Abstract
Light-activated, photosensitizer-based therapies have been established as safe modalities of tumour ablation for numerous cancer indications. Two main approaches are available: photodynamic therapy, which results in localized chemical damage in the target lesions, and photothermal therapy, which results in localized thermal damage. Whereas the administration of photosensitizers is a key component of photodynamic therapy, exogenous photothermal contrast agents are not required for photothermal therapy but can enhance the efficiency and efficacy of treatment. Over the past decades, great strides have been made in the development of phototherapeutic drugs and devices as cancer treatments, but key challenges have restricted their widespread clinical use outside of certain dermatological indications. Improvements in the tumour specificity of photosensitizers, achieved through targeting or localized activation, could provide better outcomes with fewer adverse effects, as could combinations with chemotherapies or immunotherapies. In this Review, we provide an overview of the current clinical progress of phototherapies for cancer and discuss the emerging preclinical bioengineering approaches that have the potential to overcome challenges in this area and thus improve the efficiency and utility of such treatments.
Key points
-
Photodynamic therapy is predicated on the localized activation of photosensitizers within tumours in order to induce chemical damage and thus the death of tumour cells; this approach has been used in the clinic for >40 years for the treatment of diverse cancers, including superficial skin lesions and oesophageal and lung tumours.
-
Photothermal therapy (PTT) agents, which can be used to increase the efficiency of localized light-based heating and ablation of tumour tissues, have not yet been tested in large clinical trials; laser ablation without PTT agents has been used clinically.
-
Relative to single-modality approaches, drug–device combinations complicate clinical development; therefore, compelling efficacy and safety benefits are needed to support the use of such platforms in favour of competing ablative therapies.
-
Novel preclinical phototherapy agents have been engineered with advanced targeting and activation mechanisms.
-
These next-generation molecules and nanomaterials hold the potential to reduce adverse effects and/or improve the effectiveness of photodynamic therapy and PTT, leading to better outcomes and increased clinical adoption.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Ackroyd, R., Kelty, C., Brown, N. & Reed, M. The history of photodetection and photodynamic therapy. Photochem. Photobiol. 74, 656–669 (2001).
Daniell, M. D. & Hill, J. S. A history of photodynamic therapy. Aust. N. Z. J. Surg. 61, 340–348 (1991).
Finsen, N. R. Phototherapy (Edward Arnold Publishers Ltd., 1901).
Maiman, T. H. Stimulated optical radiation in ruby. Nature 187, 493–494 (1960).
Kapany, N. S., Peppers, N. A., Zweng, H. C. & Flocks, M. Retinal photocoagulation by lasers. Nature 199, 146–149 (1963).
Goldman, L. A review: applications of the laser beam in cancer biology. Int. J. Cancer 1, 309–318 (1966).
Sultan, R. A. Tumour ablation by laser in general surgery. Lasers Med. Sci. 5, 185–193 (1990).
Perry, R. R., Smith, P. D., Evans, S. & Pass, H. I. Intravenous vs intraperitoneal sensitizer: implications for intraperitoneal photodynamic therapy. Photochem. Photobiol. 53, 335–340 (1991).
Richter, K., Haslbeck, M. & Buchner, J. The heat shock response: life on the verge of death. Mol. Cell 40, 253–266 (2010).
Knavel, E. M. & Brace, C. L. Tumor ablation: common modalities and general practices. Tech. Vasc. Interv. Radiol. 16, 192–200 (2013).
Dolmans, D. E., Fukumura, D. & Jain, R. K. Photodynamic therapy for cancer. Nat. Rev. Cancer 3, 380–387 (2003).
Juarranz, A., Jaen, P., Sanz-Rodriguez, F., Cuevas, J. & Gonzalez, S. Photodynamic therapy of cancer. Basic principles and applications. Clin. Transl Oncol. 10, 148–154 (2008).
Celli, J. P. et al. Imaging and photodynamic therapy: mechanisms, monitoring, and optimization. Chem. Rev. 110, 2795–2838 (2010).
Jung, H. S. et al. Organic molecule-based photothermal agents: an expanding photothermal therapy universe. Chem. Soc. Rev. 47, 2280–2297 (2018).
Liu, Y., Bhattarai, P., Dai, Z. & Chen, X. Photothermal therapy and photoacoustic imaging via nanotheranostics in fighting cancer. Chem. Soc. Rev. 48, 2053–2108 (2019).
Chitgupi, U., Qin, Y. & Lovell, J. F. Targeted nanomaterials for phototherapy. Nanotheranostics 1, 38–58 (2017).
Sharman, W. M., Allen, C. M. & van Lier, J. E. Photodynamic therapeutics: basic principles and clinical applications. Drug Discov. Today 4, 507–517 (1999).
Li, X. et al. Phthalocyanines as medicinal photosensitizers: developments in the last five years. Coord. Chem. Rev. 379, 147–160 (2019).
Ethirajan, M., Chen, Y., Joshi, P. & Pandey, R. K. The role of porphyrin chemistry in tumor imaging and photodynamic therapy. Chem. Soc. Rev. 40, 340–362 (2011).
Garland, M. J., Cassidy, C. M., Woolfson, D. & Donnelly, R. F. Designing photosensitizers for photodynamic therapy: strategies, challenges and promising developments. Future Med. Chem. 1, 667–691 (2009).
Wainwright, M. Non-porphyrin photosensitizers in biomedicine. Chem. Soc. Rev. 25, 351–359 (1996).
Kamkaew, A. et al. BODIPY dyes in photodynamic therapy. Chem. Soc. Rev. 42, 77–88 (2013).
Lucky, S. S., Soo, K. C. & Zhang, Y. Nanoparticles in photodynamic therapy. Chem. Rev. 115, 1990–2042 (2015).
Li, X., Kim, J., Yoon, J. & Chen, X. Cancer-associated, stimuli-driven, turn on theranostics for multimodality imaging and therapy. Adv. Mater. 29, 1606857 (2017).
Feng, G. X. & Liu, B. Aggregation-induced emission (AIE) dots: emerging theranostic nanolights. Acc. Chem. Res. 51, 1404–1414 (2018).
