Abstract
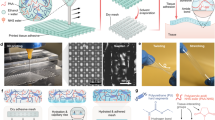
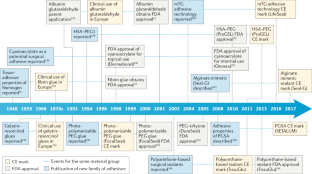
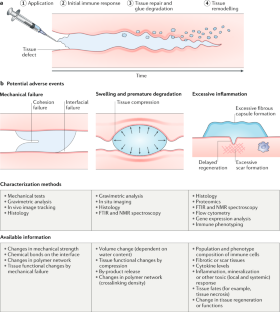
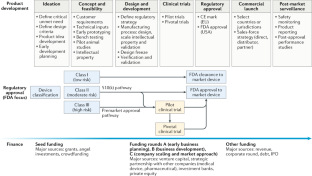
For the past few decades, tissue sealants and adhesives have been developed as an alternative to sutures and staples to close and seal wounds or incisions. These materials are advantageous because of their ease of use, short application time and minimal tissue damage, making them suitable for minimally invasive procedures. However, there is a large gap between the amount of research into tissue adhesives and the number of products available. To bridge this gap, there is a need to better understand the challenges to clinical translation of tissue adhesives. In particular, adhesive design must be informed by a deep understanding of the target tissue’s surface characteristics and environment, which vary considerably among tissue types. Moreover, understanding and monitoring the long-term performance of a material post-implantation is crucial; this includes monitoring the chemical and physical properties of the implanted adhesives over time, tissue responses and the resultant changes in adhesion and cohesion. In addition, early-stage consideration of the unmet clinical need and the regulatory and development paths could lower the barriers in the development cost and effort, facilitating clinical translation. In this Review, we identify challenges in the development of tissue adhesives and provide design criteria to translate tissue-adhesive technologies into clinical practice.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Market Research Engine. Global wound closure products market expected to be worth US $ 15 billion by 2022 (Market Research Engine, 2018).
Artzi, N. Sticking with the pattern for a safer glue. Sci. Transl Med. 5, 205ec161 (2013).
George, W. D. Suturing or stapling in gastrointestinal surgery: a prospective randomized study. Br. J. Surg. 78, 337–341 (1991).
Slieker, J. C., Daams, F., Mulder, I. M., Jeekel, J. & Lange, J. F. Systematic review of the technique of colorectal anastomosis. JAMA Surg. 148, 190–201 (2013).
Edmiston, C. E. et al. Microbiology of explanted suture segments from infected and noninfected surgical patients. J. Clin. Microbiol. 51, 417–421 (2013).
Owens, C. D. & Stoessel, K. Surgical site infections: epidemiology, microbiology and prevention. J. Hosp. Infect. 70, 3–10 (2008).
Matossian, C., Makari, S. & Potvin, R. Cataract surgery and methods of wound closure: a review. Clin. Ophthalmol. 9, 921–928 (2015).
Masket, S. et al. Hydrogel sealant versus sutures to prevent fluid egress after cataract surgery. J. Cataract Refract. Surg. 40, 2057–2066 (2014).
Lequaglie, C., Giudice, G., Marasco, R., Morte, A. D. & Gallo, M. Use of a sealant to prevent prolonged air leaks after lung resection: a prospective randomized study. J. Cardiothorac. Surg. 7, 106 (2012).
Lang, N. et al. A blood-resistant surgical glue for minimally invasive repair of vessels and heart defects. Sci. Transl Med. 6, 218ra6 (2014).
Sidle, D. M., Loos, B. M., Ramirez, A. L., Kabaker, S. S. & Maas, C. S. Use of BioGlue surgical adhesive for brow fixation in endoscopic browplasty. Arch. Facial Plast. Surg. 7, 393–397 (2005).
Petersen, B. et al. Tissue adhesives and fibrin glues. Gastrointest. Endosc. 60, 327–333 (2004).
Grand View Research. Surgical sealants and adhesives market analysis by type (natural or biological adhesives & sealants, synthetic & semi synthetic adhesives), by application, by region, and segment forecasts, 2018–2025 (Grand View Research, 2017).
Cronkite, E. P., Lozner, E. L. & Deaver, J. M. Use of thrombin and fibrinogen in skin grafting: preliminary report. JAMA 124, 976–978 (1944).
Young, J. Z. & Medawar, P. B. Fibrin suture of peripheral nerves: measurement of the rate of regeneration. Lancet 236, 126–128 (1940).
Spotnitz, W. D. Fibrin sealant: past, present, and future: a brief review. World J. Surg. 34, 632–634 (2010).
Spotnitz, W. D. Fibrin sealant: the only approved hemostat, sealant, and adhesive – a laboratory and clinical perspective. ISRN Surg. 2014, 203943 (2014).
Gundry, S. R., Black, K. & Izutani, H. Sutureless coronary artery bypass with biologic glued anastomoses: preliminary in vivo and in vitro results. J. Thorac. Cardiovasc. Surg. 120, 473–477 (2000).
Chao, H.-H. & Torchiana, D. F. BioGlue: albumin/glutaraldehyde sealant in cardiac surgery. J. Card. Surg. 18, 500–503 (2003).
Singer, A. J., Perry, L. C. & Allen, R. L. Jr In vivo study of wound bursting strength and compliance of topical skin adhesives. Acad. Emerg. Med. 15, 1290–1294 (2008).
Leggat, P. A., Smith, D. R. & Kedjarune, U. Surgical applications of cyanoacrylate adhesives: a review of toxicity. ANZ J. Surg. 77, 209–213 (2007).
