Abstract
Diabetic kidney disease is the leading cause of kidney failure worldwide; in the USA, it accounts for over 50% of individuals entering dialysis or transplant programmes. Unlike other complications of diabetes, the prevalence of diabetic kidney disease has failed to decline over the past 30 years. Hyperglycaemia is the primary aetiological factor responsible for the development of diabetic kidney disease. Once hyperglycaemia becomes established, multiple pathophysiological disturbances, including hypertension, altered tubuloglomerular feedback, renal hypoxia, lipotoxicity, podocyte injury, inflammation, mitochondrial dysfunction, impaired autophagy and increased activity of the sodium–hydrogen exchanger, contribute to progressive glomerular sclerosis and the decline in glomerular filtration rate. The quantitative contribution of each of these abnormalities to the progression of diabetic kidney disease, as well as their role in type 1 and type 2 diabetes mellitus, remains to be determined. Sodium–glucose co-transporter 2 (SGLT2) inhibitors have a beneficial impact on many of these pathophysiological abnormalities; however, as several pathophysiological disturbances contribute to the onset and progression of diabetic kidney disease, multiple agents used in combination will likely be required to slow the progression of disease effectively.
Key points
-
Multiple pathophysiological disturbances contribute to the onset and progression of diabetic kidney disease (DKD); from a clinical standpoint, this multifactorial pathogenic process implies that the use of multiple agents in combination will be required to treat the disease.
-
Hyperglycaemia and hypertension are the key factors responsible for the development of DKD, but, once established, even tight glycaemic and/or hypertension control may not be able to halt or slow disease progression.
-
Other pathogenic processes underlying the development and progression of DKD include alterations in tubuloglomerular feedback, tubule hypertrophy, hypoxia, podocyte injury, albuminuria and lipotoxicity.
-
Inflammation, endothelial dysfunction, mitochondrial injury, fibrosis and impaired autophagy also contribute to the progressive nature of DKD, but these defects are most likely to be secondary events that follow the primary events described above. Sodium–glucose co-transporter 2 (SGLT2) inhibitors correct or improve many of the pathological processes involved in the development of and progression of DKD and are likely to underlie the ability of these agents to slow progression of established DKD in large prospective clinical trials; of these mechanisms, restoration of normal tubuloglomerular feedback and reduced interglomerular pressure are especially pertinent.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Centers for Disease Control and Prevention. National Diabetes Statistical Report. Centers for Disease Control and Prevention https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf (2020).
Koye, D. N., Magliano, D. J., Nelson, R. G. & Pavkov, M. E. The global epidemiology of diabetes and kidney disease. Adv. Chronic Kidney Dis. 25, 121–132 (2018).
Gregg, E. W. et al. Changes in diabetes-related complications in the United States, 1990–2010. N. Engl. J. Med. 370, 1514–1523 (2014). Unlike the prevalence of other diabetic microvascular and macrovascular complications, which have decreased over the past 10–20 years, the prevalence of DKD has remained unchanged.
Lytvyn, Y., Bjornstad, P., van Raalte, D. H., Heerspink, H. L. & Cherney, D. Z. I. The new biology of diabetic kidney disease-mechanisms and therapeutic implications. Endocr. Rev. 41, 202–231 (2020). An excellent review of therapies for DKD currently in use or in clinical development.
Zinman, B. et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 373, 2117–2128 (2015).
Neal, B. et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N. Engl. J. Med. 377, 644–657 (2017).
Wiviott, S. D. et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 380, 347–357 (2019).
Perkovic, V. et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 380, 2295–2306 (2019). A large prospective study that demonstrated the efficacy of the SGLT2 inhibitor canagliflozin in slowing the progression of kidney disease in patients with established DKD and resulted in approval of the drug by the FDA.
Heerspink, H. J. L. et al. Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 383, 1436–1446 (2020).
Umanath, K. & Lewis, J. B. Update on diabetic nephropathy: core curriculum 2018. Am. J. Kidney Dis. 71, 884–895 (2018).
Tonneijck, L. et al. Glomerular hyperfiltration in diabetes: mechanisms, clinical significance, and treatment. J. Am. Soc. Nephrol. 28, 1023–1039 (2017). Excellent, up-to-date review about the origin, significance and treatment of hyperfiltration in diabetic nephropathy.
Markus, M. R. P. et al. Prediabetes is associated with microalbuminuria, reduced kidney function and chronic kidney disease in the general population: The KORA (Cooperative Health Research in the Augsburg Region) F4-Study. Nutr. Metab. Cardiovasc. Dis. 28, 234–242 (2018).
Diabetes, C. et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 329, 977–986 (1993). Landmark study demonstrating the importance of tight glycaemic control in the prevention of microvascular complications in patients with type 1 diabetes.
American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes-2018. Diabetes Care 41, S55–S64 (2018).
Diabetes, C. et al. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N. Engl. J. Med. 342, 381–389 (2000).
Nathan, D. M. et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N. Engl. J. Med. 353, 2643–2653 (2005).
Stratton, I. M. et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321, 405–412 (2000).
Group, A. C. et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 358, 2560–2572 (2008).
Ismail-Beigi, F. et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet 376, 419–430 (2010).
Brocco, E. et al. Evidence of a threshold value of glycated hemoglobin to improve the course of renal function in type 2 diabetes with typical diabetic glomerulopathy. J. Nephrol. 14, 461–471 (2001).
Zoungas, S. et al. Combined effects of routine blood pressure lowering and intensive glucose control on macrovascular and microvascular outcomes in patients with type 2 diabetes: new results from the ADVANCE trial. Diabetes Care 32, 2068–2074 (2009).
Tamborlane, W. V. et al. Long-term improvement of metabolic control with the insulin pump does not reverse diabetic microangiopathy. Diabetes Care 5, 58–64 (1982). Although the number of patients with diabetes was small, this study demonstrated that intensive glycaemic control with insulin in patients with type 1 diabetes cannot slow the progression of DKD once macroalbuminuria is established.
Ciavarella, A. et al. Effect of long-term near-normoglycemia on the progression of diabetic nephropathy. Diabete Metab. 11, 3–8 (1985).
Caramori, M. L., Fioretto, P. & Mauer, M. Low glomerular filtration rate in normoalbuminuric type 1 diabetic patients: an indicator of more advanced glomerular lesions. Diabetes 52, 1036–1040 (2003).
Merovci, A. et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J. Clin. Invest. 124, 509–514 (2014). To our knowledge the first study to examine the mechanisms by which SGLT2 inhibitors improve glycaemic control in patients with diabetes.
DeFronzo, R. A., Norton, L. & Abdul-Ghani, M. Renal, metabolic and cardiovascular considerations of SGLT2 inhibition. Nat. Rev. Nephrol. 13, 11–26 (2017). Comprehensive review of the pleiotrophic effects of SGLT2 inhibitors in humans.
DeFronzo, R. A. et al. Characterization of renal glucose reabsorption in response to dapagliflozin in healthy subjects and subjects with type 2 diabetes. Diabetes Care 36, 3169–3176 (2013).
Merovci, A. et al. Dapagliflozin lowers plasma glucose concentration and improves beta-cell function. J. Clin. Endocrinol. Metab. 100, 1927–1932 (2015).
