Abstract
Chronic rhinosinusitis (CRS) occurs in >10% of the adult population in Europe and the USA and can be differentiated into CRS without nasal polyps and CRS with nasal polyps (CRSwNP). Both phenotypes are characterized by a high disease burden and an overlapping spectrum of symptoms, with facial pain and loss of smell being the most differentiating. Great progress has been made in the understanding of CRS pathophysiology: from the epithelium and epithelial–mesenchymal transition to innate and adaptive immunity pathways and, finally, on the role of eosinophils and Staphylococcus aureus in the persistence of disease. Although clinical manifestations and diagnostic tools (including nasal endoscopy and imaging) have undergone major changes over the past few years, management (including pharmacotherapy, surgery and biologics) has experienced enormous progress based on the growing knowledge of key mediators in severe CRSwNP. The introduction of endotyping has led to a differentiation of ‘tailored’ surgical approaches, focusing on the mucosal concept in those with severe CRSwNP and on the identification of patients eligible for extended surgery and possibly biologics in the future.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout









Similar content being viewed by others
References
Bachert, C. et al. ICON: chronic rhinosinusitis. World Allergy Organ. J. 7, 25 (2014).
Bachert, C. et al. Presence of IL-5 protein and IgE antibodies to staphylococcal enterotoxins in nasal polyps is associated with comorbid asthma. J. Allergy Clin. Immunol. 126, 962–968.e6 (2010).
Fokkens, W. J. et al. European position paper on rhinosinusitis and nasal polyps 2012. Rhinol. Suppl. 23, 1–298 (2012).
Tomassen, P. et al. Reliability of EP3OS symptom criteria and nasal endoscopy in the assessment of chronic rhinosinusitis - a GA2LEN study. Allergy 66, 556–561 (2010).
Hastan, D. et al. Chronic rhinosinusitis in Europe — an underestimated disease. A GA2LEN study. Allergy 66, 1216–1223 (2011).
Pilan, R. R. et al. Prevalence of chronic rhinosinusitis in Sao Paulo. Rhinology 50, 129–138 (2012).
Shi, J. B. et al. Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities. Allergy 70, 533–539 (2015).
Ahn, J.-C., Kim, J.-W., Lee, C. H. & Rhee, C.-S. Prevalence and risk factors of chronic rhinosinusitus, allergic rhinitis, and nasal septal deviation. JAMA Otolaryngol. Head Neck Surg. 142, 162–167 (2016).
Hirsch, A. G. et al. Nasal and sinus symptoms and chronic rhinosinusitis in a population-based sample. Allergy 72, 274–281 (2016).
Clarhed, U. K. E. et al. Chronic rhinosinusitis related to occupational exposure. J. Occup. Environ. Med. 60, 656–660 (2018).
Sundaresan, A. S. et al. Longitudinal evaluation of chronic rhinosinusitis symptoms in a population-based sample. J. Allergy Clin. Immunol. Pract. 6, 1327–1335.e3 (2018).
Johansson, L., Åkerlund, A., Melén, I., Holmberg, K. & Bende, M. Prevalence of nasal polyps in adults: the Skovde population-based study. Ann. Otol. Rhinol. Laryngol. 112, 625–629 (2003).
Johansson, L. et al. Clinical relevance of nasal polyps in individuals recruited from a general population-based study. Acta Otolaryngol. 124, 77–81 (2004).
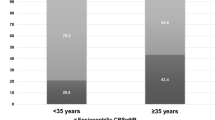
Won, H.-K. et al. Age-related prevalence of chronic rhinosinusitis and nasal polyps and their relationships with asthma onset. Ann. Allergy Asthma Immunol. 120, 389–394 (2018).
Gilani, S. & Shin, J. J. The burden and visit prevalence of pediatric chronic rhinosinusitis. Otolaryngol. Head Neck Surg. 157, 1048–1052 (2017).
Banerji, A. et al. Chronic rhinosinusitis patients with polyps or polypoid mucosa have a greater burden of illness. Am. J. Rhinol. 21, 19–26 (2007).
Khan, A. et al. The Global Allergy and Asthma European Network (GALEN rhinosinusitis cohort: a large European cross-sectional study of chronic rhinosinusitis patients with and without nasal polyps. Rhinology 57, 32–42 (2019).
Bhattacharyya, N. et al. Cost burden and resource utilization in patients with chronic rhinosinusitis and nasal polyps. Laryngoscope 129, 1969–1975 (2019).
Bachert, C., Zhang, L. & Gevaert, P. Current and future treatment options for adult chronic rhinosinusitis: Focus on nasal polyposis. J. Allergy Clin. Immunol. 136, 1431–1440 (2015).
Zhang, Y. et al. Chronic rhinosinusitis in Asia. J. Allergy Clin. Immunol. 140, 1230–1239 (2017).
Stentzel, S. et al. Staphylococcal serine protease-like proteins are pacemakers of allergic airway reactions to Staphylococcus aureus. J. Allergy Clin. Immunol. 139, 492–500.e8 (2017).
Hsu, J. et al. Genetics of chronic rhinosinusitis: state of the field and directions forward. J. Allergy Clin. Immunol. 131, 977–993 (2013).
Lee, R. J. et al. T2R38 taste receptor polymorphisms underlie susceptibility to upper respiratory infection. J. Clin. Invest. 122, 4145–4159 (2012).
Settipane, G. & Chafee, F. Nasal polyps in asthma and rhinitis. A review of 6,037 patients. J. Allergy Clin. Immunol. 59, 17–21 (1977).
Tan, B. K. et al. Incidence and associated premorbid diagnoses of patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 131, 1350–1360 (2013).
Beule, A. Epidemiology of chronic rhinosinusitis, selected risk factors, comorbidities, and economic burden. GMS Curr. Top. Otorhinolaryngol. Head Neck Surg. https://doi.org/10.3205/CTO000126 (2015).
Wolf, C. Urban air pollution and health: an ecological study of chronic rhinosinusitis in Cologne, Germany. Health Place 8, 129–139 (2002).
Thilsing, T. et al. Chronic rhinosinusitis and occupational risk factors among 20- to 75-year-old Danes-A GA2LEN-based study. Am. J. Ind. Med. 55, 1037–1043 (2012).
Gao, W.-X. et al. Occupational and environmental risk factors for chronic rhinosinusitis in China: a multicentre cross-sectional study. Respir. Res. 17, 54 (2016).
Veloso-Teles, R., Cerejeira, R., Roque-Farinha, R. & von Buchwald, C. Higher prevalence of nasal polyposis among textile workers: an endoscopic based and controlled study. Rhinology 56, 99–105 (2018).