Pascual, G. et al. Cytotoxicity of cyanoacrylate-based tissue adhesives and short-term preclinical in vivo biocompatibility in abdominal hernia repair. PLOS ONE 11, e0157920 (2016).
Dumville, J. C. et al. Tissue adhesives for closure of surgical incisions. Cochrane Database Syst. Rev. 28, CD004287 (2014).
Oliva, N. et al. Personalizing biomaterials for precision nanomedicine considering the local tissue microenvironment. Adv. Healthc. Mater. 4, 1584–1599 (2015).
Bhagat, V. & Becker, M. L. Degradable adhesives for surgery and tissue engineering. Biomacromolecules 18, 3009–3039 (2017).
Artzi, N. et al. In vivo and in vitro tracking of erosion in biodegradable materials using non-invasive fluorescence imaging. Nat. Mater. 10, 704–709 (2011).
Oliva, N. et al. Regulation of dendrimer/dextran material performance by altered tissue microenvironment in inflammation and neoplasia. Sci. Transl Med. 7, 272ra11 (2015).
López-Guerra, D. et al. Postoperative bleeding and biliary leak after liver resection: a cohort study between two different fibrin sealant patches. Sci. Rep. 9, 12001 (2019).
Vakalopoulos, K. et al. Mechanical strength and rheological properties of tissue adhesives with regard to colorectal anastomosis: an ex vivo study. Ann. Surg. 261, 323–331 (2015).
Jue, B. & Maurice, D. M. The mechanical properties of the rabbit and human cornea. J. Biomech. 19, 847–853 (1986).
Khanafer, K. et al. Determination of the elastic modulus of ascending thoracic aortic aneurysm at different ranges of pressure using uniaxial tensile testing. J. Thorac. Cardiovasc. Surg. 142, 682–686 (2011).
Park, D. Y. et al. The use of microfluidic spinning fiber as an ophthalmology suture showing the good anastomotic strength control. Sci. Rep. 7, 16264 (2017).
Roy, C. K. et al. Self-adjustable adhesion of polyampholyte hydrogels. Adv. Mater. 27, 7344–7348 (2015).
Li, J. et al. Tough adhesives for diverse wet surfaces. Science 357, 378–381 (2017).
Liu, B. et al. Hydrogen bonds autonomously powered gelatin methacrylate hydrogels with super-elasticity, self-heal and underwater self-adhesion for sutureless skin and stomach surgery and E-skin. Biomaterials 171, 83–96 (2018).
Fan, H., Wang, J., Zhang, Q. & Jin, Z. Tannic acid-based multifunctional hydrogels with facile adjustable adhesion and cohesion contributed by polyphenol supramolecular chemistry. ACS Omega 2, 6668–6676 (2017).
Matsuda, M., Inoue, M. & Taguchi, T. Adhesive properties and biocompatibility of tissue adhesives composed of various hydrophobically modified gelatins and disuccinimidyl tartrate. J. Bioact. Compat. Polym. 27, 481–498 (2012).
Mizuta, R. & Taguchi, T. Enhanced sealing by hydrophobic modification of Alaska pollock-derived gelatin-based surgical sealants for the treatment of pulmonary air leaks. Macromol. Biosci. 17, 1600349 (2017).
Yoshizawa, K. & Taguchi, T. Bonding behavior of hydrophobically modified gelatin films on the intestinal surface. J. Bioact. Compat. Polym. 29, 560–571 (2014).
Matsuda, M., Inoue, M. & Taguchi, T. Enhanced bonding strength of a novel tissue adhesive consisting of cholesteryl group-modified gelatin and disuccinimidyl tartarate. J. Bioact. Compat. Polym. 27, 31–44 (2012).
Michel, R. et al. Interfacial fluid transport is a key to hydrogel bioadhesion. Proc. Natl Acad. Sci. USA 116, 738–743 (2019).
Rogers, A. C., Turley, L. P., Cross, K. S. & McMonagle, M. P. Meta-analysis of the use of surgical sealants for suture-hole bleeding in arterial anastomoses. Br. J. Surg. 103, 1758–1767 (2016).
Murdock, M. H. et al. Cytocompatibility and mechanical properties of surgical sealants for cardiovascular applications. J. Thorac. Cardiovasc. Surg. 157, 176–183 (2019).
Matthews, P. B. et al. Mechanical properties of surgical glues used in aortic root replacement. Ann. Thorac. Surg. 87, 1154–1160 (2009).
Natour, E., Suedkamp, M. & Dapunt, O. E. Assessment of the effect on blood loss and transfusion requirements when adding a polyethylene glycol sealant to the anastomotic closure of aortic procedures: a case–control analysis of 102 patients undergoing Bentall procedures. J. Cardiothorac. Surg. 7, 105 (2012).
Skorpil, J. et al. Effective and rapid sealing of coronary, aortic and atrial suture lines. Interact. Cardiovasc. Thorac. Surg. 20, 720–724 (2015).
Bhamidipati, C. M., Coselli, J. S. & LeMaire, S. A. BioGlue® in 2011: what is its role in cardiac surgery? J. Extra. Corpor. Technol. 44, P6–P12 (2012).
LeMaire, S. A. et al. Nerve and conduction tissue injury caused by contact with BioGlue. J. Surg. Res. 143, 286–293 (2007).
LeMaire, S. A. et al. BioGlue surgical adhesive impairs aortic growth and causes anastomotic strictures. Ann. Thorac. Surg. 73, 1500–1506 (2002).
Pasic, M., Unbehaun, A., Drews, T. & Hetzer, R. Late wound healing problems after use of BioGlue® for apical hemostasis during transapical aortic valve implantation. Interact. Cardiovasc. Thorac. Surg. 13, 532–535 (2011).
