Abstract
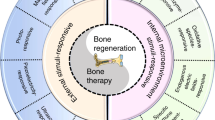
Successful materials design for bone-tissue engineering requires an understanding of the composition and structure of native bone tissue, as well as appropriate selection of biomimetic natural or tunable synthetic materials (biomaterials), such as polymers, bioceramics, metals and composites. Scalable fabrication technologies that enable control over construct architecture at multiple length scales, including three-dimensional printing and electric-field-assisted techniques, can then be employed to process these biomaterials into suitable forms for bone-tissue engineering. In this Review, we provide an overview of materials-design considerations for bone-tissue-engineering applications in both disease modelling and treatment of injuries and disease in humans. We outline the materials-design pathway from implementation strategy through selection of materials and fabrication methods to evaluation. Finally, we discuss unmet needs and current challenges in the development of ideal materials for bone-tissue regeneration and highlight emerging strategies in the field.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Annamalai, R. T. et al. Injectable osteogenic microtissues containing mesenchymal stromal cells conformally fill and repair critical-size defects. Biomaterials 208, 32–44 (2019).
Zhang, X. J., Li, Y., Chen, Y. E., Chen, J. H. & Ma, P. X. Cell-free 3D scaffold with two-stage delivery of miRNA-26a to regenerate critical-sized bone defects. Nat. Commun. 7, 10376 (2016).
Schemitsch, E. H. Size matters: defining critical in bone defect size! J. Orthop. Trauma 31, S20–S22 (2017).
Atala, A., Kasper, F. K. & Mikos, A. G. Engineering complex tissues. Sci. Transl. Med. 4, 160rv12 (2012).
McDermott, A. M. et al. Recapitulating bone development through engineered mesenchymal condensations and mechanical cues for tissue regeneration. Sci. Transl. Med. 11, eaav7756 (2019).
Lee, J. W. et al. Long-term clinical study and multiscale analysis of in vivo biodegradation mechanism of Mg alloy. Proc. Natl Acad. Sci. USA 113, 716–721 (2016). These researchers studied the bone-forming mechanism of biodegradable magnesium alloy implants and conducted a clinical study that confirmed total implant degradation and bone-defect regeneration within 1 year.
Bhumiratana, S. et al. Tissue-engineered autologous grafts for facial bone reconstruction. Sci. Transl. Med. 8, 343ra83 (2016).
Bez, M. et al. In situ bone tissue engineering via ultrasound-mediated gene delivery to endogenous progenitor cells in mini-pigs. Sci. Transl. Med. 9, eaal3128 (2017).
Norris, C. J., Meadway, G. J., O’Sullivan, M. J., Bond, I. P. & Trask, R. S. Self-healing fibre reinforced composites via a bioinspired vasculature. Adv. Funct. Mater. 21, 3624–3633 (2011).
Dorozhkin, S. V. A detailed history of calcium orthophosphates from 1770s till 1950. Mater. Sci. Eng. C 33, 3085–3110 (2013).
Woodruff, M. A. et al. Bone tissue engineering: from bench to bedside. Mater. Today 15, 430–435 (2012).
Martino, M. M. et al. Growth factors engineered for super-affinity to the extracellular matrix enhance tissue healing. Science 343, 885–888 (2014).
Liu, Y., Luo, D. & Wang, T. Hierarchical structures of bone and bioinspired bone tissue engineering. Small 12, 4611–4632 (2016).
Gentleman, E. et al. Comparative materials differences revealed in engineered bone as a function of cell-specific differentiation. Nat. Mater. 8, 763–770 (2009).
Bohner, M. & Miron, R. J. A proposed mechanism for material-induced heterotopic ossification. Mater. Today 22, 132–141 (2019).
Gautieri, A., Vesentini, S., Redaelli, A. & Buehler, M. J. Hierarchical structure and nanomechanics of collagen microfibrils from the atomistic scale up. Nano Lett. 11, 757–766 (2011).
Liu, Y. et al. Hierarchical intrafibrillar nanocarbonated apatite assembly improves the nanomechanics and cytocompatibility of mineralized collagen. Adv. Funct. Mater. 23, 1404–1411 (2013).
Feng, C. et al. 3D printing of lotus root-like biomimetic materials for cell delivery and tissue regeneration. Adv. Sci. 4, 1700401 (2017).
Zhou, T. et al. A mussel-inspired persistent ROS-scavenging, electroactive, and osteoinductive scaffold based on electrochemical-driven in situ nanoassembly. Small 15, e1805440 (2019).
Ryu, J., Ku, S. H., Lee, H. & Park, C. B. Mussel-inspired polydopamine coating as a universal route to hydroxyapatite crystallization. Adv. Funct. Mater. 20, 2132–2139 (2010).
Hu, X. X. et al. A difunctional regeneration scaffold for knee repair based on aptamer-directed cell recruitment. Adv. Mater. 29, 1605235 (2017).
Yu, L. et al. BMP9 stimulates joint regeneration at digit amputation wounds in mice. Nat. Commun. 10, 424 (2019).
Hunter, N. L. & Sherman, R. E. Combination products: modernizing the regulatory paradigm. Nat. Rev. Drug Discov. 16, 513–514 (2017).
Burdick, J. A., Mauck, R. L., Gorman, J. H. 3rd & Gorman, R. C. Acellular biomaterials: an evolving alternative to cell-based therapies. Sci. Transl. Med. 5, 176ps4 (2013).
Wang, S. et al. Mineralized collagen-based composite bone materials for cranial bone regeneration in developing sheep. ACS Biomater. Sci. Eng. 3, 1092–1099 (2017).
Wang, S. et al. A high-strength mineralized collagen bone scaffold for large-sized cranial bone defect repair in sheep. Regen. Biomater. 5, 283–292 (2018).
Kim, Y. S., Smoak, M. M., Melchiorri, A. J. & Mikos, A. G. An overview of the tissue engineering market in the United States from 2011 to 2018. Tissue Eng. A 25, 1–8 (2019).
Kretlow, J. D., Young, S., Klouda, L., Wong, M. & Mikos, A. G. Injectable biomaterials for regenerating complex craniofacial tissues. Adv. Mater. 21, 3368–3393 (2009).
Reichert, J. C. et al. A tissue engineering solution for segmental defect regeneration in load-bearing long bones. Sci. Transl. Med. 4, 141ra93 (2012).
Du, Y., Guo, J. L., Wang, J., Mikos, A. G. & Zhang, S. Hierarchically designed bone scaffolds: from internal cues to external stimuli. Biomaterials 218, 119334 (2019).
Jin, S. S. et al. A biomimetic hierarchical nanointerface orchestrates macrophage polarization and mesenchymal stem cell recruitment to promote endogenous bone regeneration. ACS Nano 13, 6581–6595 (2019).
Stuckensen, K. et al. Tissue mimicry in morphology and composition promotes hierarchical matrix remodeling of invading stem cells in osteochondral and meniscus scaffolds. Adv. Mater. 30, 1706754 (2018).
Jakus, A. E. et al. Hyperelastic “bone”: a highly versatile, growth factor-free, osteoregenerative, scalable, and surgically friendly biomaterial. Sci. Transl. Med. 8, 358ra127 (2016).
Roohani-Esfahani, S. I., Newman, P. & Zreiqat, H. Design and fabrication of 3D printed scaffolds with a mechanical strength comparable to cortical bone to repair large bone defects. Sci. Rep. 6, 19468 (2016).
Nasajpour, A. et al. A multifunctional polymeric periodontal membrane with osteogenic and antibacterial characteristics. Adv. Funct. Mater. 28, 1703437 (2018).
Holloway, J. L. One step solution for fighting bacteria and growing bone. Sci. Transl. Med. 11, eaaw5326 (2019).
