Abstract
Myopia, also known as short-sightedness or near-sightedness, is a very common condition that typically starts in childhood. Severe forms of myopia (pathologic myopia) are associated with a risk of other associated ophthalmic problems. This disorder affects all populations and is reaching epidemic proportions in East Asia, although there are differences in prevalence between countries. Myopia is caused by both environmental and genetic risk factors. A range of myopia management and control strategies are available that can treat this condition, but it is clear that understanding the factors involved in delaying myopia onset and slowing its progression will be key to reducing the rapid rise in its global prevalence. To achieve this goal, improved data collection using wearable technology, in combination with collection and assessment of data on demographic, genetic and environmental risk factors and with artificial intelligence are needed. Improved public health strategies focusing on early detection or prevention combined with additional effective therapeutic interventions to limit myopia progression are also needed.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Modjtahedi, B. S., Ferris, F. L., Hunter, D. G. & Fong, D. S. Public health burden and potential interventions for myopia. Ophthalmology 125, 628–630 (2018).
Morgan, I. G. et al. The epidemics of myopia: aetiology and prevention. Prog. Retin. Eye Res. 62, 134–149 (2018). This study summarized the increasing trend of myopia prevalence and further discussed the implication and possible aetiology of the ‘epidemics’ of myopia.
Resnikoff, S. et al. Myopia - a 21st century public health issue. Invest. Ophthalmol. Vis. Sci. 60, Mi–Mii (2019).
Young, T. L., Metlapally, R. & Shay, A. E. Complex trait genetics of refractive error. Arch. Ophthalmol. 125, 38–48 (2007).
Hashemi, H. et al. The prevalence and risk factors for keratoconus: a systematic review and meta-analysis. Cornea 39, 263–270 (2020).
Bullimore, M. A. & Brennan, N. A. Myopia control: why each diopter matters. Optom. Vis. Sci. 96, 463–465 (2019).
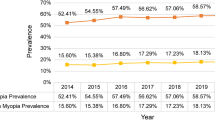
Holden, B. A. et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042 (2016). This study showed the temporal trend of myopia and high myopia prevalence supporting the notion that there will be a very high prevalence of myopia in 2050.
Mutti, D. O., Mitchell, G. L., Moeschberger, M. L., Jones, L. A. & Zadnik, K. Parental myopia, near work, school achievement, and children’s refractive error. Invest. Ophthalmol. Vis. Sci. 43, 3633–3640 (2002).
Huang, H.-M., Chang, D. S.-T. & Wu, P.-C. The association between near work activities and myopia in children-a systematic review and meta-analysis. PLoS ONE 10, e0140419 (2015).
Jin, J.-X. et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun eye care study. BMC Ophthalmol. 15, 73 (2015).
Saxena, R. et al. Prevalence of myopia and its risk factors in urban school children in Delhi: the North India myopia study (NIM study). PLoS ONE 10, e0117349 (2015).
He, M. et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA 314, 1142–1148 (2015). This study is a large RCT and confirmed that outdoor activity significantly prevented myopia onset.
Wu, P. C. et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology 125, 1239–1250 (2018). This study was the first RCT that confirmed outdoor activity significantly prevented myopia onset and myopia progression even in moderate light intensity.
Saw, S.-M., Carkeet, A. D., Chia, K.-S., Stone, R. A. & Tan, D. T. H. Component dependent risk factors for ocular parameters in Singapore Chinese children. Ophthalmology 109, 2065–2071 (2002).
He, M. et al. Refractive error and visual impairment in urban children in southern China. Invest. Ophthalmol. Vis. Sci. 45, 793–799 (2004).
Yam, J. C. et al. High prevalence of myopia in children and their parents in Hong Kong Chinese population: the Hong Kong children eye study. Acta Ophthalmol. https://doi.org/10.1111/aos.14350 (2020).
Hsu, C.-C. et al. Prevalence and risk factors for myopia in second-grade primary school children in Taipei: a population-based study. J. Chin. Med. Assoc. 79, 625–632 (2016).
Lin, L. L. K., Shih, Y. F., Hsiao, C. K. & Chen, C. J. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann. Acad. Med. Singap. 33, 27–33 (2004).
Yotsukura, E. et al. Current prevalence of myopia and association of myopia with environmental factors among schoolchildren in Japan. JAMA Ophthalmol. 137, 1233–1239 (2019).
Lim, D. H., Han, J., Chung, T., Kang, S. & Yim, H. W. Correction: the high prevalence of myopia in Korean children with influence of parental refractive errors: the 2008–2012 Korean national health and nutrition examination survey. PLoS ONE 13, e0209876 (2018).
Anera, R. G., Soler, M., de la Cruz Cardona, J., Salas, C. & Ortiz, C. Prevalence of refractive errors in school-age children in Morocco. Clin. Exp. Ophthalmol. 37, 191–196 (2009).
Casson, R. J. et al. Exceptionally low prevalence of refractive error and visual impairment in schoolchildren from Lao People’s Democratic Republic. Ophthalmology 119, 2021–2027 (2012).
Dandona, R. et al. Population-based assessment of refractive error in India: the Andhra Pradesh eye disease study. Clin. Exp. Ophthalmol. 30, 84–93 (2002).
Xiang, F. et al. Increases in the prevalence of reduced visual acuity and myopia in chinese children in Guangzhou over the past 20 years. Eye 27, 1353–1358 (2013).
Ding, B.-Y., Shih, Y.-F., Lin, L. L. K., Hsiao, C. K. & Wang, I. J. Myopia among schoolchildren in East Asia and Singapore. Surv. Ophthalmol. 62, 677–697 (2017).
Fan, D. S. et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest. Ophthalmol. Vis. Sci. 45, 1071–1075 (2004).
Zadnik, K. Myopia development in childhood. Optom. Vis. Sci. 74, 603–608 (1997).
Ip, J. M. et al. Ethnic differences in refraction and ocular biometry in a population-based sample of 11–15-year-old Australian children. Eye 22, 649–656 (2008).
Alrahili, N. H. R. et al. Prevalence of uncorrected refractive errors among children aged 3-10 years in western Saudi Arabia. Saudi Med. J. 38, 804–810 (2017).
Carter, M. J. et al. Visual acuity and refraction by age for children of three different ethnic groups in Paraguay. Arq. Bras. Oftalmol. 76, 94–97 (2013).
Gao, Z. et al. Refractive error in school children in an urban and rural setting in Cambodia. Ophthalmic Epidemiol. 19, 16–22 (2012).
Murthy, G. V. S. et al. Refractive error in children in an urban population in New Delhi. Investig. Ophthalmol. Vis. Sci. 43, 623–631 (2002).
Sapkota, Y. D., Adhikari, B. N., Pokharel, G. P., Poudyal, B. K. & Ellwein, L. B. The prevalence of visual impairment in school children of upper-middle socioeconomic status in Kathmandu. Ophthalmic Epidemiol. 15, 17–23 (2008).
Jung, S. K., Lee, J. H., Kakizaki, H. & Jee, D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Invest. Ophthalmol. Vis. Sci. 53, 5579–5583 (2012).
Lee, Y. Y., Lo, C. T., Sheu, S. J. & Lin, J. L. What factors are associated with myopia in young adults? A survey study in Taiwan military conscripts. Invest. Ophthalmol. Vis. Sci. 54, 1026–1033 (2013).
Cheng, C. Y., Hsu, W. M., Liu, J. H., Tsai, S. Y. & Chou, P. Refractive errors in an elderly chinese population in Taiwan: the Shihpai eye study. Invest. Ophthalmol. Vis. Sci. 44, 4630–4638 (2003).
Xu, L. et al. Refractive error in urban and rural adult Chinese in Beijing. Ophthalmology 112, 1676–1683 (2005).
Vitale, S., Ellwein, L., Cotch, M. F., Ferris, F. L. 3rd & Sperduto, R. Prevalence of refractive error in the United States, 1999–2004. Arch. Ophthalmol. 126, 1111–1119 (2008).
Midelfart, A., Kinge, B., Midelfart, S. & Lydersen, S. Prevalence of refractive errors in young and middle-aged adults in Norway. Acta Ophthalmol. Scand. 80, 501–505 (2002).
