Abstract
Drug metabolism is generally associated with liver enzymes. However, in the case of Mycobacterium tuberculosis (Mtb), the causative agent of tuberculosis (TB), Mtb-mediated drug metabolism plays a significant role in treatment outcomes. Mtb is equipped with enzymes that catalyse biotransformation reactions on xenobiotics with consequences either in its favour or as a hindrance by deactivating or activating chemical entities, respectively. Considering the range of chemical reactions involved in the biosynthetic pathways of Mtb, information related to the biotransformation of antitubercular compounds would provide opportunities for the development of new chemical tools to study successful TB infections while also highlighting potential areas for drug discovery, host-directed therapy, dose optimization and elucidation of mechanisms of action. In this Review, we discuss Mtb-mediated biotransformations and propose a holistic approach to address drug metabolism in TB drug discovery and related areas.

Similar content being viewed by others
Introduction
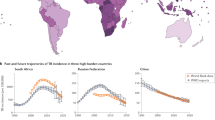
Tuberculosis (TB), a highly infectious disease caused by Mycobacterium tuberculosis (Mtb), primarily affects the lungs, causing pulmonary TB, and may affect other parts of the human body, to cause extrapulmonary TB1,2. After the severe acute respiratory syndrome coronavirus 2-related-COVID-19, TB is the second highest leading cause of death by a single infectious agent, claiming an estimated 1.6 million lives in 2021, a slight increase from 2020 (ref. 1) (here it is to be noted that the real numbers could be higher as there are no clear measures to differentiate the cause of COVID-19-related deaths in patients with TB). Drug-susceptible TB is curable; however, the treatment involves a first-line four-drug standard regimen for 6 months: an intensive phase comprising a 2-month regimen of isoniazid, rifampicin, pyrazinamide and ethambutol, followed by a continuous phase involving a 4-month regimen of isoniazid and rifampicin (Box 1). The major obstacle in eradicating TB is the increasing incidence of drug-resistant TB. Several second-line drugs are available for the treatment of drug-resistant TB, such as fluoroquinolones, injectables (capreomycin, kanamycin and amikacin), ethionamide, cycloserine, linezolid, bedaquiline and delamanid. However, the challenge of a successful TB treatment remains daunting owing to the emergence of multidrug-resistant (MDR) TB — that is, resistance to at least both isoniazid and rifampicin — and extensively drug-resistant (XDR) TB, in which MDR strains develop resistance to any fluoroquinolone and at least one of the three second-line injectable drugs. TB drug resistance is further complicated by reports of resistance to bedaquiline3,4,5, the first drug to be approved for MDR-TB treatment in over 40 years. These examples of resistance emphasize the urgent need to discover and develop novel molecules with unique mechanisms of action (MoAs) for the treatment of MDR-TB and XDR-TB. Therefore, there is a critical need to expand our understanding of the interaction between the microorganism and xenobiotics and various mechanisms of resistance presented by Mtb, identify new anti-TB chemical matter, expand our knowledge of microorganism and host interaction, and establish molecular targets for host-directed therapy.
TB-causing mycobacteria are collectively known as the Mtb complex, which includes: Mtb, the aetiologic agent of TB in humans; M. africanum, which causes TB in humans in certain regions of Africa; M. bovis, M. caprae, M. canetti, M. mungi and M. pinnipedii, responsible for TB in wild and domesticated mammals; and M. microti, the causative agent of TB in voles. Co-evolution of these strains with enhanced virulence, transmissibility and selectivity for specific hosts can be attributed to the introduction of agriculture, civilization and clustered human population in urban areas6. Classically, Mtb infection in humans can result in one of the two clinically defined states: latent TB infection or active TB disease. Mtb is carried in airborne particles, called droplet nuclei (1–5 μm in diameter), which are generated when patients with pulmonary TB cough or sneeze. For a successful infection, the aerosolized droplet containing infectious Mtb must be inhaled, travel to the lower lung and be ingested by a certain type of white blood cell (alveolar macrophage — a type of tissue-resident macrophage, monocyte-derived macrophages, dendritic cells and neutrophils)7.
Macrophages can induce a pro-inflammatory phenotype (for the containment of Mtb) and granuloma (a pathological hallmark of human TB) formation during this initial stage of infection. However, the phenotypic response of the macrophage is subsequently altered to allow Mtb growth8: a phenomenon that is less understood but believed to involve metabolic reprogramming, which has a role in controlling the response of immune cells9. Unlike other intracellular pathogens that depend on macrophages for nutrients (auxotrophs), Mtb, as a prototroph, has metabolic flexibility of catabolic and anabolic reactions to convert organic precursors into products10. This metabolic flexibility allows Mtb to survive under various stresses encountered during its life. Moreover, several human microbiome research studies conducted in a wide variety of diseases, including TB11, indicated that the microbiota exert a major influence on TB disease progression by affecting host-innate and adaptive immune responses in which metabolism has a critical role.
The biotransformation of xenobiotics in humans involves an array of metabolic reactions and is generally associated with liver enzymes, as in hepatic metabolism12 (Fig. 1). In general, these metabolic reactions can be classified as either phase I — functionalization reactions that can transform a substrate into an active or inactive species — or phase II — reactions in which small endogenous polar molecules conjugate with other molecules via functional groups either formed in phase I reactions or already present (Fig. 1). Phase II reactions increase the hydrophilicity of molecules to enhance excretion. At this juncture, it is noteworthy that biotransformation reactions may convert: 1) an active compound to a less active compound (inactivation or detoxification); 2) an active compound to a more active metabolite (bioactivation); 3) an inactive compound (prodrug) to an active metabolite (activation); 4) an active compound to an equally active metabolite; and 5) an active compound to an active metabolite with an entirely different pharmacological activity profile (Fig. 2a). In relation to the effect on TB, Mtb-mediated biotransformation reactions can be categorized into two groups: either ‘foe’ (having a negative impact on Mtb) or ‘friend’ (having a positive impact on Mtb) (Fig. 2a). Foe refers to the scenario in which the Mtb metabolic machinery converts an antitubercular prodrug into an active molecule, for example, activation of isoniazid (29) by a catalase peroxidase encoded by katG, pyrazinamide (31) by nicotinamidase (PncA) and ethionamide (33) by monooxygenases (Fig. 2b). Two nitroimidazole drugs delamanid and pretomanid (36) are also bioactivated by Mtb nitroreductases (Fig. 2b). In the context of friend, Mtb can aid TB by metabolically deactivating ‘potent’ antituberculars, such as second-line aminoglycosides in amidation, esterification or phosphorylation reactions catalysed by acetyltransferases and phosphotransferases13 (Fig. 2c). These examples highlight the need for a deeper understanding of Mtb-mediated biotransformation reactions in the context of drug discovery, host-directed therapy and MoA studies.
A, Phase I: involved in exposing or adding a functional group; following phase I, the drug may be activated or unchanged or inactivated. B, Phase II: synthetic or conjugation reactions; following phase II, generally, the drug is inactive. GSH, glutathione; NAcCys, N-acetylcysteine; NAPQI, N-acetyl-p-benzoquinoneimine; RSH, thiol-containing protein; RSSG, protein-bound glutathione.
a, Common biotransformation reactions in Mycobacterium tuberculosis (Mtb) in the context of friend or foe. b, Activation of anti-tuberculosis prodrugs by Mtb. c, Kanamycin A (38), an aminoglycoside antibiotic, is metabolized by Mtb through N-acetylation by enhanced intracellular survival protein (Eis) and O-phosphorylation by aminoglycoside-3′-phosphotransferease (APH) to afford inactive metabolite.
In this Review, we discuss the current knowledge of capability of Mtb to remodel its metabolism for biotransformation reactions on small molecule xenobiotics in the context of beneficial and detrimental outcomes for the pathogen. Additionally, we briefly discuss the role of the host microbiome in influencing the survival of Mtb. We propose using approaches to learn the metabolic liabilities of the active molecules beyond hepatic metabolism and MoA studies on generated metabolites in identifying molecular targets for TB drug discovery and host-directed therapy.
