Abstract
The human major histocompatibility complex is a family of genes that encodes HLAs, which have a crucial role in defence against foreign pathogens and immune surveillance of tumours. In the context of transplantation, HLA molecules are polymorphic antigens that comprise an immunodominant alloreactive trigger for the immune response, resulting in rejection. Remarkable advances in knowledge and technology in the field of immunogenetics have considerably enhanced the safety of transplantation. However, access to transplantation among individuals who have become sensitized as a result of previous exposure to alloantigens is reduced proportional to the breadth of their sensitization. New approaches for crossing the HLA barrier in transplantation using plasmapheresis, intravenous immunoglobulin and kidney paired donation have been made possible by the relative ease with which even low levels of anti-HLA antibodies can now be detected and tracked. The development of novel protocols for the induction of tolerance and new approaches to immunomodulation was also facilitated by advances in HLA technology. Here, we review the progress made in understanding HLAs that has enabled organ transplantation to become a life-saving endeavour that is accessible even for sensitized patients. We also discuss novel approaches to desensitization, immunomodulation and tolerance induction that have the potential to further improve transplantation access and outcomes.
Key points
-
HLA molecules are highly polymorphic antigens; antibodies against these antigens can develop as a result of pregnancy, transplantation or blood transfusion.
-
HLA sensitization adversely affects both access to and the outcomes of transplantation.
-
Remarkable advances in HLA typing, HLA antibody screening and crossmatch testing have immensely improved the safety of transplantation.
-
Innovative therapeutic strategies such as desensitization protocols and kidney paired donation have made transplantation possible for patients who are broadly sensitized to HLAs.
-
Novel agents including proteasome inhibitors, complement inhibitors, IL-6 or IL-6 receptor blockers and immunoglobulin-G-degrading enzyme of Streptococcus pyogenes are being tested as add-on therapies to improve the efficacy of desensitization.
-
Achieving long-term immunologic tolerance remains the holy grail of transplantation; the induction of mixed chimaerism through infusion of donor haematopoietic stem cells is an important step in this direction.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
The MHC sequencing consortium. Complete sequence and gene map of a human major histocompatibility complex. Nature 401, 921–923 (1999).
Womer, K. & Rabb, H. in Comprehensive Clinical Nephrology (eds Johnson, R. et al.) 1132–1143 (Elsevier, 2014).
Shiina, T., Inoko, H. & Kulski, J. K. An update of the HLA genomic region, locus information and disease associations: 2004. Tissue Antigens. 64, 631–649 (2004).
Zachary, A. A., Hart, J. M., Lucas, D. P. & Leffell, M. S. The co$t of mi$matching. Clin. Transplants. 27, 261–269 (2007).
Zachary, A. A. & Leffell, M. S. HLA mismatching strategies for solid organ transplantation — a balancing act. Front. Immunol. 7, 575 (2016).
Gorer, P. A. The detection of antigenic differences in mouse erythrocytes by the employment of immune sera. Br. J. Exp. Pathol. 17, 42–50 (1936).
Snell, G. The genetic and antigenic basis of tumor transplantation. J. Pathol. Bacteriol. 44, 691–699 (1937).
Dausset, J. Immuno-hematologie des leucocytes. Bibl Paediatr. 14, 29–56 (1958).
Kissmeyer-Nielsen, F., Olsen, S., Petersen, V. P. & Fjeldborg, O. Hyperacute rejection of kidney allografts, associated with pre-existing humoral antibodies against donor cells. Lancet 2, 662–665 (1966).
Patel, R. & Terasaki, P. I. Significance of the positive crossmatch test in kidney transplantation. N. Engl. J. Med. 280, 735–739 (1969).
Williams, G. M. et al. “Hyperacute” renal-homograft rejection in man. N. Engl. J. Med. 279, 611–618 (1968).
Yunis, E. J., Amos, D. B., Eguro, S. Y. & Dorf, M. E. Cross reactions of HL-A antibodies. I. Characterization by absorption and elution. Transplantation 14, 474–479 (1972).