Bar Dayan, Y. et al. The changing prevalence of myopia in young adults: a 13-year series of population-based prevalence surveys. Invest. Ophthalmol. Vis. Sci. 46, 2760–2765 (2005).
Williams, K. M. et al. Increasing prevalence of myopia in Europe and the impact of education. Ophthalmology 122, 1489–1497 (2015).
Chen, M. et al. The increasing prevalence of myopia and high myopia among high school students in Fenghua city, eastern China: a 15-year population-based survey. BMC Ophthalmol. 18, 159 (2018).
Sun, J. et al. High prevalence of myopia and high myopia in 5060 chinese university students in Shanghai. Investig. Ophthalmol. Vis. Sci. 53, 7504–7509 (2012).
Wu, J. F. et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong children eye study. PLoS ONE 8, e82763 (2013).
Williams, K. M. et al. Prevalence of refractive error in Europe: the European eye epidemiology (E(3)) consortium. Eur. J. Epidemiol. 30, 305–315 (2015).
Jacobsen, N., Jensen, H. & Goldschmidt, E. Prevalence of myopia in Danish conscripts. Acta Ophthalmol. Scand. 85, 165–170 (2007).
French, A. N., Morgan, I. G., Burlutsky, G., Mitchell, P. & Rose, K. A. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology 120, 1482–1491 (2013).
Willis, J. R. et al. The prevalence of myopic choroidal neovascularization in the United States: analysis of the IRIS(®) data registry and NHANES. Ophthalmology 123, 1771–1782 (2016).
Asakuma, T. et al. Prevalence and risk factors for myopic retinopathy in a Japanese population: the Hisayama study. Ophthalmology 119, 1760–1765 (2012).
Chen, S. J. et al. Prevalence and associated risk factors of myopic maculopathy in elderly Chinese: the Shihpai eye study. Invest. Ophthalmol. Vis. Sci. 53, 4868–4873 (2012).
Vongphanit, J., Mitchell, P. & Wang, J. J. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology 109, 704–711 (2002).
Myrowitz, E. H. Juvenile myopia progression, risk factors and interventions. Saudi J. Ophthalmol. 26, 293–297 (2012).
Fan, D. S., Lai, C., Lau, H. H., Cheung, E. Y. & Lam, D. S. Change in vision disorders among Hong Kong preschoolers in 10 years. Clin. Exp. Ophthalmol. 39, 398–403 (2011).
Lai, Y.-H., Hsu, H.-T., Wang, H.-Z., Chang, S.-J. & Wu, W.-C. The visual status of children ages 3 to 6 years in the vision screening program in Taiwan. J. AAPOS 13, 58–62 (2009).
Choudhury, F. et al. Prevalence and characteristics of myopic degeneration in an adult Chinese American population: the Chinese American eye study. Am. J. Ophthalmol. 187, 34–42 (2018).
Iwase, A. et al. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi study. Ophthalmology 113, 1354–1362 (2006).
Naidoo, K. S. et al. Potential lost productivity resulting from the global burden of myopia: systematic review, meta-analysis, and modeling. Ophthalmology 126, 338–346 (2019).
Seet, B. et al. Myopia in Singapore: taking a public health approach. Br. J. Ophthalmol. 85, 521–526 (2001).
Wong, Y.-L. et al. Prevalence, risk factors, and impact of myopic macular degeneration on visual impairment and functioning among adults in Singapore. Investig. Ophthalmol. Vis. Sci. 59, 4603–4613 (2018).
Liu, H. H. et al. Prevalence and progression of myopic retinopathy in Chinese adults: the Beijing eye study. Ophthalmology 117, 1763–1768 (2010).
Gao, L. Q. et al. Prevalence and characteristics of myopic retinopathy in a rural Chinese adult population: the Handan eye study. Arch. Ophthalmol. 129, 1199–1204 (2011).
Ohno-Matsui, K. et al. International photographic classification and grading system for myopic maculopathy. Am. J. Ophthalmol. 159, 877–883.e7 (2015).
Bez, D. et al. Association between type of educational system and prevalence and severity of myopia among male adolescents in Israel. JAMA Ophthalmol. 137, 1–7 (2019).
Morgan, R. W., Speakman, J. S. & Grimshaw, S. E. Inuit myopia: an environmentally induced “epidemic”? Can. Med. Assoc. J. 112, 575–577 (1975).
He, M., Zheng, Y. & Xiang, F. Prevalence of myopia in urban and rural children in mainland China. Optom. Vis. Sci. 86, 40–44 (2009).
Wong, T. Y., Foster, P. J., Johnson, G. J. & Seah, S. K. Education, socioeconomic status, and ocular dimensions in Chinese adults: the Tanjong Pagar Survey. Br. J. Ophthalmol. 86, 963–968 (2002).
de Jong, P. T. V. M. Myopia: its historical contexts. Br. J. Ophthalmol. 102, 1021–1027 (2018).
Mountjoy, E. et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ 361, k2022 (2018).
Rose, K. A. et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115, 1279–1285 (2008).
Guggenheim, J. A. et al. Time outdoors and physical activity as predictors of incident myopia in childhood: a prospective cohort study. Invest. Ophthalmol. Vis. Sci. 53, 2856–2865 (2012).
Guo, Y. et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology 120, 277–283 (2013).
Jones-Jordan, L. A. et al. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest. Ophthalmol. Vis. Sci. 53, 7169–7175 (2012).
Wu, P. C. et al. Increased time outdoors is followed by reversal of the long-term trend to reduced visual acuity in Taiwan primary school students. Ophthalmology 127, 1462–1469 (2020). This was the first large, long-term real-world population study that showed that outdoor policy reduced the prevalence of reduced visual acuity.
Fulk, G. W., Cyert, L. A. & Parker, D. A. Seasonal variation in myopia progression and ocular elongation. Optom. Vis. Sci. 79, 46–51 (2002).
Ashby, R. S. & Schaeffel, F. The effect of bright light on lens compensation in chicks. Invest. Ophthalmol. Vis. Sci. 51, 5247–5253 (2010).
Feldkaemper, M. & Schaeffel, F. An updated view on the role of dopamine in myopia. Exp. Eye Res. 114, 106–119 (2013).
Guggenheim, J. A. et al. Does vitamin D mediate the protective effects of time outdoors on myopia? Findings from a prospective birth cohort. Invest. Ophthalmol. Vis. Sci. 55, 8550–8558 (2014).
Jacobsen, N., Jensen, H. & Goldschmidt, E. Does the level of physical activity in university students influence development and progression of myopia? – a 2-year prospective cohort study. Invest. Ophthalmol. Vis. Sci. 49, 1322–1327 (2008).
Torii, H. et al. Violet light exposure can be a preventive strategy against myopia progression. EBioMedicine 15, 210–219 (2017).
Moderiano, D. et al. Influence of the time of day on axial length and choroidal thickness changes to hyperopic and myopic defocus in human eyes. Exp. Eye Res. 182, 125–136 (2019).
Wang, Y. et al. Exposure to sunlight reduces the risk of myopia in rhesus monkeys. PLoS ONE 10, e0127863 (2015).
Smith, E. L. III, Kee, C.-S., Ramamirtham, R., Qiao-Grider, Y. & Hung, L.-F. Peripheral vision can influence eye growth and refractive development in infant monkeys. Investig. Ophthalmol. Vis. Sci. 46, 3965–3972 (2005). The first in a series of studies that demonstrated that, contrary to popular belief, visual signals from the fovea (that is, central retina) were not essential for the regulation of ocular growth and that signals from the peripheral retina, probably as a consequence of areal summation, can dominate refractive development.
Sorsby, A. & Fraser, G. R. Statistical note on the components of ocular refraction in twins. J. Med. Genet. 1, 47–49 (1964). The first approach to quantify the coefficient of correlation of different ocular measures in identical and non-identical twins and that suggested that a number of genes with additive effect were inherited in myopia.
Chen, C. Y. et al. Heritability and shared environment estimates for myopia and associated ocular biometric traits: the genes in myopia (GEM) family study. Hum. Genet. 121, 511–520 (2007).