Biotransformation in mycobacteria
Owing to the complex pathophysiology of TB disease, it remains puzzling to determine the accurate metabolic status of Mtb at the disease site. Most metabolic studies have been performed using genetic tools and metabolomics to confirm various enzymatic or regulatory functions, thereby validating the metabolic role and essentiality14,15. Some of these findings and Mtb-mediated drug metabolism (pre-2017) have been reviewed previously16. In recent years, mode of action or resistance and metabolomics studies have contributed immensely towards understanding the metabolic arsenal accessible to Mtb in eluding TB treatment. In this regard, examples of biotransformation reactions on some newly identified anti-Mtb agents are briefly discussed subsequently. The discussion focuses on: 1) biotransformation mechanisms, including enzymes and chemical transformations involved, and 2) the MoA of active metabolites or mechanisms of resistance or inactivity of metabolites.
Foe biotransformation examples
Biotransformation reactions can have a negative impact on Mtb, denoted here as foe.
Triaza-coumarin congeners
A new class of 1,3,5-triazaspiro[5.5]undeca-2,4-dienes has been identified as a selective inhibitor series of dihydrofolate reductases (DHFRs), an essential enzyme involved in folate metabolism, with potent whole-Mtb cell activity17. Congeners of triaza-coumarin (39) (Fig. 3a), which bear a coumarin moiety, showed low nanomolar minimum inhibitory concentration (MIC) values of 10–200 nM against M. bovis bacillus Calmette–Guérin (BCG). Against Mtb, 39 possessed an MIC value of 25 nM but a moderate Mtb DHFR IC50 value of 820 nM, which was 18-fold higher than human DHFR. Further studies to elucidate the underlying mechanisms responsible for the whole-cell-to-enzyme potency disconnect identified two resistance mechanisms. The first mechanism was associated with low-frequency mutations in thymidylate synthase (thyA), confirming that 39 is involved in the folate pathway. The second mechanism is based on the loss of enzymes (FbiC and Fgd1) required for the biosynthesis of redox cofactor F420, which implicated metabolism by Mtb F420-dependent oxidoreductases (FDORs)17. The latter was corroborated by the generation of mutant strains harbouring loss-of-function mutations in fbiC and fgd1, which are involved in the biosynthesis of the redox cofactor F420H2, a bioactivator of pretomanid. At a molecular level, the α,β-unsaturated carbonyl group in the coumarin motif of 39 is reduced to deliver 40, which is spontaneously hydrolysed to 41 — a potent DHFR inhibitor — thereby affecting the folate pathway17 (Fig. 3a). Chemically synthesized 41 showed an IC50 value of ~10 nM against recombinant Mtb DHFR, about 100-fold more potent than the parent 39 and improved selectivity over the human DHFR. However, 41 showed lower whole-cell activity compared with 39 (M. bovis, MIC = 0.8 and 0.02 µM, respectively), which may be due to its limited permeability into Mtb cells. Compound 39 with a methyl substituent at the β-position to block reduction of the unsaturated bond showed loss of whole-cell potency (MIC = 3.2 µM), but moderate DHFR inhibitory activity with an IC50 value of 0.63 µM. Although FDORs bioactivate 39, the specific enzymes involved are yet to be determined: biochemical analyses using recombinant Mtb FDORs confirmed that 39 is a substrate of both deazaflavin-dependent nitroreductase (Ddn) and its homologue Rv1558. From a drug discovery perspective, 39 exhibits properties of a good starting point. For example, it has low cytotoxicity (SI > 4,000; SI is the selectivity index; SI = IC50:MIC90, mammalian cell-line:Mtb) and hemolytic activity (LC50 > 100 µM; LC50 is the lethal concentration that kills 50% of the target population), as well as good aqueous solubility (>100 µM, pH 7.4) and encouraging metabolic stability in rat liver microsomes18. Considering its low resistant-mutation frequency and possible pleiotropic mode of action, characterizing the specific targets of 39 while addressing the reduction will be useful to inform requisite structure–activity relationship (SAR) strategies to overcome the metabolism-induced resistance.
a, The triaza-coumarin (39) is reduced in its coumarin ring inside Mycobacterium tuberculosis (Mtb) cells to form the unstable intermediate 40, which undergoes spontaneous ring opening to form the more active 41. b, The nitrofuranyl calanolides 42 and 43 are reduced to the amino metabolite 44. c, The thienopyrimidine analogue 45 prodrug is metabolized through nitro group reduction to the reactive 46. d, The pyrano[3,2-b]indolone compound 47 releases active metabolites after reduction by Mtb. e, The thioalkylbenzoxazole analogue (THB-1; 48) underwent sulfur oxidation to produce active metabolites. f, Chemical structures of 49, 5-fluoroanthranilate 50 and indole propionic acid 51. g, Indole-4-carboxamide 52 is hydrolysed to 4-aminoindole, which is incorporated in the tryptophan biosynthetic pathway to produce toxic tryptophan metabolite (4-amino-l-Trp; 53). h, The benzoheterocyclic oxime carbamate hit compounds 54 and 55, Mtb-mediated hydrolysis of 56 and related compounds release the oxime metabolite 57. AmiC, putative amidase; Ddn, deazaflavin-dependent nitroreductase; DHFR, dihydrofolate reductase; FbiC, Fgd1, probable F420 biosynthesis protein; Mrx-2, mycoredoxin; MymA, flavin monooxygenase; TrpAB, tryptophan synthase.
Nitrofuranyl calanolides
Nitrofuranyl calanolides are natural product-inspired molecules based on calanolide A, possessing potent selective bactericidal activity against replicating and non-replicating Mtb and an ability to eliminate detectable Mtb from primary human macrophages in vitro. The nitrofuranyl calanolides 42 and 43 (Fig. 3b) showed MIC values of 0.84 and 2.25 µM and 1.68 and 2.81 µM against replicating and non-replicating Mtb, respectively19. To understand their mode of action, Mtb or M. bovis BCG-resistant mutants of 42 or 43 were generated and relevant mutations were identified in the mycothiol-dependent nitroreductase Rv2466c (Mrx-2, mycoredoxin); by investigating these mutants, Mrx-2 was found to be involved in the activation of 42 by reduction of its nitro group, resulting in amine 44 as the major metabolite: confirmed by chemical synthesis20. In addition to its function as a nitroreductase, Mrx-2 conferred partial protection to menadione stress. However, 44 showed low antimycobacterial activity when used exogenously: this low activity could be due to either poor cellular uptake or that a minor metabolite of 42, which could not be identified, is responsible for the observed in vitro antimycobacterial activity. Despite the encouraging antimycobacterial activity, 42 was found to be genotoxic presumably on account of the presence of the nitrofuran moiety, precluding its further progression.
Thienopyrimidines
Compound 45 is a new thienopyrimidine analogue with antimycobacterial activity against both replicating and non-replicating Mtb at MIC values of 0.43 and 2.7 µM, respectively. Subjecting Mtb to 45 drug pressure conferred mutations associated with the Rv2466c gene, which was shown to bioactivate 45 by reduction of its nitro group21 (Fig. 3c). However, the chemically synthesized amino derivative of 45 lacked antimycobacterial activity (MIC > 390 μM). To further understand the MoA, an assessment has been performed in purified enzyme assays and mycobacteria cultures, which showed that the mycothiol-dependent nitroreductase Mrx-2 released nitric oxide (NO) from 45 in both22. To identify the active metabolite, high-density culture of a recombinant Mtb strain overexpressing Mrx-2 was exposed to high drug pressure (400× MIC). This resulted in the generation of metabolite 46, formed by cleavage of the reduced thiophene ring to reveal a reactive thiol moiety, and is hypothesized to be responsible for the pleiotropic effects of 45 on Mtb cell growth by inhibiting lipid biosynthesis, transcription and protein synthesis.
Pyrano[3,2-b]indolones
Compound 47 (Fig. 3d) is a pyrano[3,2-b]indolone with potent MIC values of 1.26 and 1.68 µM against replicating and non-replicating (SS18b) strains of Mtb23. M. bovis BCG-resistant mutants of 47 were cross-resistant to pretomanid, suggesting a similarity in MoA. Activation of pretomanid involves either Ddn or proteins responsible for the synthesis (FbiA, FbiB and FbiC) or reduction (Fgd1) of a mature active form of cofactor F420. However, owing to the absence of a nitro group in 47, the involvement of Ddn was ruled out and focus turned to the MoA involving F420. Sanger and whole-genome sequencing of 47-resistant mutants established a role of F420-dependent enzymes (FbiC or Fgd1) in the activation of 47.
