Abstract
Climate change is the greatest existential challenge to planetary and human health and is dictated by a shift in the Earth’s weather and air conditions owing to anthropogenic activity. Climate change has resulted not only in extreme temperatures, but also in an increase in the frequency of droughts, wildfires, dust storms, coastal flooding, storm surges and hurricanes, as well as multiple compound and cascading events. The interactions between climate change and health outcomes are diverse and complex and include several exposure pathways that might promote the development of non-communicable diseases such as cardiovascular disease. A collaborative approach is needed to solve this climate crisis, whereby medical professionals, scientific researchers, public health officials and policymakers should work together to mitigate and limit the consequences of global warming. In this Review, we aim to provide an overview of the consequences of climate change on cardiovascular health, which result from direct exposure pathways, such as shifts in ambient temperature, air pollution, forest fires, desert (dust and sand) storms and extreme weather events. We also describe the populations that are most susceptible to the health effects caused by climate change and propose potential mitigation strategies, with an emphasis on collaboration at the scientific, governmental and policy levels.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Intergovernmental Panel on Climate Change. Climate change 2021: the physical science basis–the Working Group I contribution to the sixth assessment report (IPCC, 2021).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
World Health Organization. Protecting health from climate change: vulnerability and adaptation assessment. World Health Organization https://apps.who.int/iris/handle/10665/104200 (2013).
Zanobetti, A. & Peters, A. Disentangling interactions between atmospheric pollution and weather. J. Epidemiol. Community Health 69, 613–615 (2015).
Fu, T.-M. & Tian, H. Climate change penalty to ozone air quality: review of current understandings and knowledge gaps. Curr. Pollut. Rep. 5, 159–171 (2019).
Shi, L., Liu, P., Zanobetti, A. & Schwartz, J. Climate penalty: climate-driven increases in ozone and PM2.5 levels and mortality. Eviron. Epidemiol. 3, 365 (2019).
Fann, N. et al. Ch. 3: Air quality impacts. The impacts of climate change on human health in the United States: A scientific assessment. https://doi.org/10.7930/J0GQ6VP6 (2016).
Stavros, E. N., McKenzie, D. & Larkin, N. The climate-wildfire-air quality system: interactions and feedbacks across spatial and temporal scales. WIREs Clim. Change 5, 719–733 (2014).
Basu, R., Dominici, F. & Samet, J. M. Temperature and mortality among the elderly in the United States: a comparison of epidemiologic methods. Epidemiology 16, 58–66 (2005).
Jaakkola, J. J. K. Case-crossover design in air pollution epidemiology. Eur. Respir. J. Suppl. 40, 81s–85s (2003).
Zafeiratou, S. et al. A systematic review on the association between total and cardiopulmonary mortality/morbidity or cardiovascular risk factors with long-term exposure to increased or decreased ambient temperature. Sci. Total. Environ. 772, 145383 (2021).
Shi, L., Kloog, I., Zanobetti, A., Liu, P. & Schwartz, J. D. Impacts of temperature and its variability on mortality in New England. Nat. Clim. Chang. 5, 988–991 (2015).
Shi, L. et al. Chronic effects of temperature on mortality in the Southeastern USA using satellite-based exposure metrics. Sci. Rep. 6, 30161 (2016).
Rajagopalan, S. & Landrigan, P. J. Pollution and the heart. N. Engl. J. Med. 385, 1881–1892 (2021).
Rajagopalan, S., Al-Kindi, S. G. & Brook, R. D. Air pollution and cardiovascular disease: JACC state-of-the-art review. J. Am. Coll. Cardiol. 72, 2054–2070 (2018).
Münzel, T. et al. Environmental risk factors and cardiovascular diseases: a comprehensive review. Cardiovasc. Res. https://doi.org/10.1093/cvr/cvab316 (2021).
Wyzga, R. E. & Rohr, A. C. Long-term particulate matter exposure: attributing health effects to individual PM components. J. Air Waste Manag. Assoc. 65, 523–543 (2015).
World Health Organization. WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide: executive summary (WHO, 2021).
