Abstract
The ichthyoses are a large, heterogeneous group of skin cornification disorders. They can be inherited or acquired, and result in defective keratinocyte differentiation and abnormal epidermal barrier formation. The resultant skin barrier dysfunction leads to increased transepidermal water loss and inflammation. Disordered cornification is clinically characterized by skin scaling with various degrees of thickening, desquamation (peeling) and erythema (redness). Regardless of the type of ichthyosis, many patients suffer from itching, recurrent infections, sweating impairment (hypohidrosis) with heat intolerance, and diverse ocular, hearing and nutritional complications that should be monitored periodically. The characteristic clinical features are considered to be a homeostatic attempt to repair the skin barrier, but heterogeneous clinical presentation and imperfect phenotype–genotype correlation hinder diagnosis. An accurate molecular diagnosis is, however, crucial for predicting prognosis and providing appropriate genetic counselling. Most ichthyoses severely affect patient quality of life and, in severe forms, may cause considerable disability and even death. So far, treatment provides only symptomatic relief. It is lifelong, expensive, time-consuming, and often provides disappointing results. A better understanding of the molecular mechanisms that underlie these conditions is essential for designing pathogenesis-driven and patient-tailored innovative therapeutic solutions.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Oji, V. et al. Revised nomenclature and classification of inherited ichthyoses: results of the first ichthyosis consensus conference in Sorze 2009. J. Am. Acad. Dermatol. 63, 607–641 (2010). This publication delivers a general overview of the disease and the first classification of the many forms of ichthyosis, which remains the basis on which all proposed classifications are built.
Oji, V. & Traupe, H. Ichthyosis: clinical manifestations and practical treatment options. Am. J. Clin. Dermatol. 10, 351–364 (2009).
Madison, K. C. Barrier function of the skin: “La Raison d’Être” of the epidermis. J. Invest. Dermatol. 121, 231–241 (2003).
Kolarsick, P. A., Ann Kolarsick, M. & Goodwin, C. Anatomy and physiology of the skin. J. Dermatol. Nurses Assoc. 3, 203–213 (2006). This publication describes an overview of the skin structure.
Ramadon, D., McCrudden, M. T. C., Courtenay, A. J. & Donnelly, R. F. Enhancement strategies for transdermal drug delivery systems: current trends and applications. Drug Deliv. Transl Res. 12, 758 (2022).
Watt, F. M. The stem cell compartment in human interfollicular epidermis. J. Dermatol. Sci. 28, 173–180 (2002).
Fuchs, E. Epidermal differentiation and keratin gene expression. J. Cell Sci. Suppl. 17, 197–208 (1993).
Moreci, R. S. & Lechler, T. Epidermal structure and differentiation. Curr. Biol. 30, R144–R149 (2020). This paper provides an in-depth view of keratinocyte differentiation and its crucial role in epidermal formation.
Maestrini, E. et al. A molecular defect in loricrin, the major component of the cornified cell envelope, underlies Vohwinkel’s syndrome. Nat. Genet. 13, 70–77 (1996).
Nemes, Z. & Steinert, P. M. Bricks and mortar of the epidermal barrier. Exp. Mol. Med. 31, 5–19 (1999). This publication describes the bricks and mortar molecular model of the stratum corneum.
Patel, N., Spencer, L. A., English, J. C. & Zirwas, M. J. Acquired ichthyosis. J. Am. Acad. Dermatol. 55, 647–656 (2006).
Schmuth, M. et al. Inherited ichthyoses/generalized Mendelian disorders of cornification. Eur. J. Hum. Genet. 21, 123–133 (2012).
Mazereeuw-Hautier, J. et al. Management of congenital ichthyoses: European guidelines of care, part one. Br. J. Dermatol. 180, 272–281 (2019).
Mazereeuw-Hautier, J. et al. Management of congenital ichthyoses: European guidelines of care, part two. Br. J. Dermatol. 180, 484–495 (2019).
Moskowitz, D. G. et al. Pathophysiologic basis for growth failure in children with ichthyosis: an evaluation of cutaneous ultrastructure, epidermal permeability barrier function, and energy expenditure. J. Pediatr. 145, 82–92 (2004).
DiGiovanna, J. J. & Robinson-Bostom, L. Ichthyosis: etiology, diagnosis, and management. Am. J. Clin. Dermatol. 4, 81–95 (2003).
KEI. Selected government definitions of orphan or rare diseases. KEI briefing note 2020:4 table 1: country definitions of orphan or rare diseases. KEI https://www.keionline.org/wp-content/uploads/KEI-Briefing-Note-2020-4-Defining-Rare-Diseases.pdf (2020).
Brown, S. J. et al. Filaggrin haploinsufficiency is highly penetrant and is associated with increased severity of eczema: further delineation of the skin phenotype in a prospective epidemiological study of 792 school children. Br. J. Dermatol. 161, 884 (2009).
Amelina, S. S. et al. Prevalence of ichthyosis vulgaris and frequency of FLG R501X and 2282DEL4 mutations in the population of the Rostov region. Bull. Russ. State Med. Univ. 7, 51–55 (2018).
Ziprkowski, L. & Feinstein, A. A survey of ichthyosis vulgaris in Israel. Br. J. Dermatol. 86, 1–8 (1972).
Kono, M. et al. Comprehensive screening for a complete set of Japanese-population-specific filaggrin gene mutations. Allergy 69, 537–540 (2014).
Chen, H. et al. Wide spectrum of filaggrin-null mutations in atopic dermatitis highlights differences between Singaporean Chinese and European populations. Br. J. Dermatol. 165, 106–114 (2011).
Hsu, C. K. et al. Analysis of Taiwanese ichthyosis vulgaris families further demonstrates differences in FLG mutations between European and Asian populations. Br. J. Dermatol. 161, 448–451 (2009).
Akiyama, M. FLG mutations in ichthyosis vulgaris and atopic eczema: spectrum of mutations and population genetics. Br. J. Dermatol. 162, 472–477 (2010).
Wong, X. F. C. C. et al. Array-based sequencing of filaggrin gene for comprehensive detection of disease-associated variants. J. Allergy Clin. Immunol. 141, 814 (2018).
Afzal, S. et al. A novel nonsense mutation in the STS gene in a Pakistani family with X-linked recessive ichthyosis: including a very rare case of two homozygous female patients. BMC Med. Genet. 21, 20 (2020).
Craig, W. Y. et al. Prevalence of steroid sulfatase deficiency in California according to race and ethnicity. Prenat. Diagn. 30, 893–898 (2010).
Ingordo, V. et al. Frequency of X-linked ichthyosis in coastal southern Italy: a study on a representative sample of a young male population. Dermatology 207, 148–150 (2003).
Wells, R. S., Kerr, C. B. & Kerr, C. B. Clinical features of autosomal dominant and sex-linked ichthyosis in an English population. Br. Med. J. 1, 947 (1966).
de Unamuno, P., Martin‐Pascual, A. & Garcia‐Perez, A. X‐linked ichthyosis. Br. J. Dermatol. 97, 53–58 (1977).
Sakura, N., Nishimura, S. I., Matsumoto, T. & Ohsaki, M. Frequency of steroid sulfatase deficiency in Hiroshima. Pediatr. Int. 40, 63–64 (1998).
Milstone, L. M., Miller, K., Haberman, M. & Dickens, J. Incidence of moderate to severe ichthyosis in the United States. Arch. Dermatol. 148, 1080–1081 (2012).
Hernández-Martín, A. et al. Prevalence of autosomal recessive congenital ichthyosis: a population-based study using the capture-recapture method in Spain. J. Am. Acad. Dermatol. 67, 240–244 (2012).
Dreyfus, I. et al. Prevalence of inherited ichthyosis in France: a study using capture-recapture method. Orphanet J. Rare Dis. 9, 1 (2014). This paper presents an in-depth epidemiological study on the rare forms of ichthyosis.
Kurosawa, M. et al. Results of a nationwide epidemiologic survey of autosomal recessive congenital ichthyosis and ichthyosis syndromes in Japan. J. Am. Acad. Dermatol. 81, 1086–1092.e1 (2019).
