Abstract
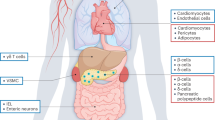
In healthy individuals, the incretin hormone glucagon-like peptide 1 (GLP1) potentiates insulin release and suppresses glucagon secretion in response to the ingestion of nutrients. GLP1 also delays gastric emptying and increases satiety. In patients with type 2 diabetes mellitus (T2DM), supraphysiological doses of GLP1 normalize the endogenous insulin response during a hyperglycaemic clamp. Owing to the short plasma half-life of native GLP1, several GLP1 receptor agonists (GLP1RAs) with longer half-lives have been developed for the treatment of T2DM. These compounds vary in chemical structure, pharmacokinetics and size, which results in different clinical effects on hyperglycaemia and body weight loss; these variations might also explain the difference in cardiovascular effect observed in large-scale cardiovascular outcome trials, in which certain GLP1RAs were shown to have a positive effect on cardiovascular outcomes. Owing to their metabolic effects, GLP1RAs are also considered for the treatment of several other lifestyle-induced conditions, such as obesity, prediabetes and liver disease. This Review provides insights into the physiology of GLP1 and its involvement in the pathophysiology of T2DM and an overview of the currently available and emerging GLP1RAs. Furthermore, we review the results from the currently available large-scale cardiovascular outcome trials and the use of GLP1RAs for other indications.
Key points
-
The incretin hormone glucagon-like peptide 1 (GLP1) promotes satiety and potentiates insulin release and suppression of glucagon release in response to the ingestion of nutrients.
-
Owing to the short plasma half-life of GLP1, several GLP1 receptor agonists (GLP1RAs) were developed with different chemical structures and pharmacokinetic profiles for type 2 diabetes mellitus (T2DM) treatment.
-
GLP1RAs can be categorized as short-acting or long-acting according to their time–action profile.
-
Both short-acting and long-acting GLP1RAs reduce body weight, whereas short-acting GLP1RAs have a greater effect on postprandial plasma levels of glucose and long-acting GLP1RAs predominantly lower fasting plasma concentrations of glucose.
-
Some GLP1RAs (liraglutide and semaglutide) have proved to have positive effects on cardiovascular outcomes in T2DM.
-
The effects of GLP1RAs are sought to be exploited in the treatment of several other conditions, including prediabetes, T1DM, obesity and liver disease.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Nauck, M. A. et al. Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. J. Clin. Endocrinol. Metab. 63, 492–498 (1986).
Holst, J. J. The physiology of glucagon-like peptide 1. Physiol. Rev. 87, 1409–1439 (2007).
Sandoval, D. A. & D’Alessio, D. A. Physiology of proglucagon peptides: role of glucagon and GLP-1 in health and disease. Physiol. Rev. 95, 513–548 (2015).
Vilsbøll, T. & Holst, J. J. Incretins, insulin secretion and Type 2 diabetes mellitus. Diabetologia 47, 357–366 (2004).
Nauck, M. A., Bartels, E., Orskov, C., Ebert, R. & Creutzfeldt, W. Additive insulinotropic effects of exogenous synthetic human gastric inhibitory polypeptide and glucagon-like peptide-1-(7–36) amide infused at near-physiological insulinotropic hormone and glucose concentrations. J. Clin. Endocrinol. Metab. 76, 912–917 (1993).
Nauck, M. A. et al. Preserved incretin activity of glucagon-like peptide 1 [7-36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J. Clin. Invest. 91, 301–307 (1993).
Kjems, L. L., Holst, J. J., Vølund, A. & Madsbad, S. The influence of GLP-1 on glucose-stimulated insulin secretion: effects on beta-cell sensitivity in type 2 and nondiabetic subjects. Diabetes 52, 380–386 (2003).
Jorsal, T. et al. Enteroendocrine K and L cells in healthy and type 2 diabetic individuals. Diabetologia 61, 284–294 (2017).
Sonne, D. P., Rehfeld, J. F., Holst, J. J., Vilsbøll, T. & Knop, F. K. Postprandial gallbladder emptying in patients with type 2 diabetes: potential implications for bile-induced secretion of glucagon-like peptide 1. Eur. J. Endocrinol. 171, 407–419 (2014).
Wettergren, A. et al. Truncated GLP-1 (proglucagon 78-107-amide) inhibits gastric and pancreatic functions in man. Dig. Dis. Sci. 38, 665–673 (1993).