Fürst, W. & Banerjee, A. Release of glutaraldehyde from an albumin-glutaraldehyde tissue adhesive causes significant in vitro and in vivo toxicity. Ann. Thorac. Surg. 79, 1522–1528 (2005).
Park, J. S. et al. Risk factors of anastomotic leakage and long-term survival after colorectal surgery. Medicine 95, e2890 (2016).
Phillips, B. Reducing gastrointestinal anastomotic leak rates: review of challenges and solutions. Open Access Surg. 9, 5–14 (2016).
Bae, K.-B., Kim, S.-H., Jung, S.-J. & Hong, K.-H. Cyanoacrylate for colonic anastomosis; is it safe? Int. J. Colorectal Dis. 25, 601–606 (2010).
Vuocolo, T. et al. A highly elastic and adhesive gelatin tissue sealant for gastrointestinal surgery and colon anastomosis. J. Gastrointest. Surg. 16, 744–752 (2012).
Li, Y.-W. et al. Very early colorectal anastomotic leakage within 5 post-operative days: a more severe subtype needs relaparatomy. Sci. Rep. 7, 39936 (2017).
Hyman, N., Manchester, T. L., Osler, T., Burns, B. & Cataldo, P. A. Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann. Surg. 245, 254–258 (2007).
Silecchia, G. et al. The use of fibrin sealant to prevent major complications following laparoscopic gastric bypass: results of a multicenter, randomized trial. Surg. Endosc. 22, 2492–2497 (2008).
Slieker, J. C., Vakalopoulos, K. A., Komen, N. A., Jeekel, J. & Lange, J. F. Prevention of leakage by sealing colon anastomosis: experimental study in a mouse model. J. Surg. Res. 184, 819–824 (2013).
Trotter, J. et al. The use of a novel adhesive tissue patch as an aid to anastomotic healing. Ann. R. Coll. Surg. Engl. 100, 230–234 (2018).
Vakalopoulos, K. A. et al. Tissue adhesives in gastrointestinal anastomosis: a systematic review. J. Surg. Res. 180, 290–300 (2013).
Nordentoft, T., Pommergaard, H. C., Rosenberg, J. & Achiam, M. P. Fibrin glue does not improve healing of gastrointestinal anastomoses: a systematic review. Eur. Surg. Res. 54, 1–13 (2014).
Goulder, F. Bowel anastomoses: the theory, the practice and the evidence base. World J. Gastrointest. Surg. 4, 208–213 (2012).
Urbanavičius, L., Pattyn, P., Van de Putte, D. & Venskutonis, D. How to assess intestinal viability during surgery: a review of techniques. World J. Gastrointest. Surg. 3, 59–69 (2011).
Shogan, B. D. et al. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci. Transl Med. 7, 286ra68 (2015).
Shogan, B. D. et al. Intestinal anastomotic injury alters spatially defined microbiome composition and function. Microbiome. 2, 35 (2014).
van Praagh, J. B. et al. Intestinal microbiota and anastomotic leakage of stapled colorectal anastomoses: a pilot study. Surg. Endosc. 30, 2259–2265 (2016).
Shakhsheer, B. et al. Morphine promotes colonization of anastomotic tissues with collagenase-producing Enterococcus faecalis and causes leak. J. Gastrointest. Surg. 20, 1744–1751 (2016).
Gaines, S., Shao, C., Hyman, N. & Alverdy, J. C. Gut microbiome influences on anastomotic leak and recurrence rates following colorectal cancer surgery. Br. J. Surg. 105, e131–e141 (2018).
Pommergaard, H. C., Rosenberg, J., Schumacher-Petersen, C. & Achiam, M. P. Choosing the best animal species to mimic clinical colon anastomotic leakage in humans: a qualitative systematic review. Eur. Surg. Res. 47, 173–181 (2011).
Nagel, S. J. et al. Spinal dura mater: biophysical characteristics relevant to medical device development. J. Med. Eng. Technol. 42, 128–139 (2018).
Protasoni, M. et al. The collagenic architecture of human dura mater. J. Neurosurg. 114, 1723–1730 (2011).
Hutter, G., von Felten, S., Sailer, M. H., Schulz, M. & Mariani, L. Risk factors for postoperative CSF leakage after elective craniotomy and the efficacy of fleece-bound tissue sealing against dural suturing alone: a randomized controlled trial. J. Neurosurg. 121, 735–744 (2014).
Esposito, F. et al. Fibrin sealants in dura sealing: a systematic literature review. PLOS ONE 12, e0175619 (2016).
Yu, F. et al. Current developments in dural repair: a focused review on new methods and materials. Front. Biosci. 18, 1335–1343 (2013).
Narotam, P. K., Qiao, F. & Nathoo, N. Collagen matrix duraplasty for posterior fossa surgery: evaluation of surgical technique in 52 adult patients. J. Neurosurg. 111, 380–386 (2009).
Spotnitz, W. D. in Musculoskeletal Tissue Regeneration (ed. Pietrzak, W. S.) 531–546 (Humana, 2008).
Kim, K. D. et al. DuraSeal Exact is a safe adjunctive treatment for durotomy in spine: postapproval study. Global Spine J. 9, 272–278 (2018).
Kinaci, A. et al. Effectiveness of dural sealants in prevention of CSF leakage after craniotomy: a systematic review. World Neurosurg. 118, 368–376 (2018).
Van Doormaal, T. et al. Usefulness of sealants for dural closure: evaluation in an in vitro model. Oper. Neurosurg. 15, 425–432 (2017).
Lee, S.-H., Park, C.-W., Lee, S.-G. & Kim, W.-K. Postoperative cervical cord compression induced by hydrogel dural sealant (DuraSeal®). Korean J. Spine 10, 44–46 (2013).
