Abstract
Diabetes mellitus is a multifactorial disease affecting increasing numbers of patients worldwide. Progression to insulin-dependent diabetes mellitus is characterized by the loss or dysfunction of pancreatic β-cells, but the pathomechanisms underlying β-cell failure in type 1 diabetes mellitus and type 2 diabetes mellitus are still poorly defined. Regeneration of β-cell mass from residual islet cells or replacement by β-like cells derived from stem cells holds great promise to stop or reverse disease progression. However, the development of new treatment options is hampered by our limited understanding of human pancreas organogenesis due to the restricted access to primary tissues. Therefore, the challenge is to translate results obtained from preclinical model systems to humans, which requires comparative modelling of β-cell biology in health and disease. Here, we discuss diverse modelling systems across different species that provide spatial and temporal resolution of cellular and molecular mechanisms to understand the evolutionary conserved genotype–phenotype relationship and translate them to humans. In addition, we summarize the latest knowledge on organoids, stem cell differentiation platforms, primary micro-islets and pseudo-islets, bioengineering and microfluidic systems for studying human pancreas development and homeostasis ex vivo. These new modelling systems and platforms have opened novel avenues for exploring the developmental trajectory, physiology, biology and pathology of the human pancreas.
Key points
-
The evolutionary differences in pancreas development, function and failure undermine the translation of successful preclinical studies from animal models to humans.
-
Establishing novel therapeutic approaches for treatment of diabetes mellitus requires comprehensive understanding of human endocrine pancreas formation and function.
-
The proper development of endocrine cells relies on the tight coupling of morphogenetic events with cell differentiation programmes.
-
3D organoids and stem cell differentiation systems provide unique platforms for modelling human endocrine cell morphogenesis and differentiation.
-
Large animals, such as minipigs, offer novel systems for modelling diabetes mellitus closely to the disease development and progression in humans.
-
Establishing organizations that provide human primary pancreatic samples that are healthy or have diabetes mellitus have increased our understanding of pathomechanism of diabetes mellitus.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Katsarou, A. et al. Type 1 diabetes mellitus. Nat. Rev. Dis. Prim. 3, 17016 (2017).
DeFronzo, R. A. et al. Type 2 diabetes mellitus. Nat. Rev. Dis. Prim. 1, 15019 (2015).
Keenan, H. A. et al. Residual insulin production and pancreatic ß-cell turnover after 50 years of diabetes: Joslin Medalist study. Diabetes 59, 2–9 (2010).
Huang, T. et al. Pancreatic islet regeneration through PDX-1/Notch-1/Ngn3 signaling after gastric bypass surgery in db/db mice. Exp. Ther. Med. 14, 2831–2838 (2017).
Zhou, X. et al. Pancreatic hyperplasia after gastric bypass surgery in a GK rat model of non-obese type 2 diabetes. J. Endocrinol. 228, 13–23 (2016).
Taylor, R. et al. Remission of human type 2 diabetes requires decrease in liver and pancreas fat content but is dependent upon capacity for β cell recovery. Cell Metab. 28, 547–556 (2018).
Shapiro, A. M. J. et al. International trial of the edmonton protocol for islet transplantation. N. Engl. J. Med. 355, 1318–1330 (2006).
Zorn, A. M. & Wells, J. M. Vertebrate endoderm development and organ formation. Annu. Rev. Cell Dev. Biol. 25, 221–251 (2009).
Zorn, A. M. & Wells, J. M. Molecular basis of vertebrate endoderm development. Int. Rev. Cytol. 259, 49–111 (2007).
Stainier, D. Y. R. A glimpse into the molecular entrails of endoderm formation. Genes Dev. 16, 893–907 (2002).
Singh, S. P. et al. Different developmental histories of beta-cells generate functional and proliferative heterogeneity during islet growth. Nat. Commun. 8, 664 (2017).
Jennings, R. E. et al. Development of the human pancreas from foregut to endocrine commitment. Diabetes 62, 3514–3522 (2013). A comprehensive study on early stages of human pancreas development.
Jennings, R. E., Berry, A. A., Strutt, J. P., Gerrard, D. T. & Hanley, N. A. Human pancreas development. Development 142, 3126–3137 (2015).
Pan, F. C. & Brissova, M. Pancreas development in humans. Curr. Opin. Endocrinol. Diabetes. Obes. 21, 77–82 (2014).
Jennings, R. E. et al. Laser capture and deep sequencing reveals the transcriptomic programmes regulating the onset of pancreas and liver differentiation in human embryos. Stem Cell Rep. 9, 1387–1394 (2017).
Leiter, E. H. & Von Herrath, M. Animal models have little to teach us about type 1 diabetes: 2. In opposition to this proposal. Diabetologia 47, 1657–1660 (2004).
Roep, B. O. & Atkinson, M. Animal models have little to teach us about type 1 diabetes: 1. In support of this proposal. Diabetologia 47, 1650–1656 (2004).
Pagliuca, F. W. et al. Generation of functional human pancreatic beta cells in vitro. Cell 159, 428–439 (2014).
Russ, H. a et al. Controlled induction of human pancreatic progenitors produces functional beta-like cells in vitro. EMBO J. 34, 1759–1772 (2015).