Jacob, D. J. & Winner, D. A. Effect of climate change on air quality. Atmos. Environ. 43, 51–63 (2009).
Camalier, L., Cox, W. & Dolwick, P. The effects of meteorology on ozone in urban areas and their use in assessing ozone trends. Atmos. Environ. 41, 7127–7137 (2007).
Di, Q. et al. Association of short-term exposure to air pollution with mortality in older adults. JAMA 318, 2446–2456 (2017).
Fann, N. et al. The geographic distribution and economic value of climate change-related ozone health impacts in the United States in 2030. J. Air Waste Manag. Assoc. 65, 570–580 (2015).
Münzel, T. et al. Environmental stressors and cardio-metabolic disease: part I–epidemiologic evidence supporting a role for noise and air pollution and effects of mitigation strategies. Eur. Heart J. 38, 550–556 (2017).
Münzel, T. et al. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur. Heart J. 38, 557–564 (2017).
Rajagopalan, S. & Brook, R. D. Air pollution and type 2 diabetes: mechanistic insights. Diabetes 61, 3037–3045 (2012).
Yang, B.-Y. et al. Ambient air pollution and diabetes: a systematic review and meta-analysis. Environ. Res. 180, 108817 (2020).
Liang, R. et al. Effect of exposure to PM2.5 on blood pressure: a systematic review and meta-analysis. J. Hypertens. 32, 2130–2140 (2014).
Giorgini, P. et al. Air pollution exposure and blood pressure: an updated review of the literature. Curr. Pharm. Des. 22, 28–51 (2016).
Cai, Y. et al. Associations of short-term and long-term exposure to ambient air pollutants with hypertension: a systematic review and meta-analysis. Hypertension 68, 62–70 (2016).
Yang, B.-Y. et al. Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ. Pollut. 235, 576–588 (2018).
Qin, P. et al. Long-term association of ambient air pollution and hypertension in adults and in children: a systematic review and meta-analysis. Sci. Total. Environ. 796, 148620 (2021).
Byrd, J. B. et al. Acute increase in blood pressure during inhalation of coarse particulate matter air pollution from an urban location. J. Am. Soc. Hypertens. 10, 133–139.e4 (2016).
Chen, R. et al. Cardiopulmonary benefits of reducing indoor particles of outdoor origin: a randomized, double-blind crossover trial of air purifiers. J. Am. Coll. Cardiol. 65, 2279–2287 (2015).
Thurston, G. D. et al. Ambient particulate matter air pollution exposure and mortality in the NIH-AARP diet and health cohort. Environ. Health Perspect. 124, 484–490 (2016).
Pinault, L. L. et al. Associations between fine particulate matter and mortality in the 2001 Canadian census health and environment cohort. Environ. Res. 159, 406–415 (2017).
Yin, P. et al. Long-term fine particulate matter exposure and nonaccidental and cause-specific mortality in a large national cohort of Chinese men. Environ. Health Perspect. 125, 117002 (2017).
Orellano, P., Reynoso, J., Quaranta, N., Bardach, A. & Ciapponi, A. Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: systematic review and meta-analysis. Environ. Int. 142, 105876 (2020).
Meng, X. et al. Short term associations of ambient nitrogen dioxide with daily total, cardiovascular, and respiratory mortality: multilocation analysis in 398 cities. BMJ 372, n534 (2021).
Turner, M. C. et al. Long-term ozone exposure and mortality in a large prospective study. Am. J. Respir. Crit. Care Med. 193, 1134–1142 (2016).
Kazemiparkouhi, F., Eum, K.-D., Wang, B., Manjourides, J. & Suh, H. H. Long-term ozone exposures and cause-specific mortality in a US Medicare cohort. J. Expo. Sci. Environ. Epidemiol. 30, 650–658 (2020).
Mustafic, H. et al. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. JAMA 307, 713–721 (2012).
Wolf, K. et al. Long-term exposure to low-level ambient air pollution and incidence of stroke and coronary heart disease: a pooled analysis of six European cohorts within the ELAPSE project. Lancet Planet. Health 5, e620–e632 (2021).