Pogue, B. W. et al. Revisiting photodynamic therapy dosimetry: reductionist & surrogate approaches to facilitate clinical success. Phys. Med. Biol. 61, R57–R89 (2016).
Lin, J. T. Progress of medical lasers: fundamentals and applications. Med. Devices Diagn. Eng. 1, 36–41 (2016).
van den Bergh, H. On the evolution of some endoscopic light delivery systems for photodynamic therapy. Endoscopy 30, 392–407 (1998).
Shafirstein, G. et al. Interstitial photodynamic therapy – a focused review. Cancers 9, 12 (2017).
Panjehpour, M., Overholt, B. F., Denovo, R. C., Sneed, R. E. & Petersen, M. G. Centering balloon to improve esophageal photodynamic therapy. Lasers Surg. Med. 12, 631–638 (1992).
Moseley, H. Light distribution and calibration of commercial PDT LED arrays. Photochem. Photobiol. Sci. 4, 911–914 (2005).
Fitzmaurice, S. & Eisen, D. B. Daylight photodynamic therapy: what is known and what is yet to be determined. Dermatol. Surg. 42, 286–295 (2016).
Allison, R. R., Sibata, C. H., Downie, G. H. & Cuenca, R. E. A clinical review of PDT for cutaneous malignancies. Photodiagnosis Photodyn. Ther. 3, 214–226 (2006).
Casas, A., Di Venosa, G., Hasan, T. & Al, B. Mechanisms of resistance to photodynamic therapy. Curr. Med. Chem. 18, 2486–2515 (2011).
Luo, D., Carter, K. A., Miranda, D. & Lovell, J. F. Chemophototherapy: an emerging treatment option for solid tumors. Adv. Sci. 4, 1600106 (2017).
Ng, C. W., Li, J. C. & Pu, K. Y. Recent progresses in phototherapy-synergized cancer immunotherapy. Adv. Funct. Mater. 28, 1804688 (2018).
Wan, M. T. & Lin, J. Y. Current evidence and applications of photodynamic therapy in dermatology. Clin. Cosmet. Investig. Dermatol. 7, 145–163 (2014).
Baskaran, R., Lee, J. & Yang, S.-G. Clinical development of photodynamic agents and therapeutic applications. Biomater. Res. 22, 25 (2018).
Dougherty, T. J. et al. Photoradiation therapy for the treatment of malignant tumors. Cancer Res. 38, 2628–2635 (1978).
Agostinis, P. et al. Photodynamic therapy of cancer: an update. CA Cancer J. Clin. 61, 250–281 (2011).
Allison, R. R., Mota, H. C. & Sibata, C. H. Clinical PD/PDT in North America: an historical review. Photodiagnosis Photodyn. Ther. 1, 263–277 (2004).
Huang, Z. An update on the regulatory status of PDT photosensitizers in China. Photodiagnosis Photodyn. Ther. 5, 285–287 (2008).
Ormond, A. B. & Freeman, H. S. Dye sensitizers for photodynamic therapy. Materials 6, 817–840 (2013).
Advanz Pharma. Advanz Pharma, June 2019 Corporate Presentation https://www.advanzpharma.com/media/uploads/ADVANZ-PHARMA_Corporate-Presentation_June-2019_VF.pdf (2019).
Dougherty, T. J., Cooper, M. T. & Mang, T. S. Cutaneous phototoxic occurrences in patients receiving Photofrin®. Lasers Surg. Med. 10, 485–488 (1990).
Hamblin, M. R. Photodynamic therapy for cancer: what's past is prologue. Photochem. Photobiol. 96, 506–516 (2020).
Oliveira, J. et al. A first in human study using photodynamic therapy with Redaporfin in advanced head and neck cancer. J. Clin. Oncol. 35, e14056 (2017).
Pandey, R. K. et al. Nature: a rich source for developing multifunctional agents. Tumor-imaging and photodynamic therapy. Lasers Surg. Med. 38, 445–467 (2006).
Fisher, C. et al. Photodynamic therapy for the treatment of vertebral metastases: a phase I clinical trial. Clin. Cancer. Res. 25, 5766–5776 (2019).
van Straten, D., Mashayekhi, V., de Bruijn, H. S., Oliveira, S. & Robinson, D. J. Oncologic photodynamic therapy: basic principles, current clinical status and future directions. Cancers 9, 19 (2017).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Qumseya, B. J., David, W. & Wolfsen, H. C. Photodynamic therapy for Barrett's esophagus and esophageal carcinoma. Clin. Endosc. 46, 30–37 (2013).
Ferguson, M. K., Martin, T. R., Reeder, L. B. & Olak, J. Mortality after esophagectomy: risk factor analysis. World J. Surg. 21, 599–604 (1997).
Lightdale, C. J. et al. Photodynamic therapy with porfimer sodium versus thermal ablation therapy with Nd:YAG laser for palliation of esophageal cancer: a multicenter randomized trial. Gastrointest. Endosc. 42, 507–512 (1995).
Litle, V. R. et al. Photodynamic therapy as palliation for esophageal cancer: experience in 215 patients. Ann. Thorac. Surg. 76, 1687–1692 (2003).
Sibille, A., Lambert, R., Souquet, J.-C., Sabben, G. & Descos, F. Long-term survival after photodynamic therapy for esophageal cancer. Gastroenterology 108, 337–344 (1995).
Wolfsen, H. C., Hemminger, L. L., Wallace, M. B. & DeVault, K. R. Clinical experience of patients undergoing photodynamic therapy for Barrett's dysplasia or cancer. Aliment. Pharmacol. Ther. 20, 1125–1131 (2004).
Overholt, B. F. et al. Photodynamic therapy with porfimer sodium for ablation of high-grade dysplasia in Barrett's esophagus: international, partially blinded, randomized phase III trial. Gastrointest. Endosc. 62, 488–498 (2005).
Kohoutova, D. et al. Long-term outcomes of the randomized controlled trial comparing 5-aminolaevulinic acid and Photofrin photodynamic therapy for Barrett’s oesophagus related neoplasia. Scand. J. Gastroenterol. 53, 527–532 (2018).