Lai, Y. X. et al. Porous composite scaffold incorporating osteogenic phytomolecule icariin for promoting skeletal regeneration in challenging osteonecrotic bone in rabbits. Biomaterials 153, 1–13 (2018).
Li, C. Y. et al. Engineered multifunctional nanomedicine for simultaneous stereotactic chemotherapy and inhibited osteolysis in an orthotopic model of bone metastasis. Adv. Mater. 29, 1605754 (2017).
Mora-Raimundo, P., Lozano, D., Manzano, M. & Vallet-Regi, M. Nanoparticles to knockdown osteoporosis-related gene and promote osteogenic marker expression for osteoporosis treatment. ACS Nano 13, 5451–5464 (2019).
Liu, M., Nakasaki, M., Shih, Y. V. & Varghese, S. Effect of age on biomaterial-mediated in situ bone tissue regeneration. Acta Biomater. 78, 329–340 (2018).
Josephson, A. M. et al. Age-related inflammation triggers skeletal stem/progenitor cell dysfunction. Proc. Natl Acad. Sci. USA 116, 6995–7004 (2019).
Feins, E. N. et al. A growth-accommodating implant for paediatric applications. Nat. Biomed. Eng. 1, 818–825 (2017).
Hollister, S. J. Paediatric devices that grow up. Nat. Biomed. Eng. 1, 777–778 (2017).
Gabel, L., Macdonald, H. M. & McKay, H. A. Sex differences and growth-related adaptations in bone microarchitecture, geometry, density, and strength from childhood to early adulthood: a mixed longitudinal HR-pQCT study. J. Bone Miner. Res. 32, 250–263 (2017).
Fong, E. L. S., Watson, B. M., Kasper, F. K. & Mikos, A. G. Building bridges: leveraging interdisciplinary collaborations in the development of biomaterials to meet clinical needs. Adv. Mater. 24, 4995–5013 (2012).
Thrivikraman, G. et al. Rapid fabrication of vascularized and innervated cell-laden bone models with biomimetic intrafibrillar collagen mineralization. Nat. Commun. 10, 3520 (2019).
Shih, Y. V. & Varghese, S. Tissue engineered bone mimetics to study bone disorders ex vivo: role of bioinspired materials. Biomaterials 198, 107–121 (2019).
Fong, E. L. S. et al. Modeling Ewing sarcoma tumors in vitro with 3D scaffolds. Proc. Natl Acad. Sci. USA 110, 6500–6505 (2013).
Martine, L. C. et al. Engineering a humanized bone organ model in mice to study bone metastases. Nat. Protoc. 12, 639–663 (2017).
He, F. et al. Multiscale characterization of the mineral phase at skeletal sites of breast cancer metastasis. Proc. Natl Acad. Sci. USA 114, 10542–10547 (2017).
Talukdar, S. & Kundu, S. C. Engineered 3D silk-based metastasis models: interactions between human breast adenocarcinoma, mesenchymal stem cells and osteoblast-like cells. Adv. Funct. Mater. 23, 5249–5260 (2013).
Dondossola, E. et al. Intravital microscopy of osteolytic progression and therapy response of cancer lesions in the bone. Sci. Transl. Med. 10, eaao5726 (2018).
Williams, D. F. The Williams Dictionary of Biomaterials (Liverpool Univ. Press, 1999).
Pajarinen, J. et al. Mesenchymal stem cell-macrophage crosstalk and bone healing. Biomaterials 196, 80–89 (2019).
Kohane, D. S. & Langer, R. Biocompatibility and drug delivery systems. Chem. Sci. 1, 441–446 (2010).
Lei, M. et al. Programmable electrofabrication of porous Janus films with tunable Janus balance for anisotropic cell guidance and tissue regeneration. Adv. Funct. Mater. 29, 1900065 (2019).
Lu, J. Y. et al. Multilayered graphene hydrogel membranes for guided bone regeneration. Adv. Mater. 28, 4025–4031 (2016).
Deng, C. J. et al. Micro/nanometer-structured scaffolds for regeneration of both cartilage and subchondral bone. Adv. Funct. Mater. 29, 1806068 (2019).
Petersen, A. et al. A biomaterial with a channel-like pore architecture induces endochondral healing of bone defects. Nat. Commun. 9, 4430 (2018). In this study, pore channels within collagen scaffolds directed cell alignment and ECM fibre orientation, resulting in fibrocartilage, which is progressively mineralized into bone.
Guo, J. L. et al. Modular, tissue-specific, and biodegradable hydrogel cross-linkers for tissue engineering. Sci. Adv. 5, eaaw7396 (2019).
Blokhuis, T. J. & Arts, J. J. C. Bioactive and osteoinductive bone graft substitutes: definitions, facts and myths. Injury 42 (Suppl. 2), S26–S29 (2011).
Gaharwar, A. K. et al. Bioactive silicate nanoplatelets for osteogenic differentiation of human mesenchymal stem cells. Adv. Mater. 25, 3329–3336 (2013).
Hoppe, A., Güldal, N. S. & Boccaccini, A. R. A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials 32, 2757–2774 (2011).
Tatara, A. M. et al. Biomaterials-aided mandibular reconstruction using in vivo bioreactors. Proc. Natl Acad. Sci. USA 116, 6954–6963 (2019). This report describes bioreactor chambers filled with bioceramics and implanted against the ribs in a large-animal model. The generated bone was used to reconstruct a craniofacial defect.
Ma, Q.-L. et al. Improved implant osseointegration of a nanostructured titanium surface via mediation of macrophage polarization. Biomaterials 35, 9853–9867 (2014).
Zhu, Y. et al. Bone regeneration with micro/nano hybrid-structured biphasic calcium phosphate bioceramics at segmental bone defect and the induced immunoregulation of MSCs. Biomaterials 147, 133–144 (2017).
Nonoyama, T. et al. Double-network hydrogels strongly bondable to bones by spontaneous osteogenesis penetration. Adv. Mater. 28, 6740–6745 (2016).
Wang, S. F. et al. Molecularly engineered biodegradable polymer networks with a wide range of stiffness for bone and peripheral nerve regeneration. Adv. Funct. Mater. 25, 2715–2724 (2015). In this study, varying the compositional ratio in copolymers of PCL and poly(propylene fumarate) enabled tuning of scaffold mechanical properties, thermal behaviour and tissue-specific regenerative capacity.
Du, Y. Z. et al. Development of a multifunctional platform based on strong, intrinsically photoluminescent and antimicrobial silica-poly(citrates)-based hybrid biodegradable elastomers for bone regeneration. Adv. Funct. Mater. 25, 5016–5029 (2015).
Takizawa, T. et al. Titanium fiber plates for bone tissue repair. Adv. Mater. 30, 1703608 (2018).
Pobloth, A.-M. et al. Mechanobiologically optimized 3D titanium-mesh scaffolds enhance bone regeneration in critical segmental defects in sheep. Sci. Transl. Med. 10, eaam8828 (2018).
Zhang, B., Filion, T. M., Kutikov, A. B. & Song, J. Facile stem cell delivery to bone grafts enabled by smart shape recovery and stiffening of degradable synthetic periosteal membranes. Adv. Funct. Mater. 27, 1604784 (2017).
Feng, P. et al. A multimaterial scaffold with tunable properties: toward bone tissue repair. Adv. Sci. 5, 1700817 (2018).
Mahony, O. et al. Silica-gelatin hybrids with tailorable degradation and mechanical properties for tissue regeneration. Adv. Funct. Mater. 20, 3835–3845 (2010).
Wei, D. X., Dao, J. W. & Chen, G. Q. A micro-ark for cells: highly open porous polyhydroxyalkanoate microspheres as injectable scaffolds for tissue regeneration. Adv. Mater. 30, 1802273 (2018).
Lin, Z. J. et al. Precisely controlled delivery of magnesium ions thru sponge-like monodisperse PLGA/nano-MgO-alginate core-shell microsphere device to enable in-situ bone regeneration. Biomaterials 174, 1–16 (2018).