Al Jobori, H. et al. Empagliflozin treatment is associated with improved beta-cell function in type 2 diabetes mellitus. J. Clin. Endocrinol. Metab. 103, 1402–1407 (2018).
Yki-Jarvinen, H Glucose toxicity. in International Textbook of Diabetes Mellitus. 4th edn. 413-425 (Wiley, 2015).
Parving, H. H., Andersen, A. R., Smidt, U. M. & Svendsen, P. A. Early aggressive antihypertensive treatment reduces rate of decline in kidney function in diabetic nephropathy. Lancet 1, 1175–1179 (1983). One of the earliest publications demonstrating the powerful effect of antihypertensive therapy in slowing the rate of GFR decline in patients with established DKD.
Xie, X. et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet 387, 435–443 (2016).
Patney, V., Whaley-Connell, A. & Bakris, G. Hypertension management in DKD. Diabetes Spectr. 28, 175–180 (2015).
Group, A. S. et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N. Engl. J. Med. 362, 1575–1585 (2010).
Group, S. R. et al. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 373, 2103–2116 (2015).
Warren, A. M., Knudsen, S. T. & Cooper, M. E. Diabetic nephropathy: an insight into molecular mechanisms and emerging therapies. Expert Opin. Ther. Targets 23, 579–591 (2019).
Ruggenenti, P., Cravedi, P. & Remuzzi, G. The RAAS in the pathogenesis and treatment of diabetic nephropathy. Nat. Rev. Nephrol. 6, 319–330 (2010). Excellent review of the renin–angiotensin–aldosterone system in the pathogenesis and treatment of DKD.
van den Meiracker, A. H. et al. Partial escape of angiotensin converting enzyme (ACE) inhibition during prolonged ACE inhibitor treatment: does it exist and does it affect the antihypertensive response? J. Hypertens. 10, 803–812 (1992).
Ingelfinger, J. R. Aliskiren and dual therapy in type 2 diabetes mellitus. N. Engl. J. Med. 358, 2503–2505 (2008).
Bolignano, D., Palmer, S. C., Navaneethan, S. D. & Strippoli, G. F. Aldosterone antagonists for preventing the progression of chronic kidney disease. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD007004.pub3 (2014).
Morales, E. et al. Renoprotective effects of mineralocorticoid receptor blockers in patients with proteinuric kidney diseases. Nephrol. Dial. Transpl. 28, 405–412 (2013).
Cherney, D. Z. et al. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation 129, 587–597 (2014). Well-designed study demonstrating that inhibition of the SGLT2 cotransporter reverses hyperfiltration in patients with type 1 diabetes.
Scheen, A. J. & Delanaye, P. Effects of reducing blood pressure on renal outcomes in patients with type 2 diabetes: focus on SGLT2 inhibitors and EMPA-REG OUTCOME. Diabetes Metab. 43, 99–109 (2017).
Brenner, B. M. Hemodynamically mediated glomerular injury and the progressive nature of kidney disease. Kidney Int. 23, 647–655 (1983). The role of altered tubuloglomerular feedback, increased intraglomerular pressure, and hyperfiltration in the development and progression of chronic kidney disease is reviewed by the original proponent of the haemodynamic theory of glomerular injury.
Thomson, S. C. & Blantz, R. C. Glomerulotubular balance, tubuloglomerular feedback, and salt homeostasis. J. Am. Soc. Nephrol. 19, 2272–2275 (2008).
Vallon, V. et al. Adenosine A(1) receptors determine glomerular hyperfiltration and the salt paradox in early streptozotocin diabetes mellitus. Nephron Physiol. 111, p30–p38 (2009).
Sallstrom, J. et al. Diabetes-induced hyperfiltration in adenosine A(1)-receptor deficient mice lacking the tubuloglomerular feedback mechanism. Acta Physiol. 190, 253–259 (2007).
Gallo, L. A., Wright, E. M. & Vallon, V. Probing SGLT2 as a therapeutic target for diabetes: basic physiology and consequences. Diab Vasc. Dis. Res. 12, 78–89 (2015).
Bank, N. & Aynedjian, H. S. Progressive increases in luminal glucose stimulate proximal sodium absorption in normal and diabetic rats. J. Clin. Invest. 86, 309–316 (1990).
Vallon, V. & Thomson, S. C. Renal function in diabetic disease models: the tubular system in the pathophysiology of the diabetic kidney. Annu. Rev. Physiol. 74, 351–375 (2012). Review of evidence supporting enhanced glucose-coupled sodium reabsorption by the proximal tubule in the development of increased intraglomerular pressure, hyperfiltration and diabetic glomerular injury.
Vallon, V., Richter, K., Blantz, R. C., Thomson, S. & Osswald, H. Glomerular hyperfiltration in experimental diabetes mellitus: potential role of tubular reabsorption. J. Am. Soc. Nephrol. 10, 2569–2576 (1999).
Bjornstad, P. et al. Rapid GFR decline is associated with renal hyperfiltration and impaired GFR in adults with Type 1 diabetes. Nephrol. Dial. Transpl. 30, 1706–1711 (2015). Prospective clinical study demonstrating that hyperfiltration predicts the decline in GFR in patients with type 1 diabetes.
Magee, G. M. et al. Is hyperfiltration associated with the future risk of developing diabetic nephropathy? A meta-analysis. Diabetologia 52, 691–697 (2009).
Ruggenenti, P. et al. Glomerular hyperfiltration and renal disease progression in type 2 diabetes. Diabetes Care 35, 2061–2068 (2012). Prospective clinical study demonstrating that hyperfiltration predicts the decline in GFR in patients with type 2 diabetes.
Nelson, R. G. et al. Development and progression of renal disease in Pima Indians with non-insulin-dependent diabetes mellitus. Diabetic Renal Disease Study Group. N. Engl. J. Med. 335, 1636–1642 (1996).
Jerums, G., Premaratne, E., Panagiotopoulos, S. & MacIsaac, R. J. The clinical significance of hyperfiltration in diabetes. Diabetologia 53, 2093–2104 (2010).
Vestri, S. et al. Changes in sodium or glucose filtration rate modulate expression of glucose transporters in renal proximal tubular cells of rat. J. Membr. Biol. 182, 105–112 (2001).
Tabatabai, N. M., Sharma, M., Blumenthal, S. S. & Petering, D. H. Enhanced expressions of sodium-glucose cotransporters in the kidneys of diabetic Zucker rats. Diabetes Res. Clin. Pract. 83, e27–e30 (2009).
Albertoni Borghese, M. F. et al. Expression and activity of SGLT2 in diabetes induced by streptozotocin: relationship with the lipid environment. Nephron Physiol. 112, p45–p52 (2009).
Norton, L. et al. Sodium-glucose co-transporter (SGLT) and glucose transporter (GLUT) expression in the kidney of type 2 diabetic subjects. Diabetes Obes. Metab. 19, 1322–1326 (2017). Renal biopsy study demonstrating that the gene transcript for SGLT1 is increased in patients with diabetes, whereas the gene transcript for SGLT2 is normal to decreased.
