Abstract
Patients with heart failure are at a higher risk of cardiovascular events compared with the general population, particularly during domestic or international travel. Patients with heart failure should adhere to specific recommendations during travel to lower their risk of developing heart failure symptoms. In this Review, we aim to provide clinicians with a set of guidelines for patients with heart failure embarking on national or international travel. Considerations when choosing a travel destination include travel distance and time, the season upon arrival, air pollution levels, jet lag and altitude level because all these factors can increase the risk of symptom development in patients with heart failure. In particular, volume depletion is of major concern while travelling given that it can contribute to worsening heart failure symptoms. Pre-travel risk assessment should be performed by a clinician 4–6 weeks before departure, and patients should receive advice on potential travel-related illness and on strategies to prevent volume depletion. Oxygen supplementation might be useful for patients who are very symptomatic. Upon arrival at the destination, potential drug-induced photosensitivity (particularly in tropical destinations) and risks associated with the local cuisine require consideration. Special recommendations are needed for patients with cardiac implantable electronic devices or left ventricular assist devices as well as for those who have undergone major cardiac surgery.
Key points
-
Patients with heart failure (HF) are recommended to schedule a specialist consultation for pre-travel risk assessment 4–6 weeks before departure.
-
Preparation for travel requires special considerations in patients with HF, including the choice of destination, availability of medical resources and strategies to prevent volume depletion.
-
Most patients with HF can travel when medically stable; patients with a ground-level oxygen saturation ≤90% or those in NYHA class III–IV might need an on-board medical oxygen supply.
-
All medication and important documents should be stored in carry-on luggage.
-
Volume depletion and dehydration are important considerations requiring meticulous attention with regards to medication adjustment and fluid intake.
-
Patients with implantable cardiac devices might require extra time at security checkpoints and additional documents; for some patients, remote monitoring of implantable cardiac devices might be useful.
Similar content being viewed by others
Introduction
Domestic and international travel are associated with increased health risks, with 20–70% of individuals reporting health issues during their travels1. During international travel, 1–5% of individuals seek medical attention and the rate of death among travellers is 1 in 100,000, with cardiovascular disease being the most frequent cause of death1. Trauma, particularly from motor vehicle accidents, is another major cause of death while travelling1. Health-care providers are frequently approached by patients for advice on how to prepare for travel or to determine whether travelling is advisable at all. General practitioners can provide information to healthy individuals but specialist consultation is of benefit for patients with underlying illnesses such heart failure (HF)2. Indeed, many patients with HF intend to travel for business or leisure. Although some guidance has been published3, a systematic overview of recommendations for patients with HF planning to travel is not yet available. In this Review, we aim to provide clinicians with recommendations for preparatory measures before travel to inform and educate patients with HF. We discuss factors that might increase the risk of HF symptom development, such as local climate, air pollution levels and altitude levels, and provide specific guidance for patients with a cardiac implantable device and those who have undergone major surgery.
Which patients with HF can travel safely?
To date, guidance on travel recommendations for patients with HF is limited. In general, patients with NYHA class I–III HF who are stable should be able to travel safely4. However, patients with NYHA class III HF who are planning to travel by air should be advised to consider on-board medical oxygen support. Patients with NYHA class IV should not travel; however, if travel is unavoidable, on-board oxygen and medical assistance should be requested. A patient with an oxygen saturation rate >90% at ground level usually will not require medical oxygen during flight5. An overview of whether travelling is advisable for different classes of HF6,7 is provided in Box 1. An overview of contraindications for air travel in patients with cardiovascular diseases is provided in Box 2.
Choice of destination
The choice of destination for travel can have important health implications for patients with HF, particularly when travelling abroad. Considerations include the local climate, air pollution levels, altitude levels, the season upon arrival, the distance and time for travelling, jet lag, and vaccines required.
Effects of transitioning climates on HF
Individuals who transition through climates different to the one they reside in (such as someone living in the arctic travelling to a tropical island) are at an increased health risk. In general, people living in warmer regions tend to be most vulnerable to cold weather and, conversely, those residing in a cold climate are most sensitive to heat8. Exposure to extreme heat has been associated with increased morbidity and mortality from heat exhaustion and heat stroke9,10. Maintenance of homeostasis during hot weather requires an increase in cardiac output; heat tolerance is impaired when cardiac output cannot be increased to meet the requirements of heat loss. Numerous medications that are frequently prescribed for individuals with HF can also increase susceptibility to heat stroke, including loop diuretics, serotonic antidepressants, angiotensin-converting enzyme inhibitors and proton-pump inhibitors11,12,13. Colder temperatures are less likely to have effects on cardiovascular health but have been associated with increased morbidity among patients with respiratory disease14. Patients with HF should be advised to choose either spring or autumn for international travel to avoid travelling during extremities in weather and to adjust medications that can contribute to volume depletion. Appropriate clothing is required for the site of departure, the destination and for the journey itself. Given the challenges in contacting a patient’s primary care physician if the patient is in a different country or continent, distant travel destinations might only be advisable for patients who are well-informed about their medication regimen, dietary restrictions and exercise limitations.
Endemic diseases
The need for immunization for travel depends on the destination. In general, the status of routine vaccinations, such as the diphtheria, measles–mumps–rubella, pertussis, tetanus and varicella vaccines, should be checked before travelling abroad. For all patients with HF, vaccines are required for pneumococcal disease, influenza and coronavirus disease 2019 (COVID-19). Other destination-dependent vaccines are provided in Table 1.
