Abstract
Growth differentiation factor 15 (GDF15) is a member of the TGFβ superfamily whose expression is increased in response to cellular stress and disease as well as by metformin. Elevations in GDF15 reduce food intake and body mass in animal models through binding to glial cell-derived neurotrophic factor family receptor alpha-like (GFRAL) and the recruitment of the receptor tyrosine kinase RET in the hindbrain. This effect is largely independent of other appetite-regulating hormones (for example, leptin, ghrelin or glucagon-like peptide 1). Consistent with an important role for the GDF15–GFRAL signalling axis, some human genetic studies support an interrelationship with human obesity. Furthermore, findings in both mice and humans have shown that metformin and exercise increase circulating levels of GDF15. GDF15 might also exert anti-inflammatory effects through mechanisms that are not fully understood. These unique and distinct mechanisms for suppressing food intake and inflammation makes GDF15 an appealing candidate to treat many metabolic diseases, including obesity, type 2 diabetes mellitus, non-alcoholic fatty liver disease, cardiovascular disease and cancer cachexia. Here, we review the mechanisms regulating GDF15 production and secretion, GDF15 signalling in different cell types, and how GDF15-targeted pharmaceutical approaches might be effective in the treatment of metabolic diseases.
Key points
-
Growth differentiation factor 15 (GDF15) is expressed in multiple cell types and can be increased by cellular stressors, including hypoxia, mitochondrial dysfunction, metformin and endurance exercise.
-
Increases in GDF15 secretion are mediated through mitochondrial stress and by activation of the integrated stress response pathway as well as, potentially, via AMPK.
-
GDF15 reduces the intake of high-fat diets in animal models through binding to glial cell-derived neurotrophic factor family receptor alpha-like (GFRAL) and the recruitment of the receptor tyrosine kinase RET in the hindbrain and this event is required for weight loss and improved glycaemic control.
-
Evidence suggests that GDF15 might alleviate non-alcoholic fatty liver disease and non-alcoholic steatohepatitis but the mechanisms mediating the anti-inflammatory effects and whether these are independent of reductions in body weight remain to be determined.
-
GDF15 might have cardioprotective effects by reducing atherosclerosis, cardiac hypertrophy and ischaemia–reperfusion injury; however, the mechanisms mediating these effects are still unclear.
-
Clinical testing of long-acting analogues of GDF15 is under way and will be important to determine whether the beneficial effects observed in animal models are translated to humans in a safe and efficacious manner.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Lyall, D. M. et al. Association of body mass index with cardiometabolic disease in the UK Biobank: a Mendelian randomization study. JAMA Cardiol. 2, 882–889 (2017).
Fabbrini, E., Sullivan, S. & Klein, S. Obesity and nonalcoholic fatty liver disease: biochemical, metabolic, and clinical implications. Hepatology 51, 679–689 (2010).
Liu, Z. et al. Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping. J. Hepatol. 73, 263–276 (2020).
Friedman, S. L., Neuschwander-Tetri, B. A., Rinella, M. & Sanyal, A. J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 24, 908–922 (2018).
Cai, J. et al. Nonalcoholic fatty liver disease pandemic fuels the upsurge in cardiovascular diseases. Circ. Res. 126, 679–704 (2020).
Kumanyika, S. K. et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation 118, 428–464 (2008).
Gadde, K. M., Martin, C. K., Berthoud, H. R. & Heymsfield, S. B. Obesity: pathophysiology and management. J. Am. Coll. Cardiol. 71, 69–84 (2018).
Lockhart, S. M., Saudek, V. & O’Rahilly, S. GDF15: a hormone conveying somatic distress to the brain. Endocr. Rev. 41, 610–642 (2020).
Hsiao, E. C. et al. Characterization of growth-differentiation factor 15, a transforming growth factor beta superfamily member induced following liver injury. Mol. Cell Biol. 20, 3742–3751 (2000).
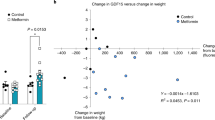
Coll, A. P. et al. GDF15 mediates the effects of metformin on body weight and energy balance. Nature 578, 444–448 (2020).
Paralkar, V. M. et al. Cloning and characterization of a novel member of the transforming growth factor-beta/bone morphogenetic protein family. J. Biol. Chem. 273, 13760–13767 (1998).
