Abstract
Obesity increases the risk of multiple gastrointestinal cancers and worsens disease outcomes. Conversely, strong inverse associations have emerged between physical activity and colon cancer and possibly other gastrointestinal malignancies. The effect of weight loss interventions — such as modifications of diet and/or physical activity or bariatric surgery — remains unclear in patients who are obese and have gastrointestinal cancer, although large clinical trials are underway. Human intervention studies have already shed light on potential mechanisms underlying the energy balance–cancer relationship, with preclinical models supporting emerging pathway effects. Central to interventions that reduce obesity or increase physical activity are pluripotent cancer-preventive effects (including reduced systemic and adipose tissue inflammation and angiogenesis, altered adipokine levels and improved insulin resistance) that directly interface with the hallmarks of cancer. Other mechanisms, such as DNA repair, oxidative stress and telomere length, immune function, effects on cancer stem cells and the microbiome, could also contribute to energy balance effects on gastrointestinal cancers. Although some mechanisms are well understood (for instance, systemic effects on inflammation and insulin signalling), other areas remain unclear. The current state of knowledge supports the need to better integrate mechanistic approaches with preclinical and human studies to develop effective, personalized diet and exercise interventions to reduce the burden of obesity on gastrointestinal cancer.
Key points
-
Energy balance interventions, such as physical activity and caloric restriction, can reduce individual cancer risk and prevent gastrointestinal carcinogenesis.
-
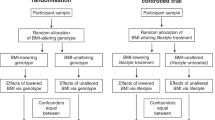
Intervention trials are instrumental in fully understanding the effects of energy balance on cancer risk, clinical outcomes and underlying biological mechanisms.
-
The main mechanistic pathways underlying the obesity–gastrointestinal cancer link include systemic inflammation, metabolic reprogramming and adipose tissue-dependent effects.
-
Additional pathways that might have a role are oxidative stress and DNA repair, proliferation, apoptosis and angiogenesis, the gut microbiome and immune function.
-
Preclinical studies using both diet-induced and genetically induced obesity models provide supporting evidence to clinical findings.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Demark-Wahnefried, W. et al. The role of obesity in cancer survival and recurrence. Cancer Epidemiol. Biomarkers Prev. 21, 1244–1259 (2012).
Romieu, I. et al. Energy balance and obesity: what are the main drivers? Cancer Causes Control 28, 247–258 (2017).
National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-term Trends in Health (National Center for Health Statistics, Hyattsville, MD, 2017).
Lauby-Secretan, B. et al. Body fatness and cancer —viewpoint of the IARC Working Group. N. Engl. J. Med. 375, 794–798 (2016).
World Cancer Research Fund (WCRF)/American Institute for Cancer Research. Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. (AICR, Washington DC, 2018).
Wolin, K. Y., Yan, Y., Colditz, G. A. & Lee, I. M. Physical activity and colon cancer prevention: a meta-analysis. Br. J. Cancer 100, 611–616 (2009).
Donnelly, J. E. et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sports Exerc. 41, 459–471 (2009).
Centers for Disease Control & Prevention. Facts about Physical Activity. Centers for Disease Control & Prevention https://www.cdc.gov/physicalactivity/data/facts.htm (2016).
Reis, R. S. et al. Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. Lancet 388, 1337–1348 (2016).
Murphy, N., Jenab, M. & Gunter, M. J. Adiposity and gastrointestinal cancers: epidemiology, mechanisms and future directions. Nat. Rev. Gastroenterol. Hepatol. https://doi.org/10.1038/s41575-018-0038-1 (2018).
Emmons, K. M. & Colditz, G. A. Realizing the potential of cancer prevention - the role of implementation science. N. Engl. J. Med. 376, 986–990 (2017).
Thomson, C. A. et al. Cancer incidence and mortality during the intervention and postintervention periods of the Women’s Health Initiative dietary modification trial. Cancer Epidemiol. Biomarkers Prev. 23, 2924–2935 (2014).
Howard, B. V. et al. Low-fat dietary pattern and weight change over 7 years: the Women’s Health Initiative dietary modification trial. JAMA 295, 39–49 (2006).
Jiao, L. et al. Low-fat dietary pattern and pancreatic cancer risk in the Women’s Health Initiative dietary modification randomized controlled trial. J. Natl Cancer Inst. 110, djx117 (2018).
Spechler, S. J. & Goyal, R. K. Barrett’s esophagus. N. Engl. J. Med. 315, 362–371 (1986).
Reid, B. J., Li, X., Galipeau, P. C. & Vaughan, T. L. Barrett’s oesophagus and oesophageal adenocarcinoma: time for a new synthesis. Nat. Rev. Cancer 10, 87–101 (2010).
Winzer, B. M., Paratz, J. D., Reeves, M. M. & Whiteman, D. C. Exercise and the Prevention of Oesophageal Cancer (EPOC) study protocol: a randomized controlled trial of exercise versus stretching in males with Barrett’s oesophagus. BMC Cancer 10, 292 (2010).
Winzer, B. M., Paratz, J. D., Whitehead, J. P., Whiteman, D. C. & Reeves, M. M. The feasibility of an exercise intervention in males at risk of oesophageal adenocarcinoma: a randomized controlled trial. PLOS One 10, e0117922 (2015).
Anderson, A. S. et al. The impact of a bodyweight and physical activity intervention (BeWEL) initiated through a national colorectal cancer screening programme: randomised controlled trial. BMJ 348, g1823 (2014).
Buchwald, H. The evolution of metabolic/bariatric surgery. Obes. Surg. 24, 1126–1135 (2014).
Adams, T. D. et al. Cancer incidence and mortality after gastric bypass surgery. Obesity 17, 796–802 (2009).
Derogar, M. et al. Increased risk of colorectal cancer after obesity surgery. Ann. Surg. 258, 983–988 (2013).
