Abstract
Endometriosis is a chronic inflammatory disease defined as the presence of endometrial tissue outside the uterus, which causes pelvic pain and infertility. This disease should be viewed as a public health problem with a major effect on the quality of life of women as well as being a substantial economic burden. In light of the considerable progress with diagnostic imaging (for example, transvaginal ultrasound and MRI), exploratory laparoscopy should no longer be used to diagnose endometriotic lesions. Instead, diagnosis of endometriosis should be based on a structured process involving the combination of patient interviews, clinical examination and imaging. Notably, a diagnosis of endometriosis often leads to immediate surgery. Therefore, rethinking the diagnosis and management of endometriosis is warranted. Instead of assessing endometriosis on the day of the diagnosis, gynaecologists should consider the patient’s ‘endometriosis life’. Medical treatment is the first-line therapeutic option for patients with pelvic pain and no desire for immediate pregnancy. In women with infertility, careful consideration should be made regarding whether to provide assisted reproductive technologies prior to performing endometriosis surgery. Modern endometriosis management should be individualized with a patient-centred, multi-modal and interdisciplinary integrated approach.
Key points
-
Endometriosis is a chronic, inflammatory, hormonal, immune, systemic and heterogeneous disease with three different phenotypes (superficial, ovarian endometrioma and deep infiltrating endometriosis), which is associated with adenomyosis in 30% of patients.
-
Diagnosis of endometriosis (and adenomyosis) should be based on patient interviews, examination and imaging; endometriosis diagnosis should no longer be considered synonymous with immediate surgery.
-
Modern management of endometriosis should be patient focused rather than focused on the endometriotic lesions; medical treatment can be administered without histological confirmation.
-
Pain symptoms should be treated without delay to avoid central sensitization, as this can become autonomous, occurring independently of the peripheral stimulus, and can explain coexisting chronic pain syndromes.
-
Medical treatment should be the first therapeutic option for patients with pelvic pain who have no immediate desire for pregnancy; assisted reproductive technologies can be performed without previous surgery for selected patients with infertility.
-
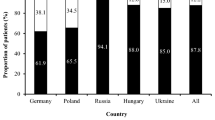
Endometriosis management should be individualized according to the patient’s intentions and priorities; management strategies can vary from country to country as pain perception and health-care systems differ around the world.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Sampson, J. A. Peritoneal endometriosis due to premenstrual dissemination of endometrial tissue into the peritoneal cavity. Am. J. Obstet. Gynecol. 14, 422–469 (1927).
Giudice, L. C. & Kao, L. C. Endometriosis. Lancet 364, 1789–1799 (2004).
Berkley, K. J., Rapkin, A. J. & Papka, R. E. The pains of endometriosis. Science 308, 1587–1589 (2005).
de Ziegler, D., Borghese, B. & Chapron, C. Endometriosis and infertility: pathophysiology and management. Lancet 376, 730–738 (2010).
Hurd, W. W. Criteria that indicate endometriosis is the cause of chronic pelvic pain. Obstet. Gynecol. 92, 1029–1032 (1998).
Hammerli, S. et al. Does endometriosis affect sexual activity and satisfaction of the man partner? a comparison of partners from women diagnosed with endometriosis and controls. J. Sex. Med. 15, 853–865 (2018).
Simoens, S. et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum. Reprod. 27, 1292–1299 (2012).
Nnoaham, K. E. et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil. Steril. 96, 366–373.e8 (2011).
Pluchino, N. et al. Sexual function in endometriosis patients and their partners: effect of the disease and consequences of treatment. Hum. Reprod. Update 22, 762–774 (2016).
Chen, L. C. et al. Risk of developing major depression and anxiety disorders among women with endometriosis: a longitudinal follow-up study. J. Affect. Disord. 190, 282–285 (2016).
Ramin-Wright, A. et al. Fatigue - a symptom in endometriosis. Hum. Reprod. 33, 1459–1465 (2018).
Fourquet, J., Baez, L., Figueroa, M., Iriarte, R. I. & Flores, I. Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertil. Steril. 96, 107–112 (2011).
Soliman, A. M. et al. The effect of endometriosis symptoms on absenteeism and presenteeism in the workplace and at home. J. Manag. Care Spec. Pharm. 23, 745–754 (2017).
Soliman, A. M., Yang, H., Du, E. X., Kelley, C. & Winkel, C. The direct and indirect costs associated with endometriosis: a systematic literature review. Hum. Reprod. 31, 712–722 (2016).
Chapron, C. et al. Surgery for bladder endometriosis: long-term results and concomitant management of associated posterior deep lesions. Hum. Reprod. 25, 884–889 (2010).
Menni, K., Facchetti, L. & Cabassa, P. Extragenital endometriosis: assessment with MR imaging. A pictorial review. Br. J. Radiol. 89, 20150672 (2016).
Chapron, C. et al. Anatomical distribution of deeply infiltrating endometriosis: surgical implications and proposition for a classification. Hum. Reprod. 18, 157–161 (2003).
Redwine, D. B. Ovarian endometriosis: a marker for more extensive pelvic and intestinal disease. Fertil. Steril. 72, 310–315 (1999).
Chapron, C. et al. Associated ovarian endometrioma is a marker for greater severity of deeply infiltrating endometriosis. Fertil. Steril. 92, 453–457 (2009).
Revised American Fertility Society classification of endometriosis: 1985. Fertil. Steril. 43, 351-352 (1985).
Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil. Steril. 67, 817-821 (1997).
Leyendecker, G. et al. Adenomyosis and endometriosis. Re-visiting their association and further insights into the mechanisms of auto-traumatisation. An MRI study. Arch. Gynecol. Obstet. 291, 917–932 (2015).
Pinzauti, S. et al. Transvaginal sonographic features of diffuse adenomyosis in 18-30-year-old nulligravid women without endometriosis: association with symptoms. Ultrasound Obstet. Gynecol. 46, 730–736 (2015).
Chapron, C. et al. Relationship between the magnetic resonance imaging appearance of adenomyosis and endometriosis phenotypes. Hum. Reprod. 32, 1–9 (2017).
Guo, S. W., Mao, X., Ma, Q. & Liu, X. Dysmenorrhea and its severity are associated with increased uterine contractility and overexpression of oxytocin receptor (OTR) in women with symptomatic adenomyosis. Fertil. Steril. 99, 231–240 (2013).
Lazzeri, L. et al. Preoperative and postoperative clinical and transvaginal ultrasound findings of adenomyosis in patients with deep infiltrating endometriosis. Reprod. Sci. 21, 1027–1033 (2014).
Kunz, G. et al. Adenomyosis in endometriosis–prevalence and impact on fertility. Evidence from magnetic resonance imaging. Hum. Reprod. 20, 2309–2316 (2005).