Kato, H. et al. Photodynamic therapy (PDT) of lung cancer: experience of the Tokyo medical university. Photodiagnosis Photodyn. Ther. 1, 49–55 (2004).
Yano, T. et al. Phase I study of photodynamic therapy using talaporfin sodium and diode laser for local failure after chemoradiotherapy for esophageal cancer. Radiat. Oncol. 7, 113 (2012).
Wu, H., Minamide, T. & Yano, T. Role of photodynamic therapy in the treatment of esophageal cancer. Dig. Endosc. 31, 508–516 (2019).
Panjehpour, M., Overholt, B. F., Haydek, J. M. & Lee, S. G. Results of photodynamic therapy for ablation of dysplasia and early cancer in Barrett’s esophagus and effect of oral steroids on stricture formation. Am. J. Gastroenterol. 95, 2177–2184 (2000).
Simone, C. B. II & Cengel, K. A. Photodynamic therapy for lung cancer and malignant pleural mesothelioma. Semin. Oncol. 41, 820–830 (2014).
Balchum, O. J., Doiron, D. R. & Huth, G. C. HpD photodynamic therapy for obstructing lung cancer. Prog. Clin. Biol. Res. 170, 727–745 (1984).
Moghissi, K. et al. The place of bronchoscopic photodynamic therapy in advanced unresectable lung cancer: experience of 100 cases1. Eur. J. Cardiothorac. Surg. 15, 1–6 (1999).
Lam, S. et al. A randomized comparative study of the safety and efficacy of photodynamic therapy using photofrin II combined with palliative radiotherapy versus palliative radiotherapy alone in patients with inoperable obstructive non-small cell bronchogenic carcinoma. Photochem. Photobiol. 46, 893–897 (1987).
Diaz-Jimenez, J. P. et al. Efficacy and safety of photodynamic therapy versus Nd-YAG laser resection in NSCLC with airway obstruction. Eur. Respir. J. 14, 800–805 (1999).
Furuse, K. et al. A prospective phase II study on photodynamic therapy with photofrin II for centrally located early-stage lung cancer. The Japan Lung Cancer Photodynamic Therapy Study Group. J. Clin. Oncol. 11, 1852–1857 (1993).
Kato, H., Okunaka, T. & Shimatani, H. Photodynamic therapy for early stage bronchogenic carcinoma. J. Clin. Laser Med. Surg. 14, 235–238 (1996).
Furukawa, K. et al. Locally recurrent central-type early stage lung cancer <1.0 cm in diameter after complete remission by photodynamic therapy. Chest 128, 3269–3275 (2005).
Wang, S., Bromley, E., Xu, L., Chen, J. C. & Keltner, L. Talaporfin sodium. Expert. Opin. Pharmacother. 11, 133–140 (2010).
Kato, H. et al. Phase II clinical study of photodynamic therapy using mono-l-aspartyl chlorin e6 and diode laser for early superficial squamous cell carcinoma of the lung. Lung Cancer 42, 103–111 (2003).
Okunaka, T. et al. Photodynamic therapy for peripheral lung cancer. Lung Cancer 43, 77–82 (2004).
Pass, H. I. et al. Phase III randomized trial of surgery with or without intraoperative photodynamic therapy and postoperative immunochemotherapy for malignant pleural mesothelioma. Ann. Surg. Oncol. 4, 628–633 (1997).
Biel, M. A. Photodynamic therapy of head and neck cancers. Methods Mol. Biol. 635, 281–293 (2010).
Nyst, H. J., Tan, I. B., Stewart, F. A. & Balm, A. J. M. Is photodynamic therapy a good alternative to surgery and radiotherapy in the treatment of head and neck cancer? Photodiagnosis Photodyn. Ther. 6, 3–11 (2009).
Jerjes, W., Upile, T., Akram, S. & Hopper, C. The surgical palliation of advanced head and neck cancer using photodynamic therapy. Clin. Oncol. 22, 785–791 (2010).
Wile, A. G., Novotny, J., Mason, G. R., Passy, V. & Berns, M. W. Photoradiation therapy of head and neck cancer. Prog. Clin. Biol. Res. 170, 681–691 (1984).
Biel, M. A. Photodynamic therapy treatment of early oral and laryngeal cancers†. Photochem. Photobiol. 83, 1063–1068 (2007).
Hopper, C. et al. mTHPC-mediated photodynamic therapy for early oral squamous cell carcinoma. Int. J. Cancer 111, 138–146 (2004).
Meulemans, J., Delaere, P. & Vander Poorten, V. Photodynamic therapy in head and neck cancer: indications, outcomes, and future prospects. Curr. Opin. Otolaryngol. Head Neck Surg. 27, 136–141 (2019).
Tan, I. B. et al. Temoporfin-mediated photodynamic therapy in patients with advanced, incurable head and neck cancer: a multicenter study. Head Neck 32, 1597–1604 (2010).
D'Cruz, A. K., Robinson, M. H. & Biel, M. A. mTHPC-mediated photodynamic therapy in patients with advanced, incurable head and neck cancer: a multicenter study of 128 patients. Head Neck 26, 232–240 (2004).
Hopper, C., Niziol, C. & Sidhu, M. The cost-effectiveness of Foscan mediated photodynamic therapy (Foscan-PDT) compared with extensive palliative surgery and palliative chemotherapy for patients with advanced head and neck cancer in the UK. Oral. Oncol. 40, 372–382 (2004).
Morton, C. A., Szeimies, R. M., Sidoroff, A. & Braathen, L. R. European guidelines for topical photodynamic therapy part 1: treatment delivery and current indications - actinic keratoses, Bowen's disease, basal cell carcinoma. J. Eur. Acad. Dermatol. Venereol. 27, 536–544 (2013).
Morton, C. A. et al. Comparison of photodynamic therapy with cryotherapy in the treatment of Bowen's disease. Br. J. Dermatol. 135, 766–771 (1996).
Ohgari, Y. et al. Mechanisms involved in δ-aminolevulinic acid (ALA)-induced photosensitivity of tumor cells: relation of ferrochelatase and uptake of ALA to the accumulation of protoporphyrin. Biochem. Pharmacol. 71, 42–49 (2005).