Rezania, A. et al. Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells. Nat. Biotechnol. 32, 1121–1133 (2014). One of the first well-established protocols for in vitro generation of pancreatic β-like cells that is used extensively by many different laboratories worldwide.
Amour, K. A. D. et al. Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells. Nat. Biotechnol. 24, 1392–1401 (2006).
Roscioni, S. S., Migliorini, A., Gegg, M. & Lickert, H. Impact of islet architecture on β-cell heterogeneity, plasticity and function. Nat. Rev. Endocrinol. 12, 695–709 (2016).
Bastidas-Ponce, A., Scheibner, K., Lickert, H. & Bakhti, M. Cellular and molecular mechanisms coordinating pancreas development. Development 144, 2873–2888 (2017).
Pan, F. C. & Wright, C. Pancreas organogenesis: from bud to plexus to gland. Dev. Dyn. 240, 530–565 (2011).
Shih, H. P., Wang, A. & Sander, M. Pancreas organogenesis: from lineage determination to morphogenesis. Annu. Rev. Cell Dev. Biol. 29, 81–105 (2013).
Larsen, H. L. & Grapin-Botton, A. The molecular and morphogenetic basis of pancreas organogenesis. Semin. Cell Dev. Biol. 66, 51–68 (2017).
Röder, P. V., Wu, B., Liu, Y. & Han, W. Pancreatic regulation of glucose homeostasis. Exp. Mol. Med. 48, e219 (2016).
Suissa, Y. et al. Gastrin: a distinct fate of neurogenin3 positive progenitor cells in the embryonic pancreas. PLOS ONE 8, e70397 (2013).
Arnes, L., Hill, J. T., Gross, S., Magnuson, M. A. & Sussel, L. Ghrelin expression in the mouse pancreas defines a unique multipotent progenitor population. PLOS ONE 7, e52026 (2012).
Gittes, G. K. Developmental biology of the pancreas: a comprehensive review. Dev. Biol. 326, 4–35 (2009).
Kesavan, G. et al. Cdc42-mediated tubulogenesis controls cell specification. Cell 139, 791–801 (2009). The first study about the molecular mechanism underlying the formation of the pancreatic epithelial network during development; this study highlights the crosstalk between cell polarity and differentiation during pancreas development.
Villasenor, A., Chong, D. C., Henkemeyer, M. & Cleaver, O. Epithelial dynamics of pancreatic branching morphogenesis. Development 137, 4295–4305 (2010).
Bankaitis, E. D., Bechard, M. E. & Wright, C. V. E. Feedback control of growth, differentiation, and morphogenesis of pancreatic endocrine progenitors in an epithelial plexus niche. Genes Dev. 29, 2203–2216 (2015). The first study that analyses the formation and characteristics of the plexus niche within embryonic pancreatic epithelium.
Gradwohl, G., Dierich, A., LeMeur, M. & Guillemot, F. Neurogenin3 is required for the development of the four endocrine cell lineages of the pancreas. Proc. Natl Acad. Sci. USA 97, 1607–1611 (2000).
Gu, G., Dubauskaite, J. & Melton, D. A. Direct evidence for the pancreatic lineage: NGN3+ cells are islet progenitors and are distinct from duct progenitors. Development 129, 2447–2457 (2002).
Gouzi, M., Kim, Y. H., Katsumoto, K., Johansson, K. & Grapin-Botton, A. Neurogenin3 initiates stepwise delamination of differentiating endocrine cells during pancreas development. Dev. Dyn. 240, 589–604 (2011).
Cleaver, O. & Dor, Y. Vascular instruction of pancreas development. Development 139, 2833–2843 (2012).
Thorens, B. Neural regulation of pancreatic islet cell mass and function. Diabetes Obes. Metab. 16, 87–95 (2014).
Slack, J. M. W. Developmental biology of the pancreas. Development 121, 1569–1580 (1995).
Polak, M., Bouchareb-Banaei, L., Scharfmann, R. & Czernichow, P. Early pattern of differentiation in the human pancreas. Diabetes 49, 225–232 (2000).
Churchill, A. J. et al. Genetic evidence that Nkx2.2 acts primarily downstream of Neurog3 in pancreatic endocrine lineage development. eLife 6, e20010 (2017).
Anderson, K. R., White, P., Kaestner, K. H. & Sussel, L. Identification of known and novel pancreas genes expressed downstream of Nkx2.2 during development. BMC Dev. Biol. 9, 65 (2009).
Salisbury, R. J. et al. The window period of NEUROGENIN3 during human gestation. Islets 6, e954436 (2014).
Jeon, J., Correa-Medina, M., Ricordi, C., Edlund, H. & Diez, J. A. Endocrine cell clustering during human pancreas development. J. Histochem. Cytochem. 57, 811–824 (2009).
Ramond, C. et al. Understanding human fetal pancreas development using subpopulation sorting, RNA sequencing and single-cell profiling. Development 145, dev165480 (2018).
Ramond, C. et al. Reconstructing human pancreatic differentiation by mapping specific cell populations during development. eLife 6, e27564 (2017).
Billings, L. K. & Florez, J. C. The genetics of type 2 diabetes: what have we learned from GWAS? Ann. NY Acad. Sci. 1212, 59–77 (2010).
Pociot, F. Type 1 diabetes genome-wide association studies: not to be lost in translation. Clin. Transl Immunol. 6, e162 (2017).
