Abstract
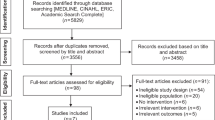
In the past decade, the introduction of molecularly targeted agents and immune-checkpoint inhibitors has led to improved survival outcomes for patients with advanced-stage lung cancer; however, this disease remains the leading cause of cancer-related mortality worldwide. Two large randomized controlled trials of low-dose CT (LDCT)-based lung cancer screening in high-risk populations — the US National Lung Screening Trial (NLST) and NELSON — have provided evidence of a statistically significant mortality reduction in patients. LDCT-based screening programmes for individuals at a high risk of lung cancer have already been implemented in the USA. Furthermore, implementation programmes are currently underway in the UK following the success of the UK Lung Cancer Screening (UKLS) trial, which included the Liverpool Health Lung Project, Manchester Lung Health Check, the Lung Screen Uptake Trial, the West London Lung Cancer Screening pilot and the Yorkshire Lung Screening trial. In this Review, we focus on the current evidence on LDCT-based lung cancer screening and discuss the clinical developments in high-risk populations worldwide; additionally, we address aspects such as cost-effectiveness. We present a framework to define the scope of future implementation research on lung cancer screening programmes referred to as Screening Planning and Implementation RAtionale for Lung cancer (SPIRAL).
Key points
-
The role of CT lung cancer screening on lung cancer-related mortality reduction has been under debate for five decades and is now an evidence-based reality.
-
The implementation of low-dose CT (LDCT)-based screening requires an optimal risk modelling methodology in order to select the high-risk population that will derive the greatest benefits.
-
Biomarkers have the potential to be included in future risk assessment models and work-up of CT nodules; laboratory tests should be developed to improve risk assessment before CT screening.
-
LDCT-based lung nodule diameter measurement cannot be used as an imaging biomarker for effective lung cancer risk stratification; however, volume doubling time can effectively be used as an imaging biomarker to rule out lesions with benign tissue growth.
-
The LDCT lung cancer screening interval should eventually be tailored to the expected mean nodule growth of the targeted population, starting with personalized screening, to improve screening performance (in particular for women).
-
Effective smoking cessation interventions must be integrated within cost-effective lung cancer screening programmes.
-
We propose a framework — the Screening Planning and Implementation RAtionale for Lung cancer (SPIRAL) — to define the scope of future implementation research on lung cancer screening programmes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68, 394–424 (2018).
Camidge, D. R., Doebele, R. C. & Kerr, K. M. Comparing and contrasting predictive biomarkers for immunotherapy and targeted therapy of NSCLC. Nat. Rev. Clin. Oncol. 16, 341–355 (2019).
Goldstraw, P. et al. International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee, Advisory Boards, and Participating Institutions; International Association for the Study of Lung Cancer Staging and Prognostic Factors Committee Advisory Boards and Participating Institutions. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 11, 39–51 (2016).
Aberle, D. R. et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 365, 395–409 (2011).
Koning, H. D. E., Van Der Aalst, C. & K. Ten Haaf, M. Oudkerk, PL02.05 effects of volume CT lung cancer screening: mortality results of the NELSON Randomised-Controlled Population Based Trial. J. Thorac. Oncol. 13, S185 (2018).
Becker, N. et al. Lung cancer mortality reduction by LDCT screening — Results from the randomized German LUSI trial. Int. J. Cancer 146, 1503–1513 (2020).
Pastorino, U. et al. Prolonged lung cancer screening reduced 10-year mortality in the MILD trial: new confirmation of lung cancer screening efficacy. Ann. Oncol. 30, 1162–1169 (2019).
Infante, M. et al. Long-term follow-up results of the DANTE trial, a randomized study of lung cancer screening with spiral computed tomography. Am. J. Respir. Crit. Care Med. 191, 1166–1175 (2015).
Paci, E. et al. Mortality, survival and incidence rates in the ITALUNG randomised lung cancer screening trial. Thorax 72, 825–831 (2017).
de Koning, H. J. et al. Oudkerk, reduced lung-cancer mortality with volume CT screening in a randomized trial. N. Engl. J. Med. https://doi.org/10.1056/nejmoa1911793 (2020).
Field, J. K. et al. UK Lung Cancer RCT Pilot Screening Trial: baseline findings from the screening arm provide evidence for the potential implementation of lung cancer screening. Thorax 71, 161–170 (2016).
