Abstract
As the prevalence of diabetes continues to climb, the number of individuals living with diabetic complications will reach an unprecedented magnitude. The emergence of new glucose-lowering agents — sodium–glucose cotransporter 2 inhibitors and incretin therapies — has markedly changed the treatment landscape of type 2 diabetes mellitus. In addition to effectively lowering glucose, incretin drugs, which include glucagon-like peptide 1 receptor (GLP1R) agonists and dipeptidyl peptidase 4 (DPP4) inhibitors, can also reduce blood pressure, body weight, the risk of developing or worsening chronic kidney disease and/or atherosclerotic cardiovascular events, and the risk of death. Although kidney disease events have thus far been secondary outcomes in clinical trials, an ongoing phase III trial in patients with diabetic kidney disease will test the effect of a GLP1R agonist on a primary kidney disease outcome. Experimental data have identified the modulation of innate immunity and inflammation as plausible biological mechanisms underpinning the kidney-protective effects of incretin-based agents. These drugs block the mechanisms involved in the pathogenesis of kidney damage, including the activation of resident mononuclear phagocytes, tissue infiltration by non-resident inflammatory cells, and the production of pro-inflammatory cytokines and adhesion molecules. GLP1R agonists and DPP4 inhibitors might also attenuate oxidative stress, fibrosis and cellular apoptosis in the kidney.
Key points
-
Glucagon-like peptide 1 receptor (GLP1R) agonists and dipeptidyl peptidase 4 (DPP4) inhibitors reduce the onset and progression of albuminuria in patients with type 2 diabetes mellitus (T2DM).
-
GLP1R agonists have been shown to delay the decline of estimated glomerular filtration rate in patients with T2DM, including those with or without moderate-to-severe chronic kidney disease. DPP4 inhibitors demonstrate only modest improvement in albuminuria, with no effect on glomerular filtration rate.
-
The kidney-protective effects of GLP1R agonists might be at least partly independent of their effects on glycaemic control.
-
In addition to improved glycaemic control, GLP1R agonists demonstrate a direct effect on the reduction of both systemic and local inflammation, which is a plausible mechanism underpinning kidney protection.
-
Experimental data show that incretin-based therapies block inflammatory cell infiltration and reduce the expression of anti-fibrotic and anti-inflammatory mediators in the diabetic kidney.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Levin, A. et al. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet 390, 1888–1917 (2017).
Saran, R. et al. US renal data system 2018 annual data report: epidemiology of kidney disease in the United States. Am. J. Kidney Dis. 73 (Suppl. 1), A7–A8 (2019).
United States Renal Data System. 2019 Annual Data Report (USRDS, 2020).
Saeedi, P. et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 157, 107843 (2019).
National Kidney Foundation. KDOQI clinical practice guideline for diabetes and CKD: 2012 Update. Am. J. Kidney Dis. 60, 850–886 (2012).
ADA. Standards of medical care in diabetes - 2020. Diabetes Care 43, S1–S212 (2020).
Cea Soriano, L., Johansson, S., Stefansson, B. & Rodriguez, L. A. Cardiovascular events and all-cause mortality in a cohort of 57,946 patients with type 2 diabetes: associations with renal function and cardiovascular risk factors. Cardiovasc. Diabetol. 14, 38 (2015).
Scirica, B. M. et al. Cardiovascular outcomes according to urinary albumin and kidney disease in patients with type 2 diabetes at high cardiovascular risk: observations from the SAVOR-TIMI 53 trial. JAMA Cardiol. 3, 155–163 (2018).
Afkarian, M. et al. Kidney disease and increased mortality risk in type 2 diabetes. J. Am. Soc. Nephrol. 24, 302–308 (2013).
Daratha, K. B. et al. Risks of subsequent hospitalization and death in patients with kidney disease. Clin. J. Am. Soc. Nephrol. 7, 409–416 (2012).
Gregg, E. W. et al. Changes in diabetes-related complications in the United States, 1990-2010. N. Engl. J. Med. 370, 1514–1523 (2014).
Harding, J. L., Pavkov, M. E., Magliano, D. J., Shaw, J. E. & Gregg, E. W. Global trends in diabetes complications: a review of current evidence. Diabetologia 62, 3–16 (2019).
Hill, N. R. et al. Global prevalence of chronic kidney disease - a systematic review and meta-analysis. PLoS ONE 11, e0158765 (2016).
Alegre-Diaz, J. et al. Diabetes and cause-specific mortality in Mexico City. N. Engl. J. Med. 375, 1961–1971 (2016).
Crews, D. C., Bello, A. K. & Saadi, G. World Kidney Day Steering Committee. Burden, access, and disparities in kidney disease. Kidney Int. 95, 242–248 (2019).
Keith, D. S., Nichols, G. A., Gullion, C. M., Brown, J. B. & Smith, D. H. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch. Intern. Med. 164, 659–663 (2004).
Liyanage, T. et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet 385, 1975–1982 (2015).
Buse, J. B. et al. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 43, 487–493 (2020).
Tuttle, K. R. et al. Dulaglutide versus insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease (AWARD-7): a multicentre, open-label, randomised trial. Lancet Diabetes Endocrinol. 6, 605–617 (2018). The participants of this trial with moderate-to-severe diabetic kidney disease who were treated with 52 weeks of dulaglutide experienced a slower decline in kidney function compared with those treated with insulin.
Gerstein, H. C. et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet 394, 121–130 (2019).
Marso, S. P. et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 375, 311–322 (2016).
Mann, J. F. E. et al. Liraglutide and renal outcomes in type 2 diabetes. N. Engl. J. Med. 377, 839–848 (2017). In this CVOT, liraglutide treatment was associated with lower rates of new-onset macroalbuminuria compared with placebo.
Pfeffer, M. A. et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N. Engl. J. Med. 373, 2247–2257 (2015).
Muskiet, M. H. A. et al. Lixisenatide and renal outcomes in patients with type 2 diabetes and acute coronary syndrome: an exploratory analysis of the ELIXA randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 6, 859–869 (2018).