Putman, B. et al. Risk factors for post-9/11 chronic rhinosinusitis in Fire Department of the City of New York workers. Occup. Environ. Med. 75, 884–889 (2018).
Beule, A. Epidemiologie der chronischen Rhinosinusitis, ausgewählter Risikofaktoren und Komorbiditäten, und ihre ökonomischen Folgen. Laryngorhinootologie 94 (Suppl. 1), S1–S23 (2015).
Min, J.-Y. & Tan, B. K. Risk factors for chronic rhinosinusitis. Curr. Opin. Allergy Clin. Immunol. 15, 1–13 (2015).
Tan, B. K. et al. Atopic profile of patients failing medical therapy for chronic rhinosinusitis. Int. Forum Allergy Rhinol. 1, 88–94 (2011).
Tint, D., Kubala, S. & Toskala, E. Risk factors and comorbidities in chronic rhinosinusitis. Curr. Allergy Asthma Rep. 16, 16 (2016).
Huang, H.-B. et al. Longitudinal assessment of prenatal phthalate exposure on serum and cord thyroid hormones homeostasis during pregnancy – Tainan birth cohort study (TBCS). Sci. Total. Environ. 619–620, 1058–1065 (2018).
DelGaudio, J. M., Loftus, P. A., Hamizan, A. W., Harvey, R. J. & Wise, S. K. Central compartment atopic disease. Am. J. Rhinol. Allergy 31, 228–234 (2017).
Jarvis, D. et al. Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe: asthma and chronic rhinosinusitis. Allergy 67, 91–98 (2012).
Stevens, W. W. et al. Clinical characteristics of patients with chronic rhinosinusitis with nasal polyps, asthma, and aspirin-exacerbated respiratory disease. J. Allergy Clin. Immunol. Pract. 5, 1061–1070.e3 (2017).
Avila, P. C. & Schleimer, R. P. in Allergy and Allergic Diseases 366–397 (Wiley-Blackwell, 2009).
Schleimer, R. P., Kato, A., Kern, R., Kuperman, D. & Avila, P. C. Epithelium: at the interface of innate and adaptive immune responses. J. Allergy Clin. Immunol. 120, 1279–1284 (2007). Focuses on the epithelium in the initiation and maintenance of mucosal inflammation is CRS.
Schleimer, R. P. & Berdnikovs, S. Etiology of epithelial barrier dysfunction in patients with type 2 inflammatory diseases. J. Allergy Clin. Immunol. 139, 1752–1761 (2017).
Bernstein, J., Gorfien, J., Noble, B. & Yankaskas, J. Nasal polyposis: Immunohistochemistry and bioelectrical findings (a hypothesis for the development of nasal polyps). J. Allergy Clin. Immunol. 99, 165–175 (1997).
Dejima, K., Randell, S. H., Stutts, M. J., Senior, B. A. & Boucher, R. C. Potential role of abnormal ion transport in the pathogenesis of chronic sinusitis. Arch. Otolaryngol. Head Neck Surg. 132, 1352 (2006).
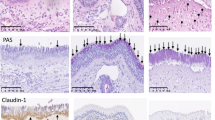
Soyka, M. B. et al. Defective epithelial barrier in chronic rhinosinusitis: the regulation of tight junctions by IFN-γ and IL-4. J. Allergy Clin. Immunol. 130, 1087–1096.e10 (2012).
Zhang, N., Van Crombruggen, K., Gevaert, E. & Bachert, C. Barrier function of the nasal mucosa in health and type-2 biased airway diseases. Allergy 71, 295–307 (2016).
Schleimer, R. P. Immunopathogenesis of chronic rhinosinusitis and nasal polyposis. Annu. Rev. Pathol. 12, 331–357 (2017).
Brożek, J. L. et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines—2016 revision. J. Allergy Clin. Immunol. 140, 950–958 (2017).
Jang, Y., Kim, H.-G., Koo, T. & Chung, P. Localization of ZO-1 and E-cadherin in the nasal polyp epithelium. Eur. Arch. Otorhinolaryngol. 259, 465–469 (2002).
Rogers, G. A. et al. Epithelial tight junction alterations in nasal polyposis. Int. Forum Allergy Rhinol. 1, 50–54 (2011).
Meng, J. et al. The development of nasal polyp disease involves early nasal mucosal inflammation and remodelling. PLoS ONE 8, e82373 (2013).
Barmeyer, C., Schulzke, J. D. & Fromm, M. Claudin-related intestinal diseases. Semin. Cell Dev. Biol. 42, 30–38 (2015).
Ordovas-Montanes, J. et al. Allergic inflammatory memory in human respiratory epithelial progenitor cells. Nature 560, 649–654 (2018).
Yang, J. & Weinberg, R. A. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev. Cell 14, 818–829 (2008).
Kalluri, R. & Weinberg, R. A. The basics of epithelial-mesenchymal transition. J. Clin. Investig. 119, 1420–1428 (2009).
Pain, M. et al. Tissue remodelling in chronic bronchial diseases: from the epithelial to mesenchymal phenotype. Eur. Respir. Rev. 23, 118–130 (2014).
Johnson, J. R., Roos, A., Berg, T., Nord, M. & Fuxe, J. Chronic respiratory aeroallergen exposure in mice induces epithelial-mesenchymal transition in the large airways. PLoS ONE 6, e16175 (2011).
Steelant, B. et al. Impaired barrier function in patients with house dust mite–induced allergic rhinitis is accompanied by decreased occludin and zonula occludens-1 expression. J. Allergy Clin. Immunol. 137, 1043–1053.e5 (2016).
Wan, H. et al. Der p 1 facilitates transepithelial allergen delivery by disruption of tight junctions. J. Clin. Investig. 104, 123–133 (1999).
Richer, S. L. et al. Epithelial genes in chronic rhinosinusitis with and without nasal polyps. Am. J. Rhinol. 22, 228–234 (2008).
Tieu, D. D., Kern, R. C. & Schleimer, R. P. Alterations in epithelial barrier function and host defense responses in chronic rhinosinusitis. J. Allergy Clin. Immunol. 124, 37–42 (2009).
Shin, H.-W. et al. Hypoxia-inducible factor 1 mediates nasal polypogenesis by inducing epithelial-to-mesenchymal transition. Am. J. Respir. Crit. Care Med. 185, 944–954 (2012).
Shaykhiev, R. & Crystal, R. G. Early events in the pathogenesis of chronic obstructive pulmonary disease. smoking-induced reprogramming of airway epithelial basal progenitor cells. Ann. Am. Thorac. Soc. 11 (Suppl. 5), 252–258 (2014).
Taniguchi, K. et al. A gp130–Src–YAP module links inflammation to epithelial regeneration. Nature 519, 57–62 (2015).