Cui, H. T., Zhu, W., Holmes, B. & Zhang, L. G. Biologically inspired smart release system based on 3D bioprinted perfused scaffold for vascularized tissue regeneration. Adv. Sci. 3, 1600058 (2016).
Luo, Z. Y. et al. Injectable 3D porous micro-scaffolds with a bio-engine for cell transplantation and tissue regeneration. Adv. Funct. Mater. 28, 1804335 (2018).
Wang, M. O. et al. Evaluating 3D-printed biomaterials as scaffolds for vascularized bone tissue engineering. Adv. Mater. 27, 138–144 (2015).
Karageorgiou, V. & Kaplan, D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26, 5474–5491 (2005).
Zhu, C. L., Pongkitwitoon, S., Qiu, J. C., Thomopoulos, S. & Xia, Y. N. Design and fabrication of a hierarchically structured scaffold for tendon-to-bone repair. Adv. Mater. 30, 1707306 (2018).
Brazill, J. M., Beeve, A. T., Craft, C. S., Ivanusic, J. J. & Scheller, E. L. Nerves in bone: evolving concepts in pain and anabolism. J. Bone Miner. Res. 34, 1393–1406 (2019).
Sayilekshmy, M. et al. Innervation is higher above bone remodeling surfaces and in cortical pores in human bone: lessons from patients with primary hyperparathyroidism. Sci. Rep. 9, 5361 (2019).
Jones, R. E. et al. Skeletal stem cell–Schwann cell circuitry in mandibular repair. Cell Rep. 28, 2757–2766 (2019).
Diba, M. et al. Composite colloidal gels made of bisphosphonate-functionalized gelatin and bioactive glass particles for regeneration of osteoporotic bone defects. Adv. Funct. Mater. 27, 1703438 (2017). These researchers demonstrated that injectable and self-healing composite gels assembled from pharmaceutical-functionalized gelatin and bioactive glass particles could regenerate bone defects and increase bone density in osteoporotic animals.
Zhang, K. Y. et al. Adaptable hydrogels mediate cofactor-assisted activation of biomarker-responsive drug delivery via positive feedback for enhanced tissue regeneration. Adv. Sci. 5, 1800875 (2018).
Rosales, A. M. & Anseth, K. S. The design of reversible hydrogels to capture extracellular matrix dynamics. Nat. Rev. Mater. 1, 15012 (2016).
Feng, Q. et al. Mechanically resilient, injectable, and bioadhesive supramolecular gelatin hydrogels crosslinked by weak host-guest interactions assist cell infiltration and in situ tissue regeneration. Biomaterials 101, 217–228 (2016).
Diba, M. et al. Self-healing biomaterials: from molecular concepts to clinical applications. Adv. Mater. Interfaces 5, 1800118 (2018).
Tan, J. L. et al. Sustained release of two bioactive factors from supramolecular hydrogel promotes periodontal bone regeneration. ACS Nano 13, 5616–5622 (2019).
Xu, B. et al. A mineralized high strength and tough hydrogel for skull bone regeneration. Adv. Funct. Mater. 27, 1604327 (2017).
Bittner, S. M., Guo, J. L., Melchiorri, A. & Mikos, A. G. Three-dimensional printing of multilayered tissue engineering scaffolds. Mater. Today 21, 861–874 (2018).
Sant, S. et al. Self-assembled hydrogel fiber bundles from oppositely charged polyelectrolytes mimic micro-/nanoscale hierarchy of collagen. Adv. Funct. Mater. 27, 1606273 (2017).
Loessner, D. et al. Functionalization, preparation and use of cell-laden gelatin methacryloyl-based hydrogels as modular tissue culture platforms. Nat. Protoc. 11, 727–746 (2016).
Ying, G. L. et al. Aqueous two-phase emulsion bioink-enabled 3D bioprinting of porous hydrogels. Adv. Mater. 30, 1805460 (2018).
Ren, X. Y. et al. Osteoprotegerin reduces osteoclast resorption activity without affecting osteogenesis on nanoparticulate mineralized collagen scaffolds. Sci. Adv. 5, eaaw4991 (2019).
Lausch, A. J., Chong, L. C., Uludag, H. & Sone, E. D. Multiphasic collagen scaffolds for engineered tissue interfaces. Adv. Funct. Mater. 28, 1804730 (2018).
Liu, Y. et al. Hierarchically staggered nanostructure of mineralized collagen as a bone-grafting scaffold. Adv. Mater. 28, 8740–8748 (2016).
Neffe, A. T. et al. One step creation of multifunctional 3D architectured hydrogels inducing bone regeneration. Adv. Mater. 27, 1738–1744 (2015).
Sarker, B. et al. Oxidized alginate-gelatin hydrogel: a favorable matrix for growth and osteogenic differentiation of adipose-derived stem cells in 3D. ACS Biomater. Sci. Eng. 3, 1730–1737 (2017).
Chang, S. W. & Buehler, M. J. Molecular biomechanics of collagen molecules. Mater. Today 17, 70–76 (2014).
Zhao, X. et al. Injectable stem cell-laden photocrosslinkable microspheres fabricated using microfluidics for rapid generation of osteogenic tissue constructs. Adv. Funct. Mater. 26, 2809–2819 (2016).
Luo, Z. Y. et al. Time-responsive osteogenic niche of stem cells: a sequentially triggered, dual-peptide loaded, alginate hybrid system for promoting cell activity and osteo-differentiation. Biomaterials 163, 25–42 (2018).
Darnell, M. et al. Material microenvironmental properties couple to induce distinct transcriptional programs in mammalian stem cells. Proc. Natl Acad. Sci. USA 115, E8368–E8377 (2018).
Jeon, O., Lee, K. & Alsberg, E. Spatial micropatterning of growth factors in 3D hydrogels for location-specific regulation of cellular behaviors. Small 14, e1800579 (2018).
Lueckgen, A. et al. Enzymatically-degradable alginate hydrogels promote cell spreading and in vivo tissue infiltration. Biomaterials 217, 119294 (2019).
Shi, L. Y. et al. Self-healing silk fibroin-based hydrogel for bone regeneration: dynamic metal-ligand self-assembly approach. Adv. Funct. Mater. 27, 1700591 (2017).
Liu, H. et al. Composite scaffolds of nano-hydroxyapatite and silk fibroin enhance mesenchymal stem cell-based bone regeneration via the interleukin 1α autocrine/paracrine signaling loop. Biomaterials 49, 103–112 (2015).
Partlow, B. P. et al. Highly tunable elastomeric silk biomaterials. Adv. Funct. Mater. 24, 4615–4624 (2014).
Marelli, B. et al. Silk fibroin derived polypeptide-induced biomineralization of collagen. Biomaterials 33, 102–108 (2012).
Rai, R., Keshavarz, T., Roether, J. A., Boccaccini, A. R. & Roy, I. Medium chain length polyhydroxyalkanoates, promising new biomedical materials for the future. Mater. Sci. Eng. R Rep. 72, 29–47 (2011).
Ruan, J. et al. Enhanced physiochemical and mechanical performance of chitosan-grafted graphene oxide for superior osteoinductivity. Adv. Funct. Mater. 26, 1085–1097 (2016).
Muller, W. E. G. et al. Transformation of amorphous polyphosphate nanoparticles into coacervate complexes: an approach for the encapsulation of mesenchymal stem cells. Small 14, e1801170 (2018).
Papageorgiou, P. et al. Expanded skeletal stem and progenitor cells promote and participate in induced bone regeneration at subcritical BMP-2 dose. Biomaterials 217, 119278 (2019).
Li, L. et al. 3D molecularly functionalized cell-free biomimetic scaffolds for osteochondral regeneration. Adv. Funct. Mater. 29, 1807356 (2019).