Alexeeff, S. E., Liao, N. S., Liu, X., Van Den Eeden, S. K. & Sidney, S. Long-term PM2.5 exposure and risks of ischemic heart disease and stroke events: review and meta-analysis. J. Am. Heart Assoc. 10, e016890 (2021).
Yang, S. et al. PM2.5 concentration in the ambient air is a risk factor for the development of high-risk coronary plaques. Eur. Heart J. Cardiovasc. Imaging 20, 1355–1364 (2019).
Shah, A. S. V. et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382, 1039–1048 (2013).
Bai, L. et al. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: a population-based study of 5.1 million Canadian adults living in Ontario. Environ. Int. 132, 105004 (2019).
Wang, M. et al. Joint exposure to various ambient air pollutants and incident heart failure: a prospective analysis in UK Biobank. Eur. Heart J. https://doi.org/10.1093/eurheartj/ehaa1031 (2021).
Niu, Z., Liu, F., Yu, H., Wu, S. & Xiang, H. Association between exposure to ambient air pollution and hospital admission, incidence, and mortality of stroke: an updated systematic review and meta-analysis of more than 23 million participants. Environ. Health Prev. Med. 26, 15 (2021).
Stafoggia, M. et al. Long-term exposure to ambient air pollution and incidence of cerebrovascular events: results from 11 European cohorts within the ESCAPE project. Environ. Health Perspect. 122, 919–925 (2014).
Shao, Q. et al. Association between air pollution and development of atrial fibrillation: a meta-analysis of observational studies. Heart Lung 45, 557–562 (2016).
Peralta, A. A. et al. Exposure to air pollution and particle radioactivity with the risk of ventricular arrhythmias. Circulation 142, 858–867 (2020).
Rich, D. Q. et al. Association of short-term ambient air pollution concentrations and ventricular arrhythmias. Am. J. Epidemiol. 161, 1123–1132 (2005).
Folino, F. et al. Association between air pollution and ventricular arrhythmias in high-risk patients (ARIA study): a multicentre longitudinal study. Lancet Planet. Health 1, e58–e64 (2017).
Zhang, Z. et al. Long-term particulate matter exposure and incidence of arrhythmias: a cohort study. J. Am. Heart Assoc. 9, e016885 (2020).
Yang, J. et al. Cardiovascular mortality risk attributable to ambient temperature in China. Heart 101, 1966–1972 (2015).
Baccini, M. et al. Heat effects on mortality in 15 European cities. Epidemiology 19, 711–719 (2008).
Silveira, I. H., Oliveira, B. F. A., Cortes, T. R. & Junger, W. L. The effect of ambient temperature on cardiovascular mortality in 27 Brazilian cities. Sci. Total. Environ. 691, 996–1004 (2019).
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1223–1249 (2020).
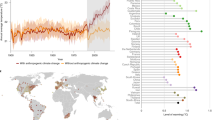
Romanello, M. et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 398, 1619–1662 (2021).
Zhao, Q. et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet. Health 5, e415–e425 (2021).
Benziger, C. P., Roth, G. A. & Moran, A. E. The global burden of disease study and the preventable burden of NCD. Glob. Heart 11, 393–397 (2016).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386, 369–375 (2015).
Gasparrini, A. et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health 1, e360–e367 (2017).
Basu, R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ. Health 8, 40 (2009).
Yu, W. et al. Daily average temperature and mortality among the elderly: a meta-analysis and systematic review of epidemiological evidence. Int. J. Biometeorol. 56, 569–581 (2012).
Gikas, A. et al. Seasonal variation in fasting glucose and HbA1c in patients with type 2 diabetes. Prim. Care Diabetes 3, 111–114 (2009).
Virtanen, K. A. et al. Functional brown adipose tissue in healthy adults. N. Engl. J. Med. 360, 1518–1525 (2009).
Lee, P. et al. Temperature-acclimated brown adipose tissue modulates insulin sensitivity in humans. Diabetes 63, 3686–3698 (2014).
Chondronikola, M. et al. Brown adipose tissue improves whole-body glucose homeostasis and insulin sensitivity in humans. Diabetes 63, 4089–4099 (2014).