Tao, W. et al. Colorectal cancer prognosis following obesity surgery in a population-based cohort study. Obes. Surg. 27, 1233–1239 (2017).
Tse, W. H. W., Kroon, H. M. & van Lanschot, J. J. B. Clinical challenges in upper gastrointestinal malignancies after bariatric surgery. Dig. Surg. 35, 183–186 (2018).
Abrahamson, P. E. et al. No effect of exercise on colon mucosal prostaglandin concentrations: a 12-month randomized controlled trial. Cancer Epidemiol. Biomarkers Prev. 16, 2351–2356 (2007).
Campbell, K. L. et al. Effect of a 12-month exercise intervention on the apoptotic regulating proteins bax and bcl-2 in colon crypts: a randomized controlled trial. Cancer Epidemiol. Biomarkers Prev. 16, 1767–1774 (2007).
McTiernan, A. et al. Effect of a 12-month exercise intervention on patterns of cellular proliferation in colonic crypts: A randomized controlled trial. Cancer Epidemiol. Biomarkers Prev. 15, 1–10 (2006).
Morey, M. C. et al. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: a randomized controlled trial. JAMA 301, 1883–1891 (2009).
Xu, Y. J. et al. A walk-and-eat intervention improves outcomes for patients with esophageal cancer undergoing neoadjuvant chemoradiotherapy. Oncologist 20, 1216–1222 (2015).
Yeo, T. P. et al. A progressive postresection walking program significantly improves fatigue and health-related quality of life in pancreas and periampullary cancer patients. J. Am. Coll. Surg. 214, 463–477 (2012).
Meyerhardt, J. A. et al. Physical activity and survival after colorectal cancer diagnosis. J. Clin. Oncol. 24, 3527–3534 (2006).
Strasser, B., Steindorf, K., Wiskemann, J. & Ulrich, C. M. Impact of resistance training in cancer survivors: a meta-analysis. Med. Sci. Sports Exerc. 45, 2080–2090 (2013).
Friedenreich, C. M., Neilson, H. K., Farris, M. S. & Courneya, K. S. Physical activity and cancer outcomes: a precision medicine approach. Clin. Cancer Res. 22, 4766–4775 (2016).
Cho, H. et al. Matched pair analysis to examine the effects of a planned preoperative exercise program in early gastric cancer patients with metabolic syndrome to reduce operative risk: the Adjuvant Exercise for General Elective Surgery (AEGES) study group. Ann. Surg. Oncol. 21, 2044–2050 (2014).
Van Blarigan, E. L. & Meyerhardt, J. A. Role of physical activity and diet after colorectal cancer diagnosis. J. Clin. Oncol. 33, 1825–1834 (2015).
Je, Y., Jeon, J. Y., Giovannucci, E. L. & Meyerhardt, J. A. Association between physical activity and mortality in colorectal cancer: a meta-analysis of prospective cohort studies. Int. J. Cancer 133, 1905–1913 (2013).
Courneya, K. S. et al. The Colon Health and Life-Long Exercise Change trial: a randomized trial of the National Cancer Institute of Canada Clinical Trials Group. Curr. Oncol. 15, 279–285 (2008).
van der Schaaf, M. K. et al. The influence of preoperative weight loss on the postoperative course after esophageal cancer resection. J. Thorac Cardiovasc. Surg. 147, 490–495 (2014).
Aoyama, T. et al. Postoperative weight loss leads to poor survival through poor S-1 efficacy in patients with stage II/III gastric cancer. Int. J. Clin. Oncol. 22, 476–483 (2017).
van Rooijen, S. J. et al. Systematic review of exercise training in colorectal cancer patients during treatment. Scand. J. Med. Sci. Sports 28, 360–370 (2018).
van Vulpen, J. K. et al. Physical ExeRcise Following Esophageal Cancer Treatment (PERFECT) study: design of a randomized controlled trial. BMC Cancer 17, 552 (2017).
Ahn, K. Y. et al. The effects of inpatient exercise therapy on the length of hospital stay in stages I-III colon cancer patients: randomized controlled trial. Int. J. Colorectal Dis. 28, 643–651 (2013).
Courneya, K. S. et al. Effects of a structured exercise program on physical activity and fitness in colon cancer survivors: one year feasibility results from the CHALLENGE trial. Cancer Epidemiol. Biomarkers Prev. 25, 969–977 (2016).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Foster-Schubert, K. E. et al. Effect of diet and exercise, alone or combined, on weight and body composition in overweight-to-obese postmenopausal women. Obesity 20, 1628–1638 (2012).
van Gemert, W. A. et al. Design of the SHAPE-2 study: the effect of physical activity, in addition to weight loss, on biomarkers of postmenopausal breast cancer risk. BMC Cancer 13, 395 (2013).
Teicher, B. A. Tumor Models in Cancer Research (Springer, 2011).
Bijlsma, M. F., Sadanandam, A., Tan, P. & Vermeulen, L. Molecular subtypes in cancers of the gastrointestinal tract. Nat. Rev. Gastroenterol. Hepatol. 14, 333–342 (2017).
Sawayama, H. et al. Clinical impact of the Warburg effect in gastrointestinal cancer (review). Int. J. Oncol. 45, 1345–1354 (2014).
Mayers, J. R. et al. Tissue of origin dictates branched-chain amino acid metabolism in mutant Kras-driven cancers. Science 353, 1161–1165 (2016).
Hanyuda, A. et al. Body mass index and risk of colorectal carcinoma subtypes classified by tumor differentiation status. Eur. J. Epidemiol. 32, 393–407 (2017).
Berriel Diaz, M., Herzig, S. & Schafmeier, T. Biological mechanisms for the effect of obesity on cancer risk: experimental evidence. Recent Results Cancer Res. 208, 219–242 (2016).