Yokoyama-Kobayashi, M., Saeki, M., Sekine, S. & Kato, S. Human cDNA encoding a novel TGF-beta superfamily protein highly expressed in placenta. J. Biochem. 122, 622–626 (1997).
Tsai, V. W. et al. Treatment with the TGF-b superfamily cytokine MIC-1/GDF15 reduces the adiposity and corrects the metabolic dysfunction of mice with diet-induced obesity. Int. J. Obes. 42, 561–571 (2018).
Tsai, V. W. et al. Anorexia/cachexia of chronic diseases: a role for the TGF-beta family cytokine MIC-1/GDF15. J. Cachexia Sarcopenia Muscle 3, 239–243 (2012).
Tsai, V. W. W., Husaini, Y., Sainsbury, A., Brown, D. A. & Breit, S. N. The MIC-1/GDF15-GFRAL pathway in energy homeostasis: implications for obesity, cachexia, and other associated diseases. Cell Metab. 28, 353–368 (2018).
Dostálová, I. et al. Increased serum concentrations of macrophage inhibitory cytokine-1 in patients with obesity and type 2 diabetes mellitus: the influence of very low calorie diet. Eur. J. Endocrinol. 161, 397–404 (2009).
Vila, G. et al. The relationship between insulin resistance and the cardiovascular biomarker growth differentiation factor-15 in obese patients. Clin. Chem. 57, 309–316 (2011).
Xiong, Y. et al. Long-acting MIC-1/GDF15 molecules to treat obesity: Evidence from mice to monkeys. Sci. Transl. Med. 9, eaan8732 (2017).
Gil, C. I. et al. Role of GDF15 in active lifestyle induced metabolic adaptations and acute exercise response in mice. Sci. Rep. 9, 20120 (2019).
Tsai, V. W. et al. Serum levels of human MIC-1/GDF15 vary in a diurnal pattern, do not display a profile suggestive of a satiety factor and are related to BMI. PLoS One 10, e0133362 (2015).
Gerstein, H. C. et al. Growth differentiation factor 15 as a novel biomarker for metformin. Diabetes Care 40, 280–283 (2017).
Altena, R. et al. Growth differentiation factor 15 (GDF-15) plasma levels increase during bleomycin- and cisplatin-based treatment of testicular cancer patients and relate to endothelial damage. PLoS One 10, e0115372 (2015).
Petry, C. J. et al. Associations of vomiting and antiemetic use in pregnancy with levels of circulating GDF15 early in the second trimester: A nested case-control study. Wellcome Open Res. 3, 123–123 (2018).
Tsai, V. W.-W. et al. TGF-b superfamily cytokine MIC-1/GDF15 is a physiological appetite and body weight regulator. PLoS One 8, e55174 (2013).
Patel, S. et al. GDF15 provides an endocrine signal of nutritional stress in mice and humans. Cell Metab. 29, 707–718.e8 (2019).
Campderros, L. et al. Brown adipocytes secrete GDF15 in response to thermogenic activation. Obesity 27, 1606–1616 (2019).
Bootcov, M. R. et al. MIC-1, a novel macrophage inhibitory cytokine, is a divergent member of the TGF-beta superfamily. Proc. Natl Acad. Sci. USA 94, 11514–11519 (1997).
Bottner, M., Suter-Crazzolara, C., Schober, A. & Unsicker, K. Expression of a novel member of the TGF-beta superfamily, growth/differentiation factor-15/macrophage-inhibiting cytokine-1 (GDF-15/MIC-1) in adult rat tissues. Cell Tissue Res. 297, 103–110 (1999).
Liu, R. & Nikolajczyk, B. S. Tissue immune cells fuel obesity-associated inflammation in adipose tissue and beyond. Front. Immunol. 10, 1587 (2019).
Ramachandran, P. et al. Resolving the fibrotic niche of human liver cirrhosis at single-cell level. Nature 575, 512–518 (2019).
Govaere, O. et al. Transcriptomic profiling across the nonalcoholic fatty liver disease spectrum reveals gene signatures for steatohepatitis and fibrosis. Sci. Transl. Med. 12, eaba4448 (2020).
Nohara, S. et al. GDF-15, a mitochondrial disease biomarker, is associated with the severity of multiple sclerosis. J. Neurol. Sci. 405, 116429 (2019).
Wollert, K. C., Kempf, T. & Wallentin, L. Growth differentiation factor 15 as a biomarker in cardiovascular disease. Clin. Chem. 63, 140–151 (2017).
