Abstract
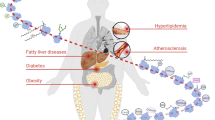
Insulin, which is released by pancreatic islet β-cells in response to elevated levels of glucose in the blood, is a critical regulator of metabolism. Insulin triggers the uptake of glucose and fatty acids into the liver, adipose tissue and muscle, and promotes the storage of these nutrients in the form of glycogen and lipids. Dysregulation of insulin synthesis, secretion, transport, degradation or signal transduction all cause failure to take up and store nutrients, resulting in type 1 diabetes mellitus, type 2 diabetes mellitus and metabolic dysfunction. In this Review, we make the case that insulin signalling is intimately coupled to protein S-nitrosylation, in which nitric oxide groups are conjugated to cysteine thiols to form S-nitrosothiols, within effectors of insulin action. We discuss the role of S-nitrosylation in the life cycle of insulin, from its synthesis and secretion in pancreatic β-cells, to its signalling and degradation in target tissues. Finally, we consider how aberrant S-nitrosylation contributes to metabolic diseases, including the roles of human genetic mutations and cellular events that alter S-nitrosylation of insulin-regulating proteins. Given the growing influence of S-nitrosylation in cellular metabolism, the field of metabolic signalling could benefit from renewed focus on S-nitrosylation in type 2 diabetes mellitus and insulin-related disorders.
Key points
-
Post-translational modification of insulin signalling proteins by S-nitrosylation is an under-appreciated, but widely used, control mechanism in health and disease.
-
S-nitrosylation of ion channels and exocytotic machinery regulates insulin secretion from pancreatic β-cells.
-
S-nitrosylation of the insulin receptor and its signalling partners modulates insulin sensitivity in normal health.
-
Obesity-driven insulin resistance is associated with increased S-nitrosylation of insulin signalling proteins.
-
Cellular stress-driven insulin resistance is associated with increased S-nitrosylation of stress response proteins.
-
Modulation of the S-nitrosylation state of many insulin-regulatory proteins might provide novel therapeutic opportunities in metabolic disorders and diabetes mellitus.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Sonksen, P. & Sonksen, J. Insulin: understanding its action in health and disease. Br. J. Anaesth. 85, 69–79 (2000).
Fu, Z., Gilbert, E. R. & Liu, D. Regulation of insulin synthesis and secretion and pancreatic beta-cell dysfunction in diabetes. Curr. Diabetes Rev. 9, 25–53 (2013).
Saklayen, M. G. The global epidemic of the metabolic syndrome. Curr. Hypertens. Rep. 20, 12 (2018).
Bahadoran, Z., Mirmiran, P. & Ghasemi, A. Role of nitric oxide in insulin secretion and glucose metabolism. Trends Endocrinol. Metab. 31, 118–130 (2020).
Knowles, R. G. & Moncada, S. Nitric oxide synthases in mammals. Biochem. J. 298, 249–258 (1994).
Shankar, R. R., Wu, Y., Shen, H. Q., Zhu, J. S. & Baron, A. D. Mice with gene disruption of both endothelial and neuronal nitric oxide synthase exhibit insulin resistance. Diabetes 49, 684–687 (2000).
Kurohane Kaneko, Y. & Ishikawa, T. Dual role of nitric oxide in pancreatic β-cells. J. Pharmacol. Sci. 123, 295–300 (2013).
Perreault, M. & Marette, A. Targeted disruption of inducible nitric oxide synthase protects against obesity-linked insulin resistance in muscle. Nat. Med. 7, 1138–1143 (2001).
Denninger, J. W. & Marletta, M. A. Guanylate cyclase and the ·NO/cGMP signaling pathway. Biochim. Biophys. Acta 1411, 334–350 (1999).
Hess, D. T., Matsumoto, A., Kim, S. O., Marshall, H. E. & Stamler, J. S. Protein S-nitrosylation: purview and parameters. Nat. Rev. Mol. Cell Biol. 6, 150–166 (2005).
Sansbury, B. E. & Hill, B. G. Regulation of obesity and insulin resistance by nitric oxide. Free Radic. Biol. Med. 73, 383–399 (2014).
Li, S. et al. pCysMod: prediction of multiple cysteine modifications based on deep learning framework. Front. Cell Dev. Biol. 9, 617366 (2021).
Abunimer, A. et al. Single-nucleotide variations in cardiac arrhythmias: prospects for genomics and proteomics based biomarker discovery and diagnostics. Genes (Basel) 5, 254–269 (2014).
Seth, D. et al. A multiplex enzymatic machinery for cellular protein S-nitrosylation. Mol. Cell 69, e6 (2018).
Stomberski, C. T., Hess, D. T. & Stamler, J. S. Protein S-nitrosylation: determinants of specificity and enzymatic regulation of S-nitrosothiol-based signaling. Antioxid. Redox Signal. 30, 1331–1351 (2019).
Zhou, H. L. et al. Metabolic reprogramming by the S-nitroso-CoA reductase system protects against kidney injury. Nature 565, 96–100 (2019).
Stomberski, C. T., Zhou, H. L., Wang, L., van den Akker, F. & Stamler, J. S. Molecular recognition of S-nitrosothiol substrate by its cognate protein denitrosylase. J. Biol. Chem. 294, 1568–1578 (2019).