Kennedy, J. C., Pottier, R. H. & Pross, D. C. Photodynamic therapy with endogenous protoporphyrin: IX: basic principles and present clinical experience. J. Photochem. Photobiol. B Biol. 6, 143–148 (1990).
Jeffes, E. W. et al. Photodynamic therapy of actinic keratosis with topical 5-aminolevulinic acid: a pilot dose-ranging study. Arch. Dermatol. 133, 727–732 (1997).
Cohen, D. K. & Lee, P. K. Photodynamic therapy for non-melanoma skin cancers. Cancers 8, 90 (2016).
Gaullier, J. M. et al. Use of 5-aminolevulinic acid esters to improve photodynamic therapy on cells in culture. Cancer Res. 57, 1481–1486 (1997).
Moloney, F. J. & Collins, P. Randomized, double-blind, prospective study to compare topical 5-aminolaevulinic acid methylester with topical 5-aminolaevulinic acid photodynamic therapy for extensive scalp actinic keratosis. Br. J. Dermatol. 157, 87–91 (2007).
Dirschka, T. et al. Photodynamic therapy with BF-200 ALA for the treatment of actinic keratosis: results of a multicentre, randomized, observer-blind phase III study in comparison with a registered methyl-5-aminolaevulinate cream and placebo. Br. J. Dermatol. 166, 137–146 (2012).
Wang, I. et al. Photodynamic therapy vs. cryosurgery of basal cell carcinomas: results of a phase III clinical trial. Br. J. Dermatol. 144, 832–840 (2001).
Szeimies, R. M. et al. A clinical study comparing methyl aminolevulinate photodynamic therapy and surgery in small superficial basal cell carcinoma (8–20 mm), with a 12-month follow-up. J. Eur. Acad. Dermatol. Venereol. 22, 1302–1311 (2008).
Rhodes, L. E. et al. Photodynamic therapy using topical methyl aminolevulinate vs surgery for nodular basal cell carcinoma: results of a multicenter randomized prospective trial. Arch. Dermatol. 140, 17–23 (2004).
Morton, C. A. et al. A randomized, multinational, noninferiority, phase III trial to evaluate the safety and efficacy of BF-200 aminolaevulinic acid gel vs. methyl aminolaevulinate cream in the treatment of nonaggressive basal cell carcinoma with photodynamic therapy. Br. J. Dermatol. 179, 309–319 (2018).
Wang, B.-C., Fu, C., Qin, L., Zeng, X.-Y. & Liu, Q. Photodynamic therapy with methyl-5-aminolevulinate for basal cell carcinoma: a systematic review and meta-analysis. Photodiagnosis Photodyn. Ther. 29, 101667 (2020).
Wiegell, S. R. et al. A randomized, multicentre study of directed daylight exposure times of 1½ vs. 2½ h in daylight-mediated photodynamic therapy with methyl aminolaevulinate in patients with multiple thin actinic keratoses of the face and scalp. Br. J. Dermatol. 164, 1083–1090 (2011).
Morton, C. A. & Braathen, L. R. Daylight photodynamic therapy for actinic keratoses. Am. J. Clin. Dermatol. 19, 647–656 (2018).
See, J.-A. et al. Consensus recommendations on the use of daylight photodynamic therapy with methyl aminolevulinate cream for actinic keratoses in Australia. Australas. J. Dermatol. 57, 167–174 (2016).
Banerjee, S. M. et al. Photodynamic therapy: Inception to application in breast cancer. Breast 31, 105–113 (2017).
Leggett, C. L. et al. Photodynamic therapy for unresectable cholangiocarcinoma: a comparative effectiveness systematic review and meta-analyses. Photodiagnosis Photodyn. Ther. 9, 189–195 (2012).
Lee, T. Y., Cheon, Y. K., Shim, C. S. & Cho, Y. D. Photodynamic therapy prolongs metal stent patency in patients with unresectable hilar cholangiocarcinoma. World J. Gastroenterol. 18, 5589–5594 (2012).
Fan, B.-G. & Andrén-Sandberg, Å. Photodynamic therapy for pancreatic cancer. Pancreas 34, 385–389 (2007).
Bown, S. G. Photodynamic therapy for cancer of the pancreas – The story so far. Photonics Lasers Med. 5, 91 (2016).
Allison, R. R. et al. PD/PDT for gynecological disease: a clinical review. Photodiagnosis Photodyn. Ther. 2, 51–63 (2005).
Baldea, I. & Filip, A. G. Photodynamic therapy in melanoma–an update. J. Physiol. Pharmacol. 63, 109–118 (2012).
Dougherty, T. J. Photodynamic therapy. Photochem. Photobiol. 58, 895–900 (1993).
Jichlinski, P. & Leisinger, H.-J. Photodynamic therapy in superficial bladder cancer: past, present and future. Urol. Res. 29, 396–405 (2001).
Jocham, D. et al. [BCG versus photodynamic therapy (PDT) for nonmuscle invasive bladder cancer-a multicentre clinical phase III study [In German]. Aktuelle Urol. 40, 91–99 (2009).
Filonenko, E. V. et al. 5-Aminolevulinic acid in intraoperative photodynamic therapy of bladder cancer (results of multicenter trial). Photodiagnosis Photodyn. Ther. 16, 106–109 (2016).
Bader, M. J. et al. Photodynamic therapy of bladder cancer - a phase I study using hexaminolevulinate (HAL). Urol. Oncol. 31, 1178–1183 (2013).
Lapini, A. et al. A comparison of hexaminolevulinate (Hexvix®) fluorescence cystoscopy and white-light cystoscopy for detection of bladder cancer: results of the HeRo observational study. Surg. Endosc. 26, 3634–3641 (2012).
Fisher, C. J. & Lilge, L. Photodynamic therapy in the treatment of intracranial gliomas: a review of current practice and considerations for future clinical directions. J. Innovative Optical Health Sci. 08, 1530005 (2015).
Stylli, S. S., Kaye, A. H., MacGregor, L., Howes, M. & Rajendra, P. Photodynamic therapy of high grade glioma – long term survival. J. Clin. Neurosci. 12, 389–398 (2005).