Lindholm, D. et al. Association of multiple biomarkers with risk of all-cause and cause-specific mortality after acute coronary syndromes: a secondary analysis of the PLATO biomarker study. JAMA Cardiol. 3, 1160–1166 (2018).
Wallentin, L. et al. GDF-15 for prognostication of cardiovascular and cancer morbidity and mortality in men. PLoS One 8, e78797 (2013).
Brown, D. A. et al. Macrophage inhibitory cytokine 1: a new prognostic marker in prostate cancer. Clin. Cancer Res. 15, 6658–6664 (2009).
Tsui, K. H. et al. Growth differentiation factor-15: a p53- and demethylation-upregulating gene represses cell proliferation, invasion, and tumorigenesis in bladder carcinoma cells. Sci. Rep. 5, 12870 (2015).
Tan, M., Wang, Y., Guan, K. & Sun, Y. PTGF-β, a type β transforming growth factor (TGF-β) superfamily member, is a p53 target gene that inhibits tumor cell growth via TGF-β signaling pathway. Proc. Natl Acad. Sci. USA 97, 109–114 (2000).
Baek, S. J., Kim, J. S., Nixon, J. B., DiAugustine, R. P. & Eling, T. E. Expression of NAG-1, a transforming growth factor-beta superfamily member, by troglitazone requires the early growth response gene EGR-1. J. Biol. Chem. 279, 6883–6892 (2004).
Li, D., Zhang, H. & Zhong, Y. Hepatic GDF15 is regulated by CHOP of the unfolded protein response and alleviates NAFLD progression in obese mice. Biochem. Biophys. Res. Commun. 498, 388–394 (2018).
Day, E. A. et al. Metformin-induced increases in GDF15 are important for suppressing appetite and promoting weight loss. Nat. Metab. 1, 1202–1208 (2019).
Quiros, P. M. et al. Multi-omics analysis identifies ATF4 as a key regulator of the mitochondrial stress response in mammals. J. Cell Biol. 216, 2027–2045 (2017).
Anderson, N. S. & Haynes, C. M. Folding the mitochondrial UPR into the integrated stress response. Trends Cell Biol. 30, 428–439 (2020).
Chung, H. K. et al. Growth differentiation factor 15 is a myomitokine governing systemic energy homeostasis. J. Cell Biol. 216, 149–165 (2017).
Choi, M. J. et al. An adipocyte-specific defect in oxidative phosphorylation increases systemic energy expenditure and protects against diet-induced obesity in mouse models. Diabetologia 63, 837–852 (2020).
Zechner, C. et al. Total skeletal muscle PGC-1 deficiency uncouples mitochondrial derangements from fiber type determination and insulin sensitivity. Cell Metab. 12, 633–642 (2010).
O’Neill, H. M. et al. AMP-activated protein kinase (AMPK) β1β2 muscle null mice reveal an essential role for AMPK in maintaining mitochondrial content and glucose uptake during exercise. Proc. Natl Acad. Sci. USA 108, 16092–16097 (2011).
Wredenberg, A. et al. Respiratory chain dysfunction in skeletal muscle does not cause insulin resistance. Biochem. Biophys. Res. Commun. 350, 202–207 (2006).
Pospisilik, J. A. et al. Targeted deletion of AIF decreases mitochondrial oxidative phosphorylation and protects from obesity and diabetes. Cell 131, 476–491 (2007).
Conte, M. et al. Human aging and longevity are characterized by high levels of mitokines. J. Gerontol. A Biol. Sci. Med. Sci. 74, 600–607 (2019).
Moon, J. S. et al. Growth differentiation factor 15 protects against the aging-mediated systemic inflammatory response in humans and mice. Aging Cell 19, e13195 (2020).
Fujita, Y., Taniguchi, Y., Shinkai, S., Tanaka, M. & Ito, M. Secreted growth differentiation factor 15 as a potential biomarker for mitochondrial dysfunctions in aging and age-related disorders. Geriatr. Gerontol. Int. 16, 17–29 (2016).
Townsend, L. K. et al. AMPK mediates energetic stress-induced liver GDF15. FASEB J. 35, e21218 (2021).
Baek, S. J. & Eling, T. Growth differentiation factor 15 (GDF15): a survival protein with therapeutic potential in metabolic diseases. Pharmacol. Ther. 198, 46–58 (2019).