Sladek, R. et al. A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature 445, 881–885 (2007).
Saxena, R. et al. Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 316, 1331–1336 (2007).
Morris, A. P. et al. Large-scale association analysis provides insights into the genetic architecture and pathophysiology of type 2 diabetes. Nat. Genet. 44, 981–990 (2012).
Mahajan, A. et al. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat. Genet. 46, 234–244 (2014).
Owen, K. R. Monogenic diabetes in adults: what are the new developments? Curr. Opin. Genet. Dev. 50, 103–110 (2018).
Meier, J. J. et al. β-Cell replication is the primary mechanism subserving the postnatal expansion of β-cell mass in humans. Diabetes 57, 1584–1594 (2008).
Heuvel-Borsboom, H., de Valk, H. W., Losekoot, M. & Westerink, J. Maturity onset diabetes of the young: seek and you will find. Neth. J. Med. 74, 193–200 (2016).
Shi, Z.-D. et al. Genome editing in hPSCs reveals GATA6 haploinsufficiency and a genetic interaction with GATA4 in human pancreatic development. Cell Stem Cell 20, 675–688 (2017).
Teo, A. K. K. et al. Early developmental perturbations in a human stem cell model of MODY5/HNF1B pancreatic hypoplasia. Stem Cell Rep. 6, 357–367 (2016).
Bastidas-Ponce, A. et al. Foxa2 and Pdx1 cooperatively regulate postnatal maturation of pancreatic β-cells. Mol. Metab. 6, 524–534 (2017).
Liu, J. S. E. & Hebrok, M. All mixed up: defining roles for β-cell subtypes in mature islets. Genes Dev. 31, 228–240 (2017).
Avrahami, D. et al. β-Cells are not uniform after all—novel insights into molecular heterogeneity of insulin-secreting cells. Diabetes Obes. Metab. 19, 147–152 (2017).
Nasteska, D. & Hodson, D. J. The role of beta cell heterogeneity in islet function and insulin release. J. Mol. Endocrinol. 61, R43–R60 (2018).
Johnston, N. R. et al. Beta cell hubs dictate pancreatic islet responses to glucose. Cell Metab. 24, 389–401 (2016). This study proves the existence of specialized β-cells that coordinate islet oscillatory behaviour.
Campanale, J. P., Sun, T. Y. & Montell, D. J. Development and dynamics of cell polarity at a glance. J. Cell Sci. 130, 1201–1207 (2017).
Bader, E. et al. Identification of proliferative and mature β-cells in the islets of langerhans. Nature 535, 430–434 (2016). The first study that presents the molecular marker for β-cell heterogeneity in mouse pancreas.
Cortijo, C., Gouzi, M., Tissir, F. & Grapin-Botton, A. Planar cell polarity controls pancreatic beta cell differentiation and glucose homeostasis. Cell Rep. 2, 1593–1606 (2012).
Dorrell, C. et al. Human islets contain four distinct subtypes of β cells. Nat. Commun. 7, 11756 (2016). The first study that reveals distinct surface markers distinguishing different human β-cell populations.
Wang, Y. J. et al. Single-cell mass cytometry analysis of the human endocrine pancreas. Cell Metab. 24, 616–626 (2016).
Oram, R. A. et al. The majority of patients with long-duration type 1 diabetes are insulin microsecretors and have functioning beta cells. Diabetologia 57, 187–191 (2014).
Butler, A. E. et al. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 52, 102–110 (2003).
Cinti, F. et al. Evidence of β-cell dedifferentiation in human type 2 diabetes. J. Clin. Endocrinol. Metab. 101, 1044–1054 (2016).
Dhawan, S., Dirice, E., Kulkarni, R. N. & Bhushan, A. Inhibition of TGF-β signaling promotes human pancreatic β-cell replication. Diabetes 65, 1208–1218 (2016).
El Ouaamari, A. et al. SerpinB1 promotes pancreatic β cell proliferation. Cell Metab. 23, 194–205 (2016).
Wang, P. et al. A high-throughput chemical screen reveals that harmine-mediated inhibition of DYRK1A increases human pancreatic beta cell replication. Nat. Med. 21, 383–388 (2015).
Puri, S. et al. Replication confers β cell immaturity. Nat. Commun. 9, 485 (2018).
Rui, J. et al. β cells that resist immunological attack develop during progression of autoimmune diabetes in NOD mice. Cell Metab. 25, 727–738 (2017). Reports that a subpopulation of β-cells can resist immune-mediated killing and might explain why residual β-cells exist in some patients with T1DM.
Wasserfall, C. et al. Persistence of pancreatic insulin mRNA expression and proinsulin protein in type 1 diabetes pancreata. Cell Metab. 26, 568–575 (2017).
Talchai, C., Xuan, S., Lin, H. V., Sussel, L. & Accili, D. Pancreatic β cell dedifferentiation as a mechanism of diabetic β cell failure. Cell 150, 1223–1234 (2012).
Wang, Z., York, N. W., Nichols, C. G. & Remedi, M. S. Pancreatic β cell dedifferentiation in diabetes and redifferentiation following insulin therapy. Cell Metab. 19, 872–882 (2014).