Hasani-Sadrabadi, M. M. et al. Hierarchically patterned polydopamine-containing membranes for periodontal tissue engineering. ACS Nano 13, 3830–3838 (2019).
Yan, Y. F. et al. Vascularized 3D printed scaffolds for promoting bone regeneration. Biomaterials 190–191, 97–110 (2019).
Kasper, F. K., Tanahashi, K., Fisher, J. P. & Mikos, A. G. Synthesis of poly(propylene fumarate). Nat. Protoc. 4, 518–525 (2009).
Wilson, J. A. et al. Magnesium catalyzed polymerization of end functionalized poly(propylene maleate) and poly(propylene fumarate) for 3D printing of bioactive scaffolds. J. Am. Chem. Soc. 140, 277–284 (2018).
Zhang, S. et al. Polylactic acid nanopillar array-driven osteogenic differentiation of human adipose-derived stem cells determined by pillar diameter. Nano Lett. 18, 2243–2253 (2018).
Yao, Q. Q. et al. Three dimensional electrospun PCL/PLA blend nanofibrous scaffolds with significantly improved stem cells osteogenic differentiation and cranial bone formation. Biomaterials 115, 115–127 (2017).
Washington, M. A. et al. The impact of monomer sequence and stereochemistry on the swelling and erosion of biodegradable poly(lactic-co-glycolic acid) matrices. Biomaterials 117, 66–76 (2017).
Kirillova, A., Kelly, C., von Windheim, N. & Gall, K. Bioinspired mineral–organic bioresorbable bone adhesive. Adv. Healthc. Mater. 7, e1800467 (2018).
Shi, X. T. et al. Periosteum-mimetic structures made from freestanding microgrooved nanosheets. Adv. Mater. 26, 3290–3296 (2014).
Johnson, C. T. et al. Hydrogel delivery of lysostaphin eliminates orthopedic implant infection by Staphylococcus aureus and supports fracture healing. Proc. Natl Acad. Sci. USA 115, E4960–E4969 (2018).
Vo, T. N. et al. Injectable dual-gelling cell-laden composite hydrogels for bone tissue engineering. Biomaterials 83, 1–11 (2016).
Lin, P., Ma, S., Wang, X. & Zhou, F. Molecularly engineered dual-crosslinked hydrogel with ultrahigh mechanical strength, toughness, and good self-recovery. Adv. Mater. 27, 2054–2059 (2015).
Rodell, C. B. et al. Shear-thinning supramolecular hydrogels with secondary autonomous covalent crosslinking to modulate viscoelastic properties in vivo. Adv. Funct. Mater. 25, 636–644 (2015).
Gong, J. P., Katsuyama, Y., Kurokawa, T. & Osada, Y. Double-network hydrogels with extremely high mechanical strength. Adv. Mater. 15, 1155–1158 (2003).
Zhao, Y. et al. Proteoglycans and glycosaminoglycans improve toughness of biocompatible double network hydrogels. Adv. Mater. 26, 436–442 (2014).
Mredha, M. T. I. et al. Anisotropic tough double network hydrogel from fish collagen and its spontaneous in vivo bonding to bone. Biomaterials 132, 85–95 (2017).
Vallet-Regí, M. & Ruiz-Hernández, E. Bioceramics: from bone regeneration to cancer nanomedicine. Adv. Mater. 23, 5177–5218 (2011).
Zhou, Y. L., Wu, C. T. & Chang, J. Bioceramics to regulate stem cells and their microenvironment for tissue regeneration. Mater. Today 24, 41–56 (2019).
Chen, L. et al. 3D printing of a lithium-calcium-silicate crystal bioscaffold with dual bioactivities for osteochondral interface reconstruction. Biomaterials 196, 138–150 (2019).
Félix Lanao, R. P., Leeuwenburgh, S. C. G., Wolke, J. G. C. & Jansen, J. A. Bone response to fast-degrading, injectable calcium phosphate cements containing PLGA microparticles. Biomaterials 32, 8839–8847 (2011).
Tang, Z., Li, X., Tan, Y., Fan, H. & Zhang, X. The material and biological characteristics of osteoinductive calcium phosphate ceramics. Regen. Biomater. 5, 43–59 (2018).
Bohner, M. et al. Characterization and distribution of mechanically competent mineralized tissue in micropores of β-tricalcium phosphate bone substitutes. Mater. Today 20, 106–115 (2017).
Groen, N. et al. Linking the transcriptional landscape of bone induction to biomaterial design parameters. Adv. Mater. 29, 1603259 (2017).
Kim, J. A. et al. Magnesium phosphate ceramics incorporating a novel indene compound promote osteoblast differentiation in vitro and bone regeneration in vivo. Biomaterials 157, 51–61 (2018).
Bunpetch, V. et al. Silicate-based bioceramic scaffolds for dual-lineage regeneration of osteochondral defect. Biomaterials 192, 323–333 (2019).
Fujishiro, Y., Hench, L. L. & Oonishi, H. Quantitative rates of in vivo bone generation for Bioglass® and hydroxyapatite particles as bone graft substitute. J. Mater. Sci. Mater. Med. 8, 649–652 (1997).
Jones, J. R. Review of bioactive glass: from Hench to hybrids. Acta Biomater. 9, 4457–4486 (2013).
Hench, L. L., Splinter, R. J., Allen, W. C. & Greenlee, T. K. Bonding mechanisms at the interface of ceramic prosthetic materials. J. Biomed. Mater. Res. 5, 117–141 (1971).
Hench, L. L. & Polak, J. M. Third-generation biomedical materials. Science 295, 1014–1017 (2002).
Zhao, F. J. et al. Promoting in vivo early angiogenesis with sub-micrometer strontium-contained bioactive microspheres through modulating macrophage phenotypes. Biomaterials 178, 36–47 (2018).
Lin, D. et al. Rapid initiation of guided bone regeneration driven by spatiotemporal delivery of IL-8 and BMP-2 from hierarchical MBG-based scaffold. Biomaterials 196, 122–137 (2019).
Rouquerol, J. et al. Recommendations for the characterization of porous solids. Pure Appl. Chem. 66, 1739–1758 (1994).
Li, J. H. et al. Valence state manipulation of cerium oxide nanoparticles on a titanium surface for modulating cell fate and bone formation. Adv. Sci. 5, 1700678 (2018).
Yu, H. J. et al. Ductile biodegradable Mg-based metallic glasses with excellent biocompatibility. Adv. Funct. Mater. 23, 4793–4800 (2013).
Jo, Y. K., Choi, B. H., Kim, C. S. & Cha, H. J. Diatom-inspired silica nanostructure coatings with controllable microroughness using an engineered mussel protein glue to accelerate bone growth on titanium-based implants. Adv. Mater. 29, 1704906 (2017).
Zhao, W. T. et al. Rapid evaluation of bioactive Ti-based surfaces using an in vitro titration method. Nat. Commun. 10, 2062 (2019).
Kohno, Y. et al. Treating titanium particle-induced inflammation with genetically modified NF-κB sensing IL-4 secreting or preconditioned mesenchymal stem cells in vitro. ACS Biomater. Sci. Eng. 5, 3032–3038 (2019).
Virtanen, S. Biodegradable Mg and Mg alloys: corrosion and biocompatibility. Mater. Sci. Eng. B 176, 1600–1608 (2011).
Cheng, P. F. et al. High-purity magnesium interference screws promote fibrocartilaginous entheses regeneration in the anterior cruciate ligament reconstruction rabbit model via accumulation of BMP-2 and VEGF. Biomaterials 81, 14–26 (2016).
Wang, Q. W. et al. Response of MAPK pathway to iron oxide nanoparticles in vitro treatment promotes osteogenic differentiation of hBMSCS. Biomaterials 86, 11–20 (2016).
