. WMHs are a very common finding on the brain MRI of patients with hypertension aged >65 years (Fig. 2) and are associated with substantial cognitive impairment, a threefold increased risk of stroke and a twofold increased risk of dementia79. WMHs are predominantly localized to the periventricular and deep white matter, corresponding to widespread white matter damage caused by microvascular pathologies79. Knowledge of the pathologies that underlie the imaging findings derives mostly from post-mortem studies. The late stages of WMHs are thought to correspond to demyelination and axonal degeneration.
The mechanisms that contribute to white matter injury include endothelial activation, inflammation, gliosis and ischaemic damage78, all of which can be exacerbated by hypertension. An important role for BBB disruption in the pathogenesis of white matter damage has also been proposed80. This putative mechanism is particularly interesting in the context of hypertension, which promotes BBB disruption and thereby exacerbates neuroinflammation in the aged brain41. Early-stage WMHs often have a focal appearance, which is consistent with the concept that focal BBB disruption and the resulting development of inflammatory loci have a key role in their genesis. Importantly, the imaging findings that are associated with hypertension-induced small vessel disease (including WMHs and lacunes) are of a dynamic nature. As the lesions are inter-related because of their shared pathogenesis, acute small subcortical infarcts can disappear, remain as WMHs or form lacunar infarcts80.
Age and hypertension are the major risk factors for WMHs81,82. A prospective study demonstrated that duration of hypertension is associated with both periventricular and subcortical white matter lesions and that this association is strongly dependent on the age of the patients81. In this study, the prevalence of subcortical and periventricular WMHs increased by 0.2% and 0.4%, respectively, per year of age81. Among participants aged 60–70 years with >20 years of hypertension, the relative risks of subcortical and periventricular white matter lesions were 24.3 and 15.8, respectively, compared with normotensive individuals81. Interestingly, the locations of WMHs have been associated with cerebral amyloid burden, suggesting a shared pathophysiology83 (for example, BBB disruption and microglia activation). In individuals aged >65 years, increased central arterial stiffness and higher pressure and/or cerebral blood flow pulsatility were associated with increased incidence and volume of white matter damage84. Successful treatment of hypertension significantly reduces the risk of developing white matter lesions81. However, data from the Cardiovascular Determinants of Dementia study suggest that ischaemia due to episodes of hypotension in patients with chronic hypertension who receive aggressive blood pressure-lowering therapy might show increased development of white matter lesions8.
‘Silent’ brain infarcts
Advances in brain imaging techniques have led to the identification of brain infarcts in a large number of otherwise healthy elderly individuals who do not have a history of transient ischaemic attacks or clinical signs or symptoms of stroke. The prevalence of these ‘silent’ brain infarcts (also known as ‘covert’ brain infarcts) among healthy elderly people was reported to be >20%85. The vast majority of ‘silent’ brain infarcts (90%) are lacunar infarcts85,86. On cerebral MRI, both WMHs and lacunar infarcts are generally considered to be neuroradiological features of small vessel disease. Lacunar infarcts are thought to develop as a consequence of hypertension-related small vessel disease when progressive vessel stenoses and/or spontaneous thrombosis of terminal vessels supplying the deep white matter and basal ganglia (which lack a collateral network) result in focal ischaemic damage to the neural tissue of sufficient severity to produce a small area of necrosis78 (Fig. 2).
Although both lacunar infarcts and WMHs are viewed as signs of small vessel disease, their location and appearance (focal versus diffuse and widespread, respectively) are different. Lacunar infarcts are predominantly localized to the cerebral white matter and subcortical structures (that is, the basal ganglia, thalamus and brainstem). Moreover, only a moderate correlation exists between WMHs and lacunar infarcts, supporting the view that they are different manifestations of hypertension-induced microvascular damage78. Despite these differences, both WMHs and lacunar infarcts are independently associated with cognitive impairment in elderly patients86.
BBB disruption and neuroinflammation
The BBB is a functional part of the neurovascular unit that acts as an interface, separating the central nervous system from the circulation. As well as acting as a physical barrier, the BBB regulates selective transport of circulating factors into the fluid compartment of the brain parenchyma. Increasing evidence suggests that BBB disruption promotes neuroinflammation and myelin damage and, therefore, has a critical role in the pathogenesis of VCI and AD87,88 (Fig. 3). Hypertension, particularly in the context of ageing, promotes substantial BBB disruption41,77, which probably contributes to the exacerbation of VCI and AD in elderly patients with hypertension.
High intraluminal pressure induces increased production of reactive oxygen species (ROS) in the walls of cerebral microvessels. The resulting oxidative stress leads to structural damage to endothelial cells, pericyte injury and increased activation of matrix metalloproteinases (MMPs). Increased MMP activity leads to disruption of tight junctions and breakdown of the extracellular matrix (ECM), resulting in damage to the blood–brain barrier. The damaged blood–brain barrier enables plasma constituents to enter the brain parenchyma, promoting microglia activation, synaptic dysfunction and myelin breakdown. Hypertension-induced neuroinflammation also contributes to synaptic dysfunction and white matter damage. JAM, junctional adhesion molecule; ZO, zonula occludens proteins.
The mechanisms that contribute to hypertension-induced progressive BBB disruption are likely to be multifaceted and involve structural, cellular and molecular deficits in the neurovascular unit41. The main cellular components of the BBB are the cerebromicrovascular endothelial cells, pericytes and astrocytic endfeet89; non-cellular components include the basement membrane and endothelial glycocalyx90. Hypertension-induced microvascular injury involves increased oxidative stress and related structural damage to endothelial cells, changes in the extracellular matrix and pericyte injury41 (Fig. 3). In particular, hypertension-induced, oxidative stress-mediated changes in cerebromicrovascular endothelial cells have a critical role in BBB disruption91,92,93,94. Evidence suggests that activation of endothelial type-1 angiotensin II receptor in arterioles and venules and activation of perivascular macrophages also contribute to BBB disruption in hypertension95.
Tight junctions that interconnect the cerebromicrovascular endothelial cells help to maintain the low paracellular diffusion of solutes through the endothelial layer. Endothelial cells are also connected by adherens junctions, which are composed of cadherins, platelet endothelial cell adhesion molecule and junctional adhesion molecules. In hypertension, the expression of multiple junctional proteins is dysregulated and tight junctions show morphological changes91,92,93,94. Hypertension-induced oxidative stress in cerebral vessels has been causally linked to increased activity of MMPs in the vascular wall63. Moreover, increased MMP activity has been shown to disrupt tight junction proteins and break down the extracellular matrix in cerebral vessels96. Importantly, hypertension-induced oxidative stress, MMP activation and cerebromicrovascular endothelial injury are all exacerbated in ageing41.
In preclinical models, hypertension-induced damage to the endothelial glycocalyx97, the vascular extracellular matrix and the vascular basement membrane98 has been well documented. Pericytes are critical cellular constituents of the BBB87 and mouse models of isolated pericyte deficiency exhibit substantial BBB disruption99. Importantly, hypertension induces substantial pericyte loss, which is associated with BBB disruption in the mouse brain41; this disruption was exacerbated in aged mice. Pericytes also have a central role in maintenance of the architecture of the cerebral microcirculatory network100. Thus, hypertension-induced pericyte loss probably contributes to exacerbation of microvascular rarefaction in the aged brain41,58. Endothelial cells regulate pericyte proliferation and function (for example, via endothelial-derived platelet-derived growth factor (PDGF)-B signalling), and pericyte loss in pathological states is thought to be a consequence of endothelial dysfunction.
Other potential cellular and molecular mechanisms of ageing that exacerbate hypertension-induced microvascular damage and BBB disruption include impaired cellular stress resilience65, mitochondrial dysfunction101, mTOR signalling102, increased inflammation (including upregulation of components of the innate immune system)103, increased oxidative stress and senescent cells in the aged neurovascular unit104, and deficiency of circulating IGF156. In animal models of hypertension, significant BBB opening has been reported on the venular side105. In older adults arterial hypertension is frequently associated with elevated systemic venous pressure (for example, heart failure leads to venous congestion and a consequent increase in venous pressure termed ‘backward failure’), which has a synergistic role in the genesis of BBB disruption and neuroinflammation106.
The pathophysiological consequences of hypertension-induced BBB disruption include neuroinflammation, synapse loss and impairment of synaptic function41,88,107. A damaged BBB enables plasma constituents, including IgG, thrombin, fibrinogen and highly inflammatory pathogen-associated molecular patterns, to enter the brain parenchyma41 where they promote neuroinflammation by activating microglia108 (Fig. 3). Direct evidence of a critical role of haemodynamic factors in neuroinflammation has been provided by preclinical studies, which showed that arterial stiffness leads to microglia activation mediated by oxidative stress109. BBB disruption also results in increased presence of serum amyloid A in the brain, which also has a role in neuroinflammation and neurodegeneration110.
Considerable interaction occurs between the immune system and the autonomic nervous system. In particular, the sympathetic nervous system is a major contributor to the pathogenesis of hypertension. The sympathetic nervous system innervates the bone marrow, spleen and peripheral lymphatic system and its increased activity promotes immune activation, which has a role in the pathogenesis of hypertension-induced organ damage, including neuroinflammation and neurodegeneration111.