Westbrook, A. M., Szakmary, A. & Schiestl, R. H. Mouse models of intestinal inflammation and cancer. Arch. Toxicol. 90, 2109–2130 (2016).
Crusz, S. M. & Balkwill, F. R. Inflammation and cancer: advances and new agents. Nat. Rev. Clin. Oncol. 12, 584–596 (2015).
Lashinger, L. M., Ford, N. A. & Hursting, S. D. Interacting inflammatory and growth factor signals underlie the obesity-cancer link. J. Nutr. 144, 109–113 (2014).
Campbell, K. L. et al. No reduction in C-reactive protein following a 12-month randomized controlled trial of exercise in men and women. Cancer Epidemiol. Biomarkers Prev. 17, 1714–1718 (2008).
Campbell, P. T. et al. A yearlong exercise intervention decreases CRP among obese postmenopausal women. Med. Sci. Sports Exerc. 41, 1533–1539 (2009).
Le, T. et al. Effects of diet composition and insulin resistance status on plasma lipid levels in a weight loss intervention in women. J. Am. Heart Assoc. 5, e002771 (2016).
Imayama, I. et al. Effects of a caloric restriction weight loss diet and exercise on inflammatory biomarkers in overweight/obese postmenopausal women: a randomized controlled trial. Cancer Res. 72, 2314–2326 (2012).
Friedenreich, C. M. et al. Inflammatory marker changes in postmenopausal women after a year-long exercise intervention comparing high versus moderate volumes. Cancer Prev. Res. 9, 196–203 (2016).
Lin, P. C., Lin, Y. J., Lee, C. T., Liu, H. S. & Lee, J. C. Cyclooxygenase-2 expression in the tumor environment is associated with poor prognosis in colorectal cancer patients. Oncol. Lett. 6, 733–739 (2013).
Maihofner, C. et al. Expression of cyclooxygenase-2 parallels expression of interleukin-1beta, interleukin-6 and NF-kappaB in human colorectal cancer. Carcinogenesis 24, 665–671 (2003).
van Gemert, W. A. et al. Effect of weight loss with or without exercise on inflammatory markers and adipokines in postmenopausal women: the SHAPE-2 trial, a randomized controlled trial. Cancer Epidemiol. Biomarkers Prev. 25, 799–806 (2016).
de Maat, M. F. et al. Epigenetic silencing of cyclooxygenase-2 affects clinical outcome in gastric cancer. J. Clin. Oncol. 25, 4887–4894 (2007).
Peng, L., Zhou, Y., Wang, Y., Mou, H. & Zhao, Q. Prognostic significance of COX-2 immunohistochemical expression in colorectal cancer: a meta-analysis of the literature. PLOS One 8, e58891 (2013).
Forsythe, L. K., Wallace, J. M. & Livingstone, M. B. Obesity and inflammation: the effects of weight loss. Nutr. Res. Rev. 21, 117–133 (2008).
Santos, J. et al. Effect of bariatric surgery on weight loss, inflammation, iron metabolism, and lipid profile. Scand. J. Surg. 103, 21–25 (2014).
Lasselin, J. et al. Adipose inflammation in obesity: relationship with circulating levels of inflammatory markers and association with surgery-induced weight loss. J. Clin. Endocrinol. Metab. 99, E53–E61 (2014).
Kelly, A. S. et al. Changes in inflammation, oxidative stress and adipokines following bariatric surgery among adolescents with severe obesity. Int. J. Obes. 40, 275–280 (2016).
Mazur-Bialy, A. I. et al. Beneficial effect of voluntary exercise on experimental colitis in mice fed a high-fat diet: the role of irisin, adiponectin and proinflammatory biomarkers. Nutrients 9, E410 (2017).
Wang, Q. et al. Differential effect of weight loss with low-fat diet or high-fat diet restriction on inflammation in the liver and adipose tissue of mice with diet-induced obesity. Atherosclerosis 219, 100–108 (2011).
Chen, F. et al. New horizons in tumor microenvironment biology: challenges and opportunities. BMC Med. 13, 45 (2015).
Perez-Hernandez, A. I., Catalan, V., Gomez-Ambrosi, J., Rodriguez, A. & Fruhbeck, G. Mechanisms linking excess adiposity and carcinogenesis promotion. Front. Endocrinol. 5, 65 (2014).
Himbert, C. et al. Signals from the adipose microenvironment and the obesity-cancer link-a systematic review. Cancer Prev. Res. 10, 494–506 (2017).
Campbell, K. L., Landells, C. E., Fan, J. & Brenner, D. R. A. Systematic review of the effect of lifestyle interventions on adipose tissue gene expression: implications for carcinogenesis. Obesity 25 (Suppl. 2), S40–S51 (2017).
Koerner, A., Kratzsch, J. & Kiess, W. Adipocytokines: leptin — the classical, resistin—the controversical, adiponectin — the promising, and more to come. Best Pract. Res. Clin. Endocrinol. Metab. 19, 525–546 (2005).
Schubel, R. et al. The effects of intermittent calorie restriction on metabolic health: Rationale and study design of the HELENA Trial. Contemp. Clin. Trials 51, 28–33 (2016).
Nakhuda, A. et al. Biomarkers of browning of white adipose tissue and their regulation during exercise- and diet-induced weight loss. Am. J. Clin. Nutr. 104, 557–565 (2016).
Brown, J. C. et al. Dose-response effects of aerobic exercise on body composition among colon cancer survivors: a randomised controlled trial. Br. J. Cancer 117, 1614–1620 (2017).
Nuri, R., Moghaddasi, M., Darvishi, H. & Izadpanah, A. Effect of aerobic exercise on leptin and ghrelin in patients with colorectal cancer. J. Cancer Res. Ther. 12, 169–174 (2016).
Lee, M. K. et al. Effect of home-based exercise intervention on fasting insulin and adipocytokines in colorectal cancer survivors: a randomized controlled trial. Metabolism 76, 23–31 (2017).