Hammond, C. J., Snieder, H., Gilbert, C. E. & Spector, T. D. Genes and environment in refractive error: the twin eye study. Invest. Ophthalmol. Vis. Sci. 42, 1232–1236 (2001).
Lyhne, N., Sjolie, A. K., Kyvik, K. O. & Green, A. The importance of genes and environment for ocular refraction and its determiners: a population based study among 20–45 year old twins. Br. J. Ophthalmol. 85, 1470–1476 (2001).
Dirani, M. et al. Heritability of refractive error and ocular biometrics: the genes in myopia (GEM) twin study. Invest. Ophthalmol. Vis. Sci. 47, 4756–4761 (2006).
Baird, P. N., Schache, M. & Dirani, M. The genes in myopia (GEM) study in understanding the aetiology of refractive errors. Prog. Retin. Eye Res. 29, 520–542 (2010).
Tedja, M. S. et al. IMI - myopia genetics report. Invest. Ophthalmol. Vis. Sci. 60, M89–M105 (2019).
Verhoeven, V. J. et al. Genome-wide meta-analyses of multiancestry cohorts identify multiple new susceptibility loci for refractive error and myopia. Nat. Genet. 45, 314–318 (2013). The first large international GWAS conducted by the CREAM, based on over 37,000 individuals from 32 European and Asian studies, identified 16 new genetic loci, of which some were shared across ethnicities.
Kiefer, A. K. et al. Genome-wide analysis points to roles for extracellular matrix remodeling, the visual cycle, and neuronal development in myopia. PLoS Genet. 9, e1003299 (2013).
Wojciechowski, R. & Hysi, P. G. Focusing in on the complex genetics of myopia. PLoS Genet. 9, e1003442 (2013).
Tedja, M. S. et al. Genome-wide association meta-analysis highlights light-induced signaling as a driver for refractive error. Nat. Genet. 50, 834–848 (2018).
Hysi, P. G. et al. Meta-analysis of 542,934 subjects of European ancestry identifies new genes and mechanisms predisposing to refractive error and myopia. Nat. Genet. 52, 401–407 (2020). The largest GWAS study to date in refractive error and myopia identifying 336 novel genetic loci.
Guggenheim, J. A. et al. Assumption-free estimation of the genetic contribution to refractive error across childhood. Mol. Vis. 21, 621–632 (2015).
Ghorbani Mojarrad, N. et al. Association between polygenic risk score and risk of myopia. JAMA Ophthalmol. 138, 7–13 (2019).
Tideman, J. W. L. et al. When do myopia genes have their effect? Comparison of genetic risks between children and adults. Genet. Epidemiol. 40, 756–766 (2016). This study demonstrated that different genes can impact on myopia at different ages.
Cheng, C. Y. et al. Nine loci for ocular axial length identified through genome-wide association studies, including shared loci with refractive error. Am. J. Hum. Genet. 93, 264–277 (2013). This study identified a number of genetic loci for axial length, including some that were shared with refractive error, using a large study cohort of the CREAM.
Hysi, P. G., Wojciechowski, R., Rahi, J. S. & Hammond, C. J. Genome-wide association studies of refractive error and myopia, lessons learned, and implications for the future. Investig. Ophthalmol. Vis. Sci. 55, 3344–3351 (2014).
Fan, Q. et al. Childhood gene-environment interactions and age-dependent effects of genetic variants associated with refractive error and myopia: the CREAM consortium. Sci. Rep. 6, 25853 (2016).
Chen, C.-J., Cohen, B. H. & Diamond, E. L. Genetic and environmental effects on the development of myopia in Chinese twin children. Ophthalmic Paediatr. Genet. 6, 113–119 (1985).
Saw, S.-M., Hong, C.-Y., Chia, K.-S., Stone, R. A. & Tan, D. Nearwork and myopia in young children. Lancet 357, 390 (2001).
Dudbridge, F. & Fletcher, O. Gene-environment dependence creates spurious gene-environment interaction. Am. J. Hum. Genet. 95, 301–307 (2014). An account of the conditions under which gene–environment dependence can arise, using as an example the potential interaction between a CYP3A variant and age at menarche on the risk of breast cancer.
Fan, Q. et al. Education influences the association between genetic variants and refractive error: a meta-analysis of five Singapore studies. Hum. Mol. Genet. 23, 546–554 (2014). A pioneering study reporting interactions between variants in SHISA6, GJD2 and ZMAT4 and level of education in determining susceptibility to myopia.
Wojciechowski, R., Yee, S. S., Simpson, C. L., Bailey-Wilson, J. E. & Stambolian, D. Matrix metalloproteinases and educational attainment in refractive error: evidence of gene–environment interactions in the age-related eye disease study. Ophthalmology 120, 298–305 (2012).
Tkatchenko, A. V. et al. APLP2 regulates refractive error and myopia development in mice and humans. PLoS Genet. 11, e1005432 (2015).
Chen, Y. P. et al. Selective breeding for susceptibility to myopia reveals a gene-environment interaction. Investig. Ophthalmol. Vis. Sci. 52, 4003–4011 (2011).
Pozarickij, A. et al. Quantile regression analysis reveals widespread evidence for gene-environment or gene-gene interactions in myopia development. Commun. Biol. 2, 167 (2019). A study suggesting that 88% of known GWAS loci for refractive error exhibit evidence of variance heterogeneity, which is a characteristic feature of involvement in a G×E interaction.
Huang, Y. et al. A genome-wide association study for susceptibility to visual experience-induced myopia. Invest. Ophthalmol. Vis. Sci. 60, 559–569 (2019).
Mutti, D. O. et al. Axial growth and changes in lenticular and corneal power during emmetropization in infants. Invest. Ophthalmol. Vis. Sci. 46, 3074–3080 (2005).
Ehrlich, D. L. et al. Infant emmetropization: longitudinal changes in refraction components from nine to twenty months of age. Optom. Vis. Sci. 74, 822–843 (1997).
Inagaki, Y. The rapid change of corneal curvature in the neonatal period and infancy. Arch. Ophthalmol. 104, 1026–1027 (1986).
Gordon, R. A. & Donzis, P. B. Refractive development of the human eye. Arch. Ophthalmol. 103, 785–789 (1985).
Fledelius, H. C. & Christensen, A. C. Reappraisal of the human ocular growth curve in fetal life, infancy, and early childhood. Br. J. Ophthalmol. 80, 918–921 (1996).
Saw, S. M. et al. Incidence and progression of myopia in Singaporean school children. Invest. Ophthalmol. Vis. Sci. 46, 51–57 (2005).
Mutti, D. O. et al. Corneal and crystalline lens dimensions before and after myopia onset. Optom. Vis. Sci. 89, 251–262 (2012).
Han, X., Guo, X., Lee, P. Y., Morgan, I. G. & He, M. Six-year changes in refraction and related ocular biometric factors in an adult Chinese population. PLoS ONE 12, e0183364 (2017).
Troilo, D. et al. IMI - report on experimental models of emmetropization and myopia. Invest. Ophthalmol. Vis. Sci. 60, M31–M88 (2019). This is the most recent and most comprehensive summary to date of the results obtained from studies of laboratory animals on the role of vision in the regulation of refractive development.
Schaeffel, F., Glasser, A. & Howland, H. C. Accommodation, refractive error and eye growth in chickens. Vis. Res. 28, 639–657 (1988).
Wallman, J. & Winawer, J. Homeostasis of eye growth and the question of myopia. Neuron 43, 447–468 (2004). This is the first comprehensive review of animal research on refractive development; it provides a unique perspective on how vision regulates ocular growth and refractive development.
Schaeffel, F. & Feldkaemper, M. P. Animal models in myopia research. Clin. Exp. Optom. 98, 507–517 (2015).
Arumugam, B., Hung, L.-F., To, C.-H., Holden, B. A. & Smith, E. L. 3rd The effects of simultaneous dual focus lenses on refractive development in infant monkeys. Investig. Ophthalmol. Vis. Sci. 55, 7423–7432 (2014).
Zhu, X. Temporal integration of visual signals in lens compensation (a review). Exp. Eye Res. 114, 69–76 (2013).