Weiss, M., Steiner, D. F. & Philipson, L. H. Insulin biosynthesis, secretion, structure, and structure-activity relationships (Endotext [Internet]. MDText.com, Inc., 2014).
Komatsu, M., Takei, M., Ishii, H. & Sato, Y. Glucose-stimulated insulin secretion: a newer perspective. J. Diabetes Investig. 4, 511–516 (2013).
Gaisano, H. Y. Recent new insights into the role of SNARE and associated proteins in insulin granule exocytosis. Diabetes Obes. Metab. 19, 115–123 (2017).
Byrne, M. M. et al. Insulin secretory abnormalities in subjects with hyperglycemia due to glucokinase mutations. J. Clin. Invest. 93, 1120–1130 (1994).
Cherrington, A. D., Sindelar, D., Edgerton, D., Steiner, K. & McGuinness, O. P. Physiological consequences of phasic insulin release in the normal animal. Diabetes 51, S103–S108 (2002).
Smukler, S. R., Tang, L., Wheeler, M. B. & Salapatek, A. M. Exogenous nitric oxide and endogenous glucose-stimulated β-cell nitric oxide augment insulin release. Diabetes 51, 3450–3460 (2002).
Rizzo, M. A. & Piston, D. W. Regulation of β cell glucokinase by S-nitrosylation and association with nitric oxide synthase. J. Cell Biol. 161, 243–248 (2003).
Gonzalez, D. R., Beigi, F., Treuer, A. V. & Hare, J. M. Deficient ryanodine receptor S-nitrosylation increases sarcoplasmic reticulum calcium leak and arrhythmogenesis in cardiomyocytes. Proc. Natl Acad. Sci. USA 104, 20612–20617 (2007).
Kawano, T. et al. Nitric oxide activates ATP-sensitive potassium channels in mammalian sensory neurons: action by direct S-nitrosylation. Mol. Pain. 5, 12 (2009).
Palmer, Z. J. et al. S-nitrosylation of syntaxin 1 at Cys(145) is a regulatory switch controlling Munc18-1 binding. Biochem. J. 413, 479–491 (2008).
Wiseman, D. A., Kalwat, M. A. & Thurmond, D. C. Stimulus-induced S-nitrosylation of syntaxin 4 impacts insulin granule exocytosis. J. Biol. Chem. 286, 16344–16354 (2011).
Matsushita, K. et al. Nitric oxide regulates exocytosis by S-nitrosylation of N-ethylmaleimide-sensitive factor. Cell 115, 139–150 (2003).
Ferre, T., Riu, E., Bosch, F. & Valera, A. Evidence from transgenic mice that glucokinase is rate limiting for glucose utilization in the liver. FASEB J. 10, 1213–1218 (1996).
Tarasov, A., Dusonchet, J. & Ashcroft, F. Metabolic regulation of the pancreatic beta-cell ATP-sensitive K+ channel: a pas de deux. Diabetes 53, S113–S122 (2004).
Roder, P. V., Wu, B., Liu, Y. & Han, W. Pancreatic regulation of glucose homeostasis. Exp. Mol. Med. 48, e219 (2016).
Postic, C. et al. Dual roles for glucokinase in glucose homeostasis as determined by liver and pancreatic β cell-specific gene knock-outs using Cre recombinase. J. Biol. Chem. 274, 305–315 (1999).
Matschinsky, F. M. Regulation of pancreatic β-cell glucokinase: from basics to therapeutics. Diabetes 51, S394–S404 (2002).
Rizzo, M. A., Magnuson, M. A., Drain, P. F. & Piston, D. W. A functional link between glucokinase binding to insulin granules and conformational alterations in response to glucose and insulin. J. Biol. Chem. 277, 34168–34175 (2002).
Stubbs, M., Aiston, S. & Agius, L. Subcellular localization, mobility, and kinetic activity of glucokinase in glucose-responsive insulin-secreting cells. Diabetes 49, 2048–2055 (2000).
Ding, S. Y. et al. Naturally occurring glucokinase mutations are associated with defects in posttranslational S-nitrosylation. Mol. Endocrinol. 24, 171–177 (2010).
Markwardt, M. L., Nkobena, A., Ding, S. Y. & Rizzo, M. A. Association with nitric oxide synthase on insulin secretory granules regulates glucokinase protein levels. Mol. Endocrinol. 26, 1617–1629 (2012).
Miller, S. P. et al. Characterization of glucokinase mutations associated with maturity-onset diabetes of the young type 2 (MODY-2): different glucokinase defects lead to a common phenotype. Diabetes 48, 1645–1651 (1999).
Holst, J. J. & Gromada, J. Role of incretin hormones in the regulation of insulin secretion in diabetic and nondiabetic humans. Am. J. Physiol. Endocrinol. Metab. 287, E199–E206 (2004).
Müller, T. D. et al. Glucagon-like peptide 1 (GLP-1). Mol. Metab. 30, 72–130 (2019).
Ding, S. Y., Nkobena, A., Kraft, C. A., Markwardt, M. L. & Rizzo, M. A. Glucagon-like peptide 1 stimulates post-translational activation of glucokinase in pancreatic β cells. J. Biol. Chem. 286, 16768–16774 (2011).
Bjorkhaug, L., Molnes, J., Sovik, O., Njolstad, P. R. & Flatmark, T. Allosteric activation of human glucokinase by free polyubiquitin chains and its ubiquitin-dependent cotranslational proteasomal degradation. J. Biol. Chem. 282, 22757–22764 (2007).