Hanssen, M. J. W. et al. Short-term cold acclimation improves insulin sensitivity in patients with type 2 diabetes mellitus. Nat. Med. 21, 863–865 (2015).
Valdés, S. et al. Ambient temperature and prevalence of diabetes and insulin resistance in the Spanish population: Di@bet.es study. Eur. J. Endocrinol. 180, 273–280 (2019).
Speakman, J. R. & Heidari-Bakavoli, S. Type 2 diabetes, but not obesity, prevalence is positively associated with ambient temperature. Sci. Rep. 6, 30409 (2016).
Blauw, L. L. et al. Diabetes incidence and glucose intolerance prevalence increase with higher outdoor temperature. BMJ Open Diabetes Res. Care 5, e000317 (2017).
Sharma, P. & Brook, R. D. Echoes from Gaea, Poseidon, Hephaestus, and Prometheus: environmental risk factors for high blood pressure. J. Hum. Hypertens. 32, 594–607 (2018).
Wang, Q. et al. Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci. Total Environ. 575, 276–286 (2017).
Fedecostante, M. et al. Summer does not always mean lower: seasonality of 24 h, daytime, and night-time blood pressure. J. Hypertens. 30, 1392–1398 (2012).
Brook, R. D. et al. Can personal exposures to higher nighttime and early-morning temperatures increase blood pressure? J. Clin. Hypertens. 13, 881–888 (2011).
Brook, R. D. The environment and blood pressure. Cardiol. Clin. 35, 213–221 (2017).
Halonen, J. I., Zanobetti, A., Sparrow, D., Vokonas, P. S. & Schwartz, J. Outdoor temperature is associated with serum HDL and LDL. Environ. Res. 111, 281–287 (2011).
Bunker, A. et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6, 258–268 (2016).
Gasparrini, A., Armstrong, B., Kovats, S. & Wilkinson, P. The effect of high temperatures on cause-specific mortality in England and Wales. Occup. Environ. Med. 69, 56–61 (2012).
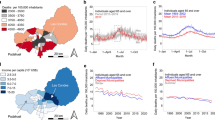
Alahmad, B. et al. Cardiovascular mortality and exposure to heat in an inherently hot region: implications for climate change. Circulation 141, 1271–1273 (2020).
Chen, R. et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ 363, k4306 (2018).
The Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. Lancet 349, 1341–1346 (1997).
Huang, C., Barnett, A. G., Wang, X. & Tong, S. Effects of extreme temperatures on years of life lost for cardiovascular deaths: a time series study in Brisbane, Australia. Circ. Cardiovasc. Qual. Outcomes 5, 609–614 (2012).
Wolf, K. et al. Air temperature and the occurrence of myocardial infarction in Augsburg, Germany. Circulation 120, 735–742 (2009).
Bhaskaran, K. et al. Short term effects of temperature on risk of myocardial infarction in England and Wales: time series regression analysis of the myocardial ischaemia national audit project (MINAP) registry. BMJ 341, c3823 (2010).
Peters, A. & Schneider, A. Cardiovascular risks of climate change. Nat. Rev. Cardiol. 18, 1–2 (2021).
Chen, K. et al. Temporal variations in the triggering of myocardial infarction by air temperature in Augsburg, Germany, 1987-2014. Eur. Heart J. 40, 1600–1608 (2019).
Sun, Z., Chen, C., Xu, D. & Li, T. Effects of ambient temperature on myocardial infarction: a systematic review and meta-analysis. Environ. Pollut. 241, 1106–1114 (2018).
Inglis, S. C. et al. Hot summers and heart failure: seasonal variations in morbidity and mortality in Australian heart failure patients (1994-2005). Eur. J. Heart Fail. 10, 540–549 (2008).
Stewart, S., McIntyre, K., Capewell, S. & McMurray, J. J. V. Heart failure in a cold climate. J. Am. Coll. Cardiol. 39, 760–766 (2002).