Garovoy, M. R. et al. Flow cytometry analysis: a high technology crossmatch technique facilitation transplantation. Transplant. Proc. 15, 1939–1943 (1983).
Cook, D. J. et al. The flow cytometry crossmatch in kidney transplantation. Clin. Transpl. 409–414 (1987).
Cardella, C. J., Falk, J. A., Nicholson, M. J., Harding, M. & Cook, G. T. Successful renal transplantation in patients with T cell reactivity to donor. Lancet. 2, 1240–1243 (1982).
Goeken, N. E. Outcome of renal transplantation following a positive cross-match with historical sera: the ASHI survey. Hum. Immunol. 14, 77–85 (1985).
Lopes, D. et al. Effect of different sensitization events on HLA alloimmunization in kidney transplantation candidates. Transplant. Proc. 47, 894–897 (2015).
Kao, K. J., Scornik, J. C. & Small, S. J. Enzyme-linked immunoassay for anti-HLA antibodies—an alternative to panel studies by lymphocytotoxicity. Transplantation 55, 192–196 (1993).
Olerup, O. & Zetterquist, H. HLA-DR typing by PCR amplification with sequence-specific primers (PCR-SSP) in 2 hours: an alternative to serological DR typing in clinical practice including donor-recipient matching in cadaveric transplantation. Tissue Antigens 39, 225–235 (1992).
Erlich, H. et al. HLA-DR, DQ and DP typing using PCR amplification and immobilized probes. Eur. J. Immunogenet. 18, 33–55 (1991).
Leffell, M. S., Montgomery, R. A. & Zachary, A. A. The changing role of antibody testing in transplantation. Clin. Transpl. 259–271 (2005).
Segev, D. L., Gentry, S. E., Warren, D. S., Reeb, B. & Montgomery, R. A. Kidney paired donation and optimizing the use of live donor organs. JAMA 293, 1883–1890 (2005).
Montgomery, R. A. et al. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation 70, 887–895 (2000).
Montgomery, R. A. et al. Domino paired kidney donation: a strategy to make best use of live non-directed donation. Lancet 368, 419–421 (2006).
Montgomery, R. A. Renal transplantation across HLA and ABO antibody barriers: integrating paired donation into desensitization protocols. Am. J. Transplant. 10, 449–457 (2010).
Ascher, N. L. et al. 100 HLA-identical sibling transplants. Prognostic factors other than histocompatibility. Ann. Surg. 189, 209–216 (1979).
Cheigh, J. S. et al. Renal transplantation between HLA identical siblings. Comparison with transplants from HLA semi-identical related donors. N. Engl. J. Med. 296, 1030–1034 (1977).
Williams, R. C., Opelz, G., McGarvey, C. J., Weil, E. J. & Chakkera, H. A. The risk of transplant failure with HLA mismatch in first adult kidney allografts from deceased donors. Transplantation 100, 1094–1102 (2016).
Opelz, G. Correlation of HLA matching with kidney graft survival in patients with or without cyclosporine treatment. Transplantation 40, 240–243 (1985).
Doxiadis, I. I. et al. Simpler and equitable allocation of kidneys from postmortem donors primarily based on full HLA-DR compatibility. Transplantation 83, 1207–1213 (2007).
Lim, W. H. et al. HLA-DQ mismatches and rejection in kidney transplant recipients. Clin. J. Am. Soc. Nephrol. 11, 875–883 (2016).
Mytilineos, J., Deufel, A. & Opelz, G. Clinical relevance of HLA-DPB locus matching for cadaver kidney retransplants: a report of the Collaborative Transplant Study. Transplantation 63, 1351–1354 (1997).
Youngs, D. HLA-DP alloantibodies. ASHI Quarterly 28, 60 (2004).
Qiu, J., Cai, J., Terasaki, P. I., El-Awar, N. & Lee, J. H. Detection of antibodies to HLA-DP in renal transplant recipients using single antigen beads. Transplantation 80, 1511–1513 (2005).