Marso, S. P. et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 375, 1834–1844 (2016). This CVOT demonstrated significantly lower rates of primary composite cardiovascular outcome and secondary kidney outcomes (new-onset or worsening nephropathy) after 2 years of treatment with oral semaglutide compared with placebo.
Holman, R. R. et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 377, 1228–1239 (2017).
Bethel, M. A. et al. Microvascular and cardiovascular outcomes according to renal function in patients treated with once-weekly exenatide: insights from the EXSCEL trial. Diabetes Care 43, 446–452 (2020).
Rosenstock, J. et al. Effect of linagliptin vs placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: the CARMELINA Randomized Clinical Trial. JAMA 321, 69–79 (2019).
Scirica, B. M. et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N. Engl. J. Med. 369, 1317–1326 (2013).
Graaf, C. et al. Glucagon-like peptide-1 and its class B G protein-coupled receptors: a long march to therapeutic successes. Pharmacol. Rev. 68, 954–1013 (2016).
Holt, M. K. et al. Preproglucagon neurons in the nucleus of the solitary tract are the main source of brain GLP-1, mediate stress-induced hypophagia, and limit unusually large intakes of food. Diabetes 68, 21–33 (2019).
Holst, J. J., Albrechtsen, N. J. W., Rosenkilde, M. M. & Deacon, C. F. Physiology of the Incretin hormones, GIP and GLP-1-regulation of release and posttranslational modifications. Compr. Physiol. 9, 1339–1381 (2019).
Zhou, B., Ji, K., Peng, A., Yang, X. & Huang, K. GLP-1(28-36) amide, a long ignored peptide revisited. Open Biochem. J. 8, 107–111 (2014).
Vahl, T. P., Paty, B. W., Fuller, B. D., Prigeon, R. L. & D’Alessio, D. A. Effects of GLP-1-(7-36)NH2, GLP-1-(7-37), and GLP-1- (9-36)NH2 on intravenous glucose tolerance and glucose-induced insulin secretion in healthy humans. J. Clin. Endocrinol. Metab. 88, 1772–1779 (2003).
Lim, G. E. & Brubaker, P. L. Glucagon-like peptide 1 secretion by the L-cell. Diabetes 55 (Suppl. 2), 70–77 (2006).
Balks, H. J., Holst, J. J., von zur Muhlen, A. & Brabant, G. Rapid oscillations in plasma glucagon-like peptide-1 (GLP-1) in humans: cholinergic control of GLP-1 secretion via muscarinic receptors. J. Clin. Endocrinol. Metab. 82, 786–790 (1997).
Ellingsgaard, H. et al. GLP-1 secretion is regulated by IL-6 signalling: a randomised, placebo-controlled study. Diabetologia 63, 362–373 (2020).
Kahles, F. et al. GLP-1 secretion is increased by inflammatory stimuli in an IL-6-dependent manner, leading to hyperinsulinemia and blood glucose lowering. Diabetes 63, 3221–3229 (2014).
Drucker, D. J. The cardiovascular biology of glucagon-like peptide-1. Cell Metab. 24, 15–30 (2016).
Drucker, D. J. Mechanisms of Action and therapeutic application of glucagon-like peptide-1. Cell Metab. 27, 740–756 (2018). This article provides historical context about the characterization of GLP1 and extensively reviews its physiological role.
Kuhre, R. E. et al. Fructose stimulates GLP-1 but not GIP secretion in mice, rats, and humans. Am. J. Physiol. Gastrointest. Liver Physiol. 306, G622–G630 (2014).
Reimann, F. et al. Glucose sensing in L cells: a primary cell study. Cell Metab. 8, 532–539 (2008).
Adam, T. C. & Westerterp-Plantenga, M. S. Nutrient-stimulated GLP-1 release in normal-weight men and women. Horm. Metab. Res. 37, 111–117 (2005).
Hirasawa, A. et al. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat. Med. 11, 90–94 (2005).
Reimann, F., Williams, L., da Silva Xavier, G., Rutter, G. A. & Gribble, F. M. Glutamine potently stimulates glucagon-like peptide-1 secretion from GLUTag cells. Diabetologia 47, 1592–1601 (2004).
Kuhre, R. E. et al. Peptide production and secretion in GLUTag, NCI-H716, and STC-1 cells: a comparison to native L-cells. J. Mol. Endocrinol. 56, 201–211 (2016).
Shah, M. et al. Effect of meal composition on postprandial glucagon-like peptide-1, insulin, glucagon, C-peptide, and glucose responses in overweight/obese subjects. Eur. J. Nutr. 56, 1053–1062 (2017).
Kendall, C. W. et al. Acute effects of pistachio consumption on glucose and insulin, satiety hormones and endothelial function in the metabolic syndrome. Eur. J. Clin. Nutr. 68, 370–375 (2014).
Kehlet, U. et al. Addition of rye bran and pea fiber to pork meatballs enhances subjective satiety in healthy men, but does not change glycemic or hormonal responses: a randomized crossover meal test study. J. Nutr. 147, 1700–1708 (2017).
Yaribeygi, H., Maleki, M., Sathyapalan, T., Jamialahmadi, T. & Sahebkar, A. Anti-inflammatory potentials of incretin-based therapies used in the management of diabetes. Life Sci. 241, 117152 (2019).
Uribarri, J. & Tuttle, K. R. Advanced glycation end products and nephrotoxicity of high-protein diets. Clin. J. Am. Soc. Nephrol. 1, 1293–1299 (2006).
Adam, T. C. & Westerterp-Plantenga, M. S. Glucagon-like peptide-1 release and satiety after a nutrient challenge in normal-weight and obese subjects. Br. J. Nutr. 93, 845–851 (2005).
Kuhne S. G., Stengel A. Alteration of peptidergic gut-brain signaling under conditions of obesity. J. Physiol. Pharmacol. https://doi.org/10.26402/jpp.2019.5.01 (2019).