Nauck, M. A. et al. Glucagon-like peptide 1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am. J. Physiol. 273, E981–E988 (1997).
Nauck, M. A., Kemmeries, G., Holst, J. J. & Meier, J. J. Rapid tachyphylaxis of the glucagon-like peptide 1–induced deceleration of gastric emptying in humans. Diabetes 60, 1561–1565 (2011).
Verdich, C. et al. A meta-analysis of the effect of glucagon-like peptide-1 (7–36) amide on ad libitum energy intake in humans. J. Clin. Endocrinol. Metab. 86, 4382–4389 (2001).
Muskiet, M. H. A. et al. GLP-1 and the kidney: from physiology to pharmacology and outcomes in diabetes. Nat. Rev. Nephrol. 13, 605–628 (2017).
Skov, J. Effects of GLP-1 in the kidney. Rev. Endocr. Metab. Disord. 15, 197–207 (2014).
Bose, A. K., Mocanu, M. M., Carr, R. D., Brand, C. L. & Yellon, D. M. Glucagon-like peptide 1 can directly protect the heart against ischemia/reperfusion injury. Diabetes 54, 146–151 (2005).
Nikolaidis, L. A. et al. Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation 109, 962–965 (2004).
Meier, J. J. et al. Glucagon-like peptide 1 abolishes the postprandial rise in triglyceride concentrations and lowers levels of non-esterified fatty acids in humans. Diabetologia 49, 452–458 (2006).
Drucker, D. J. The cardiovascular biology of glucagon-like peptide-1. Cell Metab. 24, 15–30 (2016).
Nauck, M., Stöckmann, F., Ebert, R. & Creutzfeldt, W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29, 46–52 (1986).
Vaag, A. A., Holst, J. J., Vølund, A. & Beck-Nielsen, H. B. Gut incretin hormones in identical twins discordant for non-insulin-dependent diabetes mellitus (NIDDM)—evidence for decreased glucagon-like peptide 1 secretion during oral glucose ingestion in NIDDM twins. Eur. J. Endocrinol. 135, 425–432 (1996).
Nyholm, B. et al. Twenty-four-hour insulin secretion rates, circulating concentrations of fuel substrates and gut incretin hormones in healthy offspring of Type II (non-insulin-dependent) diabetic parents: evidence of several aberrations. Diabetologia 42, 1314–1323 (1999).
Knop, F. K. et al. Reduced incretin effect in type 2 diabetes: cause or consequence of the diabetic state? Diabetes 56, 1951–1959 (2007).
Kosinski, M. et al. Postpartum reversibility of impaired incretin effect in gestational diabetes mellitus. Regul. Pept. 186, 104–107 (2013).
Færch, K. et al. GLP-1 response to oral glucose is reduced in prediabetes, screen-detected type 2 diabetes, and obesity and influenced by sex: The ADDITION-PRO Study. Diabetes 64, 2513–2525 (2015).
Calanna, S. et al. Secretion of glucagon-like peptide-1 in patients with type 2 diabetes mellitus: systematic review and meta-analyses of clinical studies. Diabetologia 56, 965–972 (2013).
Vilsbøll, T., Agersø, H., Krarup, T. & Holst, J. J. Similar elimination rates of glucagon-like peptide-1 in obese type 2 diabetic patients and healthy subjects. J. Clin. Endocrinol. Metab. 88, 220–224 (2003).
Vilsbøll, T., Krarup, T., Madsbad, S. & Holst, J. J. Defective amplification of the late phase insulin response to glucose by GIP in obese type II diabetic patients. Diabetologia 45, 1111–1119 (2002).
Nauck, M. A. et al. Normalization of fasting hyperglycaemia by exogenous glucagon-like peptide 1 (7–36 amide) in type 2 (non-insulin-dependent) diabetic patients. Diabetologia 36, 741–744 (1993).
Rachman, J., Barrow, B. A., Levy, J. C. & Turner, R. C. Near-normalisation of diurnal glucose concentrations by continuous administration of glucagon-like peptide-1 (GLP-1) in subjects with NIDDM. Diabetologia 40, 205–211 (1997).
Bhavsar, S., Mudaliar, S. & Cherrington, A. Evolution of exenatide as a diabetes therapeutic. Curr. Diabetes Rev. 9, 161–193 (2013).