Evers, S. S., Sandoval, D. A. & Seeley, R. J. The physiology and molecular underpinnings of the effects of bariatric surgery on obesity and diabetes. Annu. Rev. Physiol. 79, 313–334 (2017).
Solar, M. et al. Pancreatic exocrine duct cells give rise to insulin-producing beta cells during embryogenesis but not after birth. Dev. Cell 17, 849–860 (2009).
Zhou, Q. et al. A multipotent progenitor domain guides pancreatic organogenesis. Dev. Cell 13, 103–114 (2007).
Schaffer, A. E., Freude, K. K., Nelson, S. B. & Sander, M. Nkx6 transcription factors and Ptf1a function as antagonistic lineage determinants in multipotent pancreatic progenitors. Dev. Cell 18, 1022–1029 (2010).
Kim, Y. H. et al. Cell cycle–dependent differentiation dynamics balances growth and endocrine differentiation in the pancreas. PLOS Biol. 13, e1002111 (2015).
Bechard, M. E. et al. Precommitment low-level Neurog3 expression defines a long-lived mitotic endocrine-biased progenitor pool that drives production of endocrine-committed cells. Genes Dev. 30, 1852–1865 (2016).
Apelqvist, A. Notch signalling controls pancreatic cell differentiation. Nature 400, 877–881 (1999).
Shih, H. P. et al. A Notch-dependent molecular circuitry initiates pancreatic endocrine and ductal cell differentiation. Development 139, 2488–2499 (2012).
Larsen, B. M., Hrycaj, S. M., Newman, M., Li, Y. & Wellik, D. M. Mesenchymal Hox6 function is required for pancreatic endocrine cell differentiation. Development 142, 3859–3868 (2015).
Serafimidis, I. et al. Pancreas lineage allocation and specification are regulated by sphingosine-1-phosphate signalling. PLOS Biol. 15, e2000949 (2017).
Löf-Öhlin, Z. M. et al. EGFR signalling controls cellular fate and pancreatic organogenesis by regulating apicobasal polarity. Nat. Cell Biol. 19, 1313–1325 (2017). This study shows the direct impact of epithelial polarity and morphogenesis on endocrine cell induction and differentiation.
Johansson, K. A. et al. Temporal control of neurogenin3 activity in pancreas progenitors reveals competence windows for the generation of different endocrine cell types. Dev. Cell 12, 457–465 (2007).
Rukstalis, J. M. & Habener, J. F. Snail2, a mediator of epithelial-mesenchymal transitions, expressed in progenitor cells of the developing endocrine pancreas. Gene Expr. Patterns 7, 471–479 (2007).
Kesavan, G. et al. Cdc42/N-WASP signaling links actin dynamics to pancreatic cell delamination and differentiation. Development 141, 685–696 (2014).
Miettinen, P. J. et al. Impaired migration and delayed differentiation of pancreatic islet cells in mice lacking EGF-receptors. Development 127, 2617–2627 (2000).
Freudenblum, J. et al. In vivo imaging of emerging endocrine cells reveals a requirement for PI3K-regulated motility in pancreatic islet morphogenesis. Development 145, dev158477 (2018).
Pauerstein, P. T. et al. A radial axis defined by semaphorin-to-neuropilin signaling controls pancreatic islet morphogenesis. Development 144, 3744–3754 (2017).
Clevers, H. Modeling development and disease with organoids. Cell 165, 1586–1597 (2016).
Lancaster, M. A. & Knoblich, J. A. Organogenesisin a dish: modeling development and disease using organoid technologies. Science 345, 1247125 (2014).
Kretzschmar, K. & Clevers, H. Organoids: modeling development and the stem cell niche in a dish. Dev. Cell 38, 590–600 (2016).
Dahl-Jensen, S. & Grapin-Botton, A. The physics of organoids: a biophysical approach to understanding organogenesis. Development 144, 946–951 (2017).
Eiraku, M. et al. Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature 472, 51–56 (2011).
Sato, T. et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 459, 262–265 (2009).
Huch, M. & Koo, B.-K. Modeling mouse and human development using organoid cultures. Development 142, 3113–3125 (2015).
Hindley, C. J., Cordero-Espinoza, L. & Huch, M. Organoids from adult liver and pancreas: stem cell biology and biomedical utility. Dev. Biol. 420, 251–261 (2016).
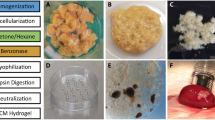
Greggio, C. et al. Artificial three-dimensional niches deconstruct pancreas development in vitro. Development 140, 4452–4462 (2013). The first study to generate pancreatic organoids from mouse embryonic pancreatic cells.
Sugiyama, T. et al. Reconstituting pancreas development from purified progenitor cells reveals genes essential for islet differentiation. Proc. Natl Acad. Sci. USA 110, 12691–12696 (2013).
Bonfanti, P. et al. Ex vivo expansion and differentiation of human and mouse fetal pancreatic progenitors are modulated by epidermal growth factor. Stem Cells Dev. 24, 1766–1778 (2015).
Hohwieler, M. et al. Human pluripotent stem cell-derived acinar/ductal organoids generate human pancreas upon orthotopic transplantation and allow disease modelling. Gut 66, 473–486 (2017).
