Abstract
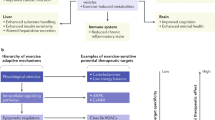
Circadian rhythms that influence mammalian homeostasis and overall health have received increasing interest over the past two decades. The molecular clock, which is present in almost every cell, drives circadian rhythms while being a cornerstone of physiological outcomes. The skeletal muscle clock has emerged as a primary contributor to metabolic health, as the coordinated expression of the core clock factors BMAL1 and CLOCK with the muscle-specific transcription factor MYOD1 facilitates the circadian and metabolic programme that supports skeletal muscle physiology. The phase of the skeletal muscle clock is sensitive to the time of exercise, which provides a rationale for exploring the interactions between the skeletal muscle clock, exercise and metabolic health. Here, we review the underlying mechanisms of the skeletal muscle clock that drive muscle physiology, with a particular focus on metabolic health. Additionally, we highlight the interaction between exercise and the skeletal muscle clock as a means of reinforcing metabolic health and discuss the possible implications of the time of exercise as a chronotherapeutic approach.
Key points
-
The BMAL1–CLOCK heterodimeric transcription factor is a key regulator of clock output; partnership with MYOD1 confers muscle specificity.
-
Skeletal muscle substrate preference, storage and transport are highly regulated by the skeletal muscle molecular clock, aligning metabolism with physical activity and feeding patterns.
-
Mice with knockouts and mutations that affect the circadian clock, and behavioural misalignment in humans, as occurs in metabolic disorders such as type 2 diabetes mellitus, have severe metabolic consequences that affect insulin sensitivity and glucose handling.
-
Exercise is a potent Zeitgeber that acts to shift skeletal muscle clocks; exercising at different times of the day results in divergent transcriptional and metabolic outputs.
-
Differential time-of-day exercise might prove to be a useful chronotherapeutic strategy for the treatment and management of metabolic diseases by improving clock alignment and therefore metabolic regulation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Zhang, R., Lahens, N. F., Ballance, H. I., Hughes, M. E. & Hogenesch, J. B. A circadian gene expression atlas in mammals: implications for biology and medicine. Proc. Natl Acad. Sci. USA 111, 16219–16224 (2014).
Vitaterna, M. H., Takahashi, J. S. & Turek, F. W. Overview of circadian rhythms. Alcohol Res. Health 25, 85–93 (2001).
Ko, C. H. & Takahashi, J. S. Molecular components of the mammalian circadian clock. Hum. Mol. Genet. 15, R271–R277 (2006).
Cox, K. H. & Takahashi, J. S. Circadian clock genes and the transcriptional architecture of the clock mechanism. J. Mol. Endocrinol. 63, R93–R102 (2019).
Bunger, M. K. et al. Mop3 is an essential component of the master circadian pacemaker in mammals. Cell 103, 1009–1017 (2000).
Gekakis, N. et al. Role of the CLOCK protein in the mammalian circadian mechanism. Science 280, 1564–1569 (1998).
King, D. P. et al. Positional cloning of the mouse circadian clock gene. Cell 89, 641–653 (1997).
Akashi, M., Tsuchiya, Y., Yoshino, T. & Nishida, E. Control of intracellular dynamics of mammalian period proteins by casein kinase I ε (CKIε) and CKIδ in cultured cells. Mol. Cell. Biol. 22, 1693–1703 (2002).
Camacho, F. et al. Human casein kinase Iδ phosphorylation of human circadian clock proteins period 1 and 2. FEBS Lett. 489, 159–165 (2001).
Eide, E. J., Vielhaber, E. L., Hinz, W. A. & Virshup, D. M. The circadian regulatory proteins BMAL1 and cryptochromes are substrates of casein kinase Iε. J. Biol. Chem. 277, 17248–17254 (2002).
Etchegaray, J.-P. et al. Casein kinase 1 delta regulates the pace of the mammalian circadian clock. Mol. Cell Biol. 29, 3853–3866 (2009).
Akashi, M. & Takumi, T. The orphan nuclear receptor RORα regulates circadian transcription of the mammalian core-clock Bmal1. Nat. Struct. Mol. Biol. 12, 441–448 (2005).
Guillaumond, F., Dardente, H., Giguère, V. & Cermakian, N. Differential control of Bmal1 circadian transcription by REV-ERB and ROR nuclear receptors. J. Biol. Rhythms 20, 391–403 (2005).
Lee, C., Weaver, D. R. & Reppert, S. M. Direct association between mouse PERIOD and CKIε is critical for a functioning circadian clock. Mol. Cell Biol. 24, 584–594 (2004).