Air pollution and HF
Air pollution can be measured by the air quality index, which integrates measures for the five main air pollutants: ground-level ozone, particulate matter, carbon monoxide, sulfur dioxide and nitrogen dioxide. An air quality index value of 0–50 indicates good air quality, 51–100 indicates moderately polluted air, >100 indicates an unhealthy level of air pollution and >300 designates a hazardous environment15. Particulate matter (PM) of ≤10 µm (PM10) or ≤2.5 µm (PM2.5) in diameter are linked with increased cardiopulmonary mortality16,17 as well as with an increased risk of hospitalization for HF18 and death19. The pathophysiological mechanisms underlying this increased risk remain elusive. Accumulating evidence points towards a crucial role of PM-induced systemic oxidative stress20 and endothelial dysfunction21 in the development of arterial vasoconstriction and elevated systemic blood pressure22. In addition, PM-induced pulmonary vasoconstriction results from increases in pulmonary and right ventricular diastolic filling pressures, which affect right ventricular performance22. Given that the effects of air pollutants on cardiovascular performance and outcomes can occur within hours or days of exposure23, patients with HF should be advised to avoid travelling to locations with high levels of air pollution.
Altitude-induced hypoxia and HF
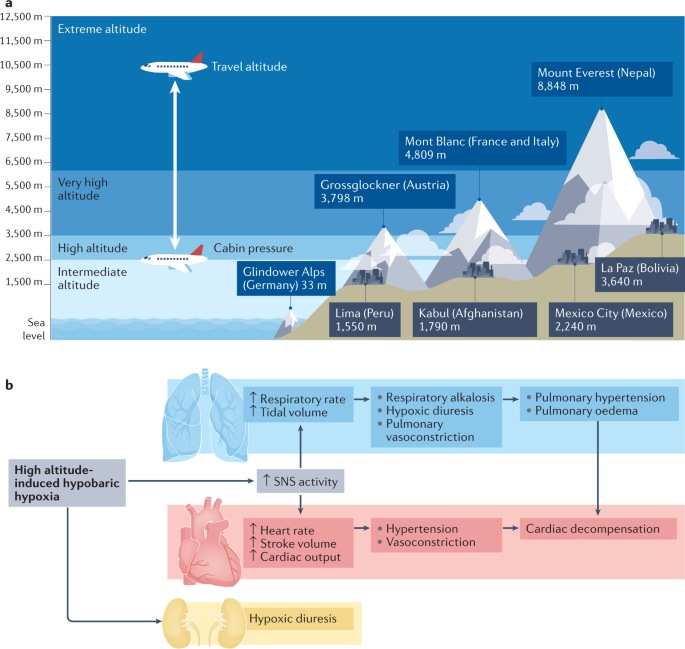
Patients with HF are more susceptible to the physiological changes induced by high altitude exposure than the general population24. During air travel, cabin pressure is required to be no less than the barometric pressure at an altitude of 2,438 m (8,000 ft), which is classified as an intermediate altitude25 (Fig. 1a). Cabin pressures usually remain higher than this altitude, particularly during long-haul flights26. Travel to high altitude locations that are >2,500 m above sea level triggers physiological acclimatization processes within the cardiocirculatory and pulmonary systems27,28 (Fig. 1b). These processes are initiated by a gradual decrease in barometric pressure, which in turn lowers the partial pressure of oxygen in inspired air. Hypobaric hypoxia leads to a fast increase in respiratory rate and tidal volume29, which leads to respiratory alkalosis and hypoxic diuresis30. Hypoxia induces pulmonary vasoconstriction and eventual pulmonary hypertension, an important trigger for high altitude pulmonary oedema31. To compensate for the lower arterial oxygen content, heart rate and stroke volume are increased via activation of the sympathetic nervous system26,32,33,34. Together, these physiological adaptations limit the exercise capacity of patients with HF and make them prone to cardiac decompensation. However, studies that assessed simulated altitude-induced hypoxia in patients with NYHA class III–IV HF showed that high altitude was not associated with angina, arrhythmia, or ischaemia35,36 and that the degree of the reduction of maximum work capacity was dependent on the individual’s exercise tolerance at sea level35. The ESC and other professional societies recommend that the assessment of safety of high altitude exposure for patients with HF should depend on their functional capacity (that is, NYHA class) at sea level35,37. Furthermore, certain drugs that are prescribed to patients with HF can further interfere with the physiological adaptation processes at high altitudes. For example, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can reduce renal erythropoietin production, thereby hampering the compensatory rise in haematocrit mediated by altitude-induced hypoxia38. Therefore, diuretic therapy should be tailored to the individual to account for clinical signs of dehydration (such as through hypoxic diuresis) or fluid gain39. Finally, anaemia reduces oxygen delivery, and muscle loss (present in patients with sarcopenia or cachexia) reduces maximal physical workload and time to fatigue; patients with these conditions in addition to HF need to have special considerations when planning to travel to high altitude locations. To summarize, travel to destinations at an intermediate altitude (~2,000 m) is safe for patients with HF who have good exercise tolerance at sea level.
a | Definitions of height and examples of mountains and cities at different altitudes. Most aircraft fly at approximately 10,000–12,000 m (33,000–42,000 ft) above sea level, with the cabin pressurized to an equivalent of 2,438 m (8,000 ft). b | High altitude-induced hypobaric hypoxia leads to an increase in respiratory rate and tidal volume, which promotes respiratory alkalosis, hypoxic diuresis, pulmonary vasoconstriction and, ultimately, pulmonary hypertension and pulmonary oedema. Compensatory mechanisms of this hypoxia include increases in heart rate and stroke volume via activation of the sympathetic nervous system (SNS). Together, these changes can limit exercise capacity and promote cardiac decompensation.