Greig, S. L. & Scott, L. J. Insulin degludec/liraglutide: a review in type 2 diabetes. Drugs 75, 1523–1534 (2015).
Scott, L. J. Insulin glargine/lixisenatide: a review in type 2 diabetes. Drugs 77, 1353–1362 (2017).
Sánchez-Garrido, M. A. et al. GLP-1/glucagon receptor co-agonism for treatment of obesity. Diabetologia 60, 1851–1861 (2017).
Henry, R. R. et al. Clinical Impact of ITCA 650, a novel drug-device GLP-1 receptor agonist, in uncontrolled type 2 diabetes and very high baseline HbA1c: The FREEDOM-1 HBL (high baseline) study. Diabetes Care 41, 613–619 (2018).
Rosenstock, J. et al. Efficacy and safety of ITCA 650, a novel drug-device GLP-1 receptor agonist, in type 2 diabetes uncontrolled with oral antidiabetes drugs: The FREEDOM-1 trial. Diabetes Care 41, 333–340 (2018).
Christensen, M., Miossec, P., Larsen, B. D., Werner, U. & Knop, F. K. The design and discovery of lixisenatide for the treatment of type 2 diabetes mellitus. Expert Opin. Drug Discov. 9, 1223–1251 (2014).
Kolterman, O. G. et al. Synthetic exendin-4 (exenatide) significantly reduces postprandial and fasting plasma glucose in subjects with type 2 diabetes. J. Clin. Endocrinol. Metab. 88, 3082–3089 (2003).
Kendall, D. M. et al. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylurea. Diabetes Care 28, 1083–1091 (2005).
Lorenz, M. et al. Effects of lixisenatide once daily on gastric emptying in type 2 diabetes—relationship to postprandial glycemia. Regul. Pept. 185, 1–8 (2013).
Kapitza, C. et al. Pharmacodynamic characteristics of lixisenatide once daily versus liraglutide once daily in patients with type 2 diabetes insufficiently controlled on metformin. Diabetes Obes. Metab. 15, 642–649 (2013).
Raccah, D., Gourdy, P., Sagnard, L. & Ceriello, A. Lixisenatide as add-on to oral anti-diabetic therapy: an effective treatment for glycaemic control with body weight benefits in type 2 diabetes. Diabetes Metab. Res. Rev. 30, 742–748 (2014).
Drucker, D. J. et al. Exenatide once weekly versus twice daily for the treatment of type 2 diabetes: a randomised, open-label, non-inferiority study. Lancet 372, 1240–1250 (2008).
Buse, J. B. et al. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet 374, 39–47 (2009).
McCormack, P. L. Exenatide twice daily: a review of its use in the management of patients with type 2 diabetes mellitus. Drugs 74, 325–351 (2014).
Anderson, S. L. & Trujillo, J. M. Lixisenatide in type 2 diabetes: latest evidence and clinical usefulness. Ther. Adv. Chronic Dis. 7, 4–17 (2016).
Madsbad, S. Review of head-to-head comparisons of glucagon-like peptide-1 receptor agonists. Diabetes Obes. Metab. 18, 317–332 (2016).
Rosenstock, J. et al. Efficacy and safety of lixisenatide once daily versus exenatide twice daily in type 2 diabetes inadequately controlled on metformin: a 24-week, randomized, open-label, active-controlled study (GetGoal-X). Diabetes Care 36, 2945–2951 (2013).
Fonseca, V. A. et al. Efficacy and safety of the once-daily GLP-1 receptor agonist lixisenatide in monotherapy: a randomized, double-blind, placebo-controlled trial in patients with type 2 diabetes (GetGoal-Mono). Diabetes Care 35, 1225–1231 (2012).
Riddle, M. C. et al. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled by established basal insulin: a 24-week, randomized, placebo-controlled comparison (GetGoal-L). Diabetes Care 36, 2489–2496 (2013).
Fineman, M. S. et al. Clinical relevance of anti-exenatide antibodies: safety, efficacy and cross-reactivity with long-term treatment. Diabetes Obes. Metab. 14, 546–554 (2012).
Buse, J. B. et al. Liraglutide treatment is associated with a low frequency and magnitude of antibody formation with no apparent impact on glycemic response or increased frequency of adverse events: results from the liraglutide effect and action in diabetes (LEAD) trials. J. Clin. Endocrinol. Metab. 96, 1695–1702 (2011).