Tammemägi, M. C. et al. Participant selection for lung cancer screening by risk modelling (the Pan-Canadian Early Detection of Lung Cancer [PanCan] study): a single-arm, prospective study. Lancet Oncol. 18, 1523–31. (2017).
Henschke, C. I. et al. Survival of patients with stage I lung cancer detected on CT screening. N. Engl. J. Med. 355, 1763–1771 (2006).
Villeneuve, P. J. Lifetime probability of developing lung cancer, by smoking status, Canada. Can. J. Public Health 85, 385–388 (1994).
Bruder, C. et al. Estimating lifetime and 10-year risk of lung cancer. Prev. Med. Reports 11, 125–130 (2018).
Oudkerk, M. et al. European position statement on lung cancer screening. Lancet Oncol. 18, e754–e766 (2017).
Ghimire, B. et al. Evaluation of a health service adopting proactive approach to reduce high risk of lung cancer: The Liverpool Healthy Lung Programme. Lung Cancer 134, 66–71 (2019).
Crosbie, P. A. et al. Implementing lung cancer screening: baseline results from a community-based “Lung Health Check” pilot in deprived areas of Manchester. Thorax 74, 405–409 (2019).
Bartlett, E. C. et al. Baseline results of the West London lung cancer screening pilot study – Impact of mobile scanners and dual risk model utilisation. Lung Cancer 148, 12–19 (2020).
ISRCTN Registry The Yorkshire Lung Screening Trial- ISRCTN42704678. https://doi.org/10.1186/ISRCTN42704678 (2019).
Raji, O. Y. et al. Predictive accuracy of the Liverpool Lung Project risk model for stratifying patients for computed tomography screening for lung cancer: a case-control and cohort validation study. Ann. Intern. Med. 157, 242–250 (2012).
Ten Haaf, K. et al. Risk prediction models for selection of lung cancer screening candidates: A retrospective validation study. PLoS Med. 14, e1002277 (2017).
Tammemägi, M. C. et al. Development and validation of a multivariable lung cancer risk prediction model that includes low-dose computed tomography screening results. JAMA Netw. Open 2, e190204. (2019).
Cassidy, A. et al. The LLP risk model: an individual risk prediction model for lung cancer. Br. J. Cancer. 98, 270–276 (2008).
Tammemagi, M. C. et al. Selection criteria for lung-cancer screening. N. Engl. J. Med. 368, 728–736 (2013).
Kovalchik, S. A. et al. Targeting of low-dose CT screening according to the risk of lung-cancer death. N. Engl. J. Med. 369, 245–254 (2013).
Katki, H. A., Kovalchik, S. A., Berg, C. D., Cheung, L. C. & Chaturvedi, A. K. Development and validation of risk models to select ever-smokers for ct lung cancer screening. JAMA 315, 2300–2311 (2016).
Field, J. K. et al. The UK lung cancer screening trial: a pilot randomised controlled trial of low-dose computed tomography screening for the early detection of lung cancer. Health Technol. Assess. 20, 1–146 (2016).
US-National-Libary-Medicine. ClinicalTrials.gov https://www.clinicaltrials.gov/ct2/show/NCT03934866 (2018).
NHS-England National-Cancer-Programme. Targeted Screening for Lung Cancer with Low Radiation Dose Computed Tomography https://www.england.nhs.uk/wp-content/uploads/2019/02/targeted-lung-health-checks-standard-protocol-v1.pdf (2019).
Ten Haaf, K. et al. A comparative modeling analysis of risk-based lung cancer screening strategies. J. Natl Cancer Inst. 112, 466–479 (2020).
Gordon, W. J., Landman, A., Zhang, H. & Bates, D. W. Beyond validation: getting health apps into clinical practice. NPJ Digit. Med. https://doi.org/10.1038/s41746-019-0212-z (2020).
Seijo, L. M. et al. Biomarkers in lung cancer screening: achievements, promises, and challenges. J. Thorac. Oncol. 14, 343–357 (2019).
Amos, C. I., Brennan, P. J., Hung, R. J. & Lin, X. Integrative analysis of lung cancer etiology and risk. Grantome.com https://grantome.com/grant/NIH/U19-CA203654-01A1 (2017).
Kachuri, L. et al. Immune-mediated genetic pathways resulting in pulmonary function impairment increase lung cancer susceptibility. Nat. Commun. https://doi.org/10.1038/s41467-019-13855-2 (2020).