Increased neuroinflammation in hypertension is associated with impaired synaptic function107, information processing and neuronal connectivity, and is likely to contribute to neurodegeneration. Neuroinflammation might promote neuronal apoptosis, lead to reduced hippocampal neurogenesis, impair synaptic plasticity and result in loss of synaptic connections. Strong evidence implicates microglial activation and neuroinflammation in hippocampal and cortical dysfunction as well as in the development of AD-like pathologies in hypertensive mice75,76,112. Studies in animal models have shown that hypertension can upregulate chemokines and that infiltration of neutrophils into the central nervous system exacerbates AD pathology and cognitive decline.
Cerebral microhaemorrhages
Cerebral microhaemorrhages (also known as cerebral microbleeds) are small focal haemorrhages (<5 mm in diameter) that are associated with the rupture of small intracerebral vessels. These microhaemorrhages are visible on gradient echo T2* MRI sequences113 (Fig. 2). Hypertension associated with advanced age, cerebral amyloid angiopathy or AD114 are the major risk factors for cerebral microhaemorrhages113. The prevalence of cerebral microhaemorrhages correlates with the duration of hypertension exposure115 and is >50% among individuals older than 65 years113. CKD is also associated with an increased prevalence of cerebral microhaemorrhages, and experimental studies suggest that this effect might be at least partly due to elevated levels of urea that alter the cytoskeleton of endothelial cells and tight junction proteins116. Cerebral microhaemorrhages are clinically important because they exacerbate cognitive decline in older adults and patients with AD117. Experimental evidence suggests that hypertension promotes the development of cerebral microhaemorrhages by inducing oxidative stress and activating MMPs, leading to breakdown of the extracellular matrix in the vascular wall63 (Fig. 4).
In elderly patients, increased intraluminal pressure and consequential increases in wall tension activate NADPH oxidases (NOX) and promote mitochondria-derived production of reactive oxygen species (mtROS) in the vascular wall. Dysregulation of nuclear factor erythroid 2-related (NRF2)-mediated antioxidant defence mechanisms in the aged vasculature exacerbates pressure-induced oxidative stress. Vascular oxidative stress contributes to increased matrix metalloproteinase (MMP) activation, which promotes degradation of the extracellular matrix (ECM) and vascular smooth muscle cell (VSMC) atrophy. These structural changes weaken the microvascular wall and increase vulnerability to rupture and the formation of cerebral microhaemorrhages. Figure adapted with permission from ref.113, American Physiological Society.
In older adults, activities that result in substantial transient elevations in blood pressure represent a dynamic challenge to the impaired autoregulatory protection of the cerebral microcirculation, resulting in transmission of high pressure waves to the vulnerable downstream microvessels and promoting the development of microhaemorrhages. Accordingly, use of the Valsalva manoeuvre, which results in transient increases in blood pressure during daily activities in which straining is present (e.g. lifting heavy weights, sexual intercourse, heavy coughing and defecation straining), has been causally linked to the development of microhaemorrhages in older individuals118.
Cerebral microhaemorrhages are also prevalent in older patients with COVID-19, probably because of SARS-CoV-2-induced endothelial inflammation and consequential increases in microvascular fragility119,120,121. Further studies are needed to determine whether convalescent older patients suffering from the late sequelae of COVID-19 have persisting microvascular fragility and are at an increased risk of developing high blood pressure-induced microhaemorrhages. If this is the case, effective blood pressure control and lifestyle adjustments (including avoiding activities that result in sudden increases in blood pressure) should be an important part of the management of patients with chronic COVID syndrome (also known as long COVID or long-haul COVID).
Capillary rarefaction
The brain is the most metabolically active organ and its adequate function relies on a continuous supply of nutrients and oxygen through a dense capillary network. Strong evidence indicates that hypertension results in cerebromicrovascular rarefaction, which contributes to decreased cerebral blood flow, compromising nutrient and oxygen delivery as well as the removal of waste products generated by neural signalling, and thus exacerbating cognitive impairment58,73. Moreover, ageing increases hypertension-induced capillary loss63. Hypertension-induced microvascular rarefaction has also been observed in the retina122, heart123, skin and skeletal muscle124. We assume that the same cellular and molecular mechanisms are responsible for hypertension-induced microvascular rarefaction in each of these vascular beds. Studies that used human nailfold capillaroscopy combined with dynamic measurements showed that decreased capillary density is associated with increased capillary pressure in untreated patients with hypertension125,126. Based on the available evidence, we posit that hypertension-induced microvascular rarefaction in the brain is a consequence of transmission of high pressure into the cerebral microcirculation.
The mechanisms that contribute to high pressure-induced capillary loss are likely to be multifaceted and may involve endothelial apoptosis, oxidative stress, pericyte damage and an imbalance in the production of pro-angiogenic and anti-angiogenic factors in the tissues (for example, owing to pericyte damage)41,58,127 (Fig. 5). The cerebral microcirculation exhibits high plasticity, and an imbalance between capillary regression and growth probably also contributes to cerebromicrovascular rarefaction127. Importantly, ageing has been shown to impair the angiogenic capacity of endothelial cells127,128. Age-related mechanisms that may promote dysregulation of endothelial angiogenic capacity may include deficiency of the pro-angiogenic trophic factors IGF1 (ref.58) and pituitary adenylate cyclase-activating polypeptide (PACAP)129,130, NAD+ deficiency and increased oxidative stress128, dysregulation of angiogenic miRNA expression131, age-related dysfunction of cytoprotective NRF2-regulated pathways65,70 and increased endothelial senescence104,132. Age-related impairment of endothelial angiogenic capacity is likely to be a critical factor that contributes to the exacerbation of hypertension-induced capillary loss in ageing63. The potential roles of increased precapillary arteriolar constriction, cessation of capillary blood flow, increased susceptibility to microemboli, platelet adhesion and macrophage activation in hypertension-induced capillary loss should also be considered.
Both hypertension and ageing promote capillary regression and impair angiogenesis. These effects exacerbate cerebromicrovascular rarefaction and compromise cerebral blood supply. The contributing mechanisms include increased oxidative stress-mediated cellular damage and endothelial cell apoptosis, pericyte injury, reduced angiogenic capacity of cerebromicrovascular endothelial cells and dysregulation of promoters and inhibitors of angiogenesis.
Impaired neurovascular coupling
Neurovascular coupling (also known as functional hyperaemia) is a critical homeostatic mechanism that ensures prompt adjustment of cerebral blood flow to the increased energy and O2 demand of active brain regions13. Neurovascular coupling is orchestrated by the interaction of activated neurons and astrocytes with cerebromicrovascular endothelial cells, VSMCs and pericytes. The mechanisms that elicit vasodilation include endothelial release of NO (probably stimulated by astrocyte-derived ATP133), astrocytic release of eicosanoid mediators and K+ mediated activation of potassium channels in VSMCs13. Pathophysiological states that compromise cerebromicrovascular health adversely affect neurovascular coupling, resulting in impaired delivery of oxygen and nutrients as well as inadequate wash-out of metabolic by-products. Experimental studies have provided evidence that a causal link exists between impaired neurovascular coupling and cognitive impairment134. Accordingly, pharmacological interventions that rescue neurovascular coupling responses have beneficial effects on cognitive function in mouse models of ageing135 and AD136,137.
Experimental studies have demonstrated that hypertension results in substantial impairment of endothelium-mediated neurovascular coupling responses owing, at least in part, to increased NADPH oxidase-derived production of ROS and a consequential reduction in the bioavailability of endothelial NO in the neurovascular unit13,138,139,140,141 (Fig. 6). Clinical investigations confirm that neurovascular coupling responses are impaired in patients with hypertension142. High levels of angiotensin II, a key mediator of hypertension, might cause neurovascular uncoupling via increased production of ROS140. In addition, evidence from studies using mouse models of carotid calcification indicates that increased pulsatile pressure owing to arterial stiffness causes neurovascular dysfunction143. Current studies also suggest that hypertension-induced BBB disruption promotes activation of perivascular macrophages, which contribute to neurovascular dysfunction by producing ROS via NADPH oxidases144. Hypertension induces microcirculatory endothelial dysfunction in the peripheral circulation145 and this effect has been causally linked to pressure-induced NADPH oxidase activation in the vascular wall146,147. In humans, endothelial function in the peripheral circulation can be improved by antihypertensive treatments such as losartan148. However, studies in spontaneously hypertensive rats suggest that established hypertension-induced neurovascular dysfunction is more difficult to reverse using antihypertensive therapy149.