Jin, L. et al. Colony-forming cells in the adult mouse pancreas are expandable in Matrigel and form endocrine/acinar colonies in laminin hydrogel. Proc. Natl Acad. Sci. USA 110, 3907–3912 (2013).
Jin, L. et al. In vitro multilineage differentiation and self-renewal of single pancreatic colony-forming cells from adult C57Bl/6 mice. Stem Cells Dev. 23, 899–909 (2014).
Huch, M. et al. Unlimited in vitro expansion of adult bi-potent pancreas progenitors through the Lgr5/R-spondin axis. EMBO J. 32, 2708–2721 (2013).
Lee, J. et al. Expansion and conversion of human pancreatic ductal cells into insulin-secreting endocrine cells. eLife 2, e00940 (2013).
Loomans, C. J. M. et al. Expansion of adult human pancreatic tissue yields organoids harboring progenitor cells with endocrine differentiation potential. Stem Cell Rep. 10, 1088–1101 (2018).
Sander, J. D. & Joung, J. K. CRISPR-Cas systems for editing, regulating and targeting genomes. Nat. Biotechnol. 32, 347–355 (2014).
Shapiro, A. M. et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N. Engl. J. Med. 343, 230–238 (2000).
Bruni, A., Gala-Lopez, B., Pepper, A. R., Abualhassan, N. S. & James Shapiro, A. M. Islet cell transplantation for the treatment of type 1 diabetes: recent advances and future challenges. Diabetes Metab. Syndr. Obes. 23, 211–223 (2014).
Assady, S. et al. Insulin production by human embryonic stem cells. Diabetes 50, 1691–1697 (2001).
Hrvatin, S. et al. Differentiated human stem cells resemble fetal, not adult, β cells. Proc. Natl Acad. Sci. USA 111, 3038–3043 (2014).
Haghverdi, L., Büttner, M., Wolf, F. A., Buettner, F. & Theis, F. J. Diffusion pseudotime robustly reconstructs lineage branching. Nat. Methods 13, 845–848 (2016).
Griffiths, J. A., Scialdone, A. & Marioni, J. C. Using single-cell genomics to understand developmental processes and cell fate decisions. Mol. Syst. Biol. 14, e8046 (2018).
Petersen, M. B. K. et al. Single-cell gene expression analysis of a human ESC model of pancreatic endocrine development reveals different paths to β-cell differentiation. Stem Cell Rep. 9, 1246–1261 (2017).
Cogger, K. F. et al. Glycoprotein 2 is a specific cell surface marker of human pancreatic progenitors. Nat. Commun. 8, 331 (2017).
Ameri, J. et al. Efficient generation of glucose-responsive beta cells from isolated GP2+ human pancreatic progenitors. Cell Rep. 19, 36–49 (2017).
Leibiger, I. B. & Berggren, P. O. Intraocular in vivo imaging of pancreatic islet cell physiology/pathology. Mol. Metab. 6, 1002–1009 (2017).
Brissova, M. et al. Assessment of human pancreatic islet architecture and composition by laser scanning confocal microscopy. J. Histochem. Cytochem. 53, 1087–1097 (2005).
Steiner, D. J., Kim, A., Miller, K. & Hara, M. Pancreatic islet plasticity: interspecies comparison of islet architecture and composition. Islets 2, 135–145 (2010).
Chambers, A. P. et al. The role of pancreatic preproglucagon in glucose homeostasis in mice. Cell Metab. 25, 927–934 (2017).
Drucker, D. J. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 27, 740–756 (2018).
van der Meulen, T. & Huising, M. O. Role of transcription factors in the transdifferentiation of pancreatic islet cells. J. Mol. Endocrinol. 54, R103–R117 (2015).
DiGruccio, M. R. et al. Comprehensive alpha, beta and delta cell transcriptomes reveal that ghrelin selectively activates delta cells and promotes somatostatin release from pancreatic islets. Mol. Metab. 5, 449–458 (2016).
Brissova, M. et al. α cell function and gene expression are compromised in type 1 diabetes. Cell Rep. 6, 2667–2676 (2018).
Kao, D. I. et al. Endothelial cells control pancreatic cell fate at defined stages through EGFl7 signaling. Stem Cell Rep. 4, 181–189 (2015).
Aamodt, K. I. & Powers, A. C. Signals in the pancreatic islet microenvironment influence β-cell proliferation. Diabetes Obes. Metab. 19, 124–136 (2017).
Camp, J. G. et al. Multilineage communication regulates human liver bud development from pluripotency. Nature 546, 533–538 (2017). This study shows the dissection of interlineage communication in human liver bud development by single-cell RNA sequencing.
Wang, X. et al. Genome-wide analysis of PDX1 target genes in human pancreatic progenitors. Mol. Metab. 9, 57–68 (2018).
Kondo, Y., Toyoda, T., Inagaki, N. & Osafune, K. iPSC technology-based regenerative therapy for diabetes. J. Diabetes Invest. 9, 234–243 (2018).
Teo, A. K. K., Gupta, M. K., Doria, A. & Kulkarni, R. N. Dissecting diabetes/metabolic disease mechanisms using pluripotent stem cells and genome editing tools. Mol. Metab. 4, 593–604 (2015).
Iovino, S. et al. Genetic insulin resistance is a potent regulator of gene expression and proliferation in human iPS cells. Diabetes 63, 4130–4142 (2014).