Wallace, A. M., Sattar, N. & McMillan, D. C. Effect of weight loss and the inflammatory response on leptin concentrations in gastrointestinal cancer patients. Clin. Cancer Res. 4, 2977–2979 (1998).
Riondino, S. et al. Obesity and colorectal cancer: role of adipokines in tumor initiation and progression. World J. Gastroenterol. 20, 5177–5190 (2014).
Holland, W. L. et al. Receptor-mediated activation of ceramidase activity initiates the pleiotropic actions of adiponectin. Nat. Med. 17, 55–63 (2011).
Park, J., Morley, T. S., Kim, M., Clegg, D. J. & Scherer, P. E. Obesity and cancer—mechanisms underlying tumour progression and recurrence. Nat. Rev. Endocrinol. 10, 455–465 (2014).
Abbenhardt, C. et al. Effects of individual and combined dietary weight loss and exercise interventions in postmenopausal women on adiponectin and leptin levels. J. Intern. Med. 274, 163–175 (2013).
Rokling-Andersen, M. H. et al. Effects of long-term exercise and diet intervention on plasma adipokine concentrations. Am. J. Clin. Nutr. 86, 1293–1301 (2007).
Friedenreich, C. M. et al. Changes in insulin resistance indicators, IGFs, and adipokines in a year-long trial of aerobic exercise in postmenopausal women. Endocr. Relat. Cancer 18, 357–369 (2011).
Kelly, K. R. et al. Lifestyle-induced decrease in fat mass improves adiponectin secretion in obese adults. Med. Sci. Sports Exerc. 46, 920–926 (2014).
Thompson, H. J. et al. Impact of weight loss on plasma leptin and adiponectin in overweight-to-obese post menopausal breast cancer survivors. Nutrients 7, 5156–5176 (2015).
Mason, C. et al. The effects of separate and combined dietary weight loss and exercise on fasting ghrelin concentrations in overweight and obese women: a randomized controlled trial. Clin. Endocrinol. 82, 369–376 (2015).
Wang, X., You, T., Murphy, K., Lyles, M. F. & Nicklas, B. J. Addition of exercise increases plasma adiponectin and release from adipose tissue. Med. Sci. Sports Exerc. 47, 2450–2455 (2015).
Christiansen, T., Paulsen, S. K., Bruun, J. M., Pedersen, S. B. & Richelsen, B. Exercise training versus diet-induced weight-loss on metabolic risk factors and inflammatory markers in obese subjects: a 12-week randomized intervention study. Am. J. Physiol. Endocrinol. Metab. 298, E824–E831 (2010).
Campbell, K. L. et al. Gene expression changes in adipose tissue with diet- and/or exercise-induced weight loss. Cancer Prev. Res. 6, 217–231 (2013).
Vaittinen, M., Kolehmainen, M., Schwab, U., Uusitupa, M. & Pulkkinen, L. Microfibrillar-associated protein 5 is linked with markers of obesity-related extracellular matrix remodeling and inflammation. Nutr. Diabetes 1, e15 (2011).
Walhin, J. P., Richardson, J. D., Betts, J. A. & Thompson, D. Exercise counteracts the effects of short-term overfeeding and reduced physical activity independent of energy imbalance in healthy young men. J. Physiol. 591, 6231–6243 (2013).
Sjogren, P. et al. Functional changes in adipose tissue in a randomised controlled trial of physical activity. Lipids Health Dis. 11, 80 (2012).
Phillips, M. D. et al. Resistance training reduces subclinical inflammation in obese, postmenopausal women. Med. Sci. Sports Exerc. 44, 2099–2110 (2012).
Sjostrom, L. et al. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol. 10, 653–662 (2009).
Herder, C. et al. Adiponectin and bariatric surgery: associations with diabetes and cardiovascular disease in the Swedish Obese Subjects study. Diabetes Care 37, 1401–1409 (2014).
Serra, A. et al. The effect of bariatric surgery on adipocytokines, renal parameters and other cardiovascular risk factors in severe and very severe obesity: 1-year follow-up. Clin. Nutr. 25, 400–408 (2006).
Frikke-Schmidt, H., O’Rourke, R. W., Lumeng, C. N., Sandoval, D. A. & Seeley, R. J. Does bariatric surgery improve adipose tissue function? Obes. Rev. 17, 795–809 (2016).
Hagman, D. K. et al. The short-term and long-term effects of bariatric/metabolic surgery on subcutaneous adipose tissue inflammation in humans. Metabolism 70, 12–22 (2017).
Sams, V. G. et al. Effect of bariatric surgery on systemic and adipose tissue inflammation. Surg. Endosc. 30, 3499–3504 (2016).
Fruhbeck, G. Bariatric and metabolic surgery: a shift in eligibility and success criteria. Nat. Rev. Endocrinol. 11, 465–477 (2015).
Falk, R. T. et al. Estrogen metabolites are not associated with colorectal cancer risk in postmenopausal women. Cancer Epidemiol. Biomarkers Prev. 24, 1419–1422 (2015).
Rudolph, A. et al. Colorectal cancer risk associated with hormone use varies by expression of estrogen receptor-beta. Cancer Res. 73, 3306–3315 (2013).
Murphy, N. et al. A prospective evaluation of endogenous sex hormone levels and colorectal cancer risk in postmenopausal women. J. Natl Cancer Inst. 107, djv210 (2015).
Limsui, D. et al. Postmenopausal hormone therapy and colorectal cancer risk by molecularly defined subtypes among older women. Gut 61, 1299–1305 (2012).
Prentice, R. L. et al. Colorectal cancer in relation to postmenopausal estrogen and estrogen plus progestin in the Women’s Health Initiative clinical trial and observational study. Cancer Epidemiol. Biomarkers Prev. 18, 1531–1537 (2009).