Seasonal variations and HF
Hospitalizations owing to worsening HF show intriguing seasonality, with a substantial decline during warmer periods and an increase during colder periods18,40, especially in older patients41. Temperature had the greatest (inverse) correlation with hospitalizations for HF among other causative environmental factors such as humidity, precipitation or irradiation16. Skin cooling has been shown to increase vascular resistance42 and plasma noradrenaline concentration43, which might lead to HF decompensation. Beyond neurohumoural activation and haemodynamic stress, respiratory infections, which peak during the colder months, can precipitate and aggravate HF symptoms41. Furthermore, vitamin D insufficiency during winter has also been linked to worsening HF44. Interestingly, the effect of seasonal variability on health is more prominent in elderly people and winter hospitalization is associated with both poorer short-term and long-term prognosis41. These observations suggest that patients with more severe HF (and worse prognosis) are prone to decompensation during winter and that these patients and older patients with more advanced disease should be advised to avoid travelling to colder regions. Of note, a study from Norway reported that the Christmas winter period was associated with the highest rates of excess all-cause and cardiovascular deaths45. Overall, appropriate clothing and heating strategies need to be carefully selected for optimal stabilization of body core temperatures, vitamin D levels should be measured before departure and supplemented if required, and vaccines against influenza and pneunococcal disease should be administered40 (Table 1).
Preparing to travel
Any patient with a history of HF should seek medical consultation before departure, particularly when travelling overseas or when leaving for a long period. Women are generally more likely to seek pre-travel medical advice than men46 and are also more likely to have travel-related worries47. A cross-sectional national survey found that a low perceived need was among the main causes for avoiding medical care, often because patients expected their illness or symptoms to improve over time48. For patients with HF, travel preparation should include a specialist consultation approximately 4–6 weeks before departure. This consultation should follow a structured and sequenced approach, which should involve risk assessment (including an evaluation of medical history and travel itinerary), interventions required before departure (including physical examination or setting up of remote monitoring for cardiac implantable devices) and focused education on topics such as medications and factors that can lead to volume depletion. For example, the presence of anaemia might cause lightheadedness, angina or loss of consciousness, particularly during flights49,50. Medication regimens should be optimized before departure and patients with iron deficiency should be considered for repletion therapy. Suggestions for topics to cover during this consultation are summarized in Box 3.
Risk assessment and medication adjustment
As mentioned in the previous section, pre-travel risk assessment should consider the type and duration of travel, the travel destination, and the medical history of the patient. Typical health emergencies that patients with HF might encounter during travel are listed in Table 2. Patients should be advised that provision of incomplete medical information during a cardiac emergency might increase the risk of death. Any accompanying travellers need to know where to find important documents (Box 4) in case of an emergency. Given the difficulty in obtaining prescription drugs in a different country as well as the different brands of drugs having varying strengths in different countries, extra medication should be brought on the trip. Importantly, some over-the-counter drugs might be legal in the patient’s home country but illegal elsewhere (such as certain analgesics).
Remote device monitoring
Remote monitoring is recommended by the ESC and other professional societies for patients with cardiac implantable devices such as pacemakers, implantable cardioverter–defibrillators (ICDs) and implantable cardiac monitors51,52,53. Most remote monitoring systems use a transmitter (base station) placed in the vicinity of the implanted device, with information sent via an internet connection to a remote monitoring service. Alternatively, alerts can be activated after events that trigger an immediate remote transmission (for example, after ICD shock, detection of ventricular tachyarrhythmias or signs of lead failure). Given that travelling is usually associated with increased physical activity levels, daily remote monitoring might be useful for the detection of events such as arrhythmias, HF decompensation or device malfunction (Box 5).
Special considerations
Patients who have undergone recent surgery
Major cardiac surgery ranges from minimally invasive approaches to complete sternotomy. The Canadian Cardiac Society guidelines on air travel recommend that patients with a haemoglobin level <9 g/dl who have undergone coronary artery bypass graft surgery should be advised against air travel54; recommendations for travel in patients with HF who have undergone coronary artery bypass graft surgery should perhaps be even more conservative. These patients should be advised not to travel by air until intrathoracic gas resorption is completed given that gas expands when air pressure is reduced with increasing altitude (the Boyle law)4. Gas resorption usually takes 3–10 days after surgery. Any air remaining in the pericardial space or in the thoracic cavity can expand by up to 60%, which might be dangerous and painful4. Indeed, the Aerospace Medical Association guidelines state that pneumothorax is an absolute contraindication to air travel and advocate an interval of 2–3 weeks before flying after thoracic surgery5. Furthermore, patients who have had a recent operation are in a state of increased oxygen consumption owing to the trauma of surgery, possible presence of sepsis and increased adrenergic outflow. A 2017 study compared complication rates between ground and air travel 5–25 days after pulmonary resection55. Air travel was as safe as ground travel if the chest tubes were removed after the absence of ongoing air leak and an output <300 ml over 24 hours combined with adequate pain medication and an active ambulation schedule.
Patients with LVADs
Left ventricular assist devices (LVADs) are increasingly implanted as a bridging strategy while patients wait for heart transplantation or as a permanent therapy for end-stage HF. Patients in either category can travel by air if medically stable and rehabilitation measures have been performed56. Box 6 lists precautions before and during travel for patients with an LVAD.
Considerations while en route
Departure from home
Patients with HF or ischaemic heart disease need to take extra caution on the way to and from the departure point, such as an airport or train station, given the multitude of stressors: commotion, a delay or any last-minute changes to the train or flight, and lifting of heavy luggage, all of which can increase physical and mental exertion and risk of myocardial ischaemia57,58. As such, travel planning should include estimation of psychological stressors and physical loads as well as a plan for any emergencies (Table 2). Pre-planned assistance with luggage or transport by wheelchair at the point of departure might reduce pre-travel stress and physical exhaustion.