Thioalkylbenzoxazoles
Thioalkylbenzoxazole analogue (48; MIC = 10 µM) is bioactivated by Mtb flavin monooxygenase (MymA) through a sulfur oxidation metabolism24 (Fig. 3e). Resistant mutants to 48 possessed an SNP (insertion of an adenine nucleotide at position 382 of the mymA (also known as rv3083) gene), translating into high MIC values against the mymA mutant strains but a similar MIC value of 10 µM against a wild-type Mtb strain. The role of MymA in Mtb-mediated biotransformations is crucial as it is also responsible for an alternative monooxygenase, which activates ethionamide25. Additionally, the role of MymA as a Toll-like receptor agonist in stimulating the release of pro-inflammatory cytokines can be crucial in designing next-generation vaccines26.
Indole-4-carboxamides
Host CD4 T cells (involved in the immune response) manage Mtb growth by starving it of tryptophan; however, Mtb can subvert this by synthesizing the amino acid under stress conditions. Examples of tryptophan biosynthesis inhibitors (Fig. 3f) include BRD4592 (49), indole propionic acid (50) and 5-fluoroanthranilate (51), which target different enzymes in the pathway27. Conversely, a new series of indole-4-carboxamides is metabolized by Mtb to 4-aminoindole which is incorporated into the tryptophan biosynthesis pathway affording 4-amino-l-Trp (53), a toxic metabolite resulting in Mtb cell death28 (Fig. 3g). Mtb has developed three resistance mechanisms against indole-4-carboxamides (exemplified by 52) (Fig. 3g), shedding light on the potential MoA of these compounds. The first mechanism involved mutations in a non-essential putative amidase AmiC. Mutated AmiC lost the ability to hydrolyse the amide bond to generate the metabolite, which maintains activity against Mtb (MIC = 4.68 µM). The second resistance mechanism involved mutations in trpE (anthranilate synthase), which converts chorismite to anthranilate, the first step in the tryptophan biosynthesis pathway. The TrpE-H170R mutant was less sensitive than TrpE (250-fold) to allosteric inhibition by l-Trp. Additionally, this mutation enhances the flux of intermediates through the pathway irrespective of l-Trp concentrations that would otherwise shut down biosynthesis, allowing Mtb to overcome inhibition by the metabolite. Finally, 52 and its metabolite conferred mutations in TrpAB (tryptophan synthase) in residues spread throughout the protein rather than in the α-subunits and β-subunits only, which are usually observed owing to TrpAB inhibitors. These mutations altered the enzymatic activity of TrpAB, which decreased the formation of toxic 4-amino-l-Trp (53) along with normal l-Trp needed for bacterial survival.
Benzoheterocyclic oxime carbamates
The anti-Mtb activity of a library of small polar molecules has been evaluated29,30 and yielded a new series of benzoheterocyclic oxime carbamate hits. Compounds 54 and 55 (Fig. 3h), two molecules explored, have good selectivity towards mycobacteria, including a panel of five clinical isolates with MIC values in the range of 0.08–0.30 µM (refs. 29,30). These compounds were hypothesized to act as prodrugs by undergoing Mtb-mediated hydrolysis of the carbamate moiety to release the more stable oximes, which are responsible for the observed activity. The oximes can bind to their protein target in Mtb; however, they have poor Mtb permeability. By exploring another hit, 56, liquid chromatography coupled with mass spectrometry in Mtb live cultures confirmed rapid metabolism to 57 (Fig. 3h), relative to culture media and heat-killed cultures, in support of the prodrug hypothesis. In addition, the chemically synthesized oxime congeners of the carbamates were inactive against Mtb (MIC > 160 µM). It has been further hypothesized that the carbamate group is essential to facilitate Mtb cell membrane permeability as free oximes of the same series were completely inactive.
Fusidic acid-3-esters
The natural product antibiotic fusidic acid (59) (Fig. 4a) showed potent antimycobacterial activity with an in vitro MIC value of <0.15 µM against Mtb. However, 59 was inactive in a mouse TB infection model presumably owing to its rapid metabolism to the substantially weakly whole-cell-active 3-epifusidic acid (60) (Fig. 4b), which was confirmed by metabolite identification studies following incubation with mouse liver microsomes31,32. Towards repositioning 59 for TB, its active alkyl esters (Fig. 4a) were used as classic prodrugs: when 58 is incubated with Mtb H37Rv cultures, 59 is slowly released as an even more active metabolite. Moreover, as expected, the levels of the biotransformation reaction product of 58 were 500-fold more when incubated with live Mtb H37Rv cultures, in comparison to metabolically inactive heat-killed Mtb cells. At this juncture, it is noteworthy that in the same experiments, the C-3 silicate ester 61 (MIC = 1.25 µM) (Fig. 4b) was not hydrolysed to 59 or any other metabolite, maintaining comparable amounts in both cell cultures. In addition, the C-21 aryl ester 62 was not metabolized to the free acid; 59 is in clinical use against Gram-positive infections, including methicillin-resistant Staphylococcus aureus33. In Mtb, 59 targets an essential elongation factor, G, which is crucial for protein translation34. Despite 58 showing improved absorption and tissue distribution in pharmacokinetic and organ distribution experiments32, preclinical development of fusidic acid as an anti-TB drug has been hampered as a pharmacology proof-of-concept study in a mouse TB infection model showed rodent-mediated metabolism to yield inactive 60. Considering this, it may be useful to progress and evaluate the pharmacokinetics of 59 in non-rodent models of TB, such as the marmoset, in which metabolism, and thus drug exposure, may be like that in humans.
a, The fusidic acid alkyl ester (58) as a prodrug is metabolized by Mycobacterium tuberculosis (Mtb) to the parent drug fusidic acid (59). b, Chemical structures of 3-epifusidic acid (60), fusidic acid 3-silicate ester (61) and fusidic acid C-21 aryl ester (62). c, p-Aminosalicylic acid (PAS; 63) undergoes mono-amino and di-amino alkylation in Mtb to produce 64 and 65. Compounds 63 and 64 are incorporated in the folate metabolism pathway; mimicking the natural substrate p-aminobenzoic acid, they form conjugates (66–69) that are able to inhibit Mtb dihydrofolate reductase (DHFR). DHFS, dihydrofolate synthase; DHPS, dihydropteroate synthase.
p-Aminosalicylic acid
The anti-TB drug p-aminosalicylic acid (PAS; 63) inhibits the folate pathway (crucial for the synthesis of cell-function precursors) of Mtb. It was assumed that 63 inhibits dihydropteroate synthase (which is involved in folic acid synthesis) by mimicking the substrate p-aminobenzoate. PAS is metabolized by Mtb via N-alkylation to the active N-methyl PAS (64) and inactive N,N-dimethyl PAS (65) and progresses through the folate pathway forming conjugates that inhibit enzymes in the pathway35 (Fig. 4c). Conjugates 66–69 were identified after exposure of Mtb to 63 through metabolomics analyses. Conjugate 68, which is responsible for the antitubercular activity of 63, was chemically synthesized and its biochemical activity was confirmed against Mtb DHFR (inhibitor constant Ki = 174 nM)36.
Friend biotransformation examples
The biotransformations described earlier detail instances which are detrimental to Mtb, but beneficial to its host. It is also possible for biotransformations to act as a friend to Mtb and aid its survival.
Bio-AMS
Bio-AMS (70) is a 5′-[N-(D-biotinoyl)sulfamoyl]amino-5′-deoxyadenosine bisubstrate inhibitor of mycobacterial biotin protein ligase (involved in lipid metabolism) with an IC50 value of 135 nM (Fig. 5a). It is potent against Mtb (MIC = 0.31–0.78 µM) with MIC values in the range of 0.16–0.625 µM against MDR–XDR strains of Mtb37,38,39. Mtb-resistant mutants to 70 showed overexpression of the type II sulfatase Rv3406. Rv3406 is involved in the oxidation of the 5′-methylene carbon of 70 to the hemiaminal (71), resulting in molecular cleavage to produce the inactive substrates, biotinoyl sulfamide (72) and adenosine 5′-aldehyde (73)37. By blocking the labile 5′-position of 70 through the introduction of a methyl substituent, a modified 5′-C-methyl derivative was no longer susceptible to enzyme inactivation40.
a, The biotinoyl adenosine analogue Bio-AMS (70) is oxidized (71) and subsequently cleaved to produce inactive metabolites (72 and 73). Rv3406 is a sulfotase. b, The benzofurazan analogue 74 releases nitric oxide (NO) inside Mycobacterium tuberculosis (Mtb) via nitro reduction to produce two amino metabolites (75 and 76). c, Pyrazolo[1,5-a]pyrimidin-7(4H)-one analogue 77 is metabolized by Mtb through hydroxylation and N-methylation to produce several metabolites (78–80). Rv1751 is an oxidoreductase.