Solini, A. et al. Sodium-glucose co-transporter (SGLT)2 and SGLT1 renal expression in patients with type 2 diabetes. Diabetes Obes. Metab. 19, 1289–1294 (2017).
Vallon, V. et al. Knockout of Na-glucose transporter SGLT2 attenuates hyperglycemia and glomerular hyperfiltration but not kidney growth or injury in diabetes mellitus. Am. J. Physiol. Ren. Physiol. 304, F156–F167 (2013). Classic study documenting that knockout of the SGLT2 transporter in the proximal tubule ameliorates hyperfiltration in diabetic mice.
Thomson, S. C. et al. Acute and chronic effects of SGLT2 blockade on glomerular and tubular function in the early diabetic rat. Am. J. Physiol. Regul. Integr. Comp. Physiol. 302, R75–R83 (2012).
Terami, N. et al. Long-term treatment with the sodium glucose cotransporter 2 inhibitor, dapagliflozin, ameliorates glucose homeostasis and diabetic nephropathy in db/db mice. PLoS ONE 9, e100777 (2014).
Kidokoro, K. et al. Evaluation of glomerular hemodynamic function by empagliflozin in diabetic mice using in vivo imaging. Circulation 140, 303–315 (2019).
van Bommel, E. J. M. et al. The renal hemodynamic effects of the SGLT2 inhibitor dapagliflozin are caused by post-glomerular vasodilatation rather than pre-glomerular vasoconstriction in metformin-treated patients with type 2 diabetes in the randomized, double-blind RED trial. Kidney Int. 97, 202–212 (2020). Provocative clinical study demonstrating that the SGLT2 inhibitor dapagliflozin reduces GFR intraglomerular pressure by causing vasodilation of the efferent arteriole in patients with type 2 diabetes, indicating that the renal haemodynamic effects in these individuals are distinct from those in patients with type 1 diabetes.
Fioretto, P., Zambon, A., Rossato, M., Busetto, L. & Vettor, R. SGLT2 inhibitors and the diabetic kidney. Diabetes Care 39, S165–S171 (2016).
Denic, A. et al. Single-nephron glomerular filtration rate in healthy adults. N. Engl. J. Med. 376, 2349–2357 (2017).
van der Sande, N. G. et al. High ratios of kidney function to kidney size are related to mortality and kidney function decline in high-risk patients. Eur. J. Prev. Cardiol. 24, 926–933 (2017).
Altay, S. et al. Renal “hyperfiltrators” are at elevated risk of death and chronic diseases. BMC Nephrol. 15, 160 (2014).
Rigalleau, V. et al. Large kidneys predict poor renal outcome in subjects with diabetes and chronic kidney disease. BMC Nephrol. 11, 3 (2010).
Hostetter, T. H. Hypertrophy and hyperfunction of the diabetic kidney. J. Clin. Invest. 107, 161–162 (2001). Insightful discussion about whether glomerular hypertrophy begets hyperfiltration or hyperfiltration begets glomerular hypertrophy in the development of DKD.
Thomas, M. C., Burns, W. C. & Cooper, M. E. Tubular changes in early diabetic nephropathy. Adv. Chronic Kidney Dis. 12, 177–186 (2005).
Tuttle, K. R. et al. Effect of strict glycemic control on renal hemodynamic response to amino acids and renal enlargement in insulin-dependent diabetes mellitus. N. Engl. J. Med. 324, 1626–1632 (1991). Clinical study that conclusively demonstrates that strict glycaemic control with insulin reverses renal hypertrophy and the exaggerated rise in GFR in response to amino acids.
Wolf, G. & Neilson, E. G. Angiotensin II as a renal growth factor. J. Am. Soc. Nephrol. 3, 1531–1540 (1993).
Huang, H. C. & Preisig, P. A. G1 kinases and transforming growth factor-beta signaling are associated with a growth pattern switch in diabetes-induced renal growth. Kidney Int. 58, 162–172 (2000).
Deng, A. et al. Increased expression of ornithine decarboxylase in distal tubules of early diabetic rat kidneys: are polyamines paracrine hypertrophic factors? Diabetes 52, 1235–1239 (2003).
Thomson, S. C. et al. Ornithine decarboxylase, kidney size, and the tubular hypothesis of glomerular hyperfiltration in experimental diabetes. J. Clin. Invest. 107, 217–224 (2001). Landmark study demonstrating that tubular hypertrophy precedes glomerular hypertrophy and that inhibition of tubular hypertrophy with an inhibitor of ornithine decarboxylase prevents subsequent glomerular hypertrophy, hyperfiltration and DKD.
Chiarelli, F., Gaspari, S. & Marcovecchio, M. L. Role of growth factors in diabetic kidney disease. Horm. Metab. Res. 41, 585–593 (2009).
Qi, W., Chen, X., Poronnik, P. & Pollock, C. A. Transforming growth factor-beta/connective tissue growth factor axis in the kidney. Int. J. Biochem. Cell Biol. 40, 9–13 (2008).
Iwano, M. et al. Quantification of glomerular TGF-beta 1 mRNA in patients with diabetes mellitus. Kidney Int. 49, 1120–1126 (1996).
Yamamoto, T., Nakamura, T., Noble, N. A., Ruoslahti, E. & Border, W. A. Expression of transforming growth factor beta is elevated in human and experimental diabetic nephropathy. Proc. Natl Acad. Sci. USA 90, 1814–1818 (1993).
McGowan, T. A., Zhu, Y. & Sharma, K. Transforming growth factor-beta: a clinical target for the treatment of diabetic nephropathy. Curr. Diab Rep. 4, 447–454 (2004).
Voelker, J. et al. Anti-TGF-beta1 antibody therapy in patients with diabetic nephropathy. J. Am. Soc. Nephrol. 28, 953–962 (2017). Large prospective clinical trial in which an anti-TGFβ1 antibody failed to slow the progression of DKD.
van Nieuwenhoven, F. A., Jensen, L. J., Flyvbjerg, A. & Goldschmeding, R. Imbalance of growth factor signalling in diabetic kidney disease: is connective tissue growth factor (CTGF, CCN2) the perfect intervention point? Nephrol. Dial. Transpl. 20, 6–10 (2005).
Riser, B. L. et al. Regulation of connective tissue growth factor activity in cultured rat mesangial cells and its expression in experimental diabetic glomerulosclerosis. J. Am. Soc. Nephrol. 11, 25–38 (2000).
Wahab, N. A., Weston, B. S. & Mason, R. M. Connective tissue growth factor CCN2 interacts with and activates the tyrosine kinase receptor TrkA. J. Am. Soc. Nephrol. 16, 340–351 (2005).
Guha, M., Xu, Z. G., Tung, D., Lanting, L. & Natarajan, R. Specific down-regulation of connective tissue growth factor attenuates progression of nephropathy in mouse models of type 1 and type 2 diabetes. FASEB J. 21, 3355–3368 (2007).
Adler, S. G. et al. Phase 1 study of anti-CTGF monoclonal antibody in patients with diabetes and microalbuminuria. Clin. J. Am. Soc. Nephrol. 5, 1420–1428 (2010).