Xu, Y. et al. Modeling of a human circadian mutation yields insights into clock regulation by PER2. Cell 128, 59–70 (2007).
Reischl, S. et al. β-TrCP1-mediated degradation of PERIOD2 is essential for circadian dynamics. J. Biol. Rhythms 22, 375–386 (2007).
Wu, G. et al. Structure of a β-TrCP1-Skp1-β-catenin complex: destruction motif binding and lysine specificity of the SCFβ-TrCP1 ubiquitin ligase. Mol. Cell 11, 1445–1456 (2003).
Ohsaki, K. et al. The role of β-TrCP1 and β-TrCP2 in circadian rhythm generation by mediating degradation of clock protein PER2. J. Biochem. 144, 609–618 (2008).
Meng, Q.-J. et al. Setting clock speed in mammals: the CK1ɛ tau mutation in mice accelerates circadian pacemakers by selectively destabilizing PERIOD proteins. Neuron 58, 78–88 (2008).
Busino, L. et al. SCF Fbxl3 controls the oscillation of the circadian clock by directing the degradation of cryptochrome proteins. Science 316, 900–904 (2007).
Lamia, K. A. et al. AMPK regulates the circadian clock by cryptochrome phosphorylation and degradation. Science 326, 437–440 (2009).
Hirano, A. et al. FBXL21 regulates oscillation of the circadian clock through ubiquitination and stabilization of cryptochromes. Cell 152, 1106–1118 (2013).
Hirano, A., Fu, Y.-H. & Ptáček, L. J. The intricate dance of post-translational modifications in the rhythm of life. Nat. Struct. Mol. Biol. 23, 1053–1060 (2016).
Wheaton, K. L. et al. The phosphorylation of CREB at serine 133 is a key event for circadian clock timing and entrainment in the suprachiasmatic nucleus. J. Biol. Rhythms 33, 497–514 (2018).
Gau, D. et al. Phosphorylation of CREB Ser142 regulates light-induced phase shifts of the circadian clock. Neuron 34, 245–253 (2002).
Travnickova-Bendova, Z., Cermakian, N., Reppert, S. M. & Sassone-Corsi, P. Bimodal regulation of mPeriod promoters by CREB-dependent signaling and CLOCK/BMAL1 activity. Proc. Natl Acad. Sci. USA 99, 7728–7733 (2002).
Impey, S. et al. Defining the CREB regulon: a genome-wide analysis of transcription factor regulatory regions. Cell 119, 1041–1054 (2004).
Tischkau, S. A., Mitchell, J. W., Tyan, S.-H., Buchanan, G. F. & Gillette, M. U. Ca2+/cAMP response element-binding protein (CREB)-dependent activation of Per1 is required for light-induced signaling in the suprachiasmatic nucleus circadian clock. J. Biol. Chem. 278, 718–723 (2003).
Small, L. et al. Contraction influences Per2 gene expression in skeletal muscle through a calcium‐dependent pathway. J. Physiol. 598, 5739–5752 (2020).
Wolff, C. A. & Esser, K. A. Exercise sets the muscle clock with a calcium assist. J. Physiol. 598, 5591–5592 (2020).
Gabriel, B. M. et al. Disrupted circadian oscillations in type 2 diabetes are linked to altered rhythmic mitochondrial metabolism in skeletal muscle. Sci. Adv. 7, eabi9654 (2021).
Koike, N. et al. Transcriptional architecture and chromatin landscape of the core circadian clock in mammals. Science 338, 349–354 (2012).
Menet, J. S., Rodriguez, J., Abruzzi, K. C. & Rosbash, M. Nascent-Seq reveals novel features of mouse circadian transcriptional regulation. eLife 1, e00011 (2012).
Davis, R., Weintraub, H. & Lassar, A. Expression of a single transfected cDNA converts fibroblasts to myoblasts. Cell 51, 987–1000 (1988).
Miller, B. H. et al. Circadian and CLOCK-controlled regulation of the mouse transcriptome and cell proliferation. Proc. Natl Acad. Sci. USA 104, 3342–3347 (2007).
Andrews, J. L. et al. CLOCK and BMAL1 regulate MyoD and are necessary for maintenance of skeletal muscle phenotype and function. Proc. Natl Acad. Sci. USA 107, 19090–19095 (2010).
Hodge, B. A. et al. MYOD1 functions as a clock amplifier as well as a critical co-factor for downstream circadian gene expression in muscle. eLife 8, e43017 (2019).
