Abstract
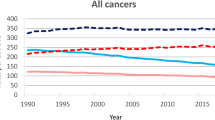
The cancer landscape of the USA is continually evolving owing to changing risk factor patterns and disease classifications, improvements in detection and treatment, and demographic changes, such as ageing and population growth. Monitoring the burden of cancer, including incidence and mortality, is a key tool for assessing progress, identifying emerging trends and setting priorities to reduce the burden. In this Perspective, we describe trends in cancer incidence and mortality in the USA overall, and for major cancer types, and describe the main contributing factors, including risk factors, screening, treatment and access to care. When relevant, we provide information based on sex and common classifications of race/ethnicity, socioeconomic status and geographical region. We then discuss the implications of the patterns of cancer incidence and mortality for cancer research, prevention and care.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 70, 7–30 (2020).
Henley, S. J. et al. Annual report to the nation on the status of cancer, part I: national cancer statistics. Cancer 124, 2785–2800 (2018).
National Institutes of Health Cancer Trends Progress Report. National Cancer Institute https://progressreport.cancer.gov (2019).
Heston, J. F., Cusano, M. M., Young, J. L. & National Cancer Institute. Forty-five years of cancer incidence in Connecticut: 1935–79. 1–706 (Department of Health and Human Services, 1986).
Freeman, H. P. Poverty, culture, and social injustice: determinants of cancer disparities. CA Cancer J. Clin. 54, 72–77 (2004).
White, M. C. et al. The history and use of cancer registry data by public health cancer control programs in the United States. Cancer 123 (Suppl. 24), 4969–4976 (2017).
Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: incidence–SEER 9 Regs research data, Nov 2018 Sub (1975–2016) –linked to county attributes–total U.S., 1969–2017 counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2019. SEER www.seer.cancer.gov (2019).
Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: mortality–all COD, total U.S. (1969–2017) –linked to county attributes–total U.S., 1969–2017 counties, National Cancer Institute, DCCPS, Surveillance Research Program, released May 2019. Underlying mortality data provided by NCHS (www.cdc.gov/nchs). SEER www.seer.cancer.gov (2019).
Howlader N. et al. (eds) SEER Cancer Statistics Review, 1975–2016 https://seer.cancer.gov/csr/1975_2016/ (National Cancer Institute, 2020).
US Census Bureau. Race & Ethnicity. US Census Bureau https://www.census.gov/mso/www/training/pdf/race-ethnicity-onepager.pdf (2017).
Murphy, S. L., Xu, J., Kochanek, K. D. & Arias, E. Mortality in the United States, 2017. NCHS Data Brief no. 328 (National Center for Health Statistics, 2018).
Colby, S. L. & Ortman, J. M. Projections of the size and composition of the U.S. population: 2014 to 2060. Current Population Reports P25-1143. (US Census Bureau, 2014).
Wingo, P. A., Tong, T. & Bolden, S. Cancer statistics, 1995. CA Cancer J. Clin. 45, 8–30 (1995).
Kochanek, K. D., Murphy, S. L., Xu, J. & Arias, E. Deaths: final data for 2017. Natl Vital. Stat. Rep. 68, 1–77 (2019).
National Center for Health Statistics. Health, United States, 2017: With special feature on mortality. (US Department of Health and Human Services, 2018).
Mokdad, A. H. et al. Trends and patterns of disparities in cancer mortality among US counties, 1980-2014. JAMA 317, 388–406 (2017).
Islami, F. et al. Potentially preventable premature lung cancer deaths in the USA if overall population rates were reduced to those of educated whites in lowerrisk states. Cancer Causes Control 26, 409–418 (2015).
Sineshaw, H. M., Ng, K., Flanders, W. D., Brawley, O. W. & Jemal, A. Factors that contribute to differences in survival of black vs white patients with colorectal cancer. Gastroenterology 154, 906–915 (2018).
Daly, B. & Olopade, O. I. A perfect storm: How tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J. Clin. 65, 221–238 (2015).
American Society of Clinical Oncology. The state of cancer care in America, 2017: a report by the American Society of Clinical Oncology. J. Oncol. Pract. 13, e353–e394 (2017).
Yabroff, K. R., Gansler, T., Wender, R. C., Cullen, K. J. & Brawley, O. W. Minimizing the burden of cancer in the United States: goals for a high-performing health care system. CA Cancer J. Clin. 69, 166–183 (2019).
Malvezzi, M. et al. European cancer mortality predictions for the year 2019 with focus on breast cancer. Ann. Oncol. 30, 781–787 (2019).