Smyth, M. D. Hydrogel-induced cervicomedullary compression after posterior fossa decompression for Chiari malformation. J. Neurosurg. Pediatr. 106, 302–304 (2007).
Chenault, H. K. et al. Sealing and healing of clear corneal incisions with an improved dextran aldehyde-PEG amine tissue adhesive. Curr. Eye Res. 36, 997–1004 (2011).
Park, H. C., Champakalakshmi, R., Panengad, P. P., Raghunath, M. & Mehta, J. S. Tissue adhesives in ocular surgery. Expert. Rev. Ophthalmol. 6, 631–655 (2011).
Baker-Schena, L. Ocular sealants: one new option, but still room for innovation (EyeNet Magazine, 2014).
Refojo, M. F. Current status of biomaterials in ophthalmology. Surv. Ophthalmol. 26, 257–265 (1982).
Sharma, A. et al. Fibrin glue versus N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology 110, 291–298 (2003).
Kasetsuwan, N. et al. Efficacy and safety of ethyl-2-cyanoacrylate adhesives for corneal gluing. Asian Biomed. 7, 437–441 (2013).
Bhatia, S. S. Ocular surface sealants and adhesives. Ocul. Surf. 4, 146–154 (2006).
Guhan, S. et al. Surgical adhesives in ophthalmology: history and current trends. Br. J. Ophthalmol. 102, 1328–1335 (2018).
Nallasamy, N., Grove, K. E., Legault, G. L., Daluvoy, M. B. & Kim, T. Hydrogel ocular sealant for clear corneal incisions in cataract surgery. J. Cataract Refract. Surg. 43, 1010–1014 (2017).
US Food and Drug Administration. ReSure® sealant. Summary of safety and effectiveness data (FDA, 2013).
Wain, J. C. et al. Trial of a novel synthetic sealant in preventing air leaks after lung resection. Ann. Thorac. Surg. 71, 1623–1629 (2001).
Okereke, I., Murthy, S. C., Alster, J. M., Blackstone, E. H. & Rice, T. W. Characterization and importance of air leak after lobectomy. Ann. Thorac. Surg. 79, 1167–1173 (2005).
Malapert, G., Hanna, H. A., Pages, P. B. & Bernard, A. Surgical sealant for the prevention of prolonged air leak after lung resection: meta-analysis. Ann. Thorac. Surg. 90, 1779–1785 (2010).
Annabi, N. et al. Engineering a highly elastic human protein-based sealant for surgical applications. Sci. Transl Med. 9, eaai7466 (2017).
Fenn, S. L., Charron, P. N. & Oldinski, R. A. Anticancer therapeutic alginate-based tissue sealants for lung repair. ACS Appl. Mater. Interfaces 9, 23409–23419 (2017).
Santini, M. et al. Use of an electrothermal bipolar tissue sealing system in lung surgery. Eur. J. Cardiothorac. Surg. 29, 226–230 (2006).
US Food and Drug Administration. Premarket approval (PMA) for ProGEL pleural air leak sealant (FDA, 2010).
Belda-Sanchís, J., Serra-Mitjans, M., Iglesias Sentis, M. & Rami, R. Surgical sealant for preventing air leaks after pulmonary resections in patients with lung cancer. Cochrane Database Syst. Rev. 20, CD003051 (2010).
ASTM International. ASTM F2392-04(2015). Standard test method for burst strength of surgical sealants (ASTM, 2015).
ASTM International. ASTM F2458-05(2015), standard test method for wound closure Strength of tissue adhesives and sealants (ASTM, 2015).
Ghobril, C. & Grinstaff, M. W. The chemistry and engineering of polymeric hydrogel adhesives for wound closure: a tutorial. Chem. Soc. Rev. 44, 1820–1835 (2015).
Annabi, N. et al. Surgical materials: current challenges and nano-enabled solutions. Nano Today 9, 574–589 (2014).
Annabi, N., Yue, K., Tamayol, A. & Khademhosseini, A. Elastic sealants for surgical applications. Eur. J. Pharm. Biopharm. 95, 27–39 (2015).
Duarte, A. P., Coelho, J. F., Bordado, J. C., Cidade, M. T. & Gil, M. H. Surgical adhesives: systematic review of the main types and development forecast. Prog. Polym. Sci. 37, 1031–1050 (2012).
Zhu, W., Chuah, Y. J. & Wang, D.-A. Bioadhesives for internal medical applications: a review. Acta Biomater. 74, 1–16 (2018).
Nair, L. S. & Laurencin, C. T. Biodegradable polymers as biomaterials. Prog. Polym. Sci. 32, 762–798 (2007).
Khanlari, S. & Dubé, M. A. Bioadhesives: a review. Macromol. React. Eng. 7, 573–587 (2013).
Marin, E., Briceño, M. I. & Caballero-George, C. Critical evaluation of biodegradable polymers used in nanodrugs. Int. J. Nanomed. 8, 3071–3091 (2013).
Caliceti, P. & Veronese, F. M. Pharmacokinetic and biodistribution properties of poly(ethylene glycol)–protein conjugates. Adv. Drug Deliv. Rev. 55, 1261–1277 (2003).
Kean, T. & Thanou, M. Biodegradation, biodistribution and toxicity of chitosan. Adv. Drug Deliv. Rev. 62, 3–11 (2010).
Yamaoka, T., Tabata, Y. & Ikada, Y. Distribution and tissue uptake of poly(ethylene glycol) with different molecular weights after intravenous administration to mice. J. Pharm. Sci. 83, 601–606 (1994).
Menovsky, T. et al. Massive swelling of Surgicel® Fibrillar™ hemostat after spinal surgery. case report and a review of the literature. Minim. Invasive Neurosurg. 54, 257–259 (2011).
