Abstract
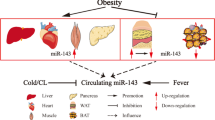
Obesity is a complex condition that is characterized by excessive fat accumulation, which can lead to the development of metabolic disorders, such as type 2 diabetes mellitus, nonalcoholic fatty liver disease and cardiovascular diseases. Evidence is accumulating that circulating microRNAs (miRNAs) act as a new class of endocrine factor. These miRNAs are released by many types of tissue, including adipose tissues. miRNAs might serve as endocrine and paracrine messengers that facilitate communication between donor cells and tissues with receptor cells or target tissues, thereby potentially having important roles in metabolic organ crosstalk. Moreover, many miRNAs are closely associated with the differentiation of adipocytes and are dysregulated in obesity. As such, circulating miRNAs are attractive potential biomarkers and hold promise for the development of miRNA-based therapeutics (such as miRNA mimetics, anti-miRNA oligonucleotides and exosomes loaded with miRNA) for obesity and related disorders. Here we review the latest research progress on the roles of circulating miRNAs in metabolic organ crosstalk. In addition, we discuss the clinical potential of circulating miRNAs as feasible biomarkers for the assessment of future risk of metabolic disorders and as therapeutic targets in obesity and related diseases.
Key points
Circulating microRNAs (miRNAs) can be secreted from different tissues, including adipose tissue, and affect the metabolic profiles of distant organs, thereby facilitating metabolic organ crosstalk.
In individuals with obesity and/or metabolic disease, the profile of circulating miRNAs is different from that seen in lean individuals.
Adipocyte-specific miRNA-deficient mouse models demonstrate the importance of circulating adipocyte-derived miRNAs for metabolic health.
Adipose tissue-derived and/or obesity-associated circulating miRNAs have potential as biomarkers for the prevention and management of obesity and metabolic diseases.
Evidence is accumulating that obesity-associated and/or adipose tissue-derived circulating miRNAs are promising new therapeutic targets for the treatment of obesity and related diseases.
The development of novel therapeutics, such as miRNA mimetics, anti-miRNA oligonucleotides and exosomes loaded with miRNAs, might allow the clinical application of miRNA-based therapeutics for obesity and metabolic disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ghaben, A. L. & Scherer, P. E. Adipogenesis and metabolic health. Nat. Rev. Mol. Cell Biol. 20, 242–258 (2019).
Reilly, J. J. Health effects of overweight and obesity in 195 countries. N. Engl. J. Med. 377, 1496 (2017).
Stern, J. H., Rutkowski, J. M. & Scherer, P. E. Adiponectin, leptin, and fatty acids in the maintenance of metabolic homeostasis through adipose tissue crosstalk. Cell Metab. 23, 770–784 (2016).
Ouchi, N., Parker, J. L., Lugus, J. J. & Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 11, 85–97 (2011).
Saltiel, A. R. & Olefsky, J. M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Invest. 127, 1–4 (2017).
Vienberg, S., Geiger, J., Madsen, S. & Dalgaard, L. T. MicroRNAs in metabolism. Acta Physiol. (Oxf) 219, 346–361 (2017).
Peng, C. & Wang, Y. L. Editorial: microRNAs as new players in endocrinology. Front. Endocrinol. (Lausanne) 9, 459 (2018).
Lee, R. C., Feinbaum, R. L. & Ambros, V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell 75, 843–854 (1993).
Wightman, B., Ha, I. & Ruvkun, G. Posttranscriptional regulation of the heterochronic gene lin-14 by lin-4 mediates temporal pattern formation in C. elegans. Cell 75, 855–862 (1993).
Jonas, S. & Izaurralde, E. Towards a molecular understanding of microRNA-mediated gene silencing. Nat. Rev. Genet. 16, 421–433 (2015).
Treiber, T., Treiber, N. & Meister, G. Regulation of microRNA biogenesis and its crosstalk with other cellular pathways. Nat. Rev. Mol. Cell Biol. 20, 5–20 (2019). Areview of current knowledge of the canonical and non-canonical miRNA biogenesis pathways.
Cortez, M. A. et al. MicroRNAs in body fluids–the mix of hormones and biomarkers. Nat. Rev. Clin. Oncol. 8, 467–477 (2011).
Chen, X., Liang, H., Zhang, J., Zen, K. & Zhang, C. Y. Secreted microRNAs: a new form of intercellular communication. Trends Cell Biol. 22, 125–132 (2012). A review of the mechanism of secreted miRNAs mediating intercellular communication.