Cheng, E. S., Weber, M., Feletto, E., Smith, M. A. & Yu, X. Q. Cancer burden and control in Australia: lessons learnt and challenges remaining. Ann. Cancer Epidemiol. 2, 1–15 (2018).
Katanoda, K. et al. An updated report on the trends in cancer incidence and mortality in Japan, 1958–2013. Jpn. J. Clin. Oncol. 45, 390–401 (2015).
Lim, D., Ha, M. & Song, I. Trends in major cancer mortality in Korea, 1983–2012, with a joinpoint analysis. Cancer Epidemiol. 39, 939–946 (2015).
Thun, M., Peto, R., Boreham, J. & Lopez, A. D. Stages of the cigarette epidemic on entering its second century. Tob. Control 21, 96–101 (2012).
US Department of Health and Human Services. The Health Consequences of Smoking — 50 Years of Progress: a Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Ward, E. et al. Annual report to the nation on the status of cancer, 1999–2015, featuring cancer in men and women ages 20–49. J. Natl Cancer Inst. 111, 1279–1297 (2019).
Siegel, R. L. et al. Colorectal cancer statistics, 2020. CA Cancer J. Clin. https://doi.org/10.3322/caac.21601 (2020).
Sung, H., Siegel, R. L., Rosenberg, P. S. & Jemal, A. Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health 4, e137–e147 (2019).
Islami, F. et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J. Clin. 68, 31–54 (2018).
Amos, A. & Haglund, M. From social taboo to “torch of freedom”: the marketing of cigarettes to women. Tob. Control 9, 3–8 (2000).
Jemal, A. et al. Higher lung cancer incidence in young women than young men in the United States. N. Engl. J. Med. 378, 1999–2009 (2018).
Sauer, A. G., Siegel, R. L., Jemal, A. & Fedewa, S. A. Updated review of prevalence of major risk factors and use of screening tests for cancer in the United States. Cancer Epidemiol. Biomarkers Prev. 26, 1192–1208 (2017).
Lortet-Tieulent, J. et al. State-level cancer mortality attributable to cigarette smoking in the United States. JAMA Intern. Med. 176, 1792–1798 (2016).
Centers for Disease Control and Prevention. Underlying Cause of Death 1999–2017. CDC WONDER http://wonder.cdc.gov/ucd-icd10.html (accessed 2019).
Jemal, A. et al. Annual report to the nation on the status of cancer, 1975–2014, featuring survival. J. Natl Cancer Inst. 109, djx030 (2017).
Jemal, A. & Fedewa, S. A. Lung cancer screening with low-dose computed tomography in the United States-2010 to 2015. JAMA Oncol. 3, 1278–1281 (2017).
Jones, G. S. & Baldwin, D. R. Recent advances in the management of lung cancer. Clin. Med. 18, s41–s46 (2018).
Singh, G. K., Miller, B. A. & Hankey, B. F. Changing area socioeconomic patterns in U.S. cancer mortality, 1950–1998: part II–lung and colorectal cancers. J. Natl Cancer Inst. 94, 916–925 (2002).
Smith, R. A. et al. Cancer screening in the United States, 2019: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J. Clin. 69, 184–210 (2019).
Siegel, R. L., Miller, K. D. & Jemal, A. Colorectal cancer mortality rates in adults aged 20 to 54 years in the United States, 1970–2014. JAMA 318, 572–574 (2017).
Siegel, R. L. et al. Global patterns and trends in colorectal cancer incidence in young adults. Gut 68, 2179–2185 (2019).
Naishadham, D., Lansdorp-Vogelaar, I., Siegel, R., Cokkinides, V. & Jemal, A. State disparities in colorectal cancer mortality patterns in the United States. Cancer Epidemiol. Biomarkers Prev. 20, 1296–1302 (2011).
Jemal, A. et al. Inequalities in premature death from colorectal cancer by state. J. Clin. Oncol. 33, 829–835 (2015).
Neuhouser, M. L. et al. Overweight, obesity, and postmenopausal invasive breast cancer risk: a secondary analysis of the Women’s Health Initiative randomized clinical trials. JAMA Oncol. 1, 611–621 (2015).
Liu, Y., Nguyen, N. & Colditz, G. A. Links between alcohol consumption and breast cancer: a look at the evidence. Womens Health 11, 65–77 (2015).
DeSantis, C. E., Ma, J., Goding Sauer, A., Newman, L. A. & Jemal, A. Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J. Clin. 67, 439–448 (2017).
Grucza, R. A. et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: a meta-analysis of 6 national survey series. Alcohol. Clin. Exp. Res. 42, 1939–1950 (2018).