Tiyaboonchai, A. et al. GATA6 plays an important role in the induction of human definitive endoderm, development of the pancreas, and Functionality of pancreatic β cells. Stem Cell Reports 8, 589–604 (2017).
Carrasco, M., Delgado, I., Soria, B., Martín, F. & Rojas, A. GATA4 and GATA6 control mouse pancreas organogenesis. J. Clin. Invest. 122, 3504–3515 (2012).
Xuan, S. et al. Pancreas-specific deletion of mouse Gata4 and Gata6 causes pancreatic agenesis. J. Clin. Invest. 122, 3516–3528 (2012).
Shang, L. et al. β-cell dysfunction due to increased ER stress in a stem cell model of wolfram syndrome. Diabetes 63, 923–933 (2014).
Sagen, J. V. et al. Permanent neonatal diabetes due to mutations in KCNJ11 encoding Kir6.2: patient characteristics and initial response to sulfonylurea therapy. Diabetes 53, 2713–2718 (2004).
Gloyn, A. L. et al. Activating mutations in the gene encoding the ATP-sensitive potassium-channel subunit Kir6.2 and permanent neonatal diabetes. N. Engl. J. Med. 350, 1838–1849 (2004).
Reissaus, C. A. & Piston, D. W. Reestablishment of glucose inhibition of glucagon secretion in small pseudoislets. Diabetes 66, 960–969 (2017).
Halban, P. A., Powers, S. L., George, K. L. & Bonner-Weir, S. Spontaneous reassociation of dispersed adult rat pancreatic islet cells into aggregates with three-dimensional architecture typical of native islets. Diabetes 36, 783–790 (1987).
Yesildag, B. et al. Using uniform reaggregated pancreatic islets in a microfluidic perifusion system enables studying insulin release dynamics at single-islet level. ethz.ch https://www.research-collection.ethz.ch/handle/20.500.11850/237502 (2017).
Marciniak, A. et al. Using pancreas tissue slices for in situ studies of islet of Langerhans and acinar cell biology. Nat. Protoc. 9, 2809–2822 (2014).
Speier, S. et al. Noninvasive in vivo imaging of pancreatic islet cell biology. Nat. Med. 14, 574–578 (2008). This study establishes a technique to transplant isolated islets into the anterior chamber of the eye, allowing live imaging of pancreatic islets in vivo.
Miyazaki, J. et al. Establishment of a pancreatic b cell line that retains glucose inducible insulin secretion: special reference to expression of glucose transporter isoforms. Endocrinology 127, 126–132 (1990).
Asfari, M. et al. Establishment of 2-mercaptoethanol-dependent differentiated insulin-secreting cell lines. Endocrinology 130, 167–178 (1992).
Iwasaki, M. et al. Establishment of new clonal pancreatic β-cell lines (MIN6-K) useful for study of incretin/cyclic adenosine monophosphate signaling. J. Diabetes Investig. 1, 137–142 (2010).
Ravassard, P. et al. A genetically engineered human pancreatic β cell line exhibiting glucose-inducible insulin secretion. J. Clin. Invest. 121, 3589–3597 (2011).
Scharfmann, R. & Pechberty, S. Development of a conditionally immortalized human pancreatic β cell line. J. Clin. Invest. 124, 2087–2098 (2014).
Benazra, M. et al. A human beta cell line with drug inducible excision of immortalizing transgenes. Mol. Metab. 4, 916–925 (2015).
Tsonkova, V. G. et al. The EndoC-βH1 cell line is a valid model of human beta cells and applicable for screenings to identify novel drug target candidates. Mol. Metab. 8, 144–157 (2018).
Hakonen, E. et al. MANF protects human pancreatic beta cells against stress-induced cell death. Diabetologia 61, 2202–2214 (2018).
Diedisheim, M. et al. Modeling human pancreatic beta cell dedifferentiation. Mol. Metab. 10, 74–86 (2018).
Lecomte, M.-J. et al. Aggregation of engineered human β-cells into pseudoislets: insulin secretion and gene expression profile in normoxic and hypoxic milieu. Cell. Med. 8, 99–112 (2016).
Skrzypek, K., Barrera, Y. B., Groth, T. & Stamatialis, D. Endothelial and beta cell composite aggregates for improved function of a bioartificial pancreas encapsulation device. Int. J. Artif. Organs 41, 152–159 (2018).
Spelios, M. G., Afinowicz, L. A., Tipon, R. C. & Akirav, E. M. Human EndoC-βH1 β-cells form pseudoislets with improved glucose sensitivity and enhanced GLP-1 signaling in the presence of islet-derived endothelial cells. Am. J. Physiol. Metab. 314, E512–E521 (2018).
Sankar, K. S. et al. Culturing pancreatic islets in microfluidic flow enhances morphology of the associated endothelial cells. PLOS ONE 6, e24904 (2011).
Komatsu, H. et al. Oxygen environment and islet size are the primary limiting factors of isolated pancreatic islet survival. PLOS ONE 12, e0183780 (2017).
Allazetta, S. & Lutolf, M. P. Stem cell niche engineering through droplet microfluidics. Curr. Opin. Biotechnol. 35, 86–93 (2015).
Bhatia, S. N. & Ingber, D. E. Microfluidic organs-on-chips. Nat. Biotechnol. 32, 760–772 (2014).