Dyar, K. A. et al. The calcineurin-NFAT pathway controls activity-dependent circadian gene expression in slow skeletal muscle. Mol. Metab. 4, 823–833 (2015).
Pizarro, A., Hayer, K., Lahens, N. F. & Hogenesch, J. B. CircaDB: a database of mammalian circadian gene expression profiles. Nucleic Acids Res. 41, D1009–D1013 (2012).
Gutierrez‐Monreal, M. A., Harmsen, J., Schrauwen, P. & Esser, K. A. Ticking for metabolic health: the skeletal‐muscle clocks. Obesity 28(Suppl. 1), 46–54 (2020).
Perrin, L. et al. Transcriptomic analyses reveal rhythmic and CLOCK-driven pathways in human skeletal muscle. eLife 7, e34114 (2018).
Rey, G. et al. Genome-wide and phase-specific DNA-binding rhythms of BMAL1 control circadian output functions in mouse liver. PLoS Biol. 9, e1000595 (2011).
Dai, Z., Ramesh, V. & Locasale, J. W. The evolving metabolic landscape of chromatin biology and epigenetics. Nat. Rev. Genet. 21, 737–753 (2020).
Grimaldi, B. et al. Chromatin remodeling and circadian control: master regulator CLOCK is an enzyme. Cold Spring Harb. Symp. Quant. Biol. 72, 105–112 (2007).
Katada, S. & Sassone-Corsi, P. The histone methyltransferase MLL1 permits the oscillation of circadian gene expression. Nat. Struct. Mol. Biol. 17, 1414–1421 (2010).
Zhu, H., Wang, G. & Qian, J. Transcription factors as readers and effectors of DNA methylation. Nat. Rev. Genet. 17, 551–565 (2016).
Menet, J. S., Pescatore, S. & Rosbash, M. CLOCK:BMAL1 is a pioneer-like transcription factor. Genes Dev. 28, 8–13 (2014).
Petrany, M. J. et al. Single-nucleus RNA-seq identifies transcriptional heterogeneity in multinucleated skeletal myofibers. Nat. Commun. 11, 6374 (2020).
Dos Santos, M. et al. Single-nucleus RNA-seq and FISH identify coordinated transcriptional activity in mammalian myofibers. Nat. Commun. 11, 5102 (2020).
Kim, M. et al. Single-nucleus transcriptomics reveals functional compartmentalization in syncytial skeletal muscle cells. Nat. Commun. 11, 6375 (2020).
Zeng, W. et al. Single-nucleus RNA-seq of differentiating human myoblasts reveals the extent of fate heterogeneity. Nucleic Acids Res. 44, e158 (2016).
Zitting, K.-M. et al. Human resting energy expenditure varies with circadian phase. Curr. Biol. 28, 3685–3690.e3 (2018).
Harmsen, J. et al. Circadian misalignment disturbs the skeletal muscle lipidome in healthy young men. FASEB J. 35, e21611 (2021).
Wefers, J. et al. Circadian misalignment induces fatty acid metabolism gene profiles and compromises insulin sensitivity in human skeletal muscle. Proc. Natl Acad. Sci. USA 115, 7789–7794 (2018).
Morris, C. J. et al. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc. Natl Acad. Sci. USA 112, E2225–E2234 (2015).
Morris, J. K. et al. Mild cognitive impairment and donepezil impact mitochondrial respiratory capacity in skeletal muscle. Function 2, zqab045 (2021).
Hodge, B. A. et al. The endogenous molecular clock orchestrates the temporal separation of substrate metabolism in skeletal muscle. Skelet. Muscle 5, 17 (2015).
Ezagouri, S. et al. Physiological and molecular dissection of daily variance in exercise capacity. Cell Metab. 30, 78–91.e4 (2019).
Harfmann, B. D. et al. Muscle-specific loss of Bmal1 leads to disrupted tissue glucose metabolism and systemic glucose homeostasis. Skelet. Muscle 6, 12 (2016).
Yin, H. et al. Metabolic‐sensing of the skeletal muscle clock coordinates fuel oxidation. FASEB J. 34, 6613–6627 (2020).
Dyar, K. A. et al. Muscle insulin sensitivity and glucose metabolism are controlled by the intrinsic muscle clock. Mol. Metab. 3, 29–41 (2014).