Li, J. J. et al. Growth differentiation factor 15 maturation requires proteolytic cleavage by PCSK3, -5, and -6. Mol. Cell Biol. 38, e00249-18 (2018).
Zhang, Z. et al. ARRB1 inhibits non-alcoholic steatohepatitis progression by promoting GDF15 maturation. J. Hepatol. 72, 976–989 (2020).
Bauskin, A. R. et al. The propeptide mediates formation of stromal stores of PROMIC-1: role in determining prostate cancer outcome. Cancer Res. 65, 2330–2336 (2005).
Bauskin, A. R. et al. The propeptide of macrophage inhibitory cytokine (MIC-1), a TGF-beta superfamily member, acts as a quality control determinant for correctly folded MIC-1. EMBO J. 19, 2212–2220 (2000).
Li, S. et al. Maturation of growth differentiation factor 15 in human placental trophoblast cells depends on the interaction with matrix metalloproteinase-26. J. Clin. Endocrinol. Metab. 99, E2277–E2287 (2014).
Abd El-Aziz, S. H., Endo, Y., Miyamaori, H., Takino, T. & Sato, H. Cleavage of growth differentiation factor 15 (GDF15) by membrane type 1-matrix metalloproteinase abrogates GDF15-mediated suppression of tumor cell growth. Cancer Sci. 98, 1330–1335 (2007).
Hsu, J. Y. et al. Non-homeostatic body weight regulation through a brainstem-restricted receptor for GDF15. Nature 550, 255–259 (2017).
Yang, L. et al. GFRAL is the receptor for GDF15 and is required for the anti-obesity effects of the ligand. Nat. Med. 23, 1158–1166 (2017).
Mullican, S. E. et al. GFRAL is the receptor for GDF15 and the ligand promotes weight loss in mice and nonhuman primates. Nat. Med. 23, 1150–1157 (2017).
Emmerson, P. J. et al. The metabolic effects of GDF15 are mediated by the orphan receptor GFRAL. Nat. Med. 23, 1215–1219 (2017).
Wong, A. et al. Phosphotyrosine 1062 is critical for the in vivo activity of the Ret9 receptor tyrosine kinase isoform. Mol. Cell. Biol. 25, 9661–9673 (2005).
Tsai, V. W. et al. The anorectic actions of the TGFbeta cytokine MIC-1/GDF15 require an intact brainstem area postrema and nucleus of the solitary tract. PLoS One 9, e100370 (2014).
Codo, P. et al. Control of glioma cell migration and invasiveness by GDF-15. Oncotarget 7, 7732–7746 (2016).
Olsen, O. E., Skjaervik, A., Stordal, B. F., Sundan, A. & Holien, T. TGF-beta contamination of purified recombinant GDF15. PLoS One 12, e0187349 (2017).
Johnen, H. et al. Tumor-induced anorexia and weight loss are mediated by the TGF-β superfamily cytokine MIC-1. Nat. Med. 13, 1333–1340 (2007).
Tsai, V. W.-W. et al. GDF15 mediates adiposity resistance through actions on GFRAL neurons in the hindbrain AP/NTS. Int. J. Obes. 43, 2370–2380 (2019).
Frikke-Schmidt, H. et al. GDF15 acts synergistically with liraglutide but is not necessary for the weight loss induced by bariatric surgery in mice. Mol. Metab. 21, 13–21 (2019).
Murphy, K. G. & Bloom, S. R. Gut hormones and the regulation of energy homeostasis. Nature 444, 854–859 (2006).
Banno, R. et al. Central administration of melanocortin agonist increased insulin sensitivity in diet-induced obese rats. FEBS Lett. 581, 1131–1136 (2007).
Zarjevski, N., Cusin, I., Vettor, R., Rohner-Jeanrenaud, F. & Jeanrenaud, B. Intracerebroventricular administration of neuropeptide Y to normal rats has divergent effects on glucose utilization by adipose tissue and skeletal muscle. Diabetes 43, 764–769 (1994).
Worth, A. A. et al. The cytokine GDF15 signals through a population of brainstem cholecystokinin neurons to mediate anorectic signalling. eLife 9, e55164 (2020).
Camilleri, M. Peripheral mechanisms in the control of appetite and related experimental therapies in obesity. Regul. Pept. 156, 24–27 (2009).
Borner, T. et al. GDF15 induces anorexia through nausea and emesis. Cell Metab. 31, 351–362.e355 (2020).