Liu, Y. et al. Rare variants in known susceptibility loci and their contribution to risk of lung cancer. J. Thorac. Oncol. 13, 1483–1495 (2018).
Ji, X. et al. Identification of susceptibility pathways for the role of chromosome 15q25.1 in modifying lung cancer risk. Nat. Commun. 9, 3221 (2018).
Guida, F. et al. Assessment of lung cancer risk on the basis of a biomarker panel of circulating proteins. JAMA Oncol. 4, e182078 (2018).
Accomasso, L., Cristallini, C. & Giachino, C. Risk assessment and risk minimization in nanomedicine: A need for predictive, alternative, and 3Rs strategies. Front. Pharmacol. 9, 228 (2018).
Pham, D., Bhandari, S., Pinkston, C., Oechsli, M. & Kloecker, G. Lung cancer screening registry reveals low-dose CT screening remains heavily underutilized. Clin. Lung Cancer 21, e206–e211 (2020).
van der Aalst, C. M., Ten Haaf, K. & de Koning, H. J. Lung cancer screening: latest developments and unanswered questions. Lancet Respir. Med. 4, 749–761 (2016).
Ali, N. et al. Barriers to uptake among high-risk individuals declining participation in lung cancer screening: a mixed methods analysis of the UK lung cancer screening (UKLS) trial. BMJ Open 5, e008254 (2015).
McRonald, F. E. et al. The UK Lung Screen (UKLS): Demographic profile of first 88,897 approaches provides recommendations for population screening. Cancer Prev. Res. 7, 362–371 (2014).
Cassim, S. et al. Patient and carer perceived barriers to early presentation and diagnosis of lung cancer: a systematic review. BMC Cancer 19, 25 (2019).
National Lung Screening Trial Research Team. et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 365, 395–409 (2011).
van Klaveren, R. J. et al. Management of lung nodules detected by volume CT scanning. N. Engl. J. Med. 361, 2221–2229 (2009).
Field, J. K., Duffy, S. W., Devaraj, A. & Baldwin, D. R. Implementation planning for lung cancer screening: five major challenges. Lancet Respir. Med. 4, 685–687 (2016).
Fontana, R. S. et al. Lung cancer screening: the Mayo program. J. Occup. Med. 28, 746–750 (1986).
Oken, M. M. et al. Screening by chest radiograph and lung cancer mortality: The Prostate, Lung, Colorectal, and Ovarian (PLCO) randomized trial. JAMA 306, 1865–1873 (2011).
American College of Radiology and Radiological Society of North America. Radiation Dose in X-Ray and CT Exams https://www.radiologyinfo.org/en/pdf/safety-xray.pdf (2019).
Field, J. K. et al. European randomized lung cancer screening trials: Post NLST. J. Surg. Oncol. 108, 280–286 (2013).
Han, D. et al. An update on the European lung cancer screening trials and comparison of lung cancer screening recommendations in Europe. J. Thorac. Imaging 34, 65–71 (2019).
American College of Radiology. Lung-RADS Version 1.1 https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads (2019).
Smith, R. A. et al. Cancer screening in the United States, 2017: a review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J. Clin. 67, 100–121 (2017).
Walter, J. E. et al. Occurrence and lung cancer probability of new solid nodules at incidence screening with low-dose CT: analysis of data from the randomised, controlled NELSON trial. Lancet Oncol. 17, 907–916 (2016).
Wilson, D. O. et al. The Pittsburgh Lung Screening Study (PLuSS): outcomes within 3 years of a first computed tomography scan. Am. J. Respir. Crit. Care Med. 178, 956–961 (2008).
Swensen, S. J. et al. CT screening for lung cancer: five-year prospective experience. Radiology 235, 259–265 (2005).
van Klaveren, R. J. et al. Management of lung nodules detected by volume CT scanning. N. Engl. J. Med. 361, 2221–2229 (2009).
Henschke, C. I. et al. Early lung cancer action project: overall design and findings from baseline screening. Lancet 354, 99–105 (1999).
Pedersen, J. H. et al. The Danish randomized lung cancer CT screening trial–overall design and results of the prevalence round. J. Thorac. Oncol. 4, 608–614 (2009).
The National Lung Screening Trial Research Team. Results of initial low-dose computed tomographic screening for lung cancer. N. Engl. J. Med. 368, 1980–1991 (2013).