Boulay, F., Berthier, F., Sisteron, O., Gendreike, Y. & Gibelin, P. Seasonal variation in chronic heart failure hospitalizations and mortality in France. Circulation 100, 280–286 (1999).
Qiu, H. et al. Is greater temperature change within a day associated with increased emergency hospital admissions for heart failure? Circ. Heart Fail. 6, 930–935 (2013).
Kim, J. & Kim, H. Influence of ambient temperature and diurnal temperature range on incidence of cardiac arrhythmias. Int. J. Biometeorol. 61, 407–416 (2017).
McGuinn, L. et al. Ambient temperature and activation of implantable cardioverter defibrillators. Int. J. Biometeorol. 57, 655–662 (2013).
Zanobetti, A. et al. Fine-scale spatial and temporal variation in temperature and arrhythmia episodes in the VA Normative Aging Study. J. Air Waste Manag. Assoc. 67, 96–104 (2017).
Fries, R. P., Heisel, A. G., Jung, J. K. & Schieffer, H. J. Circannual variation of malignant ventricular tachyarrhythmias in patients with implantable cardioverter-defibrillators and either coronary artery disease or idiopathic dilated cardiomyopathy. Am. J. Cardiol. 79, 1194–1197 (1997).
Pimentel, M., Grüdtner, L. & Zimerman, L. I. Seasonal variation of ventricular tachycardia registered in 24-hour Holter monitoring. Arq. Bras. Cardiol. 87, 403–406 (2006).
Lian, H., Ruan, Y., Liang, R., Liu, X. & Fan, Z. Short-term effect of ambient temperature and the risk of stroke: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 12, 9068–9088 (2015).
Zorrilla-Vaca, A., Healy, R. J. & Silva-Medina, M. M. Revealing the association between cerebrovascular accidents and ambient temperature: a meta-analysis. Int. J. Biometeorol. 61, 821–832 (2017).
Wang, X. et al. Ambient temperature and stroke occurrence: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 13, 698 (2016).
Song, X. et al. Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci. Total. Environ. 586, 241–254 (2017).
Xu, Z., FitzGerald, G., Guo, Y., Jalaludin, B. & Tong, S. Impact of heatwave on mortality under different heatwave definitions: a systematic review and meta-analysis. Environ. Int. 89–90, 193–203 (2016).
Guo, Y. et al. Heat wave and mortality: a multicountry, multicommunity study. Environ. Health Perspect. 125, 087006 (2017).
Cheng, J. et al. Cardiorespiratory effects of heatwaves: a systematic review and meta-analysis of global epidemiological evidence. Environ. Res. 177, 108610 (2019).
Kaiser, R. et al. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am. J. Public. Health 97 (Suppl. 1), S158–S162 (2007).
Semenza, J. C., McCullough, J. E., Flanders, W. D., McGeehin, M. A. & Lumpkin, J. R. Excess hospital admissions during the July 1995 heat wave in Chicago. Am. J. Prev. Med. 16, 269–277 (1999).
Dematte, J. E. et al. Near-fatal heat stroke during the 1995 heat wave in Chicago. Ann. Intern. Med. 129, 173–181 (1998).
Semenza, J. C. et al. Heat-related deaths during the July 1995 heat wave in Chicago. N. Engl. J. Med. 335, 84–90 (1996).
Kovats, R. S. & Kristie, L. E. Heatwaves and public health in Europe. Eur. J. Public. Health 16, 592–599 (2006).
Robine, J.-M. et al. Death toll exceeded 70,000 in Europe during the summer of 2003. C. R. Biol. 331, 171–178 (2008).
Grumm, R. H. The Central European and Russian heat event of July–August 2010. Bull. Am. Meteor. Soc. 92, 1285–1296 (2011).
Shaposhnikov, D. et al. Mortality related to air pollution with the Moscow heat wave and wildfire of 2010. Epidemiology 25, 359–364 (2014).
García-Lledó, A. et al. Heat waves, ambient temperature, and risk of myocardial infarction: an ecological study in the Community of Madrid. Rev. Esp. Cardiol. 73, 300–306 (2020).