Waks, A. G. & Winer, E. P. Breast cancer treatment: a review. JAMA 321, 288–300 (2019).
Hsieh, M. C. et al. Population-based study on cancer subtypes, guideline-concordant adjuvant therapy, and survival among women with stage I–III breast cancer. J. Natl Compr. Canc. Netw. 17, 676–686 (2019).
Jemal, A. et al. Factors that contributed to black-white disparities in survival among nonelderly women with breast cancer between 2004 and 2013. J. Clin. Oncol. 36, 14–24 (2018).
Islami, F., Moreira, D. M., Boffetta, P. & Freedland, S. J. A systematic review and meta-analysis of tobacco use and prostate cancer mortality and incidence in prospective cohort studies. Eur. Urol. 66, 1054–1064 (2014).
Lauby-Secretan, B. et al. Body fatness and cancer–viewpoint of the IARC Working Group. N. Engl. J. Med. 375, 794–798 (2016).
Houston, K. A., King, J., Li, J. & Jemal, A. Trends in prostate cancer incidence rates and prevalence of prostate specific antigen screening by socioeconomic status and regions in the United States, 2004 to 2013. J. Urol. 199, 676–682 (2018).
Negoita, S. et al. Annual report to the nation on the status of cancer, part II: recent changes in prostate cancer trends and disease characteristics. Cancer 124, 2801–2814 (2018).
Kelly, S. P., Anderson, W. F., Rosenberg, P. S. & Cook, M. B. Past, current, and future incidence rates and burden of metastatic prostate cancer in the United States. Eur. Urol. Focus. 4, 121–127 (2018).
Ahlering, T. et al. Unintended consequences of decreased PSA-based prostate cancer screening. World J. Urol. 37, 489–496 (2019).
US Preventive Services Task Force. et al. Screening for prostate cancer: US preventive services task force recommendation statement. JAMA 319, 1901–1913 (2018).
Rebbeck, T. R. Prostate cancer genetics: variation by race, ethnicity, and geography. Semin. Radiat. Oncol. 27, 3–10 (2017).
Moses, K. A., Orom, H., Brasel, A., Gaddy, J. & Underwood, W. 3rd. Racial/ethnic disparity in treatment for prostate cancer: does cancer severity matter? Urology 99, 76–83 (2017).
Krimphove, M. J. et al. Evaluation of the contribution of demographics, access to health care, treatment, and tumor characteristics to racial differences in survival of advanced prostate cancer. Prostate Cancer Prostatic Dis. 22, 125–136 (2019).
Jacobs, E. J. et al. The association of body mass index with pancreatic cancer: variation by age at body mass index assessment. Am. J. Epidemiol. https://doi.org/10.1093/aje/kwz251 (2019).
Zohar, L. et al. Adolescent overweight and obesity and the risk for pancreatic cancer among men and women: a nationwide study of 1.79 million Israeli adolescents. Cancer 125, 118–126 (2019).
Tavakkoli, A. et al. Racial disparities and trends in pancreatic cancer incidence and mortality in the United States. Clin. Gastroenterol. Hepatol. 18, 171–178 (2019).
Makarova-Rusher, O. V. et al. Population attributable fractions of risk factors for hepatocellular carcinoma in the United States. Cancer 122, 1757–1765 (2016).
Kanwal, F. et al. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin. Gastroenterol. Hepatol. 14, 301–308 (2016).
Islami, F. et al. Disparities in liver cancer occurrence in the United States by race/ethnicity and state. CA Cancer J. Clin. 67, 273–289 (2017).
Moore, K. J., Gauri, A. & Koru-Sengul, T. Prevalence and sociodemographic disparities of hepatitis C in baby boomers and the US adult population. J. Infect. Public. Health 12, 32–36 (2019).
Hales, C. M., Fryar, C. D., Carroll, M. D., Freedman, D. S. & Ogden, C. L. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA 319, 1723–1725 (2018).
Allen, A. M. et al. Nonalcoholic fatty liver disease incidence and impact on metabolic burden and death: a 20 year-community study. Hepatology 67, 1726–1736 (2018).
Menke, A., Casagrande, S., Geiss, L. & Cowie, C. C. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA 314, 1021–1029 (2012).
Denniston, M. M. et al. Chronic hepatitis C virus infection in the United States, national health and nutrition examination survey 2003 to 2010. Ann. Intern. Med. 160, 293–300 (2014).
Kowdley, K. V., Wang, C. C., Welch, S., Roberts, H. & Brosgart, C. L. Prevalence of chronic hepatitis B among foreign-born persons living in the United States by country of origin. Hepatology 56, 422–433 (2012).