Synergistic hypertension-induced and ageing-induced alterations in cerebromicrovascular endothelial cell function and endothelium-dependent neurovascular coupling mechanisms contribute to impaired functional hyperaemia and promote cognitive decline in elderly patients with hypertension. In the healthy brain, a complex interaction between neurons, astrocytes and cerebromicrovascular endothelial cells ensures adequate cerebral blood flow at all times. Neurotransmitters such as glutamate that are released from active excitatory synapses elicit elevations of intracellular Ca2+ concentration in astrocytes via G protein-coupled receptors (GPCRs), initiating the propagation of calcium waves through the processes and soma of the astrocyte to the end-feet, which are wrapped around the resistance arterioles. The surge in astrocyte end-feet Ca2+ concentration promotes ATP release and the cytochrome P450 (CYP450)-mediated and cyclooxygenase (COX)-mediated production of vasodilator eicosanoids (epoxyeicosatrienoic acids (EETs)) and prostaglandins (such as prostaglandin E2 (PGE2)), respectively. Astrocyte-derived ATP promotes endothelial release of the vasodilator nitric oxide (NO) via activation of P2Y purinoceptor 1 (P2Y1)133. High blood pressure and ageing promote the production of mitochondrial reactive oxygen species (mtROS)62,153,186 as well as ROS production by NADPH oxidases (NOX)61,72,139,140. The resulting oxidative stress impairs the bioavailability of endothelial NO and thereby impairs vasodilation, resulting in impairment of functional hyperaemia. Further research is needed to investigate the potential effects of ageing and hypertension on astrocytic regulation of pericyte function and capillary dilation. K+IR, inward rectifier potassium channel; VSMC, vascular smooth muscle cell. Figure adapted with permission from ref.39, American Physiological Society.
Evidence suggests that neurovascular coupling may be similarly affected by hypertension and biological ageing43. Both hypertension and ageing are associated with upregulation of NADPH oxidases, increased cerebrovascular oxidative stress and endothelial dysfunction43,61,150,151. Thus, the neurovascular effects of hypertension are likely to be exacerbated in older individuals. Additional mechanisms by which ageing promotes endothelial dysfunction and impairs neurovascular coupling include cellular NAD+ depletion135,152 and increased mitochondria-derived ROS production153. Hypertension might also exert synergistic effects on these pathways154. Hypertension-induced neurovascular dysfunction, superimposed on age-related microvascular pathologies, probably results in a critical mismatch between supply and demand of oxygen and metabolic substrates, and thereby exacerbates cognitive decline13.
Alzheimer’s disease pathologies
Hypertension is a major vascular risk factor that exacerbates the pathogenesis of AD and worsens the outcome of the disease155. In individuals aged >65 years, hypertension doubles the risk of AD5,6. Post-mortem histological analyses of the brains of 243 participants of a population-based, longitudinal study demonstrated that elevated SBP (≥160 mmHg) in midlife was associated with brain atrophy and increased numbers of neuritic plaques in the neocortex and hippocampus; increased DBP (≥95 mmHg) in midlife was associated with greater numbers of neurofibrillary tangles in the hippocampus7. In mouse models, hypertension has been shown to exacerbate AD pathologies, including the development of neuritic plaques and vascular Aβ deposits75,76,112. Studies in hypertensive mice with transverse aortic coarctation showed that Aβ deposits are detectable in the mouse brain as early as 4 weeks after induction of hypertension, providing proof-of-concept for a key role of high intraluminal pressure in the pathogenesis of AD76. In addition, Ang II administration increased beta-secretase activity and the rate of cleavage of the Aβ protein precursor in mice138. Emerging evidence suggests that hypertension-induced small vessel disease promotes tauopathy independently of Aβ accumulation, indicating that hypertension is an independent risk factor for increased tau burden156.
The mechanisms by which hypertension exacerbates the progression of AD are likely to include increased oxidative microvascular damage and brain inflammation75,76,138 (Fig. 7). Both ageing and hypertension promote activation of NADPH oxidase in the cerebral vasculature, which is probably a key cellular mechanism by which ageing and hypertension synergistically promote AD pathogenesis13,61,72,140,141,144. The current understanding is that hypertension exacerbates neuroinflammation in the aged brain by promoting BBB disruption and consequential microglia activation41, both of which are important manifestations of AD87,157. Evidence suggests that AD pathologies impair cerebral autoregulation158, which might represent a potential feed-forward mechanism that contributes to accelerated progression of AD in hypertension.
Alzheimer’s disease is, in part, a microvascular disorder characterized by deposition of the toxic β-amyloid peptide (Aβ) in the brain. This deposition compromises the neurovascular unit and causes multifaceted cerebromicrovascular impairment157,191. Hypertension may exacerbate the progression of Alzheimer’s disease by exerting synergistic deleterious effects on cells of the neurovascular unit that are already stressed by overproduction of Aβ. Hypertension exacerbates microvascular damage in Alzheimer’s disease and promotes blood–brain barrier disruption and consequential microglia activation, which lead to amyloid plaque formation and neuronal toxicity. In addition, hypertension promotes neurovascular uncoupling and exacerbates capillary atrophy and regression resulting in ghost vessel formation and impaired cerebral blood flow. Perivascular amyloid accumulation facilitated by endothelial damage and Aβ toxicity results in structural damage in arterioles, which promotes the development of microhaemorrhages. Together, these effects contribute to brain dysfunction.
Cerebral amyloid angiopathy is a critical risk factor for cerebral microhaemorrhages113. The prevalence of cerebral microhaemorrhages in patients with AD is ~40%113,114. These patients often have multiple cerebral microhaemorrhages, which contribute to progressive impairment of cognitive function113. Studies in mouse models of AD have demonstrated that amyloid pathologies and comorbid hypertension have synergistic effects that exacerbate the genesis of cerebral microhaemorrhages159.
The glymphatic (also known as glial-lymphatic) system is a brain-wide cerebrospinal fluid clearance pathway that uses the arteriolar perivascular space for fast inflow of cerebrospinal fluid into the brain interstitium, and the venous perivascular spaces for clearing solutes from the neuropil into meningeal and cervical lymphatic drainage vessels160. Dysfunction of the glymphatic pathway has been linked to impaired clearance of harmful metabolites, including Aβ160. Hypertension impairs glymphatic transport kinetics in rat models161, suggesting that impaired glymphatic clearance of Aβ might contribute to hypertension-induced exacerbation of AD pathologies.
Prevention of cognitive decline
Importantly, hypertension is a treatable risk factor for cognitive decline, VCI and AD162. Numerous clinical trials, including the Syst-Eur4 and HYVET163 studies, have shown that antihypertensive therapies, including angiotensin-converting enzyme (ACE) inhibitors, are effective not only in preventing major cerebrovascular events71 but also in reducing the incidence and/or delaying the progression of cognitive decline162,164. The Syst-Eur trial investigators concluded that if 1,000 patients with hypertension were treated with antihypertensive drugs for 5 years, 19 cases of dementia might be prevented4. The PROGRESS trial showed that treatment with a long-acting ACE inhibitor, perindopril, and a thiazide-like diuretic, indapamide, was associated with reduced risks of dementia and cognitive decline at a mean follow-up of 3.9 years165. In addition, clinical trials and experimental studies suggest that antihypertensive medications, including ACE inhibitors, angiotensin I receptor blockers and diuretics, may improve AD biomarkers (such as Aβ neuropathology, cerebral blood flow and inflammatory markers), and reduce the incidence and/or delay the progression of AD166.
A meta-analysis that included 12 randomized controlled trials with 92,135 participants, showed that blood pressure lowering with antihypertensive drugs was associated with a reduced risk of incident dementia or cognitive impairment167. This meta-analysis highlighted a key problem: the association of hypertension with neurocognitive syndromes, mediated through chronic cerebromicrovascular pathological alterations, has an extended time lag between cause and clinical consequence. Observational studies with extended follow-up periods (>10 years) are therefore required to evaluate the effects of anti-hypertensive treatments on neurocognitive outcomes. Taken together, the existing evidence strongly suggests that effective control of hypertension offers an opportunity to delay and possibly prevent the pathogenesis of VCI and dementia, and AD.
Notably, antihypertensive drugs might exert class-specific effects on cognition168. Both calcium channel blockers and ACE inhibitors have been reported to delay cognitive impairment166. However, data from the Canadian Study of Health and Aging suggest that individuals aged ≥65 years who were treated with calcium channel blockers had a steeper cognitive decline during a 5-year follow-up period than those who were treated with other antihypertensive medications169. These findings are particularly interesting because an increasing body of evidence suggests differential responses of the circulating and tissue renin–angiotensin systems to different antihypertensive classes170. Furthermore, calcium antagonists have the potential to impair myogenic autoregulatory protection of the cerebral microcirculation. Taking these factors into consideration, ACE inhibitors and drugs that block angiotensin receptors might be preferable to calcium channel blockers for dementia prevention in individuals with hypertension.
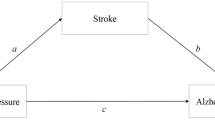
Hypertension is also a major risk factor for stroke, which doubles the risk of developing dementia171. Estimates suggest that a third of dementia cases could be prevented by preventing stroke171. Clinical trials have shown that prevention of stroke using anticoagulation in patients with atrial fibrillation and blood pressure-lowering therapies in patients with hypertension can significantly reduce the risk of dementia172. Based on these findings, the World Stroke Organization has issued a manifesto calling for the joint prevention of stroke and dementia171.
