Abstract
Solid organ transplantation (SOT) is a life-saving procedure and an established treatment for patients with end-stage organ failure. However, transplantation is also accompanied by associated cardiovascular risk factors, of which post-transplant diabetes mellitus (PTDM) is one of the most important. PTDM develops in 10–20% of patients with kidney transplants and in 20–40% of patients who have undergone other SOT. PTDM increases mortality, which is best documented in patients who have received kidney and heart transplants. PTDM results from predisposing factors (similar to type 2 diabetes mellitus) but also as a result of specific post-transplant risk factors. Although PTDM has many characteristics in common with type 2 diabetes mellitus, the prevention and treatment of the two disorders are often different. Over the past 20 years, the lifespan of patients who have undergone SOT has increased, and PTDM becomes more common over the lifespan of these patients. Accordingly, PTDM becomes an important condition not only to be aware of but also to treat. This Review presents the current knowledge on PTDM in patients receiving kidney, heart, liver and lung transplants. This information is not only for transplant health providers but also for endocrinologists and others who will meet these patients in their clinics.
Key points
Post-transplant diabetes mellitus (PTDM) is mostly studied in recipients of kidney transplants, but risk factors for development of PTDM seem to be similar in recipients of heart, liver and lung transplants.
PTDM develops in 10–40% of patients during the first year after a solid organ transplant and is a major risk factor for cardiovascular disease and death.
Major risk factors for development of PTDM are metabolic adverse effects of immunosuppressive drugs, post-transplant viral infections and hypomagnesaemia, in addition to the traditional risk factors seen in patients with type 2 diabetes mellitus.
Prevention of PTDM can be achieved by tailoring the immunosuppressant regimen and probably also by lifestyle intervention; however, this intervention is not well studied.
Patients with PTDM should be treated with hypoglycaemic agents that have been tested for efficacy and safety regarding drug–drug interactions, immunosuppressant drugs and organ function.
Large-scale long-term studies on new glucose-lowering drug classes that have shown cardiovascular protection in high-risk patients with type 2 diabetes mellitus (for example, glucagon-like protein 1 (GLP1) receptor agonists and sodium/glucose cotransporter 2 (SGLT2) inhibitors) are also warranted in patients with PTDM.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Hart, A. et al. OPTN/SRTR 2016 annual data report: kidney. Am. J. Transplant. 18 (Suppl. 1), 18–113 (2018).
Kim, W. Ret al. OPTN/SRTR 2016 annual data report: liver. Am. J. Transplant. 18 (Suppl. 1), 172–253 (2018).
Valapour, M. et al. OPTN/SRTR 2016 annual data report: lung. Am. J. Transplant. 18 (Suppl. 1), 363–433 (2018).
Colvin, M. et al. OPTN/SRTR 2016 annual data report: heart. Am. J. Transplant. 18 (Suppl. 1), 291–362 (2018).
Jenssen, T. & Hartmann, A. Emerging treatments for post-transplantation diabetes mellitus. Nat. Rev. Nephrol. 11, 465–477 (2015).
Bergrem, H. A. et al. Undiagnosed diabetes in kidney transplant candidates: a case-finding strategy. Clin. J. Am. Soc. Nephrol. 5, 616–622 (2010).
Sharif, A. et al. Proceedings from an international consensus meeting on posttransplantation diabetes mellitus: recommendations and future directions. Am. J. Transplant. 14, 1992–2000 (2014).
Eide, I. A. et al. Mortality risk in post-transplantation diabetes mellitus based on glucose and HbA1c diagnostic criteria. Transpl. Int. 29, 568–578 (2016).
Seoane-Pillado, M. T. et al. Incidence of cardiovascular events and associated risk factors in kidney transplant patients: a competing risks survival analysis. BMC Cardiovasc. Disord. 17, 72 (2017).
Cho, M. S. et al. The clinical course and outcomes of post-transplantation diabetes mellitus after heart transplantation. J. Kor. Med. Sci. 27, 1460–1467 (2012).
Martinez-Dolz, L. et al. Predictive factors for development of diabetes mellitus post-heart transplant. Transplant. Proc. 37, 4064–4066 (2005).
Kim, H. J. et al. New-onset diabetes mellitus after heart transplantation- incidence, risk factors and impact on clinical outcome. Circ. J. 81, 806–814 (2017).
Hackman, K. L., Snell, G. I. & Bach, L. A. Poor glycemic control is associated with decreased survival in lung transplant recipients. Transplantation 101, 2200–2206 (2017).
D’Avola, D. et al. Cardiovascular morbidity and mortality after liver transplantation: the protective role of mycophenolate mofetil. Liver Transpl. 23, 498–509 (2017).
Roccaro, G. A. et al. Sustained posttransplantation diabetes is associated with long-term major cardiovascular events following liver transplantation. Am. J. Transplant. 18, 207–215 (2018).