Roberts, H. et al. Prevalence of chronic hepatitis B virus (HBV) infection in U.S. households: national health and nutrition examination survey (NHANES), 1988–2012. Hepatology 63, 388–397 (2016).
Clarke, M. A., Devesa, S. S., Harvey, S. V. & Wentzensen, N. Hysterectomy-corrected uterine corpus cancer incidence trends and differences in relative survival reveal racial disparities and rising rates of nonendometrioid cancers. J. Clin. Oncol. 37, 1895–1908 (2019).
Henley, S. J., Miller, J. W., Dowling, N. F., Benard, V. B. & Richardson, L. C. Uterine cancer incidence and mortality - United States, 1999–2016. MMWR Morb. Mortal. Wkly Rep. 67, 1333–1338 (2018).
Welch, H. G., Skinner, J. S., Schroeck, F. R., Zhou, W. & Black, W. C. Regional variation of computed tomographic imaging in the United States and the risk of nephrectomy. JAMA Intern. Med. 178, 221–227 (2018).
Choueiri, T. K. & Motzer, R. J. Systemic therapy for metastatic renal-cell carcinoma. N. Engl. J. Med. 376, 354–366 (2017).
Guy, G. P. Jr. et al. Vital signs: melanoma incidence and mortality trends and projections - United States, 1982–2030. Morb. Mortal. Wkly Rep. 64, 591–596 (2015).
Shaikh, W. R. et al. Melanoma thickness and survival trends in the United States, 1989 to 2009. J. Natl Cancer Inst. 108, djv294 (2016).
Thrift, A. P. & Gudenkauf, F. J. Melanoma incidence among non-Hispanic whites in all 50 United States from 2001 through 2015. J. Natl Cancer Inst. 112, 533–539 (2019).
Holman, D. M. et al. Prevalence of sun protection use and sunburn and association of demographic and behaviorial characteristics with sunburn among US adults. JAMA Dermatol. 154, 561–568 (2018).
Islami, F. et al. Cutaneous melanomas attributable to ultraviolet radiation exposure by state. Int. J. Cancer https://doi.org/10.1002/ijc.32921 (2020).
Lim, H., Devesa, S. S., Sosa, J. A., Check, D. & Kitahara, C. M. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA 317, 1338–1348 (2017).
Shi, L. L., DeSantis, C., Jemal, A. & Chen, A. Y. Changes in thyroid cancer incidence, post-2009 American Thyroid Association guidelines. Laryngoscope 127, 2437–2441 (2017).
Van Dyne, E. A. et al. Trends in human papillomavirus-associated cancers – United States, 1999–2015. Morb. Mortal. Wkly Rep. 67, 918–924 (2018).
Islami, F., Ferlay, J., Lortet-Tieulent, J., Bray, F. & Jemal, A. International trends in anal cancer incidence rates. Int. J. Epidemiol. 46, 924–938 (2017).
Berman, T. A. & Schiller, J. T. Human papillomavirus in cervical cancer and oropharyngeal cancer: one cause, two diseases. Cancer 123, 2219–2229 (2017).
Islami, F., Fedewa, S. A. & Jemal, A. Trends in cervical cancer incidence rates by age, race/ethnicity, histological subtype, and stage at diagnosis in the United States. Prev. Med. 123, 316–323 (2019).
Ronco, G. et al. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet 383, 524–532 (2014).
McClung, N. M. et al. Estimated number of cases of high-grade cervical lesions diagnosed among women – United States, 2008 and 2016. Morb. Mortal. Wkly Rep. 68, 337–343 (2019).
Steele, C. B. et al. Vital signs: trends in incidence of cancers associated with overweight and obesity – United States, 2005–2014. Morb. Mortal. Wkly Rep. 66, 1052–1058 (2017).
Islami, F., DeSantis, C. E. & Jemal, A. Incidence trends of esophageal and gastric cancer subtypes by race, ethnicity, and age in the United States, 1997–2014. Clin. Gastroenterol. Hepatol. 17, 429–439 (2019).
Ward, E., DeSantis, C., Robbins, A., Kohler, B. & Jemal, A. Childhood and adolescent cancer statistics, 2014. CA Cancer J. Clin. 64, 83–103 (2014).
Freireich, E. J., Wiernik, P. H. & Steensma, D. P. The leukemias: a half-century of discovery. J. Clin. Oncol. 32, 3463–3469 (2014).
IARC Working Group. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, vol 100 E: Personal Habits and Indoor Combustions (IARC, 2012).