Endo, T. et al. Neurochemistry and neuropharmacology of emesis - the role of serotonin. Toxicology 153, 189–201 (2000).
Herrstedt, J. The latest consensus on antiemetics. Curr. Opin. Oncol. 30, 233–239 (2018).
Hayes, M. R. & Covasa, M. Gastric distension enhances CCK-induced Fos-like immunoreactivity in the dorsal hindbrain by activating 5-HT3 receptors. Brain Res. 1088, 120–130 (2006).
Borner, T. et al. GDF15 induces an aversive visceral malaise state that drives anorexia and weight loss. Cell Rep. 31, 107543 (2020).
Palmiter, R. D. The parabrachial nucleus: CGRP neurons function as a general alarm. Trends Neurosci. 41, 280–293 (2018).
Morton, G. J., Meek, T. H. & Schwartz, M. W. Neurobiology of food intake in health and disease. Nat. Rev. Neurosci. 15, 367–378 (2014).
Carter, M. E., Soden, M. E., Zweifel, L. S. & Palmiter, R. D. Genetic identification of a neural circuit that suppresses appetite. Nature 503, 111–114 (2013).
Chrysovergis, K. et al. NAG-1/GDF-15 prevents obesity by increasing thermogenesis, lipolysis and oxidative metabolism. Int. J. Obes. 38, 1555–1564 (2014).
Suriben, R. et al. Antibody-mediated inhibition of GDF15–GFRAL activity reverses cancer cachexia in mice. Nat. Med. 26, 1264–1270 (2020).
Beiroa, D. et al. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK. Diabetes 63, 3346–3358 (2014).
Tomas, E. et al. GLP-1(32-36)amide pentapeptide increases basal energy expenditure and inhibits weight gain in obese mice. Diabetes 64, 2409–2419 (2015).
Heppner, K. M. et al. Contribution of brown adipose tissue activity to the control of energy balance by GLP-1 receptor signalling in mice. Diabetologia 58, 2124–2132 (2015).
Harder, H., Nielsen, L., Tu, D. T. & Astrup, A. The effect of liraglutide, a long-acting glucagon-like peptide 1 derivative, on glycemic control, body composition, and 24-h energy expenditure in patients with type 2 diabetes. Diabetes Care 27, 1915–1921 (2004).
Müller, T. D. et al. Glucagon-like peptide 1 (GLP-1). Mol. Metab. 30, 72–130 (2019).
Yengo, L. et al. Meta-analysis of genome-wide association studies for height and body mass index in approximately 700000 individuals of European ancestry. Hum. Mol. Genet. 27, 3641–3649 (2018).
Pulit, S. L. et al. Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum. Mol. Genet. 28, 166–174 (2019).
Võsa, U. et al. Unraveling the polygenic architecture of complex traits using blood eQTL metaanalysis. bioRxiv https://doi.org/10.1101/447367 (2018).
Sun, B. B. et al. Genomic atlas of the human plasma proteome. Nature 558, 73–79 (2018).
Lonsdale, J. et al. The genotype-tissue expression (GTEx) project. Nat. Genet. 45, 580–585 (2013).
Machiela, M. J. & Chanock, S. J. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 31, 3555–3557 (2015).
Turcot, V. et al. Protein-altering variants associated with body mass index implicate pathways that control energy intake and expenditure in obesity. Nat. Genet. 50, 26–41 (2018).
Li, J. et al. Cryo-EM analyses reveal the common mechanism and diversification in the activation of RET by different ligands. eLife 8, e47650 (2019).
Cheung, C. L., Tan, K. C. B., Au, P. C. M., Li, G. H. Y. & Cheung, B. M. Y. Evaluation of GDF15 as a therapeutic target of cardiometabolic diseases in human: A Mendelian randomization study. EBioMedicine 41, 85–90 (2019).
Macia, L. et al. Macrophage inhibitory cytokine 1 (MIC-1/GDF15) decreases food intake, body weight and improves glucose tolerance in mice on normal & obesogenic diets. PLoS One 7, e34868 (2012).
Wang, X. et al. hNAG-1 increases lifespan by regulating energy metabolism and insulin/IGF-1/mTOR signaling. Aging 6, 690–704 (2014).
Wang, X., Chrysovergis, K., Kosak, J. & Eling, T. E. Lower NLRP3 inflammasome activity in NAG-1 transgenic mice is linked to a resistance to obesity and increased insulin sensitivity. Obesity 22, 1256–1263 (2014).