Davidson, J. et al. New-onset diabetes after transplantation: 2003 international consensus guidelines. Proceedings of an international expert panel meeting. Transplantation 75 (Suppl. 10) SS3–SS24 (2003).
Wilkinson, A. et al. Guidelines for the treatment and management of new-onset diabetes after transplantation. Clin. Transplant. 19, 291–298 (2005).
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 34, S62–S69 (2011).
Eide, I. A. et al. Limitations of hemoglobin A1c for the diagnosis of posttransplant diabetes mellitus. Transplantation 99, 629–635 (2015).
Hare, M. J., Shaw, J. E. & Zimmet, P. Z. Current controversies in the use of haemoglobin A1c. J. Intern. Med. 271, 227–236 (2012).
Pimentel, A. L., Cavagnolli, G. & Camargo, J. L. Diagnostic accuracy of glycated hemoglobin for post-transplantation diabetes mellitus after kidney transplantation: systematic review and meta-analysis. Nephrol. Dial. Transplant. 32, 565–572 (2017).
Valderhaug, T. G. et al. The association of early post-transplant glucose levels with long-term mortality. Diabetologia 54, 1341–1349 (2011).
Pimentel, A. L. & Camargo, J. L. Variability of glycated hemoglobin levels in the first year post renal transplantation in patients without diabetes. Clin. Biochem. 50, 997–1001 (2017).
Porrini, E. et al. The combined effect of pre-transplant triglyceride levels and the type of calcineurin inhibitor in predicting the risk of new onset diabetes after renal transplantation. Nephrol. Dial. Transplant. 23, 1436–1441 (2008).
Valderhaug, T. G. et al. Fasting plasma glucose and glycosylated hemoglobin in the screening for diabetes mellitus after renal transplantation. Transplantation 88, 429–434 (2009).
Hecking, M. et al. Glucose metabolism after renal transplantation. Diabetes Care 36, 2763–2771 (2013).
Heldal, T. F. et al. Inflammatory and related biomarkers are associated with post-transplant diabetes mellitus in kidney recipients. Transpl. Int. 31, 510–519 (2018).
DeFronzo, R. A., Ferrannini, E. & Simonson, D. C. Fasting hyperglycemia in non-insulin-dependent diabetes mellitus: contributions of excessive hepatic glucose production and impaired tissue glucose uptake. Metabolism 38, 387–395 (1989).
Ekstrand, A. V., Eriksson, J. G., Gronhagen-Riska, C., Ahonen, P. J. & Groop, L. C. Insulin resistance and insulin deficiency in the pathogenesis of posttransplantation diabetes in man. Transplantation 53, 563–569 (1992).
Jorgensen, M. B. et al. The impact of kidney transplantation on insulin sensitivity. Transpl. Int. 30, 295–304 (2017).
Ferrannini, E. et al. Natural history and physiological determinants of changes in glucose tolerance in a non-diabetic population: the RISC Study. Diabetologia 54, 1507–1516 (2011).
Holst, J. J., Knop, F. K., Vilsboll, T., Krarup, T. & Madsbad, S. Loss of incretin effect is a specific, important, and early characteristic of type 2 diabetes. Diabetes Care 34 (Suppl. 2), S251–S257 (2011).
Halden, T. A. et al. GLP-1 restores altered insulin and glucagon secretion in posttransplantation diabetes. Diabetes Care 39, 617–624 (2016).
Gerich, J. E. Role of the kidney in normal glucose homeostasis and in the hyperglycaemia of diabetes mellitus: therapeutic implications. Diabet. Med. 27, 136–142 (2010).
Kleinridders, A., Ferris, H. A., Cai, W. & Kahn, C. R. Insulin action in brain regulates systemic metabolism and brain function. Diabetes 63, 2232–2243 (2014).
Ferrannini, E. et al. Insulin resistance and hypersecretion in obesity. European Group for the Study of Insulin Resistance (EGIR). J. Clin. Invest. 100, 1166–1173 (1997).
Kloting, N. et al. Insulin-sensitive obesity. Am. J. Physiol. Endocrinol. Metab. 299, E506–E515 (2010).
Cron, D. C. et al. Using analytic morphomics to describe body composition associated with post-kidney transplantation diabetes mellitus. Clin. Transplant. 31, e13040 (2017).
von Düring, M. E. et al. Visceral fat is better related to impaired glucose metabolism than body mass index after kidney transplantation. Transpl. Int. 28, 1162–1171 (2015).
Despres, J. P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 444, 881–887 (2006).
Hjelmesaeth, J. et al. Hypoadiponectinemia is associated with insulin resistance and glucose intolerance after renal transplantation: impact of immunosuppressive and antihypertensive drug therapy. Clin. J. Am. Soc. Nephrol. 1, 575–582 (2006).