Camargo, M. C. et al. Sex hormones, hormonal interventions, and gastric cancer risk: a meta-analysis. Cancer Epidemiol. Biomarkers Prev. 21, 20–38 (2012).
Sukocheva, O. A., Li, B., Due, S. L., Hussey, D. J. & Watson, D. I. Androgens and esophageal cancer: what do we know? World J. Gastroenterol. 21, 6146–6156 (2015).
Petrick, J. L. et al. Association between circulating levels of sex steroid hormones and esophageal adenocarcinoma in the FINBAR Study. PLOS One 13, e0190325 (2018).
Andren-Sandberg, A. & Johansson, J. Influence of sex hormones on pancreatic cancer. Int. J. Pancreatol. 7, 167–176 (1990).
Lukanova, A. et al. Prediagnostic plasma testosterone, sex hormone-binding globulin, IGF-I and hepatocellular carcinoma: etiological factors or risk markers? Int. J. Cancer 134, 164–173 (2014).
Campbell, K. L. et al. Reduced-calorie dietary weight loss, exercise, and sex hormones in postmenopausal women: randomized controlled trial. J. Clin. Oncol. 30, 2314–2326 (2012).
McTiernan, A. et al. Effect of exercise on serum androgens in postmenopausal women: a 12-month randomized clinical trial. Cancer Epidemiol. Biomarkers Prev. 13, 1099–1105 (2004).
McTiernan, A. et al. Effect of exercise on serum estrogens in postmenopausal women: a 12-month randomized clinical trial. Cancer Res. 64, 2923–2928 (2004).
Kim, C. et al. Racial/ethnic differences in sex hormone levels among postmenopausal women in the diabetes prevention program. J. Clin. Endocrinol. Metab. 97, 4051–4060 (2012).
Hawkins, V. N. et al. Effect of exercise on serum sex hormones in men: a 12-month randomized clinical trial. Med. Sci. Sports Exerc. 40, 223–233 (2008).
Friedenreich, C. M. et al. Effects of exercise dose on endogenous estrogens in postmenopausal women: a randomized trial. Endocr. Relat. Cancer 22, 863–876 (2015).
Longnecker, D. S. Hormones and pancreatic cancer. Int. J. Pancreatol. 9, 81–86 (1991).
Armstrong, C. M., Allred, K. F., Weeks, B. R., Chapkin, R. S. & Allred, C. D. Estradiol has differential effects on acute colonic inflammation in the presence and absence of estrogen receptor beta expression. Dig. Dis. Sci. 62, 1977–1984 (2017).
Roshan, M. H., Tambo, A. & Pace, N. P. The role of testosterone in colorectal carcinoma: pathomechanisms and open questions. EPMA J. 7, 22 (2016).
Wilde, L. et al. Metabolic coupling and the reverse Warburg effect in cancer: implications for novel biomarker and anticancer agent development. Semin. Oncol. 44, 198–203 (2017).
Fu, Y. et al. The reverse Warburg effect is likely to be an Achilles’ heel of cancer that can be exploited for cancer therapy. Oncotarget 8, 57813–57825 (2017).
Faupel-Badger, J. M., Berrigan, D., Ballard-Barbash, R. & Potischman, N. Anthropometric correlates of insulin-like growth factor 1 (IGF-1) and IGF binding protein-3 (IGFBP-3) levels by race/ethnicity and gender. Ann. Epidemiol. 19, 841–849 (2009).
Smith, A. T., Clemmons, D. R., Underwood, L. E., Ben-Ezra, V. & McMurray, R. The effect of exercise on plasma somatomedin-C/insulinlike growth factor I concentrations. Metabolism 36, 533–537 (1987).
Nemet, D. et al. Negative energy balance plays a major role in the IGF-I response to exercise training. J. Appl. Physiol. (1985) 96, 276–282 (1985) (2004).
Frank, L. L. et al. Effects of exercise on metabolic risk variables in overweight postmenopausal women: a randomized clinical trial. Obes. Res. 13, 615–625 (2005).
Wang, Y. et al. The human fatty acid synthase gene and de novo lipogenesis are coordinately regulated in human adipose tissue. J. Nutr. 134, 1032–1038 (2004).
Claycombe, K. J. et al. Insulin increases fatty acid synthase gene transcription in human adipocytes. Am. J. Physiol. 274, R1253–R1259 (1998).
Ortega, F. J. et al. The gene expression of the main lipogenic enzymes is downregulated in visceral adipose tissue of obese subjects. Obesity 18, 13–20 (2010).
Mason, C. et al. Effects of dietary weight loss and exercise on insulin-like growth factor-I and insulin-like growth factor-binding protein-3 in postmenopausal women: a randomized controlled trial. Cancer Epidemiol. Biomarkers Prev. 22, 1457–1463 (2013).
Margolis, L. M. et al. Calorie restricted high protein diets downregulate lipogenesis and lower intrahepatic triglyceride concentrations in male rats. Nutrients 8, E571 (2016).
Moore, T. et al. Dietary energy balance modulates signaling through the Akt/mammalian target of rapamycin pathways in multiple epithelial tissues. Cancer Prev. Res. 1, 65–76 (2008).
Bae, J. Y. et al. Exercise and dietary change ameliorate high fat diet induced obesity and insulin resistance via mTOR signaling pathway. J. Exerc. Nutr. Biochem. 20, 28–33 (2016).
Harvey, A. E. et al. Calorie restriction decreases murine and human pancreatic tumor cell growth, nuclear factor-kappaB activation, and inflammation-related gene expression in an insulin-like growth factor-1-dependent manner. PLOS One 9, e94151 (2014).
Piguet, A. C. et al. Regular exercise decreases liver tumors development in hepatocyte-specific PTEN-deficient mice independently of steatosis. J. Hepatol. 62, 1296–1303 (2015).