Lee, Y., El Andaloussi, S. & Wood, M. J. Exosomes and microvesicles: extracellular vesicles for genetic information transfer and gene therapy. Hum. Mol. Genet. 21, R125–R134 (2012).
Guay, C. & Regazzi, R. Exosomes as new players in metabolic organ cross-talk. Diabetes Obes. Metab. 19 (Suppl 1), 137–146 (2017).
Iacomino, G. et al. Circulating microRNAs are deregulated in overweight/obese children: preliminary results of the I.Family study. Genes Nutr. 11, 7 (2016).
Ortega, F. J. et al. Profiling of circulating microRNAs reveals common microRNAs linked to type 2 diabetes that change with insulin sensitization. Diabetes Care 37, 1375–1383 (2014).
Guay, C. & Regazzi, R. Circulating microRNAs as novel biomarkers for diabetes mellitus. Nat. Rev. Endocrinol. 9, 513–521 (2013).
Pescador, N. et al. Serum circulating microRNA profiling for identification of potential type 2 diabetes and obesity biomarkers. PLOS ONE 8, e77251 (2013).
Zhang, J. et al. Exosome and exosomal microRNA: trafficking, sorting, and function. Genomics Proteom. Bioinforma. 13, 17–24 (2015).
Fabbri, M. MicroRNAs and miRceptors: a new mechanism of action for intercellular communication. Philos. Trans. R. Soc. Lond. B Biol. Sci. 373, 20160486 (2018).
Guilherme, A., Virbasius, J. V., Puri, V. & Czech, M. P. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat. Rev. Mol. Cell Biol. 9, 367–377 (2008).
Thomou, T. et al. Adipose-derived circulating miRNAs regulate gene expression in other tissues. Nature 542, 450–455 (2017). This is the first study reporting that adipose tissue-derived miRNAs are an important source of all circulating miRNAs and regulate the functions of distal metabolic organs in vivo.
Ying, W. et al. Adipose tissue macrophage-derived exosomal miRNAs can modulate in vivo and in vitro insulin sensitivity. Cell 171, 372–384 e12 (2017).
Ortega, F. J. et al. Targeting the circulating microRNA signature of obesity. Clin. Chem. 59, 781–792 (2013).
Castano, C., Kalko, S., Novials, A. & Parrizas, M. Obesity-associated exosomal miRNAs modulate glucose and lipid metabolism in mice. Proc. Natl Acad. Sci. USA 115, 12158–12163 (2018).
Al-Rawaf, H. A. Circulating microRNAs and adipokines as markers of metabolic syndrome in adolescents with obesity. Clin. Nutr. S0261-5614, 32462–32462 (2018).
Prats-Puig, A. et al. Changes in circulating microRNAs are associated with childhood obesity. J. Clin. Endocrinol. Metab. 98, E1655–E1660 (2013).
Hubal, M. J. et al. Circulating adipocyte-derived exosomal microRNAs associated with decreased insulin resistance after gastric bypass. Obesity (Silver Spring) 25, 102–110 (2017). In this biomarker study, the researchers used an adipocyte-specific marker of FABP4 to isolate adipocyte-derived exosomes in serum.
Ogawa, R. et al. Adipocyte-derived microvesicles contain RNA that is transported into macrophages and might be secreted into blood circulation. Biochem. Biophys. Res. Commun. 398, 723–729 (2010).
Villarroya, F., Cereijo, R., Villarroya, J. & Giralt, M. Brown adipose tissue as a secretory organ. Nat. Rev. Endocrinol. 13, 26–35 (2017).
Stephens, J. M. The fat controller: adipocyte development. PLOS Biol. 10, e1001436 (2012).
Weisberg, S. P. et al. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Invest. 112, 1796–1808 (2003).
Boutens, L. & Stienstra, R. Adipose tissue macrophages: going off track during obesity. Diabetologia 59, 879–894 (2016).
Russo, L. & Lumeng, C. N. Properties and functions of adipose tissue macrophages in obesity. Immunology 155, 407–417 (2018).
Zhang, Y. et al. Adipocyte-derived microvesicles from obese mice induce M1 macrophage phenotype through secreted miR-155. J. Mol. Cell Biol. 8, 505–517 (2016).
Flaherty, S. E. 3rd et al. A lipase-independent pathway of lipid release and immune modulation by adipocytes. Science 363, 989–993 (2019).
Kurowska-Stolarska, M. et al. MicroRNA-155 as a proinflammatory regulator in clinical and experimental arthritis. Proc. Natl Acad. Sci. USA 108, 11193–11198 (2011).