Henschke, C. I. et al. Survival of patients with stage I lung cancer detected on CT screening. N. Engl. J. Med. 355, 1763–1771 (2006).
Lopes Pegna, A. et al. Design, recruitment and baseline results of the ITALUNG trial for lung cancer screening with low-dose CT. Lung Cancer 64, 34–40 (2009).
Becker, N. et al. Randomized study on early detection of lung cancer with MSCT in Germany: study design and results of the first screening round. J. Cancer Res. Clin. Oncol. 138, 1475–1486 (2012).
Henschke, C. I. et al. Early lung cancer action project: initial findings on repeat screening. Cancer 92, 153–159 (2001).
Swensen, S. J. et al. Screening for lung cancer with low-dose spiral computed tomography. Am. J. Respir. Crit. Care Med. 165, 508–513 (2002).
Pinsky, P. F., Gierada, D. S., Hrudaya Nath, P. & Munden, R. Lung cancer risk associated with new solid nodules in the national lung screening trial. Am. J. Roentgenol. 209, 1009–1014 (2017).
Saghir, Z. et al. CT screening for lung cancer brings forward early disease. The randomised Danish Lung Cancer Screening Trial: status after five annual screening rounds with low-dose CT. Thorax 67, 296–301 (2012).
Heuvelmans, M. A. et al. Relationship between nodule count and lung cancer probability in baseline CT lung cancer screening: The NELSON study. Lung Cancer 113, 45–50 (2017).
Walter, J. E. et al. Relationship between the number of new nodules and lung cancer probability in incidence screening rounds of CT lung cancer screening: The NELSON study. Lung Cancer 125, 103–108 (2018).
MacMahon, H. et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology 284, 228–243 (2017).
American College of Radiology. LungRADSTM Version 1.0 Assessment Categories Release date: April 28, 2014 https://www.acr.org/-/media/ACR/Files/RADS/Lung-RADS/LungRADS_AssessmentCategories.pdf (2014).
Han, D. et al. Influence of lung nodule margin on volume-and diameter-based reader variability in CT lung cancer screening. Br. J. Radiol. 91, 20170405 (2018).
Heuvelmans, M. A. et al. Disagreement of diameter and volume measurements for pulmonary nodule size estimation in CT lung cancer screening. Thorax 73, 779–781 (2018).
Callister, M. E. J. et al. British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax 70, 1–54 (2015).
Heuvelmans, M. A. & Oudkerk, M. Pulmonary nodules measurements in CT lung cancer screening. J. Thorac. Dis. 10, S2100–S2102 (2018).
Han, D. et al. Influence of lung nodule margin on volume- and diameter-based reader variability in CT lung cancer screening. Br. J. Radiol. 91, 20170405 (2018).
Bankier, A. A. et al. Recommendations for measuring pulmonary nodules at CT: a statement from the Fleischner society. Radiology 285, 584–600 (2017).
Kakinuma, R. et al. Solitary pure ground-glass nodules 5 mm or smaller: frequency of growth. Radiology 276, 873–882 (2015).
Horeweg, N. et al. Lung cancer probability in patients with CT-detected pulmonary nodules: A prespecified analysis of data from the NELSON trial of low-dose CT screening. Lancet Oncol. 15, 1332–1341 (2014).
Henschke, C. I. et al. CT screening for lung cancer: part-solid nodules in baseline and annual repeat rounds. Am. J. Roentgenol. 207, 1176–1184 (2016).
Yip, R. et al. Lung cancer deaths in the national lung screening trial attributed to nonsolid nodules. Radiology 281, 589–596 (2016).
Walter, J. E. et al. New subsolid pulmonary nodules in lung cancer screening: the NELSON trial. J. Thorac. Oncol. 13, 1410–1414 (2018).
Henschke, C. I. et al. ELCAP Group, CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. Am. J. Roentgenol. 178, 1053–1057 (2002).
Lee, S. M. et al. Transient part-solid nodules detected at screening thin-section CT for lung cancer: comparison with persistent part-solid nodules. Radiology 255, 242–251 (2010).
Oh, J.-Y. et al. Clinical significance of a solitary ground-glass opacity (GGO) lesion of the lung detected by chest CT. Lung Cancer 55, 67–73 (2007).