Ryti, N. R. I., Guo, Y. & Jaakkola, J. J. K. Global association of cold spells and adverse health effects: a systematic review and meta-analysis. Environ. Health Perspect. 124, 12–22 (2016).
Sartini, C. et al. Effect of cold spells and their modifiers on cardiovascular disease events: evidence from two prospective studies. Int. J. Cardiol. 218, 275–283 (2016).
Pope, C. A. Respiratory disease associated with community air pollution and a steel mill, Utah Valley. Am. J. Public. Health 79, 623–628 (1989).
Pope, C. A., Dockery, D. W., Spengler, J. D. & Raizenne, M. E. Respiratory health and PM10 pollution. a daily time series analysis. Am. Rev. Respir. Dis. 144, 668–674 (1991).
Vanos, J. K., Warland, J. S., Gillespie, T. J. & Kenny, N. A. Review of the physiology of human thermal comfort while exercising in urban landscapes and implications for bioclimatic design. Int. J. Biometeorol. 54, 319–334 (2010).
McGregor, G. R. & Vanos, J. K. Heat: a primer for public health researchers. Public. Health 161, 138–146 (2018).
Armstrong, B. et al. The role of humidity in associations of high temperature with mortality: a multicountry, multicity study. Environ. Health Perspect. 127, 97007 (2019).
Fonseca-Rodríguez, O., Sheridan, S. C., Lundevaller, E. H. & Schumann, B. Effect of extreme hot and cold weather on cause-specific hospitalizations in Sweden: a time series analysis. Environ. Res. 193, 110535 (2021).
Stewart, S., Keates, A. K., Redfern, A. & McMurray, J. J. V. Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. 14, 654–664 (2017).
Liu, C., Yavar, Z. & Sun, Q. Cardiovascular response to thermoregulatory challenges. Am. J. Physiol. Heart Circ. Physiol. 309, H1793–H1812 (2015).
Rohrer, M. J. & Natale, A. M. Effect of hypothermia on the coagulation cascade. Crit. Care Med. 20, 1402–1405 (1992).
Karjalainen, J. & Viitasalo, M. Fever and cardiac rhythm. Arch. Intern. Med. 146, 1169–1171 (1986).
Kunes, J., Tremblay, J., Bellavance, F. & Hamet, P. Influence of environmental temperature on the blood pressure of hypertensive patients in Montréal. Am. J. Hypertens. 4, 422–426 (1991).
Hata, T. et al. The seasonal variation of blood pressure in patients with essential hypertension. Clin. Exp. Hypertens. A 4, 341–354 (1982).
Rose, G. Seasonal variation in blood pressure in man. Nature 189, 235 (1961).
Katayama, Y. et al. Increased plaque rupture forms peak incidence of acute myocardial infarction in winter. Int. J. Cardiol. 320, 18–22 (2020).
Gaudio, F. G. & Grissom, C. K. Cooling methods in heat stroke. J. Emerg. Med. 50, 607–616 (2016).
Epstein, Y. & Yanovich, R. Heatstroke. N. Engl. J. Med. 380, 2449–2459 (2019).
Lim, Y.-H., Park, M.-S., Kim, Y., Kim, H. & Hong, Y.-C. Effects of cold and hot temperature on dehydration: a mechanism of cardiovascular burden. Int. J. Biometeorol. 59, 1035–1043 (2015).
Heidari, L. et al. Susceptibility to heat-related fluid and electrolyte imbalance emergency department visits in Atlanta, Georgia, USA. Int. J. Environ. Res. Public Health 13, 982 (2016).
Prec, O., Rosenman, R., Braun, K., Rodbard, S. & Katz, L. N. The cardiovascular effects of acutely induced hypothermia. J. Clin. Invest. 28, 293–300 (1949).
Covino, B. G. & D’Amato, H. E. Mechanism of ventricular fibrillation in hypothermia. Circ. Res. 10, 148–155 (1962).
Vassallo, S. U., Delaney, K. A., Hoffman, R. S., Slater, W. & Goldfrank, L. R. A prospective evaluation of the electrocardiographic manifestations of hypothermia. Acad. Emerg. Med. 6, 1121–1126 (1999).