World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project Expert Report 2018. Meat, fish and dairy products and the risk of cancer. World Cancer Research Fund Network https://www.wcrf.org/sites/default/files/Meat-Fish-and-Dairy-products.pdf (2018).
World Cancer Research Fund/American Institute for Cancer Research. Continuous Update Project Expert Report 2018. Wholegrains, vegetable and fruit and the risk of cancer. World Cancer Research Fund Network https://www.wcrf.org/sites/default/files/wholegrains-veg-and-fruit.pdf (2018)
US Department of Health and Human Services. 2018 Physical Activity Guidelines Advisory Committee Scientific Report (US Department of Health and Human Services, 2018).
IARC Working Group. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, vol. 100 D: Radiation (IARC, 2012).
IARC Working Group. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, vol. 100 B: Biological Agents (IARC, 2012).
IARC Working Group. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, vol. 109: Outdoor air pollution (IARC, 2016).
IARC Working Group. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, vol, 100 C: Arsenic, Metals, Fibres, and Dusts (IARC, 2012).
Song, M. & Giovannucci, E. Preventable incidence and mortality of carcinoma associated with lifestyle factors among white adults in the United States. JAMA Oncol. 2, 1154–1161 (2016).
Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs - 2014 (US Department of Health and Human Services, 2014).
American Cancer Society. How do you measure up? A progress report on state legislative activity to reduce cancer incidence and mortality, 17th edn. Cancer Action Network https://www.fightcancer.org/how-do-you-measure-up (2019).
Campaign for Tobacco-Free Kids. State excise and sales taxes per pack of cigarettes. Campaign for Tobacco-Free Kids https://www.tobaccofreekids.org/assets/factsheets/0202.pdf (2020).
Centers for Disease Control and Prevention. State Tobacco Activities Tracking and Evaluation (STATE) system. Legislation–smokefree indoor air; updated April 23, 2020. CDC https://data.cdc.gov/Legislation/CDC-STATE-System-Tobacco-Legislation-Smokefree-Ind/2snk-eav4/data (2020).
Tsai, J. et al. Exposure to secondhand smoke among nonsmokers - United States, 1988–2014. Morb. Mortal. Wkly Rep. 67, 1342–1346 (2018).
Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. Executive Summary https://www.ncbi.nlm.nih.gov/books/NBK63956 (US Department of Health and Human Services, 2008).
Jamal, A. et al. Tobacco use screening and counseling during physician office visits among adults–National Ambulatory Medical Care Survey and National Health Interview Survey, United States, 2005–2009. MMWR Suppl. 61, 38–45 (2012).
Rosenbaum, S. The Patient Protection and Affordable Care Act: implications for public health policy and practice. Public. Health Rep. 126, 130–135 (2011).
Drope, J. et al. Key issues surrounding the health impacts of electronic nicotine delivery systems (ENDS) and other sources of nicotine. CA Cancer J. Clin. 67, 449–471 (2017).
Watkins, S. L., Glantz, S. A. & Chaffee, B. W. Association of noncigarette tobacco product use with future cigarette smoking among youth in the Population Assessment of Tobacco and Health (PATH) study, 2013–2015. JAMA Pediatr. 172, 181–187 (2018).
Cullen, K. A. et al. e-Cigarette use among youth in the United States, 2019. JAMA 322, 2095–2103 (2019).
Drazen, J. M., Morrissey, S. & Campion, E. W. The dangerous flavors of e-cigarettes. N. Engl. J. Med. 380, 679–680 (2019).
US Food and Drug Administration. FDA finalizes enforcement policy on unauthorized flavored cartridge-based e-cigarettes that appeal to children, including fruit and mint. FDA https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children (2020).
Kohler, L. N. et al. Adherence to diet and physical activity cancer prevention guidelines and cancer outcomes: a systematic review. Cancer Epidemiol. Biomarkers Prev. 25, 1018–1028 (2016).
Khan, L. K. et al. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm. Rep. 58, 1–26 (2009).
Muhammad, A., Meade, B., Marquardt, D. R. & Mozaffarian, D. Global patterns in price elasticities of sugar-sweetened beverage intake and potential effectiveness of tax policy: a cross-sectional study of 164 countries by sex, age and global-income decile. BMJ Open. 9, e026390 (2019).
Teng, A. M. et al. Impact of sugar-sweetened beverage taxes on purchases and dietary intake: systematic review and meta-analysis. Obes. Rev. 20, 1187–1204 (2019).
US Preventive Services Task Force. et al. Screening for obesity in children and adolescents: U.S. preventive services task force recommendation statement. JAMA 317, 2417–2426 (2017).