Al-Zayir, A. A. & Al-Amro Al-Alakloby, O. M. Clinico-epidemiological features of primary hereditary ichthyoses in the Eastern province of Saudi Arabia. Int. J. Dermatol. 45, 257–264 (2006).
Mohamad, J. et al. Molecular epidemiology of non-syndromic autosomal recessive congenital ichthyosis in a Middle-Eastern population. Exp. Dermatol. 30, 1290–1297 (2021).
Lima Cunha, D. et al. Unknown mutations and genotype/phenotype correlations of autosomal recessive congenital ichthyosis in patients from Saudi Arabia and Pakistan. Mol. Genet. Genom. Med. 7, 539 (2019).
Hassani, B. et al. Filaggrin gene polymorphisms in Iranian ichthyosis vulgaris and atopic dermatitis patients. Int. J. Dermatol. 57, 1485–1491 (2018).
Koshy, R., Ranawat, A. & Scaria, V. al mena: a comprehensive resource of human genetic variants integrating genomes and exomes from Arab, Middle Eastern and North African populations. J. Hum. Genet. 62, 889–894 (2017).
Israeli, S. et al. Molecular analysis of a series of Israeli families with Comèl-Netherton syndrome. Dermatology 228, 183–188 (2014).
Kamalpour, L. et al. Resource utilization and quality of life associated with congenital ichthyoses. Pediatr. Dermatol. 28, 512–518 (2011).
Murase, C. et al. Cross-sectional survey on disease severity in Japanese patients with harlequin ichthyosis/ichthyosis: syndromic forms and quality-of-life analysis in a subgroup. J. Dermatol. Sci. 92, 127–133 (2018).
Hellström Pigg, M. et al. Spectrum of autosomal recessive congenital ichthyosis in scandinavia: clinical characteristics and novel and recurrent mutations in 132 patients. Acta Derm. Venereol. 96, 932–937 (2016).
Park, J. S. et al. Acquired ichthyosis, asteatotic dermatitis or xerosis? An update on pathoetiology and drug-induced associations. J. Eur. Acad. Dermatol. Venereol. https://doi.org/10.1111/JDV.18608 (2022).
Goodman, D. S. et al. Prevalence of cutaneous disease in patients with acquired immunodeficiency syndrome (AIDS) or AIDS-related complex. J. Am. Acad. Dermatol. 17, 210–220 (1987).
Pavlović, M. D. et al. The prevalence of cutaneous manifestations in young patients with type 1 diabetes. Diabetes Care 30, 1964–1967 (2007).
Okajima, R., Oliveira, A. C., Smid, J., Casseb, J. & Sanches, J. A. High prevalence of skin disorders among HTLV-1 infected individuals independent of clinical status. PLoS Negl. Trop. Dis. 7, e2546 (2013).
Moore, R. L. & Devere, T. S. Epidermal manifestations of internal malignancy. Dermatol. Clin. 26, 17–29 (2008).
Voegeli, D. Topical steroids and emollients in atopic eczema–which should be applied first? Pract. Nurs. 28, 14–20 (2017).
Vahlquist, A., Fischer, J. & Törmä, H. Inherited nonsyndromic ichthyoses: an update on pathophysiology, diagnosis and treatment. Am. J. Clin. Dermatol. 19, 51 (2018).
Chu, P. G. & Weiss, L. M. Keratin expression in human tissues and neoplasms. Histopathology 40, 403–439 (2002).
Rothnagel, J. A. et al. Mutations in the rod domains of keratins 1 and 10 in epidermolytic hyperkeratosis. Science 257, 1128–1130 (1992).
Rothnagel, J. A. et al. Mutations in the rod domain of keratin 2e in patients with ichthyosis bullosa of Siemens. Nat. Genet. 7, 485–490 (1994).
Sybert, V. P., Dale, B. A. & Holbrook, K. A. Ichthyosis vulgaris: identification of a defect in synthesis of filaggrin correlated with an absence of keratohyaline granules. J. Invest. Dermatol. 84, 191–194 (1985).
Brown, S. J. & McLean, W. H. I. One remarkable molecule: filaggrin. J. Invest. Dermatol. 132, 751–762 (2012).
Kirchmeier, P., Zimmer, A., Bouadjar, B., Rösler, B. & Fischer, J. Whole-exome-sequencing reveals small deletions in CASP14 in patients with autosomal recessive inherited ichthyosis. Acta Derm. Venereol. 97, 102–104 (2017).
Alef, T. et al. Ichthyosis, follicular atrophoderma, and hypotrichosis caused by mutations in ST14 is associated with impaired profilaggrin processing. J. Invest. Dermatol. 129, 862–869 (2009).
Boyden, L. M. et al. Mutations in ASPRV1 cause dominantly inherited ichthyosis. Am. J. Hum. Genet. 107, 158 (2020).
Dahlqvist, J. et al. A single-nucleotide deletion in the POMP 5’ UTR causes a transcriptional switch and altered epidermal proteasome distribution in KLICK genodermatosis. Am. J. Hum. Genet. 86, 596–603 (2010).
Cassidy, A. J. et al. A homozygous missense mutation in TGM5 abolishes epidermal transglutaminase 5 activity and causes acral peeling skin syndrome. Am. J. Hum. Genet. 77, 909–917 (2005).
Akiyama, M. Acylceramide is a key player in skin barrier function: insight into the molecular mechanisms of skin barrier formation and ichthyosis pathogenesis. FEBS J. 288, 2119–2130 (2021).
Pappas, A. Epidermal surface lipids. Dermatoendocrinology 1, 72 (2009).
De Laurenzi, V. et al. Sjögren–Larsson syndrome is caused by mutations in the fatty aldehyde dehydrogenase gene. Nat. Genet. 12, 52–57 (1996).
Mueller, N. et al. De novo mutation in ELOVL1 causes ichthyosis, acanthosis nigricans, hypomyelination, spastic paraplegia, high frequency deafness and optic atrophy. J. Med. Genet. 56, 164–175 (2019).
Aldahmesh, M. A. et al. Recessive mutations in ELOVL4 cause ichthyosis, intellectual disability, and spastic quadriplegia. Am. J. Hum. Genet. 89, 745–750 (2011).
Mauldin, E. A. et al. Cellular and metabolic basis for the ichthyotic phenotype in NIPAL4 (ichthyin)–deficient canines. Am. J. Pathol. 188, 1419–1429 (2018). This paper presents research into the metabolic causes of ichthyosis; its supplementary figures provide a clear overview of the ceramide pathway.
Lefèvre, C. et al. Mutations in a new cytochrome P450 gene in lamellar ichthyosis type 3. Hum. Mol. Genet. 15, 767–776 (2006).
Ohno, Y. et al. Essential role of the cytochrome P450 CYP4F22 in the production of acylceramide, the key lipid for skin permeability barrier formation. Proc. Natl Acad. Sci. USA 112, 7707–7712 (2015).
Klar, J. et al. Mutations in the fatty acid transport protein 4 gene cause the ichthyosis prematurity syndrome. Am. J. Hum. Genet. 85, 248–253 (2009).
Yamamoto, H., Hattori, M., Chamulitrat, W., Ohno, Y. & Kihara, A. Skin permeability barrier formation by the ichthyosis-causative gene FATP4 through formation of the barrier lipid ω-O-acylceramide. Proc. Natl Acad. Sci. USA 117, 2914–2922 (2020).
Jansen, G. A. et al. Refsum disease is caused by mutations in the phytanoyl-CoA hydroxylase gene. Nat. Genet. 17, 190–193 (1997).
Mihalik, S. J. et al. Identification of PAHX, a Refsum disease gene. Nat. Genet. 17, 185–189 (1997).
Van Den Brink, D. M. et al. Identification of PEX7 as the second gene involved in Refsum disease. Am. J. Hum. Genet. 72, 471–477 (2003).
Rivier, M., Castiel, I., Safonova, I., Ailhaud, G. & Michel, S. Peroxisome proliferator-activated receptor-α enhances lipid metabolism in a skin equivalent model. J. Invest. Dermatol. 114, 681–687 (2000).
Acuna-Hidalgo, R. et al. Neu-Laxova syndrome is a heterogeneous metabolic disorder caused by defects in enzymes of the L-serine biosynthesis pathway. Am. J. Hum. Genet. 95, 285–293 (2014).