Kosmoliaptsis, V. et al. High-resolution three-dimensional modeling of human leukocyte antigen class I structure and surface electrostatic potential reveals the molecular basis for alloantibody binding epitopes. Hum. Immunol. 72, 1049–1059 (2011).
Tambur, A. R. et al. Epitope analysis of HLA-DQ antigens: what does the antibody see? Transplantation 98, 157–166 (2014).
Tambur, A. R. & Claas, F. H. HLA epitopes as viewed by antibodies: what is it all about? Am. J. Transplant. 15, 1148–1154 (2015).
Locke, J. E. et al. Proinflammatory events are associated with significant increases in breadth and strength of HLA-specific antibody. Am. J. Transplant. 9, 2136–2139 (2009).
Cecka, J. M., Kucheryavaya, A. Y., Reinsmoen, N. L. & Leffell, M. S. Calculated PRA: initial results show benefits for sensitized patients and a reduction in positive crossmatches. Am. J. Transplant. 11, 719–724 (2011).
Organ Procurement and Transplantation Network. National Data. U.S. Department of Health & Human Services https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/# (2018).
Gibney, E. M. et al. Detection of donor-specific antibodies using HLA-coated microspheres: another tool for kidney transplant risk stratification. Nephrol. Dial. Transplant. 21, 2625–2629 (2006).
Lucas, D. P., Leffell, M. S. & Zachary, A. A. Differences in immunogenicity of HLA antigens and the impact of cross-reactivity on the humoral response. Transplantation 99, 77–85 (2015).
EUROSTAM. The Allele Frequency Net Database. EUROSTAM http://www.allelefrequencies.net/default.asp (2018).
Heidt, S., Haasnoot, G. W., van Rood, J. J., Witvliet, M. D. & Claas, F. H. J. Kidney allocation based on proven acceptable antigens results in superior graft survival in highly sensitized patients. Kidney Int. 93, 491–500 (2018).
Wilk, A. R., Beck, J. & Kucheryavaya, A. Y. The kidney allocation system (KAS). The first two years. United Network for Organ Sharing https://www.transplantpro.org/wp-content/uploads/sites/3/KAS_First-two-years_041917.pdf (2017).
Baxter-Lowe, L. A., Cecka, M., Kamoun, M., Sinacore, J. & Melcher, M. L. Center-defined unacceptable HLA antigens facilitate transplants for sensitized patients in a multi-center kidney exchange program. Am. J. Transplant. 14, 1592–1598 (2014).
Bielmann, D. et al. Pretransplant risk assessment in renal allograft recipients using virtual crossmatching. Am. J. Transplant. 7, 626–632 (2007).
Tambur, A. R. et al. Perception versus reality?: virtual crossmatch — how to overcome some of the technical and logistic limitations. Am. J. Transplant. 9, 1886–1893 (2009).
Montgomery, R. A. & Zachary, A. A. Transplanting patients with a positive donor-specific crossmatch: a single center’s perspective. Pediatr. Transplant. 8, 535–542 (2004).
Bohmig, G. A. et al. Immunoadsorption in severe C4d-positive acute kidney allograft rejection: a randomized controlled trial. Am. J. Transplant. 7, 117–121 (2007).
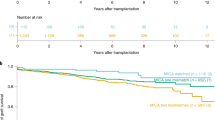
Montgomery, R. A. et al. Desensitization in HLA-incompatible kidney recipients and survival. N. Engl. J. Med. 365, 318–326 (2011).
Orandi, B. J. et al. Survival benefit with kidney transplants from HLA-incompatible live donors. N. Engl. J. Med. 374, 940–950 (2016).
Vo, A. A. et al. Rituximab and intravenous immune globulin for desensitization during renal transplantation. N. Engl. J. Med. 359, 242–251 (2008).
Burns, J. M. et al. Alloantibody levels and acute humoral rejection early after positive crossmatch kidney transplantation. Am. J. Transplant. 8, 2684–2694 (2008).
Montgomery, R. A. et al. Clinical results from transplanting incompatible live kidney donor/recipient pairs using kidney paired donation. JAMA 294, 1655–1663 (2005).