Buse, J. B. et al. DURATION-1: exenatide once weekly produces sustained glycemic control and weight loss over 52 weeks. Diabetes Care 33, 1255–1261 (2010).
Blevins, T. et al. DURATION-5: exenatide once weekly resulted in greater improvements in glycemic control compared with exenatide twice daily in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 96, 1301–1310 (2011).
Wysham, C. et al. Efficacy and safety of dulaglutide added onto pioglitazone and metformin versus exenatide in type 2 diabetes in a randomized controlled trial (AWARD-1). Diabetes Care 37, 2159–2167 (2014).
Halawi, H. et al. Effects of liraglutide on weight, satiation, and gastric functions in obesity: a randomised, placebo-controlled pilot trial. Lancet Gastroenterol. Hepatol. 2, 890–899 (2017).
Buse, J. B. et al. Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): a randomised, open-label study. Lancet 381, 117–124 (2013).
Pratley, R. E. et al. Once-weekly albiglutide versus once-daily liraglutide in patients with type 2 diabetes inadequately controlled on oral drugs (HARMONY 7): a randomised, open-label, multicentre, non-inferiority phase 3 study. Lancet Diabetes Endocrinol. 2, 289–297 (2014).
Dungan, K. M. et al. Once-weekly dulaglutide versus once-daily liraglutide in metformin-treated patients with type 2 diabetes (AWARD-6): a randomised, open-label, phase 3, non-inferiority trial. Lancet 384, 1349–1357 (2014).
Ahrén, B. et al. HARMONY 3: 104-week randomized, double-blind, placebo- and active-controlled trial assessing the efficacy and safety of albiglutide compared with placebo, sitagliptin, and glimepiride in patients with type 2 diabetes taking metformin. Diabetes Care 37, 2141–2148 (2014).
Home, P. D. et al. Efficacy and tolerability of albiglutide versus placebo or pioglitazone over 1 year in people with type 2 diabetes currently taking metformin and glimepiride: HARMONY 5. Diabetes Obes. Metab. 17, 179–187 (2015).
Nauck, M. A. et al. Efficacy and safety of once-weekly GLP-1 receptor agonist albiglutide (HARMONY 2): 52 week primary endpoint results from a randomised, placebo-controlled trial in patients with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diabetologia 59, 266–274 (2016).
Reusch, J. et al. Efficacy and safety of once-weekly glucagon-like peptide 1 receptor agonist albiglutide (HARMONY 1 trial): 52-week primary endpoint results from a randomized, double-blind, placebo-controlled trial in patients with type 2 diabetes mellitus not controlled on pioglitazone, with or without metformin. Diabetes Obes. Metab. 16, 1257–1264 (2014).
Rosenstock, J. et al. Advancing basal insulin replacement in type 2 diabetes inadequately controlled with insulin glargine plus oral agents: a comparison of adding albiglutide, a weekly GLP-1 receptor agonist, versus thrice-daily prandial insulin lispro. Diabetes Care 37, 2317–2325 (2014).
Weissman, P. N. et al. HARMONY 4: randomised clinical trial comparing once-weekly albiglutide and insulin glargine in patients with type 2 diabetes inadequately controlled with metformin with or without sulfonylurea. Diabetologia 57, 2475–2484 (2014).
Brønden, A., Knop, F. K. & Christensen, M. B. Clinical pharmacokinetics and pharmacodynamics of albiglutide. Clin. Pharmacokinet. 56, 719–731 (2017).
GlaxoSmithKline. Discontinuation of TANZEUM® [letter]. GSK https://www.gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Brands/TANZEUM/824058R0_hcpLetter.pdf (2017).
Blonde, L. & Russell-Jones, D. The safety and efficacy of liraglutide with or without oral antidiabetic drug therapy in type 2 diabetes: an overview of the LEAD 1–5 studies. Diabetes Obes. Metab. 11(Suppl. 3), 26–34 (2009).
Jendle, J. et al. Efficacy and safety of dulaglutide in the treatment of type 2 diabetes: a comprehensive review of the dulaglutide clinical data focusing on the AWARD phase 3 clinical trial program. Diabetes Metab. Res. Rev. 32, 776–790 (2016).
Lau, J. et al. Discovery of the once-weekly glucagon-like peptide-1 (GLP-1) analogue semaglutide. J. Med. Chem. 58, 7370–7380 (2015).