Yao, F. et al. Adipogenic miR-27a in adipose tissue upregulates macrophage activation via inhibiting PPARgamma of insulin resistance induced by high-fat diet-associated obesity. Exp. Cell Res. 355, 105–112 (2017).
Kang, T. et al. MicroRNA-27 (miR-27) targets prohibitin and impairs adipocyte differentiation and mitochondrial function in human adipose-derived stem cells. J. Biol. Chem. 288, 34394–34402 (2013).
Pan, Y. et al. Adipocyte-secreted exosomal microRNA-34a inhibits M2 macrophage polarization to promote obesity-induced adipose inflammation. J. Clin. Invest. 129, 834–849 (2019). This study demonstrates that adipocyte-specific knockout of miR-34a protects mice from HFD-induced glucose intolerance and insulin resistance.
Esau, C. et al. miR-122 regulation of lipid metabolism revealed by in vivo antisense targeting. Cell Metab. 3, 87–98 (2006).
Hsu, S. H. et al. Essential metabolic, anti-inflammatory, and anti-tumorigenic functions of miR-122 in liver. J. Clin. Invest. 122, 2871–2883 (2012).
Tsai, W. C. et al. MicroRNA-122 plays a critical role in liver homeostasis and hepatocarcinogenesis. J. Clin. Invest. 122, 2884–2897 (2012).
Hou, J. et al. Identification of miRNomes in human liver and hepatocellular carcinoma reveals miR-199a/b-3p as therapeutic target for hepatocellular carcinoma. Cancer Cell 19, 232–243 (2011).
Miyaaki, H. et al. Significance of serum and hepatic microRNA-122 levels in patients with non-alcoholic fatty liver disease. Liver Int. 34, e302–e307 (2014).
Pirola, C. J. et al. Circulating microRNA signature in non-alcoholic fatty liver disease: from serum non-coding RNAs to liver histology and disease pathogenesis. Gut 64, 800–812 (2015).
Younossi, Z. M. Non-alcoholic fatty liver disease - a global public health perspective. J. Hepatol. 70, 531–544 (2019).
Heneghan, H. M., Miller, N., McAnena, O. J., O’Brien, T. & Kerin, M. J. Differential miRNA expression in omental adipose tissue and in the circulation of obese patients identifies novel metabolic biomarkers. J. Clin. Endocrinol. Metab. 96, E846–E850 (2011).
Baranova, A., Maltseva, D. & Tonevitsky, A. Adipose may actively delay progression of NAFLD by releasing tumor-suppressing, anti-fibrotic miR-122 into circulation. Obes. Rev. 20, 108–118 (2019).
Yu, Y. et al. Adipocyte-derived exosomal mir-27a induces insulin resistance in skeletal muscle through repression of PPARgamma. Theranostics 8, 2171–2188 (2018).
Nunez Lopez, Y. O., Garufi, G. & Seyhan, A. A. Altered levels of circulating cytokines and microRNAs in lean and obese individuals with prediabetes and type 2 diabetes. Mol. Biosyst. 13, 106–121 (2016).
Wang, Y. C. et al. Circulating miR-130b mediates metabolic crosstalk between fat and muscle in overweight/obesity. Diabetologia 56, 2275–2285 (2013).
US National Library of Medicine. ClinicalTrials.gov [online], https://clinicaltrials.gov/ct2/show/NCT02459106 (2015).
Mziaut, H. et al. miR-132 controls pancreatic beta cell proliferation and survival in mouse model through the Pten/Akt/Foxo3 signaling. bioRxiv, 233098 (2018).
Dusaulcy, R. et al. miR-132-3p is a positive regulator of alpha-cell mass and is downregulated in obese hyperglycemic mice. Mol. Metab. 22, 84–95 (2019).
Chen, Y. et al. Exosomal microRNA miR-92a concentration in serum reflects human brown fat activity. Nat. Commun. 7, 11420 (2016).
Holmes, D. Adipose tissue: miR-92a hits the mark. Nat. Rev. Endocrinol. 12, 373 (2016).
Setyowati Karolina, D., Sepramaniam, S., Tan, H. Z., Armugam, A. & Jeyaseelan, K. miR-25 and miR-92a regulate insulin I biosynthesis in rats. RNA Biol. 10, 1365–1378 (2013).
Cui, X. et al. Change in circulating microRNA profile of obese children indicates future risk of adult diabetes. Metabolism 78, 95–105 (2018).