Tse, D. Y. & To, C.-H. Graded competing regional myopic and hyperopic defocus produce summated emmetropization set points in chicks. Investig. Ophthalmol. Vis. Sci. 52, 8056–8062 (2011).
McBrien, N. A. & Adams, D. W. A longitudinal investigation of adult-onset and adult-progression of myopia in an occupational group. Refractive and biometric findings. Invest. Ophthalmol. Vis. Sci. 38, 321–333 (1997).
Wallman, J., Gottlieb, M. D., Rajaram, V. & Fugate-Wentzek, L. Local retinal regions control local eye growth and myopia. Science 237, 73–77 (1987). This investigation demonstrated that ocular growth and refractive development are regulated by independent, local retinal mechanisms that operate in a regionally selective fashion, one of the most interesting and critical operational properties of the mechanisms that regulate refractive development.
Tkatchenko, T. V., Troilo, D., Benavente-Perez, A. & Tkatchenko, A. V. Gene expression in response to optical defocus of opposite signs reveals bidirectional mechanism of visually guided eye growth. PLoS Biol. 16, e2006021 (2018).
Fischer, A. J., McGuire, J. J., Schaeffel, F. & Stell, W. K. Light- and focus-dependent expression of the transcription factor ZENK in the chick retina. Nat. Neurosci. 2, 706–712 (1999).
Rucker, F. J. & Wallman, J. Cone signals for spectacle-lens compensation: differential responses to short and long wavelengths. Vis. Res. 48, 1980–1991 (2008).
Foulds, W. S., Barathi, V. A. & Luu, C. D. Progressive myopia or hyperopia can be induced in chicks and reversed by manipulation of the chromaticity of ambient light. Invest. Ophthalmol. Vis. Sci. 54, 8004–8012 (2013).
Hung, L. F., Arumugam, B., She, Z., Ostrin, L. & Smith, E. L. 3rd Narrow-band, long-wavelength lighting promotes hyperopia and retards vision-induced myopia in infant rhesus monkeys. Exp. Eye Res. 176, 147–160 (2018).
Hagen, L. A. et al. The association between L:M cone ratio, cone opsin genes and myopia susceptibility. Vis. Res. 162, 20–28 (2019).
Crewther, D. P. & Crewther, S. G. Refractive compensation to optical defocus depends on the temporal profile of luminance modulation of the environment. Neuroreport 13, 1029–1032 (2002).
Aleman, A. C., Wang, M. & Schaeffel, F. Reading and myopia: contrast polarity matters. Sci. Rep. 8, 10840 (2018).
Crewther, S. G. & Crewther, D. P. Inhibition of retinal ON/OFF systems differentially affects refractive compensation to defocus. Neuroreport 14, 1233–1237 (2003).
Chakraborty, R. et al. ON pathway mutations increase susceptibility to form-deprivation myopia. Exp. Eye Res. 137, 79–83 (2015).
Chakraborty, R. et al. Comparison of refractive development and retinal dopamine in OFF pathway mutant and C57BL/6J wild-type mice. Mol. Vis. 20, 1318–1327 (2014).
Wang, M., Aleman, A. C. & Schaeffel, F. Probing the potency of artificial dynamic ON or OFF stimuli to inhibit myopia development. Invest. Ophthalmol. Vis. Sci. 60, 2599–2611 (2019).
Chen, S. et al. Bright light suppresses form-deprivation myopia development with activation of dopamine D1 receptor signaling in the ON pathway in retina. Invest. Ophthalmol. Vis. Sci. 58, 2306–2316 (2017).
Zhang, Y. & Wildsoet, C. F. RPE and choroid mechanisms underlying ocular growth and myopia. Prog. Mol. Biol. Transl. Sci. 134, 221–240 (2015).
Rymer, J. & Wildsoet, C. F. The role of the retinal pigment epithelium in eye growth regulation and myopia: a review. Vis. Neurosci. 22, 251–261 (2005). It is likely that the retinal pigment epithelium plays a critical role in the signal cascade that regulates refractive development. This review provides a comprehensive summary of what is known about the pigment epithelium and vision-dependent refractive development.
Wallman, J. et al. Moving the retina: choroidal modulation of refractive state. Vis. Res. 35, 37–50 (1995).
Mertz, J. R. & Wallman, J. Choroidal retinoic acid synthesis: a possible mediator between refractive error and compensatory eye growth. Exp. Eye Res. 70, 519–527 (2000).
Wildsoet, C. & Wallman, J. Choroidal and scleral mechanisms of compensation for spectacle lenses in chicks. Vis. Res. 35, 1175–1194 (1995). This comprehensive study conclusively demonstrated that choroidal thickness was regulated by visual feedback and that changes in choroidal thickness could have a significant effect on the eye’s refractive state.
Siegwart, J. T. Jr & Norton, T. T. Regulation of the mechanical properties of tree shrew sclera by the visual environment. Vis. Res. 39, 387–407 (1999).
Rada, J. A., Nickla, D. L. & Troilo, D. Decreased proteoglycan synthesis associated with form deprivation myopia in mature primate eyes. Invest. Ophthalmol. Vis. Sci. 41, 2050–2058 (2000).
Siegwart, J. T. Jr & Norton, T. T. Selective regulation of MMP and TIMP mRNA levels in tree shrew sclera during minus lens compensation and recovery. Invest. Ophthalmol. Vis. Sci. 46, 3484–3492 (2005).
McBrien, N. A. & Gentle, A. Role of the sclera in the development and pathological complications of myopia. Prog. Retin. Eye Res. 22, 307–338 (2003).
Rada, J. A., Shelton, S. & Norton, T. T. The sclera and myopia. Exp. Eye Res. 82, 185–200 (2006). This paper reviewed the myopia-associated scleral extracellular matrix remodelling events during myopia progression in both experimental models and humans.
Wu, H. et al. Scleral hypoxia is a target for myopia control. Proc. Natl Acad. Sci. USA 115, e7091–e7100 (2018).
Zhang, S. et al. Changes in choroidal thickness and choroidal blood perfusion in guinea pig myopia. Invest. Ophthalmol. Vis. Sci. 60, 3074–3083 (2019). Scleral hypoxia can develop as a result of a decline in blood perfusion in the choroid. This paper documented that choroidal blood perfusion was significantly decreased in three models of guinea pig myopia.
Yang, Y. S. & Koh, J. W. Choroidal blood flow change in eyes with high myopia. Korean J. Ophthalmol. 29, 309–314 (2015). This paper reported a significant decrease of choroidal blood perfusion in highly myopic human eyes.
Shih, Y. F. et al. Ocular pulse amplitude in myopia. J. Ocul. Pharmacol. 7, 83–87 (1991).
Kniestedt, C. & Stamper, R. L. Visual acuity and its measurement. Ophthalmol. Clin. North Am. 16, 155–170 (2003).
Guo, X. et al. Normative distribution of visual acuity in 3- to 6-year-old Chinese preschoolers: the Shenzhen kindergarten eye study. Invest. Ophthalmol. Vis. Sci. 56, 1985–1992 (2015).
Anstice, N. S. & Thompson, B. The measurement of visual acuity in children: an evidence-based update. Clin. Exp. Optom. 97, 3–11 (2014).
Morgan, I. G., Iribarren, R., Fotouhi, A. & Grzybowski, A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 93, 581–585 (2015).
WHO. The impact of myopia and high myopia: report of the Joint World Health Organization–Brien Holden Vision Institute Global Scientific Meeting on Myopia, University of New South Wales, Sydney, Australia, 16–18 March 2015 (World Health Organization, 2017).
Negrel, A. D., Maul, E., Pokharel, G. P., Zhao, J. & Ellwein, L. B. Refractive error study in children: sampling and measurement methods for a multi-country survey. Am. J. Ophthalmol. 129, 421–426 (2000).
Wen, G. et al. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology 120, 2109–2116 (2013).
Lee, J. H., Jee, D., Kwon, J. W. & Lee, W. K. Prevalence and risk factors for myopia in a rural Korean population. Invest. Ophthalmol. Vis. Sci. 54, 5466–5471 (2013).
Parssinen, O. The increased prevalence of myopia in Finland. Acta Ophthalmol. 90, 497–502 (2012).