Lee, S.-N., Lee, D.-H., Sohn, M. H. & Yoon, J.-H. Overexpressed proprotein convertase 1/3 induces an epithelial-mesenchymal transition in airway epithelium. Eur. Respir. J. 42, 1379–1390 (2013).
Sidhu, S. S. et al. Roles of epithelial cell-derived periostin in TGF- activation, collagen production, and collagen gel elasticity in asthma. Proc. Natl Acad. Sci. USA 107, 14170–14175 (2010).
Gevaert, P. et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J. Allergy Clin. Immunol. 131, 110–116.e1 (2013). Omalizumab treatment reduces polyp size and symptoms in CRSwNP, although nasal polyps are not related to allergy: a proof-of concept study.
Gevaert, P. et al. Mepolizumab, a humanized anti–IL-5 mAb, as a treatment option for severe nasal polyposis. J. Allergy Clin. Immunol. 128, 989–995.e1-8 (2011).
Bachert, C. et al. Effect of subcutaneous dupilumab on nasal polyp burden in patients with chronic sinusitis and nasal polyposis. JAMA 315, 469–479 (2016).
LeMessurier, K. S., Tiwary, M., Morin, N. P. & Samarasinghe, A. E. Respiratory barrier as a safeguard and regulator of defense against influenza A virus and streptococcus pneumoniae. Front. Immunol. 11, 3 (2020).
Kountakis, S. E., Arango, P., Bradley, D., Wade, Z. K. & Borish, L. Molecular and cellular staging for the severity of chronic rhinosinusitis. Laryngoscope 114, 1895–1905 (2004).
Shi, L.-L. et al. Features of airway remodeling in different types of chinese chronic rhinosinusitis are associated with inflammation patterns. Allergy 68, 101–109 (2013).
Seshadri, S. et al. Reduced expression of antimicrobial PLUNC proteins in nasal polyp tissues of patients with chronic rhinosinusitis. Allergy 67, 920–928 (2012).
Chen, B. et al. Altered sinonasal ciliary dynamics in chronic rhinosinusitis. Am. J. Rhinol. 20, 325–329 (2006).
Cohen, N. A. Sinonasal mucociliary clearance in health and disease. Ann. Otol. Rhinol. Laryngol. 196, 20–26 (2006).
Gudis, D., Zhao, K.-Q. & Cohen, N. A. Acquired cilia dysfunction in chronic rhinosinusitis. Am. J. Rhinol. Allergy 26, 1–6 (2012).
Li, Y. Y. et al. Impairment of cilia architecture and ciliogenesis in hyperplastic nasal epithelium from nasal polyps. J. Allergy Clin. Immunol. 134, 1282–1292 (2014).
Wang, X. Mutation in the gene responsible for cystic fibrosis and predisposition to chronic rhinosinusitis in the general population. JAMA 284, 1814–1819 (2000).
Hamilos, D. L. Host-microbial interactions in patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 133, 640–653.e4 (2014).
Lane, A. P., Truong-Tran, Q.-A., Myers, A., Bickel, C. & Schleimer, R. P. Serum Amyloid A, properdin, complement 3, and toll-like receptors are expressed locally in human sinonasal tissue. Am. J. Rhinol. 20, 117–123 (2006).
Lee, R. J. & Cohen, N. A. Role of the bitter taste receptor T2R38 in upper respiratory infection and chronic rhinosinusitis. Curr. Opin. Allergy Clin. Immunol. 15, 14–20 (2015).
Ghafouri, B., Kihlström, E., Ståhlbom, B., Tagesson, C. & Lindahl, M. PLUNC (palate, lung and nasal epithelial clone) proteins in human nasal lavage fluid. Biochem. Soc. Trans. 31, 810–814 (2003).
Tieu, D. D. et al. Evidence for diminished levels of epithelial psoriasin and calprotectin in chronic rhinosinusitis. J. Allergy Clin. Immunol. 125, 667–675 (2010).
Tos, M., Larsen, P., Larsen, K. & Caye-Thomasen, P. in Nasal Polyposis (Springer-Verlag, 2010).
Takabayashi, T. et al. Excessive fibrin deposition in nasal polyps caused by fibrinolytic impairment through reduction of tissue plasminogen activator expression. Am. J. Respir. Crit. Care Med. 187, 49–57 (2013).
Takabayashi, T. et al. Increased expression of factor XIII-A in patients with chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 132, 584–592.e4 (2013).
Takabayashi, T. et al. Nattokinase, profibrinolytic enzyme, effectively shrinks the nasal polyp tissue and decreases viscosity of mucus. Allergol. Int. 66, 594–602 (2017).
Chen, C.-L. et al. Common fibrin deposition and tissue plasminogen activator downregulation in nasal polyps with distinct inflammatory endotypes. J. Allergy Clin. Immunol. https://doi.org/10.1016/j.jaci.2020.02.010 (2020).
Zhang, Y. et al. Th2 cytokines orchestrate the secretion of MUC 5 AC and MUC 5B in IL ‐5‐positive chronic rhinosinusitis with nasal polyps. Allergy 74, 131–140 (2019).
Van Zele, T., Holtappels, G., Gevaert, P. & Bachert, C. Differences in initial immunoprofiles between recurrent and nonrecurrent chronic rhinosinusitis with nasal polyps. Am. J. Rhinol. Allergy 28, 192–198 (2014). Important paper to show how immunology impacts on the clinic of CRSwNP in terms of recurrence of disease.
Tomassen, P. et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 137, 1449–1456.e4 (2016). A key paper showing endotypes based on cluster analysis of all forms of CRS, from uncomplicated CRSsNP to severe comorbid uncontrolled CRSwNP.
Lan, F. et al. Forkhead box protein 3 in human nasal polyp regulatory T cells is regulated by the protein suppressor of cytokine signaling 3. J. Allergy Clin. Immunol. 132, 1314–1321.e3 (2013).
Van Crombruggen, K., Taveirne, S., Holtappels, G., Leclercq, G. & Bachert, C. Innate lymphoid cells in the upper airways: importance of CD117 and IL-1RI expression. Eur. Respir. J. 52, 1800742 (2018).
Miljkovic, D. et al. Association between group 2 innate lymphoid cells enrichment, nasal polyps and allergy in chronic rhinosinusitis. Allergy 69, 1154–1161 (2014).
Mjösberg, J. et al. The transcription factor GATA3 is essential for the function of human type 2 innate lymphoid cells. Immunity 37, 649–659 (2012).
Lee, T.-J. et al. Impact of chronic rhinosinusitis on severe asthma patients. PLoS ONE 12, e0171047 (2017).
Poposki, J. A. et al. Group 2 innate lymphoid cells are elevated and activated in chronic rhinosinusitis with nasal polyps. Immun. Inflamm. Dis. 5, 233–243 (2017).