Vercellini, P. et al. Uterine adenomyosis and in vitro fertilization outcome: a systematic review and meta-analysis. Hum. Reprod. 29, 964–977 (2014).
Naftalin, J. et al. Is adenomyosis associated with menorrhagia? Hum. Reprod. 29, 473–479 (2014).
Iacovides, S., Avidon, I. & Baker, F. C. What we know about primary dysmenorrhea today: a critical review. Hum. Reprod. Update 21, 762–778 (2015).
Cheong, Y., Cameron, I. T. & Critchley, H. O. D. Abnormal uterine bleeding. Br. Med. Bull. 123, 103–114 (2017).
Kishi, Y. et al. Four subtypes of adenomyosis assessed by magnetic resonance imaging and their specification. Am. J. Obstet. Gynecol. 207, 114.e1-7 (2012).
Vannuccini, S. et al. Potential influence of in utero and early neonatal exposures on the later development of endometriosis. Fertil. Steril. 105, 997–1002 (2016).
Vercellini, P., Vigano, P., Somigliana, E. & Fedele, L. Endometriosis: pathogenesis and treatment. Nat. Rev. Endocrinol. 10, 261–275 (2014).
Chapron, C. et al. Deeply infiltrating endometriosis: pathogenetic implications of the anatomical distribution. Hum. Reprod. 21, 1839–1845 (2006).
Bricou, A., Batt, R. E. & Chapron, C. Peritoneal fluid flow influences anatomical distribution of endometriotic lesions: why Sampson seems to be right. Eur. J. Obstet. Gynecol. Reprod. Biol. 138, 127–134 (2008).
Kirschner, P. A. Porous diaphragm syndromes. Chest Surg. Clin. N. Am. 8, 449–472 (1998).
Legras, A. et al. Pneumothorax in women of child-bearing age: an update classification based on clinical and pathologic findings. Chest 145, 354–360 (2014).
Batt, R. E. et al. Mullerianosis. Histol. Histopathol. 22, 1161–1166 (2007).
Batt, R. E. & Yeh, J. Mullerianosis: four developmental (embryonic) mullerian diseases. Reprod. Sci. 20, 1030–1037 (2013).
Hufnagel, D., Li, F., Cosar, E., Krikun, G. & Taylor, H. S. The role of stem cells in the etiology and pathophysiology of endometriosis. Semin. Reprod. Med. 33, 333–340 (2015).
Jerman, L. F. & Hey-Cunningham, A. J. The role of the lymphatic system in endometriosis: a comprehensive review of the literature. Biol. Reprod. 92, 64 (2015).
Zondervan, K. T. et al. Endometriosis. Nat. Rev. Dis. Prim. 4, 9 (2018).
Samani, E. N. et al. Micrometastasis of endometriosis to distant organs in a murine model. Oncotarget 10, 2282–2291 (2019).
Bulun, S. E. Endometriosis. N. Engl J. Med. 360, 268–279 (2009).
Reis, F. M., Petraglia, F. & Taylor, R. N. Endometriosis: hormone regulation and clinical consequences of chemotaxis and apoptosis. Hum. Reprod. Update 19, 406–418 (2013).
Stefansson, H. et al. Genetic factors contribute to the risk of developing endometriosis. Hum. Reprod. 17, 555–559 (2002).
Treloar, S. A., O'Connor, D. T., O'Connor, V. M. & Martin, N. G. Genetic influences on endometriosis in an Australian twin sample. Fertil. Steril. 71, 701–710 (1999).
Saha, R. et al. Heritability of endometriosis. Fertil. Steril. 104, 947–952 (2015).
Rahmioglu, N., Missmer, S. A., Montgomery, G. W. & Zondervan, K. T. Insights into assessing the genetics of endometriosis. Curr. Obstet. Gynecol. Rep. 1, 124–137 (2012).
Rahmioglu, N., Montgomery, G. W. & Zondervan, K. T. Genetics of endometriosis. Womens Health 11, 577–586 (2015).
Treloar, S. et al. The international endogene study: a collection of families for genetic research in endometriosis. Fertil. Steril. 78, 679–685 (2002).
Treloar, S. A. et al. Genomewide linkage study in 1,176 affected sister pair families identifies a significant susceptibility locus for endometriosis on chromosome 10q26. Am. J. Hum. Genet. 77, 365–376 (2005).
Zondervan, K. T. et al. Significant evidence of one or more susceptibility loci for endometriosis with near-Mendelian inheritance on chromosome 7p13-15. Hum. Reprod. 22, 717–728 (2007).
Borghese, B., Zondervan, K. T., Abrao, M. S., Chapron, C. & Vaiman, D. Recent insights on the genetics and epigenetics of endometriosis. Clin. Genet. 91, 254–264 (2017).
Buck Louis, G. M. et al. Bisphenol A and phthalates and endometriosis: the endometriosis: natural history, diagnosis and outcomes study. Fertil. Steril. 100, 162–169.e1-2 (2013).
Upson, K. et al. Phthalates and risk of endometriosis. Environ. Res. 126, 91–97 (2013).
Martinez-Zamora, M. A. et al. Increased levels of dioxin-like substances in adipose tissue in patients with deep infiltrating endometriosis. Hum. Reprod. 30, 1059–1068 (2015).
Smarr, M. M., Kannan, K. & Buck Louis, G. M. Endocrine disrupting chemicals and endometriosis. Fertil. Steril. 106, 959–966 (2016).
Brosens, I. A. Endometriosis–a disease because it is characterized by bleeding. Am. J. Obstet. Gynecol. 176, 263–267 (1997).
Jain, S. & Dalton, M. E. Chocolate cysts from ovarian follicles. Fertil. Steril. 72, 852–856 (1999).
Vercellini, P. et al. 'Blood on the Tracks' from corpora lutea to endometriomas. BJOG 116, 366–371 (2009).
Laux-Biehlmann, A., d'Hooghe, T. & Zollner, T. M. Menstruation pulls the trigger for inflammation and pain in endometriosis. Trends Pharmacol. Sci. 36, 270–276 (2015).
Thaker, P. H. et al. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat. Med. 12, 939–944 (2006).
McKinnon, B. D., Bertschi, D., Bersinger, N. A. & Mueller, M. D. Inflammation and nerve fiber interaction in endometriotic pain. Trends Endocrinol. Metab. 26, 1–10 (2015).
Guo, S. W. Fibrogenesis resulting from cyclic bleeding: the Holy Grail of the natural history of ectopic endometrium. Hum. Reprod. 33, 353–356 (2018).
Evers, J. L. H. Is adolescent endometriosis a progressive disease that needs to be diagnosed and treated? Hum. Reprod. 28, 2023 (2013).
Fedele, L., Bianchi, S., Zanconato, G., Bettoni, G. & Gotsch, F. Long-term follow-up after conservative surgery for rectovaginal endometriosis. Am. J. Obstet. Gynecol. 190, 1020–1024 (2004).