Pan, C. W. et al. Variation in prevalence of myopia between generations of migrant indians living in Singapore. Am. J. Ophthalmol. 154, 376–381.e1 (2012).
Santodomingo-Rubido, J., Mallen, E. A. H., Gilmartin, B. & Wolffsohn, J. S. A new non-contact optical device for ocular biometry. Br. J. Ophthalmol. 86, 458–462 (2002).
Hussin, H. M., Spry, P. G., Majid, M. A. & Gouws, P. Reliability and validity of the partial coherence interferometry for measurement of ocular axial length in children. Eye 20, 1021–1024 (2006).
Curtin, B. J. & Karlin, D. B. Axial length measurements and fundus changes of the myopic eye. Am. J. Ophthalmol. 71, 42–53 (1971).
Miller, D. G. & Singerman, L. J. Natural history of choroidal neovascularization in high myopia. Curr. Opin. Ophthalmol. 12, 222–224 (2001).
Moriyama, M. et al. Topographic analyses of shape of eyes with pathologic myopia by high-resolution three-dimensional magnetic resonance imaging. Ophthalmology 118, 1626–1637 (2011). This study has established a novel technique — 3D MRI of the eye — to visualize the shape of the entire globe; an entire extent of posterior staphyloma becomes visible.
Guo, X. et al. Three-dimensional eye shape, myopic maculopathy, and visual acuity: the Zhongshan ophthalmic center-Brien Holden vision institute high myopia cohort study. Ophthalmology 124, 679–687 (2017).
Ohno-Matsui, K. & Jonas, J. B. Posterior staphyloma in pathologic myopia. Prog. Retin. Eye Res. 70, 99–109 (2019).
Ohno-Matsui, K. Proposed classification of posterior staphylomas based on analyses of eye shape by three-dimensional magnetic resonance imaging and wide-field fundus imaging. Ophthalmology 121, 1798–1809 (2014). Through the use of new techniques, 3D MRI and ultra-wide-field OCT, a novel classification has been established for posterior staphylomas.
Morgan, I. G., He, M. & Rose, K. A. Epidemic of pathologic myopia: what can laboratory studies and epidemiology tell us? Retina 37, 989–997 (2016).
Ohno-Matsui, K., Lai, T. Y. Y., Cheung, C. M. G. & Lai, C. C. Updates of pathologic myopia. Prog. Retin. Eye Res. 52, 156–187 (2016).
Ohno-Matsui, K. What is the fundamental nature of pathologic myopia? Retina 37, 1043–1048 (2016).
Yokoi, T. et al. Peripapillary diffuse chorioretinal atrophy in children as a sign of eventual pathologic myopia in adults. Ophthalmology 123, 1783–1787 (2016).
Ohno-Matsui, K. in Pathologic Myopia (eds Spaide, R. F., Ohno-Matsui, K., & Yannuzzi, L. A.) 187–210 (Springer, 2014).
Tong, L. et al. Screening for myopia and refractive errors using LogMAR visual acuity by optometrists and a simplified visual acuity chart by nurses. Optom. Vis. Sci. 81, 684–691 (2004).
Priya, A. et al. Vision screening by teachers in southern Indian schools: testing a new “all class teacher” model. Ophthalmic Epidemiol. 22, 60–65 (2015).
Sharma, A. et al. Strategies to improve the accuracy of vision measurement by teachers in rural Chinese secondary schoolchildren: Xichang Pediatric Refractive Error Study (X-PRES) report no. 6. Arch. Ophthalmol. 126, 1434–1440 (2008).
Pattison, B. & Plymat, K. Vision screening of school children: should it be continued? Contemp. Nurse 10, 163–171 (2001).
Ma, Y. et al. Myopia screening: combining visual acuity and noncycloplegic autorefraction. Optom. Vis. Sci. 90, 1479–1485 (2013).
Leone, J. F., Mitchell, P., Morgan, I. G., Kifley, A. & Rose, K. A. Use of visual acuity to screen for significant refractive errors in adolescents: is it reliable? Arch. Ophthalmol. 128, 894–899 (2010).
Tong, L. et al. Sensitivity and specificity of visual acuity screening for refractive errors in school children. Optom. Vis. Sci. 79, 650–657 (2002).
O’Donoghue, L., Rudnicka, A. R., McClelland, J. F., Logan, N. S. & Saunders, K. J. Visual acuity measures do not reliably detect childhood refractive error – an epidemiological study. PLoS ONE 7, e34441 (2012).
Lai, Y. H., Tseng, H. Y., Hsu, H. T., Chang, S. J. & Wang, H. Z. Uncorrected visual acuity and noncycloplegic autorefraction predict significant refractive errors in Taiwanese preschool children. Ophthalmology 120, 271–276 (2013).
Sherwin, J. C. et al. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology 119, 2141–2151 (2012).
Wu, P. C., Tsai, C. L., Wu, H. L., Yang, Y. H. & Kuo, H. K. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 120, 1080–1085 (2013).
Ngo, C. S. et al. A cluster randomised controlled trial evaluating an incentive-based outdoor physical activity programme to increase outdoor time and prevent myopia in children. Ophthalmic Physiol. Opt. 34, 362–368 (2014).
Jan, C. et al. Prevention of myopia, China. Bull. World Health Organ. 98, 435–437 (2020).
Chung, K., Mohidin, N. & O’Leary, D. J. Undercorrection of myopia enhances rather than inhibits myopia progression. Vis. Res. 42, 2555–2559 (2002). Undercorrection is widely practised in myopia management but this article showed that undercorrection worsened the progression of myopia.
Li, S. Y. et al. Effect of undercorrection on myopia progression in 12-year-old children. Graefes Arch. Clin. Exp. Ophthalmol. 253, 1363–1368 (2015).
Koomson, N. Y. et al. Relationship between reduced accommodative lag and myopia progression. Optom. Vis. Sci. 93, 683–691 (2016).
Walline, J. J., Greiner, K. L., McVey, M. E. & Jones-Jordan, L. A. Multifocal contact lens myopia control. Optom. Vis. Sci. 90, 1207–1214 (2013).
Cheng, D., Woo, G. C., Drobe, B. & Schmid, K. L. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: three-year results of a randomized clinical trial. JAMA Ophthalmol. 132, 258–264 (2014).
Cho, P. & Cheung, S. W. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest. Ophthalmol. Vis. Sci. 53, 7077–7085 (2012).
Edwards, M. H., Li, R. W.-H., Lam, C. S.-Y., Lew, J. K.-F. & Yu, B. S.-Y. The Hong Kong progressive lens myopia control study: study design and main findings. Invest. Ophthalmol. Vis. Sci. 43, 2852–2858 (2002).
Gwiazda, J. et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest. Ophthalmol. Vis. Sci. 44, 1492–1500 (2003).
Leung, J. T. & Brown, B. Progression of myopia in Hong Kong chinese schoolchildren is slowed by wearing progressive lenses. Optom. Vis. Sci. 76, 346–354 (1999).
Sankaridurg, P. et al. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom. Vis. Sci. 87, 631–641 (2010).
Anstice, N. S. & Phillips, J. R. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology 118, 1152–1161 (2011). The study demonstrated the feasibility of slowing myopia with multifocal-type soft contact lenses.
Lam, C. S. Y., Tang, W. C., Tse, D. Y.-Y., Tang, Y. Y. & To, C. H. Defocus incorporated soft contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br. J. Ophthalmol. 98, 40–45 (2014).
Walline, J. J., Jones, L. A. & Sinnott, L. T. Corneal reshaping and myopia progression. Br. J. Ophthalmol. 93, 1181–1185 (2009).
Cheng, X., Xu, J., Chehab, K., Exford, J. & Brennan, N. Soft contact lenses with positive spherical aberration for myopia control. Optom. Vis. Sci. 93, 353–366 (2016).
Sankaridurg, P. et al. Myopia control with novel central and peripheral plus contact lenses and extended depth of focus contact lenses: 2 year results from a randomised clinical trial. Ophthalmic Physiol. Opt. 39, 294–307 (2019).
Sankaridurg, P. et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest. Ophthalmol. Vis. Sci. 52, 9362–9367 (2011). The study demonstrated the feasibility of slowing myopia with multifocal-type soft contact lenses.