Eastman, J. J. et al. Group 2 innate lymphoid cells are recruited to the nasal mucosa in patients with aspirin-exacerbated respiratory disease. J. Allergy Clin. Immunol. 140, 101–108.e3 (2017).
Maric, J. et al. Cytokine-induced endogenous production of prostaglandin D2 is essential for human group 2 innate lymphoid cell activation. J. Allergy Clin. Immunol. 143, 2202–2214.e5 (2019).
Morita, H. et al. Induction of human regulatory innate lymphoid cells from group 2 innate lymphoid cells by retinoic acid. J. Allergy Clin. Immunol. 143, 2190–2201.e9 (2019).
Simon, H. U. et al. Direct demonstration of delayed eosinophil apoptosis as a mechanism causing tissue eosinophilia. J. Immunol. 158, 3902–3908 (1997). This paper demonstrated that eosinophils in CRSwNP live longer than in the peripheral blood and can be killed by anti-IL-5 but not by anti-IL-3 or anti-GM-CSF; it paved the way for subsequent biologics.
Barlow, J. L. et al. Innate IL-13–producing nuocytes arise during allergic lung inflammation and contribute to airways hyperreactivity. J. Allergy Clin. Immunol. 129, 191–198 (2012).
Wang, M. et al. Association of periostin expression with eosinophilic inflammation in nasal polyps. J. Allergy Clin. Immunol. 136, 1700–1703.e9 (2015).
Gevaert, P. et al. Local receptor revision and class switching to IgE in chronic rhinosinusitis with nasal polyps. Allergy 68, 55–63 (2013).
Calus, L. et al. IL-21 is increased in nasal polyposis and after stimulation with Staphylococcus aureus enterotoxin B. Int. Arch. Allergy Immunol. 174, 161–169 (2017).
Bachert, C. et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group phase 3 trials. Lancet 394, 1638–1650 (2019). This paper summarizes the first two successful phase III study results with a biologic, dupilumab, performed in CRSwNP.
Bachert, C. et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: randomized trial. J. Allergy Clin. Immunol. 140, 1024–1031.e14 (2017).
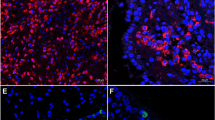
Gevaert, E. et al. Extracellular eosinophilic traps in association with Staphylococcus aureus at the site of epithelial barrier defects in patients with severe airway inflammation. J. Allergy Clin. Immunol. 139, 1849–1860.e6 (2017).
Ueki, S. et al. Eosinophil extracellular DNA trap cell death mediates lytic release of free secretion-competent eosinophil granules in humans. Blood 121, 2074–2083 (2013).
Ueki, S. et al. Charcot-Leyden crystal formation is closely associated with eosinophil extracellular trap cell death. Blood 132, 2183–2187 (2018).
Yousefi, S. et al. Catapult-like release of mitochondrial DNA by eosinophils contributes to antibacterial defense. Nat. Med. 14, 949–953 (2008).
Gevaert, E. et al. Charcot-Leyden crystals promote neutrophilic inflammation in patients with nasal polyposis. J. Allergy Clin. Immunol. 145, 427–430.e4 (2020).
Persson, E. K. et al. Protein crystallization promotes type 2 immunity and is reversible by antibody treatment. Science 364, eaaw4295 (2019). Excellent publication to show why eosinophils are not innocent bystanders but rather drivers of inflammation through the formation of Charcot–Leyden crystals in CRSwNP.
Yuan, S. et al. Oxidation increases mucin polymer cross-links to stiffen airway mucus gels. Sci. Transl Med. 7, 276ra27 (2015).
Chen, R. et al. Allergen-induced increases in sputum levels of group 2 innate lymphoid cells in subjects with asthma. Am. J. Respir. Crit. Care Med. 196, 700–712 (2017).
Baba, S., Kondo, K., Suzukawa, M., Ohta, K. & Yamasoba, T. Distribution, subtype population, and IgE positivity of mast cells in chronic rhinosinusitis with nasal polyps. Ann. Allergy Asthma Immunol. 119, 120–128 (2017).
Ryu, G. & Kim, D. W. Th2 inflammatory responses in the development of nasal polyps and chronic rhinosinusitis. Curr. Opin. Allergy Clin. Immunol. 20, 1–8 (2020).
Singh, D., Ravi, A. & Southworth, T. CRTH2 antagonists in asthma: current perspectives. Clin. Pharmacol. Adv. Appl. 9, 165–173 (2017).
Modena, B. D., Dazy, K. & White, A. A. Emerging concepts: mast cell involvement in allergic diseases. Transl Res. 174, 98–121 (2016).
Netea, M. G. et al. Defining trained immunity and its role in health and disease. Nat. Rev. Immunol. 20, 375–388 (2020).
Bach, J.-F. The effect of infections on susceptibility to autoimmune and allergic diseases. N. Engl. J. Med. 347, 911–920 (2002).
Strachan, D. P. Hay fever, hygiene, and household size. BMJ 299, 1259–1260 (1989).
Eberl, G. Immunity by equilibrium. Nat. Rev. Immunol. 16, 524–532 (2016).
Nordengrün, M., Michalik, S., Völker, U., Bröker, B. M. & Gómez-Gascón, L. The quest for bacterial allergens. Int. J. Med. Microbiol. 308, 738–750 (2018).
Wu, D., Wei, Y. & Bleier, B. S. Emerging role of proteases in the pathogenesis of chronic rhinosinusitis with nasal polyps. Front. Cell. Infect. Microbiol. 7, 538 (2017).
Wills-Karp, M. & Lewkowich, I. Fundamental Immunology (ed. Paul W. E.) 1113–1153 (Lippincott Williams & Wilkins, 2013).
Goodman, R. E. & Breiteneder, H. The WHO/IUIS allergen nomenclature. Allergy 74, 429–431 (2019).
Teufelberger, A. R., Bröker, B. M., Krysko, D. V., Bachert, C. & Krysko, O. Staphylococcus aureus orchestrates type 2 airway diseases. Trends Mol. Med. 25, 696–707 (2019).
Johannessen, M., Sollid, J. E. & Hanssen, A.-M. Host- and microbe determinants that may influence the success of S. aureus colonization. Front. Cell. Infect. Microbiol. 2, 56 (2012).
Wertheim, H. F. et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 5, 751–762 (2005).
Foster, T. J. Immune evasion by staphylococci. Nat. Rev. Microbiol. 3, 948–958 (2005).
Thammavongsa, V., Kim, H. K., Missiakas, D. & Schneewind, O. Staphylococcal manipulation of host immune responses. Nat. Rev. Microbiol. 13, 529–543 (2015).