Vallon, V. & Thomson, S. C. The tubular hypothesis of nephron filtration and diabetic kidney disease. Nat. Rev. Nephrol. 16, 317–336 (2020).
Fine, L. G., Orphanides, C. & Norman, J. T. Progressive renal disease: the chronic hypoxia hypothesis. Kidney Int. Suppl. 65, S74–S78 (1998). Early review proposing renal hypoxia as a causative factor in the development of DKD.
Mimura, I. & Nangaku, M. The suffocating kidney: tubulointerstitial hypoxia in end-stage renal disease. Nat. Rev. Nephrol. 6, 667–678 (2010).
Korner, A., Eklof, A. C., Celsi, G. & Aperia, A. Increased renal metabolism in diabetes. Mechanism and functional implications. Diabetes 43, 629–633 (1994).
Layton, A. T., Vallon, V. & Edwards, A. Predicted consequences of diabetes and SGLT inhibition on transport and oxygen consumption along a rat nephron. Am. J. Physiol. Ren. Physiol. 310, F1269–F1283 (2016). Review of oxygen consumption by nephron segments and the predicted effect of SGLT2 inhibition on sodium transport and oxygen utlization in these segments.
Soltoff, S. P. ATP and the regulation of renal cell function. Annu. Rev. Physiol. 48, 9–31 (1986).
Layton, A. T., Laghmani, K., Vallon, V. & Edwards, A. Solute transport and oxygen consumption along the nephrons: effects of Na+ transport inhibitors. Am. J. Physiol. Ren. Physiol. 311, F1217–F1229 (2016).
Franzen, S., Pihl, L., Khan, N., Gustafsson, H. & Palm, F. Pronounced kidney hypoxia precedes albuminuria in type 1 diabetic mice. Am. J. Physiol. Ren. Physiol. 310, F807–F809 (2016).
Blantz, R. C., Deng, A., Miracle, C. M. & Thomson, S. C. Regulation of kidney function and metabolism: a question of supply and demand. Trans. Am. Clin. Climatol. Assoc. 118, 23–43 (2007).
Inoue, T. et al. Noninvasive evaluation of kidney hypoxia and fibrosis using magnetic resonance imaging. J. Am. Soc. Nephrol. 22, 1429–1434 (2011).
Basile, D. P., Donohoe, D., Roethe, K. & Osborn, J. L. Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am. J. Physiol. Ren. Physiol. 281, F887–F899 (2001).
Kong, T., Eltzschig, H. K., Karhausen, J., Colgan, S. P. & Shelley, C. S. Leukocyte adhesion during hypoxia is mediated by HIF-1-dependent induction of beta2 integrin gene expression. Proc. Natl Acad. Sci. USA 101, 10440–10445 (2004).
Postlethwaite, A. E., Shigemitsu, H. & Kanangat, S. Cellular origins of fibroblasts: possible implications for organ fibrosis in systemic sclerosis. Curr. Opin. Rheumatol. 16, 733–738 (2004).
Deng, A. et al. Renal protection in chronic kidney disease: hypoxia-inducible factor activation vs. angiotensin II blockade. Am. J. Physiol. Renal Physiol. 299, F1365–F1373 (2010).
Rosenberger, C. et al. Adaptation to hypoxia in the diabetic rat kidney. Kidney Int. 73, 34–42 (2008).
Eckardt, K. U., Bernhardt, W., Willam, C. & Wiesener, M. Hypoxia-inducible transcription factors and their role in renal disease. Semin. Nephrol. 27, 363–372 (2007).
Persson, P. & Palm, F. Hypoxia-inducible factor activation in diabetic kidney disease. Curr. Opin. Nephrol. Hypertens. 26, 345–350 (2017). Supporting evidence for the role of HIF and renal hypoxia in the development of DKD.
Garcia-Pastor, C., Benito-Martinez, S., Moreno-Manzano, V., Fernandez-Martinez, A. B. & Lucio-Cazana, F. J. Mechanism and consequences of The impaired Hif-1alpha response to hypoxia in human proximal tubular HK-2 cells exposed to high glucose. Sci. Rep. 9, 15868 (2019).
O’Neill, J. et al. Acute SGLT inhibition normalizes O2 tension in the renal cortex but causes hypoxia in the renal medulla in anaesthetized control and diabetic rats. Am. J. Physiol. Renal Physiol. 309, F227–F234 (2015).
Ghanim, H. et al. Dapagliflozin suppresses hepcidin and increases erythropoiesis. J. Clin. Endocrinol. Metab. 105, dgaa057 (2020).
Mudaliar, S., Alloju, S. & Henry, R. R. Can a shift in fuel energetics explain the beneficial cardiorenal outcomes in the EMPA-REG OUTCOME Study? A unifying hypothesis. Diabetes Care 39, 1115–1122 (2016). Hypothesis and supporting evidence for energy depravation in the aetiology of diabetic renal disease.
Little, J. R. & Spitzer, J. J. Uptake of ketone bodies by dog kidney in vivo. Am. J. Physiol. 221, 679–683 (1971).
Sato, K. et al. Insulin, ketone bodies, and mitochondrial energy transduction. FASEB J. 9, 651–658 (1995).
Ferrannini, E., Mark, M. & Mayoux, E. CV Protection in the EMPA-REG OUTCOME Trial: a “thrifty substrate” hypothesis. Diabetes Care 39, 1108–1114 (2016). Novel hypothesis that ketones function as a “super fuel” for the heart and explain, in part, the beneficial cardiovascular effects of the SGLT2 inhibitor class of drugs.
Scandling, J. D. & Myers, B. D. Glomerular size-selectivity and microalbuminuria in early diabetic glomerular disease. Kidney Int. 41, 840–846 (1992).
Nakamura, Y. & Myers, B. D. Charge selectivity of proteinuria in diabetic glomerulopathy. Diabetes 37, 1202–1211 (1988).
Steffes, M. W., Schmidt, D., McCrery, R., Basgen, J. M. & International Diabetic Nephropathy Study Group. Glomerular cell number in normal subjects and in type 1 diabetic patients. Kidney Int. 59, 2104–2113 (2001).
Pagtalunan, M. E. et al. Podocyte loss and progressive glomerular injury in type II diabetes. J. Clin. Invest. 99, 342–348 (1997). Renal biopsy study in Pima Indians with type 2 diabetes with varying degrees of kidney disease demonstrating that with advancing severity of glomerulosclerosis there is a progressive loss of podocytes.
Tamsma, J. T. et al. Expression of glomerular extracellular matrix components in human diabetic nephropathy: decrease of heparan sulphate in the glomerular basement membrane. Diabetologia 37, 313–320 (1994).
de Vries, A. P. et al. Fatty kidney: emerging role of ectopic lipid in obesity-related renal disease. Lancet Diabetes Endocrinol. 2, 417–426 (2014). Review of evidence supporting lipid deposition in the kidney as a causative factor in the development of obesity-related glomerulosclerosis and hyperfiltration, as a distinct entity from diabetic nephropathy.
Nishi, H. & Nangaku, M. Podocyte lipotoxicity in diabetic kidney disease. Kidney Int. 96, 809–812 (2019).