Chistiakov, D. A., Melnichenko, A. A., Myasoedova, V. A., Grechko, A. V. & Orekhov, A. N. Mechanisms of foam cell formation in atherosclerosis. J. Mol. Med. (Berl) 95, 1153–1165 (2017).
Xie, Z. et al. Adipose-derived exosomes exert proatherogenic effects by regulating macrophage foam cell formation and polarization. J. Am. Heart Assoc. 7, e007442 (2018).
Li, F. et al. Exosomal microRNA-29a mediates cardiac dysfunction and mitochondrial inactivity in obesity-related cardiomyopathy. Endocrine 63, 480–488 (2019).
Nie, H., Pan, Y. & Zhou, Y. Exosomal microRNA-194 causes cardiac injury and mitochondrial dysfunction in obese mice. Biochem. Biophys. Res. Commun. 503, 3174–3179 (2018).
Zou, T. et al. MicroRNA-410-5p exacerbates high-fat diet-induced cardiac remodeling in mice in an endocrine fashion. Sci. Rep. 8, 8780 (2018).
Patel, V. B., Shah, S., Verma, S. & Oudit, G. Y. Epicardial adipose tissue as a metabolic transducer: role in heart failure and coronary artery disease. Heart Fail. Rev. 22, 889–902 (2017).
Mitchell, P. S. et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc. Natl Acad. Sci. USA 105, 10513–10518 (2008).
Chen, X. et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 18, 997–1006 (2008).
Gallo, W., Esguerra, J. L. S., Eliasson, L. & Melander, O. miR-483-5p associates with obesity and insulin resistance and independently associates with new onset diabetes mellitus and cardiovascular disease. PLOS ONE 13, e0206974 (2018).
Ghorbani, S. et al. Decreased serum microRNA-21 level is associated with obesity in healthy and type 2 diabetic subjects. Arch. Physiol. Biochem. 124, 300–305 (2018).
Galanakis, C. G. et al. Computed tomography-based assessment of abdominal adiposity changes and their impact on metabolic alterations following bariatric surgery. World J. Surg. 39, 417–423 (2015).
Hsieh, C. H. et al. Weight-reduction through a low-fat diet causes differential expression of circulating microRNAs in obese C57BL/6 mice. BMC Genomics 16, 699 (2015).
Manning, P. et al. Acute weight loss restores dysregulated circulating microRNAs in individuals who are obese. J. Clin. Endocrinol. Metab. 104, 1239–1248 (2019).
Tabet, F. et al. High-density lipoprotein-associated miR-223 is altered after diet-induced weight loss in overweight and obese males. PLOS ONE 11, e0151061 (2016).
Russo, A. et al. Physical activity modulates the overexpression of the inflammatory miR-146a-5p in obese patients. IUBMB Life 70, 1012–1022 (2018).
Parrizas, M. et al. Circulating miR-192 and miR-193b are markers of prediabetes and are modulated by an exercise intervention. J. Clin. Endocrinol. Metab. 100, E407–E415 (2015).
Donghui, T. et al. Improvement of microvascular endothelial dysfunction induced by exercise and diet is associated with microRNA-126 in obese adolescents. Microvasc. Res. 123, 86–91 (2019).
Kumar, S. & Kelly, A. S. Review of childhood obesity: from epidemiology, etiology, and comorbidities to clinical assessment and treatment. Mayo Clin. Proc. 92, 251–265 (2017).
Juonala, M. et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N. Engl. J. Med. 365, 1876–1885 (2011).
Yun, J. E. et al. Association of the leptin to high-molecular-weight adiponectin ratio with metabolic syndrome. Endocr. J. 58, 807–815 (2011).
Feinleib, M., Kannel, W. B., Garrison, R. J., McNamara, P. M. & Castelli, W. P. The Framingham Offspring Study. design and preliminary data. Prev. Med. 4, 518–525 (1975).
Shah, R. et al. Extracellular RNAs are associated with insulin resistance and metabolic phenotypes. Diabetes Care 40, 546–553 (2017).
Brandt, S. et al. Circulating levels of miR-122 and nonalcoholic fatty liver disease in pre-pubertal obese children. Pediatr. Obes. 13, 175–182 (2018).
Willeit, P. et al. Circulating microRNA-122 is associated with the risk of new-onset metabolic syndrome and type 2 diabetes. Diabetes 66, 347–357 (2017).
Hindson, C. M. et al. Absolute quantification by droplet digital PCR versus analog real-time PCR. Nat. Methods 10, 1003–1005 (2013).