Tuffs, S., Haeryfar, S. & McCormick, J. Manipulation of innate and adaptive immunity by staphylococcal superantigens. Pathogens 7, 53 (2018).
Lina, G. et al. Standard nomenclature for the superantigens expressed by Staphylococcus. J. Infect. Dis. 189, 2334–2336 (2004).
Hu, D.-L. & Nakane, A. Mechanisms of staphylococcal enterotoxin-induced emesis. Eur. J. Pharmacol. 722, 95–107 (2014).
Schmidt, F. et al. Characterization of human and Staphylococcus aureus proteins in respiratory mucosa by in vivo- and immunoproteomics. J. Proteom. 155, 31–39 (2017).
Nakamura, Y. et al. Staphylococcus δ-toxin induces allergic skin disease by activating mast cells. Nature 503, 397–401 (2013).
Teufelberger, A. R. et al. The IL-33/ST2 axis is crucial in type 2 airway responses induced by Staphylococcus aureus-derived serine protease-like protein D. J. Allergy Clin. Immunol. 141, 549–559.e7 (2018).
Berube, B. & Wardenburg, J. Staphylococcus aureus α-toxin: nearly a century of intrigue. Toxins 5, 1140–1166 (2013).
Murphy, J. et al. Staphylococcus aureus V8 protease disrupts the integrity of the airway epithelial barrier and impairs IL-6 production in vitro: V8 protease and airway barrier disruption. Laryngoscope 128, E8–E15 (2018).
Bachert, C. et al. Staphylococcus aureus and its IgE-inducing enterotoxins in asthma: current knowledge. Eur. Respir. J. 55, 1901592 (2020).
Fleischer, B. & Schrezenmeier, H. T cell stimulation by staphylococcal enterotoxins. Clonally variable response and requirement for major histocompatibility complex class II molecules on accessory or target cells. J. Exp. Med. 167, 1697–1707 (1988).
Proft, T. & Fraser, J. D. Bacterial superantigens. Clin. Exp. Immunol. 133, 299–306 (2003).
Marrack, P. & Kappler, J. The Staphylococcal enterotoxins and their relatives. Science 248, 705–711 (1990).
Lappin, E. & Ferguson, A. J. Gram-positive toxic shock syndromes. Lancet Infect. Dis. 9, 281–290 (2009).
Holtfreter, S. et al. Staphylococcus aureus carriers neutralize superantigens by antibodies specific for their colonizing strain: a potential explanation for their improved prognosis in severe sepsis. J. Infect. Dis. 193, 1275–1278 (2006).
Van Zele, T. et al. Staphylococcus aureus colonization and IgE antibody formation to enterotoxins is increased in nasal polyposis. J. Allergy Clin. Immunol. 114, 981–983 (2004).
Bachert, C. et al. Staphylococcus aureus enterotoxins as immune stimulants in chronic rhinosinusitis. Clin. Allergy Immunol. 20, 163–175 (2007).
Zhang, N. et al. An update on the impact of Staphylococcus aureus enterotoxins in chronic sinusitis with nasal polyposis. Rhinology 43, 162–168 (2005).
Bachert, C. & Zhang, N. Chronic rhinosinusitis and asthma: novel understanding of the role of IgE ‘above atopy’: review: chronic rhinosinusitis and asthma. J. Intern. Med. 272, 133–143 (2012).
Verkaik, N. J. et al. Immunogenicity of toxins during Staphylococcus aureus infection. Clin. Infect. Dis. 50, 61–68 (2010).
Shamji, M. H. et al. Broad IgG repertoire in patients with chronic rhinosinusitis with nasal polyps regulates proinflammatory IgE responses. J. Allergy Clin. Immunol. 143, 2086–2094.e2 (2019).
Zhang, N. et al. Mucosal tissue polyclonal IgE is functional in response to allergen and SEB. Allergy 66, 141–148 (2010).
Pryjma, J., Muñoz, J., Virella, G. & Fudenberg, H. H. Evaluation of IgM, IgG, IgA, IgD, and IgE secretion by human peripheral blood lymphocytes in cultures stimulated with pokeweed mitogen and Staphylococcus aureus Cowan I. Cell. Immunol. 50, 115–124 (1980).
Hemady, Z., Blomberg, F., Gellis, S. & Rocklin, R. IgE production in vitro by human blood mononuclear cells: a comparison between atopic and nonatopic subjects. J. Allergy Clin. Immunol. 71, 324–330 (1983).
Del Prete, G., Maggi, E., Romagnani, S. & Ricci, M. Human IgE biosynthesis in vitro. Clin. Rev. Allergy 7, 193–216 (1989).
Aman, M. J. Superantigens of a superbug: major culprits of Staphylococcus aureus disease? Virulence 8, 607–610 (2016).
Chen, W. H. et al. Safety and immunogenicity of a parenterally administered, structure-based rationally modified recombinant staphylococcal enterotoxin B protein vaccine, STEBVax. Clin. Vaccine Immunol. 23, 918–925 (2016).
Schwameis, M. et al. Safety, tolerability, and immunogenicity of a recombinant toxic shock syndrome toxin (rTSST)-1 variant vaccine: a randomised, double-blind, adjuvant-controlled, dose escalation first-in-man trial. Lancet Infect. Dis. 16, 1036–1044 (2016).
Mahdavinia, M., Keshavarzian, A., Tobin, M. C., Landay, A. L. & Schleimer, R. P. A comprehensive review of the nasal microbiome in chronic rhinosinusitis (CRS). Clin. Exp. Allergy 46, 21–41 (2016).
Meltzer, E. O. et al. Rhinosinusitis: establishing definitions for clinical research and patient care. J. Allergy Clin. Immunol. 114, 155–212 (2004).
Benninger, M. S. et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol. Head Neck Surg. 129, S1–S32 (2003).
Lanza, D. C. & Kennedy, D. W. Adult rhinosinusitis defined. Otolaryngol. Head Neck Surg. 117, S1–S7 (1997).
Falco, J. J. et al. Lack of correlation between patient reported location and severity of facial pain and radiographic burden of disease in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 6, 1173–1181 (2016).
Fokkens, W. J. et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 50, 1–12 (2012).
Akdis, C. A. et al. Endotypes and phenotypes of chronic rhinosinusitis: a PRACTALL document of the European academy of allergy and clinical immunology and the American academy of allergy, asthma & immunology. J. Allergy Clin. Immunol. 131, 1479–1490 (2013).
Beale, T. J., Madani, G. & Morley, S. J. Imaging of the paranasal sinuses and nasal cavity: normal anatomy and clinically relevant anatomical variants. Semin. Ultrasound CT MRI 30, 2–16 (2009).
Gurrola, J. & Borish, L. Chronic rhinosinusitis: endotypes, biomarkers, and treatment response. J. Allergy Clin. Immunol. 140, 1499–1508 (2017).