Shaheen, R. et al. Neu-Laxova syndrome, an inborn error of serine metabolism, is caused by mutations in PHGDH. Am. J. Hum. Genet. 94, 898–904 (2014).
Hart, C. E. et al. Phosphoserine aminotransferase deficiency: a novel disorder of the serine biosynthesis pathway. Am. J. Hum. Genet. 80, 931 (2007).
Boyden, L. M. et al. Mutations in KDSR cause recessive progressive symmetric erythrokeratoderma. Am. J. Hum. Genet. 100, 978–984 (2017).
Rabionet, M., Gorgas, K. & Sandhoff, R. Ceramide synthesis in the epidermis. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 1841, 422–434 (2014).
Linn, S. C. et al. Regulation of de novo sphingolipid biosynthesis and the toxic consequences of its disruption. Biochem. Soc. Trans. 29, 831 (2001).
Radner, F. P. W. et al. Mutations in CERS3 cause autosomal recessive congenital ichthyosis in humans. PLoS Genet. 9, e1003536 (2013).
Lefèvre, C. et al. Mutations in ichthyin a new gene on chromosome 5q33 in a new form of autosomal recessive congenital ichthyosis. Hum. Mol. Genet. 13, 2473–2482 (2004).
Honda, Y. et al. Decreased skin barrier lipid acylceramide and differentiation-dependent gene expression in ichthyosis gene Nipal4-knockout mice. J. Invest. Dermatol. 138, 741–749 (2018).
Israeli, S. et al. A mutation in LIPN, encoding epidermal lipase N, causes a late-onset form of autosomal-recessive congenital ichthyosis. Am. J. Hum. Genet. 88, 482 (2011).
Lefèvre, C. et al. Mutations in CGI-58, the gene encoding a new protein of the esterase/lipase/thioesterase subfamily, in Chanarin-Dorfman syndrome. Am. J. Hum. Genet. 69, 1002–1012 (2001).
Grall, A. et al. PNPLA1 mutations cause autosomal recessive congenital ichthyosis in golden retriever dogs and humans. Nat. Genet. 44, 140–147 (2012).
Kien, B. et al. ABHD5 stimulates PNPLA1-mediated ω-O-acylceramide biosynthesis essential for a functional skin permeability barrier. J. Lipid Res. 59, 2360–2367 (2018).
Monies, D. et al. Identification of a novel lethal form of autosomal recessive ichthyosis caused by UDP-glucose ceramide glucosyltransferase deficiency. Clin. Genet. 93, 1252–1253 (2018).
Lefèvre, C. et al. Mutations in the transporter ABCA12 are associated with lamellar ichthyosis type 2. Hum. Mol. Genet. 12, 2369–2378 (2003).
Sidransky, E. et al. The clinical, molecular, and pathological characterisation of a family with two cases of lethal perinatal type 2 Gaucher disease. J. Med. Genet. 33, 132–136 (1996).
Hirabayashi, T., Murakami, M. & Kihara, A. The role of PNPLA1 in ω-O-acylceramide synthesis and skin barrier function. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 1864, 869–879 (2019).
Jobard, F. et al. Lipoxygenase-3 (ALOXE3) and 12(R)-lipoxygenase (ALOX12B) are mutated in non-bullous congenital ichthyosiform erythroderma (NCIE) linked to chromosome 17p13.1. Hum. Mol. Genet. 11, 107–113 (2002).
Shigehara, Y. et al. Mutations in SDR9C7 gene encoding an enzyme for vitamin A metabolism underlie autosomal recessive congenital ichthyosis. Hum. Mol. Genet. 25, 4484–4493 (2016).
Huber, M. et al. Mutations of keratinocyte transglutaminase in lamellar ichthyosis. Science 267, 525–528 (1995).
Nemes, Z., Marekov, L. N., Fésüs, L. & Steinert, P. M. A novel function for transglutaminase 1: attachment of long-chain ω-hydroxyceramides to involucrin by ester bond formation. Proc. Natl Acad. Sci. USA 96, 8402–8407 (1999).
Elias, P. M. et al. Basis for the permeability barrier abnormality in lamellar ichthyosis. Exp. Dermatol. 11, 248–256 (2002).
Kuramoto, N. et al. Development of ichthyosiform skin compensates for defective permeability barrier function in mice lacking transglutaminase 1. J. Clin. Invest. 109, 243–250 (2002).
Oeffner, F. et al. IFAP syndrome is caused by deficiency in MBTPS2, an intramembrane zinc metalloprotease essential for cholesterol homeostasis and ER stress response. Am. J. Hum. Genet. 84, 459–467 (2009).
Wang, H. et al. Mutations in SREBF1, encoding sterol regulatory element binding transcription factor 1, cause autosomal-dominant IFAP syndrome. Am. J. Hum. Genet. 107, 34–45 (2020).
Kö, A., Happle, R., Bornholdt, D., Engel, H. & Grzeschik, K.-H. Mutations in the NSDHL gene, encoding a 3-hydroxysteroid dehydrogenase, cause CHILD syndrome. J. Med. Genet. 90, 339–346 (2000).
Derry, J. M. J. et al. Mutations in a delta 8-delta 7 sterol isomerase in the tattered mouse and X-linked dominant chondrodysplasia punctata. Nat. Genet. 22, 286–290 (1999).
Heinz, L. et al. Mutations in SULT2B1 cause autosomal-recessive congenital ichthyosis in humans. Am. J. Hum. Genet. 100, 926–939 (2017).
Nemes, Z., Demény, M., Marekov, L. N., Fésüs, L. & Steinert, P. M. Cholesterol 3-sulfate interferes with cornified envelope assembly by diverting transglutaminase 1 activity from the formation of cross-links and esters to the hydrolysis of glutamine. J. Biol. Chem. 275, 2636–2646 (2000).
Mohandas, T., Shapiro, L. J., Sparkes, R. S. & Sparkes, M. C. Regional assignment of the steroid sulfatase—X-linked ichthyosis locus: implications for a noninactivated region on the short arm of human X chromosome. Proc. Natl Acad. Sci. USA 76, 5779–5783 (1979).
Dierks, T. et al. Multiple sulfatase deficiency is caused by mutations in the gene encoding the human Cα-formylglycine generating enzyme. Cell 113, 435–444 (2003).
Cosma, M. P. et al. The multiple sulfatase deficiency gene encodes an essential and limiting factor for the activity of sulfatases. Cell 113, 445–456 (2003).
Sprecher, E. et al. A mutation in SNAP29, coding for a SNARE protein involved in intracellular trafficking, causes a novel neurocutaneous syndrome characterized by cerebral dysgenesis, neuropathy, ichthyosis, and palmoplantar keratoderma. Am. J. Hum. Genet. 77, 242–251 (2005).
Cullinane, A. R. et al. Mutations in VIPAR cause an arthrogryposis, renal dysfunction and cholestasis syndrome phenotype with defects in epithelial polarization. Nat. Genet. 42, 303–312 (2010).
Gissen, P. et al. Mutations in VPS33B, encoding a regulator of SNARE-dependent membrane fusion, cause arthrogryposis–renal dysfunction–cholestasis (ARC) syndrome. Nat. Genet. 36, 400–404 (2004).
Cantagrel, V. & Lefeber, D. J. From glycosylation disorders to dolichol biosynthesis defects: a new class of metabolic diseases. J. Inherit. Metab. Dis. 34, 859 (2011). This paper presents an overview of the disorders of glycosylation, the dolichol pathway and its connection to cholesterol synthesis.
Al-Gazali, L., Hertecant, J., Algawi, K., El Teraifi, H. & Dattani, M. A new autosomal recessive syndrome of ocular colobomas, ichthyosis, brain malformations and endocrine abnormalities in an inbred Emirati family. Am. J. Med. Genet. A 146A, 813–819 (2008).
Kranz, C. et al. A defect in dolichol phosphate biosynthesis causes a new inherited disorder with death in early infancy. Am. J. Hum. Genet. 80, 433 (2007).
Schenk, B. et al. MPDU1 mutations underlie a novel human congenital disorder of glycosylation, designated type If. J. Clin. Invest. 108, 1687–1695 (2001).