Zhang, Q., Duan, J., Olson, M., Fazleabas, A. & Guo, S. W. Cellular changes consistent with epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation in the progression of experimental endometriosis in baboons. Reprod. Sci. 23, 1409–1421 (2016).
Zhang, Q., Duan, J., Liu, X. & Guo, S. W. Platelets drive smooth muscle metaplasia and fibrogenesis in endometriosis through epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation. Mol. Cell. Endocrinol. 428, 1–16 (2016).
Gonzalez-Foruria, I. et al. Dysregulation of the ADAM17/Notch signalling pathways in endometriosis: from oxidative stress to fibrosis. Mol. Hum. Reprod. 23, 488–499 (2017).
Borghese, B. et al. Gene expression profile for ectopic versus eutopic endometrium provides new insights into endometriosis oncogenic potential. Mol. Endocrinol. 22, 2557–2562 (2008).
Liu, X., Long, Q. & Guo, S. W. Surgical history and the risk of endometriosis: a hospital-based case-control study. Reprod. Sci. 23, 1217–1224 (2016).
Sibiude, J. et al. Association of history of surgery for endometriosis with severity of deeply infiltrating endometriosis. Obstet. Gynecol. 124, 709–717 (2014).
Long, Q., Liu, X. & Guo, S. W. Surgery accelerates the development of endometriosis in mice. Am. J. Obstet. Gynecol. 215, 320.e1–320.e15 (2016).
Long, Q., Liu, X., Qi, Q. & Guo, S. W. Chronic stress accelerates the development of endometriosis in mouse through adrenergic receptor β2. Hum. Reprod. 31, 2506–2519 (2016).
Streuli, I., Gaitzsch, H., Wenger, J. M. & Petignat, P. Endometriosis after menopause: physiopathology and management of an uncommon condition. Climacteric 20, 138–143 (2017).
Anaf, V. et al. Pain, mast cells, and nerves in peritoneal, ovarian, and deep infiltrating endometriosis. Fertil. Steril. 86, 1336–1343 (2006).
Anaf, V. et al. Relationship between endometriotic foci and nerves in rectovaginal endometriotic nodules. Hum. Reprod. 15, 1744–1750 (2000).
McKinnon, B. D., Kocbek, V., Nirgianakis, K., Bersinger, N. A. & Mueller, M. D. Kinase signalling pathways in endometriosis: potential targets for non-hormonal therapeutics. Hum. Reprod. Update 22, 382–403 (2016).
Woolf, C. J. Central sensitization: implications for the diagnosis and treatment of pain. Pain 152, S2–S15 (2011).
Aredo, J. V., Heyrana, K. J., Karp, B. I., Shah, J. P. & Stratton, P. Relating chronic pelvic pain and endometriosis to signs of sensitization and myofascial pain and dysfunction. Semin. Reprod. Med. 35, 88–97 (2017).
Hoffman, D. Central and peripheral pain generators in women with chronic pelvic pain: patient centered assessment and treatment. Curr. Rheumatol. Rev. 11, 146–166 (2015).
Woolf, C. J. & Salter, M. W. Neuronal plasticity: increasing the gain in pain. Science 288, 1765–1769 (2000).
As-Sanie, S. et al. Changes in regional gray matter volume in women with chronic pelvic pain: a voxel-based morphometry study. Pain 153, 1006–1014 (2012).
As-Sanie, S. et al. Functional connectivity is associated with altered brain chemistry in women with endometriosis-associated chronic pelvic pain. J. Pain. 17, 1–13 (2016).
Falcone, T. & Flyckt, R. Clinical management of endometriosis. Obstet. Gynecol. 131, 557–571 (2018).
Howard, F. M. Endometriosis and mechanisms of pelvic pain. J. Minim. Invasive Gynecol. 16, 540–550 (2009).
Khan, K. N. et al. Pelvic pain in women with ovarian endometrioma is mostly associated with coexisting peritoneal lesions. Hum. Reprod. 28, 109–118 (2013).
Odagiri, K. et al. Smooth muscle metaplasia and innervation in interstitium of endometriotic lesions related to pain. Fertil. Steril. 92, 1525–1531 (2009).
Tokushige, N. et al. Nerve fibers in ovarian endometriomas. Fertil. Steril. 94, 1944-1947 (2010).
Zhang, X. et al. Nerve fibres in ovarian endometriotic lesions in women with ovarian endometriosis. Hum. Reprod. 25, 392–397 (2010).
Chapron, C. et al. Deep infiltrating endometriosis: relation between severity of dysmenorrhoea and extent of disease. Hum. Reprod. 18, 760–766 (2003).
Sampson, J. A. Intestinal adenomas of endometrial type: their importance and their relation to ovarian hematomas of endometrial type (perforating hemorrhagic cysts of the ovary). Arch. Surg. 5, 217–280 (1922).
Chapron, C. et al. Ovarian endometrioma: severe pelvic pain is associated with deeply infiltrating endometriosis. Hum. Reprod. 27, 702–711 (2012).
Fauconnier, A. et al. Relation between pain symptoms and the anatomic location of deep infiltrating endometriosis. Fertil. Steril. 78, 719–726 (2002).
Fauconnier, A. & Chapron, C. Endometriosis and pelvic pain: epidemiological evidence of the relationship and implications. Hum. Reprod. Update 11, 595–606 (2005).
Vercellini, P. et al. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: a multivariate analysis of over 1000 patients. Hum. Reprod. 22, 266–271 (2007).
Koninckx, P. R., Meuleman, C., Demeyere, S., Lesaffre, E. & Cornillie, F. J. Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil. Steril. 55, 759–765 (1991).
Raffi, F., Metwally, M. & Amer, S. The impact of excision of ovarian endometrioma on ovarian reserve: a systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 97, 3146–3154 (2012).
Santulli, P. et al. Endometriosis-related infertility: ovarian endometrioma per se is not associated with presentation for infertility. Hum. Reprod. 31, 1765–1775 (2016).
Leone Roberti Maggiore, U., Scala, C., Venturini, P. L., Remorgida, V. & Ferrero, S. Endometriotic ovarian cysts do not negatively affect the rate of spontaneous ovulation. Hum. Reprod. 30, 299–307 (2015).
Ferrero, S. et al. Second surgery for recurrent unilateral endometriomas and impact on ovarian reserve: a case-control study. Fertil. Steril. 103, 1236–1243 (2015).
Streuli, I. et al. In women with endometriosis anti-Mullerian hormone levels are decreased only in those with previous endometrioma surgery. Hum. Reprod. 27, 3294–3303 (2012).
Muzii, L. et al. Histologic analysis of endometriomas: what the surgeon needs to know. Fertil. Steril. 87, 362–366 (2007).