Anandhakrishnan, A. & Korbonits, M. Glucagon-like peptide 1 in the pathophysiology and pharmacotherapy of clinical obesity. World J. Diabetes 7, 572–598 (2016).
Neumiller, J. J. Incretin pharmacology: a review of the incretin effect and current incretin-based therapies. Cardiovasc. Hematol. Agents Med. Chem. 10, 276–288 (2012).
Bortolato, A. et al. Structure of class B GPCRs: new horizons for drug discovery. Br. J. Pharmacol. 171, 3132–3145 (2014).
Zhu, L. et al. Glucagon-like peptide-1 receptor expression and its functions are regulated by androgen. Biomed. Pharmacother. 120, 109555 (2019).
Wang, H., Brun, T., Kataoka, K., Sharma, A. J. & Wollheim, C. B. MAFA controls genes implicated in insulin biosynthesis and secretion. Diabetologia 50, 348–358 (2007).
Hall, E. et al. DNA methylation of the glucagon-like peptide 1 receptor (GLP1R) in human pancreatic islets. BMC Med. Genet. 14, 76 (2013).
Wildhage, I., Trusheim, H., Goke, B. & Lankat-Buttgereit, B. Gene expression of the human glucagon-like peptide-1 receptor is regulated by Sp1 and Sp3. Endocrinology 140, 624–631 (1999).
Pyke, C. & Knudsen, L. B. The glucagon-like peptide-1 receptor – or not? Endocrinology 154, 4–8 (2013).
Michel, M. C., Wieland, T. & Tsujimoto, G. How reliable are G-protein-coupled receptor antibodies? Naunyn Schmiedebergs Arch. Pharmacol. 379, 385–388 (2009).
Webb, D. R., Handel, T. M., Kretz-Rommel, A. & Stevens, R. C. Opportunities for functional selectivity in GPCR antibodies. Biochem. Pharmacol. 85, 147–152 (2013).
Pyke, C. et al. GLP-1 receptor localization in monkey and human tissue: novel distribution revealed with extensively validated monoclonal antibody. Endocrinology 155, 1280–1290 (2014).
Fan, Y. et al. Comparison of kidney transcriptomic profiles of early and advanced diabetic nephropathy reveals potential new mechanisms for disease progression. Diabetes 68, 2301–2314 (2019).
Baggio, L. L. et al. GLP-1 receptor expression within the human heart. Endocrinology 159, 1570–1584 (2018).
Deacon, C. F. What do we know about the secretion and degradation of incretin hormones? Regul. Pept. 128, 117–124 (2005).
Moellmann, J. et al. Glucagon-like peptide 1 and its cleavage products are renoprotective in murine diabetic nephropathy. Diabetes. 67, 2410–2419 (2018).
Burgmaier, M. et al. Glucagon-like peptide-1 (GLP-1) and its split products GLP-1(9-37) and GLP-1(28-37) stabilize atherosclerotic lesions in apoe(-)/(-) mice. Atherosclerosis 231, 427–435 (2013).
Drucker, D. J. The biology of incretin hormones. Cell Metab. 3, 153–165 (2006).
Deacon, C. F. Physiology and pharmacology of DPP-4 in glucose homeostasis and the treatment of type 2 diabetes. Front. Endocrinol. 10, 80 (2019).
Klemann, C., Wagner, L., Stephan, M. & von Horsten, S. Cut to the chase: a review of CD26/dipeptidyl peptidase-4’s (DPP4) entanglement in the immune system. Clin. Exp. Immunol. 185, 1–21 (2016).
Hasan, A. A. & Hocher, B. Role of soluble and membrane-bound dipeptidyl peptidase-4 in diabetic nephropathy. J. Mol. Endocrinol. 59, R1–R10 (2017).
Lambeir, A. M., Durinx, C., Scharpe, S. & De Meester, I. Dipeptidyl-peptidase IV from bench to bedside: an update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Crit. Rev. Clin. Lab. Sci. 40, 209–294 (2003).
Nauck, M. A. Incretin-based therapies for type 2 diabetes mellitus: properties, functions, and clinical implications. Am. J. Med. 124, S3–S18 (2011).
Ohnuma, K., Dang, N. H. & Morimoto, C. Revisiting an old acquaintance: CD26 and its molecular mechanisms in T cell function. Trends Immunol. 29, 295–301 (2008).
Shingu, K. et al. CD26 expression determines lung metastasis in mutant F344 rats: involvement of NK cell function and soluble CD26. Cancer Immunol. Immunother. 52, 546–554 (2003).
Frerker, N. et al. Phenotyping of congenic dipeptidyl peptidase 4 (DP4) deficient Dark Agouti (DA) rats suggests involvement of DP4 in neuro-, endocrine, and immune functions. Clin. Chem. Lab. Med. 47, 275–287 (2009).
Aroor, A. et al. DPP-4 Inhibitors as therapeutic modulators of immune cell function and associated cardiovascular and renal insulin resistance in obesity and diabetes. Cardiorenal Med. 3, 48–56 (2013).
Matteucci, E. & Giampietro, O. Dipeptidyl peptidase-4 (CD26): knowing the function before inhibiting the enzyme. Curr. Med. Chem. 16, 2943–2951 (2009).
Trujillo, J. M. & Nuffer, W. GLP-1 receptor agonists for type 2 diabetes mellitus: recent developments and emerging agents. Pharmacotherapy 34, 1174–1186 (2014).
Drucker, D. J. & Nauck, M. A. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 368, 1696–1705 (2006).
Drucker, D. J. et al. Exenatide once weekly versus twice daily for the treatment of type 2 diabetes: a randomised, open-label, non-inferiority study. Lancet 372, 1240–1250 (2008).
Buse, J. B. et al. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet 374, 39–47 (2009).
Meier, J. J. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat. Rev. Endocrinol. 8, 728–742 (2012).