Adachi, H. et al. Adiponectin fractions influence the development of posttransplant diabetes mellitus and cardiovascular disease in Japanese renal transplant recipients. PLOS ONE 11, e0163899 (2016).
Plotz, T. et al. The monounsaturated fatty acid oleate is the major physiological toxic free fatty acid for human beta cells. Nutr. Diabetes 7, 305 (2017).
Sharif, A., Moore, R. & Baboolal, K. Influence of lifestyle modification in renal transplant recipients with postprandial hyperglycemia. Transplantation 85, 353–358 (2008).
Cosio, F. G., Pesavento, T. E., Osei, K., Henry, M. L. & Ferguson, R. M. Post-transplant diabetes mellitus: increasing incidence in renal allograft recipients transplanted in recent years. Kidney Int. 59, 732–737 (2001).
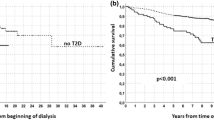
Porrini, E. L. et al. Clinical evolution of post-transplant diabetes mellitus. Nephrol. Dial. Transplant. 31, 495–505 (2016).
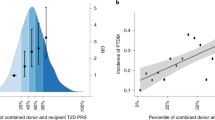
Szabo, M., Mate, B., Csep, K. & Benedek, T. Genetic approaches to the study of gene variants and their impact on the pathophysiology of type 2 diabetes. Biochem. Genet. 56, 22–55 (2018).
McCaughan, J. A., McKnight, A. J. & Maxwell, A. P. Genetics of new-onset diabetes after transplantation. J. Am. Soc. Nephrol. 25, 1037–1049 (2014).
Yalin, G. Y. et al. Evaluation of glutathione peroxidase and KCNJ11 gene polymorphisms in patients with new onset diabetes mellitus after renal transplantation. Exp. Clin. Endocrinol. Diabetes 125, 408–413 (2017).
Romanowski, M. et al. Adiponectin and leptin gene polymorphisms in patients with post-transplant diabetes mellitus. Pharmacogenomics 16, 1243–1251 (2015).
Gervasini, G., Luna, E., Garcia-Cerrada, M., Garcia-Pino, G. & Cubero, J. J. Risk factors for post-transplant diabetes mellitus in renal transplant: role of genetic variability in the CYP450-mediated arachidonic acid metabolism. Mol. Cell. Endocrinol. 419, 158–164 (2016).
Romanowski, M. et al. Interleukin-17 gene polymorphisms in patients with post-transplant diabetes mellitus. Eur. Rev. Med. Pharmacol. Sci. 19, 3152–3156 (2015).
Kim, Y. G. et al. Association of genetic polymorphisms of interleukins with new-onset diabetes after transplantation in renal transplantation. Transplantation 93, 900–907 (2012).
Kim, J. S. et al. Significant association between Toll-like receptor gene polymorphisms and posttransplantation diabetes mellitus. Nephron 133, 279–286 (2016).
Hjelmesaeth, J. et al. Glucose intolerance after renal transplantation depends upon prednisolone dose and recipient age. Transplantation 64, 979–983 (1997).
Cheungpasitporn, W., Thongprayoon, C., Vijayvargiya, P., Anthanont, P. & Erickson, S. B. The risk for new-onset diabetes mellitus after kidney transplantation in patients with autosomal dominant polycystic kidney disease: a systematic review and meta-analysis. Can. J. Diabetes 40, 521–528 (2016).
Okumi, M. et al. Diabetes mellitus after kidney transplantation in Japanese patients: the Japan Academic Consortium of Kidney Transplantation study. Int. J. Urol. 24, 197–204 (2017).
Peracha, J. et al. Risk of post-transplantation diabetes mellitus is greater in South Asian versus Caucasian kidney allograft recipients. Transpl. Int. 29, 727–739 (2016).
Sepehri, Z. et al. Inflammasomes and type 2 diabetes: an updated systematic review. Immunol. Lett. 192, 97–103 (2017).
Cantarin, M. P. et al. Association of inflammation prior to kidney transplantation with post-transplant diabetes mellitus. Cardiorenal Med. 6, 289–300 (2016).
Rodriguez-Moran, M. & Guerrero-Romero, F. Oral magnesium supplementation improves insulin sensitivity and metabolic control in type 2 diabetic subjects: a randomized double-blind controlled trial. Diabetes Care 26, 1147–1152 (2003).
Song, Y., He, K., Levitan, E. B., Manson, J. E. & Liu, S. Effects of oral magnesium supplementation on glycaemic control in Type 2 diabetes: a meta-analysis of randomized double-blind controlled trials. Diabet. Med. 23, 1050–1056 (2006).