Sieber, J. et al. Regulation of podocyte survival and endoplasmic reticulum stress by fatty acids. Am. J. Physiol. Ren. Physiol. 299, F821–F829 (2010).
Wang, Z. et al. Regulation of renal lipid metabolism, lipid accumulation, and glomerulosclerosis in FVBdb/db mice with type 2 diabetes. Diabetes 54, 2328–2335 (2005).
Hale, L. J. & Coward, R. J. The insulin receptor and the kidney. Curr. Opin. Nephrol. Hypertens. 22, 100–106 (2013).
Welsh, G. I. et al. Insulin signaling to the glomerular podocyte is critical for normal kidney function. Cell Metab. 12, 329–340 (2010).
Russo, L. M. et al. Impaired tubular uptake explains albuminuria in early diabetic nephropathy. J. Am. Soc. Nephrol. 20, 489–494 (2009).
Abbate, M., Zoja, C. & Remuzzi, G. How does proteinuria cause progressive renal damage? J. Am. Soc. Nephrol. 17, 2974–2984 (2006).
Burton, C. & Harris, K. P. The role of proteinuria in the progression of chronic renal failure. Am. J. Kidney Dis. 27, 765–775 (1996).
Dixon, R. & Brunskill, N. J. Activation of mitogenic pathways by albumin in kidney proximal tubule epithelial cells: implications for the pathophysiology of proteinuric states. J. Am. Soc. Nephrol. 10, 1487–1497 (1999).
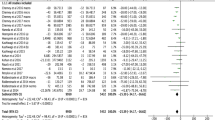
Heerspink, H. J. L. et al. Change in albuminuria as a surrogate endpoint for progression of kidney disease: a meta-analysis of treatment effects in randomised clinical trials. Lancet Diabetes Endocrinol. 7, 128–139 (2019). Metaanalysis proposing albuminuria as a surrogate end point for progression of renal disease and providing evidence for a toxic effect of albumin on the kidney.
Cassis, P. et al. SGLT2 inhibitor dapagliflozin limits podocyte damage in proteinuric nondiabetic nephropathy. JCI Insight 3, e98720 (2018).
Korbut, A. I. et al. SGLT2 inhibitor empagliflozin and DPP4 inhibitor linagliptin reactivate glomerular autophagy in db/db Mice, a model of type 2 diabetes. Int. J. Mol. Sci. 21, 2987 (2020).
Herman-Edelstein, M., Scherzer, P., Tobar, A., Levi, M. & Gafter, U. Altered renal lipid metabolism and renal lipid accumulation in human diabetic nephropathy. J. Lipid Res. 55, 561–572 (2014).
Chen, H. M. et al. Podocyte lesions in patients with obesity-related glomerulopathy. Am. J. Kidney Dis. 48, 772–779 (2006).
Sharma, S. G. et al. The modern spectrum of renal biopsy findings in patients with diabetes. Clin. J. Am. Soc. Nephrol. 8, 1718–1724 (2013).
Belfort, R. et al. Dose-response effect of elevated plasma free fatty acid on insulin signaling. Diabetes 54, 1640–1648 (2005).
Kashyap, S. et al. A sustained increase in plasma free fatty acids impairs insulin secretion in nondiabetic subjects genetically predisposed to develop type 2 diabetes. Diabetes 52, 2461–2474 (2003).
Cooper, M. E. & Jandeleit-Dahm, K. A. Lipids and diabetic renal disease. Curr. Diab Rep. 5, 445–448 (2005). Review of evidence supporting glomerular and tubular lipid deposition in the development of diabetic kidney injury.
Shevalye, H. et al. Prediabetic nephropathy as an early consequence of the high-calorie/high-fat diet: relation to oxidative stress. Endocrinology 153, 1152–1161 (2012).
Sun, Y. B. et al. Smad3 deficiency protects mice from obesity-induced podocyte injury that precedes insulin resistance. Kidney Int. 88, 286–298 (2015).
Grove, K. J. et al. Diabetic nephropathy induces alterations in the glomerular and tubule lipid profiles. J. Lipid Res. 55, 1375–1385 (2014).
Jiang, T. et al. Diet-induced obesity in C57BL/6J mice causes increased renal lipid accumulation and glomerulosclerosis via a sterol regulatory element-binding protein-1c-dependent pathway. J. Biol. Chem. 280, 32317–32325 (2005).
Zhao, X. et al. Kidney injury molecule-1 is upregulated in renal lipotoxicity and mediates palmitate-induced tubular cell injury and inflammatory response. Int J. Mol. Sci. 20, 3406 (2019).
Kim, M. Y. et al. Resveratrol prevents renal lipotoxicity and inhibits mesangial cell glucotoxicity in a manner dependent on the AMPK-SIRT1-PGC1alpha axis in db/db mice. Diabetologia 56, 204–217 (2013).
Rosca, M. G. et al. Oxidation of fatty acids is the source of increased mitochondrial reactive oxygen species production in kidney cortical tubules in early diabetes. Diabetes 61, 2074–2083 (2012).
Ohse, T. et al. Albumin induces endoplasmic reticulum stress and apoptosis in renal proximal tubular cells. Kidney Int. 70, 1447–1455 (2006).
Falkevall, A. et al. Reducing VEGF-B signaling ameliorates renal lipotoxicity and protects against diabetic kidney disease. Cell Metab. 25, 713–726 (2017).
Ferrannini, E. et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J. Clin. Invest. 124, 499–508 (2014).
Nikolic-Paterson, D. J. & Atkins, R. C. The role of macrophages in glomerulonephritis. Nephrol. Dial. Transpl. 16, 3–7 (2001).
Perez-Morales, R. E. et al. Inflammation in diabetic kidney disease. Nephron 143, 12–16 (2019). Review of inflammatory pathways that are activated in animal models of diabetes and their potential role in the development of diabetic nephropathy.
Alicic, R. Z., Johnson, E. J. & Tuttle, K. R. Inflammatory mechanisms as new biomarkers and therapeutic targets for diabetic kidney disease. Adv. Chronic Kidney Dis. 25, 181–191 (2018).
Ruster, C. & Wolf, G. The role of chemokines and chemokine receptors in diabetic nephropathy. Front. Biosci. 13, 944–955 (2008).
Dekkers, C. C. J. et al. Effects of the SGLT-2 inhibitor dapagliflozin on glomerular and tubular injury markers. Diabetes Obes. Metab. 20, 1988–1993 (2018).
Okada, S. et al. Intercellular adhesion molecule-1-deficient mice are resistant against renal injury after induction of diabetes. Diabetes 52, 2586–2593 (2003).
Nguyen, D. et al. Macrophage accumulation in human progressive diabetic nephropathy. Nephrology 11, 226–231 (2006).
You, H., Gao, T., Cooper, T. K., Brian Reeves, W. & Awad, A. S. Macrophages directly mediate diabetic renal injury. Am. J. Physiol. Renal Physiol. 305, F1719–F1727 (2013).
Awad, A. S. et al. Monocyte/macrophage chemokine receptor CCR2 mediates diabetic renal injury. Am. J. Physiol. Renal Physiol. 301, F1358–F1366 (2011).
de Zeeuw, D. et al. The effect of CCR2 inhibitor CCX140-B on residual albuminuria in patients with type 2 diabetes and nephropathy: a randomised trial. Lancet Diabetes Endocrinol. 3, 687–696 (2015).