US Preventive Services Task Force et al. Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US Preventive Services Task Force recommendation statement. JAMA 320, 1163–1171 (2018).
Wadden, T. A., Butryn, M. L., Hong, P. S. & Tsai, A. G. Behavioral treatment of obesity in patients encountered in primary care settings: a systematic review. JAMA 312, 1779–1791 (2014).
Alamuddin, N., Bakizada, Z. & Wadden, T. A. Management of obesity. J. Clin. Oncol. 34, 4295–4305 (2016).
US Department of Health and Human Services. Helping patients who drink too much: a clinician’s guide (US Department of Health and Human Services, 2005).
Keyes, K. M., Shev, A., Tracy, M. & Cerda, M. Assessing the impact of alcohol taxation on rates of violent victimization in a large urban area: an agent-based modeling approach. Addiction 114, 236–247 (2019).
National Institute on Alcohol Abuse and Alcoholism. Strategic Plan 2017–2021 (NIAAA, 2017).
Knox, J., Hasin, D. S., Larson, F. R. R. & Kranzler, H. R. Prevention, screening, and treatment for heavy drinking and alcohol use disorder. Lancet Psychiatry 6, 1054–1067 (2019).
US Department of Health and Human Services. The Surgeon General’s Call to Action to Prevent Skin Cancer (US Department of Health and Human Services, 2014).
Iannacone, M. R., Youlden, D. R., Baade, P. D., Aitken, J. F. & Green, A. C. Melanoma incidence trends and survival in adolescents and young adults in Queensland, Australia. Int. J. Cancer 136, 603–609 (2015).
Guy, G. P. Jr. et al. Trends in indoor tanning and its association with sunburn among US adults. J. Am. Acad. Dermatol. 76, 1191–1193 (2017).
Kann, L. et al. Youth risk behavior surveillance - United States, 2017. MMWR Surveill. Summ. 67, 1–114 (2018).
US Preventive Services Task Force. et al. Behavioral counseling to prevent skin cancer: US Preventive Services Task Force recommendation statement. JAMA 319, 1134–1142 (2018).
Jemal, A. et al. Annual report to the nation on the status of cancer, 1975–2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. J. Natl Cancer Inst. 105, 175–201 (2013).
Hernandez-Ramirez, R. U., Shiels, M. S., Dubrow, R. & Engels, E. A. Cancer risk in HIV-infected people in the USA from 1996 to 2012: a population-based, registry-linkage study. Lancet HIV. 4, e495–e504 (2017).
Centers for Disease Control and Prevention. Human papillomavirus (HPV) vaccination coverage among adolescents 13–17 years by State, HHS Region, and the United States, National Immunization Survey-Teen (NIS-Teen), 2018. CDC https://www.cdc.gov/vaccines/imz-managers/coverage/teenvaxview/data-reports/hpv/reports/2018.html (2019).
Jemal, A. & Fedewa, S. A. Recent hepatitis C virus testing patterns among baby boomers. Am. J. Prev. Med. 53, e31–e33 (2017).
Lo, Re,V. 3rd. et al. Disparities in absolute denial of modern hepatitis C therapy by type of insurance. Clin. Gastroenterol. Hepatol. 14, 1035–1043 (2016).
Zibbell, J. E. et al. Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. Am. J. Public. Health 108, 175–181 (2018).
Morse, A., Barritt, A. S. & Jhaveri, R. Individual state hepatitis C data supports expanding screening beyond baby boomers to all adults. Gastroenterology 154, 1850–1851 (2018).
Jaffee, E. M. et al. Future cancer research priorities in the USA: a Lancet Oncology Commission. Lancet Oncol. 18, e653–e706 (2017).
Polite, B. N. et al. Charting the future of cancer health disparities research: a position statement from the American Association for Cancer Research, the American Cancer Society, the American Society of Clinical Oncology, and the National Cancer Institute. CA Cancer J. Clin. 67, 353–361 (2017).
National Institutes of Health. Cancer Moonshot Blue Ribbon Panel report 2016. National Cancer Institute https://www.cancer.gov/research/key-initiatives/moonshot-cancer-initiative/blue-ribbon-panel/blue-ribbon-panel-report-2016.pdf (2016).
McColl, E. R., Asthana, R., Paine, M. F. & Piquette-Miller, M. The age of omics-driven precision medicine. Clin. Pharmacol. Ther. 106, 477–481 (2019).
Wild, C. P. The exposome: from concept to utility. Int. J. Epidemiol. 41, 24–32 (2012).