Tiedge, M., Richter, T. & Lenzen, S. Importance of cysteine residues for the stability and catalytic activity of human pancreatic beta cell glucokinase. Arch. Biochem. Biophys. 375, 251–260 (2000).
Graves, T. K. & Hinkle, P. M. Ca(2+)-induced Ca(2+) release in the pancreatic β-cell: direct evidence of endoplasmic reticulum Ca(2+) release. Endocrinology 144, 3565–3574 (2003).
Johnson, J. D., Kuang, S., Misler, S. & Polonsky, K. S. Ryanodine receptors in human pancreatic β cells: localization and effects on insulin secretion. FASEB J. 18, 878–880 (2004).
Dixit, S. S. et al. Effects of CaMKII-mediated phosphorylation of ryanodine receptor type 2 on islet calcium handling, insulin secretion, and glucose tolerance. PLoS ONE 8, e58655 (2013).
Santulli, G. et al. Calcium release channel RyR2 regulates insulin release and glucose homeostasis. J. Clin. Invest. 125, 4316 (2015).
Llanos, P. et al. Glucose-dependent insulin secretion in pancreatic β-cell islets from male rats requires Ca2+ release via ROS-stimulated ryanodine receptors. PLoS ONE 10, e0129238 (2015).
Sun, J. et al. Regulation of the cardiac muscle ryanodine receptor by O(2) tension and S-nitrosoglutathione. Biochemistry 47, 13985–13990 (2008).
Pipatpolkai, T., Usher, S., Stansfeld, P. J. & Ashcroft, F. M. New insights into KATP channel gene mutations and neonatal diabetes mellitus. Nat. Rev. Endocrinol. 16, 378–393 (2020).
Li, N. et al. Structure of a pancreatic ATP-sensitive potassium channel. Cell 168, 101–110.e10 (2017).
Aittoniemi, J. et al. Review. SUR1: a unique ATP-binding cassette protein that functions as an ion channel regulator. Philos. Trans. R. Soc. Lond. B Biol. Sci. 364, 257–267 (2009).
Aquilante, C. L. Sulfonylurea pharmacogenomics in type 2 diabetes: the influence of drug target and diabetes risk polymorphisms. Expert Rev. Cardiovasc. Ther. 8, 359–372 (2010).
Nichols, C. G. KATP channels as molecular sensors of cellular metabolism. Nature 440, 470–476 (2006).
Jewell, J. L., Oh, E. & Thurmond, D. C. Exocytosis mechanisms underlying insulin release and glucose uptake: conserved roles for Munc18c and syntaxin 4. Am. J. Physiol. Regul. Integr. Comp. Physiol. 298, R517–R531 (2010).
Hou, J. C., Min, L. & Pessin, J. E. Insulin granule biogenesis, trafficking and exocytosis. Vitam. Horm. 80, 473–506 (2009).
Kasai, H., Takahashi, N. & Tokumaru, H. Distinct initial SNARE configurations underlying the diversity of exocytosis. Physiol. Rev. 92, 1915–1964 (2012).
Yang, B., Steegmaier, M., Gonzalez, L. C. Jr & Scheller, R. H. nSec1 binds a closed conformation of syntaxin1A. J. Cell Biol. 148, 247–252 (2000).
Hardy, O. T., Czech, M. P. & Corvera, S. What causes the insulin resistance underlying obesity? Curr. Opin. Endocrinol. Diabetes Obes. 19, 81–87 (2012).
Henningsson, R., Salehi, A. & Lundquist, I. Role of nitric oxide synthase isoforms in glucose-stimulated insulin release. Am. J. Physiol. Cell Physiol. 283, C296–C304 (2002).
Muhammed, S. J., Lundquist, I. & Salehi, A. Pancreatic β-cell dysfunction, expression of iNOS and the effect of phosphodiesterase inhibitors in human pancreatic islets of type 2 diabetes. Diabetes Obes. Metab. 14, 1010–1019 (2012).
Zhao, C., Smith, E. C. & Whiteheart, S. W. Requirements for the catalytic cycle of the N-ethylmaleimide-sensitive factor (NSF). Biochim. Biophys. Acta 1823, 159–171 (2012).
Morrell, C. N. et al. Regulation of platelet granule exocytosis by S-nitrosylation. Proc. Natl Acad. Sci. USA 102, 3782–3787 (2005).
Ito, T., Yamakuchi, M. & Lowenstein, C. J. Thioredoxin increases exocytosis by denitrosylating N-ethylmaleimide-sensitive factor. J. Biol. Chem. 286, 11179–11184 (2011).
Yazdani, S., Jaldin-Fincati, J. R., Pereira, R. V. S. & Klip, A. Endothelial cell barriers: transport of molecules between blood and tissues. Traffic 20, 390–403 (2019).
Barrett, E. J., Wang, H., Upchurch, C. T. & Liu, Z. Insulin regulates its own delivery to skeletal muscle by feed-forward actions on the vasculature. Am. J. Physiol. Endocrinol. Metab. 301, E252–E263 (2011).
Wang, H., Wang, A. X., Aylor, K. & Barrett, E. J. Nitric oxide directly promotes vascular endothelial insulin transport. Diabetes 62, 4030–4042 (2013).