Sriwijitkamol, A. et al. Reduced skeletal muscle inhibitor of kappaB beta content is associated with insulin resistance in subjects with type 2 diabetes: reversal by exercise training. Diabetes 55, 760–767 (2006).
Barnes, P. J. & Karin, M. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N. Engl. J. Med. 336, 1066–1071 (1997).
de Zeeuw, D. et al. Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N. Engl. J. Med. 369, 2492–2503 (2013).
Marrero, M. B., Banes-Berceli, A. K., Stern, D. M. & Eaton, D. C. Role of the JAK/STAT signaling pathway in diabetic nephropathy. Am. J. Physiol. Renal Physiol. 290, F762–F768 (2006).
Berthier, C. C. et al. Enhanced expression of Janus kinase-signal transducer and activator of transcription pathway members in human diabetic nephropathy. Diabetes 58, 469–477 (2009).
Choudhury, G. G., Ghosh-Choudhury, N. & Abboud, H. E. Association and direct activation of signal transducer and activator of transcription1alpha by platelet-derived growth factor receptor. J. Clin. Invest. 101, 2751–2760 (1998).
Woroniecka, K. I. et al. Transcriptome analysis of human diabetic kidney disease. Diabetes 60, 2354–2369 (2011).
Brosius, F. C. III & He, J. C. JAK inhibition and progressive kidney disease. Curr. Opin. Nephrol. Hypertens. 24, 88–95 (2015).
Zhang, H. et al. Podocyte-specific JAK2 overexpression worsens diabetic kidney disease in mice. Kidney Int. 92, 909–921 (2017).
Tuttle, K. R. et al. JAK1/JAK2 inhibition by baricitinib in diabetic kidney disease: results from a Phase 2 randomized controlled clinical trial. Nephrol. Dial. Transpl. 33, 1950–1959 (2018).
Ortiz-Munoz, G. et al. Suppressors of cytokine signaling abrogate diabetic nephropathy. J. Am. Soc. Nephrol. 21, 763–772 (2010).
Amiri, F. et al. Angiotensin II activation of the JAK/STAT pathway in mesangial cells is altered by high glucose. Kidney Int. 61, 1605–1616 (2002).
Bonnet, F. & Scheen, A. J. Effects of SGLT2 inhibitors on systemic and tissue low-grade inflammation: the potential contribution to diabetes complications and cardiovascular disease. Diabetes Metab. 44, 457–464 (2018).
Yaribeygi, H., Butler, A. E., Atkin, S. L., Katsiki, N. & Sahebkar, A. Sodium-glucose cotransporter 2 inhibitors and inflammation in chronic kindey disease: possible molecualr pathways. J. Cell Physiol. 234, 223–230 (2019).
Jaikumkao, K. et al. Dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, slows the progression of renal complications through the suppression of renal inflammation, endoplasmic reticulum stress and apoptosis in prediabetic rats. Diabetes Obes. Metab. 20, 2617–2626 (2018).
Kim, S. R. et al. SGLT2 inhibition modulates NLRP3 inflammasome activity via ketones and insulin in diabetes with cardiovascular disease. Nat. Commun. 11, 2127 (2020).
Heerspink, H. J. L. et al. Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia 62, 1154–1166 (2019).
Lee, T. M., Chang, N. C. & Lin, S. Z. Dapagliflozin, a selective SGLT2 Inhibitor, attenuated cardiac fibrosis by regulating the macrophage polarization via STAT3 signaling in infarcted rat hearts. Free Radic. Biol. Med. 104, 298–310 (2017).
Kang, S. et al. Direct effects of empagliflozin on extracellular matrix remodeling in human cardiac fibroblasts: novel translational clues to EMPA-REG Outcome. Can. J. Cardiol. 33, S169 (2017).
Goligorsky, M. S., Chen, J. & Brodsky, S. Workshop: endothelial cell dysfunction leading to diabetic nephropathy: focus on nitric oxide. Hypertension 37, 744–748 (2001).
Xia, Y., Dawson, V. L., Dawson, T. M., Snyder, S. H. & Zweier, J. L. Nitric oxide synthase generates superoxide and nitric oxide in arginine-depleted cells leading to peroxynitrite-mediated cellular injury. Proc. Natl Acad. Sci. USA 93, 6770–6774 (1996).
Brodsky, S. V., Gao, S., Li, H. & Goligorsky, M. S. Hyperglycemic switch from mitochondrial nitric oxide to superoxide production in endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 283, H2130–H2139 (2002).
Wang, C. H. et al. A modest decrease in endothelial NOS in mice comparable to that associated with human NOS3 variants exacerbates diabetic nephropathy. Proc. Natl Acad. Sci. USA 108, 2070–2075 (2011).
Zhao, H. J. et al. Endothelial nitric oxide synthase deficiency produces accelerated nephropathy in diabetic mice. J. Am. Soc. Nephrol. 17, 2664–2669 (2006).
Morris, S. M. Jr. Gao, T., Cooper, T. K., Kepka-Lenhart, D. & Awad, A. S. Arginase-2 mediates diabetic renal injury. Diabetes 60, 3015–3022 (2011).
You, H., Gao, T., Cooper, T. K., Morris, S. M. Jr. & Awad, A. S. Arginase inhibition: a new treatment for preventing progression of established diabetic nephropathy. Am. J. Physiol. Ren. Physiol. 309, F447–F455 (2015). Evidence supporting the role of arginase inhibition in preventing kidney disease in a murine model of diabetes.
You, H., Gao, T., Cooper, T. K., Morris, S. M. Jr. & Awad, A. S. Arginase inhibition mediates renal tissue protection in diabetic nephropathy by a nitric oxide synthase 3-dependent mechanism. Kidney Int. 84, 1189–1197 (2013).
Forbes, J. M. & Cooper, M. E. Mechanisms of diabetic complications. Physiol. Rev. 93, 137–188 (2013).
Badal, S. S. & Danesh, F. R. New insights into molecular mechanisms of diabetic kidney disease. Am. J. Kidney Dis. 63, S63–S83 (2014).
Nishikawa, T. et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 404, 787–790 (2000).
Mulder, S. et al. A metabolomics-based molecular pathway analysis of how the sodium-glucose co-transporter-2 inhibitor dapagliflozin may slow kidney function decline in patients with diabetes. Diabetes Obes. Metab. 22, 1157–1166 (2020).
Shigiyama, F. et al. Effectiveness of dapagliflozin on vascular endothelial function and glycemic control in patients with early-stage type 2 diabetes mellitus: DEFENCE study. Cardiovasc. Diabetol. 16, 84 (2017).
Tanaka, A. et al. Effect of empagliflozin on endothelial function in patients with type 2 diabetes and cardiovascular disease: results from the multicenter, randomized, placebo-controlled, double-blind EMBLEM trial. Diabetes Care 42, e159–e161 (2019).