Perry, D. K. et al. Proteasome inhibition causes apoptosis of normal human plasma cells preventing alloantibody production. Am. J. Transplant. 9, 201–209 (2009).
Vo, A. A. et al. A phase I/II trial of the interleukin-6 receptor-specific humanized monoclonal (tocilizumab) + intravenous immunoglobulin in difficult to desensitize patients. Transplantation 99, 2356–2363 (2015).
Stegall, M. D. et al. Terminal complement inhibition decreases antibody-mediated rejection in sensitized renal transplant recipients. Am. J. Transplant. 11, 2405–2413 (2011).
Vo, A. A. et al. A phase I/II placebo-controlled trial of C1-inhibitor for prevention of antibody-mediated rejection in HLA sensitized patients. Transplantation 99, 299–308 (2015).
Montgomery, R. A. et al. Plasma-derived C1 esterase inhibitor for acute antibody-mediated rejection following kidney transplantation: results of a randomized double-blind placebo-controlled pilot study. Am. J. Transplant. 16, 3468–3478 (2016).
Jordan, S. C. et al. IgG endopeptidase in highly sensitized patients undergoing transplantation. N. Engl. J. Med. 377, 442–453 (2017).
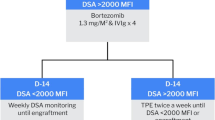
Moreno Gonzales, M. A. et al. 32 doses of bortezomib for desensitization is not well tolerated and is associated with only modest reductions in anti-HLA antibody. Transplantation 101, 1222–1227 (2017).
Everly, M. J. et al. Bortezomib provides effective therapy for antibody- and cell-mediated acute rejection. Transplantation 86, 1754–1761 (2008).
Waiser, J. et al. Comparison between bortezomib and rituximab in the treatment of antibody-mediated renal allograft rejection. Nephrol. Dial. Transplant. 27, 1246–1251 (2012).
Kwun, J. et al. Humoral compensation after bortezomib treatment of allosensitized recipients. J. Am. Soc. Nephrol. 28, 1991–1996 (2017).
Philogene, M. C., Sikorski, P., Montgomery, R. A., Leffell, M. S. & Zachary, A. A. Differential effect of bortezomib on HLA class I and class II antibody. Transplantation 98, 660–665 (2014).
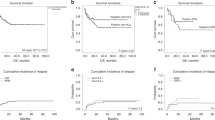
Loupy, A. et al. Complement-binding anti-HLA antibodies and kidney-allograft survival. N. Engl. J. Med. 369, 1215–1226 (2013).
Racusen, L. C. et al. Antibody-mediated rejection criteria - an addition to the Banff 97 classification of renal allograft rejection. Am. J. Transplant. 3, 708–714 (2003).
Solez, K. et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am. J. Transplant. 8, 753–760 (2008).
Sis, B. et al. Endothelial gene expression in kidney transplants with alloantibody indicates antibody-mediated damage despite lack of C4d staining. Am. J. Transplant. 9, 2312–2323 (2009).
Loupy, A. et al. Outcome of subclinical antibody-mediated rejection in kidney transplant recipients with preformed donor-specific antibodies. Am. J. Transplant. 9, 2561–2570 (2009).
Orandi, B. J. et al. Presentation and outcomes of C4d-negative antibody-mediated rejection after kidney transplantation. Am. J. Transplant. 16, 213–220 (2016).
Wiebe, C. et al. Evaluation of C1q status and titer of de novo donor-specific antibodies as predictors of allograft survival. Am. J. Transplant. 17, 703–711 (2017).
Tambur, A. R. & Wiebe, C. HLA diagnostics: evaluating DSA strength by titration. Transplantation 102, S23–S30 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01399593 (2017).
Lefaucheur, C. et al. Complement-activating anti-HLA antibodies in kidney transplantation: allograft gene expression profiling and response to treatment. J. Am. Soc. Nephrol. 29, 620–635 (2018).