Quirk, B. J. et al. Photodynamic therapy (PDT) for malignant brain tumors – where do we stand? Photodiagnosis Photodyn. Ther. 12, 530–544 (2015).
Mahmoudi, K. et al. 5-aminolevulinic acid photodynamic therapy for the treatment of high-grade gliomas. J. Neurooncol. 141, 595–607 (2019).
Stummer, W. et al. Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol. 7, 392–401 (2006).
Lau, D. et al. A prospective Phase II clinical trial of 5-aminolevulinic acid to assess the correlation of intraoperative fluorescence intensity and degree of histologic cellularity during resection of high-grade gliomas. J. Neurosurg. 124, 1300–1309 (2016).
Eljamel, M. S., Goodman, C. & Moseley, H. ALA and Photofrin® fluorescence-guided resection and repetitive PDT in glioblastoma multiforme: a single centre phase III randomised controlled trial. Lasers Med. Sci. 23, 361–367 (2008).
Johansson, A. et al. Protoporphyrin IX fluorescence and photobleaching during interstitial photodynamic therapy of malignant gliomas for early treatment prognosis. Lasers Surg. Med. 45, 225–234 (2013).
Lakomkin, N. & Hadjipanayis, C. G. Fluorescence-guided surgery for high-grade gliomas. J. Surg. Oncol. 118, 356–361 (2018).
Moore, C. M., Pendse, D. & Emberton, M. Photodynamic therapy for prostate cancer — a review of current status and future promise. Nat. Clin. Pract. Urol. 6, 18–30 (2009).
Williams, S. B. et al. Comparative effectiveness of cryotherapy vs brachytherapy for localised prostate cancer. BJU Int. 110, E92–E98 (2012).
Gheewala, T., Skwor, T. & Munirathinam, G. Photosensitizers in prostate cancer therapy. Oncotarget 8, 30524–30538 (2017).
Nathan, T. R. et al. Photodynamic therapy for prostate cancer recurrence after radiotherapy: a phase I study. J. Urol. 168, 1427–1432 (2002).
Azzouzi, A.-R. et al. Padeliporfin vascular-targeted photodynamic therapy versus active surveillance in men with low-risk prostate cancer (CLIN1001 PCM301): an open-label, phase 3, randomised controlled trial. Lancet Oncol. 18, 181–191 (2017).
Hansen, G. & Sundset, A. Transbronchial laser ablation of benign and malignant tumors. Minim. Invasive Ther. Allied Technol. 15, 4–8 (2006).
Wenger, H., Yousuf, A., Oto, A. & Eggener, S. Laser ablation as focal therapy for prostate cancer. Curr. Opin. Urol. 24, 236–240 (2014).
Gough-Palmer, A. L. & Gedroyc, W. M. W. Laser ablation of hepatocellular carcinoma — a review. World J. Gastroenterol. 14, 7170–7174 (2008).
Vogl, T. J., Straub, R., Eichler, K., Söllner, O. & Mack, M. G. Colorectal carcinoma metastases in liver: laser-induced interstitial thermotherapy — local tumor control rate and survival data. Radiology 230, 450–458 (2004).
Vogl, T. J., Straub, R., Eichler, K., Woitaschek, D. & Mack, M. G. Malignant liver tumors treated with MR imaging-guided laser-induced thermotherapy: experience with complications in 899 patients (2,520 lesions). Radiology 225, 367–377 (2002).
Arienti, V. et al. Complications of laser ablation for hepatocellular carcinoma: a multicenter study. Radiology 246, 947–955 (2008).
Belykh, E. et al. Laser application in neurosurgery. Surg. Neurol. Int. 8, 274–274 (2017).
Hawasli, A. H., Kim, A. H., Dunn, G. P., Tran, D. D. & Leuthardt, E. C. Stereotactic laser ablation of high-grade gliomas. Neurosurg. Focus 37, E1 (2014).
Lagman, C. et al. Laser neurosurgery: a systematic analysis of magnetic resonance-guided laser interstitial thermal therapies. J. Clin. Neurosci. 36, 20–26 (2017).
Bozinov, O., Yang, Y., Oertel, M. F., Neidert, M. C. & Nakaji, P. Laser interstitial thermal therapy in gliomas. Cancer Lett. 474, 151–157 (2020).
Schwartzberg, B. et al. Phase 2 open-label trial investigating percutaneous laser ablation for treatment of early-stage breast cancer: MRI, pathology, and outcome correlations. Ann. Surg. Oncol. 25, 2958–2964 (2018).
Lal, S., Clare, S. E. & Halas, N. J. Nanoshell-enabled photothermal cancer therapy: impending clinical impact. Acc. Chem. Res. 41, 1842–1851 (2008).
Rastinehad, A. R. et al. Gold nanoshell-localized photothermal ablation of prostate tumors in a clinical pilot device study. Proc. Natl Acad. Sci. USA 116, 18590–18596 (2019).
Chen, W. R., Adams, R. L., Carubelli, R. & Nordquist, R. E. Laser-photosensitizer assisted immunotherapy: a novel modality for cancer treatment. Cancer Lett. 115, 25–30 (1997).
Delaey, E. et al. A comparative study of the photosensitizing characteristics of some cyanine dyes. J. Photochem. Photobiol. B Biol. 55, 27–36 (2000).
Li, X. et al. Preliminary safety and efficacy results of laser immunotherapy for the treatment of metastatic breast cancer patients. Photochem. Photobiol. Sci. 10, 817–821 (2011).
Fang, J., Nakamura, H. & Maeda, H. The EPR effect: unique features of tumor blood vessels for drug delivery, factors involved, and limitations and augmentation of the effect. Adv. Drug Del. Rev. 63, 136–151 (2011).
Allison, R. R., Mota, H. C., Bagnato, V. S. & Sibata, C. H. Bio-nanotechnology and photodynamic therapy — state of the art review. Photodiagnosis Photodyn. Ther. 5, 19–28 (2008).
Bertrand, N., Wu, J., Xu, X. Y., Kamaly, N. & Farokhzad, O. C. Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Adv. Drug Deliv. Rev. 66, 2–25 (2014).