Benzofurazan scaffold
The antitubercular activity of the benzofurazan scaffold is well documented41; for example, the benzofurazan analogue JSF-2164 (74) is an inhibitor of purified 2-trans-enoyl-acyl carrier protein reductase (InhA, which catalyses a crucial step in type II fatty acid synthesis in Mtb; IC50 = 51 µM) with an in vitro MIC value of ~10 µM against Mtb42. Unlike the known InhA inhibitor isoniazid, which exhibits bactericidal activity, 74 was bacteriostatic, which, along with the observed disconnect between InhA inhibition and whole-cell activity, suggests that InhA inhibition is secondary to another possible mode of action. This was supported by the observation when resistant mutants to 74 exhibited mutations in the genes fbiC and fgd1. The essentiality of F420H2 to 74 activity was confirmed through resistance conferred by the fgd1::tn strain, bearing a functionally inactivated fgd1 gene. Similar to pretomanid, 74 undergoes intrabacterial F420H2-dependent NO production for the inhibition of Mtb growth (Fig. 5b). Apart from releasing NO, Mtb biotransforms 74 into two metabolites with concomitant reduction of the nitro group to an amino group. The metabolites (75; JSF-3616 and 76; JSF-3617) that were confirmed by chemical synthesis, relative to 74, showed less potent MIC values of 32 and 250 µM, respectively, against the wild-type Mtb strain, but 46% and 77% InhA inhibition at 50 µM compared with 53% for 74 at the same concentration. Metabolites 75 and 76 were produced in the fgd1::tn strain but at a slower rate compared with the wild-type Mtb strain, suggesting the involvement of other genes besides F420H2 in the metabolism of 74. Furthermore, given that the desnitro metabolite from the loss of NO in 74 was not detected, the formation of 75 and 76 supports the involvement of other nitroreductases in the intrabacterial metabolism of 74. Although 74 has a high in vitro MIC value, it may be useful as a starting point for medicinal chemistry SAR exploration as N-oxide benzofurazans with potent in vitro and in vivo antitubercular activities have been reported41.
Pyrazolo[1,5-a]pyrimidin-7(4H)-one
Antitubercular pyrazolo[1,5-a]pyrimidin-7(4H)-ones that act by targeting cell wall biosynthesis, isoprene biosynthesis and iron chelation have been reported43,44,45. Structurally, these compounds contain a substituted phenyl group at the C-3 position of the pyrazolo[1,5-a]pyrimidin-7(4H)-one core scaffold (Fig. 5c). A promising pyrazolo[1,5-a]pyrimidin-7(4H)-one hit compound (77) was identified from a high-throughput whole-cell screen46. SAR exploration revealed the importance of the C7-oxo group for antimycobacterial activity. A methyl group at the C2 position and a phenyl group at C5 were also required for potency. MoA studies by spontaneous-resistant mutant generation towards identifying the molecular target of these compounds revealed the role of a flavin adenine dinucleotide-dependent hydroxylase (Rv1751) in compound metabolism via hydroxylation leading to hydroxylated metabolites (78–80) (Fig. 5c). This finding highlights an additional MoA of the 3-phenyl pyrazolo[1,5-a]pyrimidin-7(4H)-one scaffold in Mtb. On the basis of this, it is suggested that the pyrazolo[1,5-a]pyrimidin-7(4H)-one scaffold has the potential to target several proteins in Mtb, which may make compounds based on this scaffold less susceptible to resistance.
Other examples
Contrary to PAS, the well-known sulfonamide inhibitors of the folate pathway dihydropteroate synthase are inactive (sulfanilamide and dapsone) or weakly active (sulfamethoxazole) against Mtb. These undergo Mtb-mediated metabolism by N-alkylation, N-acetylation and/or acetyl reduction to produce inactive metabolites16,35 (Supplementary Fig. 1a–c). Similarly, the methotrexate diethyl ester 87 (Supplementary Fig. 1d) and its dimethyl congener show MIC values of 0.6 and 0.2–0.4 µM against Mtb, with potent Mtb DHFR IC50 values of 30 and 50 nM, respectively. However, methotrexate is poorly active against Mtb (MIC > 100 µM), but highly active against purified DHFR with an IC50 value of 6.8 nM. Compound 87 undergoes intrabacterial hydrolysis to afford weakly whole-cell active mono-ethyl metabolites (MIC = 33 µM), which maintained DHFR inhibitory potency (IC50 = 24 and 172 nM for 88 and 99, respectively)47. A study48 uncovered N-methylation as a potential biotransformation reaction mechanism inside Mtb in the metabolism of a bactericidal pyrido-benzimidazole compound (90) (Supplementary Fig. 1e), thereby developing resistance. The S-adenosyl-l-methionine-dependent methyltransferase (Rv0560c) was involved in transferring a methyl group from S-adenosyl-l-methionine to the N-5 position of 90 to form 91 (ref. 48).
Host microbiome versus tuberculosis
The human host, born sterile, starts developing a microbiota along with the related immune system within minutes of birth. The microbiota can be defined as a collection of microbial communities living on or in a defined environment: the human body carries trillions of microbes. The related term microbiome refers to a micro-ecosystem (microbiota and their genomes). Evolution of the microbiome is a continuous process throughout the life cycle of an individual and its composition is majorly affected by, for example, diet, hormones, stress, genetics and impacting the body in healthy and adverse states. In recent times, there has been a strong interest in microbiome research resulting in a handful of applications, such as the use of probiotics, functional foods and nutraceuticals49,50,51. The microbiome–immune interactions, reviewed elsewhere52, make a strong case for host-microbiota-directed therapies as a potential adjunctive strategy to improve TB treatment for its effectiveness, treatment shortening and relapse prevention.
Additionally, as drugs can also impact the composition of microbial communities (dysbiosis)53, microbial interaction with drugs or chemicals inside the host paved the way to the new field of ‘pharmacomicrobiomics’, which studies the interactions of microbes and pharmaceuticals54. The majority of these interactions occur within the gastrointestinal tract where distinct microbial communities reside and influence or carry metabolic processes across the different regions of the gastrointestinal tract that are varying in cell type and physiology55. Generally, the bioavailability of orally administered drugs depends on the extent of first-pass metabolism by intestinal and hepatic enzymes56. However, oral drugs may encounter the gut microbiota before reaching host tissues that can affect the bioavailability of drugs by: 1) biotransformation of drugs by common reduction and hydrolysis reactions; 2) affecting drug absorption during treatment; and/or 3) bioaccumulation (Fig. 6). There is an emerging interest in understanding the effect of TB chemotherapy on gut microorganisms. An occurrence of dysbiosis was reported in which Bacteroides species were increased, whereas Clostridiales species were reduced during TB chemotherapy57. In another study, it was suggested that TB chemotherapy has a long-lasting effect on microbiome composition as the microbiome of TB-cured individuals was unique58. These observations were complemented by animal Mtb infection studies in a TB mouse infection model59. Although these studies highlight the crosstalk between gut microbiome and TB treatment, as TB is a pulmonary disease, there is a need to understand the pulmonary microbiome role in various stages of TB disease. Moreover, there are knowledge gaps in the role of microbiome composition versus latent TB infection, dysbiosis versus efficacy of TB treatment and/or role of dysbiosis in re-infection or relapse after successful treatment. Nonetheless, the fact mentioned earlier signifies the importance of understanding the ‘pharmacomicrobiomics’ of TB drugs and the impact of Mtb-mediated drug metabolism on the pharmacokinetics of antitubercular and/or coadministered drugs.
a, The gut microbiome can directly influence anti-tuberculosis drugs by metabolizing them into active, inactive or toxic metabolites. b, The gut microbiome can also affect Mycobacterium tuberculosis infection by modulating host metabolites or pathways resulting in immune interactions: before entering systemic circulation, the bioavailability of anti-tuberculosis drugs may be affected by drug absorption and/or bioaccumulation of the drugs by the gut microbiome.