Ahmann, A. J. et al. Efficacy and safety of once-weekly semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN 3): a 56-week, open-label, randomized clinical trial. Diabetes Care 41, 258–266 (2017).
Pratley, R. E. et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 41, 258–266 (2018).
Novo Nordisk. Novo Nordisk successfully completes the first phase 3a trial, PIONEER 1, with oral semaglutide. Novo Nordisk http://www.novonordisk.com/media/news-details.2170941.html (2018).
Davies, M. et al. Effect of oral semaglutide compared with placebo and subcutaneous semaglutide on glycemic control in patients with type 2 diabetes: a randomized clinical trial. JAMA 318, 1460–1470 (2017).
Henry, R. R. et al. Continuous subcutaneous delivery of exenatide via ITCA 650 leads to sustained glycemic control and weight loss for 48 weeks in metformin-treated subjects with type 2 diabetes. J. Diabetes Complications 28, 393–398 (2014).
Intarcia Therapeutics, Inc. Press release - intarcia announces FDA filing acceptance of new drug application (NDA) for ITCA 650 for the treatment of type 2 diabetes. Intarcia Therapeutics, Inc. http://www.intarcia.com/media/press-releases/2017-feb-3-intarcia-announces-fda-filing-acceptance.html (2017).
US National Library of Medicine. ClinicalTrials gov https://clinicaltrials.gov/ct2/show/NCT03353350 (2018).
Choi, I. et al. Superagonistic mechanism of increased glucodynamic and weight loss effects of LAPSCA-exendin-4 (efpeglenatide) [abstract]. Diabetologia 58 (Suppl. 1), 1–607 (2015).
Yoon, K.-H. et al. Dose-response improvements in glycaemic control and body weight reduction with HM11260C, a once weekly GLP-1 receptor agonist with liraglutide as reference, in type 2 diabetes.[abstract]. Diabetologia 58, 1–607 (2015).
US Food and Drug Administration. Guidance for industry diabetes mellitus — evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. FDA http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm071627.pdf) (2008).
European Medicines Agency. Guideline on clinical investigation of medicinal products in the treatment or prevention of diabetes mellitus. EMA http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2012/06/WC500129256.pdf (2012).
Nissen, S. E. & Wolski, K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N. Engl. J. Med. 356, 2457–2471 (2007).
Pfeffer, M. A. et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N. Engl. J. Med. 373, 2247–2257 (2015).
Marso, S. P. et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 375, 311–322 (2016).
Marso, S. P. et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 375, 1834–1844 (2016).
US Food and Drug Administration. Victoza - full prescribing information (reference ID: 4144309). FDA https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/022341s027lbl.pdf (2017).
European Medicines Agency. Summary of product characteristics. EMA http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/001026/WC500050017.pdf. (2017).
American Diabetes Association. 9. cardiovascular dis. risk management. Diabetes care 40, S75–S87 (2017).
Intarcia Therapeutics, Inc. Press release - Intarcia announces successful cardiovascular safety results in phase 3 FREEDOM-CVO Trial for ITCA 650, an investigational therapy for type 2 diabetes. Intarcia Therapeutics, Inc. https://www.intarcia.com/media/press-releases/2016-may-6-cardiovascular-safety.html (2016).
Holman, R. R. et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 377, 1228–1239 (2017).
US National Libary of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01394952 (2017).
US National Libary of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02465515 (2017).
Ferdinand, K. C., Botros, F. T., Atisso, C. M. & Sager, P. T. Cardiovascular safety for once-weekly dulaglutide in type 2 diabetes: a pre-specified meta-analysis of prospectively adjudicated cardiovascular events. Cardiovasc. Diabetol. 15, 38 (2016).
Fisher, M. et al. Cardiovascular safety of albiglutide in the harmony programme: a meta-analysis. Lancet Diabetes Endocrinol. 3, 697–703 (2015).
Garg, M. et al. Liraglutide acutely suppresses glucagon, lipolysis and ketogenesis in type 1 diabetes. Diabetes Obes. Metab. 19, 1306–1311 (2017).
Albèr, A., Brønden, A. & Knop, F. K. Short-acting glucagon-like peptide-1 receptor agonists as add-on to insulin therapy in type 1 diabetes: a review. Diabetes Obes. Metab. 19, 915–925 (2017).