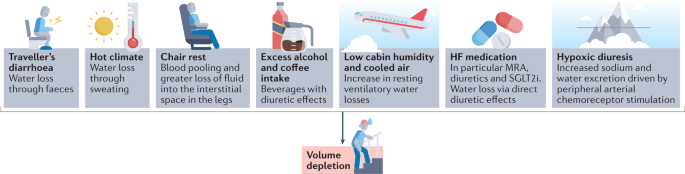
Dehydration and fluid intake
Patients with HF are susceptible to volume depletion during travel given that fluid intake, lifestyle and diuretics are tuned precisely to maintain a state of euvolaemia59 (Fig. 2). A hypovolaemic state adversely affects cardiac and renal function, aggravates HF symptoms, and might interfere with the efficacy of HF medications. Fluid loss, caused by changes in temperature, diet (higher salt intake) or as a consequence of traveller’s diarrhoea, might occur during the flight.
On board a plane, the low cabin humidity and cooled air can increase resting ventilatory water losses by approximately 200 ml per hour60. In addition, chair rest immobilization for 4 hours can decrease plasma volume by approximately 6% as a result of blood pooling and greater loss of fluid within the interstitial space in the legs60. Urinary output is often normal or only slightly reduced61. Sodium-free, alcoholic or caffeine-containing drinks consumed during the flight can promote diuresis and might further increase fluid loss. Furthermore, arrival to a hot and dry climate can result in loss of fluid through sweating and breathing by up to 1.2 l per day independently of physical activity62.
Apart from air travel and a transition in climate, acute diarrhoea is the most common illness in individuals travelling from resource-rich to resource-limited regions of the world63,64. Traveller’s diarrhoea usually occurs 4–14 days after arrival and results from bacterial (>90% of cases), viral and parasitic infections64. Approximately 10–40% of travellers to high-risk regions in Asia, Africa, and South and Central America experience diarrhoea during their travels64. Patients should be educated on food and water safety to prevent ingestion of pathogens. Cardiac dysfunction and HF management and treatment strategies, such as fluid restriction, diuretic therapy and renin–angiotensin–aldosterone system (RAAS) inhibitors, also increase the risk of diarrhoea-related complications in patients with HF during (temporal) hypovolaemia63,64.
Signs and symptoms of volume depletion and dehydration-associated electrolyte or acid–base disorders include fatigue, exercise intolerance, weight loss, increase in heart rate, muscle cramps, weakness, postural dizziness, abdominal pain, low urine volume, low blood pressure, lethargy and confusion. On the basis of invidualized risk assessment, patients should be advised to increase fluid intake by 0.5–1 l per day and to avoid alcohol or excessive coffee consumption during long-haul flights and hot weather. In case of signs and symptoms of volume depletion, therapy with diuretics, mineralocorticoid receptor antagonists and sodium–glucose cotransporter 2 inhibitors should be stopped or reduced for a day or longer until symptoms have resolved and body weight has returned to normal65. In case of postural or symptomatic hypotension, therapy with RAAS inhibitors and angiotensin receptor blocker–neprilysin inhibitors should be reduced or discontinued until symptoms have resolved; patients who experience postural or symptomatic hypotension require medical evaluation.
In a hot environment, patients with HF are advised to restrain from strenuous activity to avoid increased fluid loss. In case of uncomplicated traveller’s diarrhoea, patients need to increase fluid intake with oral rehydration solutions and monitor body weight and urinary output to avoid dehydration. Given that patients with HF are at an increased risk of complications, an antimotility agent (loperamide) and an antibiotic (azithromycin or rifaximin) can be prescribed for self-treatment63,64.
Venous thromboembolism
The risk of deep venous thrombosis (DVT) is greatly increased in patients with incident HF according to data from the ARIC cohort66 and a systematic review67. The term ‘economy class syndrome’ has been used to describe the venous complications caused by cramped seating conditions68. The risk of DVT or pulmonary embolism is increased during travel that is >4 hours in duration, most probably owing to the associated immobility that is a key component of the Virchow triad of hypercoagulability, stasis and endothelial injury. Travelling in general (>4 hours in the preceding 8 weeks) is associated with a twofold increase in the risk of venous thrombosis69. This risk seems to be similar regardless of the mode of transportation (airplane, bus or train)67. The overall absolute incidence of symptomatic venous thromboembolism (VTE) in healthy individuals within the first month after a flight lasting >4 hours is approximately 1 in 4,600 flights and increases by 18% for each additional 2 hours in flight duration2,70. Importantly, the risk of VTE in individuals with pro-thrombotic risk factors, such as chronic HF, is substantially higher than in the general population. A 2021 meta-analysis found that patients with chronic HF were at an increased risk of VTE (risk ratio 1.57, 95% CI 1.34–1.84)71. A window seat compared with an aisle seat has been associated with a twofold greater risk of VTE or a sixfold greater risk in individuals with a BMI of >30 kg/m2 (ref.72).
Strategies to prevent VTE include appropriate loose clothing, frequent walks, calf muscle exercises, use of elastic compression stockings and adequate hydration73. Leg exercises have been shown to improve popliteal venous flow during prolonged immobility in seated individuals74. Furthermore, a systematic review of 11 randomized trials that included 2,906 individuals revealed the benefits of compression stockings (15–30 mmHg) on reducing the incidence of asymptomatic DVT and, with less evidence, of leg oedema75.
The evidence for thromboprophylaxis to prevent VTE during travel is very limited. The LONFLIT-3 study76 randomly assigned 300 individuals at high risk of flight-related VTE to receive aspirin, enoxaparine (a low-molecular-weight heparin) or no prophylaxis. In total, 4.8% of patients in the control group were diagnosed with asymptomatic DVT compared with 3.6% in the aspirin group and 0% in the enoxaparine group. The authors of this small study concluded that one dose of enoxaparine might be an important option for individuals at high risk of DVT during long-haul flights76. Of note, specific studies of thromboprophylaxis during long-haul travel in patients with HF are lacking.