Kakinuma, R. et al. Natural history of pulmonary subsolid nodules: a prospective multicenter study. J. Thorac. Oncol. 11, 1012–1028 (2016).
McWilliams, A. et al. Probability of cancer in pulmonary nodules detected on first screening CT. N. Engl. J. Med. 369, 910–919 (2013).
Tammemagi, M. et al. Predicting malignancy risk of screen-detected lung nodules–mean diameter or volume. J. Thorac. Oncol. 14, 203–211 (2019).
Marcus, M. W. et al. Probability of cancer in lung nodules using sequential volumetric screening up to 12 months: the UKLS trial. Thorax 74, 761–767 (2019).
Raghu, V. K. et al. Feasibility of lung cancer prediction from low-dose CT scan and smoking factors using causal models. Thorax 74, 643–649 (2019).
Swensen, S. J., Silverstein, M. D., Ilstrup, D. M., Schleck, C. D. & Edell, E. S. The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. Arch. Intern. Med. 157, 849–855 (1997).
Li, Y., Chen, K. Z. & Wang, J. Development and validation of a clinical prediction model to estimate the probability of malignancy in solitary pulmonary nodules in Chinese people. Clin. Lung Cancer 12, 313–319 (2011).
González Maldonado, S. et al. Evaluation of prediction models for identifying malignancy in pulmonary nodules detected via low-dose computed tomography. JAMA Netw. Open 3, e1921221 (2020).
Heuvelmans, M. A. & Oudkerk, M. Less is more in lung cancer risk prediction models. JAMA Netw. Open 3, e1921492 (2020).
De Koning, H. J. et al. Benefits and harms of computed tomography lung cancer screening strategies: a comparative modeling study for the U.S. Preventive services task force. Ann. Intern. Med. 160, 311–320 (2014).
Patz, E. F. et al. Lung cancer incidence and mortality in National Lung Screening Trial participants who underwent low-dose CT prevalence screening: a retrospective cohort analysis of a randomised, multicentre, diagnostic screening trial. Lancet Oncol. 17, 590–599 (2016).
Pastorino, U. et al. Ten-year results of the Multicentric Italian Lung Detection trial demonstrate the safety and efficacy of biennial lung cancer screening. Eur. J. Cancer 118, 142–148 (2019).
Schreuder, A. et al. Lung cancer risk to personalise annual and biennial follow-up computed tomography screening. Thorax https://doi.org/10.1136/thoraxjnl-2017-211107 (2018).
Yousaf-Khan, U. et al. Final screening round of the NELSON lung cancer screening trial: the effect of a 2.5-year screening interval. Thorax 72, 1–9 (2016).
Heuvelmans, M. A. & Oudkerk, M. Appropriate screening intervals in low-dose CT lung cancer screening. Transl Lung Cancer Res. 7, 281–287 (2018).
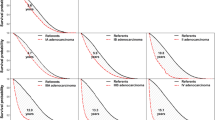
Pinsky, P. F., Church, T. R., Izmirlian, G. & Kramer, B. S. The National Lung Screening Trial: results stratified by demographics, smoking history, and lung cancer histology. Cancer 119, 3976–3983 (2013).
National Lung Screening Trial Research Team. Lung cancer incidence and mortality with extended follow-up in the national lung screening trial. J. Thorac. Oncol. 14, 1732–1742 (2019).
Ten Haaf, K., Van Rosmalen, J. & de Koning, H. J. Lung cancer detectability by test, histology, stage, and gender: Estimates from the NLST and the PLCO trials. Cancer Epidemiol. Biomarkers Prev. 24, 154–161 (2015).
Radkiewicz, C. et al. Sex and survival in non-small cell lung cancer: a nationwide cohort study. PLoS ONE 14, e0219206 (2019).
Wainer, Z. et al. Sex-dependent staging in non–small-cell lung cancer; analysis of the effect of sex differences in the eighth edition of the Tumor, Node, Metastases Staging System. Clin. Lung Cancer 19, e933–e944 (2018).
Tammemägi, M. C., Berg, C. D., Riley, T. L., Cunningham, C. R. & Taylor, K. L. Impact of lung cancer screening results on smoking cessation. J. Natl Cancer Inst. 106, dju084 (2014).
Ashraf, H. et al. Smoking habits in the randomised Danish Lung Cancer Screening Trial with low-dose CT: final results after a 5-year screening programme. Thorax 69, 574–579 (2014).