Ng, B. G. et al. Mutations in the glycosylphosphatidylinositol gene PIGL cause CHIME syndrome. Am. J. Hum. Genet. 90, 685–688 (2012).
Brandner, J. M., Haftek, M. & Niessen, C. M. Adherens junctions, desmosomes and tight junctions in epidermal barrier function. Open Dermatol. J. 4, 14–20 (2010).
Baala, L. et al. Homozygosity mapping of a locus for a novel syndromic ichthyosis to chromosome 3q27-q28. J. Invest. Dermatol. 119, 70–76 (2002).
Hadj-Rabia, S. et al. Multiplex epithelium dysfunction due to CLDN10 mutation: the HELIX syndrome. Genet. Med. 20, 190–201 (2017).
Boyden, L. M. et al. Dominant de novo mutations in GJA1 cause erythrokeratodermia variabilis et progressiva, without features of oculodentodigital dysplasia. J. Invest. Dermatol. 135, 1540–1547 (2015).
Richard, G. et al. Missense mutations in GJB2 encoding connexin-26 cause the ectodermal dysplasia keratitis-ichthyosis-deafness syndrome. Am. J. Hum. Genet. 70, 1341–1348 (2002).
Richard, G. et al. Mutations in the human connexin gene GJB3 cause erythrokeratodermia variabilis. Nat. Genet. 20, 366–369 (1998).
Macari, F. et al. Mutation in the gene for connexin 30.3 in a family with erythrokeratodermia variabilis. Am. J. Hum. Genet. 67, 1296–1301 (2000).
Jan, A. Y., Amin, S., Ratajczak, P., Richard, G. & Sybert, V. P. Genetic heterogeneity of KID syndrome: identification of a Cx30 gene (GJB6) mutation in a patient with KID syndrome and congenital atrichia. J. Invest. Dermatol. 122, 1108–1113 (2004).
Samuelov, L. et al. Desmoglein 1 deficiency results in severe dermatitis, multiple allergies and metabolic wasting. Nat. Genet. 45, 1244–1248 (2013).
McAleer, M. A. et al. Severe dermatitis, multiple allergies, and metabolic wasting syndrome caused by a novel mutation in the N-terminal plakin domain of desmoplakin. J. Allergy Clin. Immunol. 136, 1268 (2015).
Oji, V. et al. Loss of corneodesmosin leads to severe skin barrier defect, pruritus, and atopy: unraveling the peeling skin disease. Am. J. Hum. Genet. 87, 274–281 (2010).
Duchatelet, S. et al. Mutations in PERP cause dominant and recessive keratoderma. J. Invest. Dermatol. 139, 380–390 (2019).
Basel-Vanagaite, L. et al. Autosomal recessive ichthyosis with hypotrichosis caused by a mutation in ST14, encoding type II transmembrane serine protease matriptase. Am. J. Hum. Genet. 80, 467 (2007).
Pigors, M. et al. Loss-of-function mutations in SERPINB8 linked to exfoliative ichthyosis with impaired mechanical stability of intercellular adhesions. Am. J. Hum. Genet. 99, 430–436 (2016).
Chavanas, S. et al. Mutations in SPINK5, encoding a serine protease inhibitor, cause Netherton syndrome. Nat. Genet. 25, 141–142 (2000).
Deraison, C. et al. LEKTI fragments specifically inhibit KLK5, KLK7, and KLK14 and control desquamation through a pH-dependent interaction. Mol. Biol. Cell 18, 3607 (2007).
Lin, Z. et al. Loss-of-function mutations in CAST cause peeling skin, leukonychia, acral punctate keratoses, cheilitis, and knuckle pads. Am. J. Hum. Genet. 96, 440–447 (2015).
Blaydon, D. C. et al. Mutations in CSTA, encoding cystatin A, underlie exfoliative ichthyosis and reveal a role for this protease inhibitor in cell-cell adhesion. Am. J. Hum. Genet. 89, 564–571 (2011).
Alfares, A. et al. Peeling skin syndrome associated with novel variant in FLG2 gene. Am. J. Med. Genet. A 173, 3201–3204 (2017).
Mohamad, J. et al. Filaggrin 2 deficiency results in abnormal cell-cell adhesion in the cornified cell layers and causes peeling skin syndrome type A. J. Invest. Dermatol. 138, 1736–1743 (2018).
Takayama, K., Danks, D. M., Salazar, E. P., Cleaver, J. E. & Weber, C. A. DNA repair characteristics and mutations in the ERCC2 DNA repair and transcription gene in a trichothiodystrophy patient. Hum. Mutat. 9, 519–525 (1997).
Weeda, G. et al. A mutation in the XPB/ERCC3 DNA repair transcription gene, associated with trichothiodystrophy. Am. J. Hum. Genet. 60, 320 (1997).
Giglia-Mari, G. et al. A new, tenth subunit of TFIIH is responsible for the DNA repair syndrome trichothiodystrophy group A. Nat. Genet. 36, 714–719 (2004).
Kuschal, C. et al. GTF2E2 mutations destabilize the general transcription factor complex TFIIE in individuals with DNA repair-proficient trichothiodystrophy. Am. J. Hum. Genet. 98, 627–642 (2016).
Corbett, M. A. et al. A novel X-linked trichothiodystrophy associated with a nonsense mutation in RNF113A. J. Med. Genet. 52, 269–274 (2015).
Haselbach, D. et al. Structure and conformational dynamics of the human spliceosomal bact complex. Cell 172, 454–464.e11 (2018).
Lear, T. et al. RING finger protein 113A regulates C-X-C chemokine receptor type 4 stability and signaling. Am. J. Physiol. Cell Physiol. 313, C584–C592 (2017).
Botta, E. et al. Protein instability associated with AARS1 and MARS1 mutations causes trichothiodystrophy. Hum. Mol. Genet. 30, 1711–1720 (2021).
Theil, A. F. et al. Bi-allelic TARS mutations are associated with brittle hair phenotype. Am. J. Hum. Genet. 105, 434–440 (2019).
Agolini, E. et al. Expansion of the clinical and molecular spectrum of an XPD-related disorder linked to biallelic mutations in ERCC2 gene. Clin. Genet. 99, 842–848 (2021).
Helman, G. et al. Expanded phenotype of AARS1-related white matter disease. Genet. Med. 23, 2352–2359 (2021).
La Fay, C. et al. Deep phenotyping of MARS1 (interstitial lung and liver disease) and LARS1 (infantile liver failure syndrome 1) recessive multisystemic disease using human phenotype ontology annotation: overlap and differences. Case report and review of literature. Eur. J. Med. Genet. 64, 104334 (2021).
Montpetit, A. et al. Disruption of AP1S1, causing a novel neurocutaneous syndrome, perturbs development of the skin and spinal cord. PLoS Genet. 4, e1000296 (2008).
Alsaif, H. S. et al. Homozygous loss-of-function mutations in AP1B1, encoding beta-1 subunit of adaptor-related protein complex 1, cause MEDNIK-like syndrome. Am. J. Hum. Genet. 105, 1016–1022 (2019).
Wang, H. et al. Gain-of-function mutations in TRPM4 activation gate cause progressive symmetric erythrokeratodermia. J. Invest. Dermatol. 139, 1089–1097 (2019).
Nakabayashi, K. et al. Identification of C7orf11 (TTDN1) gene mutations and genetic heterogeneity in nonphotosensitive trichothiodystrophy. Am. J. Hum. Genet. 76, 510 (2005).
Zhang, Y. et al. TTDN1 is a Plk1-interacting protein involved in maintenance of cell cycle integrity. Cell. Mol. Life Sci. 64, 632–640 (2007).
Schmuth, M., Gruber, R., Elias, P. M. & Williams, M. L. Ichthyosis update: towards a function-driven model of pathogenesis of the disorders of cornification and the role of corneocyte proteins in these disorders. Adv. Dermatol. 23, 231 (2007).
Albert, A., Alexander, D. & Boesze-Battaglia, K. Cholesterol in the rod outer segment: a complex role in a ‘simple’ system. Chem. Phys. Lipids 199, 94–105 (2016).
Cortes, V. A. et al. Physiological and pathological implications of cholesterol. Front. Biosci. (Landmark Ed.) 19, 416–428 (2014).