The optimal SBP targets for prevention of dementia are a subject of debate. The SPRINT trial showed that in ambulatory adults with hypertension, more intensive blood pressure control (target SBP of <120 mmHg versus <140 mmHg) did not result in significant cognitive benefits173. An important factor to consider is that, owing to the adaptive rightward shift of the cerebral autoregulatory curve in hypertension, aggressive lowering of perfusion pressure might result in cerebral hypoperfusion and consequential negative effects on the brain. U-shaped associations between blood pressure and cognitive function in elderly patients have been reported in several studies174,175, consistent with the concept that blood pressure that is too low in old age is a risk factor for cognitive impairment176. These findings draw attention to potential risks associated with overtreating hypertension in elderly patients and highlight the importance of individualized blood pressure management for prevention of cognitive impairment.
Future perspectives
Optimization of blood pressure in patients with hypertension is expected to have a substantial public health impact owing to prevention of VCI and AD, even in the short term. Diurnal blood pressure loads are associated with lower cognitive performance in hypertensive adults aged 60–75 years, highlighting the importance of controlling blood pressure variability177. Combinations of pharmaceutical treatments and lifestyle interventions that lower blood pressure together with interventions that reduce blood pressure variability and prevent sudden surges in systolic pressure should be assessed in randomized clinical trials with clearly designed cognitive end points. In particular, trials of combination treatments that have long periods of follow-up and investigate microvascular end points as well as cognition as primary outcome measures will be very informative. Systematic, standardized neurocognitive testing of patients enrolled in these studies is also important.
Older patients with hypertension might also benefit from therapies that specifically target microvascular contributions to VCI and/or AD. Strategies that reverse cerebromicrovascular rarefaction, prevent small vessel rupture and the genesis of microhaemorrhages and protect the BBB are still in their infancy. Although preclinical and clinical data suggest that calcium antagonists, ACE inhibitors and Ang II receptor blockers might have protective effects on microvessel structure and microvascular network architecture in the peripheral circulation178, further studies are needed to test their effects, alone or in combination, on the cerebral microcirculation of patients with hypertension. Re-purposing existing drugs with microvascular protective effects (such as statins and metformin) and targeting promising novel molecular pathways and mechanisms involved in cerebromicrovascular ageing that have been identified by geroscience research might also help to improve cognitive health in older adults with hypertension.
The National Institutes of Health and other organizations have made it a priority to fund research into microvascular contributions to the pathogenesis of VCI and AD, including the role of hypertension-induced microvascular damage. New therapeutic strategies aimed at reversing ageing-induced and hypertension-induced cardiovascular and cerebromicrovascular impairment include use of mitochondrial antioxidants153,179, polyphenols and other activators of NRF2 and sirtuin 1 (refs150,180), senolytics181,182,183,184, anti-inflammatory interventions185, agents that rescue cellular energetics128,186 and/or prevent cellular NAD+ depletion135,152, AMPK activators187 and mTOR inhibitors188.
Conclusions
In summary, hypertension compromises the structural integrity, network architecture and function of the ageing cerebral microcirculation, promoting microvascular rarefaction, neurovascular dysfunction, BBB disruption, genesis of cerebral microhaemorrhages, lacunar infarcts and white matter damage, all of which exacerbate cognitive decline. Clinicians who treat patients with hypertension need to be aware of the increased risks of VCI and AD that are associated with high blood pressure. Given the high prevalence of hypertension in the ageing populations of many countries worldwide, adequate blood pressure control could reduce the incidence of cognitive impairment, which is a major cause of chronic cumulative disability. Targeting the cellular and molecular mechanisms that underlie hypertension-induced cerebromicrovascular impairment and are involved in the onset and progression of VCI and AD could have a critical role in preserving brain health and protecting cognitive function in high-risk older adults with hypertension.
References
Hurd, M. D., Martorell, P., Delavande, A., Mullen, K. J. & Langa, K. M. Monetary costs of dementia in the United States. N. Engl. J. Med. 368, 1326–1334 (2013).
Wimo, A. et al. The worldwide economic impact of dementia 2010. Alzheimers Dement. 9, 1–11.e3 (2013).
Iadecola, C. et al. Impact of hypertension on cognitive function: a scientific statement from the American Heart Association. Hypertension 68, e67–e94 (2016).
Forette, F. et al. Prevention of dementia in randomised double-blind placebo-controlled Systolic Hypertension in Europe (Syst-Eur) trial. Lancet 352, 1347–1351 (1998).
Launer, L. J. et al. Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol. Aging 21, 49–55 (2000).
Israeli-Korn, S. D. et al. Hypertension increases the probability of Alzheimer’s disease and of mild cognitive impairment in an Arab community in northern Israel. Neuroepidemiology 34, 99–105 (2010).
Petrovitch, H. et al. Midlife blood pressure and neuritic plaques, neurofibrillary tangles, and brain weight at death: the HAAS. Honolulu-Asia aging Study. Neurobiol. Aging 21, 57–62 (2000).
van Dijk, E. J. et al. The association between blood pressure, hypertension, and cerebral white matter lesions: cardiovascular determinants of dementia study. Hypertension 44, 625–630 (2004).
Baker, A. B., Resch, J. A. & Loewenson, R. B. Hypertension and cerebral atherosclerosis. Circulation 39, 701–710 (1969).
James, P. A. et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 311, 507–520 (2014).
Fryar, C. D., Ostchega, Y., Hales, C. M., Zhang, G. & Kruszon-Moran, D. Hypertension Prevalence and Control among Adults: United States 2015-1026. NCHS data brief, no 289 (National Center for Health Statistics, 2017).
Muntner, P. et al. Potential U.S. Population Impact of the 2017 ACC/AHA High Blood Pressure Guideline. J. Am. Coll. Cardiol. 71, 109–118 (2018).
Iadecola, C. & Gottesman, R. F. Neurovascular and cognitive dysfunction in hypertension. Circ. Res. 124, 1025–1044 (2019).
Wilkie, F. L., Eisdorfer, C. & Nowlin, J. B. Memory and blood pressure in the aged. Exp. Aging Res. 2, 3–16 (1976).
Kennelly, S. P., Lawlor, B. A. & Kenny, R. A. Blood pressure and dementia — a comprehensive review. Ther. Adv. Neurol. Disord. 2, 241–260 (2009).
Whitmer, R. A., Sidney, S., Selby, J., Johnston, S. C. & Yaffe, K. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 64, 277–281 (2005).
Kivipelto, M. et al. Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ 322, 1447–1451 (2001).
Walker, K. A. et al. Association of midlife to late-life blood pressure patterns with incident dementia. JAMA 322, 535–545 (2019).
Skoog, I. et al. 15-year longitudinal study of blood pressure and dementia. Lancet 347, 1141–1145 (1996).
Qiu, C., von Strauss, E., Fastbom, J., Winblad, B. & Fratiglioni, L. Low blood pressure and risk of dementia in the Kungsholmen project: a 6-year follow-up study. Arch. Neurol. 60, 223–228 (2003).
Li, G. et al. Age-varying association between blood pressure and risk of dementia in those aged 65 and older: a community-based prospective cohort study. J. Am. Geriatr. Soc. 55, 1161–1167 (2007).
Yoshitake, T. et al. Incidence and risk factors of vascular dementia and Alzheimer’s disease in a defined elderly Japanese population: the Hisayama Study. Neurology 45, 1161–1168 (1995).
Posner, H. B. et al. The relationship of hypertension in the elderly to AD, vascular dementia, and cognitive function. Neurology 58, 1175–1181 (2002).
Lopez, O. L. et al. Risk factors for mild cognitive impairment in the cardiovascular health study cognition study: part 2. Arch. Neurol. 60, 1394–1399 (2003).
Hestad, K., Engedal, K., Schirmer, H. & Strand, B. H. The effect of blood pressure on cognitive performance. an 8-year follow-up of the tromso study, comprising people aged 45–74 years. Front. Psychol. 11, 607 (2020).
Swan, G. E. et al. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology 51, 986–993 (1998).
Mills, K. T. et al. Global Disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 134, 441–450 (2016).
Chin, A. L., Negash, S. & Hamilton, R. Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer disease. Alzheimer Dis. Assoc. Disord. 25, 187–195 (2011).
Ferri, C. P. et al. Global prevalence of dementia: a Delphi consensus study. Lancet 366, 2112–2117 (2005).
Levine, D. A. et al. Association between blood pressure and later-life cognition among black and white individuals. JAMA Neurol. 77, 810–819 (2020).
Mills, K. T., Stefanescu, A. & He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 16, 223–237 (2020).
Noh, J. et al. Prevalence of comorbidity among people with hypertension: The Korea National Health and Nutrition Examination Survey 2007–2013. Korean Circ. J. 46, 672–680 (2016).
Trauernicht, A. K., Sun, H., Patel, K. P. & Mayhan, W. G. Enalapril prevents impaired nitric oxide synthase-dependent dilatation of cerebral arterioles in diabetic rats. Stroke 34, 2698–2703 (2003).