Chamberlain, P. et al. A 3-year randomized clinical trial of MiSight lenses for myopia control. Optom. Vis. Sci. 96, 556–567 (2019).
Lam, C. S. Y. et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br. J. Ophthalmol. 104, 363–368 (2020).
Kanda, H. et al. Effect of spectacle lenses designed to reduce relative peripheral hyperopia on myopia progression in Japanese children: a 2-year multicenter randomized controlled trial. Jpn. J. Ophthalmol. 62, 537–543 (2018).
Walline, J. J. et al. Effect of high add power, medium add power, or single-vision contact lenses on myopia progression in children: the BLINK randomized clinical trial. JAMA 324, 571–580 (2020).
Walline, J. J. et al. Contact lenses in pediatrics (CLIP) study: chair time and ocular health. Optom. Vis. Sci. 84, 896–902 (2007).
Walline, J. J. et al. A randomized trial of the effect of soft contact lenses on myopia progression in children. Invest. Ophthalmol. Vis. Sci. 49, 4702–4706 (2008).
Gifford, K. L. et al. IMI - clinical management guidelines report. Invest. Ophthalmol. Vis. Sci. 60, M184–M203 (2019).
Berntsen, D. A., Sinnott, L. T., Mutti, D. O. & Zadnik, K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest. Ophthalmol. Vis. Sci. 53, 640–649 (2012).
Stapleton, F. et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology 115, 1655–1662 (2008).
Ganesan, P. & Wildsoet, C. F. Pharmaceutical intervention for myopia control. Expert. Rev. Ophthalmol. 5, 759–787 (2010).
Pineles, S. L. et al. Atropine for the prevention of myopia progression in children: a report by the American Academy of Ophthalmology. Ophthalmology 124, 1857–1866 (2017).
Huang, J. et al. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology 123, 697–708 (2016). This meta-analysis compared 16 different interventions for myopia control and indicated that, while a range of interventions could significantly reduce myopia progression, the most effective interventions were pharmacological such as atropine and pirenzepine.
Li, S. M. et al. Atropine slows myopia progression more in Asian than white children by meta-analysis. Optom. Vis. Sci. 91, 342–350 (2014). This meta-analysis of RCT results showed that atropine could significantly slow myopia progression in children with a greater effect in Asian children than in white children.
Gong, Q. et al. Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. JAMA Ophthalmol. 135, 624–630 (2017).
Chia, A. et al. Atropine for the treatment of childhood myopia: changes after stopping atropine 0.01%, 0.1% and 0.5%. Am. J. Ophthalmol. 157, 451–457.e1 (2014).
Chia, A., Lu, Q. S. & Tan, D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology 123, 391–399 (2016).
Fang, P. C., Chung, M. Y., Yu, H. J. & Wu, P. C. Prevention of myopia onset with 0.025% atropine in premyopic children. J. Ocul. Pharmacol. Ther. 26, 341–345 (2010).
Tong, L. et al. Atropine for the treatment of childhood myopia: effect on myopia progression after cessation of atropine. Ophthalmology 116, 572–579 (2009).
Yam, J. C. et al. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology 126, 113–124 (2019). This study showed that the use of very low concentrations of atropine eye drops could reduce myopia progression along a concentration-dependent response, with 0.05% atropine being the most effective in controlling SE progression and AL elongation over a period of 1 year.
Yam, J. C. et al. Two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study: phase 2 report. Ophthalmology 127, 910–919 (2019). Results of this 2-year randomized trial indicated that the effect of 0.05% atropine was double that observed with 0.01% atropine in slowing myopia progression.
Bedrossian, R. H. The effect of atropine on myopia. Ophthalmology 86, 713–719 (1979).
Yi, S. et al. Therapeutic effect of atropine 1% in children with low myopia. J. AAPOS 19, 426–429 (2015).
Chua, W. H. et al. Atropine for the treatment of childhood myopia. Ophthalmology 113, 2285–2291 (2006).
Shih, Y. F. et al. Effects of different concentrations of atropine on controlling myopia in myopic children. J. Ocul. Pharmacol. Ther. 15, 85–90 (1999). This study suggested that low concentrations of atropine at 0.1%, 0.25% and 0.5% showed significant effects on controlling myopia, with 0.5% atropine treatment being the most effective.
Lee, C. Y., Sun, C. C., Lin, Y. F. & Lin, K. K. Effects of topical atropine on intraocular pressure and myopia progression: a prospective comparative study. BMC Ophthalmol. 16, 114 (2016).
Wu, T. E., Yang, C. C. & Chen, H. S. Does atropine use increase intraocular pressure in myopic children? Optom. Vis. Sci. 89, E161–E167 (2012).
Chia, A., Li, W., Tan, D. & Luu, C. D. Full-field electroretinogram findings in children in the atropine treatment for myopia (ATOM2) study. Doc. Ophthalmol. 126, 177–186 (2013).
Luu, C. D., Lau, A. M., Koh, A. H. & Tan, D. Multifocal electroretinogram in children on atropine treatment for myopia. Br. J. Ophthalmol. 89, 151–153 (2005).
McBrien, N. A., Stell, W. K. & Carr, B. How does atropine exert its anti-myopia effects? Ophthalmic Physiol. Opt. 33, 373–378 (2013).
Kinoshita, N. et al. Additive effects of orthokeratology and atropine 0.01% ophthalmic solution in slowing axial elongation in children with myopia: first year results. Jpn. J. Ophthalmol. 62, 544–553 (2018).
Wan, L. et al. The synergistic effects of orthokeratology and atropine in slowing the progression of myopia. J. Clin. Med. 7, 259 (2018).
Kinoshita, N. et al. Efficacy of combined orthokeratology and 0.01% atropine solution for slowing axial elongation in children with myopia: a 2-year randomised trial. Sci. Rep. 10, 12750 (2020).
Clark, T. Y. & Clark, R. A. Atropine 0.01% eyedrops significantly reduce the progression of childhood myopia. J. Ocul. Pharmacol. Ther. 31, 541–545 (2015). This study showed that atropine at 0.01% could significantly reduce the rate of myopic progression over 1 year in children with minimal side effects.
Anderle, R. & Ventruba, J. The current state of refractive surgery. Coll. Antropol. 37 (Suppl. 1), 237–241 (2013). This article provides an overall view of refractive surgery.
Wen, D. et al. Postoperative efficacy, predictability, safety, and visual quality of laser corneal refractive surgery: a network meta-analysis. Am. J. Ophthalmol. 178, 65–78 (2017).
Kamiya, K. et al. A multicenter retrospective survey of refractive surgery in 78,248 eyes. J. Refract. Surg. 33, 598–602 (2017).
Yuen, L. H. et al. A 10-year prospective audit of LASIK outcomes for myopia in 37,932 eyes at a single institution in Asia. Ophthalmology 117, 1236–1244 e1231 (2010). This study demonstrates the efficacy, safety and predictability of LASIK.
Kezirian, G. M. & Stonecipher, K. G. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J. Cataract Refract. Surg. 30, 804–811 (2004).
Rosman, M. et al. Comparison of efficacy and safety of laser in situ keratomileusis using 2 femtosecond laser platforms in contralateral eyes. J. Cataract Refract. Surg. 39, 1066–1073 (2013).
Zalentein, W. N., Tervo, T. M. & Holopainen, J. M. Seven-year follow-up of LASIK for myopia. J. Refract. Surg. 25, 312–318 (2009).
Giri, P. & Azar, D. T. Risk profiles of ectasia after keratorefractive surgery. Curr. Opin. Ophthalmol. 28, 337–342 (2017).
Wolle, M. A., Randleman, J. B. & Woodward, M. A. Complications of refractive surgery: ectasia after refractive surgery. Int. Ophthalmol. Clin. 56, 127–139 (2016).
Shortt, A. J. & Allan, B. D. Photorefractive keratectomy (PRK) versus laser-assisted in-situ keratomileusis (LASIK) for myopia. Cochrane Database Syst. Rev. 2, CD005135 (2006).