Gellersen, B. & Brosens, J. J. Cyclic decidualization of the human endometrium in reproductive health and failure. Endocr. Rev. 35, 851–905 (2014).
Marcellin, L. et al. Endometriosis also affects the decidua in contact with the fetal membranes during pregnancy. Hum. Reprod. 30, 392–405 (2015).
Vannuccini, S. et al. Infertility and reproductive disorders: impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum. Reprod. Update 22, 104–115 (2016).
Zullo, F. et al. Endometriosis and obstetrics complications: a systematic review and meta-analysis. Fertil. Steril. 108, 667–672.e5 (2017).
Lalani, S. et al. Endometriosis and adverse maternal, fetal and neonatal outcomes, a systematic review and meta-analysis. Hum. Reprod. 33, 1854–1865 (2018).
Glavind, M. T., Forman, A., Arendt, L. H., Nielsen, K. & Henriksen, T. B. Endometriosis and pregnancy complications: a Danish cohort study. Fertil. Steril. 107, 160–166 (2017).
Nirgianakis, K. et al. Obstetric complications after laparoscopic excision of posterior deep infiltrating endometriosis: a case-control study. Fertil. Steril. 110, 459–466 (2018).
Somigliana, E. et al. Management of endometriosis in the infertile patient. Semin. Reprod. Med. 35, 31–37 (2017).
Scala, C. et al. Influence of adenomyosis on pregnancy and perinatal outcomes in women with endometriosis. Ultrasound Obstet. Gynecol. 52, 666–671 (2018).
Juang, C. M. et al. Adenomyosis and risk of preterm delivery. BJOG 114, 165–169 (2007).
Hashimoto, A. et al. Adenomyosis and adverse perinatal outcomes: increased risk of second trimester miscarriage, preeclampsia, and placental malposition. J. Matern. Fetal Neonatal Med. 31, 364–369 (2018).
Yamaguchi, A. et al. Risk of preterm birth, low birthweight, and small-for-gestational-age infants in pregnancies with adenomyosis: a cohort study of the Japan Environment and Children’s Study. Acta Obstet. Gynecol. Scand. 98, 359–364 (2018).
Alberico, D. et al. Potential benefits of pregnancy on endometriosis symptoms. Eur. J. Obstet. Gynecol. Reprod. Biol. 230, 182–187 (2018).
Porpora, M. G. et al. Pain and ovarian endometrioma recurrence after laparoscopic treatment of endometriosis: a long-term prospective study. Fertil. Steril. 93, 716–721 (2010).
Busacca, M. et al. Determinants of long-term clinically detected recurrence rates of deep, ovarian, and pelvic endometriosis. Am. J. Obstet. Gynecol. 195, 426–432 (2006).
Zaytsev, P. & Taxy, J. B. Pregnancy-associated ectopic decidua. Am. J. Surgical Pathol. 11, 526–530 (1987).
McArthur, J. W. & Ulfelder, H. The effect of pregnancy upon endometriosis. Obstet. Gynecol. Surv. 20, 709–733 (1965).
Coccia, M. E., Rizzello, F., Palagiano, A. & Scarselli, G. The effect of the hormonal milieu of pregnancy on deep infiltrating endometriosis: serial ultrasound assessment of changes in size and pattern of deep endometriotic lesions. Eur. J. Obstet. Gynecol. Reprod. Biol. 160, 35–39 (2012).
Leone Roberti Maggiore, U. et al. A systematic review on endometriosis during pregnancy: diagnosis, misdiagnosis, complications and outcomes. Hum. Reprod. Update 22, 70–103 (2016).
Sinaii, N. et al. Differences in characteristics among 1,000 women with endometriosis based on extent of disease. Fertil. Steril. 89, 538–545 (2008).
Chapron, C. et al. Factors and regional differences associated with endometriosis: a multi-country, case-control study. Adv. Ther. 33, 1385–1407 (2016).
Ballweg, M. L. Impact of endometriosis on women's health: comparative historical data show that the earlier the onset, the more severe the disease. Best Pract. Res. Clin. Obstet. Gynaecol. 18, 201–221 (2004).
Chapron, C. et al. Magnetic resonance imaging and endometriosis: deeply infiltrating endometriosis does not originate from the rectovaginal septum. Gynecol. Obstet. Invest. 53, 204–208 (2002).
Chapron, C. et al. Routine clinical examination is not sufficient for the diagnosis and establishing the location of deeply infiltrating endometriosis. J. Am. Assoc. Gynecol. Laparosc. 9, 115–119 (2002).
Koninckx, P., Meuleman, C., Oosterlynck, D. & Cornillie, F. Diagnosis of deep endometriosis by clinical examination during menstruation and plasma CA-125 concentration. Fertil. Steril. 65, 280–287 (1996).
Guerriero, S. et al. Transvaginal ultrasound vs magnetic resonance imaging for diagnosing deep infiltrating endometriosis: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 51, 586–595 (2018).
Guerriero, S. et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: a consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet. Gynecol. 48, 318–332 (2016).
Van den Bosch, T. & Van Schoubroeck, D. Ultrasound diagnosis of endometriosis and adenomyosis: state of the art. Best Pract. Res. Clin. Obstet. Gynaecol. 51, 16–24 (2018).
Guerriero, S. et al. Deep infiltrating endometriosis: comparison between 2-dimensional ultrasonography (US), 3-dimensional US, and magnetic resonance imaging. J. Ultrasound Med. 37, 1511–1521 (2018).
Nisenblat, V., Bossuyt, P. M., Farquhar, C., Johnson, N. & Hull, M. L. Imaging modalities for the non-invasive diagnosis of endometriosis. Cochrane Database Syst. Rev. 2, CD009591 (2016).
Van den Bosch, T. et al. A sonographic classification and reporting system for diagnosing adenomyosis. Ultrasound Obstet. Gynecol. 53, 576–582 (2018).
Chapron, C. et al. Severe ureteral endometriosis: the intrinsic type is not so rare after complete surgical exeresis of deep endometriotic lesions. Fertil. Steril. 93, 2115–2120 (2010).
Seracchioli, R. et al. Importance of retroperitoneal ureteric evaluation in cases of deep infiltrating endometriosis. J. Minim. Invasive Gynecol. 15, 435–439 (2008).
Goncalves, M. O., Podgaec, S., Dias, J. A. Jr., Gonzalez, M. & Abrao, M. S. Transvaginal ultrasonography with bowel preparation is able to predict the number of lesions and rectosigmoid layers affected in cases of deep endometriosis, defining surgical strategy. Hum. Reprod. 25, 665–671 (2010).
Piketty, M. et al. Preoperative work-up for patients with deeply infiltrating endometriosis: transvaginal ultrasonography must definitely be the first-line imaging examination. Hum. Reprod. 24, 602–607 (2009).