Shazly, T. M. et al. Augmentation of postswelling surgical sealant potential of adhesive hydrogels. J. Biomed. Mater. Res. A 95, 1159–1169 (2010).
Buchowski, J., Good, C., Lenke, L. & Bridwell, K. Epidural spinal cord compression with neurologic deficit associated with intrapedicular application of FloSeal during pedicle screw insertion. Spine J. 8, 120S–121S (2008).
Pinkas, O. & Zilberman, M. Novel gelatin–alginate surgical sealants loaded with hemostatic agents. Int. J. Polym. Mater. 66, 378–387 (2017).
Unterman, S. et al. Hydrogel nanocomposites with independently tunable rheology and mechanics. ACS Nano 11, 2598–2610 (2017).
Barrett, D. G., Bushnell, G. G. & Messersmith, P. B. Mechanically robust, negative-swelling, mussel-inspired tissue adhesives. Adv. Healthc. Mater. 2, 745–755 (2013).
Cho, E., Lee, J. S. & Webb, K. Formulation and characterization of poloxamine-based hydrogels as tissue sealants. Acta Biomater. 8, 2223–2232 (2012).
Zhang, H. et al. On-demand and negative-thermo-swelling tissue adhesive based on highly branched ambivalent PEG–catechol copolymers. J. Mater. Chem. B 3, 6420–6428 (2015).
Feng, Q. et al. One-pot solvent exchange preparation of non-swellable, thermoplastic, stretchable and adhesive supramolecular hydrogels based on dual synergistic physical crosslinking. npg Asia Mater. 10, e455 (2018).
Li, C., Sajiki, T., Nakayama, Y., Fukui, M. & Matsuda, T. Novel visible-light-induced photocurable tissue adhesive composed of multiply styrene-derivatized gelatin and poly(ethylene glycol) diacrylate. J. Biomed. Mater. Res. B Appl. Biomater. 66B, 439–446 (2003).
Strong, M. J. et al. A pivotal randomized clinical trial evaluating the safety and effectiveness of a novel hydrogel dural sealant as an adjunct to dural repair. Oper. Neurosurg. 13, 204–212 (2017).
US Food and Drug Administration. Premarket approval (PMA) for adherus autospray dural sealant (FDA, 2015).
Behrens, A. M. et al. Blood-aggregating hydrogel particles for use as a hemostatic agent. Acta Biomater. 10, 701–708 (2014).
Artzi, N., Shazly, T., Baker, A. B., Bon, A. & Edelman, E. R. Aldehyde-amine chemistry enables modulated biosealants with tissue-specific adhesion. Adv. Mater. 21, 3399–3403 (2009).
Hoang Thi, T. T., Lee, Y., Park, K. M. & Park, K. D. Enhanced tissue adhesiveness of injectable gelatin-based hydrogels using thiomer. Front. Bioeng. Biotechnol. https://doi.org/10.3389/conf.FBIOE.2016.01.01392 (2016).
Li, S. Hydrolytic degradation characteristics of aliphatic polyesters derived from lactic and glycolic acids. J. Biomed. Mater. Res. 48, 342–353 (1999).
Piskin, E. Biodegradable polymers as biomaterials. J. Biomater. Sci. Polym. Ed. 6, 775–795 (1994).
Laycock, B. et al. Lifetime prediction of biodegradable polymers. Prog. Polym. Sci. 71, 144–189 (2017).
Lyu, S. & Untereker, D. Degradability of polymers for implantable biomedical devices. Int. J. Mol. Sci. 10, 4033–4065 (2009).
Anderson, J. M., Rodrigues, A. & Chang, D. T. Foreign body reaction to biomaterials. Semin. Immunol. 20, 86–100 (2007).
Franz, S., Rammelt, S., Scharnweber, D. & Simon, J. Immune responses to implants – a review of the implications for the design of immunomodulatory biomaterials. Biomaterials 32, 6692–6709 (2011).
Kopeček, J. & Ulbrich, K. Biodegradation of biomedical polymers. Prog. Polym. Sci. 9, 1–58 (1983).
Li, Y., Rodrigues, J. & Tomas, H. Injectable and biodegradable hydrogels: gelation, biodegradation and biomedical applications. Chem. Soc. Rev. 41, 2193–2221 (2012).
Kong, H. J., Kaigler, D., Kim, K. & Mooney, D. J. Controlling rigidity and degradation of alginate hydrogels via molecular weight distribution. Biomacromolecules 5, 1720–1727 (2004).
Charriere, G., Bejot, M., Schnitzler, L., Ville, G. & Hartmann, D. J. Reactions to a bovine collagen implant: clinical and immunologic study in 705 patients. J. Am. Acad. Dermatol. 21, 1203–1208 (1989).
Cooperman, L. & Michaeli, D. The immunogenicity of injectable collagen. I. A 1-year prospective study. J. Am. Acad. Dermatol. 10, 638–646 (1984).
Pereira, M. J. N. et al. Combined surface micropatterning and reactive chemistry maximizes tissue adhesion with minimal inflammation. Adv. Healthc. Mater. 3, 565–571 (2014).
Sebesta, M. J. & Bishoff, J. T. Octylcyanoacrylate skin closure in laparoscopy. J. Endourol. 17, 899–903 (2004).
Epstein, N. Dural repair with four spinal sealants: focused review of the manufacturers’ inserts and the current literature. Spine J. 10, 1065–1068 (2010).
Tamariz, E. et al. Delivery of chemotropic proteins and improvement of dopaminergic neuron outgrowth through a thixotropic hybrid nano-gel. J. Mater. Sci. Mater. Med. 22, 2097 (2011).