Peer, D. et al. Nanocarriers as an emerging platform for cancer therapy. Nat. Nanotechnol. 2, 751–760 (2007).
Danhier, F. To exploit the tumor microenvironment: since the EPR effect fails in the clinic, what is the future of nanomedicine? J. Control. Rel. 244, 108–121 (2016).
Li, Z. M. et al. RGD-conjugated dendrimer-modified gold nanorods for in vivo tumor targeting and photothermal therapy. Mol. Pharm. 7, 94–104 (2010).
Conde, J., Oliva, N., Zhang, Y. & Artzi, N. Local triple-combination therapy results in tumour regression and prevents recurrence in a colon cancer model. Nat. Mater. 15, 1128–1138 (2016).
Kotagiri, N., Sudlow, G. P., Akers, W. J. & Achilefu, S. Breaking the depth dependency of phototherapy with Cerenkov radiation and low-radiance-responsive nanophotosensitizers. Nat. Nanotechnol. 10, 370–379 (2015).
Wang, K. K. et al. Self-assembled IR780-loaded transferrin nanoparticles as an imaging, targeting and PDT/PTT agent for cancer therapy. Sci. Rep. 6, 27421 (2016).
Shieh, Y. A., Yang, S. J., Wei, M. F. & Shieh, M. J. Aptamer-based tumor-targeted drug delivery for photodynamic therapy. ACS Nano 4, 1433–1442 (2010).
Ryu, T. K., Baek, S. W., Kang, R. H. & Choi, S. W. Selective photothermal tumor therapy using nanodiamond-based nanoclusters with folic acid. Adv. Funct. Mater. 26, 6428–6436 (2016).
Li, X. et al. Nanostructured phthalocyanine assemblies with protein-driven switchable photoactivities for biophotonic imaging and therapy. J. Am. Chem. Soc. 139, 10880–10886 (2017).
Yoon, H. Y. et al. Tumor-targeting hyaluronic acid nanoparticles for photodynamic imaging and therapy. Biomaterials 33, 3980–3989 (2012).
Mew, D., Wat, C. K., Towers, G. H. & Levy, J. G. Photoimmunotherapy: treatment of animal tumors with tumor-specific monoclonal antibody-hematoporphyrin conjugates. J. Immunol. 130, 1473–1477 (1983).
Oseroff, A. R. et al. Strategies for selective cancer photochemotherapy: antibody-targeted and selective carcinoma cell photolysis. Photochem. Photobiol. 46, 83–96 (1987).
Schmidt, S., Wagner, U., Oehr, P. & Krebs, D. Clinical use of photodynamic therapy in gynecologic tumor patients — antibody-targeted photodynamic laser therapy as a new oncologic treatment procedure [In German]. Zentralbl. Gynakol. 114, 307–311 (1992).
Mitsunaga, M. et al. Cancer cell-selective in vivo near infrared photoimmunotherapy targeting specific membrane molecules. Nat. Med. 17, 1685–1691 (2011).
Cheng, L. et al. Multifunctional nanoparticles for upconversion luminescence/MR multimodal imaging and magnetically targeted photothermal therapy. Biomaterials 33, 2215–2222 (2012).
Zhou, Z. G. et al. Iron/iron oxide core/shell nanoparticles for magnetic targeting MRI and near-infrared photothermal therapy. Biomaterials 35, 7470–7478 (2014).
Yu, J. et al. Smart MoS2/Fe3O4 nanotheranostic for magnetically targeted photothermal therapy guided by magnetic resonance/photoacoustic imaging. Theranostics 5, 931–945 (2015).
Sharman, W. M., Allen, C. M. & van Lier, J. E. Role of activated oxygen species in photodynamic therapy. Methods Enzymol. 319, 376–400 (2000).
Kessel, D. & Reiners, J. J. Jr Promotion of proapoptotic signals by lysosomal photodamage. Photochem. Photobiol. 91, 931–936 (2015).
Akhlynina, T. V. et al. Nuclear targeting of chlorin e6 enhances its photosensitizing activity. J. Biol. Chem. 272, 20328–20331 (1997).
Morgan, J. & Oseroff, A. R. Mitochondria-based photodynamic anti-cancer therapy. Adv. Drug Deliv. Rev. 49, 71–86 (2001).
Vankayala, R., Kuo, C. L., Nuthalapati, K., Chiang, C. S. & Hwang, K. C. Nucleus-targeting gold nanoclusters for simultaneous in vivo fluorescence imaging, gene delivery, and NIR-light activated photodynamic therapy. Adv. Funct. Mater. 25, 5934–5945 (2015).
Chen, W. et al. A C5N2 nanoparticle based direct nucleus delivery platform for synergistic cancer therapy. Angew. Chem. Int. Ed. 58, 6290–6294 (2019).
Høgset, A. et al. Photochemical internalisation in drug and gene delivery. Adv. Drug Del. Rev. 56, 95–115 (2004).
Berg, K. et al. Disulfonated tetraphenyl chlorin (TPCS2a), a novel photosensitizer developed for clinical utilization of photochemical internalization. Photochem. Photobiol. Sci. 10, 1637–1651 (2011).
Norum, O.-J., Selbo, P. K., Weyergang, A., Giercksky, K.-E. & Berg, K. Photochemical internalization (PCI) in cancer therapy: from bench towards bedside medicine. J. Photochem. Photobiol. B Biol. 96, 83–92 (2009).
Sultan, A. A. et al. Disulfonated tetraphenyl chlorin (TPCS2a)-induced photochemical internalisation of bleomycin in patients with solid malignancies: a phase 1, dose-escalation, first-in-man trial. Lancet Oncol. 17, 1217–1229 (2016).
Håkerud, M. et al. Intradermal photosensitisation facilitates stimulation of MHC class-I restricted CD8 T-cell responses of co-administered antigen. J. Controlled Rel. 174, 143–150 (2014).
Frangioni, J. V. In vivo near-infrared fluorescence imaging. Curr. Opin. Chem. Biol. 7, 626–634 (2003).