Edwards, C. M. et al. Exendin-4 reduces fasting and postprandial glucose and decreases energy intake in healthy volunteers. Am. J. Physiol. Endocrinol. Metab. 281, E155–E161 (2001).
Nauck, M. A., Kemmeries, G., Holst, J. J. & Meier, J. J. Rapid tachyphylaxis of the glucagon-like peptide 1-induced deceleration of gastric emptying in humans. Diabetes 60, 1561–1565 (2011).
Verdich, C. et al. A meta-analysis of the effect of glucagon-like peptide-1 (7-36) amide on ad libitum energy intake in humans. J. Clin. Endocrinol. Metab. 86, 4382–4389 (2001).
Raun, K., von Voss, P. & Knudsen, L. B. Liraglutide, a once-daily human glucagon-like peptide-1 analog, minimizes food intake in severely obese minipigs. Obesity 15, 1710–1716 (2007).
Meier, J. J. et al. Secretion, degradation, and elimination of glucagon-like peptide 1 and gastric inhibitory polypeptide in patients with chronic renal insufficiency and healthy control subjects. Diabetes 53, 654–662 (2004).
Ahmann, A. J. et al. Efficacy and safety of once-weekly semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN 3): A 56-week, open-label, randomized clinical trial. Diabetes Care 41, 258–266 (2018).
Fineman, M. S. et al. Clinical relevance of anti-exenatide antibodies: safety, efficacy and cross-reactivity with long-term treatment. Diabetes Obes. Metab. 14, 546–554 (2012).
Ahren, B. Clinical results of treating type 2 diabetic patients with sitagliptin, vildagliptin or saxagliptin–diabetes control and potential adverse events. Best Pract. Res. Clin. Endocrinol. Metab. 23, 487–498 (2009).
Deacon, C. F. Therapeutic strategies based on glucagon-like peptide 1. Diabetes 53, 2181–2189 (2004).
DeFronzo, R. A. et al. Effects of exenatide versus sitagliptin on postprandial glucose, insulin and glucagon secretion, gastric emptying, and caloric intake: a randomized, cross-over study. Curr. Med. Res. Opin. 24, 2943–2952 (2008).
Chen, X. W. et al. Clinical pharmacology of dipeptidyl peptidase 4 inhibitors indicated for the treatment of type 2 diabetes mellitus. Clin. Exp. Pharmacol. Physiol. 42, 999–1024 (2015).
Scheen, A. J. Pharmacokinetics of dipeptidylpeptidase-4 inhibitors. Diabetes Obes. Metab. 12, 648–658 (2010).
Food and Drug Administration. Guidance for industry: diabetes mellitus - evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. Federal Register https://www.federalregister.gov/documents/2008/12/19/E8-30086/guidance-for-industry-on-diabetes-mellitus-evaluating-cardiovascular-risk-in-new-antidiabetic (2008).
Tuttle K. R. et al. CKD Outcomes in Type 2 Diabetes and Moderate-to-Severe CKD Treated with Dulaglutide Versus Insulin Glargine: AWARD-7 [abstract TH-OR033]. ASN Kidney Week 2018 https://www.asn-online.org/education/kidneyweek/2018/program-abstract.aspx?controlId=3008561 (2018).
Tuttle K. R0., et al. Clinical events in type 2 diabetes and moderate-to-severe CKD by albuminuria status: dulaglutide vs. insulin glargine [Abstract SA-OR081]. ASN Kidney Week 2019 https://www.asn-online.org/education/kidneyweek/2019/program-abstract.aspx?controlId=3224819 (2019).
Zavattaro, M. et al. One-year treatment with liraglutide improved renal function in patients with type 2 diabetes: a pilot prospective study. Endocrine 50, 620–626 (2015).
Davies, M. J. et al. Efficacy and safety of liraglutide versus placebo as add-on to glucose-lowering therapy in patients with type 2 diabetes and moderate renal impairment (LIRA-RENAL): a randomized clinical trial. Diabetes Care 39, 222–230 (2016).
Husain, M. et al. Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 381, 841–851 (2019).
Mann, J. F. E. et al. Effects of once-weekly subcutaneous semaglutide on kidney function and safety in patients with type 2 diabetes: a post hoc analysis of the SUSTAIN 1-7 randomized controlled trials. Lancet Diabetes Endocrinol. 8, 880–893 (2020).
Muskiet, M. H. A. et al. Exenatide twice-daily does not affect renal function or albuminuria compared to titrated insulin glargine in patients with type 2 diabetes mellitus: A post-hoc analysis of a 52-week randomised trial. Diabetes Res. Clin. Pract. 153, 14–22 (2019).
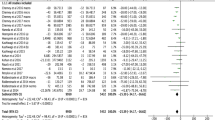
Kristensen, S. L. et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 7, 776–785 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03819153?term=semaglutide+FLOW&draw=2&rank=1 (2019).
White, W. B. et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N. Engl. J. Med. 369, 1327–1335 (2013).
Garlo, K. G. et al. Kidney biomarkers and decline in eGFR in patients with type 2 Diabetes. Clin. J. Am. Soc. Nephrol. 13, 398–405 (2018).
Groop, P. H. et al. Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: the randomized MARLINA-T2D trial. Diabetes Obes. Metab. 19, 1610–1619 (2017).
Mosenzon, O. et al. Effect of saxagliptin on renal outcomes in the SAVOR-TIMI 53 Trial. Diabetes Care 40, 69–76 (2017).
Green, J. B. et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 373, 232–242 (2015).
Cornel, J. H. et al. Effect of sitagliptin on kidney function and respective cardiovascular outcomes in type 2 diabetes: outcomes from TECOS. Diabetes Care 39, 2304–2310 (2016).
Alicic, R. Z., Rooney, M. T. & Tuttle, K. R. Diabetic kidney disease: challenges, progress, and possibilities. Clin. J. Am. Soc. Nephrol. 12, 2032–2045 (2017).