Woo, W., Hong, S., Kim, T.-H., Baek, M.-Y. & Song, S.-W. Delayed pulmonary artery rupture after using BioGlue in cardiac surgery. Korean J. Thorac. Cardiovasc. Surg. 50, 474–476 (2017).
Gaffen, A. & Coleman, G. BioGlue surgical adhesive: reported incidents of chronic inflammation and foreign-body reactions. Can. Med. Assoc. J. 175, 1013 (2006).
Ngaage, D. L., Edwards, W. D., Bell, M. R. & Sundt, T. M. A cautionary note regarding long-term sequelae of biologic glue. J. Thorac. Cardiovasc. Surg. 129, 937–938 (2005).
Cuschieri, A. Tissue adhesives in endosurgery. Surg. Innov. 8, 63–68 (2001).
Lloris-Carsí, J. M., Barrios, C., Prieto-Moure, B., Lloris-Cejalvo, J. M. & Cejalvo-Lapeña, D. The effect of biological sealants and adhesive treatments on matrix metalloproteinase expression during renal injury healing. PLOS ONE 12, e0177665 (2017).
O’Leary, D. P., Wang, J. H., Cotter, T. G. & Redmond, H. P. Less stress, more success? Oncological implications of surgery-induced oxidative stress. Gut 62, 461–470 (2013).
Hillel, A. T. et al. Photoactivated composite biomaterial for soft tissue restoration in rodents and in humans. Sci. Transl Med. 3, 93ra67 (2011).
Reid, B. et al. PEG hydrogel degradation and the role of the surrounding tissue environment. J. Tissue Eng. Regen. Med. 9, 315–318 (2015).
Mouthuy, P.-A. et al. Biocompatibility of implantable materials: an oxidative stress viewpoint. Biomaterials 109, 55–68 (2016).
Tamariz, E. & Rios-Ramírez, A. in Biodegradation-Life of Science (eds Chamy, R. & Rosenkranz, F.) (IntechOpen, 2013).
Conde, J., Oliva, N. & Artzi, N. Revisiting the ‘one material fits all’ rule for cancer nanotherapy. Trends Biotechnol. 34, 618–626 (2016).
Gül, N. et al. Surgery-induced reactive oxygen species enhance colon carcinoma cell binding by disrupting the liver endothelial cell lining. Gut 60, 1076–1086 (2011).
Duan, J. & Kasper, D. L. Oxidative depolymerization of polysaccharides by reactive oxygen/nitrogen species. Glycobiology 21, 401–409 (2011).
Xu, X., Jha, A. K., Harrington, D. A., Farach-Carson, M. C. & Jia, X. Hyaluronic acid-based hydrogels: from a natural polysaccharide to complex networks. Soft Matter 8, 3280–3294 (2012).
Xu, Q., He, C., Xiao, C. & Chen, X. Reactive oxygen species (ROS) responsive polymers for biomedical applications. Macromol. Biosci. 16, 635–646 (2016).
Soller, B. R. et al. Feasibility of non-invasive measurement of tissue pH using near-infrared reflectance spectroscopy. J. Clin. Monit. 12, 387–395 (1996).
Anderson, M., Moshnikova, A., Engelman, D. M., Reshetnyak, Y. K. & Andreev, O. A. Probe for the measurement of cell surface pH in vivo and ex vivo. Proc. Natl Acad. Sci. USA 113, 8177–8181 (2016).
Barar, J. & Omidi, Y. Dysregulated pH in tumor microenvironment checkmates cancer therapy. BioImpacts 3, 149–162 (2013).
Feng, L., Dong, Z., Tao, D., Zhang, Y. & Liu, Z. The acidic tumor microenvironment: a target for smart cancer nano-theranostics. Natl. Sci. Rev. 5, 269–286 (2018).
Lin, M.-H. et al. Monitoring the long-term degradation behavior of biomimetic bioadhesive using wireless magnetoelastic sensor. IEEE Trans. Biomed. Eng. 62, 1838–1842 (2015).
Cencer, M. et al. Effect of pH on the rate of curing and bioadhesive properties of dopamine functionalized poly(ethylene glycol) hydrogels. Biomacromolecules 15, 2861–2869 (2014).
Hong, S. et al. Hyaluronic acid catechol: a biopolymer exhibiting a pH-dependent adhesive or cohesive property for human neural stem cell engineering. Adv. Funct. Mater. 23, 1774–1780 (2013).
Kohane, D. S. & Langer, R. Biocompatibility and drug delivery systems. Chem. Sci. 1, 441–446 (2010).
Lei, K. et al. Non-invasive monitoring of in vivo degradation of a radiopaque thermoreversible hydrogel and its efficacy in preventing post-operative adhesions. Acta Biomater. 55, 396–409 (2017).
Prestwich, G. D. et al. What is the greatest regulatory challenge in the translation of biomaterials to the clinic? Sci. Transl Med. 4, 160cm14 (2012).
Krarup, P.-M., Nordholm-Carstensen, A., Jorgensen, L. N. & Harling, H. Anastomotic leak increases distant recurrence and long-term mortality after curative resection for colonic cancer: a nationwide cohort study. Ann. Surg. 259, 930–938 (2014).
Shao, H. & Stewart, R. J. Biomimetic underwater adhesives with environmentally triggered setting mechanisms. Adv. Mater. 22, 729–733 (2010).
Roche, E. T. et al. A light-reflecting balloon catheter for atraumatic tissue defect repair. Sci. Transl Med. 7, 306ra149 (2015).
Stam, M. A. W. et al. Sylys® surgical sealant: a safe adjunct to standard bowel anastomosis closure. Ann. Surg. Innov. Res. 8, 6 (2014).