Ling, F. W. Randomized controlled trial of depot leuprolide in patients with chronic pelvic pain and clinically suspected endometriosis. Pelvic Pain Study Group. Obstet. Gynecol. 93, 51–58 (1999).
Petraglia, F. et al. Reduced pelvic pain in women with endometriosis: efficacy of long-term dienogest treatment. Arch. Gynecol. Obstet. 285, 167–173 (2012).
Vercellini, P. et al. Surgical versus medical treatment for endometriosis-associated severe deep dyspareunia: I. Effect on pain during intercourse and patient satisfaction. Hum. Reprod. 27, 3450–3459 (2012).
Brown, J., Crawford, T. J., Allen, C., Hopewell, S. & Prentice, A. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. Cochrane Database Syst. Rev. 1, CD004753 (2017).
Streuli, I. et al. An update on the pharmacological management of endometriosis. Expert. Opin. Pharmacother. 14, 291–305 (2013).
Santulli, P. et al. MAP kinases and the inflammatory signaling cascade as targets for the treatment of endometriosis? Expert Opin. Ther. Targets 19, 1465–1483 (2015).
Graziottin, A. The shorter, the better: a review of the evidence for a shorter contraceptive hormone-free interval. Eur. J. Contracept. Reprod. Health Care 21, 93–105 (2016).
Ferrero, S., Alessandri, F., Racca, A. & Leone Roberti Maggiore, U. Treatment of pain associated with deep endometriosis: alternatives and evidence. Fertil. Steril. 104, 771–792 (2015).
Chapron, C. et al. Oral contraceptives and endometriosis: the past use of oral contraceptives for treating severe primary dysmenorrhea is associated with endometriosis, especially deep infiltrating endometriosis. Hum. Reprod. 26, 2028–2035 (2011).
Ferrero, S., Evangelisti, G. & Barra, F. Current and emerging treatment options for endometriosis. Expert Opin. Pharmacother. 19, 1109–1125 (2018).
Taylor, H. S. et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N. Engl. J. Med. 377, 28–40 (2017).
Vercellini, P. et al. Medical treatment of endometriosis-related pain. Best Pract. Res. Clin. Obstet. Gynaecol. 51, 68–91 (2018).
Vercellini, P. et al. Estrogen-progestins and progestins for the management of endometriosis. Fertil. Steril. 106, 1552–1571.e2 (2016).
Brown, J., Pan, A. & Hart, R. J. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst. Rev. 12, CD008475 (2010).
Olive, D. L. Optimizing gonadotropin-releasing hormone agonist therapy in women with endometriosis. Treat. Endocrinol. 3, 83–89 (2004).
DiVasta, A. D. et al. Hormonal add-back therapy for females treated with gonadotropin-releasing hormone agonist for endometriosis: a randomized controlled trial. Obstet. Gynecol. 126, 617–627 (2015).
Seracchioli, R. et al. Long-term oral contraceptive pills and postoperative pain management after laparoscopic excision of ovarian endometrioma: a randomized controlled trial. Fertil. Steril. 94, 464–471 (2010).
Vercellini, P. et al. Comparison of a levonorgestrel-releasing intrauterine device versus expectant management after conservative surgery for symptomatic endometriosis: a pilot study. Fertil. Steril. 80, 305–309 (2003).
Tanmahasamut, P. et al. Postoperative levonorgestrel-releasing intrauterine system for pelvic endometriosis-related pain: a randomized controlled trial. Obstet. Gynecol. 119, 519–526 (2012).
Vercellini, P. et al. Postoperative oral contraceptive exposure and risk of endometrioma recurrence. Am. J. Obstet. Gynecol. 198, 504.e1-5 (2008).
Takamura, M. et al. Post-operative oral contraceptive use reduces the risk of ovarian endometrioma recurrence after laparoscopic excision. Hum. Reprod. 24, 3042–3048 (2009).
Seracchioli, R. et al. Long-term cyclic and continuous oral contraceptive therapy and endometrioma recurrence: a randomized controlled trial. Fertil. Steril. 93, 52–56 (2010).
Lee, D. Y., Bae, D. S., Yoon, B. K. & Choi, D. Post-operative cyclic oral contraceptive use after gonadotrophin-releasing hormone agonist treatment effectively prevents endometrioma recurrence. Hum. Reprod. 25, 3050–3054 (2010).
Cucinella, G. et al. Oral contraceptives in the prevention of endometrioma recurrence: does the different progestins used make a difference? Arch. Gynecol. Obstet. 288, 821–827 (2013).
Sulak, P. J., Kuehl, T. J., Ortiz, M. & Shull, B. L. Acceptance of altering the standard 21-day/7-day oral contraceptive regimen to delay menses and reduce hormone withdrawal symptoms. Am. J. Obstet. Gynecol. 186, 1142–1149 (2002).
Allaire, C. et al. An interdisciplinary approach to endometriosis-associated persistent pelvic pain. J. Endometr. Pelvic Pain Disord. 9, 77–86 (2017).
Vercellini, P. et al. Surgery for endometriosis-associated infertility: a pragmatic approach. Hum. Reprod. 24, 254–269 (2009).
Vercellini, P. et al. The effect of surgery for symptomatic endometriosis: the other side of the story. Hum. Reprod. Update 15, 177–188 (2009).
Carmona, F. et al. Does the learning curve of conservative laparoscopic surgery in women with rectovaginal endometriosis impair the recurrence rate? Fertil. Steril. 92, 868–875 (2009).
Busacca, M. et al. Postsurgical ovarian failure after laparoscopic excision of bilateral endometriomas. Am. J. Obstet. Gynecol. 195, 421–425 (2006).
Lessey, B. A. et al. Ovarian endometriosis and infertility: in vitro fertilization (IVF) or surgery as the first approach? Fertil. Steril. 110, 1218–1226 (2018).
Parker, J. D. et al. Persistence of dysmenorrhea and nonmenstrual pain after optimal endometriosis surgery may indicate adenomyosis. Fertil. Steril. 86, 711–715 (2006).
Somigliana, E. & Garcia-Velasco, J. A. Treatment of infertility associated with deep endometriosis: definition of therapeutic balances. Fertil. Steril. 104, 764–770 (2015).
Bendifallah, S. et al. Colorectal endometriosis-associated infertility: should surgery precede ART? Fertil. Steril. 108, 525–531.e4 (2017).
Bianchi, P. H. et al. Extensive excision of deep infiltrative endometriosis before in vitro fertilization significantly improves pregnancy rates. J. Minim. Invasive Gynecol. 16, 174–180 (2009).
Rossi, A. C. & Prefumo, F. The effects of surgery for endometriosis on pregnancy outcomes following in vitro fertilization and embryo transfer: a systematic review and meta-analysis. Arch. Gynecol. Obstet. 294, 647–655 (2016).