Medical emergencies during air travel
Patients with HF can travel by air if their condition is stable (Box 1). Commercial airplanes are required to carry basic emergency medical equipment according to regulations of the Federal Aviation Administration (FAA) in the USA and the European Aviation Safety Agency (EASA) in Europe77. Commercial aircrafts travelling from Europe to the USA have to meet both FAA and EASA requirements and, thus, must carry on board an external automated defibrillator, a saline infusion system and a bag-valve mask resuscitator77.
Data on on-board medical emergencies are sparse owing to the lack of international registries78. According to the available data provided by the airline Lufthansa, which contains details on approximately 20,000 on-board medical events from 2000 to 2011, cardiac emergencies accounted for 43% of on-board incidents77. Reported medical issues included circulatory collapse, high blood pressure, chest symptoms and dehydration47. On-board treatment included blood pressure management in 76% of incidents, drug administration in 54%, oxygen delivery in 48%, blood glucose measurement in 9%, monitoring of oxygen saturation in 6% and use of an automated external defibrillator in 6%77.
Considerations at the destination
Dietary considerations
Dietary intake of fluids, sodium, potassium and alcohol during travel should be guided by current ESC recommendations for the management of patients with HF3,79. According to the guidelines, fluid restriction of 1.5–2.0 l per day might be considered in patients with severe HF to relieve symptoms and congestion80. When travelling to hot and dry destinations, an additional intake of 0.5–1.0 l per day of non-alcoholic drinks is recommended. Patients at risk of volume overload or on moderate-to-high doses of diuretics should be advised to regularly check their body weight. In case of body weight changes, patients can adjust doses of diuretics and the amount of fluid intake for a few days until body weight has normalized. Controlling sodium intake is important for patients at risk of hyponatraemia and for the management of oedema, although evidence showing the effects of sodium intake on HF outcomes is scarce3. During travel, increased consumption of foods high in salt can adversely affect sodium and volume balance and thereby exacerbate HF symptoms by causing fluid retention. Patients with HF and cardiorenal syndrome and/or treated with RAAS inhibitors are at increased risk of hyperkalaemia81. In patients with advanced chronic kidney disease (estimated glomerular filtration rate <30 ml/min/1.73 m²), a daily sodium intake of <3 g is recommended81. These patients should also be aware that certain foods, such as fresh fruits, juices, vegetables and milk products, contain high amounts of potassium.
Drinking habits also change during vacation. Moderate-to-heavy alcohol consumption is associated with increased risk of supraventricular arrhythmias, especially atrial fibrillation, and high blood pressure82,83. Therefore, increased intake of alcoholic beverages might aggravate HF symptoms and promote volume overload. Alcohol intake should be limited to two units per day for men with HF, one unit for women with HF, or no intake if alcohol has caused or contributed to the individual’s HF, as recommended by the ESC3.
Drug-induced photosensitivity
Numerous classes of drugs commonly used for the treatment of patients with HF have been associated with photo-induced, cutaneous drug eruptions, which are adverse effects that occur as a result of the exposure to a drug (and its presence in the skin) and ultraviolet or visible radiation84. Box 7 provides an overview of drugs that have been linked with drug-induced photosensitivity. Amiodarone can cause drug-induced photosensitivity in >50% of treated patients84. The typical presentation of this adverse effect is a burning and tingling sensation in sun-exposed skin, with associated erythema. Amiodarone induces a distinctive blue–grey pigmentation on sun-exposed sites in 1–2% of patients, particularly after long-term sun exposure. Another prototypical drug class associated with photosensitivity is thiazide diuretics, which includes hydrochlorothiazide85. Thiazide diuretics can trigger a variety of photosensitive eruptions, including an exaggerated sunburn reaction, dermatitis and a lichenoid eruption.
Various factors, such as time of day, season, geographical location, altitude and weather conditions, can affect the amount of ultraviolet radiation exposure86. In general, patients with HF should be advised to seek shade when outside, in particular around midday, and to keep in mind that radiation can be stronger when reflected by water, sand or snow. Patients in areas with high sun exposure should wear clothing that protects as much of the body as possible as well as sunglasses and broad-brimmed hats. Broad-spectrum sunscreens with a sun protection factor of 30 or higher are recommended86.
Considerations for drivers
Driving regulations for individuals with HF take into account the severity of HF (NYHA class plus left ventricular ejection fraction)54. In the European Union, individuals with NYHA class I–III HF but not those with NYHA class IV HF are permitted to drive private vehicles. Patients with HF should ensure that they are permitted to drive in their travelling destination by accessing country-specific driving regulations online.
Considerations for patients with ICDs
Electromagnetic interference
Many patients with HF are fitted with cardiac implantable electronic devices (CIEDs; namely ICDs), cardiac resynchronization therapy devices or pacemakers. These devices might be subject to electromagnetic interference (EMI) if exposed to a strong electromagnetic field (Table 3). Exposure of the device to EMI can result in device failure (loss of anti-bradycardia pacing with the risk of asystole), switch to asynchronous mode (pacing at a preset rate independent of intrinsic rhythm with the risk of inducing arrhythmias, including ventricular fibrillation), inappropriate tracking (atrial oversensing leading to rapid, irregular ventricular pacing) and in the inappropriate detection of ventricular tachyarrhythmias by ICDs, potentially with inappropriate shock therapy. High-voltage lines above trains, for example, have a strong electromagnetic field but the patient is shielded when inside the train. In trams or underground trains, electric motors can be located under the seat, whereas in cars and motorbikes, the only relevant source of EMI is the ignition system. Patients with a cardiac implantable device should be careful not lean over an unshielded, running motor.
Air travel
Metal detectors at airport security checkpoints do not interfere with CIEDs87,88. However, patients with ICDs should be advised to have their device card ready to show to airport personnel before walking through the security checkpoint. To minimize the risk of interference, patients should move through metal detector gates at normal walking speed and should not linger. Hand-held scanners should not affect CIED functionality89 but patients should ask personnel to move the wand over the device quickly and only once.