Wang, H., Wang, A. X., Liu, Z. & Barrett, E. J. Insulin signaling stimulates insulin transport by bovine aortic endothelial cells. Diabetes 57, 540–547 (2008).
Wang, H., Wang, A. X. & Barrett, E. J. Caveolin-1 is required for vascular endothelial insulin uptake. Am. J. Physiol. Endocrinol. Metab. 300, E134–E144 (2011).
Haddad, D., Al Madhoun, A., Nizam, R. & Al-Mulla, F. Role of caveolin-1 in diabetes and its complications. Oxid. Med. Cell Longev. 2020, 9761539 (2020).
Cohen, A. W. et al. Caveolin-1-deficient mice show insulin resistance and defective insulin receptor protein expression in adipose tissue. Am. J. Physiol. Cell Physiol. 285, C222–C235 (2003).
Chen, Z. et al. Reciprocal regulation of eNOS and caveolin-1 functions in endothelial cells. Mol. Biol. Cell 29, 1190–1202 (2018).
Song, H. et al. Release of matrix metalloproteinases-2 and 9 by S-nitrosylated caveolin-1 contributes to degradation of extracellular matrix in tPA-treated hypoxic endothelial cells. PLoS ONE 11, e0149269 (2016).
Bakhshi, F. R. et al. Nitrosation-dependent caveolin 1 phosphorylation, ubiquitination, and degradation and its association with idiopathic pulmonary arterial hypertension. Pulm. Circ. 3, 816–830 (2013).
Tang, W. J. Targeting insulin-degrading enzyme to treat type 2 diabetes mellitus. Trends Endocrinol. Metab. 27, 24–34 (2016).
Pivovarova, O., Hohn, A., Grune, T., Pfeiffer, A. F. & Rudovich, N. Insulin-degrading enzyme: new therapeutic target for diabetes and Alzheimer’s disease? Ann. Med. 48, 614–624 (2016).
Farris, W. et al. Insulin-degrading enzyme regulates the levels of insulin, amyloid β-protein, and the β-amyloid precursor protein intracellular domain in vivo. Proc. Natl Acad. Sci. USA 100, 4162–4167 (2003).
Wroblewski, V. J., Masnyk, M., Khambatta, S. S. & Becker, G. W. Mechanisms involved in degradation of human insulin by cytosolic fractions of human, monkey, and rat liver. Diabetes 41, 539–547 (1992).
Fakhrai-Rad, H. et al. Insulin-degrading enzyme identified as a candidate diabetes susceptibility gene in GK rats. Hum. Mol. Genet. 9, 2149–2158 (2000).
Ralat, L. A., Ren, M., Schilling, A. B. & Tang, W. J. Protective role of Cys-178 against the inactivation and oligomerization of human insulin-degrading enzyme by oxidation and nitrosylation. J. Biol. Chem. 284, 34005–34018 (2009).
Cordes, C. M., Bennett, R. G., Siford, G. L. & Hamel, F. G. Nitric oxide inhibits insulin-degrading enzyme activity and function through S-nitrosylation. Biochem. Pharmacol. 77, 1064–1073 (2009).
Akhtar, M. W. et al. Elevated glucose and oligomeric β-amyloid disrupt synapses via a common pathway of aberrant protein S-nitrosylation. Nat. Commun. 7, 10242 (2016).
Ward, C. W. & Lawrence, M. C. Ligand-induced activation of the insulin receptor: a multi-step process involving structural changes in both the ligand and the receptor. Bioessays 31, 422–434 (2009).
Kadowaki, T., Ueki, K., Yamauchi, T. & Kubota, N. SnapShot: insulin signaling pathways. Cell 148, 624.e1 (2012).
Kadowaki, T., Kubota, N., Ueki, K. & Yamauchi, T. SnapShot: physiology of insulin signaling. Cell 148, 834–834.e1 (2012).
Duplain, H. et al. Insulin resistance, hyperlipidemia, and hypertension in mice lacking endothelial nitric oxide synthase. Circulation 104, 342–345 (2001).
Vecoli, C. et al. Partial deletion of eNOS gene causes hyperinsulinemic state, unbalance of cardiac insulin signaling pathways and coronary dysfunction independently of high fat diet. PLoS One 9, e104156 (2014).
Nakagawa, T. et al. Diabetic endothelial nitric oxide synthase knockout mice develop advanced diabetic nephropathy. J. Am. Soc. Nephrol. 18, 539–550 (2007).
Kashyap, S. R. et al. Insulin resistance is associated with impaired nitric oxide synthase activity in skeletal muscle of type 2 diabetic subjects. J. Clin. Endocrinol. Metab. 90, 1100–1105 (2005).
Hsu, M. F. & Meng, T. C. Enhancement of insulin responsiveness by nitric oxide-mediated inactivation of protein-tyrosine phosphatases. J. Biol. Chem. 285, 7919–7928 (2010).
Barrett, D. M. et al. Inhibition of protein-tyrosine phosphatases by mild oxidative stresses is dependent on S-nitrosylation. J. Biol. Chem. 280, 14453–14461 (2005).
Numajiri, N. et al. On-off system for PI3-kinase-Akt signaling through S-nitrosylation of phosphatase with sequence homology to tensin (PTEN). Proc. Natl Acad. Sci. USA 108, 10349–10354 (2011).