Darocha, T. et al. Electrocardiographic changes caused by severe accidental hypothermia. J. Cardiothorac. Vasc. Anesth. 29, e83–e86 (2015).
Xu, R. et al. Wildfires, global climate change, and human health. N. Engl. J. Med. 383, 2173–2181 (2020).
Williams, A. P. et al. Observed impacts of anthropogenic climate change on wildfire in California. Earth’s Future https://doi.org/10.1029/2019EF001210 (2019).
Rappold, A. G., Reyes, J., Pouliot, G., Cascio, W. E. & Diaz-Sanchez, D. Community vulnerability to health impacts of wildland fire smoke exposure. Environ. Sci. Technol. 51, 6674–6682 (2017).
Reid, C. E. et al. Critical review of health impacts of wildfire smoke exposure. Environ. Health Perspect. 124, 1334–1343 (2016).
Cascio, W. E. Wildland fire smoke and human health. Sci. Total Environ. 624, 586–595 (2018).
DeFlorio-Barker, S., Crooks, J., Reyes, J. & Rappold, A. G. Cardiopulmonary effects of fine particulate matter exposure among older adults, during wildfire and non-wildfire periods, in the United States 2008–2010. Environ. Health Perspect. 127, 37006 (2019).
Henderson, S. B., Brauer, M., Macnab, Y. C. & Kennedy, S. M. Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ. Health Perspect. 119, 1266–1271 (2011).
Moore, D. et al. Population health effects of air quality changes due to forest fires in British Columbia in 2003. Can. J. Public. Health 97, 105–108 (2006).
Hanigan, I. C., Johnston, F. H. & Morgan, G. G. Vegetation fire smoke, indigenous status and cardio-respiratory hospital admissions in Darwin, Australia, 1996–2005: a time-series study. Environ. Health 7, 42 (2008).
Delfino, R. J. et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup. Environ. Med. 66, 189–197 (2009).
Mott, J. A. et al. Cardiorespiratory hospitalizations associated with smoke exposure during the 1997, Southeast Asian forest fires. Int. J. Hyg. Environ. Health 208, 75–85 (2005).
Al-Kindi, S. G., Brook, R. D., Biswal, S. & Rajagopalan, S. Environmental determinants of cardiovascular disease: lessons learned from air pollution. Nat. Rev. Cardiol. 17, 656–672 (2020).
Middleton, N. & Kang, U. Sand and dust storms: impact mitigation. Sustainability 9, 1053 (2017).
Wu, Y., Wen, B., Li, S. & Guo, Y. Sand and dust storms in Asia: a call for global cooperation on climate change. Lancet Planet. Health 5, e329–e330 (2021).
Zhang, X. et al. A systematic review of global desert dust and associated human health effects. Atmosphere 7, 158 (2016).
Hashizume, M. et al. Health effects of Asian dust: a systematic review and meta-analysis. Environ. Health Perspect. 128, 66001 (2020).
Tobías, A. & Stafoggia, M. Modeling desert dust exposures in epidemiologic short-term health effects studies. Epidemiology 31, 788–795 (2020).
Vandentorren, S. et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur. J. Public. Health 16, 583–591 (2006).
Son, J.-Y., Liu, J. C. & Bell, M. L. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ. Res. Lett. 14, 073004 (2019).
O’Neill, M. S., Zanobetti, A. & Schwartz, J. Modifiers of the temperature and mortality association in seven US cities. Am. J. Epidemiol. 157, 1074–1082 (2003).
O’Neill, M. S., Zanobetti, A. & Schwartz, J. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J. Urban Health 82, 191–197 (2005).
Hansen, A., Bi, L., Saniotis, A. & Nitschke, M. Vulnerability to extreme heat and climate change: is ethnicity a factor? Glob. Health Action. 6, 21364 (2013).
Moyce, S. C. & Schenker, M. Migrant workers and their occupational health and safety. Annu. Rev. Public. Health 39, 351–365 (2018).
Alahmad, B. et al. Extreme temperatures and mortality in Kuwait: who is vulnerable? Sci. Total. Environ. 732, 139289 (2020).