Anseth, K. S. & Burdick, J. A. New directions in photopolymerizable biomaterials. MRS Bull. 27, 130–136 (2002).
Sabnis, A., Rahimi, M., Chapman, C. & Nguyen, K. T. Cytocompatibility studies of an in situ photopolymerized thermoresponsive hydrogel nanoparticle system using human aortic smooth muscle cells. J. Biomed. Mater. Res. A 91, 52–59 (2009).
Williams, C. G., Malik, A. N., Kim, T. K., Manson, P. N. & Elisseeff, J. H. Variable cytocompatibility of six cell lines with photoinitiators used for polymerizing hydrogels and cell encapsulation. Biomaterials 26, 1211–1218 (2005).
Pellenc, Q. et al. Preclinical and clinical evaluation of a novel synthetic bioresorbable, on-demand, light-activated sealant in vascular reconstruction. J. Cardiovasc. Surg. 60, 599–611 (2019).
Elvin, C. M. et al. The development of photochemically crosslinked native fibrinogen as a rapidly formed and mechanically strong surgical tissue sealant. Biomaterials 30, 2059–2065 (2009).
Fu, A., Gwon, K., Kim, M., Tae, G. & Kornfield, J. A. Visible-light-initiated thiol-acrylate photopolymerization of heparin-based hydrogels. Biomacromolecules 16, 497–506 (2015).
Tan, H. & Marra, K. G. Injectable, biodegradable hydrogels for tissue engineering applications. Materials 3, 1746–1767 (2010).
Li, L. et al. Biodegradable and injectable in situ cross-linking chitosan-hyaluronic acid based hydrogels for postoperative adhesion prevention. Biomaterials 35, 3903–3917 (2014).
Mo, X., Iwata, H., Matsuda, S. & Ikada, Y. Soft tissue adhesive composed of modified gelatin and polysaccharides. J. Biomater. Sci. Polym. Ed. 11, 341–351 (2000).
Tan, H., Chu, C. R., Payne, K. A. & Marra, K. G. Injectable in situ forming biodegradable chitosan–hyaluronic acid based hydrogels for cartilage tissue engineering. Biomaterials 30, 2499–2506 (2009).
Nair, D. P. et al. The thiol-Michael addition click reaction: a powerful and widely used tool in materials chemistry. Chem. Mater. 26, 724–744 (2014).
Lee, Y. et al. Thermo-sensitive, injectable, and tissue adhesive sol–gel transition hyaluronic acid/pluronic composite hydrogels prepared from bio-inspired catechol-thiol reaction. Soft Matter 6, 977–983 (2010).
Metters, A. & Hubbell, J. Network formation and degradation behavior of hydrogels formed by Michael-type addition reactions. Biomacromolecules 6, 290–301 (2005).
Nie, W., Yuan, X., Zhao, J., Zhou, Y. & Bao, H. Rapidly in situ forming chitosan/ε-polylysine hydrogels for adhesive sealants and hemostatic materials. Carbohydr. Polym. 96, 342–348 (2013).
Lamph, S. Regulation of medical devices outside the European Union. J. R. Soc. Med. 105, 12–21 (2012).
Mahdavi, A. et al. A biodegradable and biocompatible gecko-inspired tissue adhesive. Proc. Natl Acad. Sci. USA 105, 2307–2312 (2008).
Coover, H. W. Chemistry and performance of cyanoacrylate adhesives. J. Soc. Plast. Eng. 15, 413–417 (1959).
Tatooles, C. J. & Braunwald, N. S. The use of crosslinked gelatin as a tissue adhesive to control hemorrhage from liver and kidney. Surgery 60, 857–861 (1966).
Mintz, P. D. et al. Fibrin sealant: clinical use and the development of the University of Virginia Tissue Adhesive Center. Ann. Clin. Lab. Sci. 31, 108–118 (2001).
Ennker, J. et al. The impact of gelatin-resorcinol glue on aortic tissue: a histomorphologic evaluation. J. Vasc. Surg. 20, 34–43 (1994).
Kowanko, N. Adhesive composition and method. US Patent US5385606A (1993).
Sawhney, A. S., Pathak, C. P. & Hubbell, J. A. Bioerodible hydrogels based on photopolymerized poly(ethylene glycol)-co-poly(α-hydroxy acid) diacrylate macromers. Macromolecules 26, 581–587 (1993).
FDA. Premarket Approval (PMA) for Dermabond® https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=p960052 (1998).
Barrows, T. H., Lewis, T. W. & Truong, M. T. Adhesive sealant composition. US Patent US5583114A (1994).
Holowka, E. P. & Bhatia, S. K. Drug Delivery: Materials Design and Clinical Perspective (Springer, 2014).
US Food and Drug Administration. Premarket approval (PMA) for BioGlue® (FDA, 2001).
Zhang, J.-Y., Doll, B. A., Beckman, E. J. & Hollinger, J. O. Three-dimensional biocompatible ascorbic acid-containing scaffold for bone tissue engineering. Tissue Eng. 9, 1143–1157 (2003).
McDermott, M. K., Chen, T., Williams, C. M., Markley, K. M. & Payne, G. F. Mechanical properties of biomimetic tissue adhesive based on the microbial transglutaminase-catalyzed crosslinking of gelatin. Biomacromolecules 5, 1270–1279 (2004).
Bitton, R. & Bianco-Peled, H. Novel biomimetic adhesives based on algae glue. Macromol. Biosci. 8, 393–400 (2008).
US Food and Drug Administration. Premarket approval (PMA) for DuraSeal dural sealant system (FDA, 2005).
US Food and Drug Administration. Premarket approval (PMA) for Ethicon OMNEX surgical sealant (FDA, 2010).
US Food and Drug Administration. Premarket approval (PMA) for Cohera Medical TissuGlu (2015).