McCarthy, J. J. et al. Identification of the circadian transcriptome in adult mouse skeletal muscle. Physiol. Genomics 31, 86–95 (2007).
van Moorsel, D. et al. Demonstration of a day-night rhythm in human skeletal muscle oxidative capacity. Mol. Metab. 5, 635–645 (2016).
de Goede, P. et al. Time-restricted feeding improves glucose tolerance in rats, but only when in line with the circadian timing system. Front. Endocrinol. 10, 554 (2019).
de Goede, P. et al. Differential effects of diet composition and timing of feeding behavior on rat brown adipose tissue and skeletal muscle peripheral clocks. Neurobiol. Sleep Circadian Rhythms 4, 24–33 (2018).
Lamia, K. A., Storch, K.-F. & Weitz, C. J. Physiological significance of a peripheral tissue circadian clock. Proc. Natl Acad. Sci. USA 105, 15172–15177 (2008).
Kondratov, R. V., Kondratova, A. A., Gorbacheva, V. Y., Vykhovanets, O. V. & Antoch, M. P. Early aging and age-related pathologies in mice deficient in BMAL1, the core component of the circadian clock. Genes Dev. 20, 1868–1873 (2006).
Dyar, K. A. et al. Transcriptional programming of lipid and amino acid metabolism by the skeletal muscle circadian clock. PLoS Biol. 16, e2005886 (2018).
Schroder, E. A. et al. Intrinsic muscle clock is necessary for musculoskeletal health. J. Physiol. 593, 5387–5404 (2015).
Lee, S. & Dong, H. H. FoxO integration of insulin signaling with glucose and lipid metabolism. J. Endocrinol. 233, R67–R79 (2017).
Karanth, S. et al. FOXN3 controls liver glucose metabolism by regulating gluconeogenic substrate selection. Physiol. Rep. 7, e14238 (2019).
Bruno, N. E. et al. Creb coactivators direct anabolic responses and enhance performance of skeletal muscle. EMBO J. 33, 1027–1043 (2014).
Bruno, N. E. et al. Activation of Crtc2/Creb1 in skeletal muscle enhances weight loss during intermittent fasting. FASEB J. 35, e21999 (2021).
Pillon, N. J. et al. Transcriptomic profiling of skeletal muscle adaptations to exercise and inactivity. Nat. Commun. 11, 470 (2020).
Pastore, S. & Hood, D. A. Endurance training ameliorates the metabolic and performance characteristics of circadian Clock mutant mice. J. Appl. Physiol. 114, 1076–1084 (2013).
Bae, K. et al. Differential effects of two period genes on the physiology and proteomic profiles of mouse anterior tibialis muscles. Mol. Cell 22, 275–284 (2006).
Woldt, E. et al. Rev-erb-α modulates skeletal muscle oxidative capacity by regulating mitochondrial biogenesis and autophagy. Nat. Med. 19, 1039–1046 (2013).
Jordan, S. D. et al. CRY1/2 selectively repress PPARδ and limit exercise capacity. Cell Metab. 26, 243–255.e6 (2017).
Fan, W. et al. PPARδ promotes running endurance by preserving glucose. Cell Metab. 25, 1186–1193.e4 (2017).
Yamamoto, H. et al. NCoR1 is a conserved physiological modulator of muscle mass and oxidative function. Cell 147, 827–839 (2011).
Marcheva, B. et al. Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 466, 627–631 (2010).
Loizides-Mangold, U. et al. Lipidomics reveals diurnal lipid oscillations in human skeletal muscle persisting in cellular myotubes cultured in vitro. Proc. Natl Acad. Sci. USA 114, E8565–E8574 (2017).
Dibner, C. The importance of being rhythmic: living in harmony with your body clocks. Acta Physiol. 228, e13281 (2020).
Vetter, C. Circadian disruption: what do we actually mean? Eur. J. Neurosci. 51, 531–550 (2020).
Harmsen, J.-F. et al. The influence of bright and dim light on substrate metabolism, energy expenditure and thermoregulation in insulin-resistant individuals depends on time of day. Diabetologia 65, 721–732 (2022).
Morris, C. J., Purvis, T. E., Mistretta, J. & Scheer, F. A. J. L. Effects of the internal circadian system and circadian misalignment on glucose tolerance in chronic shift workers. J. Clin. Endocrinol. Metab. 101, 1066–1074 (2016).
Qian, J. & Scheer, F. A. Circadian system and glucose metabolism: implications for physiology and disease. Trends Endocrinol. Metab. 27, 282–293 (2016).
Scheer, F. A. J. L., Hilton, M. F., Mantzoros, C. S. & Shea, S. A. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc. Natl Acad. Sci. USA 106, 4453–4458 (2009).