Weiss, E. P., Reeds, D. N., Ezekiel, U. R., Albert, S. G. & Villareal, D. T. Circulating cytokines as determinants of weight loss-induced improvements in insulin sensitivity. Endocrine 55, 153–164 (2017).
Mason, C. et al. Dietary weight loss and exercise effects on insulin resistance in postmenopausal women. Am. J. Prev. Med. 41, 366–375 (2011).
Rock, C. L. et al. Effects of diet composition on weight loss, metabolic factors and biomarkers in a 1-year weight loss intervention in obese women examined by baseline insulin resistance status. Metabolism 65, 1605–1613 (2016).
Hanyuda, A. et al. Survival benefit of exercise differs by tumor IRS1 expression status in colorectal cancer. Ann. Surg. Oncol. 23, 908–917 (2016).
Brown, J. C. et al. Dose-response effects of aerobic exercise among colon cancer survivors: a randomized phase II trial. Clin. Colorectal Cancer 17, 32–40 (2018).
Sainsbury, A. et al. Increased colorectal epithelial cell proliferation and crypt fission associated with obesity and roux-en-Y gastric bypass. Cancer Epidemiol. Biomarkers Prev. 17, 1401–1410 (2008).
Zhu, Z., Jiang, W. & Thompson, H. J. Effect of energy restriction on tissue size regulation during chemically induced mammary carcinogenesis. Carcinogenesis 20, 1721–1726 (1999).
Olivo-Marston, S. E. et al. Effects of calorie restriction and diet-induced obesity on murine colon carcinogenesis, growth and inflammatory factors, and microRNA expression. PLOS One 9, e94765 (2014).
Bruss, M. D., Thompson, A. C., Aggarwal, I., Khambatta, C. F. & Hellerstein, M. K. The effects of physiological adaptations to calorie restriction on global cell proliferation rates. Am. J. Physiol. Endocrinol. Metab. 300, E735–E745 (2011).
Kant, P. et al. Mucosal biomarkers of colorectal cancer risk do not increase at 6 months following sleeve gastrectomy, unlike gastric bypass. Obesity 22, 202–210 (2014).
Kant, P. et al. Rectal epithelial cell mitosis and expression of macrophage migration inhibitory factor are increased 3 years after Roux-en-Y gastric bypass (RYGB) for morbid obesity: implications for long-term neoplastic risk following RYGB. Gut 60, 893–901 (2011).
Appleton, G. V., Wheeler, E. E., Al-Mufti, R., Challacombe, D. N. & Williamson, R. C. Rectal hyperplasia after jejunoileal bypass for morbid obesity. Gut 29, 1544–1548 (1988).
Thompson, H. J., Zhu, Z. & Jiang, W. Identification of the apoptosis activation cascade induced in mammary carcinomas by energy restriction. Cancer Res. 64, 1541–1545 (2004).
Bouis, D., Kusumanto, Y., Meijer, C., Mulder, N. H. & Hospers, G. A. A review on pro- and anti-angiogenic factors as targets of clinical intervention. Pharmacol. Res. 53, 89–103 (2006).
Duggan, C., Tapsoba, J. D., Wang, C. Y., Foster-Schubert, K. E. & McTiernan, A. Long-term effects of weight loss & exercise on biomarkers associated with angiogenesis. Cancer Epidemiol. Biomarkers Prev. 26, 1788–1794 (2017).
Duggan, C., Xiao, L., Wang, C. Y. & McTiernan, A. Effect of a 12-month exercise intervention on serum biomarkers of angiogenesis in postmenopausal women: a randomized controlled trial. Cancer Epidemiol. Biomarkers Prev. 23, 648–657 (2014).
Duggan, C., Tapsoba Jde, D., Wang, C. Y. & McTiernan, A. Dietary weight loss and exercise effects on serum biomarkers of angiogenesis in overweight postmenopausal women: a randomized controlled trial. Cancer Res. 76, 4226–4235 (2016).
Cullberg, K. B. et al. Effect of weight loss and exercise on angiogenic factors in the circulation and in adipose tissue in obese subjects. Obesity 21, 454–460 (2013).
Sabater, M. et al. Circulating pigment epithelium-derived factor levels are associated with insulin resistance and decrease after weight loss. J. Clin. Endocrinol. Metab. 95, 4720–4728 (2010).
Kurki, E., Shi, J., Martonen, E., Finckenberg, P. & Mervaala, E. Distinct effects of calorie restriction on adipose tissue cytokine and angiogenesis profiles in obese and lean mice. Nutr. Metab. 9, 64 (2012).
Mukherjee, P., Abate, L. E. & Seyfried, T. N. Antiangiogenic and proapoptotic effects of dietary restriction on experimental mouse and human brain tumors. Clin. Cancer Res. 10, 5622–5629 (2004).
Pavlova, N. N. & Thompson, C. B. The emerging hallmarks of cancer metabolism. Cell Metab. 23, 27–47 (2016).
Marseglia, L. et al. Oxidative stress in obesity: a critical component in human diseases. Int. J. Mol. Sci. 16, 378–400 (2015).
Furukawa, S. et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Invest. 114, 1752–1761 (2004).
Meijer, E. P., Goris, A. H., van Dongen, J. L., Bast, A. & Westerterp, K. R. Exercise-induced oxidative stress in older adults as a function of habitual activity level. J. Am. Geriatr. Soc. 50, 349–353 (2002).
Campbell, P. T. et al. Effect of exercise on oxidative stress: a 12-month randomized, controlled trial. Med. Sci. Sports Exerc. 42, 1448–1453 (2010).
Duggan, C. et al. Dietary weight loss, exercise, and oxidative stress in postmenopausal women: a randomized controlled trial. Cancer Prev. Res. 9, 835–843 (2016).