Mathieu, C. et al. Efficacy and safety of liraglutide added to insulin treatment in type 1 diabetes: the ADJUNCT ONE treat-to-target randomized trial. Diabetes Care 39, 1702–1710 (2016).
Ahrén, B. et al. Efficacy and safety of liraglutide added to capped insulin treatment in subjects with type 1 diabetes: the ADJUNCT TWO randomized trial. Diabetes Care 39, 1693–1701 (2016).
le Roux, C. W. et al. 3 years of liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: a randomised, double-blind trial. Lancet 389, 1399–1409 (2017).
Rosenstock, J. et al. Effects of exenatide and lifestyle modification on body weight and glucose tolerance in obese subjects with and without pre-diabetes. Diabetes Care 33, 1173–1175 (2010).
Blackman, A. et al. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: the SCALE sleep apnea randomized clinical trial. Int. J. Obes. 40, 1310–1319 (2016).
Davies, M. J. et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA 314, 687–699 (2015).
Pi-Sunyer, X. et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N. Engl. J. Med. 373, 11–22 (2015).
Wadden, T. A. et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE maintenance randomized study. Int. J. Obes. 37, 1443–1451 (2013).
Madsbad, S. et al. Early weight loss responders to liraglutide 3.0 mg achieved greater weight loss and regression to normoglycaemia, and reduced development of T2D at 3 years, versus early nonresponders in the SCALE obesity and prediabetes trial [abstract]. Obes. Facts 9, 1–376 (2016).
Novo Nordisk. Novo Nordisk reports up to 13.8% weight loss in people with obesity receiving semaglutide in phase 2 trial. Novo Nordisk http://www.novonordisk.com/media/news-details.2115373.html (2017).
US National Libary of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02453711 (2018).
Carbone, L. J., Angus, P. W. & Yeomans, N. D. Incretin-based therapies for the treatment of non-alcoholic fatty liver disease: a systematic review and meta-analysis. J. Gastroenterol. Hepatol. 31, 23–31 (2016).
Armstrong, M. J. et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet 387, 679–690 (2016).
Khoo, J., Hsiang, J., Taneja, R., Law, N.-M. & Ang, T.-L. Comparative effects of liraglutide 3 mg versus structured lifestyle modification on body weight, liver fat and liver function in obese patients with non-alcoholic fatty liver disease: a pilot randomized trial. Diabetes Obes. Metab. 19, 1814–1817 (2017).
Athauda, D. et al. Exenatide once weekly versus placebo in Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet 390, 1664–1675 (2017).
US National Libary of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02953665 (2017).
Gejl, M. et al. In Alzheimer’s disease, 6-month treatment with GLP-1 analog prevents decline of brain glucose metabolism: randomized, placebo-controlled, double-blind clinical trial. Front. Aging Neurosci. 8, 108 (2016).
Elashoff, M., Matveyenko, A. V., Gier, B., Elashoff, R. & Butler, P. C. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology 141, 150–156 (2011).
Egan, A. G. et al. Pancreatic safety of incretin-based drugs — FDA and EMA assessment. N. Engl. J. Med. 370, 794–797 (2014).
Storgaard, H., Cold, F., Gluud, L. L., Vilsbøll, T. & Knop, F. K. Glucagon-like peptide-1 receptor agonists and risk of acute pancreatitis in patients with type 2 diabetes. Diabetes Obes. Metab. 19, 906–908 (2017).
Azoulay, L. et al. Incretin based drugs and the risk of pancreatic cancer: international multicentre cohort study. BMJ 352, i581 (2016).
Bjerre Knudsen, L. et al. Glucagon-like peptide-1 receptor agonists activate rodent thyroid C-cells causing calcitonin release and C-cell proliferation. Endocrinology 151, 1473–1486 (2010).
Song, Y. et al. Expression of GLP-1 receptor and CD26 in human thyroid C-cells: the association of thyroid C-cell tumorigenesis with incretin-based medicine. Oncol. Lett. 13, 2684–2690 (2017).
Faillie, J.-L. et al. Association of bile duct and gallbladder diseases with the use of incretin-based drugs in patients with type 2 diabetes mellitus. JAMA Intern. Med. 176, 1474–1481 (2016).
Keller, J. et al. Effect of exenatide on cholecystokinin-induced gallbladder emptying in fasting healthy subjects. Regul. Pept. 179, 77–83 (2012).