Magnets are not allowed in carry-on luggage and thus cannot be used to remedy inappropriate device activity on airplanes. EMI inside airplanes is rare but has been reported, for example, in association with electronic chair handles. Finally, cosmic radiation is approximately 100-fold higher during air travel, which increases the risk of radiation-induced EMI (for example, power-on reset).
Conclusions
The list of considerations for patients with HF embarking on national or international travel is extensive. Patients should be aware of an increased risk of cardiovascular events during their travels, which can be reduced with meticulous pre-travel risk assessment, physical examination, therapy adjustment and education. Pre-travel risk assessment should involve research into the local climate, air pollution levels, the distance and time for travelling, potential jet lag and altitude. En route, patients with HF should avoid volume depletion caused by extended chair rest, low cabin humidity and cooled air, excess alcohol or coffee intake, drugs with diuretic effects, hypoxia or traveller’s diarrhoea. Upon arrival at the destination, drug-induced photosensitivity and the health effects of local foods and beverages require consideration. Special recommendations are needed for patients after implantation of cardiac rhythm devices or LVADs as well as for patients who have undergone major cardiac surgery.
References
Ryan, E. T. & Kain, K. C. Health advice and immunizations for travelers. N. Engl. J. Med. 342, 1716–1725 (2000).
Freedman, D. O., Chen, L. H. & Kozarsky, P. E. Medical considerations before international travel. N. Engl. J. Med. 375, 247–260 (2016).
Jaarsma, T. et al. Self-care of heart failure patients: practical management recommendations from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 23, 157–174 (2021).
Smith, D. et al. Fitness to fly for passengers with cardiovascular disease. Heart 96 (Suppl. 2), ii1–ii16 (2010).
Aerospace Medical Association. Medical considerations for airline travel: surgical conditions (ASMA, 2021).
Dharmarajan, K. et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ 350, h411 (2015).
Alba, C. et al. Complications after heart transplantation: hope for the best, but prepare for the worst. Int. J. Transpl. Res. Med. 2, 022 (2016).
Curriero, F. C. et al. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 155, 80–87 (2002).
De Blois, J. et al. The effects of climate change on cardiac health. Cardiology 131, 209–217 (2015).
Kenny, G. P., Yardley, J., Brown, C., Sigal, R. J. & Jay, O. Heat stress in older individuals and patients with common chronic diseases. CMAJ 182, 1053–1060 (2010).
Bouchama, A. & Knochel, J. P. Heat stroke. N. Engl. J. Med. 346, 1978–1988 (2002).
Faunt, J. D. et al. The effete in the heat: heat-related hospital presentations during a ten day heat wave. Aust. N. Z. J. Med. 25, 117–121 (1995).
Sommet, A., Durrieu, G., Lapeyre-Mestre, M., Montastruc, J. L. & Association of French PharmacoVigilance Centres. A comparative study of adverse drug reactions during two heat waves that occurred in France in 2003 and 2006. Pharmacoepidemiol. Drug Saf. 21, 285–288 (2012).
McCormack, M. C. et al. Colder temperature is associated with increased COPD morbidity. Eur. Respir. J. 49, 1601501 (2017).
AirNow. Air Quality Index (AQI) basics. AirNow https://airnow.gov/index.cfm?action=aqibasics.aqi (2019).
Miller, K. A. et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N. Engl. J. Med. 356, 447–458 (2007).
Pope, C. A. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287, 1132–1141 (2002).
Escolar, V. et al. Impact of environmental factors on heart failure decompensations. ESC Heart Fail. 6, 1226–1232 (2019).
Shah, A. S. et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382, 1039–1048 (2013).
Barregard, L. et al. Experimental exposure to wood-smoke particles in healthy humans: effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal. Toxicol. 18, 845–853 (2006).
Törnqvist, H. et al. Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am. J. Respir. Crit. Care Med. 176, 395–400 (2007).
Wold, L. E. et al. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ. Heart Fail. 5, 452–461 (2012).
Tofler, G. H. & Muller, J. E. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation 114, 1863–1872 (2006).
Higgins, J. P., Tuttle, T. & Higgins, J. A. Altitude and the heart: is going high safe for your cardiac patient? Am. Heart J. 159, 25–32 (2010).
US Office of the Federal Register. Code of Federal Regulations: Title 14 aeronautics and space, part 25.841 (US Government Printing Office, 1986).
Seccombe, L. M. & Peters, M. J. Physiology in medicine: acute altitude exposure in patients with pulmonary and cardiovascular disease. J. Appl. Physiol. 116, 478–485 (2014).
Imray, C., Booth, A., Wright, A. & Bradwell, A. Acute altitude illnesses. BMJ 343, d4943 (2011).
Bärtsch, P. & Gibbs, J. S. Effect of altitude on the heart and the lungs. Circulation 116, 2191–2202 (2007).
Jones, J. G., Bakewell, S. E., Heneghan, C. P., Jones, S. E. & Snape, S. L. Profound hypoxemia in pulmonary patients in airline-equivalent hypoxia: roles of VA/Q and shunt. Aviat. Space Env. Med. 79, 81–86 (2008).
Sawka, M. N., Convertino, V. A., Eichner, E. R., Schnieder, S. M. & Young, A. J. Blood volume: importance and adaptations to exercise training, environmental stresses, and trauma/sickness. Med. Sci. Sports Exerc. 32, 332–348 (2000).
Cheung, S. S. et al. Ventilatory chemosensitivity, cerebral and muscle oxygenation, and total hemoglobin mass before and after a 72-day mt. Everest expedition. High Alt. Med. Biol. 15, 331–340 (2014).