Buchowski, M. S. et al. Effect of modest caloric restriction on oxidative stress in women, a randomized trial. PLOS One 7, e47079 (2012).
Gutierrez-Lopez, L. et al. Hypocaloric diet and regular moderate aerobic exercise is an effective strategy to reduce anthropometric parameters and oxidative stress in obese patients. Obes. Facts 5, 12–22 (2012).
Chae, J. S. et al. Mild weight loss reduces inflammatory cytokines, leukocyte count, and oxidative stress in overweight and moderately obese participants treated for 3 years with dietary modification. Nutr. Res. 33, 195–203 (2013).
Meydani, M., Das, S., Band, M., Epstein, S. & Roberts, S. The effect of caloric restriction and glycemic load on measures of oxidative stress and antioxidants in humans: results from the CALERIE Trial of Human Caloric Restriction. J. Nutr. Health Aging 15, 456–460 (2011).
Friedenreich, C. M. et al. Effects of exercise on markers of oxidative stress: an ancillary analysis of the Alberta Physical Activity and Breast Cancer Prevention Trial. BMJ Open Sport Exerc. Med. 2, e000171 (2016).
Repka, C. P. & Hayward, R. Oxidative stress and fitness changes in cancer patients after exercise training. Med. Sci. Sports Exerc. 48, 607–614 (2016).
Shimizu, I., Yoshida, Y., Suda, M. & Minamino, T. DNA damage response and metabolic disease. Cell Metab. 20, 967–977 (2014).
Habermann, N. et al. No effect of caloric restriction or exercise on radiation repair capacity. Med. Sci. Sports Exerc. 47, 896–904 (2015).
Mundstock, E. et al. Effect of obesity on telomere length: systematic review and meta-analysis. Obesity 23, 2165–2174 (2015).
Mason, C. et al. Independent and combined effects of dietary weight loss and exercise on leukocyte telomere length in postmenopausal women. Obesity 21, E549–E554 (2013).
Garcia-Calzon, S. et al. Telomere length as a biomarker for adiposity changes after a multidisciplinary intervention in overweight/obese adolescents: the EVASYON study. PLOS One 9, e89828 (2014).
Werner, C. et al. Physical exercise prevents cellular senescence in circulating leukocytes and in the vessel wall. Circulation 120, 2438–2447 (2009).
Turnbaugh, P. J. & Gordon, J. I. The core gut microbiome, energy balance and obesity. J. Physiol. 587, 4153–4158 (2009).
Aguirre, M., Bussolo de Souza, C. & Venema, K. The gut microbiota from lean and obese subjects contribute differently to the fermentation of arabinogalactan and inulin. PLOS One 11, e0159236 (2016).
Jakobsdottir, G., Xu, J., Molin, G., Ahrne, S. & Nyman, M. High-fat diet reduces the formation of butyrate, but increases succinate, inflammation, liver fat and cholesterol in rats, while dietary fibre counteracts these effects. PLOS One 8, e80476 (2013).
Le Chatelier, E. et al. Richness of human gut microbiome correlates with metabolic markers. Nature 500, 541–546 (2013).
Cani, P. D., Delzenne, N. M., Amar, J. & Burcelin, R. Role of gut microflora in the development of obesity and insulin resistance following high-fat diet feeding. Pathol. Biol. 56, 305–309 (2008).
Cani, P. D. et al. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia 50, 2374–2383 (2007).
Roager, H. M. et al. Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut https://doi.org/10.1136/gutjnl-2017-314786 (2017).
Djuric, Z. Obesity-associated cancer risk: the role of intestinal microbiota in the etiology of the host proinflammatory state. Transl Res. 179, 155–167 (2017).
Alang, N. & Kelly, C. R. Weight gain after fecal microbiota transplantation. Open Forum Infect. Dis. 2, ofv004 (2015).
Higgins, J. A. Resistant starch and energy balance: impact on weight loss and maintenance. Crit. Rev. Food Sci. Nutr. 54, 1158–1166 (2014).
Murphy, G. et al. Serum ghrelin is inversely associated with risk of subsequent oesophageal squamous cell carcinoma. Gut 61, 1533–1537 (2012).
de Martel, C. et al. Serum ghrelin levels and risk of subsequent adenocarcinoma of the esophagus. Am. J. Gastroenterol. 102, 1166–1172 (2007).
Hooper, L. E. et al. Frequent intentional weight loss is associated with higher ghrelin and lower glucose and androgen levels in postmenopausal women. Nutr. Res. 30, 163–170 (2010).
Cui, H., Lopez, M. & Rahmouni, K. The cellular and molecular bases of leptin and ghrelin resistance in obesity. Nat. Rev. Endocrinol. 13, 338–351 (2017).
Koelwyn, G. J., Wennerberg, E., Demaria, S. & Jones, L. W. Exercise in regulation of inflammation-immune axis function in cancer initiation and progression. Oncology (Williston Park) 29, 908–922 (2015).
Walsh, N. P. et al. Position statement. Part one: immune function and exercise. Exerc. Immunol. Rev. 17, 6–63 (2011).
Walsh, N. P. et al. Position statement. Part two: maintaining immune health. Exerc. Immunol. Rev. 17, 64–103 (2011).
Campbell, P. T. et al. Effect of exercise on in vitro immune function: a 12-month randomized, controlled trial among postmenopausal women. J. Appl. Physiol. 104, 1648–1655 (2008).
Nieman, D. C. et al. Immune response to exercise training and/or energy restriction in obese women. Med. Sci. Sports Exerc. 30, 679–686 (1998).
Martinez-Carrillo, B. E., Jarillo-Luna, R. A., Campos-Rodriguez, R., Valdes-Ramos, R. & Rivera-Aguilar, V. Effect of diet and exercise on the peripheral immune system in young Balb/c mice. Biomed. Res. Int. 2015, 458470 (2015).