Bachert, C. & Akdis, C. A. Phenotypes and emerging endotypes of chronic rhinosinusitis. J. Allergy Clin. Immunol. Pract. 4, 621–628 (2016).
DeConde, A. S. & Smith, T. L. Classification of chronic rhinosinusitis — working toward personalized diagnosis. Otolaryngol. Clin. North. Am. 50, 1–12 (2017).
DeConde, A. S. et al. Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope 127, 550–555 (2017). This paper describes the results of surgery (recurrence of nasal polyps over 18 months) performed in university level clinics.
Vlaminck, S. et al. The importance of local eosinophilia in the surgical outcome of chronic rhinosinusitis: a 3-year prospective observational study. Am. J. Rhinol. Allergy 28, 260–264 (2014).
Bachert, C. et al. Endotypes of chronic rhinosinusitis with nasal polyps: pathology and possible therapeutic implications. J. Allergy Clin. Immunol. Pract. 8, 1514–1519 (2020).
Delemarre, T. et al. Type 2 inflammation in chronic rhinosinusitis without nasal polyps: another relevant endotype. J. Allergy Clin. Immunol. 146, 337–343.e6 (2020).
Kim, J. H. et al. Prevalence and risk factors of chronic rhinosinusitis in South Korea according to diagnostic criteria. Rhinology 54, 329–335 (2016).
Bhattacharyya, N. Incremental health care utilization and expenditures for chronic rhinosinusitis in the United States. Ann. Otol. Rhinol. Laryngol. 120, 423–427 (2011).
Bhattacharyya, N., Orlandi, R. R., Grebner, J. & Martinson, M. Cost burden of chronic rhinosinusitis. Otolaryngol. Head Neck Surg. 144, 440–445 (2011).
Cho, I. & Blaser, M. J. The human microbiome: at the interface of health and disease. Nat. Rev. Genet. 13, 260–270 (2012).
Choi, E.-B. et al. Decreased diversity of nasal microbiota and their secreted extracellular vesicles in patients with chronic rhinosinusitis based on a metagenomic analysis. Allergy 69, 517–526 (2014).
Liu, C. M. et al. Medical therapy reduces microbiota diversity and evenness in surgically recalcitrant chronic rhinosinusitis. Int. Forum Allergy Rhinol. 3, 775–781 (2013).
Maxfield, A. Z. et al. General antibiotic exposure is associated with increased risk of developing chronic rhinosinusitis: antibiotics promote the development of CRS. Laryngoscope 127, 296–302 (2017).
Orlandi, R. R. et al. International consensus statement on allergy and rhinology: rhinosinusitis. Int. Forum Allergy Rhinol. 6 (Suppl. 1), 22–209 (2016).
Chong, L. Y. et al. Different types of intranasal steroids for chronic rhinosinusitis. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD011993.pub2 (2016).
Chong, L. Y. et al. Intranasal steroids versus placebo or no intervention for chronic rhinosinusitis. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD011996.pub2 (2016).
Lund, V. J., Black, J. H., Szabó, L. Z., Schrewelius, C. & Akerlund, A. Efficacy and tolerability of budesonide aqueous nasal spray in chronic rhinosinusitis patients. Rhinology 42, 57–62 (2004).
Rudmik, L. et al. Utilization patterns of topical intranasal steroid therapy for chronic rhinosinusitis. JAMA Otolaryngol. Head Neck Surg. 142, 1056–1062 (2016).
Sastre, J. & Mosges, R. Local and systemic safety of intranasal corticosteroids. J. Investig. Allergol. Clin. Immunol. 22, 1–12 (2012).
Harvey, R. J., Snidvongs, K., Kalish, L. H., Oakley, G. M. & Sacks, R. Corticosteroid nasal irrigations are more effective than simple sprays in a randomized double-blinded placebo-controlled trial for chronic rhinosinusitis after sinus surgery. Int. Forum Allergy Rhinol. 8, 461–470 (2018).
Kalish, L., Snidvongs, K., Sivasubramaniam, R., Cope, D. & Harvey, R. J. Topical steroids for nasal polyps. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD006549.pub2 (2012).
Leopold, D. A. et al. NAVIGATE II: randomized, double-blind trial of the exhalation delivery system with fluticasone for nasal polyposis. J. Allergy Clin. Immunol. 143, 126–134.e5 (2019).
Han, J. K. & Kern, R. C. Topical therapies for management of chronic rhinosinusitis: steroid implants. Int. Forum Allergy Rhinol. 9 (S1), 22–26 (2019).
Kern, R. C. et al. A phase 3 trial of mometasone furoate sinus implants for chronic sinusitis with recurrent nasal polyps. Int. Forum Allergy Rhinol. 8, 471–481 (2018).
Chong, L. Y. et al. Saline irrigation for chronic rhinosinusitis. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD011995.pub2 (2016).
Head, K. et al. Short-course oral steroids alone for chronic rhinosinusitis. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD011991.pub2 (2016).
Won, T.-B., Jang, E., Min, S. K. & Kim, S. W. Treatment outcomes and predictors for systemic steroids in nasal polyposis. Acta Otolaryngol. 132 (Suppl. 1), S82–S87 (2012).
Kowalski, M. L. Oral and nasal steroids for nasal polyps. Curr. Allergy Asthma Rep. 11, 187–188 (2011).
Zhang, Y., Wang, C., Huang, Y., Lou, H. & Zhang, L. Efficacy of short-term systemic corticosteroid therapy in chronic rhinosinusitis with nasal polyps: a meta-analysis of randomized controlled trials and systematic review. Am. J. Rhinol. Allergy 33, 567–576 (2019).
Leung, R. M., Dinnie, K. & Smith, T. L. When do the risks of repeated courses of corticosteroids exceed the risks of surgery? Int. Forum Allergy Rhinol. 4, 871–876 (2014).
Fokkens, W. J. et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 58, 1–464 (2020).
Wallwork, B., Coman, W., Mackay-Sim, A., Greiff, L. & Cervin, A. A double-blind, randomized, placebo-controlled trial of macrolide in the treatment of chronic rhinosinusitis. Laryngoscope 116, 189–193 (2006).
Zeng, M., Long, X.-B., Cui, Y.-H. & Liu, Z. Comparison of efficacy of mometasone furoate versus clarithromycin in the treatment of chronic rhinosinusitis without nasal polyps in Chinese adults. Am. J. Rhinol. Allergy 25, e203–e207 (2011).
Videler, W. J. et al. Lack of efficacy of long-term, low-dose azithromycin in chronic rhinosinusitis: a randomized controlled trial: no efficacy of macrolides in chronic rhinosinusitis. Allergy 66, 1457–1468 (2011).