Addressing biotransformation peril
To avoid the Mtb-friendly biotransformation setbacks during various phases of the drug discovery and development process as highlighted earlier, cognisant of recommendations by Awasthi and Freundlich16, we propose a small molecule hit compound progression cascade that includes frontloading Mtb-mediated metabolism studies (Fig. 7). Here, we propose to evaluate the stability of hit compounds in 1) assay media, 2) the presence of Mtb, 3) the host cell line and 4) intracellular Mtb. Additionally, our current efforts are focused on developing and using in vitro medium-throughput assays involving recombinant Mtb overexpressor strains, expressing common compound-metabolizing recombinant enzymes. This will be complemented with metabolite identification to determine likely Mtb-mediated metabolic outcomes of newly identified small molecule starting points, which will facilitate hit triaging and identification of an active metabolite (of a prodrug) and may guide MoA deconvolution. Subsequently, to predict in vivo stability of lead molecules in humans, studies in model assays (for example, solubility, hepatocyte or microsomal fractions) offer an opportunity to further probe compound metabolism.
An early tuberculosis drug discovery cascade is proposed, in which the potential hits can be triaged for associated Mycobacterium tuberculosis (Mtb)-mediated biotransformation liability immediately after screening. This can be achieved by incubating the compound in the relevant growth medium and/or with Mtb (in vitro), with THP.1 human cell-line-derived macrophages and intracellular Mtb (ex vivo), followed by metabolite identification. Additionally, the compounds can be titrated against recombinant Mtb overexpressor strains, expressing validated recombinant enzymes involved in biotransformation. CARA, charcoal agar resazurin assay; FHA, formal hit assessment; HepG2, human liver cancer cell line; MBC, minimum bactericidal concentration; Met-ID, metabolite identification; MIC, minimum inhibitory concentration (7–14 days); MoA, mechanism of action; SDR, single drug resistant; SI, selectivity index.
The outcomes will then guide the optimization of lead compounds for optimal in vivo pharmacokinetic and pharmacodynamic properties with minimum safety liabilities and more accurate human dose prediction. There are useful approaches to identify metabolic ‘soft spots’ (that is, labile or susceptible groups) of drugs60. For example, it is widely accepted that the allylic methyl, benzylic C–H bond and the O-methyl, N-methyl and S-methyl groups are preferred metabolic soft spots of P450-mediated metabolism, in the absence of steric hinderance61. These soft spots can be addressed by structure–metabolism relationship studies in which bioisosteres are used to replace the identified soft spots; for example, replacing a benzylic methyl group with a fluorine or a chlorine atom, or a trifluoromethyl group. Furthermore, these metabolic studies may inform the selection of suitable candidates with the optimum dosing route for the required oral formulation of TB drugs: a long treatment is required for this slow-growing Mtb pathogen.
Application of metabolic wisdom
Historically, in TB drug discovery, when compared with target-based screening, phenotypic whole-cell screening has been relatively more successful to deliver desired outcomes, from hit to preclinical and clinical candidate identification62. The current TB drug discovery and clinical pipeline comprise a diverse set of drug-like molecules acting on various metabolic targets. However, the attrition rate in drug development is high and demands continued discovery efforts to replenish the pipeline. The most advanced drug candidates target energy metabolism, for example, a pyrazolo[1,5-a]pyridine-3-carboxamide hybrid (92) (Supplementary Fig. 2) is active against both drug-susceptible and drug-resistant clinical Mtb isolates and targets the QcrB subunit of the respiratory cytochrome bc1 complex63. Moreover, a novel class of benzoxaboroles (93) (Supplementary Fig. 2) inhibits leucyl-tRNA synthetase, an essential enzyme for protein synthesis in Mtb, and displays excellent in vivo efficacy in TB animal infection models64. However, as stated earlier, owing to the complexity of the disease pathophysiology, metabolic target: inhibitor pairs do not always translate into successful outcomes and caution is needed. Generally, validation of target essentiality or vulnerability is governed by genetic depletion of the target, which is indicative of the consequences of target depletion. Whereas the less-validated chemical inhibition of the target would result in modulating the related metabolome, which is not always predictable. This is further complicated by the rescue of target depletion or chemical toxicity by available metabolites. For example, the essential inosine monophosphate dehydrogenase was validated as genetically essential but the chemical inhibitor could not translate the genetic vulnerability into chemical vulnerability in the mouse TB infection model, possibly owing to the availability of target metabolite (metabolites) at the disease site65,66. Similarly, the presence of an alternative pathway can rescue bacteria from the adverse effect of an inhibitor, as in the case of Q203 and related derivatives in which the inhibitor activity is alleviated by the presence of glycerol supplementation via upregulation of the cytochrome bd oxidase, which compensates for the inhibition of target cytochrome bc1:aa3 terminal oxidase67. Therefore, it is necessary to ascertain the genetic and chemical vulnerability of a target along with confirmation of on-target activity in in vitro and in vivo environments. Nonetheless, information on drug metabolism remains crucial. For example, a new metabolic target mycobacterial membrane protein Large 3 (MmpL3) — an inner membrane protein transporting trehalose-monomycolates, precursors for trehalose-dimycolates and mycolic acids — has been reported to be a target of a diverse range of compounds68. One of these is the clinical candidate SQ109 (94) (Supplementary Fig. 2), a 1,2-ethylenediamine that interacts synergistically with other anti-TB drugs such as rifampicin, isoniazid and bedaquiline69,70. Compound 94 is currently in phase II clinical trials for the treatment of MDR-TB. Since the discovery of 94, it has been suggested that 94 inhibits multiple targets in Mtb. Owing to the various possible soft spots in 94 that can be oxygenated by cytochromes (CYPs), 94 is metabolized by human, dog and murine liver microsomes71. As Mtb also carries multiple cytochromes72, a role for Mtb CYP124 (Rv2266) in hydroxylating 94 to a monohydroxylated metabolite has recently been established73. It was proposed that this newly formed 95 (Supplementary Fig. 2) metabolite affects binding to the relevant pocket in mycobacterial membrane protein Large 3. This study supported the hypothesis that 94 is a prodrug activated by Mtb CYPs, in which CYP124 exemplifies an Mtb CYP that functions similarly to drug-metabolizing human CYPs.
The adaptability of Mtb can also be measured in developing drug-tolerant persister cells, which may emerge due to the metabolic alteration, induced drug resistance or genetic mutation to survive drug toxicity or host environmental stress74. For example, conditional tolerance to isoniazid, ofloxacin and rifampicin was associated with a mutation in transcription factor, prpR, that affects propionyl-CoA metabolism75. Similarly, the significance of a detailed understanding of metabolic reactions or pathways in reversing TB drug resistance cannot be overlooked. For example, the prodrug ethionamide is activated by a monooxygenase (EthA) generating an active metabolite that inhibits mycolic acid biosynthesis by targeting InhA76,77 (mycolic acids, α-branched, β-hydroxy long-chain fatty acids, are the hallmark of the cell envelope of Mtb). Overexpression of EthA is directly under the control of EthR, a TetR-type transcriptional repressor78. This implies that EthR can be targeted to stimulate EthA expression, thereby boosting the potency of ethionamide79. Recently, 96 (Supplementary Fig. 2) was identified from the spiroisoxazoline class of small molecules aborting resistance (SMARt): it stimulated ethionamide activity and reversed EthA-mediated resistance owing to its unique action in the ethR2–ethA2 region80. This work was further extended and resulted in the identification of 97 (Supplementary Fig. 2) from an N-acylated 4-phenylpiperidine compound series that interacts with VirS, another transcriptional regulator for regulating the mymA operon that encodes an alternative monooxygenase responsible for activating ethionamide25.