Alicic, R. Z., Johnson, E. J. & Tuttle, K. R. Inflammatory mechanisms as new biomarkers and therapeutic targets for diabetic kidney disease. Adv. Chronic Kidney Dis. 25, 181–191 (2018).
Anderberg, R. J. et al. Serum amyloid A and inflammation in diabetic kidney disease and podocytes. Lab. Invest. 95, 250–262 (2015).
Alicic, R. Z., Neumiller, J. J., Johnson, E. J., Dieter, B. & Tuttle, K. R. Sodium-glucose cotransporter 2 inhibition and diabetic kidney disease. Diabetes 68, 248–257 (2019).
Pichler, R., Afkarian, M., Dieter, B. P. & Tuttle, K. R. Immunity and inflammation in diabetic kidney disease: translating mechanisms to biomarkers and treatment targets. Am. J. Physiol. Ren. Physiol. 312, F716–F731 (2017).
Tang, S. C. W. & Yiu, W. H. Innate immunity in diabetic kidney disease. Nat. Rev. Nephrol. 16, 206–222 (2020). Extensive review of the role of dysregulated immunity and inflammation in diabetes.
Tuttle, K. R. et al. Effect of strict glycemic control on renal hemodynamic response to amino acids and renal enlargement in insulin-dependent diabetes mellitus. N. Engl. J. Med. 324, 1626–1632 (1991).
Tuttle, K. R. & Bruton, J. L. Effect of insulin therapy on renal hemodynamic response to amino acids and renal hypertrophy in non-insulin-dependent diabetes. Kidney Int. 42, 167–173 (1992).
Tuttle, K. R., Puhlman, M. E., Cooney, S. K. & Short, R. A. Effects of amino acids and glucagon on renal hemodynamics in type 1 diabetes. Am. J. Physiol. Ren. Physiol. 282, F103–F112 (2002).
Jha, J. C. et al. NADPH oxidase Nox5 accelerates renal injury in diabetic nephropathy. Diabetes 66, 2691–2703 (2017).
Hendarto, H. et al. GLP-1 analog liraglutide protects against oxidative stress and albuminuria in streptozotocin-induced diabetic rats via protein kinase A-mediated inhibition of renal NAD(P)H oxidases. Metabolism 61, 1422–1434 (2012).
Sancar-Bas, S., Gezginci-Oktayoglu, S. & Bolkent, S. Exendin-4 attenuates renal tubular injury by decreasing oxidative stress and inflammation in streptozotocin-induced diabetic mice. Growth Factors 33, 419–429 (2015).
Kodera, R. et al. Glucagon-like peptide-1 receptor agonist ameliorates renal injury through its anti-inflammatory action without lowering blood glucose level in a rat model of type 1 diabetes. Diabetologia 54, 965–978 (2011). Very early report of direct, glucose-independent anti-inflammatory effects of GLP1 agonists in the kidney.
Katagiri, D. et al. Protection of glucagon-like peptide-1 in cisplatin-induced renal injury elucidates gut-kidney connection. J. Am. Soc. Nephrol. 24, 2034–2043 (2013).
Yang, H. et al. Exendin-4 ameliorates renal ischemia-reperfusion injury in the rat. J. Surg. Res. 185, 825–832 (2013).
Turner, J. E., Becker, M., Mittrucker, H. W. & Panzer, U. Tissue-resident lymphocytes in the kidney. J. Am. Soc. Nephrol. 29, 389–399 (2018).
Ferdinand, K. C. et al. Effects of the once-weekly glucagon-like peptide-1 receptor agonist dulaglutide on ambulatory blood pressure and heart rate in patients with type 2 diabetes mellitus. Hypertension 64, 731–737 (2014).
Bunck, M. C. et al. Exenatide affects circulating cardiovascular risk biomarkers independently of changes in body composition. Diabetes Care 33, 1734–1737 (2010).
Tremblay, A. J., Lamarche, B., Deacon, C. F., Weisnagel, S. J. & Couture, P. Effects of sitagliptin therapy on markers of low-grade inflammation and cell adhesion molecules in patients with type 2 diabetes. Metabolism 63, 1141–1148 (2014).
Mazidi, M., Karimi, E., Rezaie, P. & Ferns, G. A. Treatment with GLP1 receptor agonists reduce serum CRP concentrations in patients with type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. J. Diabetes Complications 31, 1237–1242 (2017).
Hadjiyanni, I., Siminovitch, K. A., Danska, J. S. & Drucker, D. J. Glucagon-like peptide-1 receptor signalling selectively regulates murine lymphocyte proliferation and maintenance of peripheral regulatory T cells. Diabetologia 53, 730–740 (2010). This study provided the first experimental evidence for the anti-inflammatory and immunomodulatory properties of GLP1.
Lebherz, C. et al. Interleukin-6 predicts inflammation-induced increase of Glucagon-like peptide-1 in humans in response to cardiac surgery with association to parameters of glucose metabolism. Cardiovasc. Diabetol. 15, 21 (2016).
Ceriello, A. et al. Simultaneous GLP-1 and insulin administration acutely enhances their vasodilatory, antiinflammatory, and antioxidant action in type 2 diabetes. Diabetes Care 37, 1938–1943 (2014).
Arakawa, M. et al. Inhibition of monocyte adhesion to endothelial cells and attenuation of atherosclerotic lesion by a glucagon-like peptide-1 receptor agonist, exendin-4. Diabetes 59, 1030–1037 (2010).
He, L. et al. Anti-inflammatory effects of exendin-4, a glucagon-like peptide-1 analog, on human peripheral lymphocytes in patients with type 2 diabetes. J. Diabetes Investig. 4, 382–392 (2013).
Hogan, A. E. et al. Glucagon-like peptide 1 analogue therapy directly modulates innate immune-mediated inflammation in individuals with type 2 diabetes mellitus. Diabetologia 57, 781–784 (2014).
Shiraishi, D., Fujiwara, Y., Komohara, Y., Mizuta, H. & Takeya, M. Glucagon-like peptide-1 (GLP-1) induces M2 polarization of human macrophages via STAT3 activation. Biochem. Biophys. Res. Commun. 425, 304–308 (2012).