Lund, A., Knop, F. K. & Vilsbøll, T. Glucagon-like peptide-1 receptor agonists for the treatment of type 2 diabetes: differences and similarities. Eur. J. Intern. Med. 25, 407–414 (2014).
Dalsgaard, N. B., Brønden, A., Vilsbøll, T. & Knop, F. K. Cardiovascular safety and benefits of GLP-1 receptor agonists. Expert Opin. Drug Saf. 16, 351–363 (2017).
Zinman, B. et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 373, 2117–2128 (2015).
Neal, B. et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N. Engl. J. Med. 377, 644–657 (2017).
Sivertsen, J., Rosenmeier, J., Holst, J. J. & Vilsbøll, T. The effect of glucagon-like peptide 1 on cardiovascular risk. Nat. Rev. Cardiol. 9, 209–222 (2012).
Villanueva-Peñacarrillo, M. L., Márquez, L., González, N., Díaz-Miguel, M. & Valverde, I. Effect of GLP-1 on lipid metabolism in human adipocytes. Horm. Metab. Res. 33, 73–77 (2001).
Buteau, J. GLP-1 receptor signaling: effects on pancreatic beta-cell proliferation and survival. Diabetes Metab. 34 (Suppl. 2), 73–77 (2008).
Lee, Y.-M. et al. Analysis of absorption and excretion route of efpeglenatide using radiolabeled [125I-CA-Ex4] efpeglenatide, [125I-IgG4 Fc] efpeglenatide and [14C-PEG] efpeglenatide [poster]. American Diabetes Association http://www.hanmi.co.kr/hanmi/img/rnd/2016_ADA_(HM11260C).pdf (2016).
Sorli, C. et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): a double-blind, randomised, placebo-controlled, parallel-group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol. 5, 251–260 (2017).
Ahrén, B. et al. Efficacy and safety of once-weekly semaglutide versus once-daily sitagliptin as an add-on to metformin, thiazolidinediones, or both, in patients with type 2 diabetes (SUSTAIN 2): a 56-week, double-blind, phase 3a, randomised trial. Lancet Diabetes Endocrinol. 5, 341–354 (2017).
Pratley, R. et al. Significant effects of HM11260C (efpeglenatide) on body weight over 20 weeks in obese subjects without diabetes: a randomised, double-blind, placebo controlled study [abstract]. Diabetologia (2015).
US National Libary of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02692716 (2017).
Author information
Authors and Affiliations
Contributions
A.A. researched data for the article and wrote the first draft. A.A., A.L., F.K.K. and T.V. contributed substantially to the discussion of content and reviewed and/or edited the article before submission.
Corresponding author
Ethics declarations
Competing interests
A.A. and A.L. have no competing interests. Until 2018, T.V. served on scientific advisory panels and/or speakers’ bureaus and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer, Bristol-Myers Squibb, Eli Lilly, Merck Sharp & Dohme, Novo Nordisk and Sanofi. Thereafter, she has no competing interests. F.K.K. has served on scientific advisory panels and/or speaker's bureaus and served as a consultant to and/or received research support from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Fractyl, Gubra, Merck Sharp & Dohme, Novo Nordisk, Sanofi and Zealand Pharma.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reviewer information
Nature Reviews Endocrinology thanks M. Nauck and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Rights and permissions
About this article
Cite this article
Andersen, A., Lund, A., Knop, F.K. et al. Glucagon-like peptide 1 in health and disease. Nat Rev Endocrinol 14, 390–403 (2018). https://doi.org/10.1038/s41574-018-0016-2
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-018-0016-2
This article is cited by
-
Glucagon-Like Peptide-1 Receptor Agonist Cases Reported to United States Poison Centers, 2017–2022
Journal of Medical Toxicology (2024)
-
Effects of GLP1RAs on pregnancy rate and menstrual cyclicity in women with polycystic ovary syndrome: a meta-analysis and systematic review
BMC Endocrine Disorders (2023)
-
Efficacy and safety of tirzepatide, dual GLP-1/GIP receptor agonists, in the management of type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials
Diabetology & Metabolic Syndrome (2023)
-
Idiopathic intracranial hypertension: a step change in understanding the disease mechanisms
Nature Reviews Neurology (2023)
-
GLP-1R signaling neighborhoods associate with the susceptibility to adverse drug reactions of incretin mimetics
Nature Communications (2023)