Matsumoto, J. C. & Chu, Y. S. Epi-LASIK update: overview of techniques and patient management. Int. Ophthalmol. Clin. 46, 105–115 (2006).
Sia, R. K., Coe, C. D., Edwards, J. D., Ryan, D. S. & Bower, K. S. Visual outcomes after Epi-LASIK and PRK for low and moderate myopia. J. Refract. Surg. 28, 65–71 (2012).
Kuryan, J., Cheema, A. & Chuck, R. S. Laser-assisted subepithelial keratectomy (LASEK) versus laser-assisted in-situ keratomileusis (LASIK) for correcting myopia. Cochrane Database Syst. Rev. 2, CD011080 (2017).
Naderi, M., Jadidi, K., Mosavi, S. A. & Daneshi, S. A. Transepithelial photorefractive keratectomy for low to moderate myopia in comparison with conventional photorefractive keratectomy. J. Ophthalmic Vis. Res. 11, 358–362 (2016).
Shortt, A. J., Allan, B. D. S. & Evans, J. R. Laser-assisted in-situ keratomileusis (LASIK) versus photorefractive keratectomy (PRK) for myopia. Cochrane Database Syst. Rev. 1, CD005135 (2013).
Santhiago, M. R., Netto, M. V. & Wilson, S. E. Mitomycin C: biological effects and use in refractive surgery. Cornea 31, 311–321 (2012).
Wallau, A. D. & Campos, M. Photorefractive keratectomy with mitomycin C versus LASIK in custom surgeries for myopia: a bilateral prospective randomized clinical trial. J. Refract. Surg. 24, 326–336 (2008).
Agca, A. et al. Refractive lenticule extraction (ReLEx) through a small incision (SMILE) for correction of myopia and myopic astigmatism: current perspectives. Clin. Ophthalmol. 10, 1905–1912 (2016). This article provides an overall view of SMILE.
Chan, C., Lawless, M., Sutton, G., Versace, P. & Hodge, C. Small incision lenticule extraction (SMILE) in 2015. Clin. Exp. Optom. 99, 204–212 (2016).
Cai, W. T. et al. Dry eye and corneal sensitivity after small incision lenticule extraction and femtosecond laser-assisted in situ keratomileusis: a Meta-analysis. Int. J. Ophthalmol. 10, 632–638 (2017).
Fernandez, J., Valero, A., Martinez, J., Pinero, D. P. & Rodriguez-Vallejo, M. Short-term outcomes of small-incision lenticule extraction (SMILE) for low, medium, and high myopia. Eur. J. Ophthalmol. 27, 153–159 (2017).
Kim, J. R., Kim, B. K., Mun, S. J., Chung, Y. T. & Kim, H. S. One-year outcomes of small-incision lenticule extraction (SMILE): mild to moderate myopia vs. high myopia. BMC Ophthalmol. 15, 59 (2015).
Osman, I. M., Helaly, H. A., Abdalla, M. & Shousha, M. A. Corneal biomechanical changes in eyes with small incision lenticule extraction and laser assisted in situ keratomileusis. BMC Ophthalmol. 16, 123 (2016).
Guell, J. L., Morral, M., Kook, D. & Kohnen, T. Phakic intraocular lenses part 1: historical overview, current models, selection criteria, and surgical techniques. J. Cataract Refract. Surg. 36, 1976–1993 (2010). This article provides an overall view of PIOL.
Lackner, B. et al. Long-term results of implantation of phakic posterior chamber intraocular lenses. J. Cataract Refract. Surg. 30, 2269–2276 (2004).
Perez-Cambrodi, R. J., Piñero, D. P., Ferrer-Blasco, T., Cerviño, A. & Brautaset, R. The posterior chamber phakic refractive lens (PRL): a review. Eye 27, 14–21 (2013).
Lee, J. et al. Long-term clinical results of posterior chamber phakic intraocular lens implantation to correct myopia. Clin. Exp. Ophthalmol. 44, 481–487 (2016).
Guerra, M. G. et al. Phakic intraocular lens implantation: refractive outcome and safety in patients with anterior chamber depth between 2.8 and 3.0 versus >/=3.0 mm. Ophthalmic Res. 57, 239–246 (2017).
AlSabaani, N. A. et al. Causes of phakic implantable collamer lens explantation/exchange at king khaled eye specialist hospital. Middle East Afr. J. Ophthalmol. 23, 293–295 (2016).
Fernandes, P. et al. Implantable collamer posterior chamber intraocular lenses: a review of potential complications. J. Refract. Surg. 27, 765–776 (2011).
Arne, J. L. Phakic intraocular lens implantation versus clear lens extraction in highly myopic eyes of 30- to 50-year-old patients. J. Cataract Refract. Surg. 30, 2092–2096 (2004).
Nanavaty, M. A. & Daya, S. M. Refractive lens exchange versus phakic intraocular lenses. Curr. Opin. Ophthalmol. 23, 54–61 (2012).
Basch, E. Patient-reported outcomes - harnessing patients’ voices to improve clinical care. N. Engl. J. Med. 376, 105–108 (2017).
Sensaki, S. et al. An ecologic study of trends in the prevalence of myopia in Chinese adults in Singapore born from the 1920s to 1980s. Ann. Acad. Med. Singap. 46, 229–236 (2017).
Coletta, N. J. & Watson, T. Effect of myopia on visual acuity measured with laser interference fringes. Vis. Res. 46, 636–651 (2006).
Mitchell, P., Hourihan, F., Sandbach, J. & Wang, J. J. The relationship between glaucoma and myopia: the Blue Mountains eye study. Ophthalmology 106, 2010–2015 (1999).
Polkinghorne, P. J. & Craig, J. P. Northern New Zealand rhegmatogenous retinal detachment study: epidemiology and risk factors. Clin. Exp. Ophthalmol. 32, 159–163 (2004).
Praveen, M. R., Vasavada, A. R., Jani, U. D., Trivedi, R. H. & Choudhary, P. K. Prevalence of cataract type in relation to axial length in subjects with high myopia and emmetropia in an Indian population. Am. J. Ophthalmol. 145, 176–181 (2008).
Tan, D., Tay, S. A., Loh, K. L. & Chia, A. Topical atropine in the control of myopia. Asia Pac. J. Ophthalmol. 5, 424–428 (2016).
Lamoureux, E. L. et al. The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay eye study. Invest. Ophthalmol. Vis. Sci. 50, 2614–2620 (2009).
Kandel, H. et al. Uncorrected and corrected refractive error experiences of Nepalese adults: a qualitative study. Ophthalmic Epidemiol. 25, 147–161 (2018).
Ayaki, M., Torii, H., Tsubota, K. & Negishi, K. Decreased sleep quality in high myopia children. Sci. Rep. 6, 33902 (2016).
Rose, K. et al. Quality of life in myopia. Br. J. Ophthalmol. 84, 1031–1034 (2000).
Gwiazda, J. Treatment options for myopia. Optom. Vis. Sci. 86, 624–628 (2009).
Sutton, G., Lawless, M. & Hodge, C. Laser in situ keratomileusis in 2012: a review. Clin. Exp. Optom. 97, 18–29 (2014).
Uusitalo, R. J., Aine, E., Sen, N. H. & Laatikainen, L. Implantable contact lens for high myopia. J. Cataract Refract. Surg. 28, 29–36 (2002).
Markoulli, M. & Kolanu, S. Contact lens wear and dry eyes: challenges and solutions. Clin. Optom. 9, 41–48 (2017).
Shtein, R. M. Post-LASIK dry eye. Expert Rev. Ophthalmol. 6, 575–582 (2011).
Kandel, H., Khadka, J., Goggin, M. & Pesudovs, K. Impact of refractive error on quality of life: a qualitative study. Clin. Exp. Ophthalmol. 45, 677–688 (2017).
Van Der Wees, P. J. et al. Integrating the use of patient-reported outcomes for both clinical practice and performance measurement: views of experts from 3 countries. Milbank Q. 92, 754–775 (2014).
Pesudovs, K., Garamendi, E. & Elliott, D. B. The quality of life impact of refractive correction (QIRC) questionnaire: development and validation. Optom. Vis. Sci. 81, 769–777 (2004).