Ronaldson-Bouchard, K. & Vunjak-Novakovic, G. Organs-on-a-chip: a fast track for engineered human tissues in drug development. Cell Stem Cell 22, 310–324 (2018).
Nguyen, D. T. T., Van Noort, D., Jeong, I. K. & Park, S. Endocrine system on chip for a diabetes treatment model. Biofabrication 9, 015021 (2017).
Ortega-Prieto, A. M. et al. 3D microfluidic liver cultures as a physiological preclinical tool for hepatitis B virus infection. Nat. Commun. 9, 682 (2018).
Brandenberg, N. & Lutolf, M. P. In situ patterning of microfluidic networks in 3D cell-laden hydrogels. Adv. Mater. 28, 7450–7456 (2016).
Silva, P. N., Green, B. J., Altamentova, S. M. & Rocheleau, J. V. A microfluidic device designed to induce media flow throughout pancreatic islets while limiting shear-induced damage. Lab. Chip 13, 4374 (2013).
Mohammed, J. S., Wang, Y., Harvat, T. A., Oberholzer, J. & Eddington, D. T. Microfluidic device for multimodal characterization of pancreatic islets. Lab. Chip 9, 97–106 (2009).
Bauer, S. et al. Functional coupling of human pancreatic islets and liver spheroids on-a-chip: towards a novel human ex vivo type 2 diabetes model. Sci. Rep. 7, 14620 (2017).
Tritschler, S., Theis, F. J., Lickert, H. & Böttcher, A. Systematic single-cell analysis provides new insights into heterogeneity and plasticity of the pancreas. Mol. Metab. 6, 974–990 (2017).
King, A. J. F. The use of animal models in diabetes research. Br. J. Pharmacol. 166, 877–894 (2012).
Dufrane, D. et al. Streptozotocin-induced diabetes in large animals (pigs/primates): role of GLUT2 transporter and β-cell plasticity. Transplantation 81, 36–45 (2006).
Kleinert, M. et al. Animal models of obesity and diabetes mellitus. Nat. Rev. Endocrinol. 14, 140–162 (2018).
Ionut, V. et al. Novel canine models of obese prediabetes and mild type 2 diabetes. Am. J. Physiol. Endocrinol. Metab. 298, E38–E48 (2010).
Henson, M. S. & O’Brien, T. D. Feline models of type 2 diabetes mellitus. ILAR J. 47, 234–242 (2006).
de Koning, E. J., Bodkin, N. L., Hansen, B. C. & Clark, A. Diabetes mellitus in Macaca mulatta monkeys is characterised by islet amyloidosis and reduction in beta-cell population. Diabetologia 36, 378–384 (1993).
Wagner, J. D. et al. Old world nonhuman primate models of type 2 diabetes mellitus. ILAR J. 47, 259–271 (2006).
Renner, S. et al. Metabolic syndrome and extensive adipose tissue inflammation in morbidly obese Göttingen minipigs. Mol. Metab. 16, 180–190 (2018).
Bellinger, D. A., Merricks, E. P. & Nichols, T. C. Swine models of type 2 diabetes mellitus: insulin resistance, glucose tolerance, and cardiovascular complications. ILAR J. 47, 243–258 (2006).
Kobayashi, T. et al. Principles of early human development and germ cell program from conserved model systems. Nature 546, 416–420 (2017).
Kemter, E. et al. INS-eGFP transgenic pigs: a novel reporter system for studying maturation, growth and vascularisation of neonatal islet-like cell clusters. Diabetologia 60, 1152–1156 (2017).
Umeyama, K. et al. Dominant-negative mutant hepatocyte nuclear factor 1α induces diabetes in transgenic-cloned pigs. Transgen. Res. 18, 697–706 (2009).
Renner, S. et al. Permanent neonatal diabetes in INSC94Y transgenic pigs. Diabetes 62, 1505–1511 (2013).
Ludwig, B. et al. Favorable outcome of experimental islet xenotransplantation without immunosuppression in a nonhuman primate model of diabetes. Proc. Natl Acad. Sci. USA 114, 11745–11750 (2017).
Salama, B. F. & Korbutt, G. S. Porcine islet xenografts: a clinical source of ß-cell grafts. Curr. Diabetes Rep. 17, 14 (2017).
Wu, J. et al. Interspecies chimerism with mammalian pluripotent stem cells. Cell 168, 473–486 (2017).
Wu, J. & Belmonte, J. C. I. Interspecies chimeric complementation for the generation of functional human tissues and organs in large animal hosts. Transgen. Res. 25, 375–384 (2016).
Yamaguchi, T. et al. Interspecies organogenesis generates autologous functional islets. Nature 542, 191–196 (2017).
Matsunari, H. et al. Blastocyst complementation generates exogenic pancreas in vivo in apancreatic cloned pigs. Proc. Natl Acad. Sci. USA 110, 4557–4562 (2013).
Kobayashi, T. et al. Generation of rat pancreas in mouse by interspecific blastocyst injection of pluripotent stem cells. Cell 142, 787–799 (2010).
Korbutt, G. S. et al. Large scale isolation, growth, and function of porcine neonatal islet cells. J. Clin. Invest. 97, 2119–2129 (1996).