Chaudhuri, A. et al. Exenatide exerts a potent antiinflammatory effect. J. Clin. Endocrinol. Metab. 97, 198–207 (2012).
Akarte, A. S., Srinivasan, B. P., Gandhi, S. & Sole, S. Chronic DPP-IV inhibition with PKF-275-055 attenuates inflammation and improves gene expressions responsible for insulin secretion in streptozotocin induced diabetic rats. Eur. J. Pharm. Sci. 47, 456–463 (2012).
Tian, L. et al. Reversal of new-onset diabetes through modulating inflammation and stimulating beta-cell replication in nonobese diabetic mice by a dipeptidyl peptidase IV inhibitor. Endocrinology 151, 3049–3060 (2010).
Moschovaki Filippidou, F. et al. Glucagon-like peptide-1 receptor agonism improves nephrotoxic serum nephritis by inhibiting T-cell proliferation. Am. J. Pathol. 190, 400–411 (2020).
Kim, S. J. et al. DPP-4 inhibition enhanced renal tubular and myocardial GLP-1 receptor expression decreased in CKD with myocardial infarction. BMC Nephrol. 20, 75 (2019).
Higashijima, Y., Tanaka, T., Yamaguchi, J., Tanaka, S. & Nangaku, M. Anti-inflammatory role of DPP-4 inhibitors in a nondiabetic model of glomerular injury. Am. J. Physiol. Ren. Physiol. 308, F878–F887 (2015).
Hasan, A. A. et al. Mechanisms of GLP-1 receptor-independent renoprotective effects of the dipeptidyl peptidase type 4 inhibitor linagliptin in GLP-1 receptor knockout mice with 5/6 nephrectomy. Kidney Int. 95, 1373–1388 (2019).
Ronn, J., Jensen, E. P., Wewer Albrechtsen, N. J., Holst, J. J. & Sorensen, C. M. Glucagon-like peptide-1 acutely affects renal blood flow and urinary flow rate in spontaneously hypertensive rats despite significantly reduced renal expression of GLP-1 receptors. Physiol Rep. 5, e13503 (2017).
Thomson, S. C., Kashkouli, A., Liu, Z. Z. & Singh, P. Renal hemodynamic effects of glucagon-like peptide-1 agonist are mediated by nitric oxide but not prostaglandin. Am. J. Physiol. Ren. Physiol. 313, F854–F858 (2017).
Tang-Christensen, M. et al. Central administration of GLP-1-(7-36) amide inhibits food and water intake in rats. Am. J. Physiol. 271, R848–R856 (1996).
Tonneijck, L. et al. Postprandial renal haemodynamic effect of lixisenatide vs once-daily insulin-glulisine in patients with type 2 diabetes on insulin-glargine: An 8-week, randomised, open-label trial. Diabetes Obes. Metab. 19, 1669–1680 (2017).
Skov, J. et al. Glucagon-like peptide-1 (GLP-1): effect on kidney hemodynamics and renin-angiotensin-aldosterone system in healthy men. J. Clin. Endocrinol. Metab. 98, E664–E671 (2013).
Gutzwiller, J. P. et al. Glucagon-like peptide 1 induces natriuresis in healthy subjects and in insulin-resistant obese men. J. Clin. Endocrinol. Metab. 89, 3055–3061 (2004).
Carraro-Lacroix, L. R., Malnic, G. & Girardi, A. C. Regulation of Na+/H+ exchanger NHE3 by glucagon-like peptide 1 receptor agonist exendin-4 in renal proximal tubule cells. Am. J. Physiol. Ren. Physiol. 297, F1647–F1655 (2009).
Tonneijck, L. et al. Renal tubular effects of prolonged therapy with the GLP-1 receptor agonist lixisenatide in patients with type 2 diabetes mellitus. Am. J. Physiol. Ren. Physiol. 316, F231–F240 (2019).
Crajoinas, R. O. et al. Mechanisms mediating the diuretic and natriuretic actions of the incretin hormone glucagon-like peptide-1. Am. J. Physiol. Ren. Physiol. 301, F355–F363 (2011).
Rieg, T. et al. Natriuretic effect by exendin-4, but not the DPP-4 inhibitor alogliptin, is mediated via the GLP-1 receptor and preserved in obese type 2 diabetic mice. Am. J. Physiol. Ren. Physiol. 303, F963–F971 (2012).
Girardi, A. C., Fukuda, L. E., Rossoni, L. V., Malnic, G. & Reboucas, N. A. Dipeptidyl peptidase IV inhibition downregulates Na+- H+ exchanger NHE3 in rat renal proximal tubule. Am. J. Physiol. Ren. Physiol. 294, F414–F422 (2008).
van Baar, M. J. B. et al. The incretin pathway as a therapeutic target in diabetic kidney disease: a clinical focus on GLP-1 receptor agonists. Ther. Adv. Endocrinol. Metab. 10, 2042018819865398 (2019).
Farah, L. X. et al. The physiological role of glucagon-like peptide-1 in the regulation of renal function. Am. J. Physiol. Ren. Physiol. 310, F123–F127 (2016).
Muskiet, M. H. A. et al. GLP-1 and the kidney: from physiology to pharmacology and outcomes in diabetes. Nat. Rev. Nephrol. 13, 605–628 (2017). Comprehensive review of the role of GLP1 in the kidney and of its treatment potential.
Tonneijck, L. et al. Acute renal effects of the GLP-1 receptor agonist exenatide in overweight type 2 diabetes patients: a randomised, double-blind, placebo-controlled trial. Diabetologia 59, 1412–1421 (2016).
Gilbert, M. P. & Pratley, R. E. GLP-1 analogs and DPP-4 inhibitors in type 2 diabetes therapy: review of head-to-head clinical trials. Front. Endocrinol. 11, 178 (2020).