Van Zele, T. et al. Oral steroids and doxycycline: two different approaches to treat nasal polyps. J. Allergy Clin. Immunol. 125, 1069–1076.e4 (2010).
Varvyanskaya, A. & Lopatin, A. Efficacy of long-term low-dose macrolide therapy in preventing early recurrence of nasal polyps after endoscopic sinus surgery. Int. Forum Allergy Rhinol. 4, 533–541 (2014).
Smith, T. L. & Sautter, N. B. Is montelukast indicated for treatment of chronic rhinosinusitis with polyposis? Laryngoscope 124, 1735–1736 (2013).
Sacks, P.-L., Harvey, R. J., Rimmer, J., Gallagher, R. M. & Sacks, R. Topical and systemic antifungal therapy for the symptomatic treatment of chronic rhinosinusitis. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD008263.pub2 (2011).
Hellings, P. W. et al. Positioning the principles of precision medicine in care pathways for allergic rhinitis and chronic rhinosinusitis - A EUFOREA-ARIA-EPOS-AIRWAYS ICP statement. Allergy 72, 1297–1305 (2017).
Rudmik, L. et al. Defining appropriateness criteria for endoscopic sinus surgery during management of uncomplicated adult chronic rhinosinusitis: a RAND/UCLA appropriateness study. Rhinology 54, 117–128 (2016).
Alsharif, S. et al. Endoscopic sinus surgery for type‐2 CRS wNP: an endotype‐based retrospective study. Laryngoscope 129, 1286–1292 (2019). First description of the reboot technique, from rationale to technique, for severe CRSwNP.
Jankowski, R. & Bodino, C. Evolution of symptoms associated to nasal polyposis following oral steroid treatment and nasalization of the ethmoid–radical ethmoidectomy is functional surgery for NPS. Rhinology 41, 211–219 (2003).
Loftus, C. A. et al. Revision surgery rates in chronic rhinosinusitis with nasal polyps: meta‐analysis of risk factors. Int. Forum Allergy Rhinol. 10, 199–207 (2020).
Rudmik, L. et al. Evaluating surgeon-specific performance for endoscopic sinus surgery. JAMA Otolaryngol. Head Neck Surg. 143, 891-898 (2017).
Bassiouni, A. & Wormald, P.-J. Role of frontal sinus surgery in nasal polyp recurrence. Laryngoscope 123, 36–41 (2013).
Bachert, C., Zhang, N., Hellings, P. W. & Bousquet, J. Endotype-driven care pathways in patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 141, 1543–1551 (2018).
Bachert, C. & Zhang, N. Medical algorithm: diagnosis and treatment of chronic rhinosinusitis. Allergy 75, 240–242 (2020). A short paper to describe care pathways for severe CRSwNP in the new age of treatment possibilities, implementing the mucosal concept for surgery and the type 2 biologics for pharmacotherapy beyond corticosteroids.
Soler, Z. M. & Smith, T. L. Quality of life outcomes after functional endoscopic sinus surgery. Otolaryngol. Clin. North. Am. 43, 605–612 (2010).
Rudmik, L. et al. Productivity costs in patients with refractory chronic rhinosinusitis. Laryngoscope 124, 2007–2012 (2014).
DeConde, A. S., Bodner, T. E., Mace, J. C. & Smith, T. L. Response shift in quality of life after endoscopic sinus surgery for chronic rhinosinusitis. JAMA Otolaryngol. Head Neck Surg. 140, 712 (2014).
Alt, J. A., Smith, T. L., Mace, J. C. & Soler, Z. M. Sleep quality and disease severity in patients with chronic rhinosinusitis. Laryngoscope 123, 2364–2370 (2013).
Soler, Z. M., Eckert, M. A., Storck, K. & Schlosser, R. J. Cognitive function in chronic rhinosinusitis: a controlled clinical study. Int. Forum Allergy Rhinol. 5, 1010–1017 (2015).
Tomoum, M. O., Klattcromwell, C., DelSignore, A., Ebert, C. & Senior, B. A. Depression and anxiety in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 5, 674–681 (2015).
Stewart, M. G. & Smith, T. L. Objective versus subjective outcomes assessment in rhinology. Am. J. Rhinol. 19, 529–535 (2005).
Bhattacharyya, N. A comparison of symptom scores and radiographic staging systems in chronic rhinosinusitis. Am. J. Rhinol. 19, 175–179 (2005).
Psaltis, A. J., Li, G., Vaezeafshar, R., Cho, K. & Hwang, P. H. Modification of the lund‐kennedy endoscopic scoring system improves its reliability and correlation with patient‐reported outcome measures. Laryngoscope 124, 2216–2223 (2014).
Soler, Z. M., Hyer, J. M., Karnezis, T. T. & Schlosser, R. J. The olfactory cleft endoscopy scale correlates with olfactory metrics in patients with chronic rhinosinusitis. Int. Forum Allergy Rhinol. 6, 293–298 (2016).
Soler, Z. M. et al. Volumetric computed tomography analysis of the olfactory cleft in patients with chronic rhinosinusitis. Int. Forum Allergy Rhinol. 5, 846–854 (2015).
Ranford, D. et al. Co-morbid anxiety and depression impacts on the correlation between symptom and radiological severity in patients with chronic rhinosinusitis*. Rhinology https://doi.org/10.4193/Rhin20.075 (2020).
Smith, T. L. et al. Medical therapy vs surgery for chronic rhinosinusitis: a prospective, multi-institutional study. Int. Forum Allergy Rhinol. 1, 235–241 (2011).
Soler, Z. M. et al. Sino-Nasal outcome test-22 outcomes after sinus surgery: a systematic review and meta-analysis. Laryngoscope 128, 581–592 (2018).
DeConde, A. S., Suh, J. D., Mace, J. C., Alt, J. A. & Smith, T. L. Outcomes of complete vs targeted approaches to endoscopic sinus surgery. Int. Forum Allergy Rhinol. 5, 691–700 (2015).
Smith, T. L. et al. Comparing surgeon outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope 127, 14–21 (2016).
Smith, T. L. et al. Determinants of outcomes of sinus surgery: a multi-institutional prospective cohort study. Otolaryngol. Head Neck Surg. 142, 55–63 (2010).
Gevaert, P. et al. Efficacy and safety of omalizumab in nasal polyposis: 2 randomized phase 3 trials. J. Allergy Clin. Immunol. 146, 595–605 (2020).
Krug, N. et al. Allergen-induced asthmatic responses modified by a GATA3-specific DNAzyme. N. Engl. J. Med. 372, 1987–1995 (2015).
Hosemann, W. & Draf, C. Danger points, complications and medico-legal aspects in endoscopic sinus surgery. GMS Curr. Top. Otorhinolaryngol. Head Neck Surg. 12, Doc06 (2013).