Elchebly, M. et al. Increased insulin sensitivity and obesity resistance in mice lacking the protein tyrosine phosphatase-1B gene. Science 283, 1544–1548 (1999).
Chen, Y. Y. et al. Cysteine S-nitrosylation protects protein-tyrosine phosphatase 1B against oxidation-induced permanent inactivation. J. Biol. Chem. 283, 35265–35272 (2008).
Chen, C. Y., Chen, J., He, L. & Stiles, B. L. PTEN: tumor suppressor and metabolic regulator. Front. Endocrinol. 9, 338 (2018).
Kurlawalla-Martinez, C. et al. Insulin hypersensitivity and resistance to streptozotocin-induced diabetes in mice lacking PTEN in adipose tissue. Mol. Cell Biol. 25, 2498–2510 (2005).
Pei, D. S., Sun, Y. F. & Song, Y. J. S-nitrosylation of PTEN invovled in ischemic brain injury in rat hippocampal CA1 region. Neurochem. Res. 34, 1507–1512 (2009).
Zhu, L. et al. NOS1 S-nitrosylates PTEN and inhibits autophagy in nasopharyngeal carcinoma cells. Cell Death Discov. 3, 17011 (2017).
Kwak, Y. D. et al. NO signaling and S-nitrosylation regulate PTEN inhibition in neurodegeneration. Mol. Neurodegener. 5, 49 (2010).
Choi, M. S. et al. Transnitrosylation from DJ-1 to PTEN attenuates neuronal cell death in Parkinson’s disease models. J. Neurosci. 34, 15123–15131 (2014).
Bonifati, V. et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science 299, 256–259 (2003).
Clement, S. et al. The lipid phosphatase SHIP2 controls insulin sensitivity. Nature 409, 92–97 (2001).
Montagnani, M., Chen, H., Barr, V. A. & Quon, M. J. Insulin-stimulated activation of eNOS is independent of Ca2+ but requires phosphorylation by Akt at Ser(1179). J. Biol. Chem. 276, 30392–30398 (2001).
Muoio, D. M. & Newgard, C. B. Molecular and metabolic mechanisms of insulin resistance and β-cell failure in type 2 diabetes. Nat. Rev. Mol. Cell Biol. 9, 193–205 (2008).
Cerf, M. E. Beta cell dysfunction and insulin resistance. Front. Endocrinol. 4, 37 (2013).
Lackey, D. E. & Olefsky, J. M. Regulation of metabolism by the innate immune system. Nat. Rev. Endocrinol. 12, 15–28 (2016).
Kahn, S. E., Hull, R. L. & Utzschneider, K. M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444, 840–846 (2006).
Kim, J. H., Bachmann, R. A. & Chen, J. Interleukin-6 and insulin resistance. Vitam. Horm. 80, 613–633 (2009).
Salvado, L., Palomer, X., Barroso, E. & Vazquez-Carrera, M. Targeting endoplasmic reticulum stress in insulin resistance. Trends Endocrinol. Metab. 26, 438–448 (2015).
Boucher, J., Kleinridders, A. & Kahn, C. R. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb. Perspect. Biol. 6, a009191 (2014).
Copps, K. D. & White, M. F. Regulation of insulin sensitivity by serine/threonine phosphorylation of insulin receptor substrate proteins IRS1 and IRS2. Diabetologia 55, 2565–2582 (2012).
Schiattarella, G. G. et al. Nitrosative stress drives heart failure with preserved ejection fraction. Nature 568, 351–356 (2019).
Yang, L. et al. S-Nitrosylation links obesity-associated inflammation to endoplasmic reticulum dysfunction. Science 349, 500–506 (2015).
Katashima, C. K., Silva, V. R. R., Lenhare, L., Marin, R. M. & Carvalheira, J. B. C. iNOS promotes hypothalamic insulin resistance associated with deregulation of energy balance and obesity in rodents. Sci. Rep. 7, 9265 (2017).
Shinozaki, S. et al. Liver-specific inducible nitric-oxide synthase expression is sufficient to cause hepatic insulin resistance and mild hyperglycemia in mice. J. Biol. Chem. 286, 34959–34975 (2011).
Carvalho-Filho, M. A. et al. S-nitrosation of the insulin receptor, insulin receptor substrate 1, and protein kinase B/Akt: a novel mechanism of insulin resistance. Diabetes 54, 959–967 (2005).
Kaneki, M., Shimizu, N., Yamada, D. & Chang, K. Nitrosative stress and pathogenesis of insulin resistance. Antioxid. Redox Signal. 9, 319–329 (2007).
Yasukawa, T. et al. S-nitrosylation-dependent inactivation of Akt/protein kinase B in insulin resistance. J. Biol. Chem. 280, 7511–7518 (2005).
Carvalho-Filho, M. A., Ueno, M., Carvalheira, J. B., Velloso, L. A. & Saad, M. J. Targeted disruption of iNOS prevents LPS-induced S-nitrosation of IRβ/IRS-1 and Akt and insulin resistance in muscle of mice. Am. J. Physiol. Endocrinol. Metab. 291, E476–E482 (2006).
Ropelle, E. R. et al. Targeted disruption of inducible nitric oxide synthase protects against aging, S-nitrosation, and insulin resistance in muscle of male mice. Diabetes 62, 466–470 (2013).