Additionally, caution needs to be exercised in evaluating covalent inhibitors that may behave unexpectedly under different conditions, for example, ‘irreversible’ under chemically simple conditions but ‘reversible’ in the complex in vivo environment81. This concept is illustrated by β-lactam antibiotics, which target peptidoglycan biosynthesis, an essential component of bacterial cell envelope, commonly by irreversible, covalent inhibition of penicillin-binding proteins. Meropenem (98) (Supplementary Fig. 2) is a broad-spectrum carbapenem β-lactam antibiotic that inhibits the L,D-transpeptidase biosynthetic enzymes in Mtb. Recently, it has been observed that meropenem unexpectedly engages with its target in the form of reversible and nonhydrolytic offloading reactions82. This reversibility could lead to degradation of meropenem to inactive meropenem β-lactone and hydrolysed forms, resulting in ineffective treatment. A similar observation has been noted with D-cycloserine (DCS, 99) (Supplementary Fig. 2), a key antitubercular used for the treatment of MDR-TB and XDR-TB, which targets two essential enzymes, alanine racemase and D-Ala:D-Ala ligase, in the peptidoglycan biosynthesis pathway. It is commonly believed that the alanine racemase inhibition mechanism involves an irreversible route. In Mtb, alanine racemase activity was detected after exposure to clinically relevant DCS concentrations. A detailed mechanistic investigation revealed a slow, reversible covalent mechanism of DCS inhibiting the alanine racemase in Mtb81. The knowledge gained from these two unconventional mechanisms strengthens the approach of having mechanistic insight in guiding the design and synthesis of improved chemical matter.
Conclusions
The mechanisms underpinning intrabacterial biotransformation are useful in discovering next-generation antituberculars well suited to treat TB. Although the search for new antitubercular agents remains an active research endeavour, with a plethora of very promising agents under development, understanding the innate metabolic capabilities of Mtb will require combined learnings from the biotransformation of specific antitubercular agents. Such knowledge will inform chemists of potential metabolic soft spots in compounds that lend themselves to Mtb-mediated metabolism early in the drug discovery process and how to potentially address this liability. Additionally, using machine learning tools, predicting the biotransformation of xenobiotics in the human gut by metabolic enzymes of gut microbes83 combined with predictions of phase I and phase II drug metabolism using various software such as MetaSite84, Metaprint2D85, ADMET predictor (simulations plus, USA), RS-WebPredictor86 and FAME87 could be a powerful strategy towards identifying metabolic liabilities of novel small molecules. Novel putative drug targets have been identified through analyses of metabolic pathways and the proteins associated with bacterial drug resistance88. Furthermore, Mtb displays a co-evolution of virulence and antibiotic resistance in which enhanced intracellular survival protein not only protects Mtb from host immunity and helps in the survival of the pathogen in macrophages but also acetylates various aminoglycosides and cyclic peptide antibiotics rendering them inactive89,90. Therefore, understanding metabolic pathways involved in making Mtb refractory to anti-TB drugs and targeting these metabolic mechanisms can lead to the development of effective strategies for the management of anti-TB drugs as well as potentially faster cures and thus treatment-shortening. In parallel, metabolism has a crucial role in successful TB infection as host cells undergo profound metabolic changes to influence the function of immune cells. This metabolic reprogramming in immune cells has developed a new field of study known as immunometabolism. Here, a clear understanding of metabolic interactions between the host and Mtb can potentially lead to the identification of molecular targets for host-directed therapy.
References
World Health Organization. Global tuberculosis report (WHO, 2022).
Segal, L. N. et al. Anaerobic bacterial fermentation products increase tuberculosis risk in antiretroviral-drug-treated HIV patients. Cell Host Microbe 21, 530–537.e4 (2017).
Ghajavand, H. et al. High prevalence of bedaquiline resistance in treatment-naive tuberculosis patients and verapamil effectiveness. Antimicrob. Agents Chemother. 63, e02530-18 (2019).
Nimmo, C. et al. Population-level emergence of bedaquiline and clofazimine resistance-associated variants among patients with drug-resistant tuberculosis in southern Africa: a phenotypic and phylogenetic analysis. Lancet Microbe 1, e165–e174 (2020).
Villellas, C. et al. Unexpected high prevalence of resistance-associated Rv0678 variants in MDR-TB patients without documented prior use of clofazimine or bedaquiline. J. Antimicrob. Chemother. 72, 684–690 (2017).
Comas, I. et al. Out-of-Africa migration and Neolithic coexpansion of Mycobacterium tuberculosis with modern humans. Nat. Genet. 45, 1176–1182 (2013).
Cohen, S. B. et al. Alveolar macrophages provide an early Mycobacterium tuberculosis niche and initiate dissemination. Cell Host Microbe 24, 439–446.e4 (2018).
Huang, L., Nazarova, E. V., Tan, S., Liu, Y. & Russell, D. G. Growth of Mycobacterium tuberculosis in vivo segregates with host macrophage metabolism and ontogeny. J. Exp. Med. 215, 1135–1152 (2018).
Pearce, E. L. & Pearce, E. J. Metabolic pathways in immune cell activation and quiescence. Immunity 38, 633–643 (2013).
Cole, S. T. et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393, 537–544 (1998).
Namasivayam, S., Sher, A., Glickman, M. S. & Wipperman, M. F. The microbiome and tuberculosis: early evidence for cross talk. mBio 9, e01420-18 (2018). This thought-provoking review discusses how the microbiome may influence the TB infection/life cycle.
Patel, M., Taskar, K. S. & Zamek-Gliszczynski, M. J. Importance of hepatic transporters in clinical disposition of drugs and their metabolites. J. Clin. Pharmacol. 56, S23–S39 (2016).
Chen, W., Biswas, T., Porter, V. R., Tsodikov, O. V. & Garneau-Tsodikova, S. Unusual regioversatility of acetyltransferase Eis, a cause of drug resistance in XDR-TB. Proc. Natl Acad. Sci. USA 108, 9804–9808 (2011).
Barry, C. E. III et al. The spectrum of latent tuberculosis: rethinking the biology and intervention strategies. Nat. Rev. Microbiol. 7, 845–855 (2009).
Jansen, R. S. et al. Aspartate aminotransferase Rv3722c governs aspartate-dependent nitrogen metabolism in Mycobacterium tuberculosis. Nat. Commun. 11, 1960 (2020).
Awasthi, D. & Freundlich, J. S. Antimycobacterial metabolism: illuminating Mycobacterium tuberculosis biology and drug discovery. Trends Microbiol. 25, 756–767 (2017). This review describes antimycobacterial metabolism and associated reactions.
Aragaw, W. W. et al. Potency boost of a Mycobacterium tuberculosis dihydrofolate reductase inhibitor by multienzyme F420H2-dependent reduction. Proc. Natl Acad. Sci. USA 118, e2025172118 (2021).
Yang, X. et al. 1,3,5-Triazaspiro[5.5]undeca-2,4-dienes as selective Mycobacterium tuberculosis dihydrofolate reductase inhibitors with potent whole cell activity. Eur. J. Med. Chem. 144, 262–276 (2018).
Zheng, P. et al. Synthetic calanolides with bactericidal activity against replicating and nonreplicating Mycobacterium tuberculosis. J. Med. Chem. 57, 3755–3772 (2014).
Negri, A. et al. Identification of a mycothiol-dependent nitroreductase from Mycobacterium tuberculosis. ACS Infect. Dis. 4, 771–787 (2018).
Albesa-Jove, D. et al. Rv2466c mediates the activation of TP053 to kill replicating and non-replicating Mycobacterium tuberculosis. ACS Chem. Biol. 9, 1567–1575 (2014).
Chiarelli, L. R. et al. New insights into the mechanism of action of the thienopyrimidine antitubercular prodrug TP053. ACS Infect. Dis. 6, 313–323 (2020).
Monakhova, N. et al. Design and synthesis of pyrano[3,2-b]indolones showing antimycobacterial activity. ACS Infect. Dis. 7, 88–100 (2021).
Moure, A. L. et al. MymA bioactivated thioalkylbenzoxazole prodrug family active against Mycobacterium tuberculosis. J. Med. Chem. 63, 4732–4748 (2020).
Flipo, M. et al. The small-molecule SMARt751 reverses Mycobacterium tuberculosis resistance to ethionamide in acute and chronic mouse models of tuberculosis. Sci. Transl Med. 14, 6280 (2022). This study emphasizes the role of metabolic knowledge in designing a compound that reverses the resistance mechanism of the target drug.
Saraav, I., Singh, S., Pandey, K., Sharma, M. & Sharma, S. Mycobacterium tuberculosis MymA is a TLR2 agonist that activate macrophages and a TH1 response. Tuberculosis 106, 16–24 (2017).
Lott, J. S. The tryptophan biosynthetic pathway is essential for Mycobacterium tuberculosis to cause disease. Biochem. Soc. Trans. 48, 2029–2037 (2020).