Gault, C. R., Obeid, L. M. & Hannun, Y. A. An overview of sphingolipid metabolism: from synthesis to breakdown. Adv. Exp. Med. Biol. 688, 1–23 (2010).
Delmar, M. & McKenna, W. J. The cardiac desmosome and arrhythmogenic cardiomyopathies. Circ. Res. 107, 700–714 (2010).
Boyden, L. M. et al. Dominant de novo DSP mutations cause erythrokeratodermia-cardiomyopathy syndrome. Hum. Mol. Genet. 25, 348 (2016).
Kurzen, H. et al. Compositionally different desmosomes in the various compartments of the human hair follicle. Differentiation 63, 295–304 (1998).
Martínez, A. D., Acuña, R., Figueroa, V., Maripillan, J. & Nicholson, B. Gap-junction channels dysfunction in deafness and hearing loss. Antioxid. Redox Signal. 11, 309 (2009).
Duncker, S. V. et al. Otoferlin couples to clathrin-mediated endocytosis in mature cochlear inner hair cells. J. Neurosci. 33, 9508–9519 (2013).
Sidiropoulos, P. N. M. et al. Dynamin 2 mutations in Charcot-Marie-Tooth neuropathy highlight the importance of clathrin-mediated endocytosis in myelination. Brain 135, 1395–1411 (2012).
Malik, K. et al. Ichthyosis molecular fingerprinting shows profound TH17 skewing and a unique barrier genomic signature. J. Allergy Clin. Immunol. 143, 604–618 (2019).
Paller, A. S. et al. An IL-17–dominant immune profile is shared across the major orphan forms of ichthyosis. J. Allergy Clin. Immunol. 139, 152–165 (2017).
Tham, K. C. et al. Distinct skin microbiome community structures in congenital ichthyosis. Br. J. Dermatol. 187, 557–570 (2022).
Traupe, H., Fischer, J. & Oji, V. Nonsyndromic types of ichthyoses-an update. J. Dtsch Dermatol. Ges. 12, 109–121 (2014).
Akiyama, M. ABCA12 mutations and autosomal recessive congenital ichthyosis: a review of genotype/phenotype correlations and of pathogenetic concepts. Hum. Mutat. 31, 1090–1096 (2010).
Rajpopat, S. et al. Harlequin ichthyosis: a review of clinical and molecular findings in 45 cases. Arch. Dermatol. 147, 681–686 (2011).
Shibata, A. & Akiyama, M. Epidemiology, medical genetics, diagnosis and treatment of harlequin ichthyosis in Japan. Pediatr. Int. 57, 516–522 (2015).
Elias, P. M. et al. Basis for abnormal desquamation and permeability barrier dysfunction in RXLI. J. Invest. Dermatol. 122, 314–319 (2004).
Simpson, J. K. et al. Genotype–phenotype correlation in a large English cohort of patients with autosomal recessive ichthyosis. Br. J. Dermatol. 182, 729–737 (2020).
Chiramel, M. J. et al. Genotype of autosomal recessive congenital ichthyosis from a tertiary care center in India. Pediatr. Dermatol. 39, 420–424 (2022).
Sun, Q. et al. The genomic and phenotypic landscape of ichthyosis: an analysis of 1000 kindreds. JAMA Dermatol. 158, 16–25 (2022).
Cuperus, E. et al. Proposal for a 6-step approach for differential diagnosis of neonatal erythroderma. J. Eur. Acad. Dermatol. Venereol. 36, 973–986 (2022). This publication provides a diagnostic approach to ichthyosis in newborns.
Cakmak, E. & Bagci, G. Chanarin-dorfman syndrome: a comprehensive review. Liver Int. 41, 905–914 (2021).
Zhou, Y. & Zhang, J. Arthrogryposis–renal dysfunction–cholestasis (ARC) syndrome: from molecular genetics to clinical features. Ital. J. Pediatr. 40, 77 (2014).
Metze, D., Traupe, H. & Süßmuth, K. Ichthyoses—a clinical and pathological spectrum from heterogeneous cornification disorders to inflammation. Dermatopathology 8, 107 (2021).
Ong, C. et al. LEKTI demonstrable by immunohistochemistry of the skin: a potential diagnostic skin test for Netherton syndrome. Br. J. Dermatol. 151, 1253–1257 (2004).
Smith, V. V., Anderson, G., Malone, M. & Sebire, N. J. Light microscopic examination of scalp hair samples as an aid in the diagnosis of paediatric disorders: retrospective review of more than 300 cases from a single centre. J. Clin. Pathol. 58, 1294–1298 (2005).
Rodríguez-Pazos, L., Ginarte, M., Vega, A. & Toribio, J. Autosomal recessive congenital ichthyosis. Actas Dermosifiliogr. 104, 270–284 (2017).
Liu, J. et al. Case report: prenatal diagnosis of a fetus with harlequin ichthyosis identifies novel compound heterozygous variants: a case report. Front. Genet. 11, 1756 (2021).
Jian, W. et al. Prenatal diagnose of a fetus with Harlequin ichthyosis in a Chinese family. Taiwan. J. Obstet. Gynecol. 57, 452–455 (2018).
Hongyan, L. et al. Early warning of low maternal unconjugated estriol level by prenatal screening for fetus with X-linked ichthyosis [Chinese]. Zhonghua Fu Chan Ke Za Zhi 57, 407–412 (2022).
Rathore, S., David, L. S., Beck, M. M., Bindra, M. S. & Arunachal, G. Harlequin ichthyosis: prenatal diagnosis of a rare yet severe genetic dermatosis. J. Clin. Diagn. Res. 9, QDO4–QD06 (2015).
Tang, X. et al. Maternal Xp22.31 copy-number variations detected in non-invasive prenatal screening effectively guide the prenatal diagnosis of X-linked ichthyosis. Front. Genet. 13, 934952 (2022).
Parikh, F. et al. Evolution and utility of preimplantation genetic testing for monogenic disorders in assisted reproduction - a narrative review. J. Hum. Reprod. Sci. 14, 329 (2021).
Hernández-Martin, A., Aranegui, B., Martin-Santiago, A. & Garcia-Doval, I. A systematic review of clinical trials of treatments for the congenital ichthyoses, excluding ichthyosis vulgaris. J. Am. Acad. Dermatol. 69, 544–549.e8 (2013).
Vahlquist, A., Gånemo, A. & Virtanen, M. Congenital ichthyosis: an overview of current and emerging therapies. Acta Derm. Venereol. 88, 4–14 (2008).
Wohlrab, J. Influence of keratolytics on cutaneous pharmacokinetics of glucocorticoids. J. Dtsch Dermatol. Ges. 19, 554–561 (2021).
Ramírez, M. E. et al. Acute percutaneous lactic acid poisoning in a child. Pediatr. Dermatol. 23, 282–285 (2006).
Madan, R. K. & Levitt, J. A review of toxicity from topical salicylic acid preparations. J. Am. Acad. Dermatol. 70, 788–792 (2014).
Menter, A. et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. Section 3. Guidelines of care for the management and treatment of psoriasis with topical therapies. J. Am. Acad. Dermatol. 60, 643–659 (2009).
Hanson, B. et al. Ectropion improvement with topical tazarotene in children with lamellar ichthyosis. Pediatr. Dermatol. 34, 584–589 (2017).
Ogawa, M. & Akiyama, M. Successful topical adapalene treatment for the facial lesions of an adolescent case of epidermolytic ichthyosis. J. Am. Acad. Dermatol. 71, e103–e105 (2014).
Hofmann, B., Stege, H., Ruzicka, T. & Lehmann, P. Effect of topical tazarotene in the treatment of congenital ichthyoses. Br. J. Dermatol. 141, 642–646 (1999).
Nguyen, V., Cunningham, B. B., Eichenfield, L. F., Alió, A. B. & Buka, R. L. Treatment of ichthyosiform diseases with topically applied tazarotene: risk of systemic absorption. J. Am. Acad. Dermatol. 57 (Suppl. 5), S123–S125 (2007).
Teng, J. M. C. et al. The CONTROL study: a randomized, double-blind vehicle-controlled phase 2b study of novel topical isotretinoin formulation demonstrates improvement in recessive X-linked and autosomal recessive lamellar congenital ichthyosis. J. Am. Acad. Dermatol. 87, 1455–1458 (2022).