Brain, K. et al. Impact of low-dose CT screening on smoking cessation among high-risk participants in the UK Lung Cancer Screening trial. Thorax 72, 912–918 (2017).
Kummer, S. et al. Mapping the spectrum of psychological and behavioural responses to low-dose CT lung cancer screening offered within a Lung Health Check. Health Expect. 23, 433–441 (2020).
Villanti, A. C., Jiang, Y., Abrams, D. B. & Pyenson, B. S. A cost-utility analysis of lung cancer screening and the additional benefits of incorporating smoking cessation interventions. PLoS ONE 8, e71379 (2013).
Black, W. C. et al. Cost-effectiveness of CT screening in the National Lung Screening Trial. N. Engl. J. Med. 371, 1793–1802 (2014).
Criss, S. D. et al. Cost-effectiveness analysis of lung cancer screening in the United States: a Comparative Modeling Study. Ann. Intern. Med. 171, 796–804 (2019).
Toumazis, I. et al. Cost-effectiveness analysis of lung cancer screening accounting for the effect of indeterminate findings. JNCI Cancer Spectr. 3, pkz035 (2019).
Pyenson, B. S., Henschke, C. I., Yankelevitz, D. F., Yip, R. & Dec, E. Offering lung cancer screening to high-risk medicare beneficiaries saves lives and is cost-effective: an actuarial analysis. Am. Health Drug Benefits 7, 272–282 (2014).
Goffin, J. R. et al. Biennial lung cancer screening in Canada with smoking cessation — outcomes and cost-effectiveness. Lung Cancer 101, 98–103 (2016).
Ten Haaf, K. et al. Performance and cost-effectiveness of computed tomography lung cancer screening scenarios in a population-based setting: a microsimulation modeling analysis in Ontario, Canada. PLOS Med. 14, e1002225 (2017).
Cressman, S. et al. The cost-effectiveness of high-risk lung cancer screening and drivers of program efficiency. J. Thorac. Oncol. 12, 1210–1222 (2017).
Tomonaga, Y. et al. Cost-effectiveness of low-dose CT screening for lung cancer in a European country with high prevalence of smoking — a modelling study. Lung Cancer 121, 61–69 (2018).
Kumar, V. et al. Risk-targeted lung cancer screening a cost-effectiveness analysis. Ann. Intern. Med. 168, 161–169 (2018).
Hinde, S. et al. The cost-effectiveness of the Manchester ‘lung health checks’, a community-based lung cancer low-dose CT screening pilot. Lung Cancer 126, 119–124 (2018).
Snowsill, T. et al. Low-dose computed tomography for lung cancer screening in high-risk populations: a systematic review and economic evaluation. Health Technol. Assess. 22, 1–276 (2018).
Whynes, D. K. Could CT screening for lung cancer ever be cost effective in the United Kingdom? Cost Eff. Resour. Alloc. 6, 5 (2008).
Zeng, H. et al. Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob. Health 6, e555–e567 (2018).
Chen, W. et al. Cancer incidence and mortality in China, 2014. Chin. J. Cancer Res. 30, 1–12 (2018).
Martín-Sánchez, J. C. et al. Projections in breast and lung cancer mortality among women: a Bayesian analysis of 52 countries worldwide. Cancer Res. 78, 4436–4442 (2018).
Cheng, Y. I., Davies, M. P. A., Liu, D., Li, W. & Field, J. K. Implementation planning for lung cancer screening in China. Precis. Clin. Med. 2, 13–44 (2019).
Zhou, Q. et al. Demonstration program of population-based lung cancer screening in China: Rationale and study design. Thorac. Cancer 5, 197–203 (2014).
Wang, Z. et al. Mortality outcomes of low-dose computed tomography screening for lung cancer in urban China: a decision analysis and implications for practice. Chin. J. Cancer 36, 57 (2017).
Fan, L. et al. Lung cancer screening with low-dose CT: baseline screening results in Shanghai. Acad. Radiol. 26, 1283–1291 (2019).
Luo, X. et al. Should nonsmokers be excluded from early lung cancer screening with low-dose spiral computed tomography? community-based practice in Shanghai. Transl Oncol. 10, 485–490 (2017).
Nawa, T. et al. A decrease in lung cancer mortality following the introduction of low-dose chest CT screening in Hitachi, Japan. Lung Cancer 78, 225–228 (2012).