Barton, C. H., Vaziri, N. D., Martin, D. C., Choi, S. & Alikhani, S. Hypomagnesemia and renal magnesium wasting in renal transplant recipients receiving cyclosporine. Am. J. Med. 83, 693–699 (1987).
Garg, N. et al. Lower magnesium level associated with new-onset diabetes and pre-diabetes after kidney transplantation. J. Nephrol. 27, 339–344 (2014).
Huang, J. W., Famure, O., Li, Y. & Kim, S. J. Hypomagnesemia and the risk of new-onset diabetes mellitus after kidney transplantation. J. Am. Soc. Nephrol. 27, 1793–1800 (2016).
Van Laecke, S. et al. Effect of magnesium supplements on insulin secretion after kidney transplantation: a randomized controlled trial. Ann. Transplant. 22, 524–531 (2017).
Van Laecke, S. et al. The effect of magnesium supplements on early post-transplantation glucose metabolism: a randomized controlled trial. Transpl. Int. 27, 895–902 (2014).
Baid, S. et al. Posttransplant diabetes mellitus in liver transplant recipients: risk factors, temporal relationship with hepatitis C virus allograft hepatitis, and impact on mortality. Transplantation 72, 1066–1072 (2001).
Chen, T. et al. New onset diabetes mellitus after liver transplantation and hepatitis C virus infection: meta-analysis of clinical studies. Transpl. Int. 22, 408–415 (2009).
Delaunay, F. et al. Pancreatic beta cells are important targets for the diabetogenic effects of glucocorticoids. J. Clin. Invest. 100, 2094–2098 (1997).
Andrews, R. C. & Walker, B. R. Glucocorticoids and insulin resistance: old hormones, new targets. Clin. Sci. 96, 513–523 (1999).
Schacke, H., Docke, W. D. & Asadullah, K. Mechanisms involved in the side effects of glucocorticoids. Pharmacol. Ther. 96, 23–43 (2002).
Boots, J. M., van Duijnhoven, E. M., Christiaans, M. H., Wolffenbuttel, B. H. & van Hooff, J. P. Glucose metabolism in renal transplant recipients on tacrolimus: the effect of steroid withdrawal and tacrolimus trough level reduction. J. Am. Soc. Nephrol. 13, 221–227 (2002).
Midtvedt, K. et al. Insulin resistance after renal transplantation: the effect of steroid dose reduction and withdrawal. J. Am. Soc. Nephrol. 15, 3233–3239 (2004).
Cohen, D. J. et al. Cyclosporine: a new immunosuppressive agent for organ transplantation. Ann. Intern. Med. 101, 667–682 (1984).
Ozbay, L. A. et al. Cyclosporin and tacrolimus impair insulin secretion and transcriptional regulation in INS-1E beta-cells. Br. J. Pharmacol. 162, 136–146 (2011).
Ekberg, H. et al. Reduced exposure to calcineurin inhibitors in renal transplantation. N. Engl. J. Med. 357, 2562–2575 (2007).
Vincenti, F. et al. Results of an international, randomized trial comparing glucose metabolism disorders and outcome with cyclosporine versus tacrolimus. Am. J. Transplant. 7, 1506–1514 (2007).
Webster, A. C., Woodroffe, R. C., Taylor, R. S., Chapman, J. R. & Craig, J. C. Tacrolimus versus ciclosporin as primary immunosuppression for kidney transplant recipients: meta-analysis and meta-regression of randomised trial data. BMJ 331, 810 (2005).
Chakkera, H. A. & Mandarino, L. J. Calcineurin inhibition and new-onset diabetes mellitus after transplantation. Transplantation 95, 647–652 (2013).
Heit, J. J. et al. Calcineurin/NFAT signalling regulates pancreatic beta-cell growth and function. Nature 443, 345–349 (2006).
Hernandez-Fisac, I. et al. Tacrolimus-induced diabetes in rats courses with suppressed insulin gene expression in pancreatic islets. Am. J. Transplant. 7, 2455–2462 (2007).
Trinanes, J. et al. Deciphering tacrolimus-induced toxicity in pancreatic beta cells. Am. J. Transplant. 17, 2829–2840 (2017).
Johnston, O., Rose, C. L., Webster, A. C. & Gill, J. S. Sirolimus is associated with new-onset diabetes in kidney transplant recipients. J. Am. Soc. Nephrol. 19, 1411–1418 (2008).
Teutonico, A., Schena, P. F. & Di Paolo, S. Glucose metabolism in renal transplant recipients: effect of calcineurin inhibitor withdrawal and conversion to sirolimus. J. Am. Soc. Nephrol. 16, 3128–3135 (2005).
Bell, E. et al. Rapamycin has a deleterious effect on MIN-6 cells and rat and human islets. Diabetes 52, 2731–2739 (2003).