Quan, P. L., Sauzade, M. & Brouzes, E. dPCR: a technology review. Sensors 18, 1271 (2018).
Gu, Y. et al. An exploration of nucleic acid liquid biopsy using a glucose meter. Chem. Sci. 9, 3517–3522 (2018).
Luck, M. E., Muljo, S. A. & Collins, C. B. Prospects for therapeutic targeting of microRNAs in human immunological diseases. J. Immunol. 194, 5047–5052 (2015).
Sethupathy, P. The promise and challenge of therapeutic microRNA silencing in diabetes and metabolic diseases. Curr. Diab. Rep. 16, 52 (2016).
Simion, V. et al. Pharmacomodulation of microRNA expression in neurocognitive diseases: obstacles and future opportunities. Curr. Neuropharmacol. 15, 276–290 (2017).
Catela Ivkovic, T., Voss, G., Cornella, H. & Ceder, Y. microRNAs as cancer therapeutics: a step closer to clinical application. Cancer Lett. 407, 113–122 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT00979927 (2009).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01200420 (2010).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01646489 (2012).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT00688012 (2008).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01872936 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01727934 (2012).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02508090 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02452814 (2014).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01829971 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02862145 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02369198 (2014).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02580552 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03713320 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03603431 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02603224 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03601052 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02826525 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02612662 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02579187 (2015).
Lares, M. R., Rossi, J. J. & Ouellet, D. L. RNAi and small interfering RNAs in human disease therapeutic applications. Trends Biotechnol. 28, 570–579 (2010).
FDA. FDA approves first-of-its kind targeted RNA-based therapy to treat a rare disease. FDA www.fda.gov, https://www.fda.gov/news-events/press-announcements/fda-approves-first-its-kind-targeted-rna-based-therapy-treat-rare-disease.
Lindow, M. & Kauppinen, S. Discovering the first microRNA-targeted drug. J. Cell Biol. 199, 407–412 (2012).
Janssen, H. L. et al. Treatment of HCV infection by targeting microRNA. N. Engl. J. Med. 368, 1685–1694 (2013). The study reports clinical trial results for miravirsen for the treatment of HCV infection. Miravirsen was the first miRNA-targeted drug to enter human clinical trials.
Rupaimoole, R. & Slack, F. J. MicroRNA therapeutics: towards a new era for the management of cancer and other diseases. Nat. Rev. Drug. Discov. 16, 203–222 (2017). A review focused on miRNA-based therapies.
Zaiou, M., El Amri, H. & Bakillah, A. The clinical potential of adipogenesis and obesity-related microRNAs. Nutr. Metab. Cardiovasc. Dis. 28, 91–111 (2018).
Trajkovski, M. et al. MicroRNAs 103 and 107 regulate insulin sensitivity. Nature 474, 649–653 (2011).
Xihua, L. et al. Circulating miR-143-3p inhibition protects against insulin resistance in metabolic syndrome via targeting of the insulin-like growth factor 2 receptor. Transl. Res. 205, 33–43 (2018).
Fu, T. et al. MicroRNA 34a inhibits beige and brown fat formation in obesity in part by suppressing adipocyte fibroblast growth factor 21 signaling and SIRT1 function. Mol. Cell Biol. 34, 4130–4142 (2014).
Sun, L. & Trajkovski, M. MiR-27 orchestrates the transcriptional regulation of brown adipogenesis. Metabolism 63, 272–282 (2014).
Wang, W., Wang, J., Yan, M., Jiang, J. & Bian, A. MiRNA-92a protects pancreatic B-cell function by targeting KLF2 in diabetes mellitus. Biochem. Biophys. Res. Commun. 500, 577–582 (2018).
Huang-Doran, I., Zhang, C. Y. & Vidal-Puig, A. Extracellular vesicles: novel mediators of cell communication in metabolic disease. Trends Endocrinol. Metab. 28, 3–18 (2017).
Ohno, S. et al. Systemically injected exosomes targeted to EGFR deliver antitumor microRNA to breast cancer cells. Mol. Ther. 21, 185–191 (2013).
Naseri, Z., Oskuee, R. K., Jaafari, M. R. & Forouzandeh Moghadam, M. Exosome-mediated delivery of functionally active miRNA-142-3p inhibitor reduces tumorigenicity of breast cancer in vitro and in vivo. Int. J. Nanomed. 13, 7727–7747 (2018).
Armstrong, J. P., Holme, M. N. & Stevens, M. M. Re-engineering extracellular vesicles as smart nanoscale therapeutics. ACS Nano 11, 69–83 (2017).