Hong, J. H. et al. GDF15 is a novel biomarker for impaired fasting glucose. Diabetes Metab. J. 38, 472–479 (2014).
Kempf, T. et al. Growth differentiation factor 15 predicts future insulin resistance and impaired glucose control in obese nondiabetic individuals: results from the XENDOS trial. Eur. J. Endocrinol. 167, 671–678 (2012).
Carstensen, M. et al. Macrophage inhibitory cytokine-1 is increased in individuals before type 2 diabetes diagnosis but is not an independent predictor of type 2 diabetes: the Whitehall II study. Eur. J. Endocrinol. 162, 913–917 (2010).
Schernthaner-Reiter, M. H. et al. GDF15 reflects beta cell function in obese patients independently of the grade of impairment of glucose metabolism. Nutr. Metab. Cardiovasc. Dis. 29, 334–342 (2019).
Nakayasu, E. S. et al. Comprehensive proteomics analysis of stressed human islets identifies GDF15 as a target for type 1 diabetes intervention. Cell Metab. 31, 363–374.e6 (2020).
Yi, H. S. et al. T-cell senescence contributes to abnormal glucose homeostasis in humans and mice. Cell Death Dis. 10, 249 (2019).
Jung, S. B. et al. Reduced oxidative capacity in macrophages results in systemic insulin resistance. Nat. Commun. 9, 1551 (2018).
Lee, S. E. et al. Growth differentiation factor 15 mediates systemic glucose regulatory action of T-helper type 2 cytokines. Diabetes 66, 2774–2788 (2017).
Foretz, M., Guigas, B. & Viollet, B. Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus. Nat. Rev. Endocrinol. 15, 569–589 (2019).
Steinberg, G. R. Cellular energy sensing and metabolism—implications for treating diabetes: the 2017 outstanding scientific achievement award lecture. Diabetes 67, 169–179 (2018).
Natali, A. et al. Metformin is the key factor in elevated plasma growth differentiation factor-15 levels in type 2 diabetes: a nested, case-control study. Diabetes Obes. Metab. 21, 412–416 (2019).
Colberg, S. R. et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 39, 2065–2079 (2016).
Kleinert, M. et al. Exercise increases circulating GDF15 in humans. Mol. Metab. 9, 187–191 (2018).
Tchou, I. et al. Growth-differentiation factor-15, endoglin and N-terminal pro-brain natriuretic peptide induction in athletes participating in an ultramarathon foot race. Biomarkers 14, 418–422 (2009).
Zhang, H., Fealy, C. E. & Kirwan, J. P. Exercise training promotes a GDF15-associated reduction in fat mass in older adults with obesity. Am. J. Physiol. Endocrinol. Metab. 316, E829–E836 (2019).
Laurens, C. et al. Growth and differentiation factor 15 is secreted by skeletal muscle during exercise and promotes lipolysis in humans. JCI insight 5, e131870 (2020).
Klein, A. B. et al. Pharmacological but not physiological GDF15 suppresses feeding and the motivation to exercise. Nat. Commun. 12, 1041 (2021).
Yardley, M. et al. Immediate response in markers of inflammation and angiogenesis during exercise: a randomised cross-over study in heart transplant recipients. Open Heart 4, e000635 (2017).
Murphy, R. M., Watt, M. J. & Febbraio, M. A. Metabolic communication during exercise. Nat. Metab. 2, 805–816 (2020).
Camacho, R. C., Donahue, E. P., James, F. D., Berglund, E. D. & Wasserman, D. H. Energy state of the liver during short-term and exhaustive exercise in C57BL/6J mice. Am. J. Physiol. Endocrinol. Metab. 290, E405–E408 (2006).
Kim, K. H. et al. Growth differentiation factor 15 ameliorates nonalcoholic steatohepatitis and related metabolic disorders in mice. Sci. Rep. 8, 6789 (2018).
Koo, B. K. et al. Growth differentiation factor 15 predicts advanced fibrosis in biopsy-proven non-alcoholic fatty liver disease. Liver Int. 38, 695–705 (2018).
Chung, H. K. et al. GDF15 deficiency exacerbates chronic alcohol- and carbon tetrachloride-induced liver injury. Sci. Rep. 7, 17238 (2017).
Luan, H. H. et al. GDF15 is an inflammation-induced central mediator of tissue tolerance. Cell 178, 1231–1244.e11 (2019).