Zahr, E. et al. Rapamycin impairs in vivo proliferation of islet beta-cells. Transplantation 84, 1576–1583 (2007).
Shivaswamy, V. et al. Tacrolimus and sirolimus have distinct effects on insulin signaling in male and female rats. Transl Res. 163, 221–231 (2014).
Fraenkel, M. et al. mTOR inhibition by rapamycin prevents beta-cell adaptation to hyperglycemia and exacerbates the metabolic state in type 2 diabetes. Diabetes 57, 945–957 (2008).
Taniguchi, C. M., Emanuelli, B. & Kahn, C. R. Critical nodes in signalling pathways: insights into insulin action. Nat. Rev. Mol. Cell Biol. 7, 85–96 (2006).
Vanrenterghem, Y. et al. Belatacept-based regimens are associated with improved cardiovascular and metabolic risk factors compared with cyclosporine in kidney transplant recipients (BENEFIT and BENEFIT-EXT studies). Transplantation 91, 976–983 (2011).
Delgado-Borrego, A. et al. Hepatitis C virus is independently associated with increased insulin resistance after liver transplantation. Transplantation 77, 703–710 (2004).
Fabrizi, F. et al. Post-transplant diabetes mellitus and HCV seropositive status after renal transplantation: meta-analysis of clinical studies. Am. J. Transplant. 5, 2433–2440 (2005).
Hjelmesaeth, J. et al. Asymptomatic cytomegalovirus infection is associated with increased risk of new-onset diabetes mellitus and impaired insulin release after renal transplantation. Diabetologia 47, 1550–1556 (2004).
Einollahi, B., Motalebi, M., Salesi, M., Ebrahimi, M. & Taghipour, M. The impact of cytomegalovirus infection on new-onset diabetes mellitus after kidney transplantation: a review on current findings. J. Nephropathol. 3, 139–148 (2014).
Valderhaug, T. G. et al. Reduced incidence of new-onset posttransplantation diabetes mellitus during the last decade. Transplantation 84, 1125–1130 (2007).
Kasiske, B. L., Snyder, J. J., Gilbertson, D. & Matas, A. J. Diabetes mellitus after kidney transplantation in the United States. Am. J. Transplant. 3, 178–185 (2003).
Cosio, F. G. et al. New onset hyperglycemia and diabetes are associated with increased cardiovascular risk after kidney transplantation. Kidney Int. 67, 2415–2421 (2005).
Valderhaug, T. G. et al. Early posttransplantation hyperglycemia in kidney transplant recipients is associated with overall long-term graft losses. Transplantation 94, 714–720 (2012).
Nieuwenhuis, M. G. & Kirkels, J. H. Predictability and other aspects of post-transplant diabetes mellitus in heart transplant recipients. J. Heart Lung Transplant. 20, 703–708 (2001).
Depczynski, B., Daly, B., Campbell, L. V., Chisholm, D. J. & Keogh, A. Predicting the occurrence of diabetes mellitus in recipients of heart transplants. Diabet Med. 17, 15–19 (2000).
Ye, X. et al. Risk factors for development of new-onset diabetes mellitus in adult heart transplant recipients. Transplantation 89, 1526–1532 (2010).
Sehgal, S. et al. New-onset diabetes mellitus after heart transplantation in children - Incidence and risk factors. Pediatr. Transplant. 20, 963–969 (2016).
Foroutan, F. et al. Predictors of 1-year mortality in heart transplant recipients: a systematic review and meta-analysis. Heart 104, 151–160 (2018).
Stehlik, J. et al. The Registry of the International Society for Heart and Lung Transplantation: twenty-seventh official adult heart transplant report—2010. J. Heart Lung Transplant. 29, 1089–1103 (2010).
Linder, K. E. et al. Evaluation of posttransplantation diabetes mellitus after liver transplantation: assessment of insulin administration as a risk factor. Ann. Pharmacother. 50, 369–375 (2016).
Moon, J. I., Barbeito, R., Faradji, R. N., Gaynor, J. J. & Tzakis, A. G. Negative impact of new-onset diabetes mellitus on patient and graft survival after liver transplantation: long-term follow up. Transplantation 82, 1625–1628 (2006).
Xue, M. et al. Effect of interleukin-2 receptor antagonists on new-onset diabetes after liver transplantation: a retrospective cohort study. J. Diabetes 8, 579–587 (2016).
Xue, M. et al. Donor liver steatosis: a risk factor for early new-onset diabetes after liver transplantation. J. Diabetes Investig. 8, 181–187 (2017).
Stepanova, M. et al. Risk of de novo post-transplant type 2 diabetes in patients undergoing liver transplant for non-alcoholic steatohepatitis. BMC Gastroenterol. 15, 175 (2015).
Ling, Q. et al. New-onset diabetes after liver transplantation: a national report from China Liver Transplant Registry. Liver Int. 36, 705–712 (2016).