Hughson, R. L., Yamamoto, Y., McCullough, R. E., Sutton, J. R. & Reeves, J. T. Sympathetic and parasympathetic indicators of heart rate control at altitude studied by spectral analysis. J. Appl. Physiol. 77, 2537–2542 (1994).
Vogel, J. A. & Harris, C. W. Cardiopulmonary responses of resting man during early exposure to high altitude. J. Appl. Physiol. 22, 1124–1128 (1967).
Heistad, D. D., Abboud, F. M. & Dickinson, W. Richards Lecture: circulatory adjustments to hypoxia. Circulation 61, 463–470 (1980).
Agostoni, P. et al. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am. J. Med. 109, 450–455 (2000).
Negrao, C. E. & Middlekauff, H. R. Adaptations in autonomic function during exercise training in heart failure. Heart Fail. Rev. 13, 51–60 (2008).
Parati, G. et al. Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: a joint statement by the European Society of Cardiology, the Council on Hypertension of the European Society of Cardiology, the European Society of Hypertension, the International Society of Mountain Medicine, the Italian Society of Hypertension and the Italian Society of Mountain Medicine. Eur. Heart J. 39, 1546–1554 (2018).
Pratt, M. C. et al. Effect of angiotensin converting enzyme inhibitors on erythropoietin concentrations in healthy volunteers. Br. J. Clin. Pharmacol. 34, 363–365 (1992).
Swenson, E. R. Carbonic anhydrase inhibitors and high altitude illnesses. Subcell. Biochem. 75, 361–386 (2014).
Stewart, S., Keates, A. K., Redfern, A. & McMurray, J. J. V. Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. 14, 654–664 (2017).
Stewart, S., McIntyre, K., Capewell, S. & McMurray, J. J. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. J. Am. Coll. Cardiol. 39, 760–766 (2002).
Hayward, J. M., Holmes, W. F. & Gooden, B. A. Cardiovascular responses in man to a stream of cold air. Cardiovasc. Res. 10, 691–696 (1976).
Westheim, A. et al. Haemodynamic and neurohumoral effects of cold pressor test in severe heart failure. Clin. Physiol. 12, 95–106 (1992).
Barnett, A. G., de Looper, M. & Fraser, J. F. The seasonality in heart failure deaths and total cardiovascular deaths. Aust. N. Z. J. Public Health 32, 408–413 (2008).
Moholdt, T. Excess mortality at Christmas due to cardiovascular disease in the HUNT study prospective population-based cohort in Norway. BMC Public Health 21, 549 (2021).
Schlagenhauf, P. et al. Sex and gender differences in travel-associated disease. Clin. Infect. Dis. 50, 826–832 (2010).
McIntosh, I. B., Power, K. G. & Reed, J. M. Prevalence, intensity, and sex differences in travel related stressors. J. Travel Med. 3, 96–102 (1996).
Taber, J. M., Leyva, B. & Persoskie, A. Why do people avoid medical care? A qualitative study using national data. J. Gen. Intern. Med. 30, 290–297 (2015).
Aerospace Medical Association. Medical considerations for airline travel: anemia (ASMA, 2021).
Roig, E. et al. Disabling angina pectoris with normal coronary arteries in patients undergoing long-term hemodialysis. Am. J. Med. 71, 431–434 (1981).
Brignole, M. et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur. Heart J. 34, 2281–2329 (2013).
Dubner, S. et al. ISHNE/EHRA expert consensus on remote monitoring of cardiovascular implantable electronic devices (CIEDs). Ann. Noninvasive Electrocardiol. 17, 36–56 (2012).
Slotwiner, D. et al. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm 12, e69–e100 (2015).
Simpson, C. et al. Canadian cardiovascular society consensus conference. Assessment of the cardiac patient for fitness to drive and fly – executive summary. Can. J. Cardiol. 20, 1313–1323 (2004).
Cassivi, S. D. et al. Safety of air travel in the immediate postoperative period after anatomic pulmonary resection. J. Thorac. Cardiovasc. Surg. 153, 1191–1196.e1 (2017).
MyLVAD Foundation. 10 Tips for traveling with an LVAD. MyLVAD https://www.mylvad.com/patients-caregivers/discuss-connect/forums/1048-10-tips-traveling-lvad (2011).
Kupper, N., Denollet, J., Widdershoven, J. & Kop, W. J. Cardiovascular reactivity to mental stress and mortality in patients with heart failure. JACC Heart Fail. 3, 373–382 (2015).
Strike, P. C. & Steptoe, A. A systematic review of mental stress-induced myocardial ischaemia. Eur. Heart J. 24, 690e703 (2003).
Mullens, W. et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21, 137–155 (2019).
Greenleaf, J. E., Rehrer, N. J., Mohler, S. R., Quach, D. T. & Evans, D. G. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? Sports Med. 34, 705–725 (2004).
Greenleaf, J. E., Shvartz, E., Kravik, S. & Keil, I. C. Fluid shifts and endocrine responses during chair rest and water immersion in man. J. Appl. Physiol. 48, 79–88 (1980).
Better, O. S. Impaired fluid and electrolyte balance in hot climates. Kidney Int. Suppl. 21, S97–S101 (1987).
Riddle, M. S. et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J. Travel Med. 24 (Suppl. 2), S57–S74 (2017).
Steffen, R., Hill, D. R. & DuPont, H. L. JAMA patient page. Traveler’s diarrhea. JAMA 313, 108 (2015).
Rosenstock, J. & Ferrannini, E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care 38, 1638–1642 (2015).
Fanola, C. L. et al. Incident heart failure and long-term risk for venous thromboembolism. J. Am. Coll. Cardiol. 75, 148–158 (2020).
Trujillo-Santos, A. J., Jiménez-Puente, A. & Perea-Milla, E. Association between long travel and venous thromboembolic disease: a systematic review and meta-analysis of case-control studies. Ann. Hematol. 87, 79–86 (2008).