Jito, J., Nitta, N. & Nozaki, K. Delayed cerebrospinal fluid leak after watertight dural closure with a polyethylene glycol hydrogel dural sealant in posterior fossa surgery: case report. Neurol. Med. Chir. 54, 634–639 (2014).
Sani, E. S. et al. Sutureless repair of corneal injuries using naturally derived bioadhesive hydrogels. Sci. Adv. 5, eaav1281 (2019).
Wuyts, F. L. et al. Elastic properties of human aortas in relation to age and atherosclerosis: a structural model. Phys. Med. Biol. 40, 1577–1597 (1995).
Annabi, N. et al. Engineering a sprayable and elastic hydrogel adhesive with antimicrobial properties for wound healing. Biomaterials 139, 229–243 (2017).
Helander, H. F. & Fändriks, L. Surface area of the digestive tract – revisited. Scand. J. Gastroenterol. 49, 681–689 (2014).
Lee, S., Pham, A. M., Pryor, S. G., Tollefson, T. & Sykes, J. M. Efficacy of Crosseal fibrin sealant (human) in rhytidectomy. Arch. Facial Plast. Surg. 11, 29–33 (2009).
Azuma, K. et al. Biological adhesive based on carboxymethyl chitin derivatives and chitin nanofibers. Biomaterials 42, 20–29 (2015).
Walgenbach, K. J., Bannasch, H., Kalthoff, S. & Rubin, J. P. Randomized, prospective study of TissuGlu® surgical adhesive in the management of wound drainage following abdominoplasty. Aesthetic Plast. Surg. 36, 491–496 (2012).
Kawai, H. et al. Usefulness of a new gelatin glue sealant system for dural closure in a rat durotomy model. Neurol. Med. Chir. 54, 640–646 (2014).
Lin, K. L. et al. DuraSeal as a ligature in the anastomosis of rat sciatic nerve gap injury. J. Surg. Res. 161, 101–110 (2010).
Assmann, A. et al. A highly adhesive and naturally derived sealant. Biomaterials 140, 115–127 (2017).
Florek, H.-J. et al. Results from a first-in-human trial of a novel vascular sealant. Front. Surg. 2, 29 (2015).
Coselli, J. S. et al. Prospective randomized study of a protein-based tissue adhesive used as a hemostatic and structural adjunct in cardiac and vascular anastomotic repair procedures. J. Am. Coll. Surg. 197, 243–252 (2003).
Kopelman, Y. et al. A gelatin-based prophylactic sealant for bowel wall closure, initial evaluation in mid-rectal anastomosis in a large animal model. J. Gastrointest. Dig. Syst. 5, 1–6 (2015).
Tjandra, J. J. & Chan, M. K. Y. A sprayable hydrogel adhesion barrier facilitates closure of defunctioning loop ileostomy: a randomized trial. Dis. Colon Rectum 51, 956–960 (2008).
Muto, G., D’Urso, L., Castelli, E., Formiconi, A. & Bardari, F. Cyanoacrylic glue: a minimally invasive nonsurgical first line approach for the treatment of some urinary fistulas. J. Urol. 174, 2239–2243 (2005).
Sanders, L., Stone, R., Webb, K., Mefford, T. & Nagatomi, J. Mechanical characterization of a bifunctional Tetronic hydrogel adhesive for soft tissues. J. Biomed. Mater. Res. A 103, 861–868 (2015).
Acknowledgements
This work was supported by the Korea Institute for Advancement of Technology (N0002123) to Y.L., the MIT Deshpande Center and BioDevek to N.A. and the National Institutes of Health through the R01 grant HL095722 to J.M.K.
Author information
Authors and Affiliations
Contributions
All authors researched data and contributed to the discussion, writing and revising of the content.
Corresponding authors
Ethics declarations
Competing interests
G.M.T. is employed by BioDevek, a company that has filed patents based on materials described in this manuscript. G.M.T benefits from the stock options compensation plan from BioDevek. M.J.N.P. is an employee and holds stock options in TISSIUM, a company that further licensed intellectual property (IP) generated by M.J.N.P. and that may benefit financially if the IP is further validated. M.J.N.P. has filed patents based on materials described in this manuscript. J.M.K. holds equity in TISSIUM, a company that has an option to license IP generated by J.M.K. and that may benefit financially if the IP is licensed and further validated. The interests of J.M.K. were reviewed and are subject to a management plan overseen by their institutions in accordance with their conflict of interest policies. J.M.K. has filed patents based on materials described in this manuscript. N.A. holds equity in BioDevek, a company that has an option to license IP generated by N.A. and that may benefit financially if the IP is licensed and further validated. The interests of N.A. were reviewed and are subject to a management plan overseen by their institutions in accordance with their conflict of interest policies. N.A. has filed patents based on materials described in this manuscript. Y.L. has filed patents based on materials described in this manuscript. The other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Taboada, G.M., Yang, K., Pereira, M.J.N. et al. Overcoming the translational barriers of tissue adhesives. Nat Rev Mater 5, 310–329 (2020). https://doi.org/10.1038/s41578-019-0171-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41578-019-0171-7
This article is cited by
-
Swim bladder-derived biomaterials: structures, compositions, properties, modifications, and biomedical applications
Journal of Nanobiotechnology (2024)
-
A 3D printable tissue adhesive
Nature Communications (2024)
-
Ultraviolet light blocking optically clear adhesives for foldable displays via highly efficient visible-light curing
Nature Communications (2024)
-
Hydrogel bioadhesives harnessing nanoscale phase separation for Achilles tendon repairing
Nano Research (2024)
-
Progress of tissue adhesives based on proteins and synthetic polymers
Biomaterials Research (2023)