Libardo, M. D. J. et al. Resistance of Mycobacterium tuberculosis to indole 4-carboxamides occurs through alterations in drug metabolism and tryptophan biosynthesis. Cell Chem. Biol. 28, e1120 (2021).
van der Westhuyzen, R. et al. Pyrrolo[3,4-c]pyridine-1,3(2H)-diones: a novel antimycobacterial class targeting mycobacterial respiration. J. Med. Chem. 58, 9371–9381 (2015).
van der Westhuyzen, R. et al. Benzoheterocyclic oxime carbamates active against Mycobacterium tuberculosis: synthesis, structure–activity relationship, metabolism, and biology triaging. J. Med. Chem. 64, 9444–9457 (2021).
Njoroge, M. et al. Semisynthetic antimycobacterial C-3 silicate and C-3/C-21 ester derivatives of fusidic acid: pharmacological evaluation and stability studies in liver microsomes, rat plasma, and Mycobacterium tuberculosis culture. ACS Infect. Dis. 5, 1634–1644 (2019). This study addresses the metabolic liability of fusidic acid.
Strydom, N. et al. Pharmacokinetics and organ distribution of C-3 alkyl esters as potential antimycobacterial prodrugs of fusidic acid. ACS Infect. Dis. 6, 459–466 (2020).
Sahm, D. F., Deane, J., Pillar, C. M. & Fernandes, P. In vitro activity of CEM-102 (fusidic acid) against prevalent clones and resistant phenotypes of Staphylococcus aureus. Antimicrob. Agents Chemother. 57, 4535–4536 (2013).
Singh, V., Dziwornu, G. A., Mabhula, A. & Chibale, K. Rv0684/fusA1, an essential gene, is the target of fusidic acid and its derivatives in Mycobacterium tuberculosis. ACS Infect. Dis. 7, 2437–2444 (2021).
Chakraborty, S., Gruber, T., Barry, C. E. III, Boshoff, H. I. & Rhee, K. Y. Para-aminosalicylic acid acts as an alternative substrate of folate metabolism in Mycobacterium tuberculosis. Science 339, 88–91 (2013).
Dawadi, S., Kordus, S. L., Baughn, A. D. & Aldrich, C. C. Synthesis and analysis of bacterial folate metabolism intermediates and antifolates. Org. Lett. 19, 5220–5223 (2017).
Bockman, M. R. et al. Targeting Mycobacterium tuberculosis biotin protein ligase (MtBPL) with nucleoside-based bisubstrate adenylation inhibitors. J. Med. Chem. 58, 7349–7369 (2015).
Duckworth, B. P. et al. Bisubstrate adenylation inhibitors of biotin protein ligase from Mycobacterium tuberculosis. Chem. Biol. 18, 1432–1441 (2011).
Shi, C. et al. Bisubstrate inhibitors of biotin protein ligase in Mycobacterium tuberculosis resistant to cyclonucleoside formation. ACS Med. Chem. Lett. 4, 1213–1217 (2013).
Bockman, M. R. et al. Avoiding antibiotic inactivation in Mycobacterium tuberculosis by Rv3406 through strategic nucleoside modification. ACS Infect. Dis. 4, 1102–1113 (2018). This study presents an example of addressing the issue of Mtb-mediated biotransformation by strategic modification of the identified soft spot.
Dos Santos Fernandes, G. F. et al. Design, synthesis, and characterization of N-oxide-containing heterocycles with in vivo sterilizing antitubercular activity. J. Med. Chem. 60, 8647–8660 (2017).
Wang, X. et al. Intrabacterial metabolism obscures the successful prediction of an InhA inhibitor of Mycobacterium tuberculosis. ACS Infect. Dis. 5, 2148–2163 (2019).
Ioerger, T. R. et al. Identification of new drug targets and resistance mechanisms in Mycobacterium tuberculosis. PLoS ONE 8, e75245 (2013).
Mao, J. et al. Structure–activity relationships of compounds targeting mycobacterium tuberculosis 1-deoxy-D-xylulose 5-phosphate synthase. Bioorg. Med. Chem. Lett. 18, 5320–5323 (2008).
Dragset, M. S. et al. A novel antimycobacterial compound acts as an intracellular iron chelator. Antimicrob. Agents Chemother. 59, 2256–2264 (2015).
Oh, S. et al. Structure–activity relationships of pyrazolo[1,5-a]pyrimidin-7(4H)-ones as antitubercular agents. ACS Infect. Dis. 7, 479–492 (2021).
Nixon, M. R. et al. Folate pathway disruption leads to critical disruption of methionine derivatives in Mycobacterium tuberculosis. Chem. Biol. 21, 819–830 (2014).
Warrier, T. et al. N-methylation of a bactericidal compound as a resistance mechanism in Mycobacterium tuberculosis. Proc. Natl Acad. Sci. USA 113, 4523–4530 (2016).
Beck, L. C. et al. Strain-specific impacts of probiotics are a significant driver of gut microbiome development in very preterm infants. Nat. Microbiol. 7, 1525–1535 (2022).
Farag, M. A. et al. Metabolomics reveals impact of seven functional foods on metabolic pathways in a gut microbiota model. J. Adv. Res. 23, 47–59 (2020).
Chen, R. Y. et al. A microbiota-directed food intervention for undernourished children. N. Engl. J. Med. 384, 1517–1528 (2021).
Mori, G., Morrison, M. & Blumenthal, A. Microbiome–immune interactions in tuberculosis. PLoS Pathog. 17, e1009377 (2021).
Weersma, R. K., Zhernakova, A. & Fu, J. Interaction between drugs and the gut microbiome. Gut 69, 1510–1519 (2020). This review discusses the bidirectional interactions between the gut microbiome and drugs.
Rizkallah, R. M., Saad, R. & Aziz, K. R. The human microbiome project, personalized medicine and the birth of pharmacomicrobiomics. Curr. Pharmacogenom. Pers. Med. 8, 182–193 (2010).
Sender, R., Fuchs, S. & Milo, R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol. 14, e1002533 (2016).
Pond, S. M. & Tozer, T. N. First-pass elimination basic concepts and clinical consequences. Clin. Pharmacokinet. 9, 1–25 (1984).
Hu, Y. et al. Gut microbiota associated with pulmonary tuberculosis and dysbiosis caused by anti-tuberculosis drugs. J. Infect. 78, 317–322 (2019).
Wipperman, M. F. et al. Antibiotic treatment for tuberculosis induces a profound dysbiosis of the microbiome that persists long after therapy is completed. Sci. Rep. 7, 10767 (2017).
Namasivayam, S. et al. Longitudinal profiling reveals a persistent intestinal dysbiosis triggered by conventional anti-tuberculosis therapy. Microbiome 5, 71 (2017).
Zhang, D., Luo, G., Ding, X. & Lu, C. Preclinical experimental models of drug metabolism and disposition in drug discovery and development. Acta Pharmaceut. Sin. B 2, 549–561 (2012).
Trunzer, M., Faller, B. & Zimmerlin, A. Metabolic soft spot identification and compound optimization in early discovery phases using MetaSite and LC-MS/MS validation. J. Med. Chem. 52, 329–335 (2009). This article describes a procedure for identifying a metabolic soft spot of compounds.
Huszar, S., Chibale, K. & Singh, V. The quest for the holy grail: new antitubercular chemical entities, targets and strategies. Drug Discov. Today 25, 772–780 (2020).
Lu, X. et al. Pyrazolo[1,5- a]pyridine inhibitor of the respiratory cytochrome bcc complex for the treatment of drug-resistant tuberculosis. ACS Infect. Dis. 5, 239–249 (2019).
Li, X. et al. Discovery of a potent and specific M. tuberculosis leucyl-tRNA synthetase inhibitor: (S)-3-(aminomethyl)-4-chloro-7-(2-hydroxyethoxy)benzo[c][1,2]oxaborol-1(3H)-ol (GSK656). J. Med. Chem. 60, 8011–8026 (2017).
Singh, V. et al. The inosine monophosphate dehydrogenase, GuaB2, is a vulnerable new bactericidal drug target for tuberculosis. ACS Infect. Dis. 3, 5–17 (2017).