Pollard, J. W. Trophic macrophages in development and disease. Nat. Rev. Immunol. 9, 259–270 (2009).
Catalan, V., Gomez-Ambrosi, J., Rodriguez, A. & Fruhbeck, G. Adipose tissue immunity and cancer. Front. Physiol. 4, 275 (2013).
Koelwyn, G. J., Quail, D. F., Zhang, X., White, R. M. & Jones, L. W. Exercise-dependent regulation of the tumour microenvironment. Nat. Rev. Cancer 17, 620–632 (2017).
Duffaut, C., Galitzky, J., Lafontan, M. & Bouloumie, A. Unexpected trafficking of immune cells within the adipose tissue during the onset of obesity. Biochem. Biophys. Res. Commun. 384, 482–485 (2009).
Michelotti, G. A., Machado, M. V. & Diehl, A. M. NAFLD. NASH and liver cancer. Nat. Rev. Gastroenterol. Hepatol. 10, 656–665 (2013).
Smart, N. A., King, N., McFarlane, J. R., Graham, P. L. & Dieberg, G. Effect of exercise training on liver function in adults who are overweight or exhibit fatty liver disease: a systematic review and meta-analysis. Br. J. Sports Med. 52, 834–843 (2016).
Goodpaster, B. H. et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA 304, 1795–1802 (2010).
Hallsworth, K. et al. Resistance exercise reduces liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Gut 60, 1278–1283 (2011).
Larson-Meyer, D. E. et al. Effect of 6-month calorie restriction and exercise on serum and liver lipids and markers of liver function. Obesity 16, 1355–1362 (2008).
Razavi Zade, M. et al. The effects of DASH diet on weight loss and metabolic status in adults with non-alcoholic fatty liver disease: a randomized clinical trial. Liver Int. 36, 563–571 (2016).
Zhang, H. J. et al. Effects of moderate and vigorous exercise on nonalcoholic fatty liver disease: a randomized clinical trial. JAMA Intern. Med. 176, 1074–1082 (2016).
Katsagoni, C. N., Georgoulis, M., Papatheodoridis, G. V., Panagiotakos, D. B. & Kontogianni, M. D. Effects of lifestyle interventions on clinical characteristics of patients with non-alcoholic fatty liver disease: a meta-analysis. Metabolism 68, 119–132 (2017).
Kenneally, S., Sier, J. H. & Moore, J. B. Efficacy of dietary and physical activity intervention in non-alcoholic fatty liver disease: a systematic review. BMJ Open Gastroenterol. 4, e000139 (2017).
Orci, L. A. et al. Exercise-based Interventions for nonalcoholic fatty liver disease: a meta-analysis and meta-regression. Clin. Gastroenterol. Hepatol. 14, 1398–1411 (2016).
Quante, M. & Wang, T. C. Stem cells in gastroenterology and hepatology. Nat. Rev. Gastroenterol. Hepatol. 6, 724–737 (2009).
Zeuner, A., Todaro, M., Stassi, G. & De Maria, R. Colorectal cancer stem cells: from the crypt to the clinic. Cell Stem Cell 15, 692–705 (2014).
Lee, C. J., Dosch, J. & Simeone, D. M. Pancreatic cancer stem cells. J. Clin. Oncol. 26, 2806–2812 (2008).
Takaishi, S., Okumura, T. & Wang, T. C. Gastric cancer stem cells. J. Clin. Oncol. 26, 2876–2882 (2008).
Sell, S. & Leffert, H. L. Liver cancer stem cells. J. Clin. Oncol. 26, 2800–2805 (2008).
Zheng, Q. et al. Leptin deficiency suppresses MMTV-Wnt-1 mammary tumor growth in obese mice and abrogates tumor initiating cell survival. Endocr. Relat. Cancer 18, 491–503 (2011).
Bellows, C. F., Zhang, Y., Simmons, P. J., Khalsa, A. S. & Kolonin, M. G. Influence of BMI on level of circulating progenitor cells. Obesity 19, 1722–1726 (2011).
Colditz, G. A. & Peterson, L. L. Obesity and cancer: evidence, impact, and future directions. Clin. Chem. 64, 154–162 (2018).
Acknowledgements
C.M.U. was supported by grants from the US National Institutes of Health (NIH)–US National Cancer Institute (NCI) (R01 CA189184, R01 CA207371 and U01 CA206110). C.M.U. and C.H. were also supported by NIH–NCI grant R01 CA211705. A.N.H. was supported by the NIH under Ruth L. Kirschstein National Research Service Award T32 HG008962 from the US National Human Genome Research Institute. S.D.H. was supported by NIH–NCI grant R35 CA197627.
Reviewer information
Nature Reviews Gastroenterology & Hepatology thanks N. Berger and other anonymous reviewer(s) for their contribution to the peer review of this work
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ulrich, C.M., Himbert, C., Holowatyj, A.N. et al. Energy balance and gastrointestinal cancer: risk, interventions, outcomes and mechanisms. Nat Rev Gastroenterol Hepatol 15, 683–698 (2018). https://doi.org/10.1038/s41575-018-0053-2
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-018-0053-2
This article is cited by
-
MIIP downregulation drives colorectal cancer progression through inducing peri-cancerous adipose tissue browning
Cell & Bioscience (2024)
-
Associations of combined physical activity and body mass index groups with colorectal cancer survival outcomes
BMC Cancer (2023)
-
A feasibility study to investigate the utility of a home-based exercise intervention during and after neo-adjuvant chemotherapy for oesophago-gastric cancer—the ChemoFit study protocol
Pilot and Feasibility Studies (2020)
-
Metabolomics profiling of visceral and abdominal subcutaneous adipose tissue in colorectal cancer patients: results from the ColoCare study
Cancer Causes & Control (2020)
-
Physical activity and risks of breast and colorectal cancer: a Mendelian randomisation analysis
Nature Communications (2020)