Levy, J. H., & O’Donnell, P. S. The therapeutic potential of a kallikrein inhibitor for treating hereditary angioedema. Expert Opin. Investigat. Drugs 15, 1077–1090 (2006).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02547220 (2017).
Tanaka, T. & Kishimoto, T. The biology and medical implications of interleukin-6. Cancer Immunol. Res. 2, 288–294 (2014).
Mease, P. J. et al. The efficacy and safety of clazakizumab, an anti-interleukin-6 monoclonal antibody, in a phase IIb study of adults with active psoriatic arthritis. Arthritis. Rheumatol. 68, 2163–2173 (2016).
Choi, J. et al. Assessment of tocilizumab (anti-interleukin-6 receptor monoclonal) as a potential treatment for chronic antibody-mediated rejection and transplant glomerulopathy in HLA-sensitized renal allograft recipients. Am. J. Transplant. 17, 2381–2389 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03380377 (2018).
Wenig, K. et al. Structure of the streptococcal endopeptidase IdeS, a cysteine proteinase with strict specificity for IgG. Proc. Natl Acad. Sci. USA 101, 17371–17376 (2004).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02790437 (2018).
Jarnum, S., Bockermann, R., Runstrom, A., Winstedt, L. & Kjellman, C. The bacterial enzyme IdeS cleaves the IgG-type of B cell receptor (BCR), abolishes BCR-mediated cell signaling, and inhibits memory B cell activation. J. Immunol. 195, 5592–5601 (2015).
Montgomery, R. A., Lonze, B. E. & Tatapudi, V. S. IgG degrading enzyme of Streptococcus pyogenes: an exciting new development in desensitization therapy. Transplantation 102, 2–4 (2018).
Hariharan, S. et al. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N. Engl. J. Med. 342, 605–612 (2000).
Salama, A. D., Womer, K. L. & Sayegh, M. H. Clinical transplantation tolerance: many rivers to cross. J. Immunol. 178, 5419–5423 (2007).
Fehr, T. & Sykes, M. Clinical experience with mixed chimerism to induce transplantation tolerance. Transpl. Int. 21, 1118–1135 (2008).
Pilat, N. & Wekerle, T. Transplantation tolerance through mixed chimerism. Nat. Rev. Nephrol. 6, 594–605 (2010).
Denton, M. D., Magee, C. C. & Sayegh, M. H. Immunosuppressive strategies in transplantation. Lancet 353, 1083–1091 (1999).
Madariaga, M. L. et al. Effect of tolerance versus chronic immunosuppression protocols on the quality of life of kidney transplant recipients. JCI insight 1, e87019 (2016).
Montgomery, R. A. One kidney for life. Am. J. Transplant. 14, 1473–1474 (2014).
Cobbold, S. P., Martin, G., Qin, S. & Waldmann, H. Monoclonal antibodies to promote marrow engraftment and tissue graft tolerance. Nature 323, 164–166 (1986).
Kawai, T. et al. CD154 blockade for induction of mixed chimerism and prolonged renal allograft survival in nonhuman primates. Am. J. Transplant. 4, 1391–1398 (2004).
Kawai, T. et al. HLA-mismatched renal transplantation without maintenance immunosuppression. N. Engl. J. Med. 358, 353–361 (2008).
Scandling, J. D. et al. Tolerance and chimerism after renal and hematopoietic-cell transplantation. N. Engl. J. Med. 358, 362–368 (2008).
Leventhal, J. R. et al. HLA identical non-chimeric and HLA disparate chimeric renal transplant tolerance. Clin. Transpl. 145–156 (2013).
Strober, S., Lowsky, R. J., Shizuru, J. A., Scandling, J. D. & Millan, M. T. Approaches to transplantation tolerance in humans. Transplantation 77, 932–936 (2004).
Millan, M. T. et al. Mixed chimerism and immunosuppressive drug withdrawal after HLA-mismatched kidney and hematopoietic progenitor transplantation. Transplantation 73, 1386–1391 (2002).