Lee, J. S. & Murphy, W. L. Functionalizing calcium phosphate biomaterials with antibacterial silver particles. Adv. Mater. 25, 1173–1179 (2013).
Shimizu, M. et al. Carbon nanotubes induce bone calcification by bidirectional interaction with osteoblasts. Adv. Mater. 24, 2176–2185 (2012).
Nardecchia, S. et al. Osteoconductive performance of carbon nanotube scaffolds homogeneously mineralized by flow-through electrodeposition. Adv. Funct. Mater. 22, 4411–4420 (2012).
Nayak, T. R. et al. Graphene for controlled and accelerated osteogenic differentiation of human mesenchymal stem cells. ACS Nano 5, 4670–4678 (2011).
Lee, W. C. et al. Origin of enhanced stem cell growth and differentiation on graphene and graphene oxide. ACS Nano 5, 7334–7341 (2011).
Li, K. H. et al. Biomimetic ultralight, highly porous, shape-adjustable, and biocompatible 3D graphene minerals via incorporation of self-assembled peptide nanosheets. Adv. Funct. Mater. 28, 1801056 (2018).
Ma, H. S. et al. A bifunctional biomaterial with photothermal effect for tumor therapy and bone regeneration. Adv. Funct. Mater. 26, 1197–1208 (2016).
Arnold, A. M., Holt, B. D., Daneshmandi, L., Laurencin, C. T. & Sydlik, S. A. Phosphate graphene as an intrinsically osteoinductive scaffold for stem cell-driven bone regeneration. Proc. Natl Acad. Sci. USA 116, 4855–4860 (2019). These researchers generated graphene oxide nanosheets functionalized with polyphosphates, which resulted in graphene-based materials capable of releasing osteoinductive phosphate and calcium ions, and, thereby, promoting the in vivo formation of mineralized matrix.
Wang, Y. Q. et al. Bioinspired extracellular vesicles embedded with black phosphorus for molecular recognition-guided biomineralization. Nat. Commun. 10, 2829 (2019).
Yang, B. W. et al. 2D-black-phosphorus-reinforced 3D-printed scaffolds: a stepwise countermeasure for osteosarcoma. Adv. Mater. 30, 1705611 (2018).
Wang, X. Z. et al. Near-infrared light-triggered drug delivery system based on black phosphorus for in vivo bone regeneration. Biomaterials 179, 164–174 (2018).
Laurenti, M. et al. Two-dimensional magnesium phosphate nanosheets form highly thixotropic gels that up-regulate bone formation. Nano Lett. 16, 4779–4787 (2016).
Yoo, S. C., Park, Y. K., Park, C., Ryu, H. & Hong, S. H. Biomimetic artificial nacre: boron nitride nanosheets/gelatin nanocomposites for biomedical applications. Adv. Funct. Mater. 28, 1805948 (2018).
Tiwari, J. N. et al. Accelerated bone regeneration by two-photon photoactivated carbon nitride nanosheets. ACS Nano 11, 742–751 (2017).
Ma, C. Y. et al. Citrate-based materials fuel human stem cells by metabonegenic regulation. Proc. Natl Acad. Sci. USA 115, E11741–E11750 (2018).
Du, Y. Y. et al. Selective laser sintering scaffold with hierarchical architecture and gradient composition for osteochondral repair in rabbits. Biomaterials 137, 37–48 (2017).
Moreau, D., Chauvet, C., Etienne, F., Rannou, F. P. & Corte, L. Hydrogel films and coatings by swelling-induced gelation. Proc. Natl Acad. Sci. USA 113, 13295–13300 (2016).
Lai, Y. X. et al. Osteogenic magnesium incorporated into PLGA/TCP porous scaffold by 3D printing for repairing challenging bone defect. Biomaterials 197, 207–219 (2019).
Zhai, X. Y. et al. 3D-bioprinted osteoblast-laden nanocomposite hydrogel constructs with induced microenvironments promote cell viability, differentiation, and osteogenesis both in vitro and in vivo. Adv. Sci. 5, 1700550 (2018).
Basu, S. et al. Harnessing the noncovalent interactions of DNA backbone with 2D silicate nanodisks to fabricate injectable therapeutic hydrogels. ACS Nano 12, 9866–9880 (2018).
Yun, H. M. et al. Magnetic nanocomposite scaffolds combined with static magnetic field in the stimulation of osteoblastic differentiation and bone formation. Biomaterials 85, 88–98 (2016).
Liu, Y. et al. Thermodynamically controlled self-assembly of hierarchically staggered architecture as an osteoinductive alternative to bone autografts. Adv. Funct. Mater. 29, 1806445 (2019).
Sun, J. L. et al. Intrafibrillar silicified collagen scaffold modulates monocyte to promote cell homing, angiogenesis and bone regeneration. Biomaterials 113, 203–216 (2017).
Zhang, J. et al. Ionic colloidal molding as a biomimetic scaffolding strategy for uniform bone tissue regeneration. Adv. Mater. 29, 1605546 (2017).
Canadas, R. F. et al. Biochemical gradients to generate 3D heterotypic-like tissues with isotropic and anisotropic architectures. Adv. Funct. Mater. 28, 1804148 (2018).
Goldberg, O., Greenfeld, I. & Wagner, H. D. Composite reinforcement by magnetic control of fiber density and orientation. ACS Appl. Mater. Interfaces 10, 16802–16811 (2018).
Fu, Q., Saiz, E., Rahaman, M. N. & Tomsia, A. P. Toward strong and tough glass and ceramic scaffolds for bone repair. Adv. Funct. Mater. 23, 5461–5476 (2013).
Zhu, Y. et al. Protein corona of magnetic hydroxyapatite scaffold improves cell proliferation via activation of mitogen-activated protein kinase signaling pathway. ACS Nano 11, 3690–3704 (2017).
Martin-Moldes, Z. et al. Intracellular pathways involved in bone regeneration triggered by recombinant silk-silica chimeras. Adv. Funct. Mater. 28, 1702570 (2018).
Tolba, E. et al. In situ polyphosphate nanoparticle formation in hybrid poly(vinyl alcohol)/karaya gum hydrogels: a porous scaffold inducing infiltration of mesenchymal stem cells. Adv. Sci. 6, 1801452 (2019).
Zinger, A. et al. Proteolytic nanoparticles replace a surgical blade by controllably remodeling the oral connective tissue. ACS Nano 12, 1482–1490 (2018).
Kang, M. S. et al. Nanocements produced from mesoporous bioactive glass nanoparticles. Biomaterials 162, 183–199 (2018).
Wang, Y. C. et al. Fracture-targeted delivery of β-catenin agonists via peptide-functionalized nanoparticles augments fracture healing. ACS Nano 11, 9445–9458 (2017).
Geuli, O., Metoki, N., Eliaz, N. & Mandler, D. Electrochemically driven hydroxyapatite nanoparticles coating of medical implants. Adv. Funct. Mater. 26, 8003–8010 (2016).
Zheng, C. P. et al. Functional selenium nanoparticles enhanced stem cell osteoblastic differentiation through BMP signaling pathways. Adv. Funct. Mater. 24, 6872–6883 (2014).
Yu, X. H., Khalil, A., Dang, P. N., Alsberg, E. & Murphy, W. L. Multilayered inorganic microparticles for tunable dual growth factor delivery. Adv. Funct. Mater. 24, 3082–3093 (2014).
Cheng, G. et al. Controlled co-delivery of growth factors through layer-by-layer assembly of core-shell nanofibers for improving bone regeneration. ACS Nano 13, 6372–6382 (2019).
Naskar, D. et al. Dual growth factor loaded nonmulberry silk fibroin/carbon nanofiber composite 3D scaffolds for in vitro and in vivo bone regeneration. Biomaterials 136, 67–85 (2017).
Newcomb, C. J. et al. Supramolecular nanofibers enhance growth factor signaling by increasing lipid raft mobility. Nano Lett. 16, 3042–3050 (2016).