Van Zele, T. et al. Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy 61, 1280–1289 (2006).
Abdurrahman, G., Schmiedeke, F., Bachert, C., Bröker, B. M. & Holtfreter, S. Allergy — a new role for T cell superantigens of Staphylococcus aureus? Toxins 12, 176 (2020).
Bader, J. P. & Ray, D. A. MC29 virus-coded protein occurs as monomers and dimers in transformed cells. J. Virol. 53, 509–514 (1985).
Szczeklik, A., Niżankowska, E. & Duplaga, M. Natural history of aspirin-induced asthma. AIANE Investigators. European Network on Aspirin-Induced Asthma. Eur. Respir. J. 16, 432-436 (2000).
Cahill, K. N., Bensko, J. C., Boyce, J. A. & Laidlaw, T. M. Prostaglandin D2: a dominant mediator of aspirin-exacerbated respiratory disease. J. Allergy Clin. Immunol. 135, 245–252 (2015).
Samter, M. & Beers, R. F. Jr Intolerance to Aspirin. Clinical studies and consideration of its pathogenesis. Ann. Intern. Med. 68, 975-983 (1968).
Rajan, J. P., Wineinger, N. E., Stevenson, D. D. & White, A. A. Prevalence of aspirin-exacerbated respiratory disease among asthmatic patients: a meta-analysis of the literature. J. Allergy Clin. Immunol. 135, 676–681.e1 (2015).
DeGregorio, G., Singer, J., Cahill, K. N. & Laidlaw, T. M. A 1-day, 90-minute aspirin challenge and desensitization protocol in aspirin-exacerbated respiratory disease. J. Allergy Clin. Immunol. 143, 1174–1180 (2019).
Pelletier, T. et al. Comparable safety of 2 aspirin desensitization protocols for aspirin exacerbated respiratory disease. J. Allergy Clin. Immunol. Pract. 7, 1319–1321 (2019).
Hope, A. P., Woessner, K. A., Simon, R. A. & Stevenson, D. D. Rational approach to aspirin dosing during oral challenges and desensitization of patients with aspirin-exacerbated respiratory disease. J. Allergy Clin. Immunol. 123, 406–410 (2009).
Berges-Gimeno, M. P., Simon, R. A. & Stevenson, D. D. Long-term treatment with aspirin desensitization in asthmatic patients with aspirin-exacerbated respiratory disease. J. Allergy Clin. Immunol. 111, 180–186 (2003).
Mosmann, T. R., Cherwinski, H., Bond, M. W., Giedlin, M. A. & Coffman, R. L. Two types of murine helper T cell clone. I. Definition according to profiles of lymphokine activities and secreted proteins. J. Immunol. 136, 2348–2357 (1986).
Annunziato, F., Romagnani, C. & Romagnani, S. The 3 major types of innate and adaptive cell-mediated effector immunity. J. Allergy Clin. Immunol. 135, 626–635 (2015).
Sakaguchi, S. et al. Regulatory T cells and human disease. Annu. Rev. Immunol. 38, 541–566 (2020).
Author information
Authors and Affiliations
Contributions
Introduction (C.B.); Epidemiology (W.-J.S.); Mechanisms/pathophysiology (R.P.S., B.N.L. and B.M.B.); Diagnosis, screening and prevention (B.M., C.B., C.H. and T.L.); Management (C.H. and R.J.S.); Quality of life (R.J.S.); Outlook (C.B.); Overview of Primer (C.B.).
Corresponding author
Ethics declarations
Competing interests
C.B. serves in advisory boards for AstraZeneca, GlaxoSmithKline, Mylan, Novartis and Sanofi-Aventis. R.J.S. has served as a consultant for GlaxoSmithKline, Healthy Humming, Optinose, Sanofi, and Stryker and has received grant support from AstraZeneca, Optinose and Stryker. C.H. has served on advisory boards for AstraZeneca, Olympus, Sanofi and Smith & Nephew. R.P.S. is a consultant for Actobio Therapeutics, Allakos, Aqualung Therapeutics Corp., Astellas Pharm. Inc., AstraZeneca/Medimmune, Aurasense, BioMarck, Celgene Corp., Exicure, Genentech, Genzyme/Sanofi Corp., GlaxoSmithKline, Intersect ENT, Lyra Therapeutics, Merck, Otsuka, and Sanofi and he owns stocks or stock options for Allakos, Aqualung Therapeutics Corp., Aurasense, BioMarck, and Exicure. Furthermore, he owns Allakos Siglec-8 and Siglec-8 ligand related patents; as a result of the Allakos licensing agreement, per Johns Hopkins University policy, he may be entitled to a share of future royalties regarding the sale of Siglec-8 related products, although no such royalties exist at the time of writing. T.L. has served on scientific advisory boards for GlaxoSmithKline, Optinose, Regeneron and Sanofi-Genzyme. B.N.L. serves in advisory boards for GlaxoSmithKline, Novartis, OncoArendi and Argenx. All other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Disease Primers thanks N. Cohen, A. Lane, V. Ramakrishnan, P. Wormald and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Hyposmia
-
Reduced ability to smell.
- Anosmia
-
Loss of smell.
- Mucosal concept
-
The role of prominent immune responses/endotypes in the sinus mucosa, which lead to different phenotypes of chronic rhinosinusitis and related clinical characteristics (asthma comorbidity and disease recurrence).
- Acanthosis
-
Epithelial hyperplasia.
- Acantholysis
-
Epithelial shedding.
- Allergens
-
Proteins with a propensity to induce an adaptive type 2 immune response characterized by specific IgE and type 2 T helper cells.
Rights and permissions
About this article
Cite this article
Bachert, C., Marple, B., Schlosser, R.J. et al. Adult chronic rhinosinusitis. Nat Rev Dis Primers 6, 86 (2020). https://doi.org/10.1038/s41572-020-00218-1
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-020-00218-1
This article is cited by
-
The chronic rhinosinusitis with nasal polyp patient journey in the United States and Europe
Allergy, Asthma & Clinical Immunology (2024)
-
Construction of PLGA nanoparticles modified with RWrNM and DLPC and their application in acute rhinosinusitis
Drug Delivery and Translational Research (2024)
-
Causal analysis between gastroesophageal reflux disease and chronic rhinosinusitis
European Archives of Oto-Rhino-Laryngology (2024)
-
Multidisciplinary Decision-Making—ITAlian Consensus After Two Years of Real Practice on the Management of Severe Uncontrolled CRSwNP by Biologics (ITACA Study)
Current Allergy and Asthma Reports (2024)
-
Simple, low-cost, and well-performing method, the outgrowth technique, for the isolation of cells from nasal polyps
BMC Molecular and Cell Biology (2023)