Moon, H. S., Kim, M. K. & Son, M. H. The development of non-peptide glucagon-like peptide-1 receptor agonist for the treatment of type 2 diabetes. Arch. Pharm. Res. 34, 1041–1043 (2011).
Chepurny, O. G. et al. Synthetic small molecule GLP-1 secretagogues prepared by means of a three-component indole annulation strategy. Sci. Rep. 6, 28934 (2016).
Perkovic, V. et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N. Engl. J. Med. 380, 2295–2306 (2019).
Heerspink, H. J. L. et al. Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 383, 1436–1446 (2020).
Packer, M. et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N. Engl. J. Med. 383, 1413–1424 (2020).
Jensen, E. P. et al. Activation of GLP-1 receptors on vascular smooth muscle cells reduces the autoregulatory response in afferent arterioles and increases renal blood flow. Am. J. Physiol. Ren. Physiol. 308, F867–F877 (2015).
Korner, M., Stockli, M., Waser, B. & Reubi, J. C. GLP-1 receptor expression in human tumors and human normal tissues: potential for in vivo targeting. J. Nucl. Med. 48, 736–743 (2007).
Fujita, H. et al. The protective roles of GLP-1R signaling in diabetic nephropathy: possible mechanism and therapeutic potential. Kidney Int. 85, 579–589 (2014). This study reported on the antioxidative and anti-inflammatory effects of GLP1R agonists in the kidney and demonstrated improved kidney function and histology.
Sharkovska, Y. et al. Blood pressure and glucose independent renoprotective effects of dipeptidyl peptidase-4 inhibition in a mouse model of type-2 diabetic nephropathy. J. Hypertens. 32, 2211–2223 (2014).
Schlatter, P., Beglinger, C., Drewe, J. & Gutmann, H. Glucagon-like peptide 1 receptor expression in primary porcine proximal tubular cells. Regul. Pept. 141, 120–128 (2007).
Jackson, E. K., Kochanek, S. J. & Gillespie, D. G. Dipeptidyl peptidase IV regulates proliferation of preglomerular vascular smooth muscle and mesangial cells. Hypertension 60, 757–764 (2012).
Kettmann, U., Humbel, B. & Holzhausen, H. J. Ultrastructural localization of dipeptidylpeptidase IV in the glomerulum of the rat kidney. Acta Histochem. 92, 225–227 (1992).
Hartel, S., Gossrau, R., Hanski, C. & Reutter, W. Dipeptidyl peptidase (DPP) IV in rat organs. Comparison of immunohistochemistry and activity histochemistry. Histochemistry 89, 151–161 (1988).
Stange, T., Kettmann, U. & Holzhausen, H. J. Immunoelectron microscopic single and double labelling of aminopeptidase N (CD 13) and dipeptidyl peptidase IV (CD 26). Acta Histochem. 98, 323–331 (1996).
Yang, J. et al. Increase in DPP-IV in the intestine, liver and kidney of the rat treated with high fat diet and streptozotocin. Life Sci. 81, 272–279 (2007).
Takeda Pharmaceuticals America, Inc. Alogliptin (Nesina®) Tablets. Prescribing Information (Takeda Pharmaceuticals America, Inc., 2019).
Boehringer Ingelheim Pharmaceuticals, Inc. Linagliptin (Tradjenta®) Tablets. Prescribing Information (Boehringer Ingelheim Pharmaceuticals, Inc., 2019)
AstraZeneca Pharmaceuticals LP. Saxagliptin (Onglyza®) Tablets. Prescribing Information (AstraZeneca Pharmaceuticals LP, 2019).
Merck & Co., Inc. Sitagliptin (Januvia®) Tablets. Prescribing Information. (Merck & Co., Inc., 2019).
Novartis Pharma. Vildagliptin (Galvus). Summary of Product Characteristics. (Novartis Pharma, 2012).
AstraZeneca Pharmaceuticals LP. Exenatide (Byetta®) Injection. Prescribing Information (AstraZeneca Pharmaceuticals LP, 2018).
Sanofi-aventis U.S., LLC. Lixisenatide (Adlyxin®) Injection. Prescribing Information (Sanofi-aventis U.S., LLC, 2019).
Novo Nordisk, Inc. Liraglutide (Victoza®) Injection. Prescribing Information (Novo Nordisk, Inc., 2019).
Eli Lilly and Company. Dulaglutide (Trulicity®) Injection. Prescribing Information (Eli Lilly and Company, 2019).
Novo Nordisk, Inc. Semaglutide (Ozempic®) Injection. Prescribing Information (Novo Nordisk, Inc., 2019).
Novo Nordisk, Inc. Semaglutide (Rybelsus®) Tablets. Prescribing Information (Novo Nordisk, Inc., 2019).
AstraZeneca Pharmaceuticals LP. Exenatide Extended-Release (Bydureon®) Injectable Suspension. Prescribing Information (AstraZeneca Pharmaceuticals LP, 2019).
Park, C. W. et al. Long-term treatment of glucagon-like peptide-1 analog exendin-4 ameliorates diabetic nephropathy through improving metabolic anomalies in db/db mice. J. Am. Soc. Nephrol. 18, 1227–1238 (2007).
Ishibashi, Y., Nishino, Y., Matsui, T., Takeuchi, M. & Yamagishi, S. Glucagon-like peptide-1 suppresses advanced glycation end product-induced monocyte chemoattractant protein-1 expression in mesangial cells by reducing advanced glycation end product receptor level. Metabolism. 60, 1271–1277 (2011).
Gangadharan Komala, M., Gross, S., Zaky, A., Pollock, C. & Panchapakesan, U. Saxagliptin reduces renal tubulointerstitial inflammation, hypertrophy and fibrosis in diabetes. Nephrology 21, 423–431 (2016).
Liu, W. J. et al. Dipeptidyl peptidase IV inhibitor attenuates kidney injury in streptozotocin-induced diabetic rats. J. Pharmacol. Exp. Ther. 340, 248–255 (2012).