Berry, S., Mangione, C. M., Lindblad, A. S. & McDonnell, P. J. Development of the national eye institute refractive error correction quality of life questionnaire: focus groups. Ophthalmology 110, 2285–2291 (2003).
Vitale, S., Schein, O. D., Meinert, C. L. & Steinberg, E. P. The refractive status and vision profile: a questionnaire to measure vision-related quality of life in persons with refractive error. Ophthalmology 107, 1529–1539 (2000).
Kandel, H., Khadka, J., Goggin, M. & Pesudovs, K. Patient-reported outcomes for assessment of quality of life in refractive error: a systematic review. Optom. Vis. Sci. 94, 1102–1119 (2017). Comprehensive overview of current myopia-specific instruments and the shortcomings of each instrument, highlighting the current gap in myopia PROM assessment.
Cella, D., Gershon, R., Lai, J. S. & Choi, S. The future of outcomes measurement: item banking, tailored short-forms, and computerized adaptive assessment. Qual. Life Res. 16 (Suppl. 1), 133–141 (2007).
Gershon, R. C. Computer adaptive testing. J. Appl. Meas. 6, 109–127 (2005).
Baumhauer, J. F. & Bozic, K. J. Value-based healthcare: patient-reported outcomes in clinical decision making. Clin. Orthop. Relat. Res. 474, 1375–1378 (2016). This is a detailed look at how PROMs are becoming increasingly important in this era of value-based and personalized health care.
Hu, Y. et al. Association of age at myopia onset with risk of high myopia in adulthood in a 12-year follow-up of a Chinese cohort. JAMA Ophthalmol. https://doi.org/10.1001/jamaophthalmol.2020.3451 (2020).
Chia, A. et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2). Ophthalmology 119, 347–354 (2012).
Hyman, L. et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch. Ophthalmol. 123, 977–987 (2005).
Zhao, J. et al. The progression of refractive error in school-age children: Shunyi district, China. Am. J. Ophthalmol. 134, 735–743 (2002).
Chen, Y. et al. Contribution of genome-wide significant single nucleotide polymorphisms in myopia prediction: findings from a 10-year cohort of Chinese twin children. Ophthalmology 126, 1607–1614 (2019).
Lin, H. et al. Prediction of myopia development among Chinese school-aged children using refraction data from electronic medical records: a retrospective, multicentre machine learning study. PLoS Med. 15, e1002674 (2018).
Chen, Y., Zhang, J., Morgan, I. G. & He, M. Identifying children at risk of high myopia using population centile curves of refraction. PLoS ONE 11, e0167642 (2016).
Chua, S. Y. et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 36, 388–394 (2016).
Zadnik, K. et al. Prediction of juvenile-onset myopia. JAMA Ophthalmol. 133, 683–689 (2015).
Tideman, J. W. L. et al. Axial length growth and the risk of developing myopia in european children. Acta Ophthalmol. 96, 301–309 (2018).
Verkicharla, P. K. et al. Development of the fitsight fitness tracker to increase time outdoors to prevent myopia. Transl. Vis. Sci. Technol. 6, 20 (2017).
Wen, L. et al. An objective comparison of light intensity and near-visual tasks between rural and urban school children in China by a wearable device Clouclip. Transl. Vis. Sci. Technol. 8, 15 (2019).
Lanca, C. & Saw, S. M. The association between digital screen time and myopia: a systematic review. Ophthalmic Physiol. Opt. 40, 216–229 (2020).
Smith, E. L. III Prentice award lecture 2010: a case for peripheral optical treatment strategies for myopia. Optometry Vis. Sci. 88, 1029–1044 (2011).
Acknowledgements
The authors thank Ian Morgan (Australian National University) for his tremendous help on preparing this manuscript. This study was supported by the Australian National Health and Medical Research Council (NHMRC) through project grant 1034329 and a Senior Research Fellowship (1138585 to P.N.B.); the National Medical Research Council (NRMC) Grant NMRC/CIRG/1446/2017 and A*STAR World Without Disease (Grant JRBMRR 151701) (S.-M.S. and C.L.); Clinician Scientist Award (Senior; NMRC/CSA-SI/0009/2016) (E.L.L.) and Transition Award (MOH-TA19may-0002) (R.M.); National Institutes of Health Grant EY-03611 and funds from the Brien Holden Vision Institute (E.L.S.); grants 81800860, 81422007 and 81371047 from the National Natural Science Foundation of China (X.Z.); Fight for Sight and Welsh Government Project Grant (Ref: 24WG201) (J.A.G.); and Fundamental Research Funds of the State Key Laboratory of Ophthalmology, the Research Accelerator Program at the University of Melbourne and the CERA Foundation in Australia (M.H.).
Author information
Authors and Affiliations
Contributions
Introduction (M.H., P.N.B. and J.A.G.); Epidemiology (S.-M.S., C.L., M.H., J.A.G. and P.N.B.); Mechanisms/Pathophysiology (M.H., P.N.B., J.A.G., E.L.S. and X.Z.); Diagnosis, screening and prevention (M.H. and K.-O.M.); Management (P.-C.W., P.S., A.C. and M.R.); Quality of life (E.L.L. and R.M.); Outlook (P.N.B., M.H. and J.A.G.); Overview of Primer (P.N.B. and M.H.).
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks C. Leung, F. Schaeffel, K. Tsubota, T. Young and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Form deprivation myopia
-
Placing a diffusing filter in front of the eye.
- Myopic defocus
-
Image formed in front of retinal plane.
- Axial length
-
The distance from the anterior surface of the cornea to the retina.
- Hyperopic
-
Ability to focus on distant objects.
- Emmetropization
-
The development of the eye towards emmetropia, wherein the focus of distant objects is on the retina when the lens is in a relaxed state.
- Accommodation
-
The ability of the eye to change its focus from near to far.
- Hyperopic defocus
-
Blur resulting from the image formed behind the retinal plane.
- Choroid
-
A highly vascularized layer between the sclera and the retina.
- Cycloplegia
-
Paralysis of the ciliary muscles of the eye.
- Fundus
-
The interior surface of the back of the eye, comprising the retina, choroid and sclera.
- Indirect ophthalmoscopy
-
Examination to provide a wide view of the back of the eye using a beam of light and a hand-held lens.
- Staphyloma
-
Protrusion of a limited area of the posterior sclera.
- Choroidal neovascularization
-
The formation of new blood vessels in the choroid of the eye.
- Orthokeratology lenses
-
Rigid, gas-permeable lenses to flatten corneal curvature during overnight wear.
- Photophobia
-
Sensitivity to light.
- Excimer or femtosecond laser
-
A laser emitting concentrated light in the ultraviolet region of the spectrum.
- Phakic intraocular lens
-
(PIOL). Silicon or plastic lenses inserted into a person’s eye to restore vision but leaves the eye’s natural lens intact.
- Corneal ectasia
-
Abnormal change in shape of the cornea.
- Haze
-
A granular scarring of the corneal stroma due to inflammation.
- Corneal lenticule tissue
-
A small piece of corneal or synthetic material with a precise shape and thickness implanted into the cornea in order to change the corneal curvature.
- Infective endophthalmitis
-
Infection of the interior of the eye.
- Ocular biometry
-
Measurement of specific features that are common to the eye.
- Rasch analysis
-
A psychometric model for analysing categorical data, typically in the form of a questionnaire.
Rights and permissions
About this article
Cite this article
Baird, P.N., Saw, SM., Lanca, C. et al. Myopia. Nat Rev Dis Primers 6, 99 (2020). https://doi.org/10.1038/s41572-020-00231-4
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-020-00231-4
This article is cited by
-
Scleral remodeling during myopia development in mice eyes: a potential role of thrombospondin-1
Molecular Medicine (2024)
-
The influence of the environment and lifestyle on myopia
Journal of Physiological Anthropology (2024)
-
Association between weight-adjusted waist index and myopia in adolescents and young adults: results from NHANES 1999–2008
BMC Ophthalmology (2024)
-
Associations between corneal curvature and other anterior segment biometrics in young myopic adults
Scientific Reports (2024)
-
Eye morphometry, body size, and flexibility parameters in myopic adolescents
Scientific Reports (2024)