Czuprynska, J. & Arya, R. Annotation: travel and thrombosis. Br. J. Haematol. 188, 838–843 (2020).
Cannegieter, S. C., Doggen, C. J., van Houwelingen, H. C. & Rosendaal, F. R. Travel-related venous thrombosis: results from a large population-based case control study (MEGA study). PLoS Med. 3, e307 (2006).
Kahn, S. R. et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141 (Suppl. 2), e195S–e226S (2012).
Xu, T. et al. Heart failure is associated with increased risk of long-term venous thromboembolism. Korean Circ. J. 51, 766–780 (2021).
Schreijer, A. J., Cannegieter, S. C., Doggen, C. J. & Rosendaal, F. R. The effect of flight-related behaviour on the risk of venous thrombosis after air travel. Br. J. Haematol. 144, 425–429 (2009).
Dusse, L. M. S., Silva, M. V. F., Freitas, L. G., Marcolino, M. S. & Carvalho, M. D. G. Economy class syndrome: what is it and who are the individuals at risk? Rev. Bras. Hematol. Hemoter. 39, 349–353 (2017).
Hitos, K., Cannon, M., Cannon, S., Garth, S. & Fletcher, J. P. Effect of leg exercises on popliteal venous blood flow during prolonged immobility of seated subjects: implications for prevention of travel-related deep vein thrombosis. J. Thromb. Haemost. 5, 1890–1895 (2007).
Clarke, M. J., Broderick, C., Hopewell, S., Juszczak, E. & Eisinga, A. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst. Rev. 9, CD004002 (2016).
Cesarone, M. R. et al. Venous thrombosis from air travel: the LONFLIT3 study–prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: a randomized trial. Angiology 53, 1–6 (2002).
Graf, J., Stüben, U. & Pump, S. In-flight medical emergencies. Dtsch. Arztebl Int. 109, 591–602 (2012).
Goodwin, T. In-flight medical emergencies: an overview. BMJ 321, 1338 (2000).
McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42, 3599–3726 (2021).
Seferovic, P. M. et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21, 1169–1186 (2019).
Kalantar-Zadeh, K. & Fouque, D. Nutritional management of chronic kidney disease. N. Engl. J. Med. 377, 1765–1776 (2017).
Hindricks, G. et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 42, 373–498 (2021); erratum 42, 507 (2021); erratum 42, 546–547 (2021).
Tasnim, S., Tang, C., Musini, V. M. & Wright, J. M. Effect of alcohol on blood pressure. Cochrane Database Syst. Rev. 7, CD012787 (2020).
Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity: culprit drugs, management and prevention. Drug Saf. 34, 821–837 (2011).
Blakely, K. M., Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity-an update: culprit drugs, prevention and management. Drug Saf. 42, 827–847 (2019).
US Food and Drug Administration. The Sun and your medicine (FDA, 2015).
Kolb, C. et al. Do airport metal detectors interfere with implantable pacemakers or cardioverter-defibrillators? J. Am. Coll. Cardiol. 41, 2054–2059 (2003).
Copperman, Y., Zarfati, D. & Laniado, S. The effect of metal detector gates on implanted permanent pacemakers. Pacing Clin. Electrophysiol. 11, 1386–1387 (1988).
Jilek, C. et al. Safety of screening procedures with hand-held metal detectors among patients with implanted cardiac rhythm devices: a cross-sectional analysis. Ann. Intern. Med. 155, 587–592 (2011).
Acknowledgements
This Review is the result of a cooperation under the umbrella of the Study Group 10 (heart failure) of the German Cardiac Society. S.v.H. has received research funding from the German Center for Cardiovascular Research (DZHK). T.K. has received research funding from the German Heart Research Foundation and is supported by the German Research Foundation (Clinical Research Unit KFO311). R.W. has received research support from the German Center for Cardiovascular Research (DZHK).
Author information
Authors and Affiliations
Contributions
S.v.H. wrote the article. All the authors researched data for the article, contributed to discussion of content, and reviewed and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
S.v.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, BRAHMS, Chugai, Grünenthal, Helsinn, Hexal, Novartis, Pharmacosmos, Respicardia, Roche, Servier, Sorin, and Vifor and has received research funding from Amgen, Boehringer Ingelheim and IMI. T.K. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Novartis, Pharmacosmos, and Vifor and has received research support from Vifor. P.R. has been a paid consultant for and/or received honoraria payments from Abbott, AstraZeneca, Bayer, BDI, Biotronik, Conventus Congressmanagement & Marketing GmbH, CTI GmbH, Daiichi-Sankyo, Deutsche Gesellschaft für Kardiologie, Diaplan, Edwards, Elisabeth-KH Essen, Heart Institute GmbH, Herzzentrum Leipzig, Kelcon, Medizinische Ausstellungs- und Werbegesellschaft Wien, Medtronic, Novartis and Vifor. R.W. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, BMS, Boehringer Ingelheim, CVRx, Daiichi, Medtronic, Novartis, Pfizer, Pharmacosmos and Servier. R.W. has received research support from Boehringer Ingelheim, Bundesministerium für Bildung und Forschung, Deutsche Forschungsgemeinschaft, European Union and Medtronic. G.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Berlin Chemie, Boehringer Ingelheim, Corvia, Impulse Dynamics, Novartis, Servier, Springer and Vifor. All other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks Biykem Bozkurt, Tiny Jaarsma and Simon Stewart for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
von Haehling, S., Birner, C., Dworatzek, E. et al. Travelling with heart failure: risk assessment and practical recommendations. Nat Rev Cardiol 19, 302–313 (2022). https://doi.org/10.1038/s41569-021-00643-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-021-00643-z
This article is cited by
-
Heart failure with preserved ejection fraction: diagnosis, risk assessment, and treatment
Clinical Research in Cardiology (2024)