Oleinick, N. L. & Evans, H. H. The photobiology of photodynamic therapy: cellular targets and mechanisms. Radiat. Res. 150, S146–S156 (1998).
Simpson, C. R., Kohl, M., Essenpreis, M. & Cope, M. Near-infrared optical properties of ex vivo human skin and subcutaneous tissues measured using the Monte Carlo inversion technique. Phys. Med. Biol. 43, 2465–2478 (1998).
Bolze, F., Jenni, S., Sour, A. & Heitz, V. Molecular photosensitisers for two-photon photodynamic therapy. Chem. Commun. 53, 12857–12877 (2017).
Chen, G. Y., Qju, H. L., Prasad, P. N. & Chen, X. Y. Upconversion nanoparticles: design, nanochemistry, and applications in theranostics. Chem. Rev. 114, 5161–5214 (2014).
Zhu, S. J., Tian, R., Antaris, A. L., Chen, X. Y. & Dai, H. J. Near-infrared-II molecular dyes for cancer imaging and surgery. Adv. Mater. 31, e1900321 (2019).
Ge, X. G. et al. Photoacoustic imaging and photothermal therapy in the second near-infrared window. New J. Chem. 43, 8835–8851 (2019).
Fan, W. P., Huang, P. & Chen, X. Y. Overcoming the Achilles' heel of photodynamic therapy. Chem. Soc. Rev. 45, 6488–6519 (2016).
Ni, K. Y. et al. Nanoscale metal-organic frameworks for mitochondria-targeted radiotherapy-radiodynamic therapy. Nat. Commun. 9, 4321 (2018).
Xu, X. Q. et al. A self-illuminating nanoparticle for inflammation imaging and cancer therapy. Sci. Adv. 5, eaat2953 (2019).
Abdurahman, R., Yang, C.-X. & Yan, X.-P. Conjugation of a photosensitizer to near infrared light renewable persistent luminescence nanoparticles for photodynamic therapy. Chem. Commun. 52, 13303–13306 (2016).
Fan, W. et al. Enhanced afterglow performance of persistent luminescence implants for efficient repeatable photodynamic therapy. ACS Nano 11, 5864–5872 (2017).
Brown, J. M. & William, W. R. Exploiting tumour hypoxia in cancer treatment. Nat. Rev. Cancer 4, 437–447 (2004).
Li, X. S., Kwon, N., Guo, T., Liu, Z. & Yoon, J. Innovative strategies for hypoxic-tumor photodynamic therapy. Angew. Chem. Int. Ed. 57, 11522–11531 (2018).
Song, X. J., Feng, L. Z., Liang, C., Yang, K. & Liu, Z. Ultrasound triggered tumor oxygenation with oxygen-shuttle nanoperfluorocarbon to overcome hypoxia-associated resistance in cancer therapies. Nano Lett. 16, 6145–6153 (2016).
Turan, I. S., Yildiz, D., Turksoy, A., Gunaydin, G. & Akkaya, E. U. A bifunctional photosensitizer for enhanced fractional photodynamic therapy: singlet oxygen generation in the presence and absence of light. Angew. Chem. Int. Ed. 55, 2875–2878 (2016).
Li, X. S., Lee, D. Y., Huang, J. D. & Yoon, J. Y. Phthalocyanine-assembled nanodots as photosensitizers for highly efficient type I photoreactions in photodynamic therapy. Angew. Chem. Int. Ed. 57, 9885–9890 (2018).
Feng, L. et al. Theranostic liposomes with hypoxia-activated prodrug to effectively destruct hypoxic tumors post-photodynamic therapy. ACS Nano 11, 927–937 (2017).
Li, X. et al. Facile supramolecular approach to nucleic-acid-driven activatable nanotheranostics that overcome drawbacks of photodynamic therapy. ACS Nano 12, 681–688 (2018).
Huang, Z. A review of progress in clinical photodynamic therapy. Technol. Cancer Res. Treat. 4, 283–293 (2005).
Vrouenraets, M. B., Visser, G. W. M., Snow, G. B. & van Dongen, G. A. M. S. Basic principles, applications in oncology and improved selectivity of photodynamic therapy. Anticancer Res. 23, 505–522 (2003).
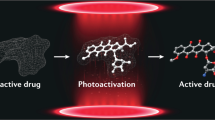
Lovell, J. F., Liu, T. W. B., Chen, J. & Zheng, G. Activatable photosensitizers for imaging and therapy. Chem. Rev. 110, 2839–2857 (2010).
Li, X. S., Kolemen, S., Yoon, J. & Akkaya, E. U. Activatable photosensitizers: agents for selective photodynamic therapy. Adv. Funct. Mater. 27, 1604053 (2017).
Li, X. S. et al. A tumor-pH-responsive supramolecular photosensitizer for activatable photodynamic therapy with minimal in vivo skin phototoxicity. Theranostics 7, 2746–2756 (2017).
Li, X. S. et al. Sequential protein-responsive nanophotosensitizer complex for enhancing tumor-specific therapy. ACS Nano 13, 6702–6710 (2019).
Tian, B., Wang, C., Zhang, S., Feng, L. Z. & Liu, Z. Photothermally enhanced photodynamic therapy delivered by nano-graphene oxide. ACS Nano 5, 7000–7009 (2011).
Xiao, Q. F. et al. A core/satellite multifunctional nanotheranostic for in vivo imaging and tumor eradication by radiation/photothermal synergistic therapy. J. Am. Chem. Soc. 135, 13041–13048 (2013).
Tang, Z. M. et al. Pyroelectric nanoplatform for NIR-II-triggered photothermal therapy with simultaneous pyroelectric dynamic therapy. Mater. Horiz. 5, 946–952 (2018).
Wang, S. J. et al. Single continuous wave laser induced photodynamic/plasmonic photothermal therapy using photosensitizer-functionalized gold nanostars. Adv. Mater. 25, 3055–3061 (2013).
Yang, T. et al. Bifunctional tellurium nanodots for photo-induced synergistic cancer therapy. ACS Nano 11, 10012–10024 (2017).