Beuzelin, D. & Kaeffer, B. Exosomes and miRNA-loaded biomimetic nanovehicles, a focus on their potentials preventing type-2 diabetes linked to metabolic syndrome. Front. Immunol. 9, 2711 (2018).
Li, Z. et al. In vitro and in vivo RNA inhibition by CD9-HuR functionalized exosomes encapsulated with miRNA or CRISPR/dCas9. Nano Lett. 19, 19–28 (2018).
Santangelo, L. et al. The RNA-binding protein SYNCRIP is a component of the hepatocyte exosomal machinery controlling microRNA sorting. Cell Rep. 17, 799–808 (2016).
Villarroya-Beltri, C. et al. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat. Commun. 4, 2980 (2013).
Hoshino, A. et al. Tumour exosome integrins determine organotropic metastasis. Nature 527, 329–335 (2015).
Hoshino, D. et al. Exosome secretion is enhanced by invadopodia and drives invasive behavior. Cell Rep. 5, 1159–1168 (2013).
Christianson, H. C., Svensson, K. J., van Kuppevelt, T. H., Li, J. P. & Belting, M. Cancer cell exosomes depend on cell-surface heparan sulfate proteoglycans for their internalization and functional activity. Proc. Natl Acad. Sci. USA 110, 17380–17385 (2013).
Ostrowski, M. et al. Rab27a and Rab27b control different steps of the exosome secretion pathway. Nat. Cell Biol. 12, 19–30 (2010).
Kalinava, N. et al. C. elegans heterochromatin factor set-32 plays an essential role in transgenerational establishment of nuclear RNAi-mediated epigenetic silencing. Cell Rep. 25, 2273–2284.e3 (2018).
Acknowledgements
The authors acknowledge the support of the National Natural Science Foundation of China (grant nos 81200642, 81670773 and 81770866) and the Jiangsu Provincial Key Research and Development Programme (grant nos BE2016619 and BE2018614).
Author information
Authors and Affiliations
Contributions
C.J. and X.G. provided a substantial contribution to discussion of content, wrote the article and reviewed and edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Endocrinology thanks J.-M. Fernandez-Real and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Exosomes
-
Homogenous extracellular vesicles (40–100 nm) that originate from the endocytic recycling pathway, with specific markers such as CD9, CD63, ALIX, flotillin 1 and TSG101.
- Microvesicles
-
Heterogeneous extracellular vesicles (50–1,000 nm) that are produced directly through the outward budding and fission of membrane vesicles from the plasma membrane with no definite markers.
- Lipodystrophy
-
A genetic or acquired disorder characterized by a lack of adipose tissue.
- Nonalcoholic steatohepatitis
-
(NASH). A severe form of nonalcoholic fatty liver disease characterized by abnormal accumulation of fat and liver inflammation that is not caused by alcohol abuse, which might lead to complications such as cirrhosis, liver cancer and liver failure.
- Polypyrimidine tract-binding protein 1
-
(PTBP1). A protein that can stabilize insulin mRNA and facilitate insulin translation.
- Macrophage foam cell
-
A type of macrophage containing cholesterol with a foamy appearance that has a key role in the development of atherosclerosis.
- Droplet digital PCR
-
A technique used to quantify the absolute copies of nucleic acids directly.
- Small interfering RNAs
-
A class of exogenous double-stranded RNA molecules, 20–25 base pairs in length, similar to microRNAs, and used widely as a gene silencing tool.
- Keloids
-
A type of fibrous scar tissue.
Rights and permissions
About this article
Cite this article
Ji, C., Guo, X. The clinical potential of circulating microRNAs in obesity. Nat Rev Endocrinol 15, 731–743 (2019). https://doi.org/10.1038/s41574-019-0260-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-019-0260-0
This article is cited by
-
DNA-based molecular classifiers for the profiling of gene expression signatures
Journal of Nanobiotechnology (2024)
-
CVD phenotyping in oncologic disorders: cardio-miRNAs as a potential target to improve individual outcomes in revers cardio-oncology
Journal of Translational Medicine (2024)
-
Inter-organ crosstalk during development and progression of type 2 diabetes mellitus
Nature Reviews Endocrinology (2024)
-
Identification of a circulating three-miRNA panel for the diagnosis of primary open angle glaucoma
International Ophthalmology (2024)
-
Dynamics of serum exosome microRNA profile altered by chemically induced estropause and rescued by estrogen therapy in female mice
GeroScience (2024)