Gazquez, G. C. et al. Flexible yttrium-stabilized zirconia nanofibers offer bioactive cues for osteogenic differentiation of human mesenchymal stromal cells. ACS Nano 10, 5789–5799 (2016).
Xue, J. J. et al. Electrospun microfiber membranes embedded with drug-loaded clay nanotubes for sustained antimicrobial protection. ACS Nano 9, 1600–1612 (2015).
Li, L. et al. Controlled dual delivery of BMP-2 and dexamethasone by nanoparticle-embedded electrospun nanofibers for the efficient repair of critical-sized rat calvarial defect. Biomaterials 37, 218–229 (2015).
Cheng, Z. A. et al. Nanoscale coatings for ultralow dose BMP-2-driven regeneration of critical-sized bone defects. Adv. Sci. 6, 1800361 (2019).
Min, J. H. et al. Designer dual therapy nanolayered implant coatings eradicate biofilms and accelerate bone tissue repair. ACS Nano 10, 4441–4450 (2016).
Machillot, P. et al. Automated buildup of biomimetic films in cell culture microplates for high-throughput screening of cellular behaviors. Adv. Mater. 30, 1801097 (2018).
Ha, Y. et al. Phase-transited lysozyme as a universal route to bioactive hydroxyapatite crystalline film. Adv. Funct. Mater. 28, 1704476 (2018).
Jordahl, J. H. et al. 3D jet writing: functional microtissues based on tessellated scaffold architectures. Adv. Mater. 30, 1707196 (2018).
Gao, F. et al. Direct 3D printing of high strength biohybrid gradient hydrogel scaffolds for efficient repair of osteochondral defect. Adv. Funct. Mater. 28, 1706644 (2018).
Chisca, S., Musteata, V.-E., Sougrat, R., Behzad, A. R. & Nunes, S. P. Artificial 3D hierarchical and isotropic porous polymeric materials. Sci. Adv. 4, eaat0713 (2018).
Zhang, W. J. et al. 3D-printed scaffolds with synergistic effect of hollow-pipe structure and bioactive ions for vascularized bone regeneration. Biomaterials 135, 85–95 (2017).
Deng, C. J. et al. 3D printing of bilineage constructive biomaterials for bone and cartilage regeneration. Adv. Funct. Mater. 27, 1703117 (2017).
Pati, F. et al. Ornamenting 3D printed scaffolds with cell-laid extracellular matrix for bone tissue regeneration. Biomaterials 37, 230–241 (2015).
Bose, S., Vahabzadeh, S. & Bandyopadhyay, A. Bone tissue engineering using 3D printing. Mater. Today 16, 496–504 (2013).
Chen, Y. et al. A biocompatible thermoset polymer binder for direct ink writing of porous titanium scaffolds for bone tissue engineering. Mater. Sci. Eng. C 95, 160–165 (2019).
Kolken, H. M. A. et al. Rationally designed meta-implants: a combination of auxetic and conventional meta-biomaterials. Mater. Horiz. 5, 28–35 (2018).
Farahani, R. D., Dube, M. & Therriault, D. Three-dimensional printing of multifunctional nanocomposites: manufacturing techniques and applications. Adv. Mater. 28, 5794–5821 (2016).
Gremare, A. et al. Characterization of printed PLA scaffolds for bone tissue engineering. J. Biomed. Mater. Res. A 106, 887–894 (2018).
Guvendiren, M., Molde, J., Soares, R. M. & Kohn, J. Designing biomaterials for 3D printing. ACS Biomater. Sci. Eng. 2, 1679–1693 (2016).
Korpela, J. et al. Biodegradable and bioactive porous scaffold structures prepared using fused deposition modeling. J. Biomed. Mater. Res. B Appl. Biomater. 101, 610–619 (2013).
Franco, J., Hunger, P., Launey, M. E., Tomsia, A. P. & Saiz, E. Direct write assembly of calcium phosphate scaffolds using a water-based hydrogel. Acta Biomater. 6, 218–228 (2010).
Peng, E., Zhang, D. & Ding, J. Ceramic robocasting: recent achievements, potential, and future developments. Adv. Mater. 30, e1802404 (2018).
Placone, J. K. & Engler, A. J. Recent advances in extrusion-based 3D printing for biomedical applications. Adv. Healthc. Mater. 7, e1701161 (2018).
Hinton, T. J. et al. Three-dimensional printing of complex biological structures by freeform reversible embedding of suspended hydrogels. Sci. Adv. 1, e1500758 (2015).
Surjadi, J. U. et al. Mechanical metamaterials and their engineering applications. Adv. Eng. Mater. 21, 1800864 (2019).
Rajasekharan, A. K., Bordes, R., Sandstrom, C., Ekh, M. & Andersson, M. Hierarchical and heterogeneous bioinspired composites — merging molecular self-assembly with additive manufacturing. Small 13, 1700550 (2017).
Liu, W. et al. Rapid continuous multimaterial extrusion bioprinting. Adv. Mater. 29, 1604630 (2017).
Diaz-Gomez, L. et al. Multimaterial segmented fiber printing for gradient tissue engineering. Tissue Eng. C 25, 12–24 (2019).
Diaz-Gomez, L., Kontoyiannis, P. D., Melchiorri, A. J. & Mikos, A. G. Three-dimensional printing of tissue engineering scaffolds with horizontal pore and composition gradients. Tissue Eng. C 25, 411–420 (2019).
Costantini, M. et al. 3D-printing of functionally graded porous materials using on-demand reconfigurable microfluidics. Angew. Chem. Int. Ed. 58, 7620–7625 (2019).
Raman, R. et al. High-resolution projection microstereolithography for patterning of neovasculature. Adv. Healthc. Mater. 5, 610–619 (2016).
Grigoryan, B. et al. Multivascular networks and functional intravascular topologies within biocompatible hydrogels. Science 364, 458–464 (2019).
Bernal, P. N. et al. Volumetric bioprinting of complex living-tissue constructs within seconds. Adv. Mater. 31, e1904209 (2019).
Yavari, S. A. et al. Bone regeneration performance of surface-treated porous titanium. Biomaterials 35, 6172–6181 (2014).
Kamboj, N., Aghayan, M., Rodrigo-Vazquez, C. S., Rodríguez, M. A. & Hussainova, I. Novel silicon-wollastonite based scaffolds for bone tissue engineering produced by selective laser melting. Ceram. Int. 45, 24691–24701 (2019).
Brunello, G. et al. Powder-based 3D printing for bone tissue engineering. Biotechnol. Adv. 34, 740–753 (2016).
Duan, B. & Wang, M. Selective laser sintering and its application in biomedical engineering. MRS Bull. 36, 998–1005 (2011).
Marino, A. et al. The osteoprint: a bioinspired two-photon polymerized 3-D structure for the enhancement of bone-like cell differentiation. Acta Biomater. 10, 4304–4313 (2014).
Cui, H. et al. Hierarchical fabrication of engineered vascularized bone biphasic constructs via dual 3D bioprinting: integrating regional bioactive factors into architectural design. Adv. Healthc. Mater. 5, 2174–2181 (2016).
Li, T. et al. 3D printing of hot dog-like biomaterials with hierarchical architecture and distinct bioactivity. Adv. Sci. 6, 1901146 (2019).
Lui, Y. S. et al. 4D printing and stimuli-responsive materials in biomedical aspects. Acta Biomater. 92, 19–36 (2019).
Kirillova, A., Maxson, R., Stoychev, G., Gomillion, C. T. & Ionov, L. 4D biofabrication using shape-morphing hydrogels. Adv. Mater. 29, 1703443 (2017).
Jiang, T., Carbone, E. J., Lo, K. W. H. & Laurencin, C. T. Electrospinning of polymer nanofibers for tissue regeneration. Prog. Polym. Sci. 46, 1–24 (2015).