Younis, M. R. et al. Low power single laser activated synergistic cancer phototherapy using photosensitizer functionalized dual plasmonic photothermal nanoagents. ACS Nano 13, 2544–2557 (2019).
He, C. B., Liu, D. M. & Lin, W. B. Self-assembled core-shell nanoparticles for combined chemotherapy and photodynamic therapy of resistant head and neck cancers. ACS Nano 9, 991–1003 (2015).
Wang, Z. G., Ma, R., Yan, L., Chen, X. F. & Zhu, G. Y. Combined chemotherapy and photodynamic therapy using a nanohybrid based on layered double hydroxides to conquer cisplatin resistance. Chem. Commun. 51, 11587–11590 (2015).
Ullah, M. F. Cancer multidrug resistance (MDR): a major impediment to effective chemotherapy. Asian Pac. J. Cancer Prev. 9, 1–6 (2008).
He, Q. J. et al. A pH-responsive mesoporous silica nanoparticles-based multi-drug delivery system for overcoming multi-drug resistance. Biomaterials 32, 7711–7720 (2011).
Gao, Y. et al. Controlled intracellular release of doxorubicin in multidrug-resistant cancer cells by tuning the shell-pore sizes of mesoporous silica nanoparticles. ACS Nano 5, 9788–9798 (2011).
Duan, X. P. et al. Smart pH-sensitive and temporal-controlled polymeric micelles for effective combination therapy of doxorubicin and disulfiram. ACS Nano 7, 5858–5869 (2013).
Zhao, C. Y., Cheng, R., Yang, Z. & Tian, Z. M. Nanotechnology for cancer therapy based on chemotherapy. Molecules 23, 826 (2018).
Moulder, J. E. & Rockwell, S. Tumor hypoxia: its impact on cancer therapy. Cancer Metastasis Rev. 5, 313–341 (1987).
Castano, A. P., Mroz, P. & Hamblin, M. R. Photodynamic therapy and anti-tumour immunity. Nat. Rev. Cancer 6, 535–545 (2006).
Naylor, M. F., Chen, W. R., Teague, T. K., Perry, L. A. & Nordquist, R. E. In situ photoimmunotherapy: a tumour-directed treatment for melanoma. Br. J. Dermatol. 155, 1287–1292 (2006).
Mroz, P., Hashmi, J. T., Huang, Y. Y., Lang, N. & Hamblin, M. R. Stimulation of anti-tumor immunity by photodynamic therapy. Expert Rev. Clin. Immunol. 7, 75–91 (2011).
Chen, Q. et al. Photothermal therapy with immune-adjuvant nanoparticles together with checkpoint blockade for effective cancer immunotherapy. Nat. Commun. 7, 13193 (2016).
Santos, L. L., Oliveira, J., Monteiro, E., Santos, J. & Sarmento, C. Treatment of head and neck cancer with photodynamic therapy with redaporfin: a clinical case report. Case Rep. Oncol. 11, 769–776 (2018).
Acknowledgements
The work of the authors is supported by the National Research Foundation of Korea (NRF), which is funded by the Korean government Ministry of Science (grant 2012R1A3A2048814 to J.Y.), the US NIH (grants R01EB017270 and DP5OD017898 to J.F.L.), the US National Science Foundation (grant 1555220 to J.F.L.), and the Intramural Research Program (IRP) of the NIH’s National Institute of Biomedical Imaging and Bioengineering (NIBIB) (X.C.). The authors would like to thank Dr David Kessel for providing valuable feedback on the manuscript and Tian Guo and Rui Wang for their assistance in formatting the manuscript.
Reviewer information
Nature Reviews Clinical Oncology thanks Liang Cheng, Michael R. Hamblin, Zhuang Liu and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
X.L., J.F.L. and X.C. made substantial contributions to discussions of content, all authors contributed to the writing of the manuscript, and J.F.L., J.Y. and X.C. reviewed and/or edited the manuscript before submission.
Corresponding authors
Ethics declarations
Competing interests
J.F.L. holds stocks in POP Biotechnologies. The other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Chromophores
-
Light-absorbing molecules that impart colour.
- Photosensitizers
-
Chromophores that generate reactive oxygen species upon irradiation.
- Singlet state
-
A molecular quantum state in which all the electron spins are paired.
- Triplet state
-
A molecular quantum state in which an excited electron spin is unpaired.
- Fluence rate
-
The radiant energy incident per second crossing a sectional area of an irradiated spot, equating to the light power transferred per unit area, for example, in W/cm2 (1 W = 1 J/s).
- Total fluence
-
The total energy of light crossing a sectional area of an irradiated spot (exposed light energy per unit area, J/cm2).
- Aptamers
-
Oligonucleotides or peptides that bind to a specific target molecule.
- Absorption maxima
-
The specific wavelength of light that chromophores absorb most intensely.
- Two-photon excitation
-
Simultaneous excitation by two photons at double the excitation wavelength.
- Upconverting nanoparticles
-
Particles that convert near-infrared excitation light into visible and ultraviolet emission light.
- Quenching moiety
-
A molecule that attenuates the fluorescence or singlet oxygen generation of a fluorophore or photosensitizer.
Rights and permissions
About this article
Cite this article
Li, X., Lovell, J.F., Yoon, J. et al. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat Rev Clin Oncol 17, 657–674 (2020). https://doi.org/10.1038/s41571-020-0410-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41571-020-0410-2
This article is cited by
-
Biomimetic MDSCs membrane coated black phosphorus nanosheets system for photothermal therapy/photodynamic therapy synergized chemotherapy of cancer
Journal of Nanobiotechnology (2024)
-
A pH-responsive nanoplatform with dual-modality imaging for enhanced cancer phototherapy and diagnosis of lung metastasis
Journal of Nanobiotechnology (2024)
-
Recent advances in nanomaterial-driven strategies for diagnosis and therapy of vascular anomalies
Journal of Nanobiotechnology (2024)
-
A novel multifunctional microneedle patch for synergistic photothermal- gas therapy against maxillofacial malignant melanoma and associated skin defects
Journal of Nanobiotechnology (2024)
-
A TME-activated nano-catalyst for triple synergistic therapy of colorectal cancer
Scientific Reports (2024)