Achilleos, S. et al. Acute effects of air pollution on mortality: a 17-year analysis in Kuwait. Environ. Int. 126, 476–483 (2019).
United Nations. The Paris Agreement (UN, 2015).
Vicedo-Cabrera, A. M. et al. Temperature-related mortality impacts under and beyond Paris Agreement climate change scenarios. Clim. Change 150, 391–402 (2018).
Lelieveld, J. et al. Effects of fossil fuel and total anthropogenic emission removal on public health and climate. Proc. Natl Acad. Sci. USA 116, 7192–7197 (2019).
Stein, B. A. et al. Preparing for and managing change: climate adaptation for biodiversity and ecosystems. Front. Ecol. Environ. 11, 502–510 (2013).
MacNaughton, P. et al. Energy savings, emission reductions, and health co-benefits of the green building movement. J. Expo. Sci. Env. Epidemiol. 28, 307–318 (2018).
Wheeler, S. M. State and municipal climate change plans: the first generation. J. Am. Plan. Assoc. 74, 481–496 (2008).
Martinez, G. S. et al. Heat-health action plans in Europe: challenges ahead and how to tackle them. Environ. Res. 176, 108548 (2019).
Toloo, G., FitzGerald, G., Aitken, P., Verrall, K. & Tong, S. Evaluating the effectiveness of heat warning systems: systematic review of epidemiological evidence. Int. J. Public. Health 58, 667–681 (2013).
Haddock-Fraser, J. E. & Tourelle, M. Corporate motivations for environmental sustainable development: exploring the role of consumers in stakeholder engagement. Bus. Strat. Environ. 19, 527–542 (2010).
Rajagopalan, S. et al. Personal-level protective actions against particulate matter air pollution exposure: a scientific statement from the American Heart Association. Circulation 142, e411–e431 (2020).
Philipsborn, R. P. et al. Climate change and the practice of medicine: essentials for resident education. Acad. Med. 96, 355–367 (2021).
Kotcher, J. et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet. Health 5, e316–e323 (2021).
Mora, C., Counsell, C. W. W., Bielecki, C. R. & Louis, L. V. Twenty-seven ways a heat wave can kill you: deadly heat in the era of climate change. Circ. Cardiovasc. Qual. Outcomes 10, e004233 (2017).
Acknowledgements
The authors are funded by the Kuwait Foundation for the Advancement of Sciences-KFAS (CR19-13NH-01), the Medical Research Council UK (MR/R013349/1), the Natural Environment Research Council UK (NE/R009384/1) and the European Union’s Horizon 2020 Project Exhaustion (820655). This work was carried out on behalf of the Environmental Cardiovascular Collaborative (EnCC) Group.
Author information
Authors and Affiliations
Contributions
H.K. and A.A. researched data for the article. H.K., B.A., R.L.O. Jr, M.A., S.G.A.-K., A.G. and S.R. contributed to the discussion of its content. H.K., B.A., R.L.O. Jr., A.A., N.V., M.M.C., A.Z. and S.R. wrote the manuscript. H.K., B.A., R.L.O. Jr., A.A., M.A., M.M.C., S.G.A.-K., A.Z., A.G. and S.R. reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Guoxing Li, Annette Peters and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Khraishah, H., Alahmad, B., Ostergard, R.L. et al. Climate change and cardiovascular disease: implications for global health. Nat Rev Cardiol 19, 798–812 (2022). https://doi.org/10.1038/s41569-022-00720-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-022-00720-x
This article is cited by
-
Impact of El Niño on public health and its preparedness measures
Bulletin of the National Research Centre (2024)
-
Geospatial techniques for monitoring and mitigating climate change and its effects on human health
International Journal of Health Geographics (2023)
-
Heat-related mortality in Europe during the summer of 2022
Nature Medicine (2023)
-
Mortality risks from a spectrum of causes associated with sand and dust storms in China
Nature Communications (2023)
-
Diabetes and climate change: current evidence and implications for people with diabetes, clinicians and policy stakeholders
Diabetologia (2023)