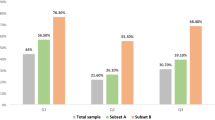
Maignien, C. et al. Prognostic factors for assisted reproductive technology in women with endometriosis-related infertility. Am. J. Obstet. Gynecol. 216, 280.e1–280.e9 (2017).
Coughlan, C. et al. Recurrent implantation failure: definition and management. Reprod. Biomed. Online 28, 14–38 (2014).
Littman, E. et al. Role of laparoscopic treatment of endometriosis in patients with failed in vitro fertilization cycles. Fertil. Steril. 84, 1574–1578 (2005).
Soriano, D. et al. Fertility outcome of laparoscopic treatment in patients with severe endometriosis and repeated in vitro fertilization failures. Fertil. Steril. 106, 1264–1269 (2016).
D'Hooghe, T. M., Denys, B., Spiessens, C., Meuleman, C. & Debrock, S. Is the endometriosis recurrence rate increased after ovarian hyperstimulation? Fertil. Steril. 86, 283–290 (2006).
van der Houwen, L. E. et al. Efficacy and safety of intrauterine insemination in patients with moderate-to-severe endometriosis. Reprod. Biomed. Online 28, 590–598 (2014).
Harb, H. M., Gallos, I. D., Chu, J., Harb, M. & Coomarasamy, A. The effect of endometriosis on in vitro fertilisation outcome: a systematic review and meta-analysis. BJOG 120, 1308–1320 (2013).
Hamdan, M., Omar, S. Z., Dunselman, G. & Cheong, Y. Influence of endometriosis on assisted reproductive technology outcomes: a systematic review and meta-analysis. Obstet. Gynecol. 125, 79–88 (2015).
Barbosa, M. A. et al. Impact of endometriosis and its staging on assisted reproduction outcome: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 44, 261–278 (2014).
Barnhart, K., Dunsmoor-Su, R. & Coutifaris, C. Effect of endometriosis on in vitro fertilization. Fertil. Steril. 77, 1148–1155 (2002).
Gupta, S., Agarwal, A., Agarwal, R. & Loret de Mola, J. R. Impact of ovarian endometrioma on assisted reproduction outcomes. Reprod. Biomed. Online 13, 349–360 (2006).
Hamdan, M., Dunselman, G., Li, T. C. & Cheong, Y. The impact of endometrioma on IVF/ICSI outcomes: a systematic review and meta-analysis. Hum. Reprod. Update 21, 809–825 (2015).
Yang, C., Geng, Y., Li, Y., Chen, C. & Gao, Y. Impact of ovarian endometrioma on ovarian responsiveness and IVF: a systematic review and meta-analysis. Reprod. Biomed. Online 31, 9–19 (2015).
Bourdon, M. et al. Endometriosis and ART: a prior history of surgery for OMA is associated with a poor ovarian response to hyperstimulation. PLOS ONE 13, e0202399 (2018).
Younes, G. & Tulandi, T. Effects of adenomyosis on in vitro fertilization treatment outcomes: a meta-analysis. Fertil. Steril. 108, 483–490.e3 (2017).
Vercellini, P. et al. Adenomyosis and reproductive performance after surgery for rectovaginal and colorectal endometriosis: a systematic review and meta-analysis. Reprod. Biomed. Online 28, 704–713 (2014).
Sallam, H. N., Garcia-Velasco, J. A., Dias, S. & Arici, A. Long-term pituitary down-regulation before in vitro fertilization (IVF) for women with endometriosis. Cochrane Database Syst. Rev. 1, CD004635 (2006).
de Ziegler, D. et al. Use of oral contraceptives in women with endometriosis before assisted reproduction treatment improves outcomes. Fertil. Steril. 94, 2796–2799 (2010).
Drakopoulos, P. et al. Does the type of GnRH analogue used, affect live birth rates in women with endometriosis undergoing IVF/ICSI treatment, according to the rAFS stage? Gynecol. Endocrinol. 34, 884–889 (2018).
Pabuccu, R., Onalan, G. & Kaya, C. GnRH agonist and antagonist protocols for stage I-II endometriosis and endometrioma in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil. Steril. 88, 832–839 (2007).
Rodriguez-Purata, J. et al. Endometriosis and IVF: are agonists really better? Analysis of 1180 cycles with the propensity score matching. Gynecol. Endocrinol. 29, 859–862 (2013).
Bourdon, M. et al. Does GnRH agonist triggering control painful symptom scores during assisted reproductive technology? a retrospective study. Reprod. Sci. 24, 1325–1333 (2017).
Bourdon, M. et al. The deferred embryo transfer strategy improves cumulative pregnancy rates in endometriosis-related infertility: a retrospective matched cohort study. PLOS ONE 13, e0194800 (2018).
Benaglia, L. et al. IVF and endometriosis-related symptom progression: insights from a prospective study. Hum. Reprod. 26, 2368–2372 (2011).
Santulli, P. et al. Endometriosis-related infertility: assisted reproductive technology has no adverse impact on pain or quality-of-life scores. Fertil. Steril. 105, 978–987.e4 (2016).
van der Houwen, L. E. et al. Efficacy and safety of IVF/ICSI in patients with severe endometriosis after long-term pituitary down-regulation. Reprod. Biomed. Online 28, 39–46 (2014).
Villette, C. et al. Risks of tubo-ovarian abscess in cases of endometrioma and assisted reproductive technologies are both under- and overreported. Fertil. Steril. 106, 410–415 (2016).
Pandey, S., Shetty, A., Hamilton, M., Bhattacharya, S. & Maheshwari, A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum. Reprod. Update 18, 485–503 (2012).
Palomba, S., Homburg, R., Santagni, S., La Sala, G. B. & Orvieto, R. Risk of adverse pregnancy and perinatal outcomes after high technology infertility treatment: a comprehensive systematic review. Reprod. Biol. Endocrinol. 14, 76 (2016).
Qin, J., Liu, X., Sheng, X., Wang, H. & Gao, S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil. Steril. 105, 73–85.e1-6 (2016).
Qin, J. et al. Pregnancy-related complications and adverse pregnancy outcomes in multiple pregnancies resulting from assisted reproductive technology: a meta-analysis of cohort studies. Fertil. Steril. 103, 1492–1508.e1-7 (2015).
Martinez, F., International Society for Fertility Preservation–ESHRE–ASRM Expert Working Group. Update on fertility preservation from the Barcelona International Society for Fertility Preservation-ESHRE-ASRM 2015 expert meeting: indications, results and future perspectives. Fertil. Steril. 108, 407–415.e11 (2017).
Elizur, S. E. et al. Cryopreservation of oocytes in a young woman with severe and symptomatic endometriosis: a new indication for fertility preservation. Fertil. Steril. 91 293.e1-3 (2009).
Oktay, K. & Oktem, O. Ovarian cryopreservation and transplantation for fertility preservation for medical indications: report of an ongoing experience. Fertil. Steril. 93, 762–768 (2010).