Kawai, T., Sachs, D. H., Sykes, M., Cosimi, A. B. & Immune Tolerance Network. HLA-mismatched renal transplantation without maintenance immunosuppression. N. Engl. J. Med. 368, 1850–1852 (2013).
Luznik, L. et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol. Blood Marrow Transplant. 14, 641–650 (2008).
Bolanos-Meade, J. et al. HLA-haploidentical bone marrow transplantation with posttransplant cyclophosphamide expands the donor pool for patients with sickle cell disease. Blood 120, 4285–4291 (2012).
Leventhal, J. et al. Chimerism and tolerance without GVHD or engraftment syndrome in HLA-mismatched combined kidney and hematopoietic stem cell transplantation. Sci. Transl Med. 4, 124ra28 (2012).
Tang, Q. & Bluestone, J. A. Regulatory T cell therapy in transplantation: moving to the clinic. Cold Spring Harb. Perspect. Med. 3, a015552 (2013).
Hori, S., Nomura, T. & Sakaguchi, S. Control of regulatory T cell development by the transcription factor Foxp3. Science 299, 1057–1061 (2003).
Gregersen, P. K. & Behrens, T. W. Genetics of autoimmune diseases — disorders of immune homeostasis. Nat. Rev. Genet. 7, 917–928 (2006).
Muthukumar, T. et al. Messenger RNA for FOXP3 in the urine of renal-allograft recipients. N. Engl. J. Med. 353, 2342–2351 (2005).
Zwang, N. A. & Leventhal, J. R. Cell therapy in kidney transplantation: focus on regulatory T cells. J. Am. Soc. Nephrol. 28, 1960–1972 (2017).
Roncarolo, M. G. & Battaglia, M. Regulatory T cell immunotherapy for tolerance to self antigens and alloantigens in humans. Nat. Rev. Immunol. 7, 585–598 (2007).
Bluestone, J. A. et al. Type 1 diabetes immunotherapy using polyclonal regulatory T cells. Sci. Transl Med. 7, 315ra189 (2015).
Jones, A. G. & Hattersley, A. T. The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabet. Med. 30, 803–817 (2013).
Leighton, E., Sainsbury, C. A. & Jones, G. C. A practical review of C-peptide testing in diabetes. Diabetes Ther. 8, 475–487 (2017).
Trzonkowski, P. et al. First-in-man clinical results of the treatment of patients with graft versus host disease with human ex vivo expanded CD4+CD25+CD127- T regulatory cells. Clin. Immunol. 133, 22–26 (2009).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02129881 (2014).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02088931 (2016).
Todo, S. et al. A pilot study of operational tolerance with a regulatory T cell-based cell therapy in living donor liver transplantation. Hepatology 64, 632–643 (2016).
Yang, J. et al. Allograft rejection mediated by memory T cells is resistant to regulation. Proc. Natl Acad. Sci. USA 104, 19954–19959 (2007).
Korn, T. et al. Myelin-specific regulatory T cells accumulate in the CNS but fail to control autoimmune inflammation. Nat. Med. 13, 423–431 (2007).
Li, X. C. & Turka, L. A. An update on regulatory T cells in transplant tolerance and rejection. Nat. Rev. Nephrol. 6, 577–583 (2010).
Taylor, C. J., Chapman, J. R., Ting, A. & Morris, P. J. Characterization of lymphocytotoxic antibodies causing a positive crossmatch in renal transplantation. Relationship to primary and regraft outcome. Transplantation 48, 953–958 (1989).
Tinckam, K. Histocompatibility methods. Transplantat. Rev. 23, 80–93 (2009).
Zangwill, S. D. et al. The virtual crossmatch—a screening tool for sensitized pediatric heart transplant recipients. Pediatr. Transplant. 10, 38–41 (2006).
Appel, J. Z. et al. Role of flow cytometry to define unacceptable HLA antigens in lung transplant recipients with HLA-specific antibodies. Transplantation 81, 1049–1057 (2006).
Johnson, C. & Ellis, T. Reply to “Allocation Based on Virtual Crossmatch Alone: Not. Yet Ready for Primetime”. Am. J. Transplant. 16, 3578–3579 (2016).