Park, Y. et al. Essential but not vulnerable: indazole sulfonamides targeting inosine monophosphate dehydrogenase as potential leads against Mycobacterium tuberculosis. ACS Infect. Dis. 3, 18–33 (2017).
Kalia, N. P. et al. Carbon metabolism modulates the efficacy of drugs targeting the cytochrome bc1:aa3 in Mycobacterium tuberculosis. Sci. Rep. 9, 8608 (2019).
McNeil, M. B. et al. Multiple mutations in Mycobacterium tuberculosis MmpL3 increase resistance to MmpL3 inhibitors. mSphere 5, e00985-20 (2020).
Chen, P., Gearhart, J., Protopopova, M., Einck, L. & Nacy, C. A. Synergistic interactions of SQ109, a new ethylene diamine, with front-line antitubercular drugs in vitro. J. Antimicrob. Chemother. 58, 332–337 (2006).
Reddy, V. M., Einck, L., Andries, K. & Nacy, C. A. In vitro interactions between new antitubercular drug candidates SQ109 and TMC207. Antimicrob. Agents Chemother. 54, 2840–2846 (2010).
Jia, L. et al. Interspecies pharmacokinetics and in vitro metabolism of SQ109. Br. J. Pharmacol. 147, 476–485 (2006).
Ortiz de Montellano, P. R. Potential drug targets in the Mycobacterium tuberculosis cytochrome P450 system. J. Inorg. Biochem. 180, 235–245 (2018).
Bukhdruker, S. et al. Hydroxylation of antitubercular drug candidate, SQ109, by mycobacterial cytochrome P450. Int. J. Mol. Sci. 21, 7683 (2020).
Ehrt, S., Schnappinger, D. & Rhee, K. Y. Metabolic principles of persistence and pathogenicity in Mycobacterium tuberculosis. Nat. Rev. Microbiol. 16, 496–507 (2018). This review discusses the metabolic principles involved in various phases of Mtb.
Hicks, N. D. et al. Clinically prevalent mutations in Mycobacterium tuberculosis alter propionate metabolism and mediate multidrug tolerance. Nat. Microbiol. 3, 1032–1042 (2018).
DeBarber, A. E., Mdluli, K., Bosman, M., Bekker, L. G. & Barry, C. E. III Ethionamide activation and sensitivity in multidrug-resistant Mycobacterium tuberculosis. Proc. Natl Acad. Sci. USA 97, 9677–9682 (2000).
Banerjee, A. et al. inhA, a gene encoding a target for isoniazid and ethionamide in Mycobacterium tuberculosis. Science 263, 227–230 (1994).
Baulard, A. R. et al. Activation of the pro-drug ethionamide is regulated in mycobacteria. J. Biol. Chem. 275, 28326–28331 (2000).
Willand, N. et al. Synthetic EthR inhibitors boost antituberculous activity of ethionamide. Nat. Med. 15, 537–544 (2009).
Blondiaux, N. et al. Reversion of antibiotic resistance in Mycobacterium tuberculosis by spiroisoxazoline SMARt-420. Science 355, 1206–1211 (2017).
de Chiara, C. et al. D-cycloserine destruction by alanine racemase and the limit of irreversible inhibition. Nat. Chem. Biol. 16, 686–694 (2020).
Zandi, T. A. & Townsend, C. A. Competing off-loading mechanisms of meropenem from an L,D-transpeptidase reduce antibiotic effectiveness. Proc. Natl Acad. Sci. USA 118, e2008610118 (2021).
Sharma, A. K., Jaiswal, S. K., Chaudhary, N. & Sharma, V. K. A novel approach for the prediction of species-specific biotransformation of xenobiotic/drug molecules by the human gut microbiota. Sci. Rep. 7, 9751 (2017).
Cruciani, G. et al. MetaSite: understanding metabolism in human cytochromes from the perspective of the chemist. J. Med. Chem. 48, 6970–6979 (2005).
Boyer, S. et al. Reaction site mapping of xenobiotic biotransformations. J. Chem. Inf. Model. 47, 583–590 (2007).
Zaretzki, J. et al. RS-WebPredictor: a server for predicting CYP-mediated sites of metabolism on drug-like molecules. Bioinformatics 29, 497–498 (2013).
Kirchmair, J. et al. Fast metabolizer (FAME): a rapid and accurate predictor of sites of metabolism in multiple species by endogenous enzymes. J. Chem. Inf. Model. 53, 2896–2907 (2013).
Cloete, R., Oppon, E., Murungi, E., Schubert, W. D. & Christoffels, A. Resistance related metabolic pathways for drug target identification in Mycobacterium tuberculosis. BMC Bioinformatics 17, 75 (2016).
Chen, W., Green, K. D., Tsodikov, O. V. & Garneau-Tsodikova, S. Aminoglycoside multiacetylating activity of the enhanced intracellular survival protein from Mycobacterium smegmatis and its inhibition. Biochemistry 51, 4959–4967 (2012).
Gygli, S. M., Borrell, S., Trauner, A. & Gagneux, S. Antimicrobial resistance in Mycobacterium tuberculosis: mechanistic and evolutionary perspectives. FEMS Microbiol. Rev. 41, 354–373 (2017).
World Health Organization. WHO operational handbook on tuberculosis: module 4: treatment: drug-susceptible tuberculosis treatment (WHO, 2022); https://www.who.int/publications/i/item/9789240065116.
Acknowledgements
The Bill and Melinda Gates Foundation (Global Health Grant Number OPP1066878), South African Medical Research Council (SAMRC), Strategic Health Innovation Partnerships unit of the SAMRC, Technology Innovation Agency and South African Department of Science and Innovation/National Research Foundation Research are gratefully acknowledged for support. K.C. is the Neville Isdell Chair in African-centric Drug Discovery and Development and thanks N. Isdell for generously funding the Chair.
Author information
Authors and Affiliations
Contributions
V.S. and K.C. designed the content and flow of the paper. V.S. and G.A.D. collected the necessary information and data. V.S., G.A.D. and K.C. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Chemistry thanks Jianping Xie and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Working Group on New TB Drugs: https://www.newtbdrugs.org
Working Group on New TB Drugs — Clinical Pipeline: https://www.newtbdrugs.org/pipeline/clinical
Supplementary information
Glossary
- Auxotrophs
-
Organisms that are unable to synthesize one or more essential growth components.
- Bioavailability
-
Measure of the rate and fraction of the drug dosage that reaches either the site of action or the bodily fluid from which the intended targets of the drug have unimpeded access.
- Bioisosteres
-
Substituents or groups that have chemical or physical similarities and related molecular shapes and may result in similar biological activities.
- Dysbiosis
-
Negative imbalance in the microbial communities of the human body (for example, gut bacteria) that are linked to health problems and diseases.
- Functional foods
-
Foods that offer health benefits beyond their nutritional value, for example, whole, fortified, enriched or enhanced foods.
- Granuloma
-
A distinctive pattern of chronic inflammation characterized by cellular aggregates that assume an epithelioid appearance; although capable of limiting Mycobacterium tuberculosis growth, it also provides a survival niche from which M. tuberculosis may disseminate.
- Latent TB infection
-
A state of persistent anti-Mycobacterium tuberculosis immune response without evidence of clinically manifested active disease.
- Minimum inhibitory concentration
-
(MIC). The lowest concentration of a compound that inhibits ≥90% in vitro growth of Mycobacterium tuberculosis.
- Nutraceuticals
-
Products that are food or part of food providing physiological benefit or protection against chronic disease.
- Persister cells
-
A subpopulation of Mycobacterium tuberculosis that is genetically identical to drug-susceptible M. tuberculosis, but can survive antibiotic treatment.
- Pleiotropic
-
Responsible for or affecting more than one phenotypic characteristic.
- Prototroph
-
Organism that can synthesize its required nutrients from inorganic substances.
- Structure–activity relationship
-
(SAR). An approach designed to investigate relationships between chemical structure and biological activity of studied compounds, allowing the selection and optimization of ideal drug candidates.
- Xenobiotics
-
Chemicals found within an organism that are not naturally produced or expected to be present within the organism and are extrinsic to the normal metabolism of that organism.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, V., Dziwornu, G.A. & Chibale, K. The implication of Mycobacterium tuberculosis-mediated metabolism of targeted xenobiotics. Nat Rev Chem 7, 340–354 (2023). https://doi.org/10.1038/s41570-023-00472-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41570-023-00472-3