Tarantini, S. et al. Nrf2 deficiency exacerbates obesity-induced oxidative stress, neurovascular dysfunction, blood brain barrier disruption, neuroinflammation, amyloidogenic gene expression and cognitive decline in mice, mimicking the aging phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 73, 853–863 (2018).
Tucsek, Z. et al. Obesity in aging exacerbates blood brain barrier disruption, neuroinflammation and oxidative stress in the mouse hippocampus: effects on expression of genes involved in beta-amyloid generation and Alzheimer’s disease. J. Gerontol. A Biol. Sci. Med. Sci. 69, 1212–1226 (2014).
Valcarcel-Ares, M. N. et al. Obesity in aging exacerbates neuroinflammation, dysregulating synaptic function-related genes and altering eicosanoid synthesis in the mouse hippocampus: potential role in impaired synaptic plasticity and cognitive decline. J. Gerontol. A Biol. Sci. Med. Sci. 74, 290–298 (2018).
Viggiano, D. et al. Mechanisms of cognitive dysfunction in CKD. Nat. Rev. Nephrol. 16, 452–469 (2020).
Hooghiemstra, A. M. et al. Frequent cognitive impairment in patients with disorders along the heart-brain axis. Stroke 50, 3369–3375 (2019).
Toth, P., Tarantini, S., Csiszar, A. & Ungvari, Z. Functional vascular contributions to cognitive impairment and dementia: mechanisms and consequences of cerebral autoregulatory dysfunction, endothelial impairment, and neurovascular uncoupling in aging. Am. J. Physiol. Heart Circ. Physiol. 312, H1–H20 (2017).
Fulop, G. A. et al. IGF-1 deficiency promotes pathological remodeling of cerebral arteries: a potential mechanism contributing to the pathogenesis of intracerebral hemorrhages in aging. J. Gerontol. A Biol. Sci. Med. Sci. 74, 446–454 (2018).
Toth, P. et al. Age-related autoregulatory dysfunction and cerebromicrovascular injury in mice with angiotensin II-induced hypertension. J. Cereb. Blood Flow. Metab. 33, 1732–1742 (2013).
Harder, D. R., Smeda, J. & Lombard, J. Enhanced myogenic depolarization in hypertensive cerebral arterial muscle. Circ. Res. 57, 319–322 (1985).
Iadecola, C., Park, L. & Capone, C. Threats to the mind: aging, amyloid, and hypertension. Stroke 40, S40–S44 (2009).
Toth, P. et al. Role of 20-HETE, TRP channels and BKCa in dysregulation of pressure-induced Ca2+ signaling and myogenic constriction of cerebral arteries in aged hypertensive mice. Am. J. Physiol. Heart Circ. Physiol. 305, H1698–H1708 (2013).
Choi, S. K., Yeon, S. I., Kwon, Y., Byeon, S. & Lee, Y. H. Involvement of epithelial Na+ channel in the elevated myogenic response in posterior cerebral arteries from spontaneously hypertensive rats. Sci. Rep. 7, 45996 (2017).
Diaz-Otero, J. M. et al. Mineralocorticoid receptor antagonism improves parenchymal arteriole dilation via a TRPV4-dependent mechanism and prevents cognitive dysfunction in hypertension. Am. J. Physiol. Heart Circ. Physiol. 315, H1304–H1315 (2018).
Jarajapu, Y. P. & Knot, H. J. Relative contribution of Rho kinase and protein kinase C to myogenic tone in rat cerebral arteries in hypertension. Am. J. Physiol. Heart Circ. Physiol. 289, H1917–H1922 (2005).
Tomoto, T., Sugawara, J., Nogami, Y., Aonuma, K. & Maeda, S. The influence of central arterial compliance on cerebrovascular hemodynamics: insights from endurance training intervention. J. Appl. Physiol. 119, 445–451 (2015).
Diaz-Otero, J. M., Garver, H., Fink, G. D., Jackson, W. F. & Dorrance, A. M. Aging is associated with changes to the biomechanical properties of the posterior cerebral artery and parenchymal arterioles. Am. J. Physiol. Heart Circ. Physiol. 310, H365–H375 (2016).
Webb, A. J. et al. Increased cerebral arterial pulsatility in patients with leukoaraiosis: arterial stiffness enhances transmission of aortic pulsatility. Stroke 43, 2631–2636 (2012).
Mitchell, G. F. et al. Arterial stiffness, pressure and flow pulsatility and brain structure and function: the Age, Gene/Environment Susceptibility — Reykjavik study. Brain 134, 3398–3407 (2011).
Brown, I. A. M. et al. Vascular smooth muscle remodeling in conductive and resistance arteries in hypertension. Arterioscler. Thromb. Vasc. Biol. 38, 1969–1985 (2018).
Springo, Z. et al. Aging impairs myogenic adaptation to pulsatile pressure in mouse cerebral arteries. J. Cereb. Blood Flow. Metab. 35, 527–530 (2015).
Ascenzi, F. et al. Effects of IGF-1 isoforms on muscle growth and sarcopenia. Aging Cell 18, e12954 (2019).
Tarantini, S. et al. Insulin-like growth factor 1 deficiency exacerbates hypertension-induced cerebral microhemorrhages in mice, mimicking the aging phenotype. Aging Cell 16, 469–479 (2017).
Toth, P. et al. IGF-1 deficiency impairs cerebral myogenic autoregulation in hypertensive mice. J. Cereb. Blood Flow. Metab. 34, 1887–1897 (2014).
Sonntag, W. E. et al. Insulin-like growth factor-1 in CNS and cerebrovascular aging. Front. Aging Neurosci. 5, 27 (2013).
Tarantini, S. et al. Circulating IGF-1 deficiency exacerbates hypertension-induced microvascular rarefaction in the mouse hippocampus and retrosplenial cortex: implications for cerebromicrovascular and brain aging. Age 38, 273–289 (2016).
Angelini, A. et al. Insulin-like growth factor-1 (IGF-1): relation with cognitive functioning and neuroimaging marker of brain damage in a sample of hypertensive elderly subjects. Arch. Gerontol. Geriatr. 49 (Suppl 1), 5–12 (2009).
Johnsen, S. P. et al. Insulin-like growth factor (IGF) I, -II, and IGF binding protein-3 and risk of ischemic stroke. J. Clin. Endocrinol. Metab. 90, 5937–5941 (2005).
Park, L., Anrather, J., Girouard, H., Zhou, P. & Iadecola, C. Nox2-derived reactive oxygen species mediate neurovascular dysregulation in the aging mouse brain. J. Cereb. Blood Flow. Metab. 27, 1908–1918 (2007).
Springo, Z. et al. Aging exacerbates pressure-induced mitochondrial oxidative stress in mouse cerebral arteries. J. Gerontol. A Biol. Sci. Med. Sci 70, 1355–1359 (2015).
Toth, P. et al. Aging exacerbates hypertension-induced cerebral microhemorrhages in mice: role of resveratrol treatment in vasoprotection. Aging Cell 14, 400–408 (2015).
Ungvari, Z. et al. Vascular oxidative stress in aging: a homeostatic failure due to dysregulation of Nrf2-mediated antioxidant response. Am. J. Physiol. Heart Circ. Physiol. 301, H363–H372 (2011).
Ungvari, Z. et al. Nrf2 dysfunction and impaired cellular resilience to oxidative stressors in the aged vasculature: from increased cellular senescence to the pathogenesis of age-related vascular diseases. Geroscience 41, 727–738 (2019).
Fulop, G. A. et al. Nrf2 deficiency in aged mice exacerbates cellular senescence promoting cerebrovascular inflammation. Geroscience 40, 513–521 (2018).
Bailey-Downs, L. C. et al. Liver-specific knockdown of IGF-1 decreases vascular oxidative stress resistance by impairing the Nrf2-dependent antioxidant response: a novel model of vascular aging. J. Gerontol. A Biol. Sci. Med. Sci. 67, 313–329 (2012).
Csiszar, A. et al. Caloric restriction confers persistent anti-oxidative, pro-angiogenic, and anti-inflammatory effects and promotes anti-aging miRNA expression profile in cerebromicrovascular endothelial cells of aged rats. Am. J. Physiol. Heart Circ. Physiol. 307, H292–H306 (2014).
Ungvari, Z. et al. Age-associated vascular oxidative stress, Nrf2 dysfunction and NF-kB activation in the non-human primate Macaca mulatta. J. Gerontol. A Biol. Sci. Med. Sci. 66, 866–875 (2011).
Valcarcel-Ares, M. N. et al. Disruption of Nrf2 signaling impairs angiogenic capacity of endothelial cells: implications for microvascular aging. J. Gerontol. A Biol. Sci. Med. Sci. 67, 821–829 (2012).
Gorelick, P. B. et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42, 2672–2713 (2011).
Girouard, H., Park, L., Anrather, J., Zhou, P. & Iadecola, C. Cerebrovascular nitrosative stress mediates neurovascular and endothelial dysfunction induced by angiotensin II. Arterioscler. Thromb. Vasc. Biol. 27, 303–309 (2007).