Ishibashi, Y., Matsui, T. & Yamagishi, S. Tofogliflozin, a highly selective inhibitor of SGLT2 blocks proinflammatory and proapoptotic effects of glucose overload on proximal tubular cells partly by suppressing oxidative stress generation. Horm. Metab. Res. 48, 191–195 (2016).
Salim, H. M. et al. Glycemic control with ipragliflozin, a novel selective SGLT2 inhibitor, ameliorated endothelial dysfunction in streptozotocin-induced diabetic mouse. Front. Cardiovasc. Med. 3, 43 (2016).
Juni, R. R. Cardiac microvascular endothelial enhancement of cardiomyocyte function is impaired by inflammation and restored by empagliflozin. JACC BasicTransl. Sci. 4, 575–591 (2019).
Sharma, K. Mitochondrial hormesis and diabetic complications. Diabetes 64, 663–672 (2015). Interesting review about the role and source of ROS in the development of DKD and challenging the dogma that ROS are derived from mitochondrial overproduction.
Zhan, M., Brooks, C., Liu, F., Sun, L. & Dong, Z. Mitochondrial dynamics: regulatory mechanisms and emerging role in renal pathophysiology. Kidney Int. 83, 568–581 (2013).
Funk, J. A., Odejinmi, S. & Schnellmann, R. G. SRT1720 induces mitochondrial biogenesis and rescues mitochondrial function after oxidant injury in renal proximal tubule cells. J. Pharmacol. Exp. Ther. 333, 593–601 (2010).
Scarpulla, R. C. Transcriptional paradigms in mammalian mitochondrial biogenesis and function. Physiol. Rev. 88, 611–638 (2008).
Sharma, K. et al. Metabolomics reveals signature of mitochondrial dysfunction in diabetic kidney disease. J. Am. Soc. Nephrol. 24, 1901–1912 (2013).
Rasbach, K. A. & Schnellmann, R. G. PGC-1alpha over-expression promotes recovery from mitochondrial dysfunction and cell injury. Biochem. Biophys. Res. Commun. 355, 734–739 (2007).
Zhao, M. et al. PGC-1alpha overexpression protects against aldosterone-induced podocyte depletion: role of mitochondria. Oncotarget 7, 12150–12162 (2016).
Sharma, K. Obesity and diabetic kidney disease: role of oxidant stress and redox balance. Antioxid. Redox Signal. 25, 208–216 (2016).
Sedeek, M. et al. Critical role of Nox4-based NADPH oxidase in glucose-induced oxidative stress in the kidney: implications in type 2 diabetic nephropathy. Am. J. Physiol. Renal Physiol. 299, F1348–F1358 (2010).
Gorin, Y. et al. Targeting NADPH oxidase with a novel dual Nox1/Nox4 inhibitor attenuates renal pathology in type 1 diabetes. Am. J. Physiol. Renal Physiol. 308, F1276–F1287 (2015).
Gray, S. P. et al. Combined NOX1/4 inhibition with GKT137831 in mice provides dose-dependent reno- and atheroprotection even in established micro- and macrovascular disease. Diabetologia 60, 927–937 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02010242 (2015).
Takagi, S. et al. Ipragliflozin improves mitochondrial abnormalities in renal tubules induced by a high-fat diet. J. Diabetes Investig. 9, 1025–1032 (2018).
Ishibashi, Y., Matsui, T., Yamagishi, S. & Tofogliflozin, A. Highly selective inhibitor of SGLT2 blocks proinflammatory and proapoptotic effects of glucose overload on proximal tubular cells partly by suppressing oxidative stress generation. Horm. Metab. Res. 48, 191–195 (2016).
Fioretto, P., Zambon, A., Rassato, M., Busetto, L. & Vettor, R. SGLT inhibitors and the diabetic kidney. Diabetes Care 39, S165–S171 (2016).
Bielesz, B. et al. Epithelial Notch signaling regulates interstitial fibrosis development in the kidneys of mice and humans. J. Clin. Invest. 120, 4040–4054 (2010).
Mariappan, M. M. et al. Combined acute hyperglycemic and hyperinsulinemic clamp induced profibrotic and proinflammatory responses in the kidney. Am. J. Physiol. Cell Physiol. 306, C202–C211 (2014). This study documents that hyperinsulinaemia, as a compensatory response to insulin resistance, activates multiple profibrotic and pro-inflammatory genes in the kidney.
Park, I. S., Kiyomoto, H., Abboud, S. L. & Abboud, H. E. Expression of transforming growth factor-beta and type IV collagen in early streptozotocin-induced diabetes. Diabetes 46, 473–480 (1997).
Meng, X. M., Nikolic-Paterson, D. J. & Lan, H. Y. TGF-β: the master regulator of fibrosis. Nat. Rev. Nephrol. 12, 325–338 (2016). Excellent review on the role of TGFβ in chronic kidney disease.
Hunt, K. J. et al. Levels of connective tissue growth factor (CTGF) predict development of kidney dysfunction in type 2 diabetes — the VADT study. Diabetes https://doi.org/10.2337/db18-528-P (2018).
Rysz, J. et al. Serum matrix metalloproteinases MMP-2 and MMP-9 and metalloproteinase tissue inhibitors TIMP-1 and TIMP-2 in diabetic nephropathy. J. Nephrol. 20, 444–452 (2007).
Vallon, V. The proximal tubule in the pathophysiology of the diabetic kidney. Am. J. Physiol. Regul. Integr. Comp. Physiol. 300, R1009–R1022 (2011).
Koszegi, S. et al. RAAS inhibitors directly reduce diabetes-induced renal fibrosis via growth factor inhibition. J. Physiol. 597, 193–209 (2019).
Panchapakesan, U. et al. Effects of SGLT2 inhibition in human kidney proximal tubular cells–renoprotection in diabetic nephropathy? PLoS One 8, e54442 (2013).
Li, C. et al. SGLT2 inhibition with empagliflozin attenuates myocardial oxidative stress and fibrosis in diabetic mice heart. Cardiovasc. Diabetol. 18, 15 (2019).
Kang, S. et al. Direct effects of empagliflozin on extracellular matrix remodelling in human cardiac myofibroblasts: novel translational clues to explain EMPA-REG OUTCOME results. Can. J. Cardiol. 36, 543–553 (2020).
Packer, M. Activation and inhibition of sodium-hydrogen exchanger is a mechanism that links the pathophysiology and treatment of diabetes mellitus with that of heart failure. Circulation 136, 1548–1559 (2017). Comprehensive overview of the role of the NHE in the development of myocardial fibrosis, oxidative stress, inflammation and cardiac remodelling.
Wilcox, C. S. Antihypertensive and renal mechanisms of SGLT2 (Sodium-Glucose Linked Transporter 2) inhibitors. Hypertension 75, 894–901 (2020).
Klisic, J., Nief, V., Reyes, L. & Ambuhl, P. M. Acute and chronic regulation of the renal Na/H+ exchanger NHE3 in rats with STZ-induced diabetes mellitus. Nephron Physiol. 102, 27–35 (2006).
Beloto-Silva, O., Machado, U. F. & Oliveira-Souza, M. Glucose-induced regulation of NHEs activity and SGLTs expression involves the PKA signaling pathway. J. Membr. Biol. 239, 157–165 (2011).