Adela, R. & Banerjee, S. K. GDF-15 as a target and biomarker for diabetes and cardiovascular diseases: a translational prospective. J. Diabetes Res. 2015, 490842 (2015).
Xu, J. et al. GDF15/MIC-1 functions as a protective and antihypertrophic factor released from the myocardium in association with SMAD protein activation. Circ. Res. 98, 342–350 (2006).
Kempf, T. et al. The transforming growth factor-beta superfamily member growth-differentiation factor-15 protects the heart from ischemia/reperfusion injury. Circ. Res. 98, 351–360 (2006).
Kempf, T. & Wollert, K. C. Growth differentiation factor-15: a new biomarker in cardiovascular disease. Herz 34, 594–599 (2009).
Lusis, A. J. Atherosclerosis. Nature 407, 233–241 (2000).
Wang, D. et al. Targeting foam cell formation in atherosclerosis: therapeutic potential of natural products. Pharmacol. Rev. 71, 596–670 (2019).
Bentzon, J. F., Otsuka, F., Virmani, R. & Falk, E. Mechanisms of plaque formation and rupture. Circ. Res. 114, 1852–1866 (2014).
Bonaterra, G. A. et al. Growth differentiation factor-15 deficiency inhibits atherosclerosis progression by regulating interleukin-6-dependent inflammatory response to vascular injury. J. Am. Heart Assoc. 1, e002550 (2012).
de Jager, S. C. et al. Growth differentiation factor 15 deficiency protects against atherosclerosis by attenuating CCR2-mediated macrophage chemotaxis. J. Exp. Med. 208, 217–225 (2011).
Preusch, M. R. et al. GDF-15 protects from macrophage accumulation in a mousemodel of advanced atherosclerosis. Eur. J. Med. Res. 18, 19 (2013).
Johnen, H. et al. Increased expression of the TGF-b superfamily cytokine MIC-1/GDF15 protects ApoE(-/-) mice from the development of atherosclerosis. Cardiovasc. Pathol. 21, 499–505 (2012).
Tian, X. Y. et al. Thermoneutral housing accelerates metabolic inflammation to potentiate atherosclerosis but not insulin resistance. Cell Metab. 23, 165–178 (2016).
Skop, V. et al. Mouse thermoregulation: introducing the concept of the thermoneutral point. Cell Rep. 31, 107501 (2020).
Silvestre-Roig, C., Braster, Q., Ortega-Gomez, A. & Soehnlein, O. Neutrophils as regulators of cardiovascular inflammation. Nat. Rev. Cardiol. 17, 327–340 (2020).
Thygesen, K. et al. Third universal definition of myocardial infarction. Nat. Rev. Cardiol. 9, 620–633 (2012).
Saver, J. L. Proposal for a universal definition of cerebral infarction. Stroke 39, 3110–3115 (2008).
Kempf, T. et al. GDF-15 is an inhibitor of leukocyte integrin activation required for survival after myocardial infarction in mice. Nat. Med. 17, 581–588 (2011).
Zhang, Y. et al. Over-expression of growth differentiation factor 15 (GDF15) preventing cold ischemia reperfusion (I/R) injury in heart transplantation through Foxo3a signaling. Oncotarget 8, 36531–36544 (2017).
Rossaint, J., Vestweber, D. & Zarbock, A. GDF-15 prevents platelet integrin activation and thrombus formation. J. Thromb. Haemost. 11, 335–344 (2013).
Sen-Chowdhry, S., Jacoby, D., Moon, J. C. & McKenna, W. J. Update on hypertrophic cardiomyopathy and a guide to the guidelines. Nat. Rev. Cardiol. 13, 651–675 (2016).
Xu, X. Y. et al. Growth differentiation factor (GDF)-15 blocks norepinephrine-induced myocardial hypertrophy via a novel pathway involving inhibition of epidermal growth factor receptor transactivation. J. Biol. Chem. 289, 10084–10094 (2014).
Tisdale, M. J. Molecular pathways leading to cancer cachexia. Physiology 20, 340–348 (2005).
Lerner, L. et al. MAP3K11/GDF15 axis is a critical driver of cancer cachexia. J. Cachexia, Sarcopenia Muscle 7, 467–482 (2016).
Breen, D. M. et al. GDF-15 neutralization alleviates platinum-based chemotherapy-induced emesis, anorexia, and weight loss in mice and nonhuman primates. Cell Metab. 32, 938–950.e6 (2020).