Suzuki, K., Masawa, N., Sakata, N. & Takatama, M. Pathologic evidence of microvascular rarefaction in the brain of renal hypertensive rats. J. Stroke Cerebrovasc. Dis. 12, 8–16 (2003).
Jimenez-Balado, J. et al. Prevalence of hippocampal enlarged perivascular spaces in a sample of patients with hypertension and their relation with vascular risk factors and cognitive function. J. Neurol. Neurosurg. Psychiatry 89, 651–656 (2018).
Carnevale, D. et al. Role of neuroinflammation in hypertension-induced brain amyloid pathology. Neurobiol. Aging 33, 205.e19–e29 (2012).
Carnevale, D. et al. Hypertension induces brain β-amyloid accumulation, cognitive impairment, and memory deterioration through activation of receptor for advanced glycation end products in brain vasculature. Hypertension 60, 188–197 (2012).
Zhang, M., Mao, Y., Ramirez, S. H., Tuma, R. F. & Chabrashvili, T. Angiotensin II induced cerebral microvascular inflammation and increased blood-brain barrier permeability via oxidative stress. Neuroscience 171, 852–858 (2010).
Jorgensen, D. R. et al. A population neuroscience approach to the study of cerebral small vessel disease in midlife and late life: an invited review. Am. J. Physiol. Heart Circ. Physiol. 314, H1117–H1136 (2018).
Alber, J. et al. White matter hyperintensities in vascular contributions to cognitive impairment and dementia (VCID): knowledge gaps and opportunities. Alzheimers Dement. 5, 107–117 (2019).
Wardlaw, J. M., Valdes Hernandez, M. C. & Munoz-Maniega, S. What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J. Am. Heart Assoc. 4, 001140 (2015).
de Leeuw, F. E. et al. Hypertension and cerebral white matter lesions in a prospective cohort study. Brain 125, 765–772 (2002).
Guevarra, A. C. et al. Age moderates associations of hypertension, white matter hyperintensities, and cognition. J. Alzheimers Dis. 75, 1351–1360 (2020).
Weaver, N. A. et al. Cerebral amyloid burden is associated with white matter hyperintensity location in specific posterior white matter regions. Neurobiol. Aging 84, 225–234 (2019).
Tsao, C. W. et al. Relations of arterial stiffness and endothelial function to brain aging in the community. Neurology 81, 984–991 (2013).
Vermeer, S. E., Longstreth, W. T. Jr. & Koudstaal, P. J. Silent brain infarcts: a systematic review. Lancet Neurol. 6, 611–619 (2007).
Geerlings, M. I. et al. Association of white matter lesions and lacunar infarcts with executive functioning: the SMART-MR study. Am. J. Epidemiol. 170, 1147–1155 (2009).
Zlokovic, B. V. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron 57, 178–201 (2008).
Kerkhofs, D. et al. Pharmacological depletion of microglia and perivascular macrophages prevents vascular cognitive impairment in Ang II-induced hypertension. Theranostics 10, 9512–9527 (2020).
Sweeney, M. D., Zhao, Z., Montagne, A., Nelson, A. R. & Zlokovic, B. V. Blood-brain barrier: from physiology to disease and back. Physiol. Rev. 99, 21–78 (2019).
Xu, L., Nirwane, A. & Yao, Y. Basement membrane and blood-brain barrier. Stroke Vasc. Neurol. 4, 78–82 (2019).
Bailey, E. L. et al. Cerebral small vessel endothelial structural changes predate hypertension in stroke-prone spontaneously hypertensive rats: a blinded, controlled immunohistochemical study of 5- to 21-week-old rats. Neuropathol. Appl. Neurobiol. 37, 711–726 (2011).
Fan, Y. et al. Tight junction disruption of blood-brain barrier in white matter lesions in chronic hypertensive rats. Neuroreport 26, 1039–1043 (2015).
Setiadi, A., Korim, W. S., Elsaafien, K. & Yao, S. T. The role of the blood-brain barrier in hypertension. Exp. Physiol. 103, 337–342 (2018).
Yang, Y. et al. Vascular tight junction disruption and angiogenesis in spontaneously hypertensive rat with neuroinflammatory white matter injury. Neurobiol. Dis. 114, 95–110 (2018).
Santisteban, M. M. et al. Endothelium-macrophage crosstalk mediates blood-brain barrier dysfunction in hypertension. Hypertension 76, 795–807 (2020).
Yang, Y., Estrada, E. Y., Thompson, J. F., Liu, W. & Rosenberg, G. A. Matrix metalloproteinase-mediated disruption of tight junction proteins in cerebral vessels is reversed by synthetic matrix metalloproteinase inhibitor in focal ischemia in rat. J. Cereb. Blood Flow. Metab. 27, 697–709 (2007).
Ueno, M. et al. Blood-brain barrier disruption in the hypothalamus of young adult spontaneously hypertensive rats. Histochem. Cell Biol. 122, 131–137 (2004).
Roggendorf, W., Opitz, H. & Schuppan, D. Altered expression of collagen type VI in brain vessels of patients with chronic hypertension. A comparison with the distribution of collagen IV and procollagen III. Acta Neuropathol. 77, 55–60 (1988).
Bell, R. D. et al. Pericytes control key neurovascular functions and neuronal phenotype in the adult brain and during brain aging. Neuron 68, 409–427 (2010).
Winkler, E. A., Bell, R. D. & Zlokovic, B. V. Central nervous system pericytes in health and disease. Nat. Neurosci. 14, 1398–1405 (2011).
Sure, V. N. et al. A novel high-throughput assay for respiration in isolated brain microvessels reveals impaired mitochondrial function in the aged mice. Geroscience 40, 365–375 (2018).
Van Skike, C. E. et al. Inhibition of mTOR protects the blood-brain barrier in models of Alzheimer’s disease and vascular cognitive impairment. Am. J. Physiol. Heart Circ. Physiol. 314, H693–H703 (2018).
Wilhelm, I., Nyul-Toth, A., Kozma, M., Farkas, A. E. & Krizbai, I. A. Role of pattern recognition receptors of the neurovascular unit in inflamm-aging. Am. J. Physiol. Heart Circ. Physiol 313, H1000–H1012 (2017).
Kiss, T. et al. Single-cell RNA sequencing identifies senescent cerebromicrovascular endothelial cells in the aged mouse brain. Geroscience 42, 429–444 (2020).
Mayhan, W. G. & Heistad, D. D. Role of veins and cerebral venous pressure in disruption of the blood-brain barrier. Circ. Res. 59, 216–220 (1986).
Fulop, G. A. et al. Cerebral venous congestion promotes blood-brain barrier disruption and neuroinflammation, impairing cognitive function in mice. Geroscience 41, 575–589 (2019).
Tucsek, Z. et al. Hypertension-induced synapse loss and impairment in synaptic plasticity in the mouse hippocampus mimics the aging phenotype: implications for the pathogenesis of vascular cognitive impairment. Geroscience 39, 385–406 (2017).
Davalos, D. et al. Fibrinogen-induced perivascular microglial clustering is required for the development of axonal damage in neuroinflammation. Nat. Commun. 3, 1227 (2012).
Sadekova, N. et al. Arterial stiffness induced by carotid calcification leads to cerebral gliosis mediated by oxidative stress. J. Hypertens. 36, 286–298 (2018).
Bowman, G. L. et al. Blood-brain barrier breakdown, neuroinflammation, and cognitive decline in older adults. Alzheimers Dement. 14, 1640–1650 (2018).
Singh, M. V., Chapleau, M. W., Harwani, S. C. & Abboud, F. M. The immune system and hypertension. Immunol. Res. 59, 243–253 (2014).
Carnevale, D. & Lembo, G. ‘Alzheimer-like’ pathology in a murine model of arterial hypertension. Biochem. Soc. Trans. 39, 939–944 (2011).
Ungvari, Z., Tarantini, S., Kirkpatrick, A. C., Csiszar, A. & Prodan, C. I. Cerebral microhemorrhages: mechanisms, consequences, and prevention. Am. J. Physiol. Heart Circ. Physiol. 312, H1128–H1143 (2017).
Yates, P. A. et al. Cerebral microhemorrhage and brain β-amyloid in aging and Alzheimer disease. Neurology 77, 48–54 (2011).
Petrea, R. E. et al. Mid to late life hypertension trends and cerebral small vessel disease in the framingham heart study. Hypertension 76, 707–714 (2020).
Lau, W. L. et al. Chronic kidney disease increases cerebral microbleeds in mouse and man. Transl. Stroke Res. 11, 122–134 (2020).
Ungvari, Z., Tarantini, S., Kirkpatrick, A. C., Csiszar, A. & Prodan, C. I. Cerebral microhemorrhages: mechanisms, consequences and prevention. Am. J. Physiol. Heart Circ. Physiol. 312, H1128–H1143 (2017).
Ungvari, Z. et al. Repeated Valsalva maneuvers promote symptomatic manifestations of cerebral microhemorrhages: implications for the pathogenesis of vascular cognitive impairment in older adults. Geroscience 40, 485–496 (2018).