Garcia-Velasco, J. A. et al. Five years' experience using oocyte vitrification to preserve fertility for medical and nonmedical indications. Fertil. Steril. 99, 1994–1999 (2013).
Cobo, A., Garcia-Velasco, J., Domingo, J., Pellicer, A. & Remohi, J. Elective and onco-fertility preservation: factors related to IVF outcomes. Hum. Reprod. 33, 2222–2231 (2018).
Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis: a committee opinion. Fertil. Steril. 101, 927–935 (2014).
Leyland, N., Casper, R., Laberge, P., Singh, S. S. & SOGC. Endometriosis: diagnosis and management. J. Obstet. Gynaecol. Can. 32, S1–S32 (2010).
American College of Obstetricians and Gynecologists. ACOG: Practice bulletin no. 114: Management of endometriosis. Obstet. Gynecol. 116, 223–236 (2010).
Johnson, N. P. & Hummelshoj, L. World Endometriosis Society Montpellier, C. Consensus on current management of endometriosis. Hum. Reprod. 28, 1552–1568 (2013).
Dunselman, G. A. et al. ESHRE guideline: management of women with endometriosis. Hum. Reprod. 29, 400–412 (2014).
National Institute for Health and Care Excellence (NICE). Diagnosis and management of endometriosis: summary of NICE guidance. BMJ 358, 4227 (2017).
Hudelist, G. et al. Combination of transvaginal sonography and clinical examination for preoperative diagnosis of pelvic endometriosis. Hum. Reprod. 24, 1018–1024 (2009).
Nnoaham, K. E. et al. Developing symptom-based predictive models of endometriosis as a clinical screening tool: results from a multicenter study. Fertil. Steril. 98, 692–701.e5 (2012).
Lafay Pillet, M. C. et al. A clinical score can predict associated deep infiltrating endometriosis before surgery for an endometrioma. Hum. Reprod. 29, 1666–1676 (2014).
Soliman, A. M., Fuldeore, M. & Snabes, M. C. Factors associated with time to endometriosis diagnosis in the United States. J. Womens Health 26, 788–797 (2017).
Abrao, M. S. et al. Deep endometriosis infiltrating the recto-sigmoid: critical factors to consider before management. Hum. Reprod. Update 21, 329–339 (2015).
Murta, M. et al. Endometriosis does not affect live birth rates of patients submitted to assisted reproduction techniques: analysis of the latin american network registry database from 1995 to 2011. J. Assist. Reprod. Genet. 35, 1395–1399 (2018).
Garcia-Velasco, J. A. & Arici, A. Surgery for the removal of endometriomas before in vitro fertilization does not increase implantation and pregnancy rates. Fertil. Steril. 81, 1206 (2004).
Ballester, M. et al. Cumulative pregnancy rate after ICSI-IVF in patients with colorectal endometriosis: results of a multicentre study. Hum. Reprod. 27, 1043–1049 (2012).
AlKudmani, B. et al. In vitro fertilization success rates after surgically treated endometriosis and effect of time interval between surgery and in vitro fertilization. J. Minim. Invasive Gynecol. 25, 99–104 (2018).
Huang, X. W., Qiao, J., Xia, E. L., Ma, Y. M. & Wang, Y. Effect of interval after surgery on in vitro fertilization/ intracytoplasmic sperm injection outcomes in patients with stage III/IV endometriosis. Chin. Med. J. 123, 2176–2180 (2010).
Somigliana, E. et al. Effect of delaying post-operative conception after conservative surgery for endometriosis. Reprod. Biomed. Online 20, 410–415 (2010).
Vercellini, P. et al. The effect of second-line surgery on reproductive performance of women with recurrent endometriosis: a systematic review. Acta Obstet. Gynecol. Scand. 88, 1074–1082 (2009).
Mathews, T. J. & Hamilton, B. E. Mean age of mothers is on the rise: United States, 2000-2014. NCHS Data Briefs 232, 1-8 (2016).
Burney, R. O. et al. Gene expression analysis of endometrium reveals progesterone resistance and candidate susceptibility genes in women with endometriosis. Endocrinology 148, 3814–3826 (2007).
Kao, L. C. et al. Expression profiling of endometrium from women with endometriosis reveals candidate genes for disease-based implantation failure and infertility. Endocrinology 144, 2870–2881 (2003).
Vercellini, P., Giudice, L. C., Evers, J. L. & Abrao, M. S. Reducing low-value care in endometriosis between limited evidence and unresolved issues: a proposal. Hum. Reprod. 30, 1996–2004 (2015).
Gordts, S., Brosens, J. J., Fusi, L., Benagiano, G. & Brosens, I. Uterine adenomyosis: a need for uniform terminology and consensus classification. Reprod. Biomed. Online 17, 244–248 (2008).
Levgur, M., Abadi, M. A. & Tucker, A. Adenomyosis: symptoms, histology, and pregnancy terminations. Obstet. Gynecol. 95, 688–691 (2000).
Van den Bosch, T. et al. Terms, definitions and measurements to describe sonographic features of myometrium and uterine masses: a consensus opinion from the Morphological Uterus Sonographic Assessment (MUSA) group. Ultrasound Obstet. Gynecol. 46, 284–298 (2015).
Chapron, C. et al. Relationship between the magnetic resonance imaging appearance of adenomyosis and endometriosis phenotypes. Hum. Reprod. 32, 1393–1401 (2017).
Bazot, M. & Darai, E. Role of transvaginal sonography and magnetic resonance imaging in the diagnosis of uterine adenomyosis. Fertil. Steril. 109, 389–397 (2018).
Vannuccini, S. et al. Pathogenesis of adenomyosis: an update on molecular mechanisms. Reprod. Biomed. Online 35, 592–601 (2017).
Benagiano, G., Brosens, I. & Habiba, M. Structural and molecular features of the endomyometrium in endometriosis and adenomyosis. Hum. Reprod. Update 20, 386–402 (2014).
Nelsen, L. M. et al. Experience of symptoms and disease impact in patients with adenomyosis. Patient 11, 319–328 (2018).
Pearce, C. L. et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 13, 385–394 (2012).
Guo, S. W. Endometriosis and ovarian cancer: potential benefits and harms of screening and risk-reducing surgery. Fertil. Steril. 104, 813–830 (2015).
Kim, H. S., Kim, T. H., Chung, H. H. & Song, Y. S. Risk and prognosis of ovarian cancer in women with endometriosis: a meta-analysis. Br. J. Cancer 110, 1878–1890 (2014).
Wentzensen, N. et al. Ovarian cancer risk factors by histologic subtype: an analysis from the ovarian cancer cohort consortium. J. Clin. Oncol. 34, 2888–2898 (2016).