Milstone, L. M. Scaly skin and bath pH: rediscovering baking soda. J. Am. Acad. Dermatol. 62, 885–886 (2010).
Traupe, H. & Happle, R. Alopecia ichthyotica. A characteristic feature of congenital ichthyosis. Dermatologica 167, 225–230 (1983).
Mazereeuw-Hautier, J. et al. Chronic ulceration of the scalp associated with genetically different types of congenital ichthyosis: a series of four cases. Acta Derm. Venereol. 101, 959 (2021).
Ogiso, T. et al. Transfollicular drug delivery: penetration of drugs through human scalp skin and comparison of penetration between scalp and abdominal skins in vitro. J. Drug Target. 10, 369–378 (2002).
Tada, Y. et al. Treatment patterns, healthcare resource utilization, and costs in patients with moderate-to-severe psoriasis treated with systemic therapy in Japan: a retrospective claims database study. J. Dermatol. 49, 1106–1117 (2022).
Verfaille, C. J., Vanhoutte, F. P., Blanchet-Bardon, C., Van Steensel, M. A. & Steijlen, P. M. Oral liarozole vs. acitretin in the treatment of ichthyosis: a phase II/III multicentre, double-blind, randomized, active-controlled study. Br. J. Dermatol. 156, 965–973 (2007).
Vahlquist, A. et al. Oral liarozole in the treatment of patients with moderate/severe lamellar ichthyosis: results of a randomized, double-blind, multinational, placebo-controlled phase II/III trial. Br. J. Dermatol. 170, 173–181 (2014).
Common, J. E. A. et al. Clinical and genetic heterogeneity of erythrokeratoderma variabilis. J. Invest. Dermatol. 125, 920–927 (2005).
Zaenglein, A. L. et al. Consensus recommendations for the use of retinoids in ichthyosis and other disorders of cornification in children and adolescents. Pediatr. Dermatol. 38, 164 (2021).
Katugampola, R. P. & Finlay, A. Y. Oral retinoid therapy for disorders of keratinization: single-centre retrospective 25 years’ experience on 23 patients. Br. J. Dermatol. 154, 267–276 (2006).
Stern, R. S. et al. The safety of etretinate as long-term therapy for psoriasis: results of the etretinate follow-up study. J. Am. Acad. Dermatol. 33, 44–52 (1995).
Digiovanna, J. J., Mauro, T., Milstone, L. M., Schmuth, M. & Toro, J. R. Systemic retinoids in the management of ichthyoses and related skin types. Dermatol. Ther. 26, 26–38 (2013).
Larsen, F. G. et al. Acitretin is converted to etretinate only during concomitant alcohol intake. Br. J. Dermatol. 143, 1164–1169 (2000).
Baden, H. P., Buxman, M. M., Weinstein, G. D. & Yoder, F. W. Treatment of ichthyosis with isotretinoin. J. Am. Acad. Dermatol. 6, 716–720 (1982).
Onnis, G. et al. Alitretinoin reduces erythema in inherited ichthyosis. Orphanet J. Rare Dis. 13, 1–6 (2018).
Czarnowicki, T. et al. The major orphan forms of ichthyosis are characterized by systemic T-cell activation and Th-17/Tc-17/Th-22/Tc-22 polarization in blood. J. Invest. Dermatol. 138, 2157–2167 (2018).
Paller, A. S. Profiling immune expression to consider repurposing therapeutics for the ichthyoses. J. Invest. Dermatol. 139, 535–540 (2019).
Paller, A. S. et al. The spectrum of manifestations in desmoplakin gene (DSP) spectrin repeat 6 domain mutations: immunophenotyping and response to ustekinumab. J. Am. Acad. Dermatol. 78, 498–505.e2 (2018).
Sun, Q., Wine Lee, L., Hall, E. K., Choate, K. A. & Elder, R. W. Hair and skin predict cardiomyopathies: carvajal and erythrokeratodermia cardiomyopathy syndromes. Pediatr. Dermatol. 38, 31–38 (2021).
Hernández-Martín, A. et al. Imbalance in T-helper 17 cells and targeted therapy in an infant with SAM-like syndrome. N. Engl. J. Med. 381, 2176–2178 (2019).
Godsel, L. M. et al. Translational implications of Th17-skewed inflammation due to genetic deficiency of a cadherin stress sensor. J. Clin. Invest. 132, e144363 (2022).
Yogarajah, J. et al. Efficacy and safety of secukinumab for the treatment of severe ABCA12 deficiency-related ichthyosis in a child. Skin Health Dis. 1, e25 (2021).
Lefferdink, R. et al. Secukinumab responses vary across the spectrum of congenital ichthyosis in adults. Arch. Dermatol. Res. https://doi.org/10.1007/S00403-022-02325-3 (2022).
Barbieux, C. et al. Netherton syndrome subtypes share IL-17/IL-36 signature with distinct IFN-α and allergic responses. J. Allergy Clin. Immunol. 149, 1358–1372 (2022).
Wang, J. et al. Successful treatment of Netherton syndrome with dupilumab: a case report and review of the literature. J. Dermatol. 49, 165–167 (2022).
De Palma, A. M. et al. Burden of itch in ichthyosis: a multicentre study in 94 patients. J. Eur. Acad. Dermatol. Venereol. 33, 2095–2100 (2019).
Süßmuth, K. et al. Response to dupilumab in two children with Netherton syndrome: improvement of pruritus and scaling. J. Eur. Acad. Dermatol. Venereol. 35, e152–e155 (2021).
Volc, S., Maier, L., Gritsch, A., Aichelburg, M. C. & Volc-Platzer, B. Successful treatment of Netherton syndrome with ustekinumab in a 15-year-old girl. Br. J. Dermatol. 183, 165–167 (2020).
Markó, L. et al. Keratinocyte ATP binding cassette transporter expression is regulated by ultraviolet light. J. Photochem. Photobiol. B. 116, 79–88 (2012).
Malhotra, R., Hernández-Martln, A. & Oji, V. Ocular manifestations, complications and management of congenital ichthyoses: a new look. Br. J. Ophthalmol. 102, 586–592 (2018).
Litwin, A. S. et al. Nonsurgical treatment of congenital ichthyosis cicatricial ectropion and eyelid retraction using Restylane hyaluronic acid. Br. J. Dermatol. 173, 601–603 (2015).
Zachara, M. G., Drozdowski, P. H. & Łatkowski, I. T. Surgical management of ichtyosis-related ectropion. Description of four cases and a Literature review. J. Plast. Surg. Hand Surg. 48, 179–182 (2014).
Martín-Santiago, A., Rodríguez-Pascual, M., Knöpfel, N. & Hernández-Martín, A. Otologic manifestations of autosomal recessive congenital ichthyosis in children. Actas Dermosifiliogr. 106, 733–739 (2015).
Jamal, A., Alsabea, A. & Tarakmeh, M. Effect of ear infections on hearing ability: a narrative review on the complications of otitis media. Cureus 14, e27400 (2022).
Rodríguez-Manchón, S., Pedrón-Giner, C., Cañedo-Villarroya, E., Muñoz-Codoceo, R. A. & Hernández-Martín, Á. Malnutrition in children with ichthyosis: recommendations for monitoring from a multidisciplinary clinic experience. J. Am. Acad. Dermatol. 85, 144–151 (2021).
Sethuraman, G. et al. Vitamin D: a new promising therapy for congenital ichthyosis. Pediatrics 137, e20151313 (2016).
Dreyfus, I. et al. Factors associated with impaired quality of life in adult patients suffering from ichthyosis. Acta Derm. Venereol. 94, 344–346 (2014). This publication reports statistical analysis of the factors affecting QoL in patients with ichthyosis.
Quittkat, H. L., Hartmann, A. S., Düsing, R., Buhlmann, U. & Vocks, S. Body dissatisfaction, importance of appearance, and body appreciation in men and women over the lifespan. Front. Psychiatry 10, 864 (2019).
Dreyfus, I. et al. Burden of inherited ichthyosis: a French national survey. Acta Derm. Venereol. 95, 326–328 (2015).
Mazereeuw-Hautier, J. et al. Factors influencing quality of life in patients with inherited ichthyosis: a qualitative study in adults using focus groups. Br. J. Dermatol. 166, 646–648 (2012).