Eckel, R. H. et al. Morning circadian misalignment during short sleep duration impacts insulin sensitivity. Curr. Biol. 25, 3004–3010 (2015).
Karthikeyan, R. et al. Should we listen to our clock to prevent type 2 diabetes mellitus? Diabetes Res. Clin. Pract. 106, 182–190 (2014).
Hansen, J. et al. Synchronized human skeletal myotubes of lean, obese and type 2 diabetic patients maintain circadian oscillation of clock genes. Sci. Rep. 6, 35047 (2016).
Cardinali, D. P., Brown, G. M. & Pandi-Perumal, S. R. in The Human Hypothalamus: Anterior Region Handbook of Clinical Neurology series vol. 179 (eds Swaab, D. F., Kreier, F., Lucassen, P. J., Salehe, A. & Buijs, R. M.) 357–370 (Elsevier, 2021).
Lee, Y., Field, J. M. & Sehgal, A. Circadian rhythms, disease and chronotherapy. J. Biol. Rhythms 36, 503–531 (2021).
Ruan, W., Yuan, X. & Eltzschig, H. K. Circadian rhythm as a therapeutic target. Nat. Rev. Drug. Discov. 20, 287–307 (2021).
Yoo, S.-H. et al. PERIOD2: LUCIFERASE real-time reporting of circadian dynamics reveals persistent circadian oscillations in mouse peripheral tissues. Proc. Natl Acad. Sci. USA 101, 5339–5346 (2004).
Wolff, G. & Esser, K. A. Scheduled exercise phase shifts the circadian clock in skeletal muscle. Med. Sci. Sports Exerc. 44, 1663–1670 (2012).
Kemler, D., Wolff, C. A. & Esser, K. A. Time‐of‐day dependent effects of contractile activity on the phase of the skeletal muscle clock. J. Physiol. 598, 3631–3644 (2020).
Adamovich, Y. et al. Clock proteins and training modify exercise capacity in a daytime-dependent manner. Proc. Natl Acad. Sci. USA 118, e2101115118 (2021).
Hoffman, N. J. et al. Global phosphoproteomic analysis of human skeletal muscle reveals a network of exercise-regulated kinases and AMPK substrates. Cell Metab. 22, 922–935 (2015).
Vieira, E. et al. Relationship between AMPK and the transcriptional balance of clock-related genes in skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 295, E1032–E1037 (2008).
Casanova-Vallve, N. et al. Daily running enhances molecular and physiological circadian rhythms in skeletal muscle. Mol. Metab. 61, 101504 (2022).
Sato, S. et al. Time of exercise specifies the impact on muscle metabolic pathways and systemic energy homeostasis. Cell Metab. 30, 92–110.e4 (2019).
Hawley, J. A., Sassone-Corsi, P. & Zierath, J. R. Chrono-nutrition for the prevention and treatment of obesity and type 2 diabetes: from mice to men. Diabetologia 63, 2253–2259 (2020).
Savikj, M. et al. Afternoon exercise is more efficacious than morning exercise at improving blood glucose levels in individuals with type 2 diabetes: a randomised crossover trial. Diabetologia 62, 233–237 (2019).
Savikj, M. et al. Exercise timing influences multi-tissue metabolome and skeletal muscle proteome profiles in type 2 diabetic patients — a randomized crossover trial. Metabolism 135, 155268 (2022).
Moholdt, T. et al. The effect of morning vs evening exercise training on glycaemic control and serum metabolites in overweight/obese men: a randomised trial. Diabetologia 64, 2061–2076 (2021).
Mancilla, R. et al. Exercise training elicits superior metabolic effects when performed in the afternoon compared to morning in metabolically compromised humans. Physiol. Rep. 8, e14669 (2021).
Acknowledgements
The authors acknowledge the support of NIH grants U01AG055137 and R01AR079220 to K.A.E. The authors also thank L. Denes, Institute for Systems Genetics, New York, for kindly providing the image of the myofibre in Fig. 4b.
Author information
Authors and Affiliations
Contributions
R.A.M. and M.R.V. researched data for the article. R.A.M, M.R.V and K.A.E. contributed substantially to discussion of the content, wrote the article and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks Charna Dibner, Ke Ma and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martin, R.A., Viggars, M.R. & Esser, K.A. Metabolism and exercise: the skeletal muscle clock takes centre stage. Nat Rev Endocrinol 19, 272–284 (2023). https://doi.org/10.1038/s41574-023-00805-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-023-00805-8
This article is cited by
-
Exercise metabolism and adaptation in skeletal muscle
Nature Reviews Molecular Cell Biology (2023)