US Preventive Services Task Force. et al. Screening for pancreatic cancer: US preventive services task force reaffirmation recommendation statement. JAMA 322, 438–444 (2019).
Schiffman, J. D., Fisher, P. G. & Gibbs, P. Early detection of cancer: past, present, and future. Am. Soc. Clin. Oncol. Educ. Book 35, 57–65 (2015).
US Preventive Services Task Force. et al. Screening for cervical cancer: US preventive services task force recommendation statement. JAMA 320, 674–686 (2018).
Menon, U. et al. Risk algorithm using serial biomarker measurements doubles the number of screen-detected cancers compared with a single-threshold rule in the United Kingdom Collaborative Trial of Ovarian Cancer Screening. J. Clin. Oncol. 33, 2062–2071 (2015).
Cohen, J. D. et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 359, 926–930 (2018).
Heitzer, E., Haque, I. S., Roberts, C. E. S. & Speicher, M. R. Current and future perspectives of liquid biopsies in genomics-driven oncology. Nat. Rev. Genet. 20, 71–88 (2019).
Mariotto, A. B., Etzioni, R., Hurlbert, M., Penberthy, L. & Mayer, M. Estimation of the number of women living with metastatic breast cancer in the United States. Cancer Epidemiol. Biomarkers Prev. 26, 809–815 (2017).
Conforti, F. et al. Cancer immunotherapy efficacy and patients’ sex: a systematic review and meta-analysis. Lancet Oncol. 19, 737–746 (2018).
Perez-Ruiz, E. et al. Prophylactic TNF blockade uncouples efficacy and toxicity in dual CTLA-4 and PD-1 immunotherapy. Nature 569, 428–432 (2019).
Chen, Y., Wang, H., Kantarjian, H. & Cortes, J. Trends in chronic myeloid leukemia incidence and survival in the United States from 1975 to 2009. Leuk. Lymphoma 54, 1411–1417 (2013).
Marquart, J., Chen, E. Y. & Prasad, V. Estimation of the percentage of US patients with cancer who benefit from genome-driven oncology. JAMA Oncol. 4, 1093–1098 (2018).
Joyner, M. J. & Paneth, N. Promises, promises, and precision medicine. J. Clin. Invest. 129, 946–948 (2019).
Khoury, M. J. et al. A collaborative translational research framework for evaluating and implementing the appropriate use of human genome sequencing to improve health. PLoS Med. 15, e1002631 (2018).
All of Us Research Program Investigators. et al. The “All of Us” research program. N. Engl. J. Med. 381, 668–676 (2019).
Pal, S. K. et al. Clinical cancer advances 2019: annual report on progress against cancer from the American Society of Clinical Oncology. J. Clin. Oncol. 37, 834–849 (2019).
Kotecha, R. R., Motzer, R. J. & Voss, M. H. Towards individualized therapy for metastatic renal cell carcinoma. Nat. Rev. Clin. Oncol. 16, 621–633 (2019).
Le Tourneau, C., Borcoman, E. & Kamal, M. Molecular profiling in precision medicine oncology. Nat. Med. 25, 711–712 (2019).
Pantel, K. & Alix-Panabieres, C. Liquid biopsy and minimal residual disease — latest advances and implications for cure. Nat. Rev. Clin. Oncol. 16, 409–424 (2019).
White, A. et al. Cancer screening test use — United States, 2015. Morb. Mortal. Wkly Rep. 66, 201–206 (2017).
Doubeni, C. A. et al. Timely follow-up of positive cancer screening results: a systematic review and recommendations from the PROSPR Consortium. CA Cancer J. Clin. 68, 199–216 (2018).
Peters, D. H., Adam, T., Alonge, O., Agyepong, I. A. & Tran, N. Implementation research: what it is and how to do it. BMJ 347, f6753 (2013).
Briant, K. J. et al. Using a culturally tailored intervention to increase colorectal cancer knowledge and screening among Hispanics in a rural community. Cancer Epidemiol. Biomarkers Prev. 27, 1283–1288 (2018).
Champion, V. L. et al. A randomized trial to compare a tailored web-based intervention and tailored phone counseling to usual care for increasing colorectal cancer screening. Cancer Epidemiol. Biomarkers Prev. 27, 1433–1441 (2018).
Nebraska Department of Health and Human Services. Immunization Program, 2018 legislative report. https://nebraskalegislature.gov/FloorDocs/105/PDF/Agencies/Health_and_Human_Services__Department_of/497_20181221-142336.pdf (2018).
Institute of Medicine. Best Care at Lower Cost: The Path to Continuous Learning Health Care in America (National Academies Press, 2013).