Tait, B. D. et al. Review article: Luminex technology for HLA antibody detection in organ transplantation. Nephrology 14, 247–254 (2009).
Tait, B. D. et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation 95, 19–47 (2013).
Organ Procurement and Transplantation Network. Kidney allocation system webinar — what referring physicians need to know. U.S. Department of Health and Human Services https://optn.transplant.hrsa.gov/news/kidney-allocation-system-webinar-what-referring-physicians-need-toknow/ (2014).
Author information
Authors and Affiliations
Contributions
All authors researched the data, discussed the content, wrote the manuscript and reviewed and/or edited the text before submission.
Corresponding author
Ethics declarations
Competing interests
R.A.M. has served on advisory boards for Genentech Scientific/ROCHE, True North Therapeutics/iPierian, Alexion, Novartis and Hansa Medical and has received consulting fees from OrbiMed, GuidePoint Global, Sucampo Pharmaceuticals, Astellas Pharma and Shire. He has also received research grants from the Immune Tolerance Network, ViroPharma, Hansa and Alexion. V.S.T., M.S.L. and A.A.Z. declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Tolerance
-
Defined in the context of transplantation as the clinical state of acceptance of allograft by the recipient without chronic immunosuppression.
- Sequence-specific priming
-
(SSP). A molecular method of HLA typing in which isolated DNA is amplified in the presence of specific primers that are complementary to the HLA alleles of interest.
- Reverse sequence-specific oligonucleotide probing
-
(rSSOP). A molecular method of HLA typing in which amplified DNA is mixed with oligonucleotide probes that are complementary to the unique segments of the DNA that encode the HLA alleles of interest.
- Class I and class II antigens
-
HLA class I (HLA-A, HLA-B and HLA-C) antigens and HLA class II (HLA-DP, HLA-DQ and HLA-DR) antigens are molecules encoded by genes in the major histocompatibility complex and play a key role in antigen presentation to T cells that orchestrate immune responses and tumour surveillance.
- Hyperacute rejection
-
A severe form of rejection that occurs within minutes or hours of allograft reperfusion that is caused by preformed donor-specific antibodies.
- Anergic state
-
A tolerance mechanism in which the lymphocyte is functionally inactivated following an antigen encounter in the absence of co-stimulation.
- Co-stimulatory blockade
-
Inhibition of T cell activation by prevention of interaction between co-stimulatory molecules expressed on T cells and antigen-presenting cells.
- Transient chimaerism
-
Clinical state following haematopoietic cell transplantation in which chimaerism is achieved only transiently.
- Full-donor chimaerism
-
Clinical state following haematopoietic cell transplantation in which the recipient exhibits haematopoietic cells only of donor origin. Full-donor chimaerism has been attempted as a tolerance protocol in experimental transplant models and in humans.
- Graft versus host disease
-
(GVHD). Multisystem disorder that may occur following allogeneic haematopoietic cell transplant owing to immune response directed by donor immune cells against the recipient.
Rights and permissions
About this article
Cite this article
Montgomery, R.A., Tatapudi, V.S., Leffell, M.S. et al. HLA in transplantation. Nat Rev Nephrol 14, 558–570 (2018). https://doi.org/10.1038/s41581-018-0039-x
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-018-0039-x
This article is cited by
-
The construction of modular universal chimeric antigen receptor T (MU-CAR-T) cells by covalent linkage of allogeneic T cells and various antibody fragments
Molecular Cancer (2024)
-
Tutorial: a statistical genetics guide to identifying HLA alleles driving complex disease
Nature Protocols (2023)
-
High-throughput sequencing defines donor and recipient HLA B-cell epitope frequencies for prospective matching in transplantation
Communications Biology (2021)
-
Galectin-9 is required for endometrial regenerative cells to induce long-term cardiac allograft survival in mice
Stem Cell Research & Therapy (2020)
-
Current status and future perspectives of HLA-edited induced pluripotent stem cells
Inflammation and Regeneration (2020)