Zeng, C. et al. Pseudotemporal ordering of single cells reveals metabolic control of postnatal β cell proliferation. Cell Metab. 25, 1160–1175 (2017). This study uses single-cell RNA sequencing analysis of β-cells at different postnatal stages to reveal metabolic pathways regulating postnatal β-cell proliferation.
Qiu, W. L. et al. Deciphering pancreatic islet β cell and α cell maturation pathways and characteristic features at the single-cell level. Cell Metab. 25, 1194–1205 (2017). This study uses single-cell RNA sequencing analysis of α-cells and β-cells at different postnatal stages to reveal the signalling pathways regulating postnatal β-cell maturation.
Wolf, E., Braun-Reichhart, C., Streckel, E. & Renner, S. Genetically engineered pig models for diabetes research. Transgen. Res. 23, 27–38 (2014).
Renner, S. et al. Glucose intolerance and reduced proliferation of pancreatic β-cells in transgenic pigs with impaired glucose-dependent insulinotropic polypeptide function. Diabetes 59, 1228–1238 (2010).
Liu, M. et al. INS-gene mutations: from genetics and beta cell biology to clinical disease. Mol. Aspects Med. 42, 3–18 (2015).
Szabat, M. et al. Reduced insulin production relieves endoplasmic reticulum stress and induces β cell proliferation. Cell Metab. 23, 179–193 (2016).
O’Sullivan-Murphy, B. & Urano, F. ER stress as a trigger for β-cell dysfunction and autoimmunity in type 1 diabetes. Diabetes 61, 780–781 (2012).
Cui, Y. et al. Fluctuation localization imaging-based fluorescence in situ hybridization (fliFISH) for accurate detection and counting of RNA copies in single cells. Nucleic Acids Res. 46, e7 (2018).
Thiery, G. et al. Multiplex target protein imaging in tissue sections by mass spectrometry - TAMSIM. Rapid Commun. Mass Spectrom. 21, 823–829 (2007).
Kang, C. C. et al. Single cell-resolution western blotting. Nat. Protoc. 11, 1508–1530 (2016).
Wells, J. M. & Melton, D. A. Vertebrate endoderm development. Annu. Rev. Cell Dev. Biol. 15, 393–410 (1999).
Carlsson, G. L., Scott Heller, R., Serup, P. & Hyttel, P. Immunohistochemistry of pancreatic development in cattle and pig. Anat. Histol. Embryol. 39, 107–119 (2010).
Zabel, M. et al. Immunocytochemical studies on endocrine cells of alimentary tract of the pig in the embryonic and fetal period of life. Folia Morphol. (Warsz) 54, 69–80 (1995).
Alumets, J., Håkanson, R. & Sundler, F. Ontogeny of endocrine cells in porcine gut and pancreas. An immunocytochemical study. Gastroenterology 85, 1359–1372 (1983).
Piper, K. et al. Beta cell differentiation during early human pancreas development. J. Endocrinol. 181, 11–23 (2004).
Kim, A. et al. Islet architecture: a comparative study. Islets 1, 129–136 (2009).
Marchetti, P. et al. Morphometrical and immunocytochemical characterization of the porcine endocrine pancreas. Transpl. Proc. 22, 727–728 (1990).
Orci, L., Malaisse-Lagae, F., Baetens, D. & Perrelet, A. Pancreatic-polypeptide-rich regions in human pancreas. Lancet 312, 1200–1201 (1978).
Bosco, D. et al. Unique arrangement of alpha- and beta-cells in human islets of Langerhans. Diabetes 59, 1202–1210 (2010).
Acknowledgements
The authors apologize to those whose work has not been cited due to limited space. The authors would like to thank Ciro Salinno for helpful comments on the manuscript. The authors acknowledge the support of the Helmholtz Association (Helmholtz-Gemeinschaft), German Research Foundation (Deutsche Forschungsgemeinschaft) and German Center for Diabetes Research (Deutsches Zentrum für Diabetes Forschung, DZD e.V.).
Reviewer information
Nature Reviews Endocrinology thanks A. Pugliese and the other anonymous reviewers for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to researching data for the article, discussion of content, writing the article and reviewing and/or editing the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Juvenile Diabetes Research Foundation (JDRF) network program: www.JDRFnPOD.org
Integrated islet distribution program (IIDP): https://iidp.coh.org
Human islet research network (HIRN): https://hirnetwork.org
Rights and permissions
About this article
Cite this article
Bakhti, M., Böttcher, A. & Lickert, H. Modelling the endocrine pancreas in health and disease. Nat Rev Endocrinol 15, 155–171 (2019). https://doi.org/10.1038/s41574-018-0132-z
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-018-0132-z
This article is cited by
-
ISL1 controls pancreatic alpha cell fate and beta cell maturation
Cell & Bioscience (2023)
-
Delineating mouse β-cell identity during lifetime and in diabetes with a single cell atlas
Nature Metabolism (2023)
-
Modelling metabolic diseases and drug response using stem cells and organoids
Nature Reviews Endocrinology (2022)
-
Synaptotagmin-13 orchestrates pancreatic endocrine cell egression and islet morphogenesis
Nature Communications (2022)
-
Regenerative approaches to preserve pancreatic β-cell mass and function in diabetes pathogenesis
Endocrine (2022)