Qin, J., Saraiya, M., Martinez, G. & Sawaya, G. F. Prevalence of potentially unnecessary bimanual pelvic examinations and papanicolaou tests among adolescent girls and young women aged 15–20 years in the United States. JAMA Intern. Med. 180, 274–280 (2020).
Sineshaw, H. M. et al. Treatment patterns among de novo metastatic cancer patients who died within 1 month of diagnosis. JNCI Cancer Spectr. 3, pkz021 (2019).
Norton, W. E., Chambers, D. A. & Kramer, B. S. Conceptualizing de-implementation in cancer care delivery. J. Clin. Oncol. 37, 93–96 (2019).
National Academies of Sciences, Engineering, and Medicine. Long-Term Survivorship Care After Cancer Treatment: Proceedings of a Workshop (The National Academies Press, 2018).
Alfano, C. M., Jefford, M., Maher, J., Birken, S. A. & Mayer, D. K. Building personalized cancer follow-up care pathways in the united states: lessons learned from implementation in England, Northern Ireland, and Australia. Am. Soc. Clin. Oncol. Educ. Book. 39, 625–639 (2019).
Yang, W. et al. Projected supply of and demand for oncologists and radiation oncologists through 2025: an aging, better-insured population will result in shortage. J. Oncol. Pract. 10, 39–45 (2014).
Rubin, G. et al. The expanding role of primary care in cancer control. Lancet Oncol. 16, 1231–1272 (2015).
Halpern, M. T. & Argenbright, K. E. Evaluation of effectiveness of survivorship programmes: how to measure success? Lancet Oncol. 18, e51–e59 (2017).
Ward, E. et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J. Clin. 58, 9–31 (2008).
Halpern, M. T. et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol. 9, 222–231 (2008).
Dickman, S. L., Himmelstein, D. U. & Woolhandler, S. Inequality and the health-care system in the USA. Lancet 389, 1431–1441 (2017).
Ramsey, S. et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff. 32, 1143–1152 (2013).
Han, X. et al. Changes in noninsurance and care unaffordability among cancer survivors following the Affordable Care Act. J. Natl Cancer Inst. https://doi.org/10.1093/jnci/djz218 (2019).
Mazurenko, O., Balio, C. P., Agarwal, R., Carroll, A. E. & Menachemi, N. The effects of Medicaid expansion under the ACA: a systematic review. Health Aff. 37, 944–950 (2018).
Guth, M., Garfield, R. & Rudowitz, R. The effects of Medicaid expansion under the ACA: updated findings from a literature review. Kaiser Family Foundation http://files.kff.org/attachment/Report-The-Effects-of-Medicaid-Expansion-under-the-ACA-Updated-Findings-from-a-Literature-Review.pdf (2020).
Kaiser Family Foundation. Status of state action on the Medicaid expansion decision. Updated January 10, 2020. Kaiser Family Foundation https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act (2020).
Sommers, B. D., Long, S. K. & Baicker, K. Changes in mortality after Massachusetts health care reform: a quasi-experimental study. Ann. Intern. Med. 160, 585–593 (2014).
Sabik, L. M. et al. The Impact of Massachusetts health reform on colorectal and breast cancer stage at diagnosis. Med. Care 58, 183–191 (2020).
Grubbs, S. S. et al. Eliminating racial disparities in colorectal cancer in the real world: it took a village. J. Clin. Oncol. 31, 1928–1930 (2013).
Acknowledgements
This work was supported by the Intramural Research Department of the American Cancer Society.
Author information
Authors and Affiliations
Contributions
All authors made a substantial contribution to all aspects of the preparation of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors are employed by the American Cancer Society, which receives grants from private and corporate foundations, including foundations associated with companies in the health-care sector for research outside of the submitted work. The authors are not funded by any of these grants and their salaries are solely funded through American Cancer Society funds.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Cancer Statistics Center: https://cancerstatisticscenter.cancer.org/
Supplementary information
Rights and permissions
About this article
Cite this article
Islami, F., Siegel, R.L. & Jemal, A. The changing landscape of cancer in the USA — opportunities for advancing prevention and treatment. Nat Rev Clin Oncol 17, 631–649 (2020). https://doi.org/10.1038/s41571-020-0378-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41571-020-0378-y
This article is cited by
-
Cause-specific mortality in a population-level cohort of diffuse large B-cell lymphoma following chemotherapy in the early 21st century
Annals of Hematology (2024)
-
Proteomic characterization of primary and metastatic prostate cancer reveals reduced proteinase activity in aggressive tumors
Scientific Reports (2021)