Vercellini, P. et al. The 'incessant menstruation' hypothesis: a mechanistic ovarian cancer model with implications for prevention. Hum. Reprod. 26, 2262–2273 (2011).
Somigliana, E. et al. Risks of conservative management in women with ovarian endometriomas undergoing IVF. Hum. Reprod. Update 21, 486–499 (2015).
Borghese, B. et al. Low birth weight is strongly associated with the risk of deep infiltrating endometriosis: results of a 743 case-control study. PLOS ONE 10, e0117387 (2015).
Vitonis, A. F., Baer, H. J., Hankinson, S. E., Laufer, M. R. & Missmer, S. A. A prospective study of body size during childhood and early adulthood and the incidence of endometriosis. Hum. Reprod. 25, 1325–1334 (2010).
Liebermann, C. et al. Maltreatment during childhood: a risk factor for the development of endometriosis? Hum. Reprod. 33, 1449–1458 (2018).
DiVasta, A. D., Vitonis, A. F., Laufer, M. R. & Missmer, S. A. Spectrum of symptoms in women diagnosed with endometriosis during adolescence vs adulthood. Am. J. Obstet. Gynecol. 218, 324.e1–324.e11 (2018).
Chapron, C. et al. Questioning patients about their adolescent history can identify markers associated with deep infiltrating endometriosis. Fertil. Steril. 95, 877–881 (2011).
Miller, J. A. et al. Prevalence of migraines in adolescents with endometriosis. Fertil. Steril. 109, 685–690 (2018).
Vigano, P. et al. Principles of phenomics in endometriosis. Hum. Reprod. Update 18, 248–259 (2012).
Kvaskoff, M. et al. Endometriosis: a high-risk population for major chronic diseases? Hum. Reprod. Update 21, 500–516 (2015).
Santulli, P. et al. Increased rate of spontaneous miscarriages in endometriosis-affected women. Hum. Reprod. 31, 1014–1023 (2016).
Acknowledgements
The authors thank staff members for their contribution to the multidisciplinary management and clinical research of endometriotic patients: (i) Gynecological Surgery: H. Foulot, A. Bourret, P. Marzouk, G. Pierre, M. C. Lafay-Pillet, F. Decuypere, L. Campin and M. C. Lamau; (ii) Gynecological Endocrinology: G. Plu-Bureau, L. Maitrot-Mantelet and J. Hugon-Rodin; (iii) Assisted Reproductive Technology: M. Bourdon, C. Maignien, S. Eskenazi and F. Kefelian; (iv) Reproductive Biology: J. P. Wolf, C. Patrat, K. Pocate-Cheriet and C. Chalas; (v) Obstetrics: F. Goffinet; (vi) Intestinal Surgery: B. Dousset, S. Gaujoux, and M. Leconte; (vii) Urological Surgery: M. Peyromaure and N. Barry Delongchamps; (viii) Thoracic Surgery: M. Alifano; (ix) Radiology: A. E. Millischer, C. Bordonne and F. Bourret-Cassaigne; (x) Pathology: B. Terris, M. C. Vacher-Lavenu and P. A. Just; (xi) Pelvic Pain Center : S. Perrot; (xii) Psychologist: V. Antoine; (xiii) Epidemiology: P. Y. Ancel; (xiv) Biochemistry: D. Borderie and (xv) Paramedical Staff : K. Hillion, M. Meno, S. Odic and V. Blanchet. The authors also wish to thank F. Batteux, S. Chouzenoux and their team and D. Vaiman and his team (Development, Reproduction and Cancer, Institut Cochin, INSERM U1016, Université Paris Descartes, Sorbonne Paris Cité, Paris, France) for their collaboration in the scientific research.
Author information
Authors and Affiliations
Contributions
C.C. supervised the project. All of the authors researched data for the article, substantially contributed to discussions of the content and wrote the article. C.C. and P.S. carried out the review and editing of the mauscript.
Corresponding author
Ethics declarations
Competing interests
Until recently, C.C was the president of the Society of Endometriosis Disorders (SEUD) and of the Society of Gynecological and Pelvic Surgery (SCGP). Over the past 3 years, C.C. has been a consultant for AbbVie, Bayer, Gedeon Richter and Ipsen. P.S. has been a consultant for Gedeon Richter and Ipsen. L.M. has been a consultant for Ipsen. B.B. has no potential conflicts of interest to disclose.
Additional information
Peer review information
Nature Reviews Endocrinology thanks S. Ferrero, K. Koga and P. Rogers for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Ureterohydronephrosis
-
The dilatation of the renal pelvis and/or calyces and ureter as a result of obstruction.
- Adhesions
-
Fibrous bands of scar-like tissue that form between tissues and organs, connecting structures that are not normally connected.
- Menorrhagia
-
Menstrual periods with abnormally heavy or prolonged bleeding.
- Metrorrhagia
-
Uterine bleeding at irregular intervals, particularly between the expected menstrual periods.
- Müllerian metaplasia
-
Tissues derived from the celomic epithelium, such as the peritoneum, have the potential to differentiate into epithelium and stroma.
- Central sensitization
-
The amplification of pain by the central nervous system.
- Myofascial pain
-
Pain that originates from myofascial trigger points in skeletal muscle, sometimes in seemingly unrelated parts of the body.
- Vulvodynia
-
Chronic pain that affects the vulvar area and sometimes has no identifiable cause.
- Dysmenorrhea
-
Pain during menstruation.
- Myometrial hypertonia
-
Intense and persistent uterine myometrial contraction.
- Adnexal masses
-
Lumps in tissues of the adnexa of the uterus (such as the ovaries and fallopian tubes).
- Retroverted uterus
-
The position of the uterus, tipped backwards so that its fundus is aimed towards the rectum.
- Operative laparoscopy
-
Minimally invasive surgery for therapeutic interventions with a few small cuts in the abdomen.
- Fertility preservation
-
The procedure used to help retain the ability to procreate, including gamete and/or gonad cryopreservation.
Rights and permissions
About this article
Cite this article
Chapron, C., Marcellin, L., Borghese, B. et al. Rethinking mechanisms, diagnosis and management of endometriosis. Nat Rev Endocrinol 15, 666–682 (2019). https://doi.org/10.1038/s41574-019-0245-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-019-0245-z
This article is cited by
-
Endometriosis MR mimickers: T1-hyperintense lesions
Insights into Imaging (2024)
-
Endometriosis MR mimickers: T2-hypointense lesions
Insights into Imaging (2024)
-
An integrated multi-tissue approach for endometriosis candidate biomarkers: a systematic review
Reproductive Biology and Endocrinology (2024)
-
Genetically identification of endometriosis and cancers risk in women through a two-sample Mendelian randomization study
Scientific Reports (2024)
-
Relugolix/Estradiol/Norethisterone Acetate: A Review in Endometriosis-Associated Pain
Drugs (2024)