Honda, M. et al. Incidence and risk factors for new-onset diabetes in living-donor liver transplant recipients. Clin. Transplant. 27, 426–435 (2013).
Liu, F. C., Lin, J. R., Chen, H. P., Tsai, Y. F. & Yu, H. P. Prevalence, predictive factors, and survival outcome of new-onset diabetes after liver transplantation: a population-based cohort study. Medicine (Baltimore) 95, e3829 (2016).
Morbitzer, K. A. et al. The impact of diabetes mellitus and glycemic control on clinical outcomes following liver transplant for hepatitis C. Clin. Transplant. 28, 862–868 (2014).
Lv, C. et al. New-onset diabetes after liver transplantation and its impact on complications and patient survival. J. Diabetes 7, 881–890 (2015).
Hackman, K. L., Snell, G. I. & Bach, L. A. Prevalence and predictors of diabetes after lung transplantation: a prospective, longitudinal study. Diabetes Care 37, 2919–2925 (2014).
Belle-van Meerkerk, G. et al. Diabetes before and after lung transplantation in patients with cystic fibrosis and other lung diseases. Diabet. Med. 29, e159–e162 (2012).
Ollech, J. E. et al. Post-transplant diabetes mellitus in lung transplant recipients: incidence and risk factors. Eur. J. Cardiothorac. Surg. 33, 844–848 (2008).
Savioli, G. et al. Early development of metabolic syndrome in patients subjected to lung transplantation. Clin. Transplant. 27, E237–E243 (2013).
Yusen, R. D. et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-third adult lung and heart-lung transplant report-2016; focus theme: primary diagnostic indications for transplant. J. Heart Lung Transplant. 35, 1170–1184 (2016).
Klomjit, N., Mehrnia, A., Sampaio, M. & Bunnapradist, S. Impact of diabetes mellitus on survival outcome of lung transplant recipients: an analysis of OPTN/UNOS data. Clin. Transpl. 31, 43–55 (2015).
Hackman, K. L., Bailey, M. J., Snell, G. I. & Bach, L. A. Diabetes is a major risk factor for mortality after lung transplantation. Am. J. Transplant. 14, 438–445 (2014).
Bergrem, H. A. et al. Glucose tolerance before and after renal transplantation. Nephrol. Dial. Transplant. 25, 985–992 (2010).
Hornum, M., Lindahl, J. P., von Zur-Mühlen, B., Jenssen, T. & Feldt-Rasmussen, B. Diagnosis, management and treatment of glucometabolic disorders emerging after kidney transplantation: a position statement from the Nordic Transplantation Societies. Transpl. Int. 26, 1049–1060 (2013).
Costanzo, M. R. et al. The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J. Heart Lung Transplant. 29, 914–956 (2010).
Wanner, C. & Tonelli, M. & The Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. KDIGO Clinical Practice Guideline for lipid management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 85, 1303–1309 (2014).
Kahn, S. E., Cooper, M. E. & Del Prato, S. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet 383, 1068–1083 (2014).
Hecking, M. et al. Early basal insulin therapy decreases new-onset diabetes after renal transplantation. J. Am. Soc. Nephrol. 23, 739–749 (2012).
Werzowa, J. et al. Vildagliptin and pioglitazone in patients with impaired glucose tolerance after kidney transplantation: a randomized, placebo-controlled clinical trial. Transplantation 95, 456–462 (2013).
Lane, J. T. et al. Sitagliptin therapy in kidney transplant recipients with new-onset diabetes after transplantation. Transplantation 92, e56–e57 (2011).
Strom Halden, T. A., Asberg, A., Vik, K., Hartmann, A. & Jenssen, T. Short-term efficacy and safety of sitagliptin treatment in long-term stable renal recipients with new-onset diabetes after transplantation. Nephrol. Dial. Transplant. 29, 926–933 (2014).
Alnasrallah, B., Pilmore, H. & Manley, P. Protocol for a pilot randomised controlled trial of metformin in pre-diabetes after kidney transplantation: the transplantation and diabetes (Transdiab) study. BMJ Open 7, e016813 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03157414 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03113110 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02233491 (2017).
Luan, F. L., Steffick, D. E. & Ojo, A. O. New-onset diabetes mellitus in kidney transplant recipients discharged on steroid-free immunosuppression. Transplantation 91, 334–341 (2011).
Rizzari, M. D. et al. Ten-year outcome after rapid discontinuation of prednisone in adult primary kidney transplantation. Clin. J. Am. Soc. Nephrol. 7, 494–503 (2012).
Pirsch, J. D. et al. New-onset diabetes after transplantation: results from a double-blind early corticosteroid withdrawal trial. Am. J. Transplant. 15, 1982–1990 (2015).