Keller, L. et al. Preclinical safety study of a combined therapeutic bone wound dressing for osteoarticular regeneration. Nat. Commun. 10, 2156 (2019).
Xue, J. J. et al. Drug loaded homogeneous electrospun PCL/gelatin hybrid nanofiber structures for anti-infective tissue regeneration membranes. Biomaterials 35, 9395–9405 (2014).
Kishan, A. P. et al. Fabrication of macromolecular gradients in aligned fiber scaffolds using a combination of in-line blending and air-gap electrospinning. Acta Biomater. 56, 118–128 (2017).
Xie, M. J. et al. Electro-assisted bioprinting of low-concentration GelMA microdroplets. Small 15, 1804216 (2019).
Brown, T. D., Dalton, P. D. & Hutmacher, D. W. Melt electrospinning today: an opportune time for an emerging polymer process. Prog. Polym. Sci. 56, 116–166 (2016).
Brown, T. D., Dalton, P. D. & Hutmacher, D. W. Direct writing by way of melt electrospinning. Adv. Mater. 23, 5651–5657 (2011).
Wunner, F. M. et al. Melt electrospinning writing of highly ordered large volume scaffold architectures. Adv. Mater. 30, 1706570 (2018).
Workman, V. L., Tezera, L. B., Elkington, P. T. & Jayasinghe, S. N. Controlled generation of microspheres incorporating extracellular matrix fibrils for three-dimensional cell culture. Adv. Funct. Mater. 24, 2648–2657 (2014).
de Jonge, L. T., Leeuwenburgh, S. C. G., van den Beucken, J. J. J. P., Wolke, J. G. C. & Jansen, J. A. Electrosprayed enzyme coatings as bioinspired alternatives to bioceramic coatings for orthopedic and oral implants. Adv. Funct. Mater. 19, 755–762 (2009).
Song, J. et al. Electrophoretic deposition of chitosan coatings modified with gelatin nanospheres to tune the release of antibiotics. ACS Appl. Mater. Interfaces 8, 13785–13792 (2016).
Avcu, E. et al. Electrophoretic deposition of chitosan-based composite coatings for biomedical applications: a review. Prog. Mater. Sci. 103, 69–108 (2019).
Qassemyar, Q., Assouly, N., Madar, Y., Temam, S. & Kolb, F. Total nasal reconstruction with 3D custom made porous titanium prosthesis and free thoracodorsal artery perforator flap: a case report. Microsurgery 38, 567–571 (2018).
Kieser, D. C. et al. The use of an Ossis custom 3D-printed tri-flanged acetabular implant for major bone loss: minimum 2-year follow-up. HIP Int. 28, 668–674 (2018).
Li, J., Hsu, Y., Luo, E., Khadka, A. & Hu, J. Computer-aided design and manufacturing and rapid prototyped nanoscale hydroxyapatite/polyamide (n-HA/PA) construction for condylar defect caused by mandibular angle ostectomy. Aesthetic Plast. Surg. 35, 636–640 (2011).
Ahn, G., Lee, J. S., Yun, W. S., Shim, J. H. & Lee, U. L. Cleft alveolus reconstruction using a three-dimensional printed bioresorbable scaffold with human bone marrow cells. J. Craniofac. Surg. 29, 1880–1883 (2018).
Walsh, W. R. et al. Does implantation site influence bone ingrowth into 3D-printed porous implants? Spine J. 19, 1885–1898 (2019).
Jacome-Galarza, C. E. et al. Developmental origin, functional maintenance and genetic rescue of osteoclasts. Nature 568, 541–545 (2019).
Diesendruck, C. E. et al. Mechanically triggered heterolytic unzipping of a low-ceiling-temperature polymer. Nat. Chem. 6, 623–628 (2014).
Lin, K. L. et al. Enhanced osteoporotic bone regeneration by strontium-substituted calcium silicate bioactive ceramics. Biomaterials 34, 10028–10042 (2013).
Hayder, M. et al. A phosphorus-based dendrimer targets inflammation and osteoclastogenesis in experimental arthritis. Sci. Transl. Med. 3, 81ra35 (2011).
Jin, X. et al. Self-adaptive antibacterial porous implants with sustainable responses for infected bone defect therapy. Adv. Funct. Mater. 29, 1807915 (2019).
Li, J. et al. Balancing bacteria–osteoblast competition through selective physical puncture and biofunctionalization of ZnO/polydopamine/arginine-glycine-aspartic acid-cysteine nanorods. ACS Nano 11, 11250–11263 (2017).
Zhao, H. et al. Antitumor effect by hydroxyapatite nanospheres: activation of mitochondria dependent apoptosis and negative regulation of phosphatidylinositol-3-kinase/protein kinase B pathway. ACS Nano 12, 7838–7854 (2018).
James, A. W. et al. A review of the clinical side effects of bone morphogenetic protein-2. Tissue Eng. B 22, 284–297 (2016).
Chaudhuri, O. et al. Hydrogels with tunable stress relaxation regulate stem cell fate and activity. Nat. Mater. 15, 326–334 (2016). These researchers developed alginate hydrogels with differing stress-relaxation properties but similar elasticity. They showed that hydrogel stress-relaxation behaviour regulates osteogenic differentiation of encapsulated MSCs.
Watson, B. M., Kasper, F. K., Engel, P. S. & Mikos, A. G. Synthesis and characterization of injectable, biodegradable, phosphate-containing, chemically cross-linkable, thermoresponsive macromers for bone tissue engineering. Biomacromolecules 15, 1788–1796 (2014).
Watson, B. M. et al. Biodegradable, phosphate-containing, dual-gelling macromers for cellular delivery in bone tissue engineering. Biomaterials 67, 286–296 (2015).
Badeau, B. A., Comerford, M. P., Arakawa, C. K., Shadish, J. A. & DeForest, C. A. Engineered modular biomaterial logic gates for environmentally triggered therapeutic delivery. Nat. Chem. 10, 251–258 (2018).
Liu, W. et al. Zinc-modified sulfonated polyetheretherketone surface with immunomodulatory function for guiding cell fate and bone regeneration. Adv. Sci. 5, 1800749 (2018).
Kim, C. S. et al. A specific groove pattern can effectively induce osteoblast differentiation. Adv. Funct. Mater. 27, 1703569 (2017).
Chrzanowski, W. et al. Nano-bio-chemical braille for cells: the regulation of stem cell responses using bi-functional surfaces. Adv. Funct. Mater. 25, 193–205 (2015).
Alakpa, E. V. et al. Nacre topography produces higher crystallinity in bone than chemically induced osteogenesis. ACS Nano 11, 6717–6727 (2017).
Bencherif, S. A. et al. Injectable preformed scaffolds with shape-memory properties. Proc. Natl Acad. Sci. USA 109, 19590–19595 (2012).
Gorgin Karaji, Z. et al. Additively manufactured and surface biofunctionalized porous nitinol. ACS Appl. Mater. Interfaces 9, 1293–1304 (2017).
Zadpoor, A. A. Meta-biomaterials. Biomater. Sci. 8, 18–38 (2019).
Han, H. Y. et al. Silk biomaterials with vascularization capacity. Adv. Funct. Mater. 26, 421–432 (2016).
Cai, L., Chen, J. H., Rondinone, A. J. & Wang, S. F. Injectable and biodegradable nanohybrid polymers with simultaneously enhanced stiffness and toughness for bone repair. Adv. Funct. Mater. 22, 3181–3190 (2012).
Shen, X. F. et al. Sequential and sustained release of SDF-1 and BMP-2 from silk fibroin-nanohydroxyapatite scaffold for the enhancement of bone regeneration. Biomaterials 106, 205–216 (2016).
Quinlan, E. et al. Hypoxia-mimicking bioactive glass/collagen glycosaminoglycan composite scaffolds to enhance angiogenesis and bone repair. Biomaterials 52, 358–366 (2015).