Cortés, H. et al. Increased risk of depression and impairment in quality of life in patients with lamellar ichthyosis. Dermatol. Ther. 34, e14628 (2021).
Cannon Homaei, S. et al. ADHD symptoms in neurometabolic diseases: underlying mechanisms and clinical implications. Neurosci. Biobehav. Rev. 132, 838–856 (2022).
Bodemer, C. et al. Short- and medium-term efficacy of specific hydrotherapy in inherited ichthyosis. Br. J. Dermatol. 165, 1087–1094 (2011).
Young, I. D. & Hughes, H. E. Sex-linked mental retardation, short stature, obesity and hypogonadism: report of a family. J. Ment. Defic. Res. 26, 153–162 (1982).
Amano, R., Ohtsuka, Y. & Ohtahara, S. Monozygotic twin patients with congenital ichthyosis, microcephalus, spastic quadriplegia, myoclonus, and EEG abnormalities. Pediatr. Neurol. 12, 255–259 (1995).
Jagell, S. F., Holmgren, G. & Hofer, P. Congenital ichthyosis with alopecia, eclabion, ectropion and mental retardation–a new genetic syndrome. Clin. Genet. 31, 102–108 (1987).
Harper, P. S., Marks, R., Dykes, P. J. & Young, I. D. Ichthyosis, hepatosplenomegaly, and cerebellar degeneration in a sibship. J. Med. Genet. 17, 212–215 (1980).
Passwell, J. H., Goodman, R. M., Ziprkowski, M. & Cohen, B. E. Congenital ichthyosis, mental retardation, dwarfism and renal impairment: a new syndrome. Clin. Genet. 8, 59–65 (1975).
Clayton-Smith, J. & Donnai, D. A new recessive syndrome of unusual facies, digital abnormalities, and ichthyosis. J. Med. Genet. 26, 339–342 (1989).
Capra, R. et al. Two sisters with multiple sclerosis, lamellar ichthyosis, beta thalassaemia minor and a deficiency of factor VIII. J. Neurol. 240, 336–338 (1993).
Gunal, I., Taymaz, A., Karatosun, V., Toylu, A. & Degirmenci, B. Mixed sclerosing dysplasia of the bone associated with ovarian and skin problems. Clin. Orthop. Relat. Res. 436, 270–276 (2005).
Liao, H. et al. Filaggrin mutations are genetic modifying factors exacerbating X-linked ichthyosis. J. Invest. Dermatol. 127, 2795–2798 (2007).
Mohamad, J. et al. Phenotypic suppression of acral peeling skin syndrome in a patient with autosomal recessive congenital ichthyosis. Exp. Dermatol. 29, 742–748 (2020).
Ngcungcu, T. et al. Duplicated enhancer region increases expression of CTSB and segregates with keratolytic winter erythema in South African and Norwegian families. Am. J. Hum. Genet. 100, 737–750 (2017).
Bochner, R. et al. Calpain 12 function revealed through the study of an atypical case of autosomal recessive congenital ichthyosis. J. Invest. Dermatol. 137, 385–393 (2017).
Joosten, M. D. W., Clabbers, J. M. K., Jonca, N., Mazereeuw-Hautier, J. & Gostyński, A. H. New developments in the molecular treatment of ichthyosis: review of the literature. Orphanet J. Rare Dis. 17, 269 (2022).
Kallis, P., Bisbee, E., Garganta, C. & Schoch, J. J. Rapid improvement of skin lesions in CHILD syndrome with topical 5% simvastatin ointment. Pediatr. Dermatol. 39, 151–152 (2022).
Paller, A. S. et al. Pathogenesis-based therapy reverses cutaneous abnormalities in an inherited disorder of distal cholesterol metabolism. J. Invest. Dermatol. 131, 2242–2248 (2011).
Atzmony, L. et al. Topical cholesterol/lovastatin for the treatment of porokeratosis: a pathogenesis-directed therapy. J. Am. Acad. Dermatol. 82, 123–131 (2020).
Chulpanova, D. S. et al. Current strategies for the gene therapy of autosomal recessive congenital ichthyosis and other types of inherited ichthyosis. Int. J. Mol. Sci. 23, 2506 (2022). This review discusses the treatment of ichthyosis with an emphasis on novel gene therapy studies.
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04047732 (2022).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01545323 (2022).
Plank, R. et al. Transglutaminase 1 replacement therapy successfully mitigates the autosomal recessive congenital ichthyosis phenotype in full-thickness skin disease equivalents. J. Invest. Dermatol. 139, 1191–1195 (2019).
Aufenvenne, K. et al. Topical enzyme-replacement therapy restores transglutaminase 1 activity and corrects architecture of transglutaminase-1-deficient skin grafts. Am. J. Hum. Genet. 93, 620–630 (2013).
Valentin, F. et al. Development of a pathogenesis-based therapy for peeling skin syndrome type 1. Br. J. Dermatol. 184, 1123–1131 (2021).
Zani, M. B., Sant’Ana, A. M., Tognato, R. C., Chagas, J. R. & Puzer, L. Human tissue kallikreins-related peptidases are targets for the treatment of skin desquamation diseases. Front. Med. 8, 777619 (2022).
Liddle, J. et al. A potent and selective kallikrein-5 inhibitor delivers high pharmacological activity in skin from patients with netherton syndrome. J. Invest. Dermatol. 141, 2272–2279 (2021).
Crumrine, D. et al. Mutations in recessive congenital ichthyoses illuminate the origin and functions of the corneocyte lipid envelope. J. Invest. Dermatol. 139, 760–768 (2019).
Veit, J. G. S. et al. Characterization of CYP26B1-selective inhibitor, DX314, as a potential therapeutic for keratinization disorders. J. Invest. Dermatol. 141, 72–83.e6 (2021).
Kurosawa, M. et al. Epidemiology and clinical characteristics of bullous congenital ichthyosiform erythroderma (keratinolytic ichthyosis) in Japan: results from a nationwide survey. J. Am. Acad. Dermatol. 68, 278–283 (2013).
Müller, F. B. et al. A human keratin 10 knockout causes recessive epidermolytic hyperkeratosis. Hum. Mol. Genet. 15, 1133–1141 (2006).
Sybert, V. P. et al. Cyclic ichthyosis with epidermolytic hyperkeratosis: a phenotype conferred by mutations in the 2B domain of keratin K1. Am. J. Hum. Genet. 64, 732 (1999).
Joh, G. Y. et al. A novel dinucleotide mutation in keratin 10 in the annular epidermolytic ichthyosis variant of bullous congenital ichthyosiform erythroderma. J. Invest. Dermatol. 108, 357–361 (1997).
Tsubota, A. et al. Keratin 1 gene mutation detected in epidermal nevus with epidermolytic hyperkeratosis. J. Invest. Dermatol. 127, 1371–1374 (2007).
Paller, S. et al. Genetic and clinical mosaicism in a type of epidermal nevus. N. Engl. J. Med. 331, 1408–1415 (1994).
Diociaiuti, A. et al. First case of KRT2 epidermolytic nevus and novel clinical and genetic findings in 26 Italian patients with keratinopathic ichthyoses. Int. J. Mol. Sci. 21, 7707 (2020).
Sprecher, E. et al. Evidence for novel functions of the keratin tail emerging from a mutation causing ichthyosis hystrix. J. Invest. Dermatol. 116, 511–519 (2001).
Choate, K. A. et al. Frequent somatic reversion of KRT1 mutations in ichthyosis with confetti. J. Clin. Invest. 125, 1703–1707 (2015).
Choate, K. A. et al. Mitotic recombination in patients with ichthyosis causes reversion of dominant mutations in KRT10. Science 330, 94 (2010).
Lesueur, F. et al. Novel mutations in ALOX12B in patients with autosomal recessive congenital ichthyosis and evidence for genetic heterogeneity on chromosome 17p13. J. Invest. Dermatol. 127, 829–834 (2007).
Sugiura, K. & Akiyama, M. Lamellar ichthyosis caused by a previously unreported homozygous ALOXE3 mutation in East Asia. Acta Derm. Venereol. 95, 858–859 (2015).