Crunfli, F. et al. NO-dependent Akt Inactivation by S-nitrosylation as a possible mechanism of STZ-induced neuronal insulin resistance. J. Alzheimers Dis. 65, 1427–1443 (2018).
Wu, M. et al. Aging-associated dysfunction of Akt/protein kinase B: S-nitrosylation and acetaminophen intervention. PLoS ONE 4, e6430 (2009).
Lee, Y. S. et al. Increased adipocyte O2 consumption triggers HIF-1α, causing inflammation and insulin resistance in obesity. Cell 157, 1339–1352 (2014).
Carvalho-Filho, M. A. et al. Aspirin attenuates insulin resistance in muscle of diet-induced obese rats by inhibiting inducible nitric oxide synthase production and S-nitrosylation of IRβ/IRS-1 and Akt. Diabetologia 52, 2425–2434 (2009).
Tsuzuki, T. et al. Voluntary exercise can ameliorate insulin resistance by reducing iNOS-mediated S-nitrosylation of Akt in the liver in obese rats. PLoS ONE 10, e0132029 (2015).
Pauli, J. R. et al. Acute physical exercise reverses S-nitrosation of the insulin receptor, insulin receptor substrate 1 and protein kinase B/Akt in diet-induced obese Wistar rats. J. Physiol. 586, 659–671 (2008).
Muniyappa, R. & Sowers, J. R. Role of insulin resistance in endothelial dysfunction. Rev. Endocr. Metab. Disord. 14, 5–12 (2013).
Potenza, M. A. et al. Insulin resistance in spontaneously hypertensive rats is associated with endothelial dysfunction characterized by imbalance between NO and ET-1 production. Am. J. Physiol. Heart Circ. Physiol. 289, H813–H822 (2005).
Montagnani, M. et al. Inhibition of phosphatidylinositol 3-kinase enhances mitogenic actions of insulin in endothelial cells. J. Biol. Chem. 277, 1794–1799 (2002).
Mukai, Y., Wang, C. Y., Rikitake, Y. & Liao, J. K. Phosphatidylinositol 3-kinase/protein kinase Akt negatively regulates plasminogen activator inhibitor type 1 expression in vascular endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 292, H1937–H1942 (2007).
Patel, P. & Woodgett, J. R. Glycogen synthase kinase 3: a kinase for all pathways? Curr. Top. Dev. Biol. 123, 277–302 (2017).
Dibble, C. C. & Cantley, L. C. Regulation of mTORC1 by PI3K signaling. Trends Cell Biol. 25, 545–555 (2015).
Wang, S. B. et al. Protein S-nitrosylation controls glycogen synthase kinase 3β function independent of its phosphorylation state. Circ. Res. 122, 1517–1531 (2018).
Lopez-Rivera, E. et al. Inducible nitric oxide synthase drives mTOR pathway activation and proliferation of human melanoma by reversible nitrosylation of TSC2. Cancer Res. 74, 1067–1078 (2014).
Lee, S. & Dong, H. H. FoxO integration of insulin signaling with glucose and lipid metabolism. J. Endocrinol. 233, R67–R79 (2017).
DiPilato, L. M. et al. The role of PDE3B phosphorylation in the inhibition of lipolysis by insulin. Mol. Cell Biol. 35, 2752–2760 (2015).
Scherer, P. E. The multifaceted roles of adipose tissue–therapeutic targets for diabetes and beyond: the 2015 Banting Lecture. Diabetes 65, 1452–1461 (2016).
Tontonoz, P., Hu, E. & Spiegelman, B. M. Stimulation of adipogenesis in fibroblasts by PPARɣ2, a lipid-activated transcription factor. Cell 79, 1147–1156 (1994).
Tontonoz, P. & Spiegelman, B. M. Fat and beyond: the diverse biology of PPARɣ. Annu. Rev. Biochem. 77, 289–312 (2008).
Yin, R. et al. Pro-inflammatory macrophages suppress PPARɣ activity in adipocytes via S-nitrosylation. Free Radic. Biol. Med. 89, 895–905 (2015).
Guilherme, A., Virbasius, J. V., Puri, V. & Czech, M. P. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat. Rev. Mol. Cell Biol. 9, 367–377 (2008).
Ovadia, H. et al. Increased adipocyte S-nitrosylation targets anti-lipolytic action of insulin: relevance to adipose tissue dysfunction in obesity. J. Biol. Chem. 286, 30433–30443 (2011).
Choi, Y. H. et al. Alterations in regulation of energy homeostasis in cyclic nucleotide phosphodiesterase 3B-null mice. J. Clin. Invest. 116, 3240–3251 (2006).
Yeung, F. et al. Modulation of NF-κB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J. 23, 2369–2380 (2004).
Gauglitz, G. G. et al. Post-burn hepatic insulin resistance is associated with endoplasmic reticulum (ER) stress. Shock 33, 299–305 (2010).
Nakazawa, H. et al. iNOS as a driver of inflammation and apoptosis in mouse skeletal muscle after burn injury: possible involvement of Sirt1 S-nitrosylation-mediated acetylation of p65 NF-κB and p53. PLoS ONE 12, e0170391 (2017).
Shinozaki, S. et al. Inflammatory stimuli induce inhibitory S-nitrosylation of the deacetylase SIRT1 to increase acetylation and activation of p53 and p65. Sci. Signal. 7, ra106 (2014).