Ganz, M. B., Hawkins, K. & Reilly, R. F. High glucose induces the activity and expression of Na(+)/H(+) exchange in glomerular mesangial cells. Am. J. Physiol. Renal Physiol. 278, F91–F96 (2000).
Thomson, S. C. & Vallon, V. Renal effects of sodium-glucose co-transporter inhibitors. Am. J. Med. 132, S30–S38 (2019). The review emphasizes the link between SGLT2 inhibitors and NHE in the development of DKD.
Coady, M. J. et al. MAP17 is a necessary activator of renal Na+/Glucose cotransporter SGLT2. J. Am. Soc. Nephrol. 28, 85–93 (2017). This article demonstrates that MAP links SGLT and NHE, providing a mechanism via which SGLT2 inhibitors can block the sodium–hydrogen exchanger.
Inoue, B. H. et al. Increased NHE3 abundance and transport activity in renal proximal tubule of rats with heart failure. Am. J. Physiol. Regul. Integr. Comp. Physiol. 302, R166–R174 (2012).
Baartscheer, A. et al. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia 60, 568–573 (2017).
von Lewinski, D. et al. Glucose-transporter-mediated positive inotropic effects in human myocardium of diabetic and nondiabetic patients. Metabolism 59, 1020–1028 (2010).
Pessoa, T. D., Campos, L. C., Carraro-Lacroix, L., Girardi, A. C. & Malnic, G. Functional role of glucose metabolism, osmotic stress, and sodium-glucose cotransporter isoform-mediated transport on Na+/H+ exchanger isoform 3 activity in the renal proximal tubule. J. Am. Soc. Nephrol. 25, 2028–2039 (2014).
Onishi, A. et al. Effect of renal tubule-specific knockdown of the Na+/H+ exchanger NHE3 in Akita diabetic mice. Am. J. Physiol. Renal Physiol. 317, F419–F434 (2019).
Cuervo, A. M. et al. Autophagy and aging: the importance of maintaining “clean” cells. Autophagy 1, 131–140 (2005).
Jheng, H. F. et al. Mitochondrial fission contributes to mitochondrial dysfunction and insulin resistance in skeletal muscle. Mol. Cell Biol. 32, 309–319 (2012).
Huber, T. B. et al. Emerging role of autophagy in kidney function, diseases and aging. Autophagy 8, 1009–1031 (2012).
Higgins, G. C. & Coughlan, M. T. Mitochondrial dysfunction and mitophagy: the beginning and end to diabetic nephropathy? Br. J. Pharmacol. 171, 1917–1942 (2014).
Lin, T.-A., Wu, V. C.-C. & Wang, C.-Y. Autophagy in chronic kidney disease. Cells 8, 61 (2019). Up-to-date review on the role of autophagy in the development of chronic kidney disease.
Ding, Y. & Choi, M. E. Autophagy in diabetic nephropathy. J. Endocrinol. 224, R15–R30 (2015).
Xin, W. et al. Autophagy protects human podocytes from high glucose-induced injury by preventing insulin resistance. Metabolism 65, 1307–1315 (2016).
Kitada, M. et al. Dietary restriction ameliorates diabetic nephropathy through anti-inflammatory effects and regulation of the autophagy via restoration of Sirt1 in diabetic Wistar fatty (fa/fa) rats: a model of type 2 diabetes. Exp. Diabetes Res. 2011, 908185 (2011).
Lee, S.-Y. et al. PGC1 α activators mitigate diabetic tubulopathy by improving mitochondrial dynamics and quality control. J. Diabetes Res. 2017, 6483572 (2017).
Yu, L. et al. Termination of autophagy and reformation of lysosomes regulated by mTOR. Nature 465, 942–946 (2010).
Lee, Y. H. et al. Empagliflozin attenuates diabetic tubulopathy by improving mitochondrial fragmentation and autophagy. Am. J. Physiol. Renal Physiol. 317, F767–F780 (2019).
Hawley S. A. et al. Diabetes 65, 2784–2794 (2016).
Daniele, G. et al. Dapagliflozin enhances fat oxidation and ketone production in patients with type 2 diabetes. Diabetes Care 39, 2036–2041 (2016). This article demonstrates that SGLT2 inhibitors create a state of energy depletion, which can secondarily improve autophagy and mitochondrial dysfunction in patients with type 2 diabetes.
Ferrannini, E. et al. Shift to fatty substrate utilization in response to sodium-glucose cotransporter 2 inhibition in subjects without diabetes and patients with type 2 diabetes. Diabetes 65, 1190–1195 (2016).
Acknowledgements
The authors wish to thank Lorrie Albarado (UT Health, San Antonio, Texas) for assistance in the preparation of the manuscript before submission.
Author information
Authors and Affiliations
Contributions
A.S.A. and R.A.D. wrote the first draft of the manuscript, which was subsequently revised by all authors. The final version of the manuscript was reviewed by all authors.
Corresponding author
Ethics declarations
Competing interests
R.A.D. is a member of the Speakers Bureau for AstraZeneca and Novo Nordisk, a member of the Advisory Board of AstraZeneca, Janssen, Intarcia and Boehringer-Ingelheim, and has received research grants from AstraZeneca, Janssen and Merck. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Nephrology thanks C. Pollock, A. Scheen and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Angiotensin escape
-
The inability of angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers to reduce circulating angiotensin II concentrations to undetectable levels.
- Aldosterone escape
-
The inability of angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers to reduce circulating aldosterone concentrations to undetectable levels.
- BOLD-MRI
-
Blood oxygen level-dependent (BOLD)-MRI represents a non-invasive technique for assessing renal hypoxia by measuring tissue oxygen bioavailability through measurements of relative changes in deoxyhaemoglobin.
- Mitochondrial fission
-
The splitting of mitochondria into two, which, together with mitochondrial fusion, is required for mitochondrial homeostasis.
- Mitochondrial fusion
-
The combining of two mitochondria, which, together with mitochondrial fission, is required for mitochondrial homeostasis.
Rights and permissions
About this article
Cite this article
DeFronzo, R.A., Reeves, W.B. & Awad, A.S. Pathophysiology of diabetic kidney disease: impact of SGLT2 inhibitors. Nat Rev Nephrol 17, 319–334 (2021). https://doi.org/10.1038/s41581-021-00393-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-021-00393-8
This article is cited by
-
SGLT2 inhibition, high-density lipoprotein, and kidney function: a mendelian randomization study
Lipids in Health and Disease (2024)
-
Progress and application of adipose-derived stem cells in the treatment of diabetes and its complications
Stem Cell Research & Therapy (2024)
-
ALCAT1-mediated abnormal cardiolipin remodelling promotes mitochondrial injury in podocytes in diabetic kidney disease
Cell Communication and Signaling (2024)
-
Angiotensin II type 1 receptor-associated protein deletion combined with angiotensin II stimulation accelerates the development of diabetic kidney disease in mice on a C57BL/6 strain
Hypertension Research (2024)
-
CCDC92 promotes podocyte injury by regulating PA28α/ABCA1/cholesterol efflux axis in type 2 diabetic mice
Acta Pharmacologica Sinica (2024)