Woodle, E. S. et al. A prospective, randomized, double-blind, placebo-controlled multicenter trial comparing early (7 day) corticosteroid cessation versus long-term, low-dose corticosteroid therapy. Ann. Surg. 248, 564–577 (2008).
Yates, C. J., Fourlanos, S., Colman, P. G. & Cohney, S. J. Divided dosing reduces prednisolone-induced hyperglycaemia and glycaemic variability: a randomized trial after kidney transplantation. Nephrol. Dial. Transplant. 29, 698–705 (2014).
Handisurya, A. et al. Conversion from tacrolimus to cyclosporine A improves glucose tolerance in HCV-positive renal transplant recipients. PLOS ONE 11, e0145319 (2016).
Wissing, K. M. et al. Prospective randomized study of conversion from tacrolimus to cyclosporine A to improve glucose metabolism in patients with posttransplant diabetes mellitus after renal transplantation. Am. J. Transplant. 18, 1726–1734 (2018).
Andreassen, A. K. et al. Everolimus initiation with early calcineurin inhibitor withdrawal in de novo heart transplant recipients: three-year results from the randomized SCHEDULE study. Am. J. Transplant. 16, 1238–1247 (2016).
Ar’Rajab, A. & Ahren, B. Prevention of hyperglycemia improves the long-term result of islet transplantation in streptozotocin-diabetic rats. Pancreas 7, 435–442 (1992).
Koh, A. et al. Insulin-heparin infusions peritransplant substantially improve single-donor clinical islet transplant success. Transplantation 89, 465–471 (2010).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01683331 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03507829 (2018).
Gerstein, H. C. et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N. Engl. J. Med. 367, 319–328 (2012).
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352, 837–853 (1998).
Burroughs, T. E. et al. Diabetic complications associated with new-onset diabetes mellitus in renal transplant recipients. Transplantation 83, 1027–1034 (2007).
Zoungas, S. et al. Severe hypoglycemia and risks of vascular events and death. N. Engl. J. Med. 363, 1410–1418 (2010).
Gerstein, H. C. et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 286, 421–426 (2001).
UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352, 854–865 (1998).
Boussageon, R. et al. Are concomitant treatments confounding factors in randomized controlled trials on intensive blood-glucose control in type 2 diabetes? a systematic review. BMC Med. Res. Methodol. 13, 107 (2013).
Hemmingsen, B. et al. Comparison of metformin and insulin versus insulin alone for type 2 diabetes: systematic review of randomised clinical trials with meta-analyses and trial sequential analyses. BMJ 344, e1771 (2012).
Sharif, A. Should metformin be our antiglycemic agent of choice post-transplantation? Am. J. Transplant. 11, 1376–1381 (2011).
Dichtwald, S., Weinbroum, A. A., Sorkine, P., Ekstein, M. P. & Dahan, E. Metformin-associated lactic acidosis following acute kidney injury. Efficacious treatment with continuous renal replacement therapy. Diabet. Med. 29, 245–250 (2012).
Turk, T. et al. Repaglinide in the management of new-onset diabetes mellitus after renal transplantation. Am. J. Transplant. 6, 842–846 (2006).
Voytovich, M. H. et al. Nateglinide improves postprandial hyperglycemia and insulin secretion in renal transplant recipients. Clin. Transplant. 21, 246–251 (2007).
Haidinger, M. et al. Efficacy and safety of vildagliptin in new-onset diabetes after kidney transplantation — a randomized, double-blind, placebo-controlled trial. Am. J. Transplant. 14, 115–123 (2014).
Green, J. B. et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 373, 232–242 (2015).
Luther, P. & Baldwin, D. Jr. Pioglitazone in the management of diabetes mellitus after transplantation. Am. J. Transplant. 4, 2135–2138 (2004).
Lo, C. et al. Glucose-lowering agents for treating pre-existing and new-onset diabetes in kidney transplant recipients. Cochrane Database Syst. Rev. 2, CD009966 (2017).
Conte, C. & Secchi, A. Post-transplantation diabetes in kidney transplant recipients: an update on management and prevention. Acta Diabetol. 55, 763–779 (2018).
Ojo, A. O. et al. Chronic renal failure after transplantation of a nonrenal organ. N. Engl. J. Med. 349, 931–940 (2003).
Gaede, P., Lund-Andersen, H., Parving, H. H. & Pedersen, O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N. Engl. J. Med. 358, 580–591 (2008).
Gaede, P. et al. Years of life gained by multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia 59, 2298–2307 (2016).
Marso, S. P. et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 375, 1834–1844 (2016).
Marso, S. P. et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 375, 311–322 (2016).
Neal, B. et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N. Engl. J. Med. 377, 644–657 (2017).
Zinman, B. et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 373, 2117–2128 (2015).