Sagawa, M. et al. Efficacy of low-dose computed tomography screening for lung cancer: the current state of evidence of mortality reduction. Surg. Today 47, 783–788 (2017).
Nawa, T. et al. A population-based cohort study to evaluate the effectiveness of lung cancer screening using low-dose CT in Hitachi city, Japan. Jpn. J. Clin. Oncol. 49, 130–136 (2019).
Lee, J. et al. Development of protocol for Korean Lung Cancer Screening Project (K-LUCAS) to evaluate effectiveness and feasibility to implement national cancer screening program. Cancer Res. Treat. 51, 1285–1294 (2019).
The Royal College of Radiologists. www.rcr.ac.uk/publication/clinical-radiology-uk-workforce-census-report-2018 (2019).
Ather, S., Kadir, T. & Gleeson, F. Artificial intelligence and radiomics in pulmonary nodule management: current status and future applications. Clin. Radiol. 75, 13–19 (2020).
Christe, A. et al. Lung cancer screening with CT: Evaluation of radiologists anddifferent computer assisted detection software (CAD) as first and second readers for lung nodule detection at different dose levels. Eur. J. Radiol. 82, e873–8 (2013).
Wang, Y. et al. No benefit for consensus double reading at baseline screening for lung cancer with the use of semiautomated volumetry software. Radiology 262, 320–326 (2012).
Liang, M. et al. Low-dose CT screening for lung cancer: computer-aided detection of missed lung cancers. Radiology 281, 279–288 (2016).
Vlahos, I. et al. Lung cancer screening: Nodule identification and characterization. Transl Lung Cancer Res. 7, 288–303 (2018).
Ebner, L. et al. Maximum-intensity-projection and computer-aided-detection algorithms as stand-alone reader devices in lung cancer screening using different dose levels and reconstruction kernels. Am. J. Roentgenol. 207, 282–288 (2016).
Ciompi, F. et al. Towards automatic pulmonary nodule management in lung cancer screening with deep learning. Sci. Rep. 7, 46479 (2017).
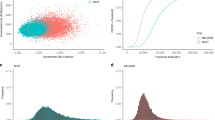
Ardila, D. et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 25, 954–961 (2019).
Huang, P. et al. Prediction of lung cancer risk at follow-up screening with low-dose CT: a training and validation study of a deep learning method. Lancet Digit. Health 1, e353–e362 (2019).
Baldwin, D. R. et al. External validation of a convolutional neural network artificial intelligence tool to predict malignancy in pulmonary nodules. Thorax 75, 306–312 (2020).
Liu, K. et al. Evaluating a fully automated pulmonary nodule detection approach and its impact on radiologist performance. Radiol. Artif. Intell. https://doi.org/10.1148/ryai.2019180084 (2019).
Duffy, S. W. & Field, J. K. Mortality reduction with low-dose CT screening for lung cancer. N. Engl. J. Med. 382, 572–573 (2020).
Author information
Authors and Affiliations
Contributions
M.O. contributed to all aspects of the preparation of this article. S.L. and J.E.W. researched data. M.A.H. contributed to discussions, researched data and supported the draft of the manuscript. J.K.F. contributed to all aspects of the preparation of this article. The final manuscript was approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Clinical Oncology thanks S. Lam, U. Pastorino and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Oudkerk, M., Liu, S., Heuvelmans, M.A. et al. Lung cancer LDCT screening and mortality reduction — evidence, pitfalls and future perspectives. Nat Rev Clin Oncol 18, 135–151 (2021). https://doi.org/10.1038/s41571-020-00432-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41571-020-00432-6
This article is cited by
-
Comparison of different classification systems for pulmonary nodules: a multicenter retrospective study in China
Cancer Imaging (2024)
-
Folate-modified liposomes mediate the co-delivery of cisplatin with miR-219a-5p for the targeted treatment of cisplatin-resistant lung cancer
BMC Pulmonary Medicine (2024)
-
Is low-dose computed tomography for lung cancer screening conveniently accessible in China? A spatial analysis based on cross-sectional survey
BMC Cancer (2024)
-
Multi-instance learning based lung nodule system for assessment of CT quality after small-field-of-view reconstruction
Scientific Reports (2024)
-
Nanogenosensors based on aptamers and peptides for bioelectrochemical cancer detection: an overview of recent advances in emerging materials and technologies
Discover Applied Sciences (2024)