Choi, Y. & Lee, M. K. Neuroimaging findings of brain MRI and CT in patients with COVID-19: a systematic review and meta-analysis. Eur. J. Radiol. 133, 109393 (2020).
Haroon, K. H., Patro, S. N., Hussain, S., Zafar, A. & Muhammad, A. Multiple microbleeds: a serious neurological manifestation in a critically ill COVID-19 patient. Case Rep. Neurol. 12, 373–377 (2020).
Kirschenbaum, D. et al. Intracerebral endotheliitis and microbleeds are neuropathological features of COVID-19. Neuropathol. Appl. Neurobiol. 47, 454–459 (2020).
Bosch, A. J. et al. Retinal capillary rarefaction in patients with untreated mild-moderate hypertension. BMC Cardiovasc. Disord. 17, 300 (2017).
Hoenig, M. R., Bianchi, C., Rosenzweig, A. & Sellke, F. W. The cardiac microvasculature in hypertension, cardiac hypertrophy and diastolic heart failure. Curr. Vasc. Pharmacol. 6, 292–300 (2008).
Kubis, N. et al. Decreased arteriolar density in endothelial nitric oxide synthase knockout mice is due to hypertension, not to the constitutive defect in endothelial nitric oxide synthase enzyme. J. Hypertens. 20, 273–280 (2002).
Williams, S. A. et al. Capillary hypertension and abnormal pressure dynamics in patients with essential hypertension. Clin. Sci. 79, 5–8 (1990).
Antonios, T. F., Singer, D. R., Markandu, N. D., Mortimer, P. S. & MacGregor, G. A. Structural skin capillary rarefaction in essential hypertension. Hypertension 33, 998–1001 (1999).
Ungvari, Z. et al. Endothelial dysfunction and angiogenesis impairment in the ageing vasculature. Nat. Rev. Cardiol. 15, 555–565 (2018).
Kiss, T. et al. Nicotinamide mononucleotide (NMN) treatment attenuates oxidative stress and rescues angiogenic capacity in aged cerebromicrovascular endothelial cells: a potential mechanism for the prevention of vascular cognitive impairment. Geroscience 41, 619–630 (2019).
Banki, E. et al. Age-related decline of autocrine pituitary adenylate cyclase-activating polypeptide impairs angiogenic capacity of rat cerebromicrovascular endothelial cells. J. Gerontol. A Biol. Sci. Med. Sci. 70, 665–674 (2015).
Reglodi, D. et al. PACAP deficiency as a model of aging. Geroscience 40, 437–452 (2018).
Ungvari, Z. et al. Aging-induced dysregulation of dicer1-dependent microRNA expression impairs angiogenic capacity of rat cerebromicrovascular endothelial cells. J. Gerontol. A Biol. Sci. Med. Sci. 68, 877–891 (2013).
Ungvari, Z. et al. Ionizing radiation promotes the acquisition of a senescence-associated secretory phenotype and impairs angiogenic capacity in cerebromicrovascular endothelial cells: role of increased DNA damage and decreased DNA repair capacity in microvascular radiosensitivity. J. Gerontol. A Biol. Sci. Med. Sci. 68, 1443–1457 (2013).
Toth, P. et al. Purinergic glio-endothelial coupling during neuronal activity: role of P2Y1 receptors and eNOS in functional hyperemia in the mouse somatosensory cortex. Am. J. Physiol. Heart Circ. Physiol. 309, H1837–H1845 (2015).
Tarantini, S. et al. Pharmacologically-induced neurovascular uncoupling is associated with cognitive impairment in mice. J. Cereb. Blood Flow. Metab. 35, 1871–1881 (2015).
Tarantini, S. et al. Treatment with the poly(ADP-ribose) polymerase inhibitor PJ-34 improves cerebromicrovascular endothelial function, neurovascular coupling responses and cognitive performance in aged mice, supporting the NAD+ depletion hypothesis of neurovascular aging. Geroscience 41, 533–542 (2019).
Tong, X. K., Lecrux, C., Rosa-Neto, P. & Hamel, E. Age-dependent rescue by simvastatin of Alzheimer’s disease cerebrovascular and memory deficits. J. Neurosci. 32, 4705–4715 (2012).
Nicolakakis, N. et al. Complete rescue of cerebrovascular function in aged Alzheimer’s disease transgenic mice by antioxidants and pioglitazone, a peroxisome proliferator-activated receptor gamma agonist. J. Neurosci. 28, 9287–9296 (2008).
Faraco, G. et al. Hypertension enhances Aβ-induced neurovascular dysfunction, promotes β-secretase activity, and leads to amyloidogenic processing of APP. J. Cereb. Blood Flow. Metab. 36, 241–252 (2016).
Girouard, H., Park, L., Anrather, J., Zhou, P. & Iadecola, C. Angiotensin II attenuates endothelium-dependent responses in the cerebral microcirculation through nox-2-derived radicals. Arterioscler. Thromb. Vasc. Biol. 26, 826–832 (2006).
Kazama, K. et al. Angiotensin II impairs neurovascular coupling in neocortex through NADPH oxidase-derived radicals. Circ. Res. 95, 1019–1026 (2004).
Kazama, K., Wang, G., Frys, K., Anrather, J. & Iadecola, C. Angiotensin II attenuates functional hyperemia in the mouse somatosensory cortex. Am. J. Physiol. Heart Circ. Physiol. 285, H1890–H1899 (2003).
Wong, R. et al. Assessment of cerebral blood flow in adult patients with aortic coarctation. Cardiol. Young 27, 1606–1613 (2017).
Muhire, G. et al. Arterial stiffness due to carotid calcification disrupts cerebral blood flow regulation and leads to cognitive deficits. J. Am. Heart Assoc. 8, e011630 (2019).
Faraco, G. et al. Perivascular macrophages mediate the neurovascular and cognitive dysfunction associated with hypertension. J. Clin. Invest. 126, 4674–4689 (2016).
Huang, A., Sun, D. & Koller, A. Endothelial dysfunction augments myogenic arteriolar constriction in hypertension. Hypertension 22, 913–921 (1993).
Ungvari, Z. et al. High pressure induces superoxide production in isolated arteries via protein kinase C-dependent activation of NAD(P)H oxidase. Circulation 108, 1253–1258 (2003).
Ungvari, Z., Csiszar, A., Kaminski, P. M., Wolin, M. S. & Koller, A. Chronic high pressure-induced arterial oxidative stress: Involvement of protein kinase C-dependent NAD(P)H oxidase and local renin-angiotensin system. Am. J. Pathol. 165, 219–226 (2004).
Koh, K. K. et al. Comparison of effects of losartan, irbesartan, and candesartan on flow-mediated brachial artery dilation and on inflammatory and thrombolytic markers in patients with systemic hypertension. Am. J. Cardiol. 93, 1432–1435, A1410 (2004).
Calcinaghi, N. et al. Multimodal imaging in rats reveals impaired neurovascular coupling in sustained hypertension. Stroke 44, 1957–1964 (2013).
Wiedenhoeft, T. et al. Fusogenic liposomes effectively deliver resveratrol to the cerebral microcirculation and improve endothelium-dependent neurovascular coupling responses in aged mice. Geroscience 41, 711–725 (2019).
Toth, P. et al. Resveratrol treatment rescues neurovascular coupling in aged mice: role of improved cerebromicrovascular endothelial function and downregulation of NADPH oxidase. Am. J. Physiol. Heart Circ. Physiol. 306, H299–H308 (2014).
Liang, E. S. et al. PARP-1 (Poly[ADP-Ribose] Polymerase 1) inhibition protects from Ang II (Angiotensin II)-induced abdominal aortic aneurysm in mice. Hypertension 72, 1189–1199 (2018).
Tarantini, S. et al. Treatment with the mitochondrial-targeted antioxidant peptide SS-31 rescues neurovascular coupling responses and cerebrovascular endothelial function and improves cognition in aged mice. Aging Cell 17, e12731 (2018).
Dikalov, S. I. et al. Nox2-induced production of mitochondrial superoxide in angiotensin II-mediated endothelial oxidative stress and hypertension. Antioxid. Redox Signal. 20, 281–294 (2014).
Iadecola, C. & Gottesman, R. F. Cerebrovascular alterations in alzheimer disease. Circ. Res. 123, 406–408 (2018).
Kim, H. J. et al. Assessment of extent and role of tau in subcortical vascular cognitive impairment using 18F-AV1451 positron emission tomography imaging. JAMA Neurol. 75, 999–1007 (2018).
Zlokovic, B. V. Neurovascular pathways to neurodegeneration in Alzheimer’s disease and other disorders. Nat. Rev. Neurosci. 12, 723–738 (2011).
Niwa, K. et al. Cerebrovascular autoregulation is profoundly impaired in mice overexpressing amyloid precursor protein. Am. J. Physiol. Heart Circ. Physiol. 283, H315–H323 (2002).
Nyul-Toth, A. et al. Increases in hypertension-induced cerebral microhemorrhages exacerbate gait dysfunction in a mouse model of Alzheimer’s disease. Geroscience 42, 1685–1698 (2020).