Wiviott, S. D. et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. https://doi.org/10.1056/NEJMoa1812389 (2018).
Heerspink, H. J. et al. Canagliflozin slows progression of renal function decline independently of glycemic effects. J. Am. Soc. Nephrol. 28, 368–375 (2017).
Wanner, C. et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N. Engl. J. Med. 375, 323–334 (2016).
Dubois-Laforgue, D., Boutboul, D., Levy, D. J., Joly, D. & Timsit, J. Severe acute renal failure in patients treated with glucagon-like peptide-1 receptor agonists. Diabetes Res. Clin. Pract. 103, e53–e55 (2014).
Jabbour, S. et al. Dapagliflozin in patients with type 2 diabetes mellitus: a pooled analysis of safety data from phase IIb/III clinical trials. Diabetes Obes. Metab. 20, 620–628 (2018).
Yale, J. F. et al. Efficacy and safety of canagliflozin in subjects with type 2 diabetes and chronic kidney disease. Diabetes Obes. Metab. 15, 463–473 (2013).
Christians, U., Jacobsen, W., Benet, L. Z. & Lampen, A. Mechanisms of clinically relevant drug interactions associated with tacrolimus. Clin. Pharmacokinet. 41, 813–851 (2002).
Dai, Y. et al. Effect of CYP3A5 polymorphism on tacrolimus metabolic clearance in vitro. Drug Metab. Dispos. 34, 836–847 (2006).
Wallia, A., Illuri, V. & Molitch, M. E. Diabetes care after transplant: definitions, risk factors, and clinical management. Med. Clin. North Am. 100, 535–550 (2016).
Wiggins, B. S. et al. Recommendations for management of clinically significant drug-drug interactions with statins and select agents used in patients with cardiovascular disease: a scientific statement from the american heart association. Circulation 134, e468–e495 (2016).
Chang, S. H. et al. Association between use of non-vitamin K oral anticoagulants with and without concurrent medications and risk of major bleeding in nonvalvular atrial fibrillation. JAMA 318, 1250–1259 (2017).
Wannhoff, A., Weiss, K. H., Schemmer, P., Stremmel, W. & Gotthardt, D. N. Increased levels of rivaroxaban in patients after liver transplantation treated with cyclosporine A. Transplantation 98, e12–e13 (2014).
Poulsen, B. K., Grove, E. L. & Husted, S. E. New oral anticoagulants: a review of the literature with particular emphasis on patients with impaired renal function. Drugs 72, 1739–1753 (2012).
Kothari, J., Nash, M., Zaltzman, J. & Ramesh Prasad, G. V. Diltiazem use in tacrolimus-treated renal transplant recipients. J. Clin. Pharm. Ther. 29, 425–430 (2004).
Zhou, S. F., Xue, C. C., Yu, X. Q., Li, C. & Wang, G. Clinically important drug interactions potentially involving mechanism-based inhibition of cytochrome P450 3A4 and the role of therapeutic drug monitoring. Ther. Drug Monit. 29, 687–710 (2007).
Zimmerman, J. J. Exposure-response relationships and drug interactions of sirolimus. AAPS J. 6, e28 (2004).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01928199 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01680185 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02095418 (2014).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03304626 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02083991 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01560572 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01265537 (2016).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02316938 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02036554 (2014).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01875224 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01431430 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01291030 (2017).
Acknowledgements
Reviewer information
Nature Reviews Endocrinology thanks L. Rostaing, A. Secchi and other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
Both authors contributed to researching the data for the article, discussion of content, writing the article and reviewing and/or editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
T.J. has received lecture honoraria from AstraZeneca, Boehringer Ingelheim, Merck Sharpe and Dohme and Novo Nordisk. He also has received an unrestricted research grant from Boehringer Ingelheim Norway. A.H. has received lecture honoraria from AstraZeneca.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jenssen, T., Hartmann, A. Post-transplant diabetes mellitus in patients with solid organ transplants. Nat Rev Endocrinol 15, 172–188 (2019). https://doi.org/10.1038/s41574-018-0137-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-018-0137-7
This article is cited by
-
Multifunctional and Reconfigurable Electronic Fabrics Assisted by Artificial Intelligence for Human Augmentation
Advanced Fiber Materials (2024)
-
Prevalence of new-onset diabetes mellitus after kidney transplantation: a systematic review and meta-analysis
Acta Diabetologica (2024)
-
Metformin attenuates chronic lung allograft dysfunction: evidence in rat models
Respiratory Research (2023)
-
Glomerular proteomic profiling reveals early differences between preexisting and de novo type 2 diabetes in human renal allografts
BMC Nephrology (2023)
-
Pancreatic β-cell mitophagy as an adaptive response to metabolic stress and the underlying mechanism that involves lysosomal Ca2+ release
Experimental & Molecular Medicine (2023)