Gillum, M. P. et al. SirT1 regulates adipose tissue inflammation. Diabetes 60, 3235–3245 (2011).
Wang, R. H. et al. Hepatic Sirt1 deficiency in mice impairs mTorc2/Akt signaling and results in hyperglycemia, oxidative damage, and insulin resistance. J. Clin. Invest. 121, 4477–4490 (2011).
Poitout, V. et al. Glucolipotoxicity of the pancreatic beta cell. Biochim. Biophys. Acta 1801, 289–298 (2010).
Ye, R., Onodera, T. & Scherer, P. E. Lipotoxicity and β cell maintenance in obesity and type 2 diabetes. J. Endocr. Soc. 3, 617–631 (2019).
Heimann, E. et al. Expression and regulation of cyclic nucleotide phosphodiesterases in human and rat pancreatic islets. PLoS ONE 5, e14191 (2010).
Dubois, M. et al. Expression of peroxisome proliferator-activated receptor ɣ (PPARɣ) in normal human pancreatic islet cells. Diabetologia 43, 1165–1169 (2000).
Bordone, L. et al. Sirt1 regulates insulin secretion by repressing UCP2 in pancreatic β cells. PLoS Biol. 4, e31 (2006).
Lin, J. H., Walter, P. & Yen, T. S. Endoplasmic reticulum stress in disease pathogenesis. Annu. Rev. Pathol. 3, 399–425 (2008).
Walter, P. & Ron, D. The unfolded protein response: from stress pathway to homeostatic regulation. Science 334, 1081–1086 (2011).
Higuchi-Sanabria, R., Frankino, P. A., Paul, J. W. 3rd, Tronnes, S. U. & Dillin, A. A futile battle? Protein quality control and the stress of aging. Dev. Cell 44, 139–163 (2018).
Volpi, V. G., Touvier, T. & D’Antonio, M. Endoplasmic reticulum protein quality control failure in myelin disorders. Front. Mol. Neurosci. 9, 162 (2016).
Hetz, C. The unfolded protein response: controlling cell fate decisions under ER stress and beyond. Nat. Rev. Mol. Cell Biol. 13, 89–102 (2012).
Anholt, R. R. & Carbone, M. A. A molecular mechanism for glaucoma: endoplasmic reticulum stress and the unfolded protein response. Trends Mol. Med. 19, 586–593 (2013).
Ghosh, R., Colon-Negron, K. & Papa, F. R. Endoplasmic reticulum stress, degeneration of pancreatic islet β-cells, and therapeutic modulation of the unfolded protein response in diabetes. Mol. Metab. 27S, S60–S68 (2019).
Zhang, K. & Kaufman, R. J. From endoplasmic-reticulum stress to the inflammatory response. Nature 454, 455–462 (2008).
Matus, S., Glimcher, L. H. & Hetz, C. Protein folding stress in neurodegenerative diseases: a glimpse into the ER. Curr. Opin. Cell Biol. 23, 239–252 (2011).
Ren, J., Bi, Y., Sowers, J. R., Hetz, C. & Zhang, Y. Endoplasmic reticulum stress and unfolded protein response in cardiovascular diseases. Nat. Rev. Cardiol. 18, 499–521 (2021).
Nakato, R. et al. Regulation of the unfolded protein response via S-nitrosylation of sensors of endoplasmic reticulum stress. Sci. Rep. 5, 14812 (2015).
Fonseca, S. G., Burcin, M., Gromada, J. & Urano, F. Endoplasmic reticulum stress in β-cells and development of diabetes. Curr. Opin. Pharmacol. 9, 763–770 (2009).
Huang, C. J. et al. High expression rates of human islet amyloid polypeptide induce endoplasmic reticulum stress mediated β-cell apoptosis, a characteristic of humans with type 2 but not type 1 diabetes. Diabetes 56, 2016–2027 (2007).
Zhang, L., Lai, E., Teodoro, T. & Volchuk, A. GRP78, but not protein-disulfide isomerase, partially reverses hyperglycemia-induced inhibition of insulin synthesis and secretion in pancreatic β-cells. J. Biol. Chem. 284, 5289–5298 (2009).
Jang, I. et al. PDIA1/P4HB is required for efficient proinsulin maturation and β cell health in response to diet induced obesity. eLife 8, e44528 (2019).
Wilkinson, B. & Gilbert, H. F. Protein disulfide isomerase. Biochim. Biophys. Acta 1699, 35–44 (2004).
Wadham, C., Parker, A., Wang, L. & Xia, P. High glucose attenuates protein S-nitrosylation in endothelial cells: role of oxidative stress. Diabetes 56, 2715–2721 (2007).
Uehara, T. et al. S-nitrosylated protein-disulphide isomerase links protein misfolding to neurodegeneration. Nature 441, 513–517 (2006).
Hu, Y. et al. Endoplasmic reticulum-associated degradation (ERAD) has a critical role in supporting glucose-stimulated insulin secretion in pancreatic β-cells. Diabetes 68, 733–746 (2019).
Lopata, A., Kniss, A., Lohr, F., Rogov, V. V. & Dotsch, V. Ubiquitination in the ERAD process. Int. J. Mol. Sci. 21, 5369 (2020).
Azzam, S. K. et al. Genetic associations with diabetic retinopathy and coronary artery disease in Emirati patients with type-2 diabetes mellitus. Front. Endocrinol. 10, 283 (2019).