Laiho, E. et al. Transglutaminase 1 mutations in autosomal recessive congenital ichthyosis: private and recurrent mutations in an isolated population. Am. J. Hum. Genet. 61, 529–538 (1997).
Kelsell, D. P. et al. Mutations in ABCA12 underlie the severe congenital skin disease harlequin ichthyosis. Am. J. Hum. Genet. 76, 794–803 (2005).
Harting, M. et al. Self-healing collodion membrane and mild nonbullous congenital ichthyosiform erythroderma due to 2 novel mutations in the ALOX12B gene. Arch. Dermatol. 144, 351–356 (2008).
Vahlquist, A. et al. Genotypic and clinical spectrum of self-improving collodion ichthyosis: ALOX12B, ALOXE3, and TGM1 mutations in Scandinavian patients. J. Invest. Dermatol. 130, 438–443 (2010).
Noguera-Morel, L. et al. Two cases of autosomal recessive congenital ichthyosis due to CYP4F22 mutations: expanding the genotype of self-healing collodion baby. Pediatr. Dermatol. 33, e48–e51 (2016).
Raghunath, M. et al. Self-healing collodion baby: a dynamic phenotype explained by a particular transglutaminase-1 mutation. J. Invest. Dermatol. 120, 224–228 (2003).
Mazereeuw-Hautier, J. et al. Acral self-healing collodion baby: report of a new clinical phenotype caused by a novel TGM1 mutation. Br. J. Dermatol. 161, 456–463 (2009).
Oji, V. et al. Bathing suit ichthyosis is caused by transglutaminase-1 deficiency: evidence for a temperature-sensitive phenotype. Hum. Mol. Genet. 15, 3083–3097 (2006).
Takeichi, T. et al. Biallelic mutations in KDSR disrupt ceramide synthesis and result in a spectrum of keratinization disorders associated with thrombocytopenia. J. Invest. Dermatol. 137, 2344 (2017).
Ma, W. et al. Novel microdeletion in the X chromosome leads to kallmann syndrome, ichthyosis, obesity, and strabismus. Front. Genet. 11, 596 (2020).
Milunsky, J. M., Maher, T. A. & Metzenberg, A. B. Molecular, biochemical, and phenotypic analysis of a hemizygous male with a severe atypical phenotype for X-linked dominant Conradi-Hunermann-Happle syndrome and a mutation in EBP. Am. J. Med. Genet. A 116A, 249–254 (2003).
Gruber, R. et al. Autosomal recessive keratoderma-ichthyosis-deafness (ARKID) syndrome is caused by VPS33B mutations affecting rab protein interaction and collagen modification. J. Invest. Dermatol. 137, 845–854 (2017).
Norgett, E. E. et al. Recessive mutation in desmoplakin disrupts desmoplakin–intermediate filament interactions and causes dilated cardiomyopathy, woolly hair and keratoderma. Hum. Mol. Genet. 9, 2761–2766 (2000).
Muttardi, K., Nitoiu, D., Kelsell, D. P., O’Toole, E. A. & Batta, K. Acral peeling skin syndrome associated with a novel CSTA gene mutation. Clin. Exp. Dermatol. 41, 394–398 (2016).
Titeux, M. et al. Keratitis-ichthyosis-deafness syndrome caused by GJB2 maternal mosaicism. J. Invest. Dermatol. 129, 776–779 (2009).
Boyden, L. M. et al. Recessive mutations in AP1B1 cause ichthyosis, deafness, and photophobia. Am. J. Hum. Genet. 105, 1023 (2019).
Wick, M. R. & Patterson, J. W. Cutaneous paraneoplastic syndromes. Semin. Diagn. Pathol. 36, 211–228 (2019).
López Aventín, D., Gallardo, F., Yébenes, M., Lloreta, J. & Pujol, R. M. Acquired ichthyosis associated with primary cutaneous CD30+lymphoproliferative disorders. Eur. J. Dermatol. 24, 105–106 (2014).
Badawy, E. et al. Ichthyosiform mycosis fungoides. Eur. J. Dermatol. 12, 594–596 (2002).
Ramos-e-Silva, M., Carvalho, J. C. & Carneiro, S. C. Cutaneous paraneoplasia. Clin. Dermatol. 29, 541–547 (2011).
Lee, H. W. et al. Acquired ichthyosis associated with an overlap syndrome of systemic sclerosis and systemic lupus erythematosus. J. Dermatol. 33, 52–54 (2006).
Valle, S. L. Dermatologic findings related to human immunodeficiency virus infection in high-risk individuals. J. Am. Acad. Dermatol. 17, 951–961 (1987).
Holzman, S. B. & Durso, S. C. Nutritional deficiency and acquired ichthyosis. J. Gen. Intern. Med. 32, 1161 (2017).
Menni, S., Boccardi, D. & Brusasco, A. Ichthyosis revealing coeliac disease. Eur. J. Dermatol. 10, 398–399 (2000).
Sparsa, A. et al. Acquired ichthyosis with pravastatin. J. Eur. Acad. Dermatol. Venereol. 21, 549–550 (2007).
Errichetti, E., Stinco, G., Pegolo, E. & Patrone, P. Acquired ichthyosis during acitretin therapy for psoriasis vulgaris. J. Eur. Acad. Dermatol. Venereol. 30, 181–182 (2016).
Riley, C. A., Badri, T. & Hafsi, W. Pityriasis Rotunda. StatPearls [online] https://www.ncbi.nlm.nih.gov/books/NBK459240/ (updated 12 Sep 2022).
Berkowitz, I., Hodkinson, H. J., Kew, M. C. & DiBisceglie, A. M. Pityriasis rotunda as a cutaneous marker of hepatocellular carcinoma: a comparison with its prevalence in other diseases. Br. J. Dermatol. 120, 545–549 (1989).
Author information
Authors and Affiliations
Contributions
Introduction (A.H.-M., C.G.-C. and R.G.-S.); Epidemiology (A.H.-M., C.G.-C., E.S. and R.G.-S.); Mechanisms/pathophysiology (C.G.-C., E.S., M.A. and R.G.-S.); Diagnosis/screening/prevention (A.H.-M., C.G.-C., E.S., A.S.P. and R.G.-S.); Management (A.H.-M., E.S., A.S.P., M.A. and J.M.-H.); Quality of life (A.H.-M., C.G.-C., E.S. and A.S.P.); Outlook (A.H.-M., C.G.-C. and R.G.-S.); Overview of the Primer (A.H.-M.).
Corresponding author
Ethics declarations
Competing interests
The authors declare the following competing interests: A.S.P.: investigator for AbbVie, AnaptysBio, Eli Lilly, Incyte, Janssen, Krystal Biotech, Regeneron Pharmaceuticals Inc. and UCB; consultant with honorarium for AbbVie, Acrotech, Almirall, Amgen, Amryt Pharma, Arcutis Biotherapeutics, Arena Pharmaceuticals, Azitra, BioCryst, BiomX, BMS, BridgeBio, Castle Creek Biosciences, Catawba Research, Eli Lilly, Exicure, Gilead, Incyte, Janssen, Johnson & Johnson, Kamari Pharma, LEO Pharma, Novartis, OM Pharma, Pfizer, Pierre Fabre, RAPT Therapeutics, Regeneron Pharmaceuticals, Inc., Sanofi, Seanergy and UCB; data and safety monitoring board for AbbVie, Abeona Therapeutics, Bausch Health, Galderma and Novan. J.M.-H.: investigator for Sanofi, Mayne Pharma and Timber Pharmaceuticals. A.H.-M.: investigator for Mayne Pharma and Celgene. C.G.-C., E.S., M.A. and R.G.-S. declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks I. Hausser, W. Rizzo and M. Schmuth for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
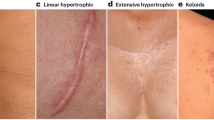
Informed consent The authors affirm that human research participants provided informed consent for publication of the images in Fig. 4.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gutiérrez-Cerrajero, C., Sprecher, E., Paller, A.S. et al. Ichthyosis. Nat Rev Dis Primers 9, 2 (2023). https://doi.org/10.1038/s41572-022-00412-3
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-022-00412-3
This article is cited by
-
Neonatale Erythrodermie
Monatsschrift Kinderheilkunde (2023)