Tran, T., Yang, J., Gardner, J. & Xiong, Y. GDF15 deficiency promotes high fat diet-induced obesity in mice. PLoS One 13, e0201584 (2018).
Acknowledgements
G.R.S. acknowledges the support of a Diabetes Canada Investigator Award (DI-5-17-5302-GS), a Canadian Institutes of Health Research Foundation Grant (201709FDN-CEBA-116200), a Tier 1 Canada Research Chair in Metabolic Diseases and a J. Bruce Duncan Endowed Chair in Metabolic Diseases. L.K.T. acknowledges the support of a CIHR Post-Doctoral Fellowship Award and Michael DeGroote Fellowship Award in Basic Biomedical Science.
Author information
Authors and Affiliations
Contributions
D.W. researched data for the article. All authors made substantial contributions to the discussion of content, wrote the article, and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
D.D. and S.B.J. are employees of Novo Nordisk A/S, a pharmaceutical company producing and selling medicine for the treatment of diabetes and obesity. G.R.S. is a co-founder and shareholder of Espervita Therapeutics, a company developing new medications for liver cancer. McMaster University has received funding from Espervita Therapeutics, Esperion Therapeutics, Poxel Pharmaceuticals and Novo Nordisk for research conducted in the laboratory of G.R.S. G.R.S. has received consulting/speaking fees from Astra Zeneca, Eli Lilly, Esperion Therapeutics, Merck, Poxel Pharmaceuticals and Takeda. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Endocrinology thanks S. Breit, S. O’Rahilly and M. Shong for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Common Metabolic Diseases Knowledge Portal: https://t2d.hugeamp.org/region.html?chr=19&end=18549986&phenotype=WHRadjBMI&start=18435541
The Blood Atlas: https://www.proteinatlas.org/humanproteome/blood
the Human Protein Atlas GFRAL expression: https://www.proteinatlas.org/ENSG00000187871-GFRAL/blood
Glossary
- Non-alcoholic fatty liver disease
-
(NAFLD). A spectrum of liver pathology ranging from liver steatosis (>5% lipids) to inflammation and fibrosis, known as non-alcoholic steatohepatitis, that is an important risk factor for type 2 diabetes mellitus, cardiovascular disease, liver cirrhosis and hepatocellular carcinoma.
- Integrated stress response
-
A eukaryotic cellular stress response to restore cellular homeostasis by phosphorylation of eIF2 by four specialized kinases (PERK, GCN2, PKR and HRI), leading to a decrease in global protein synthesis and an increase in the expression of specific genes, including ATF4.
- Mitochondrial unfolded protein response
-
(UPR). This cellular stress response is triggered when unfolded or misfolded proteins accumulate in mitochondria beyond the protective capacity of chaperone proteins.
- Cancer cachexia
-
This state is characterized by reductions in appetite and increases in energy expenditure, which leads to involuntary loss of adipose and lean mass that is associated with poor quality of life and reduced survival.
- Foam cells
-
Macrophages or vascular smooth muscle cells with a foamy appearance, which are over-laden with lipids and are a key cell type contributing to the development of atherosclerotic cardiovascular disease (coronary artery disease).
Rights and permissions
About this article
Cite this article
Wang, D., Day, E.A., Townsend, L.K. et al. GDF15: emerging biology and therapeutic applications for obesity and cardiometabolic disease. Nat Rev Endocrinol 17, 592–607 (2021). https://doi.org/10.1038/s41574-021-00529-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-021-00529-7
This article is cited by
-
Skin advanced glycation end-products as indicators of the metabolic profile in diabetes mellitus: correlations with glycemic control, liver phenotypes and metabolic biomarkers
BMC Endocrine Disorders (2024)
-
A novel bystander effect in tamoxifen treatment: PPIB derived from ER+ cells attenuates ER− cells via endoplasmic reticulum stress-induced apoptosis
Cell Death & Disease (2024)
-
Obesity and the kidney: mechanistic links and therapeutic advances
Nature Reviews Endocrinology (2024)
-
Plasma proteomic profiles predict future dementia in healthy adults
Nature Aging (2024)
-
Evaluation of the relation between subclinical systolic dysfunction defined by four-dimensional speckle-tracking echocardiography and growth differentiation factor-15 levels in patients with acromegaly
Hormones (2024)