Marques, C. et al. Sitagliptin prevents inflammation and apoptotic cell death in the kidney of type 2 diabetic animals. Mediators Inflamm. 2014, 538737 (2014).
Nakashima, S., Matsui, T., Takeuchi, M. & Yamagishi, S. I. Linagliptin blocks renal damage in type 1 diabetic rats by suppressing advanced glycation end products-receptor axis. Horm. Metab. Res. 46, 717–721 (2014).
Kanasaki, K. et al. Linagliptin-mediated DPP-4 inhibition ameliorates kidney fibrosis in streptozotocin-induced diabetic mice by inhibiting endothelial-to-mesenchymal transition in a therapeutic regimen. Diabetes 63, 2120–2131 (2014).
Kodera, R. et al. Dipeptidyl peptidase-4 inhibitor ameliorates early renal injury through its anti-inflammatory action in a rat model of type 1 diabetes. Biochem. Biophys. Res. Commun. 443, 828–833 (2014). Early study demonstrating that a reduction of albuminuria and amelioration of histological changes in the kidneys of diabetic rats was mediated through anti-inflammatory rather than anti-hyperglycaemic effects.
Ceriello, A. et al. Glucagon-like peptide 1 reduces endothelial dysfunction, inflammation, and oxidative stress induced by both hyperglycemia and hypoglycemia in type 1 diabetes. Diabetes Care 36, 2346–2350 (2013).
Wu, J. D. et al. Effect of exenatide on inflammatory and oxidative stress markers in patients with type 2 diabetes mellitus. Diabetes Technol. Ther. 13, 143–148 (2011).
Buldak, L. et al. Exenatide (a GLP-1 agonist) expresses anti-inflammatory properties in cultured human monocytes/macrophages in a protein kinase A and B/Akt manner. Pharmacol. Rep. 68, 329–337 (2016).
Rahman, K. et al. Inflammatory Ly6Chi monocytes and their conversion to M2 macrophages drive atherosclerosis regression. J. Clin. Invest. 127, 2904–2915 (2017).
Bruen, R. et al. Liraglutide attenuates preestablished atherosclerosis in apolipoprotein E-deficient mice via regulation of immune cell phenotypes and proinflammatory mediators. J. Pharmacol. Exp. Ther. 370, 447–458 (2019).
Eissele, R. et al. Glucagon-like peptide-1 cells in the gastrointestinal tract and pancreas of rat, pig and man. Eur. J. Clin. Invest. 22, 283–291 (1992).
Holst, J. J. & Gromada, J. Role of incretin hormones in the regulation of insulin secretion in diabetic and nondiabetic humans. Am. J. Physiol. Endocrinol. Metab. 287, E199–E206 (2004).
Billing, L. J. et al. Co-storage and release of insulin-like peptide-5, glucagon-like peptide-1 and peptideYY from murine and human colonic enteroendocrine cells. Mol. Metab. 16, 65–75 (2018).
Worthington, J. J., Reimann, F. & Gribble, F. M. Enteroendocrine cells-sensory sentinels of the intestinal environment and orchestrators of mucosal immunity. Mucosal Immunol. 11, 3–20 (2018).
Gribble, F. M. The gut endocrine system as a coordinator of postprandial nutrient homoeostasis. Proc. Nutr. Soc. 71, 456–462 (2012).
Tolhurst, G. et al. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes 61, 364–371 (2012).
Anini, Y., Hansotia, T. & Brubaker, P. L. Muscarinic receptors control postprandial release of glucagon-like peptide-1: in vivo and in vitro studies in rats. Endocrinology 143, 2420–2426 (2002).
Zhang, Y. et al. GLP-1 receptor in pancreatic alpha-cells regulates glucagon secretion in a glucose-dependent bidirectional manner. Diabetes 68, 34–44 (2019).
Chen, Y. T. et al. Exendin-4 and sitagliptin protect kidney from ischemia-reperfusion injury through suppressing oxidative stress and inflammatory reaction. J. Transl Med. 11, 270 (2013).
Acknowledgements
K.R.T. is supported by four NIDDK/NIH grants, one NCATS/NIH grant, one NIMHD/NIH grant, and a CDC contract, all from the US government, as well as a research grant from Goldfinch Bio.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content, wrote the manuscript, and reviewed or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
K.R.T. has received consulting fees for diabetes and CKD from Eli Lilly and Company, Boehringer Ingelheim, AstraZeneca, Gilead, Goldfinch Bio, Novo Nordisk and Bayer. J.J.N. has received consulting fees from Novo Nordisk. R.Z.A. has received consulting fees from Boehringer Ingelheim. E.J.C. declares no competing interests.
Additional information
Peer review information
Nature Reviews Nephrology thanks P. Rossing and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Anorexigenic gut peptides
-
Appetite-reducing peptides.
- Tachyphylaxis
-
Rapid loss or downregulation of a response to a drug.
- Volume of distribution
-
The volume required to dilute a drug to its observed concentration in plasma.
Rights and permissions
About this article
Cite this article
Alicic, R.Z., Cox, E.J., Neumiller, J.J. et al. Incretin drugs in diabetic kidney disease: biological mechanisms and clinical evidence. Nat Rev Nephrol 17, 227–244 (2021). https://doi.org/10.1038/s41581-020-00367-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-020-00367-2
This article is cited by
-
(Pro)renin receptor mediates tubular epithelial cell pyroptosis in diabetic kidney disease via DPP4-JNK pathway
Journal of Translational Medicine (2024)
-
Combination therapy for kidney disease in people with diabetes mellitus
Nature Reviews Nephrology (2024)
-
Renal effects of GLP-1 receptor agonists and tirzepatide in individuals with type 2 diabetes: seeds of a promising future
Endocrine (2024)
-
The cardio-renal-metabolic connection: a review of the evidence
Cardiovascular Diabetology (2023)
-
Exenatide regulates Th17/Treg balance via PI3K/Akt/FoxO1 pathway in db/db mice
Molecular Medicine (2022)