Yang, Y. et al. Influence of cell spreading area on the osteogenic commitment and phenotype maintenance of mesenchymal stem cells. Sci. Rep. 9, 6891 (2019).
Seo, B. B., Koh, J. T. & Song, S. C. Tuning physical properties and BMP-2 release rates of injectable hydrogel systems for an optimal bone regeneration effect. Biomaterials 122, 91–104 (2017).
Dashnyam, K. et al. Promoting angiogenesis with mesoporous microcarriers through a synergistic action of delivered silicon ion and VEGF. Biomaterials 116, 145–157 (2017).
Spiller, K. L. et al. Sequential delivery of immunomodulatory cytokines to facilitate the M1-to-M2 transition of macrophages and enhance vascularization of bone scaffolds. Biomaterials 37, 194–207 (2015).
Hao, J. et al. Multigrowth factor delivery via immobilization of gene therapy vectors. Adv. Mater. 28, 3145–3151 (2016).
Cui, Z. K. et al. Design and characterization of a therapeutic non-phospholipid liposomal nanocarrier with osteoinductive characteristics to promote bone formation. ACS Nano 11, 8055–8063 (2017).
Zeng, H. C. et al. MicroRNA miR-23a cluster promotes osteocyte differentiation by regulating TGF-β signalling in osteoblasts. Nat. Commun. 8, 15000 (2017).
Yang, L., Tsang, K. Y., Tang, H. C., Chan, D. & Cheah, K. S. Hypertrophic chondrocytes can become osteoblasts and osteocytes in endochondral bone formation. Proc. Natl Acad. Sci. USA 111, 12097–12102 (2014).
Wolff, J. The Law of Bone Remodelling (Springer, 1986).
Ruff, C., Holt, B. & Trinkaus, E. Who’s afraid of the big bad Wolff?: “Wolff’s law” and bone functional adaptation. Am. J. Phys. Anthropol. 129, 484–498 (2006).
Shi, M. C. et al. Europium-doped mesoporous silica nanosphere as an immune-modulating osteogenesis/angiogenesis agent. Biomaterials 144, 176–187 (2017).
Dhand, C. et al. Bio-inspired in situ crosslinking and mineralization of electrospun collagen scaffolds for bone tissue engineering. Biomaterials 104, 323–338 (2016).
Damaraju, S. M. et al. Three-dimensional piezoelectric fibrous scaffolds selectively promote mesenchymal stem cell differentiation. Biomaterials 149, 51–62 (2017).
Daly, A. C., Pitacco, P., Nulty, J., Cunniffe, G. M. & Kelly, D. J. 3D printed microchannel networks to direct vascularisation during endochondral bone repair. Biomaterials 162, 34–46 (2018).
Vergroesen, P. P., Kroeze, R. J., Helder, M. N. & Smit, T. H. The use of poly(l-lactide-co-caprolactone) as a scaffold for adipose stem cells in bone tissue engineering: application in a spinal fusion model. Macromol. Biosci. 11, 722–730 (2011).
Boden, S. D. Overview of the biology of lumbar spine fusion and principles for selecting a bone graft substitute. Spine 27, S26–S31 (2002).
Johnson, E. O., Troupis, T. & Soucacos, P. N. Tissue-engineered vascularized bone grafts: basic science and clinical relevance to trauma and reconstructive microsurgery. Microsurgery 31, 176–182 (2011).
Frick, S. L. in Green’s Skeletal Trauma in Children (eds Mencio, G. A. & Swiontkowski, M. F.) 1–15 (Elsevier Saunders, 2015).
Thapa, M. & Pruthi, S. in Pediatric Radiology (eds Reid, J., Lee, E., Paladin, A., Carrico, C. & Davros, W.) 273–277 (Oxford Univ. Press, 2014).
Conith, A. J., Lam, D. T. & Albertson, R. C. Muscle-induced loading as an important source of variation in craniofacial skeletal shape. Genesis 57, e23263 (2019).
Kneser, U., Schaefer, D. J., Polykandriotis, E. & Horch, R. E. Tissue engineering of bone: the reconstructive surgeon’s point of view. J. Cell. Mol. Med. 10, 7–19 (2006).
Nyberg, E. L. et al. 3D-printing technologies for craniofacial rehabilitation, reconstruction, and regeneration. Ann. Biomed. Eng. 45, 45–57 (2017).
Hollister, S. J. et al. Design control for clinical translation of 3D printed modular scaffolds. Ann. Biomed. Eng. 43, 774–786 (2015).
O’Donnell, B. T., Ives, C. J., Mohiuddin, O. A. & Bunnell, B. A. Beyond the present constraints that prevent a wide spread of tissue engineering and regenerative medicine approaches. Front. Bioeng. Biotechnol. 7, 95 (2019).
Webber, M. J., Khan, O. F., Sydlik, S. A., Tang, B. C. & Langer, R. A perspective on the clinical translation of scaffolds for tissue engineering. Ann. Biomed. Eng. 43, 641–656 (2015).
Morrison, R. J. et al. Regulatory considerations in the design and manufacturing of implantable 3D-printed medical devices. Clin. Transl. Sci. 8, 594–600 (2015).
Lee, M. H. et al. Considerations for tissue-engineered and regenerative medicine product development prior to clinical trials in the United States. Tissue Eng. B 16, 41–54 (2010).
Kang, H. M. et al. Remote control of intracellular calcium using upconversion nanotransducers regulates stem cell differentiation in vivo. Adv. Funct. Mater. 28, 1802642 (2018).
Kallai, I. et al. Microcomputed tomography-based structural analysis of various bone tissue regeneration models. Nat. Protoc. 6, 105–110 (2011).
Shah, S. R. et al. A composite critical-size rabbit mandibular defect for evaluation of craniofacial tissue regeneration. Nat. Protoc. 11, 1989–2009 (2016).
Seeherman, H. J. et al. A BMP/activin A chimera is superior to native BMPs and induces bone repair in nonhuman primates when delivered in a composite matrix. Sci. Transl. Med. 11, eaar4953 (2019).
Bourgine, P. E. et al. Engineered extracellular matrices as biomaterials of tunable composition and function. Adv. Funct. Mater. 27, 1605486 (2017).
Acknowledgements
The authors’ work towards the development of materials for bone-tissue-engineering applications has been supported by the US National Institutes of Health grants P41 EB023833, R01 AR068073 and R01 CA180279 (to A.G.M.). G.L.K. is supported by the Robert and Janice McNair Foundation MD/PhD Student Scholar Program. M.D. is supported by a Rubicon postdoctoral fellowship from the Netherlands Organisation for Scientific Research (project no. 019.182EN.004).
Author information
Authors and Affiliations
Contributions
G.L.K. and M.D. researched the literature and wrote the article. G.L.K., M.D. and A.G.M. discussed, reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koons, G.L., Diba, M. & Mikos, A.G. Materials design for bone-tissue engineering. Nat Rev Mater 5, 584–603 (2020). https://doi.org/10.1038/s41578-020-0204-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41578-020-0204-2
This article is cited by
-
Cartilage-like protein-polysaccharide hybrid hydrogel for enhancing chondrogenic differentiation of bone marrow mesenchymal stem cells
Collagen and Leather (2024)
-
Utilizing bioprinting to engineer spatially organized tissues from the bottom-up
Stem Cell Research & Therapy (2024)
-
Gradient matters via filament diameter-adjustable 3D printing
Nature Communications (2024)
-
Ultrasound-activated piezo-hot carriers trigger tandem catalysis coordinating cuproptosis-like bacterial death against implant infections
Nature Communications (2024)
-
The Synergetic Effect of 3D Printing and Electrospinning Techniques in the Fabrication of Bone Scaffolds
Annals of Biomedical Engineering (2024)