Rasmussen, M. K., Mestre, H. & Nedergaard, M. The glymphatic pathway in neurological disorders. Lancet Neurol. 17, 1016–1024 (2018).
Mortensen, K. N. et al. Impaired glymphatic transport in spontaneously hypertensive rats. J. Neurosci. 39, 6365–6377 (2019).
Rouch, L. et al. Antihypertensive drugs, prevention of cognitive decline and dementia: a systematic review of observational studies, randomized controlled trials and meta-analyses, with discussion of potential mechanisms. CNS Drugs 29, 113–130 (2015).
Peters, R. et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 7, 683–689 (2008).
Menezes, S. T. et al. Hypertension, prehypertension, and hypertension control: association with decline in cognitive performance in the ELSA-Brasil cohort. Hypertension 77, 672–681 (2020).
Tzourio, C. et al. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch. Intern. Med. 163, 1069–1075 (2003).
Barthold, D., Joyce, G., Wharton, W., Kehoe, P. & Zissimopoulos, J. The association of multiple anti-hypertensive medication classes with Alzheimer’s disease incidence across sex, race, and ethnicity. PLoS One 13, e0206705 (2018).
Hughes, D. et al. Association of blood pressure lowering with incident dementia or cognitive impairment: a systematic review and meta-analysis. JAMA 323, 1934–1944 (2020).
Maxwell, C. J., Hogan, D. B. & Ebly, E. M. Calcium-channel blockers and cognitive function in elderly people: results from the Canadian study of health and aging. CMAJ 161, 501–506 (1999).
Tu, K. et al. Antihypertensive drug prescribing and persistence among new elderly users: implications for persistence improvement interventions. Can. J. Cardiol. 30, 647–652 (2014).
Quitterer, U. & AbdAlla, S. Improvements of symptoms of Alzheimer’s disease by inhibition of the angiotensin system. Pharmacol. Res. 154, 104230 (2020).
Hachinski, V. et al. Preventing dementia by preventing stroke: The Berlin Manifesto. Alzheimers Dement. 15, 961–984 (2019).
Friberg, L. & Rosenqvist, M. Less dementia with oral anticoagulation in atrial fibrillation. Eur. Heart J. 39, 453–460 (2018).
SPRINT MIND Investigators for the SPRINT Research Group. et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA 321, 553–561 (2019).
Lv, Y. B. et al. A U-shaped association between blood pressure and cognitive impairment in chinese elderly. J. Am. Med. Dir. Assoc. 18, 193.e7–193.e13 (2017).
Waldstein, S. R., Giggey, P. P., Thayer, J. F. & Zonderman, A. B. Nonlinear relations of blood pressure to cognitive function: the baltimore longitudinal study of aging. Hypertension 45, 374–379 (2005).
Nilsson, S. E. et al. Low systolic blood pressure is associated with impaired cognitive function in the oldest old: longitudinal observations in a population-based sample 80 years and older. Aging Clin. Exp. Res. 19, 41–47 (2007).
Noriega de la Colina, A. et al. Diurnal blood pressure loads are associated with lower cognitive performances in controlled-hypertensive elderly individuals. J. Hypertens. 37, 2168–2179 (2019).
Xie, Z., Gao, M., Togashi, H., Saito, H. & Koyama, T. Improvement in the capillarity of the left ventricular wall of stroke-prone spontaneously hypertensive rats following angiotensin II receptor blockade. Clin. Exp. Hypertens. 21, 441–452 (1999).
Whitson, J. A. et al. SS-31 and NMN: Two paths to improve metabolism and function in aged hearts. Aging Cell 19, e13213 (2020).
Lee, G. H. et al. Anthocyanins attenuate endothelial dysfunction through regulation of uncoupling of nitric oxide synthase in aged rats. Aging Cell 19, e13279 (2020).
Walaszczyk, A. et al. Pharmacological clearance of senescent cells improves survival and recovery in aged mice following acute myocardial infarction. Aging Cell 18, e12945 (2019).
Lewis-McDougall, F. C. et al. Aged-senescent cells contribute to impaired heart regeneration. Aging Cell 18, e12931 (2019).
Yang, D. et al. Histone methyltransferase Smyd3 is a new regulator for vascular senescence. Aging Cell 19, e13212 (2020).
Ogrodnik, M., Salmonowicz, H. & Gladyshev, V. N. Integrating cellular senescence with the concept of damage accumulation in aging: relevance for clearance of senescent cells. Aging Cell 18, e12841 (2019).
Marin-Aguilar, F. et al. NLRP3 inflammasome suppression improves longevity and prevents cardiac aging in male mice. Aging Cell 19, e13050 (2020).
Tarantini, S. et al. Nicotinamide mononucleotide (NMN) supplementation rescues cerebromicrovascular endothelial function and neurovascular coupling responses and improves cognitive function in aged mice. Redox Biol. 24, 101192 (2019).
Sardu, C. et al. Effects of metformin therapy on coronary endothelial dysfunction in patients with prediabetes with stable angina and nonobstructive coronary artery stenosis: the CODYCE multicenter prospective study. Diabetes Care 42, 1946–1955 (2019).
Van Skike, C. E. et al. mTOR drives cerebrovascular, synaptic, and cognitive dysfunction in normative aging. Aging Cell 19, e13057 (2020).
Toth, P. et al. IGF-1 deficiency impairs neurovascular coupling in mice: implications for cerebromicrovascular aging. Aging Cell (2015).
PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 358, 1033–1041 (2001).
Cortes-Canteli, M. & Iadecola, C. Alzheimer’s disease and vascular aging: JACC focus seminar. J. Am. Coll. Cardiol. 75, 942–951 (2020).
Acknowledgements
The authors’ work was supported by grants from the American Heart Association, the Oklahoma Center for the Advancement of Science and Technology, the Presbyterian Health Foundation and the Department of Veterans Affairs (award Number CX000340).
Author information
Authors and Affiliations
Contributions
All authors contributed to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Nephrology thanks Prasad Katakam, Anja Meissner and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Lacunar infarcts
-
Small infarcts (2–20 mm in diameter) in the deep cerebral white matter, basal ganglia, or pons that are presumed to result from the occlusion of a single small perforating artery supplying the subcortical areas of the brain.
- White matter lesions
-
Areas of abnormal myelination in the brain that are best visualized as hyperintensities on T2-weighted and fluid-attenuated inversion recovery (FLAIR) MRI sequences.
- Abstract reasoning
-
A cognitive domain that is closely related to fluid intelligence. The ability to quickly reason with information to solve new, unfamiliar problems, independent of any prior knowledge.
- Executive function
-
A set of mental skills that include working memory, flexible thinking and self-control.
- Digit Symbol Substitution Test
-
A paper-and-pencil cognitive test that requires matching of symbols to numbers.
- Mini-Mental State Examination
-
(MMSE). A test of cognitive function that is widely used for elderly people. The MMSE includes tests of orientation, attention, memory, language and visuo-spatial skills.
- Lipohyalinosis
-
Cerebral small vessel disease affecting the small arteries and arterioles in the brain. Lipohyalinosis is characterized by vessel wall thickening and a resultant reduction in luminal diameter.
- Lacunes
-
Small subcortical infarcts (<15 mm in diameter) in the territory of the deep penetrating arteries. These lesions may present with specific lacunar syndromes or they may be asymptomatic.
- Gliosis
-
An inflammatory process leading to scars in the central nervous system that involves the production of a dense fibrous network of neuroglia in areas of damage.
- Astrocytic endfeet
-
Processes that physically connect the astrocyte cell body to the outside of capillary walls.
- Pathogen-associated molecular patterns
-
Small molecular motifs that are recognized by Toll-like receptors. PAMPS activate innate immune responses that protect the host from infection.
- Transverse aortic coarctation
-
Narrowing of the transverse aortic arch.
- Neuropil
-
A dense network of interwoven nerve fibres and their branches and synapses together with glial filaments.
- Senolytics
-
A class of small molecules that selectively induce death of senescent cells. Senolytics are being developed with the aim of delaying, preventing, alleviating or reversing age-related diseases and improving human health.
Rights and permissions
About this article
Cite this article
Ungvari, Z., Toth, P., Tarantini, S. et al. Hypertension-induced cognitive impairment: from pathophysiology to public health. Nat Rev Nephrol 17, 639–654 (2021). https://doi.org/10.1038/s41581-021-00430-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-021-00430-6
This article is cited by
-
Sex and gender correlates of sexually polymorphic cognition
Biology of Sex Differences (2024)
-
Blood pressure variability supersedes heart rate variability as a real-world measure of dementia risk
Scientific Reports (2024)
-
Investigating the effect of hypertension on vascular cognitive impairment by using the resting-state functional connectome
Scientific Reports (2024)
-
Atherosclerotic burden and cerebral small vessel disease: exploring the link through microvascular aging and cerebral microhemorrhages
GeroScience (2024)
-
Effects of physical activity and depressive symptoms on cognitive function in older adults: National Health and Nutrition Examination Survey
Neurological Sciences (2024)