Fujikawa, K. et al. S-Nitrosylation at the active site decreases the ubiquitin-conjugating activity of ubiquitin-conjugating enzyme E2 D1 (UBE2D1), an ERAD-associated protein. Biochem. Biophys. Res. Commun. 524, 910–915 (2020).
Choi, A. M., Ryter, S. W. & Levine, B. Autophagy in human health and disease. N. Engl. J. Med. 368, 1845–1846 (2013).
Watada, H. & Fujitani, Y. Minireview: Autophagy in pancreatic β-cells and its implication in diabetes. Mol. Endocrinol. 29, 338–348 (2015).
Yang, L., Li, P., Fu, S., Calay, E. S. & Hotamisligil, G. S. Defective hepatic autophagy in obesity promotes ER stress and causes insulin resistance. Cell Metab. 11, 467–478 (2010).
Arai, C. et al. Trehalose prevents adipocyte hypertrophy and mitigates insulin resistance in mice with established obesity. J. Nutr. Sci. Vitaminol. 59, 393–401 (2013).
Singh, R. et al. Autophagy regulates lipid metabolism. Nature 458, 1131–1135 (2009).
Qian, Q. et al. S-Nitrosoglutathione reductase dysfunction contributes to obesity-associated hepatic insulin resistance via regulating autophagy. Diabetes 67, 193–207 (2018).
Liu, L. et al. Essential roles of S-nitrosothiols in vascular homeostasis and endotoxic shock. Cell 116, 617–628 (2004).
Kroemer, G., Marino, G. & Levine, B. Autophagy and the integrated stress response. Mol. Cell 40, 280–293 (2010).
Ebato, C. et al. Autophagy is important in islet homeostasis and compensatory increase of beta cell mass in response to high-fat diet. Cell Metab. 8, 325–332 (2008).
Masini, M. et al. Autophagy in human type 2 diabetes pancreatic beta cells. Diabetologia 52, 1083–1086 (2009).
Wright, C., Iyer, A. K., Kulkarni, Y. & Azad, N. S-Nitrosylation of Bcl-2 negatively affects autophagy in lung epithelial cells. J. Cell Biochem. 117, 521–532 (2016).
Montagna, C. et al. To eat, or NOt to eat: S-nitrosylation signaling in autophagy. FEBS J. 283, 3857–3869 (2016).
Luchsinger, J. A., Tang, M. X., Shea, S. & Mayeux, R. Hyperinsulinemia and risk of Alzheimer disease. Neurology 63, 1187–1192 (2004).
Sergi, D., Renaud, J., Simola, N. & Martinoli, M. G. Diabetes, a contemporary risk for Parkinson’s disease: epidemiological and cellular evidences. Front. Aging Neurosci. 11, 302 (2019).
Lee, S., Tong, M., Hang, S., Deochand, C. & de la Monte, S. CSF and brain indices of insulin resistance, oxidative stress and neuro-inflammation in early versus late Alzheimer’s disease. J. Alzheimers Dis. Parkinsonism 3, 128 (2013).
de la Monte, S. M. & Wands, J. R. Alzheimer’s disease is type 3 diabetes–evidence reviewed. J. Diabetes Sci. Technol. 2, 1101–1113 (2008).
Acknowledgements
The authors acknowledge the support of National Institutes of Health grants DK119506, HL158507, DK128347 and HL157151.
Author information
Authors and Affiliations
Contributions
J.S.S., H.-L.Z. and R.T.P. contributed substantially to the discussion of the content and reviewed and/or edited the article before submission. H.-L.Z. researched data for the article and wrote the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Endocrinology thanks the anonymous reviewers for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Thiol
-
A sulfhydryl group (SH) in the amino acid cysteine. The thiol group in proteins is the site of post-translational modification by S-nitrosylation.
- LMW SNOs
-
Low molecular weight S-nitrosothiols, which serve as cofactors in protein denitrosylases. Common examples include S-nitrosoglutathione (GSNO) and S-nitroso-co-enzyme A (SNO-CoA), which serve as substrates in GSNO reductases and SNO-CoA reductases, respectively.
- Quantal size
-
The elementary unit of synaptic transmission elicited by the release of neurotransmitters from a single vesicle. Changes in quantal size might be regulated by postsynaptic modification of receptor sensitivity and/or alterations in vesicle filling.
- Weibel–Palade bodies
-
Storage granules in endothelial cells containing and releasing von Willebrand factor and P-selectin to regulate haemostasis and inflammation.
- Nitrosative stress
-
A state of cellular stress characterized by excessive S-nitrosylation of proteins. Nitrosative stress is usually caused by either increased production of nitric oxide or decreased metabolism of S-nitrosothiols.
Rights and permissions
About this article
Cite this article
Zhou, HL., Premont, R.T. & Stamler, J.S. The manifold roles of protein S-nitrosylation in the life of insulin. Nat Rev Endocrinol 18, 111–128 (2022). https://doi.org/10.1038/s41574-021-00583-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-021-00583-1
This article is cited by
-
Redox regulation of m6A methyltransferase METTL3 in β-cells controls the innate immune response in type 1 diabetes
Nature Cell Biology (2024)
-
Inhibition of NOS1 promotes the interferon response of melanoma cells
Journal of Translational Medicine (2022)